Abstract
Renal cell carcinoma (RCC) is the second lethal urogenital malignancy with the increasing incidence and mortality in the world. Clear cell renal cell carcinoma (ccRCC) is one major subtype of RCC, which accounts for about 70 to 80% of all RCC cases. Although many innovative therapeutic options have emerged during the last few decades, the efficacy of these treatments for ccRCC patients is very limited. To date, the prognosis of patients with advanced or metastatic ccRCC is still poor. The 5-year survival rate of these patients remains less than 10%, which mainly attributes to the complexity and heterogeneity of the tumor microenvironment (TME). It has been demonstrated that long non-coding RNAs (lncRNAs) perform an indispensable role in the initiation and progression of various tumors. They mostly function as sponges for microRNAs (miRNAs) to regulate the expression of target genes, finally influence the growth, metastasis, apoptosis, drug resistance and TME of tumor cells. However, the role of lncRNA/miRNA/mRNA axis in the TME of ccRCC remains poorly understood. In this review, we summarized the biological function of lncRNA/miRNA/mRNA axis in the pathogenesis of ccRCC, then discussed how lncRNA/miRNA/mRNA axis regulate the TME, finally highlighted their potential application as novel biomarkers and therapeutic targets for ccRCC.
Keywords: Clear cell renal cell carcinoma, lncRNA, miRNA, Regulatory network, TME
Introduction
Renal cell carcinoma (RCC) is one of the most lethal urogenital malignancies with an increasing morbidity and mortality in the world [1]. According to the global cancer statistics report, RCC is the ninth most frequently diagnosed cancer in men, which has approximately 432,000 new cases and 180,000 deaths in 2020 [2]. The major histological subtype of RCC is clear cell RCC (ccRCC), which accounts for about 75% of all RCC cases, followed by papillary RCC (pRCC) and chromophobe RCC (chRCC) (representing ~ 15–20% and ~ 5% of RCC, respectively) [3]. Due to the high rate of recurrence or metastasis and difficulties in the early diagnosis, it is conceivable that the prognosis of patients with ccRCC is still very poor. Until now, radical nephrectomy remains the best treatment and crucial intervention for local ccRCC. However, up to one-third of patients are initially diagnosed with metastatic ccRCC, at which point they are no longer suitable for surgical treatment [4, 5]. Moreover, roughly 20 to 30% of patients will relapse within 2 years after radical nephrectomy, and almost all of them are extremely resistant to both chemotherapeutics and radiation therapy [4, 6]. During the last few decades, owing to the rapid development of targeted and immunological drugs, the therapeutic options for ccRCC patients have been greatly expanded. Unfortunately, the efficacy of these treatments for patients with advanced or metastatic ccRCC is still very limited, which mainly attributes to the complexity and heterogeneity of tumor microenvironment (TME). Therefore, it is extremely urgent to understand the molecular mechanism in the tumorigenesis and progression of ccRCC, especially its dynamic TME, which may be helpful to discover novel effective biomarkers and therapeutic targets of ccRCC.
The carcinogenesis of ccRCC is a complicated biological process, which is closely associated with gene mutation, genome instability, and epigenetic disorder [7]. Some important genes are well known to participate in the occurrence and development of ccRCC, for instance, the von Hippel-Lindau (VHL) gene. It has been demonstrated that VHL is mutated in ccRCC, and its mutation leads to an activation of hypoxia-inducible factor (HIF), thereby inducing the expression alteration of angiogenic factors including vascular endothelial growth factor (VEGF) and platelet-derived growth factor (PDGF) [8]. Moreover, VHL mutation also activates the mammalian target of rapamycin (mTOR) signaling pathway, which in turn upregulates HIF and angiogenesis, subsequently accelerating the progression of ccRCC [9]. Consequently, drugs directly target VEGF/VEGF receptor (VEGFR), PDGF/PDGF receptor (PDGFR), and the mTOR pathway have been dramatically developed [9]. Nevertheless, there are no credible diagnostic and prognostic biomarkers for ccRCC that have yet been applied into clinical practice. In recent years, the epigenetics of ccRCC, including non-coding RNAs (ncRNAs), have greatly attracted the attention of researchers. A large amount of ncRNAs are found to be aberrantly expressed in diverse tumors, indicating ncRNAs play critical roles in tumorigenesis and development [10–12]. Thus, further identifying and understanding the function of ncRNAs may contribute to the early diagnosis and treatment of ccRCC.
NcRNAs can be classified into long ncRNAs (lncRNAs) and small ncRNAs (sncRNAs) based on their length [13]. As for lncRNAs, there are more than 200 nucleotides in their molecular sequences, but they are not responsible for protein-coding [14]. LncRNAs have been found to be localized both in the nuclear and cytoplasmic compartments. Studies have demonstrated that lncRNAs can influence many cellular processes depending on their location. In the nucleus, lncRNAs can regulate gene expression by recruiting chromatin-modifying complexes, or by changing the spatial conformation of chromosomes [15]. Moreover, they can also influence the efficiency of transcriptional factors or pre-mRNA spliceosomes to modulate mRNA expression. In the cytoplasm, lncRNAs can regulate transcription by influencing mRNA stability, mRNA translation, or miRNA binding [14]. Additionally, few lncRNAs can also be translated into biological active small peptides [16]. In contrast to lncRNAs, sncRNAs are a series of RNAs with about 19 to 25 nucleotides in length. MicroRNAs (miRNAs) are one subclass of sncRNAs, which are small single-stranded RNA molecules and exert their functions exclusively at the post-transcriptional level [13]. MiRNAs can induce the transcriptional silence of target genes by binding to their 3’untranslated region (3’UTR) sequences [17]. More importantly, a growing body of studies have discovered that miRNAs have a close interaction with lncRNAs. LncRNAs can act as sponges to interact with miRNAs, and also have an effect on their production and degradation, eventually leading to the alteration of target genes [18]. In addition, both lncRNAs and miRNAs are known to be involved in cell proliferation, apoptosis, metastasis, and tumor microenvironment (TME) [19, 20]. Therefore, regulation of aberrant lncRNAs and miRNAs may alleviate the initiation and development of various tumors. Although the current knowledge of lncRNAs and miRNAs is still inadequate, an increasing number of studies have emphasized their indispensable role in tumorigenesis. In this review, we aim to summarize the latest advances regarding lncRNA/miRNA/mRNA axis in the pathogenesis of ccRCC, then discuss how lncRNA/miRNA/mRNA axis regulate TME, and finally highlight their potential application as novel biomarkers and therapeutic targets for ccRCC.
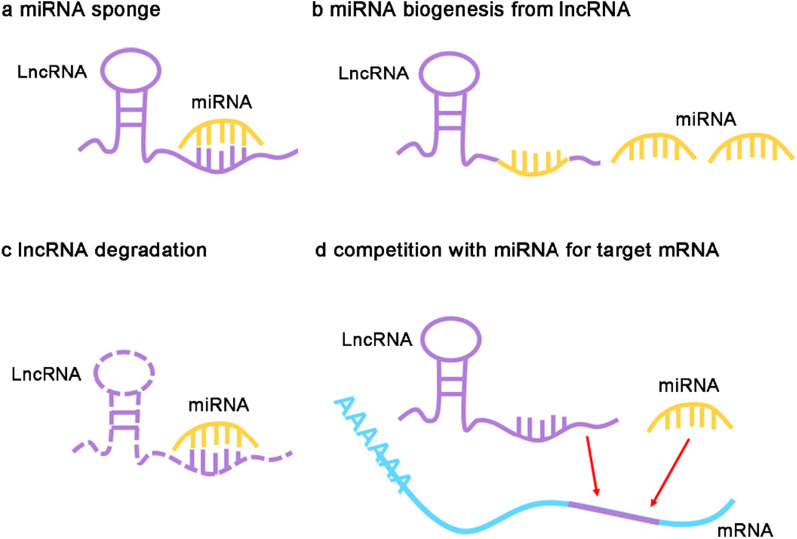
The regulatory mode between lncRNA and miRNA
Based on the previous reports, the interaction between lncRNA and miRNA can be summarized as four regulatory modes, namely sponges for miRNA, production of miRNA, degradation of lncRNA, and competition with miRNA for target genes (Fig. 1). To be specific, lncRNAs can act as miRNA sponges, which directly target miRNAs to suppress the combination between miRNAs and their target genes, subsequently leading to the expression changes of target genes. Up to now, most studies have been predominantly focused on this regulatory mode, which can be defined as lncRNA/miRNA/mRNA axis [21, 22]. In addition to serving as miRNA sponges, lncRNAs are also responsible for the biogenesis of miRNAs because some nucleotides in the lncRNA sequences were the same as miRNAs. In this process, lncRNAs can be cleaved into miRNAs by Dicer and/or Drosha, then alter the transcriptional expression of downstream genes [23]. In contrast, miRNAs also can induce the degradation of lncRNAs through binding with lncRNAs, and eventually repress the mRNA expression of downstream genes [24]. Additionally, lncRNAs can directly interact with the target genes of miRNAs, which restrain the binding between miRNAs and their target genes, and finally affect the activity of miRNAs [25, 26].
Fig. 1.
The regulatory mode between lncRNA and miRNA. a LncRNA acts as a sponge for miRNA, which prohibits the binding between miRNA and its targets. b LncRNA can be digested to produce miRNA and influence the transcriptional expression of downstream genes. c MiRNA can induce the degradation of lncRNA via binding to lncRNAs, and eventually suppress the mRNA levels of target genes. d LncRNA can competitively interact with the target genes of miRNA
Biological role of lncRNA/miRNA/mRNA axis in ccRCC
LncRNA/miRNA/mRNA axis plays a vital role in the initiation and development of different carcinomas, such as ccRCC. Studies have shown that some oncogenic miRNAs are upregulated in ccRCC, while some tumor suppressor miRNAs are downregulated. In that case, lncRNAs combine with oncogenic miRNAs will result in tumor inhibition, and those interact with suppressor miRNAs will influence the tumor in reverse.
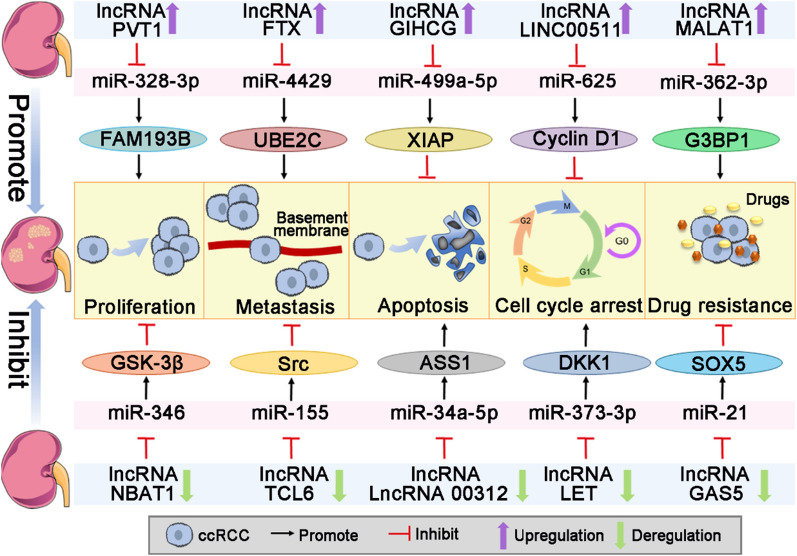
Role in promoting tumor progression
Previous studies have demonstrated that lncRNA/miRNA/mRNA axis is critical in the progression of ccRCC, which can facilitate cell proliferation, migration, invasion, cell cycle and inhibit apoptosis (Fig. 2). Xie et al. have illustrated that lncRNA PVT1 could promote ccRCC cell proliferation by directly targeting miR-328-3p, then induce the expression of family with sequence similarity 193 member B (FAM193B), and activate the PI3K/AKT and MAPK/ERK signal pathways [27]. PI3K/AKT and MAPK/ERK pathways are crucial for cell proliferation, metastasis, and angiogenesis, and they have been found to be dysregulated in ccRCC [28]. On the other hand, Chen et al. have discovered that PVT1 was remarkably upregulated in ccRCC tissues based on the high-throughput analysis, and its upregulation was closely associated with the lower overall survival (OS) rate of ccRCC patients [29]. Furthermore, PVT1 also functioned as a competing endogenous RNA (ceRNA) of miR-145-5p to increase the expression of T-box transcription factor 15 (TBX15) in ccRCC cells [30]. TBX15 expression is positively related to the poor prognosis of ccRCC patients, who have a shorter OS and disease-free survival (DFS) [30]. Overexpression of PVT1 could promote the migration and invasion of ccRCC cells via inhibiting miR-16-5p [31].
Fig. 2.
Role of lncRNA/miRNA/mRNA axis in the progression of ccRCC. LncRNA/miRNA/mRNA axis plays an important role in promoting or inhibiting the progression of ccRCC, which has an effect on cell proliferation, metastasis, apoptosis, cell cycle and drug resistance
LncRNA MALAT1 expression is markedly increased in ccRCC tissues than that in the normal controls, and its high expression promotes ccRCC cell proliferation and invasion by sponging miR-200s, thereby inducing the expression of zinc finger E-box-binding homeobox 2 (ZEB2) [10]. ZEB2 acts as a DNA-binding transcriptional repressor, which is elevated in ccRCC and negatively correlated with the tumor metastasis and prognosis [32]. Chen et al. have reported that ZEB2 could be regulated by miR-30a-5p and miR-206, which influenced the proliferation, migration and invasion of ccRCC cells [33, 34]. Notably, the high level of MALAT1 is also associated with the worse prognosis of ccRCC patients [35]. Besides, MALAT1 could competitively sponge miR-194-5p to activate activin A receptor type 2B (ACVR2B), which resulted in the increase of cell proliferation and suppression of apoptosis [36]. The promoting effect of ACVR2B on ccRCC progression is dependent on the activation of activin A, which can be activated by the dimerization of activin receptor types I and II [36]. Additionally, silencing of MALAT1 in ccRCC cells could enhance the sensitivity to sunitinib by modulating miR-362-3p/Ras-GTPase-activating SH3-domain-binding protein 1 (G3BP1) axis [37]. G3BP1 is important for the progression and metastasis of ccRCC, which can facilitate cell proliferation, migration and invasion by regulating IL-6/G3BP1/STAT3 signaling pathway [38]. Furthermore, lncRNA DARS-AS1 can upregulate the level of aspartyl-tRNA synthetase (DARS) through sequestering miR-194-5p, then contribute to the malignant progression of ccRCC [39]. Zhu et al. have found that lncRNA GIHCG could sponge miR-499a-5p to boost the expression of X-linked inhibitor of apoptosis protein (XIAP), thereby promoting the proliferation, migration and cell cycle of ccRCC cells and inhibiting apoptosis [40]. In addition, high expression of lncRNA LINC00511 could accelerate ccRCC cell proliferation and inhibit cell cycle arrest at G0-G1 by modulating miR-625/Cyclin D1 signaling [41]. A recent study demonstrated that lncRNA FTX is abnormally upregulated in ccRCC, which promotes the viability, migration and invasion of ccRCC by sponging miR-4429 to induce the expression of ubiquitin-mediated proteolysis genes (UBE2C) [42]. To conclude, numerous lncRNAs have a positive effect on the progression of ccRCC through regulating different miRNA/mRNA axis (Table 1).
Table 1.
Role of lncRNA/miRNA/mRNA axis in promoting ccRCC progression
| LncRNA | MiRNA | Gene | Biological behavior of ccRCC | Types of ccRCC tissues and cell lines | Refs. |
|---|---|---|---|---|---|
| PVT1 |
miR-328-3p, miR-145-5p, miR-16-5p, miR-200s |
FAM193B, TBX15, BMI1, ZEB1, ZEB2 |
Proliferation, migration, invasion, apoptosis, cell cycle, EMTa |
Tissues: 210 NTb Cells: 769-P, UMRC6, RCCJF, A498, ACHN, 786-O, OS-RC-2, Caki-1, HEK-293T, HK-2 |
[27, 30, 31, 43] |
| HILAR |
miR-613, miR-206, miR-1-1-3p |
Jagged1, CXCR4 |
Proliferation, migration, invasion, EMT | Cells: ACHN, Caki-1, SN12-PM6 | [44] |
| TUG1 |
miR-299-3p, miR-9, miR-31-5p, miR-196a |
VEGFR, YAP, FLOT1, AKT, ERK, JNK |
Proliferation, migration, invasion, apoptosis, autophagy, EMT |
Tissues: 99 NT Cells: ACHN, OS-RC-2, 786-O, 769-P, A498, A704, HEK-293, HK-2 |
[45–48] |
| ITGB2-AS1 | miR-328-5p | HMGA1 | Proliferation, apoptosis |
Tissues: 33 NT Cells: OS-RC-2, SW839, A498, SN12-PM6, Caki-1, HK-2 |
[49] |
| LUCAT1 |
miR-495-3p, miR-375 |
SATB1, YAP1 |
Proliferation, migration, invasion |
Tissues: 126 NT Cells: 786-O, Caki-1, A498, 769-P, ACHN, HK-2 |
[50, 51] |
| MEG8 | miR-495-3p | G3BP1 | Proliferation, migration, invasion |
Tissues: 62 NT Cells: A498, Caki-1,786-O, 769-P, ACHN |
[52] |
| RP11-436H11.5 | miR-335-5p | BCL-W | Proliferation, invasion |
Tissues: 20 NT Cells: A498, 786-O, OS-RC-2 |
[53] |
| PCED1B-AS1 | miR-484 | ZEB1 | Proliferation, migration, EMT |
Tissues: 40 NT Cells: 786-O, A498, ACHN, Caki-1, HK-2 |
[54] |
| CRNDE | miR-136-5p |
N-Cadherin, Vimentin |
Proliferation, migration, invasion, EMT |
Tissues: 45 NT Cells: A498, ACHN |
[55] |
| DARS-AS1 | miR-194-5p | DARS | Proliferation, apoptosis |
Tissues: 70 NT Cells: ClearCa-1, HH332, Caki-1, KMRC-2, KN-41, HK-2 |
[39] |
| LINC01094 |
miR-224-5p, miR-184 |
CHSY1, SLC2A3 |
Proliferation, migration, EMT |
Tissues: 56 NT Cells: ACHN, 769-P, Caki-1, 786-O, HK-2 |
[56, 57] |
| LINC02747 | miR-608 | TFE3 | Proliferation |
Tissues: 70 NT Cells: 786-O, ACHN, Caki-1, Caki-2 |
[58] |
| LINC00973 | miR-7109-3p | Siglec-15 | Immune escape |
Tissues: 100 NT Cells: 786-O, 769-P, A704, A498, ACNH, Caki-1, Caki-2, RCC4, HK-2 |
[59] |
| LINC01426 | miR-423-5p | FOXM1 | Proliferation, migration | Cells: A498, ACHN, Caki-1, 786-O, HEK-293T, HK-2 | [60] |
| LINC00511 | miR-625 | CCND1 | Proliferation, migration, invasion, apoptosis, cell cycle |
Tissues: 49 NT Cells: A498, 786-O, ACHN, Caki-2, HK-2 |
[41] |
| HOXA11‐AS | miR-146b-5p | MMP16 | Proliferation, invasion, apoptosis, EMT |
Tissues: 52 NT Cells: ACHN, 786-O, A498, OS-RC-2, HK-2 |
[61] |
| CDKN2B-AS1 | miR-141 |
Cyclin D1, Cyclin D2 |
Proliferation, migration, invasion, apoptosis | Cells: RPTEC, ACHN, Caki-1 | [62] |
| DNAJC3-AS1 | miR-27a-3p | PRDM14 | Proliferation, migration, invasion, apoptosis |
Tissues: 30 NT Cells: 769-P, ACHN, Caki-1, 786-O, HK-2 |
[63] |
| FGD5-AS1 | miR-5590-3p | ERK/AKT | Proliferation, migration, invasion, EMT |
Tissues: 28 NT Cells: 786-O, ACHN, SN12-PM6, HK-2 |
[64] |
| HCG18 | miR-152-3p | RAB14 | Proliferation, migration, invasion |
Tissues: 32 NT Cells: Caki-1, 786-O, 769-P, ACHN, HK-2 |
[65] |
| SNHG12 |
miR-200c-5p, miR-30a-3p, miR-129-5p |
COL11A1, RUNX2, WNT2, IGF-1R, MDM4 |
Proliferation, invasion, apoptosis, cell cycle |
Tissues: 148 NT Cells: OS-RC-2, 786-O, Caki-1, Caki-2, A498, ACHN, 769-P, HK-2 |
[66–68] |
| SNHG5 |
miR-205-5p, miR-363-3p |
ZEB1, Twist |
Proliferation, migration, invasion, apoptosis, EMT |
Tissues: 20 NT Cells: ACHN, 786-O, A498, SN12-PM6, SW13, Caki-1, HK-2 |
[69, 70] |
| PCAT1 |
miR-656, miR-539 |
YAP | Proliferation, migration, invasion |
Tissues: 85 NT Cells: 786-O, Caki-2, 769-P, OS-RC-2, ACHN, HK-2 |
[71] |
| H19 | miR-29a-3p | E2F1 | Proliferation, migration, invasion |
Tissues: 30 NT Cell: 786-O |
[72] |
| NNT-AS1 | miR-137 | Y-box | Proliferation, migration and invasion |
Tissues: 40 NT Cells: 786-O, OS-RC-2, A498, Caki-1, HEK-293T |
[73] |
| HCP5 |
miR-214-3p, miR-140-5p |
MAPK1, IGF1R |
Proliferation, migration, invasion, apoptosis, cell cycle |
Tissues: 142 NT Cells: 786-O, Caki-1, Caki-2, ACHN, A498, 769-P, OS-RC-2, HEK-293T, HK-2 |
[74, 75] |
| MIR4435-2HG | miR-513a-5p | KLF6 | Proliferation, migration, invasion |
Tissues: 40 NT Cells: 786-O, 769-P, Caki-1, Caki-2, ACHN, A498, HK-2, HEK-293T |
[76] |
| PCGEM1 | miR-433-3p | FGF2 | Proliferation, migration, apoptosis |
Tissues: 47 NT Cells: OS-RC-2, ACHN, A498, 786-O |
[77] |
| MALAT1 |
miR-200s, miR-194-5p, miR‐203, miR-205, miR-429, miR-182-5p, miR-1271-5p |
ZEB2, ACVR2B, BIRC5, KIAA1324 |
Proliferation, migration, invasion, apoptosis, cell cycle |
Tissues: 531 NT Cells: 786-O, ACHN, SN12-PM6, OS-RC-2, Caki-2, Caki-1, A498, HK-2 |
[10, 36, 78–82] |
| RCAT1 | miR-214-5p | E2F2 | Proliferation, migration, invasion |
Tissues: 52 NT Cells: ACHN, 786-O, 769-P, Caki-1, A498, HK-2 |
[83] |
| MSC‐AS1 | miR-3924 | WNT5A | Proliferation, migration |
Tissues: 27NT Cells: 786-O, 769-P, A498, Caki-1, HK-2 |
[84] |
| ROR | miR-206 | VEGF | Proliferation, migration and invasion |
Tissues: 36 NT Cells: Caki-1, Caki-2, HK-2 |
[85] |
| ZFAS1 | miR-10a | SKA1 | Proliferation, migration and invasion |
Tissues: 20 NT Cells: 786-O, Caki-1, ACHN, HEK-293T, HK-2 |
[86] |
| SNHG3 |
miR-139-5p, miR-10b-5p |
TOP2A; BIRC5 | Proliferation, migration, invasion |
Tissues: 70 NT Cells: A498, ACHN, Caki-1, 786-O, HK-2 |
[87, 88] |
| SNHG17 | miR-328-3p | H2AX | Proliferation, migration, invasion, apoptosis, cell cycle |
Tissues: 84 NT Cells: 786-O, ACHN, Caki-1, 769-P, HK-2 |
[89] |
| UCA1 |
miR-495, miR-182-5p |
EZH2, DLL4 |
Proliferation, migration, cell cycle |
Tissues: 130 NT Cells: 786-O, ACHN, Caki-1, Caki-2, HEK-293T, HK-2 |
[90, 91] |
| LOXL1-AS1 | miR-589-5p | CBX5 | Proliferation, migration |
Tissues: 60 NT Cells: 786-O, A498, 769-P, HEK-293 |
[92] |
| HIF1A-AS2 | miR-130a-5p | ERBB2 | Proliferation, migration, invasion, apoptosis, cell cycle |
Tissues: 42 NT Cells: ACHN, OSRC-2, 786-O, Caki-1, HK-2 |
[93] |
| HOTTIP | miR-615-3p | IGF-2 | Proliferation, migration, invasion, apoptosis, cell cycle |
Tissues: 57 NT Cells: A498, 786-O, Caki-1, Caki-2, ACHN, HK-2, HEK-293T |
[94] |
| LINC00641 | miR-340-5p | c-Myc, CyclinD1, MMP-2 | Proliferation and invasion |
Tissues: 48 NT Cells: GRC-1, 786-O, SN12-PM6, A498, ACHN, HK-2 |
[95] |
| SNHG1 |
miR-129-3p, miR-137 miR-103a |
STAT3, PD-L1 HMGA2 |
Proliferation, migration, invasion, cell cycle, apoptosis, EMT |
Tissues: 60 NT Cells: ACHN, A498, 786-O, Caki-1, HK-2 |
[96–98] |
| LINC01133 | miR-30b-5p | Rab-3D | Proliferation, migration, invasion |
Tissues: 34 NT Cells: ACHN, A498, 786-O, SN12-PM6, HK-2 |
[99] |
| HOTAIR |
miR-217, miR-138, miR-200c, miR-204, miR-124, miR-203, miR-141 |
HIF-1α, AXL, EZH2, VIM, ZEB1, ADAM9, CCND2, VEGFA, ZEB2, ST8SIA4; |
Proliferation, migration, invasion, apoptosis, cell cycle, EMT |
Tissues: 54 NT Cells: ACHN, 786-O, 769-P, A498, Caki-1, HK-2 |
[100–104] |
| SBF2-AS1 | miR-338-3p | ETS1 | Proliferation, migration, invasion, apoptosis, autophagy |
Tissues: 46 NT Cells: Caki-1, UT14, UT16, UT33a, 768-O, HK-2 |
[105] |
| MIAT | miR-29c | LOXL2 | Proliferation, migration, invasion |
Tissues: 45 NT Cells: Caki-1, ACHN, 786-O, HK-2 |
[106] |
| ARAP1-AS1 | miR-361-3p | PGF | Proliferation, migration, apoptosis |
Tissues: 16 NT Cells: HK-2, Caki-1, A498 |
[107] |
| MIR155HG |
miR-155-5p, miR-155-3p |
MMP2, MMP9 | Proliferation, migration, invasion | Cells: HKC-5, LoMet-ccRCC, 786-O, A498, Caki-1, HK-2 | [108] |
| DUXAP8 | miR-126 | CED-9 | Proliferation, invasion | Cells: A498, 786-O | [109] |
| SNHG16 | miR-1303-p | STARD9 | Proliferation, apoptosis |
Tissues: 45 NT Cells: A498, 786-O, Caki-1, OSRC-2, HK-2 |
[110] |
| DLX6-AS1 | miR-26a | PTEN | Proliferation, apoptosis |
Tissues: 52 NT Cells: A498, ACHN, Caki-1, Caki-2, 786-O, G401, HK-2 |
[111] |
| EMBP1 | miR-9-5p | KLF4, NANOG, CCNE2 | Proliferation, migration, invasion, EMT |
Tissues: 65 NT Cells: ACHN, Caki-1, HK-2 |
[112] |
| LINC02738 | miR-20b | SOX4 | Proliferation, invasion, apoptosis |
Tissues: 50 NT Cells: ACHN, 786-O, OS-RC-2, Caki-2, HK-2 |
[113] |
| GAPLINC | miR-135b-5p | CSF1 | Proliferation, migration | Cells: A498, OSRC-2, ACHN, 786-O, Caki-1, HK-2 | [114] |
| SNHG4 | miR-204-5p | RUNX2 | Proliferation, migration, invasion, apoptosis |
Tissues: 99 NT Cells: Caki-1, Caki-2, ACHN, 786-O, 769-P, HK-2 |
[115] |
| TTN-AS1 | miR-195 | Cyclin D1 | Proliferation, cell cycle |
Tissues: 145 NT Cells: ACHN, 786-O, SN12-PM6, HK-2 |
[116] |
| ZFPM2-AS1 | miR-130a-3p | ESCO2 | Proliferation, migration, invasion, apoptosis |
Tissues: 60 NT Cells: 786-O, KETR3, G401, HK-2 |
[117] |
| SLC16A1-AS1 | miR-143-3p | SLC7A11 | Proliferation, migration, invasion | Cells: 786-O, A498, Caki-1, HK-2 | [118] |
| DLEU2 | miR-30a-5p | ZEB2 | Proliferation, invasion |
Tissues: 40 NT Cells: ACHN, Caki-1, 769-P, 786-O, HK-2 |
[33] |
| LINC01232 | miR-204-5p | RAB22A | Proliferation, migration, invasion |
Tissues: 122 NT Cells: Caki-1, A498, KN-41, 786-O, ClearCa-1, HK-2 |
[119] |
| GIHCG | miR-499a-5p | XIAP | Proliferation, migration, apoptosis, cell cycle | Cells: HK-2, Caki-1, 786-O, A498, SN12C-PM6 | [40] |
| CYTOR | miR-136-5p | MAT2B | Proliferation, invasion, apoptosis | Cells: 786-O, Caki-1 | [120] |
| CASC19 | miR-532 | ETS1 | Proliferation, migration, apoptosis |
Tissues: 51 NT Cells: Caki-1, A498,786-O |
[121] |
| FTX | miR-4429 | UBE2C | Proliferation, migration, invasion, cell cycle |
Tissues: 51 NT Cells: A498, A704, SN12C, 769-P |
[42] |
aEpithelial-Mesenchymal Transition
bPaired tumor and adjacent tissues
Role in inhibiting tumor progression
Several studies have revealed that lncRNAs severed as a suppressive factor for the development of ccRCC (Fig. 2). Ye et al. reported that lncRNA LET was downregulated in ccRCC tissues and cells, which mediated the tumor suppression by directly binding with miR-373-3p to reduce the levels of dickkopf-1 (DKK1) and tissue inhibitor of metalloproteinase-2 (TIMP2) [122]. Overexpression of LET could repress cell cycle and induce apoptosis of ccRCC cells in vitro, and inhibit ccRCC tumor growth in vivo [122]. DKK1 is a member of the dickkopf family, which can inhibit Wnt signaling and regulate immune cells in the tumor microenvironment [123]. Wnt signal pathway plays a crucial role in embryonic development and regulates nephrogenesis in mesenchymal cells [124]. TIMP2 is a member of the TIMP family, which is a natural inhibitor of the matrix metalloproteinases and directly suppresses tumor metastasis by degrading extracellular matrix and basal membrane [125]. Moreover, TIMP2 is downregulated in ccRCC and inhibits the proliferation, migration and invasion of ccRCC cells [126].
LncRNA TCL6 level has been found to be decreased in ccRCC tissues, which inhibited ccRCC metastasis via interacting with miR-155 to influence Src/Akt pathway [12]. The Src/Akt pathway participates in the carcinogenesis and development of ccRCC, whose activation contributes to the malignant phenotypes and tumor progression of ccRCC [127]. Zeng et al. reported that lncRNA 00312 was remarkably downregulated in ccRCC tissues and cell lines compared to the normal controls, which was significantly correlated with the unfavorable prognosis, including tumor size, pathological grade and tumor-node-metastasis (TNM) stage [128]. Additionally, lncRNA 00312 could also act as a sponge of miR-34a-5p to modulate argininosuccinate synthetase 1 (ASS1) expression, thereby promoting cell apoptosis and alleviating the development of ccRCC [128]. LncRNA NBAT1 has been confirmed that it was significantly decreased in ccRCC cells, which could suppress cell proliferation and metastasis through NBAT1/miR-346/glycogen synthase kinase-3β (GSK-3β) axis [11]. Moreover, miR-346 increase or GSK-3β silencing in ccRCC cells could reverse NBAT1-mediated inhibitory effect on cell proliferation, migration, and invasion [11]. The binding of lncRNA GAS5 to miR-21 upregulates the expression of sex-determining region Y-box protein 5 (SOX5), which in turn increases the sorafenib sensitivity of ccRCC [129]. Thus, in the lncRNA/miRNA/mRNA axis, lncRNAs bind to oncogenic miRNAs act as suppressors for ccRCC progression (Table 2).
Table 2.
Role of lncRNA/miRNA/mRNA axis in inhibiting ccRCC progression
| LncRNA | MiRNA | Gene | Biological behavior of ccRCC | Samples | Refs. |
|---|---|---|---|---|---|
| LET | miR-373-3p | DKK1, TIMP2 | Proliferation, apoptosis, cell cycle | Tissues: 16 NTa Cells: Caki-1, 786-O, 769-P, HEK-293T | [122] |
| TCL6 | miR-155 | Src | Proliferation, migration, invasion, apoptosis, cell cycle, EMTb | Cells: Caki-1, 786-O, HK-2 | [12] |
| LncRNA 00312 | miR-34a-5p | ASS1 | Proliferation, invasion, apoptosis | Tissues: 47 NT Cells: A498, ACHN, 786-O, 769-P, HK-2 | [128] |
| NBAT1 | miR-346 | GSK-3β | Proliferation, migration, invasion | Cells: 786-O, ACHN, Caki-1, Caki-2, HK-2 | [11] |
| PENG | miR-15b | PDZK1 | Proliferation | Tissues: 90 NT Cells: ACHN, 769-P, HEK-293 | [130] |
| MEG3 | miR-7 | RASL11B | Proliferation, migration, invasion, cell cycle, apoptosis | Tissues: 72 NT Cells: A498, 786-O, HK-2 | [131] |
| LINC01939 | miR-154 | Notch | Proliferation, migration, apoptosis | Tissues: 18 NT Cells: ACHN, Caki-1 | [132] |
| ENTPD3-AS1 | miR-155-5p | HIF-1α | Proliferation, migration | Tissues: 105 NT Cells: 786-O, A498, 769-P, ACHN, OS-RC-2 | [133] |
| XIST | miR-106b-5p | P21 | Proliferation, cell cycle | Tissues: 50 NT Cells: ACHN, Caki-1, Caki-2, 786-O, HK-2 | [134] |
| ASB16-AS1 | miR-185-5p, miR-214-3p | LARP1 | Proliferation, migration, invasion | Tissues: 42 NT Cells: A498, 786-O, 769-P, Caki-1, OS-RC-2, ACHN, HEK-293T, HK-2 | [135] |
| COL18A1-AS1 | miR-1286 | KLF12 | Proliferation, migration, invasion | Tissues: 50 NT Cells: ACHN, A498, Caki-1, OS-RC-2, 786-O, HK-2 | [136] |
aPaired tumor and adjacent tissues
bEpithelial-Mesenchymal Transition
Clinical significance of lncRNAs and miRNAs
To date, effective biomarkers for the early diagnosis and prognosis of ccRCC are still scarce in the clinic. Biomarkers, especially in the serum, have attracted great attention for predicting the initiation and development of ccRCC, because they are easy to obtain and assess. Therefore, identification of valuable biomarkers may resolve the difficulties in diagnosis and therapy for ccRCC.
Recent studies have indicated that lncRNAs are potential diagnostic and prognostic biomarkers for ccRCC (Table 3). He et al. reported that lncRNA GIHCG was markedly upregulated in the tissues and serums of ccRCC patients when compared to the healthy control group (AUC = 0.886, 95% CI: 0.812–0.959), with a sensitivity and specificity of 80.7% and 84.8%, respectively. Moreover, the high level of GIHCG in serum was positively correlated with the advanced TNM stages (P = 0.028), Fuhrman grades (P = 0.032), and a worse OS (P = 0.038) [137]. A recent study has demonstrated that the combination of five lncRNAs (LET, PVT1, PANDAR, PTENP1 and LINC00963) could discriminate ccRCC patients from normal controls, with a high specificity of 88.9% and a sensitivity of 79.2%; this finding included 71 ccRCC patients, 8 patients with benign renal tumors, and 62 healthy controls [138]. Tissue lncRNA OTUD6B-AS1 was significantly downregulated in ccRCC patients and exhibited obvious discrimination in the diagnosis (AUC = 0.792, 95% CI: 0.715–0.870) with a sensitivity of 77.3% and specificity of 81.4% [139]. The expression of lncRNA CADM1-AS1 was decreased in ccRCC tissues, and its downregulation was positively related to the AJCC stage (P = 0.039) and lower survival rate of ccRCC patients (P < 0.05). Furthermore, a multivariate analysis found that CADM1-AS1 was an independent prognostic factor for OS (HR = 0.211, 95% CI: 0.088–0.504) [140]. In the metastatic ccRCC patients, lncRNA PGM5-AS1 was reduced, and exerted as an independent prognostic predictor for OS (HR = 2.897, 95% CI: 1.275–4.387) and DFS (HR = 2.875, 95% CI: 1.185–4.462) [141]. LncRNA TCL6 levels in tissues were decreased in ccRCC, which were notably associated with the tumor stages, distant and lymphatic metastasis. Additionally, TCL6 is an independent predictor for Fuhrman grade of ccRCC patients (HR = 4.05, 95% CI: 1.08–15.17) [142].
Table 3.
Potential lncRNAs and miRNAs biomarkers in ccRCC
| Samples | NcRNAs | Sensitivity (%) | Specificity (%) | Refs. | |
|---|---|---|---|---|---|
| Tissue | LncRNA | APOC1P1 | 73.3 | 93.3 | [149] |
| OTUD6B-AS1 | 77.3 | 81.4 | [139] | ||
| ZNF180-2 | 90.0 | 55.9 | [150] | ||
| FZD1-2 | 85.5 | 94.2 | [151] | ||
| BMP2-2 | 85.5 | 100.0 | [151] | ||
| SPAM1-6 | 83.6 | 94.2 | [151] | ||
| ITPR2-3 | 90.9 | 96.2 | [151] | ||
| CPN2-1 | 90.9 | 98.1 | [151] | ||
| TTC34-3 | 98.1 | 96.4 | [151] | ||
| ACACA-1 | 94.2 | 100.0 | [151] | ||
| LCP2-2 | 98.1 | 89.1 | [151] | ||
| FOXG1-2 | 96.2 | 89.1 | [151] | ||
| RP3-368B9.1.1-1 | 86.5 | 94.5 | [151] | ||
| SLC30A4-1 | 90.9 | 96.2 | [151] | ||
| Fer1L4 | 73.2 | 95.5 | [152] | ||
| miRNA | Combination of miR-224-5p, miR-34b-3p and miR-182-5p | 80.3 | 66.3 | [153] | |
| miRNA-135a-5p | 45.5 | 81.1 | [154] | ||
| miR-720 | 80.0 | 100.0 | [155] | ||
| miR-129-3p | 75.9 | 62.1 | [156] | ||
| miR-182-5p | 90.0 | 97.0 | [81] | ||
| Combination of miR-21 and miR-194 | 80.0 | 97.5 | [157] | ||
| miR-142-3p | 62.0 | 56.0 | [158] | ||
| miR-21 | 90.0 | 83.0 | [147] | ||
| Combination of miR-10b, miR-139-5p, miR-130b and miR-199b | 76.0 | 100.0 | [159] | ||
| Serum | LncRNA | LET | 70.8 | 59.3 | [138] |
| LINC00887 | 71.1 | 89.9 | [160] | ||
| PVT1 | 70.8 | 63.0 | [138] | ||
| PANDAR | 75.0 | 63.0 | [138] | ||
| PTENP1 | 79.2 | 77.8 | [138] | ||
| Linc00963 | 83.3 | 66.7 | [138] | ||
| GIHCG | 87.0 | 84.8 | [137] | ||
| miRNA | Combination of miR-378 and miR-210 | 80.0–83.8 | 57.1–78.0 | [145, 161] | |
| Combination of miR-10a-5p, miR-10b-5p and miR-223-3p | 86.7 | 75.0 | [162] | ||
| Combination of miR-21-5p, miR-150-5p, miR-145-5p and miR-146a-5p | 90.8 | 93.8 | [163] | ||
| Combination of miR-378 and miR-451 | 81.0 | 83.0 | [146] | ||
| miR-1233 | 77.4–81.0 | 37.6–76.0 | [164, 165] | ||
| miR-210 | 67.5–82.5 | 62.2–80.0 | [144, 165–167] | ||
| miR-106a | 78.1 | 75.0 | [168] | ||
| miR-206 | 83.8 | 57.1 | [161] | ||
| miR-34a | 80.8 | 80.0 | [148] | ||
| miR-141 | 75.0 | 73.3 | [148] | ||
| Urine | miRNA | miR-15a | 98.1 | 100.0 | [169] |
| miR-30a-5p me | 63.0 | 67.0 | [170] | ||
| miR-210 | 57.8 | 80.0 | [171] | ||
| miR-30c-5p | 68.6 | 100.0 | [172] | ||
| Combination of miR-122, miR-1271 and miR-15b | 100.0 | 86.0 | [173] | ||
| let-7 | 71.0 | 81.0 | [174] | ||
| Combination of miR-122-5p, miR-1271-5p and miR-15b-5p | 96.0 | 65.0 | [175] | ||
| Plasma | miRNA | miR-210 | 60.9 | 73.1 | [176] |
| miR-221 | 71.4 | 65.0 | [176] | ||
| miR-1233 | 39.1 | 92.6 | [176] | ||
| miR-424-3p | 75.0 | 81.8 | [177] | ||
| miR-144-3p | 87.1 | 83.0 | [178] | ||
MiRNAs have also been reported as potential biomarkers for diagnosis, prognosis, and therapy of ccRCC (Table 3). A systematic analysis has identified that there were 118 miRNAs that could be diagnostic biomarkers, 28 miRNAs were prognostic biomarkers, and 80 miRNAs were therapeutic biomarkers [143]. Serum levels of miR-210 were particularly elevated in ccRCC patients, which could be a diagnostic biomarker for ccRCC with a sensitivity of 67.5%, and a specificity of 70% [144]. Moreover, a combination of serum miR-210 and miR-378 could definitely enhance the discriminatory ability of ccRCC, with a sensitivity and specificity of 80% and 78%, respectively [145]. The expression level of serum miR-378 was significantly upregulated in ccRCC patients with an AUC of 0.71, and its overexpression was positively correlated with DFS and clinical stage [145, 146]. Moreover, a combination of serum miR-378 and miR-451 increased the diagnostic efficiency (AUC = 0.86), and a sensitivity of 81% and specificity of 83% [146]. Tissue miR-21 levels were associated with the histological classification of RCC, such as, ccRCC, pRCC, chRCC, and eosinophilia, which could be a diagnostic biomarker with a specificity of 90% (95% CI: 0.639–0.981) and sensitivity of 83% (95% CI: 0.535–0.976%) [147]. In addition, miR-34a and miR-141 were obviously decreased in the serum samples of ccRCC patients, which might be a diagnostic biomarker for ccRCC with a sensitivity of 80.76% and 75%, and specificity of 80% and 73.33%, respectively [148]. Hence, lncRNAs combined with miRNAs might be a promising strategy for ccRCC diagnosis and prognosis.
Role in drug resistance
Radical nephrectomy and nephron-preserving surgery are the best therapeutic strategies for ccRCC patients at the early stage; however, approximately 30% of patients were initially diagnosed at the metastatic stage [4]. In that case, targeted drugs such as sunitinib, sorafenib, everolimus, are often recommended for their treatments [179]. Nevertheless, a large number of ccRCC patients are exclusively resistant to the targeted therapy, which leads to therapeutic failure and little clinical benefit. Although systemic treatment has been implemented in ccRCC patients, drug resistance is still the primary problem that needs to be overcome [180]. Many studies have proposed that lncRNA/miRNA/mRNA axis has a pivotal role in drug resistance of ccRCC (Table 4).
Table 4.
LncRNA/miRNA/mRNA axis in ccRCC drug resistance
| LncRNA | Therapy | Mechanism | Resistance | Refs. |
|---|---|---|---|---|
| LINC00461 | Sunitinib | miR-942/SALL1, METAP1, DCAF11 | Enhance | [181] |
| SARCC | Sunitinib | miR-143-3p/AKT, MMP13, K-RAS, p-ERK | Weaken | [182] |
| ARSR | Sunitinib | miR-34/AXL, miR-449/c-MET | Enhance | [183] |
| HOTAIR | Sunitinib | miR-17-5p/Beclin1 | Enhance | [184] |
| ADAMTS9-AS2 | Cisplatin and 5-Fluorouracil | miR-27a-3p/FOXO1 | Weaken | [21] |
| MALAT1 | Sunitinib | miR-362-3p/G3BP1 | Enhance | [37] |
| LINC02532 | Radiotherapy | miR-654-5p/YY1 | Enhance | [185] |
| GAS5 | Sorafenib | miR-21/Sox5 | Weaken | [129] |
| KIF9-AS1 | Sorafenib | miR-497-5p/autophagy signaling | Enhance | [22] |
| PLK1S1 | Sorafenib | miR-653/CXCR5 | Enhance | [186] |
| NEAT1 | Sorafenib | miR-34a/c-Met | Enhance | [187] |
LncRNA ARSR was upregulated in ccRCC cells and its high expression enhanced sunitinib resistance [183]. In this process, lncARSR functions as a ceRNA and sponges miR-34 and miR-449, then induces the expression of AXL and c-MET. LncRNA HOTAIR expression was markedly elevated in ccRCC sunitinib-resistant cells and increased Beclin1 expression by competing with miR-17-5p, thus enhancing sunitinib resistance [184]. Moreover, lncRNA MALAT1/miR-362-3p and LINC00461/miR-942 axis have also been shown to enhance sunitinib resistance. The levels of lncRNA SARCC were increased in sunitinib-treated ccRCC cells, and high expression of SARCC enhanced the sensitivity of ccRCC cells to sunitinib [182]. Mechanistically, SARCC interacted with androgen receptor (AR) and diminished its stability, thereby inhibiting miR-143-3p transcription and downstream signal activation [182]. Additionally, SARCC also regulates AR/HIF-2α/c-Myc axis to promote cell proliferation and ccRCC progression [188]. ccRCC cells with high lncRNA KIF9-AS1 expression enhanced sorafenib resistance by sponging miR-497-5p and activating transforming growth factor-β (TGF-β) signaling [22]. LncRNA GAS5 was downregulated in sorafenib-resistant ccRCC cells, which could upregulate the expression of SOX5 by binding with miR-21 and weaken the sorafenib sensitivity [129]. SOX5 belongs to the SOX family, which contains more than 20 members and some are highly expressed in chemotherapy-resistant cells [189]. Knockdown of lncRNA LINC02532 increases radiosensitivity in ccRCC cells by regulating the miR-654-5p/Yin Yang-1(YY1) axis [185]. YY1 is a DNA/RNA binding transcription factor, and plays an important role in tumorigenesis and radiation resistance [190]. Overexpression of lncRNA ADAMTS9-AS2 in ccRCC cells reduced 5-fluorouracil resistance via sponging miR-27a-3p to upregulate forkhead box protein O1 (FOXO1) [21]. FOXO1 is a transcription factor for tumor suppressor, which is inactivated in tumor cells and acts as a target of the AR/ERβ pathway [191]. In ccRCC cells and tissues, the FOXO1 level was decreased, and overexpression of FOXO1 could induce cell cycle arrest and promote apoptosis. Additionally, FOXO1 expression is closely associated with the pathological classification, tumor grade and tumor stage of ccRCC [192].
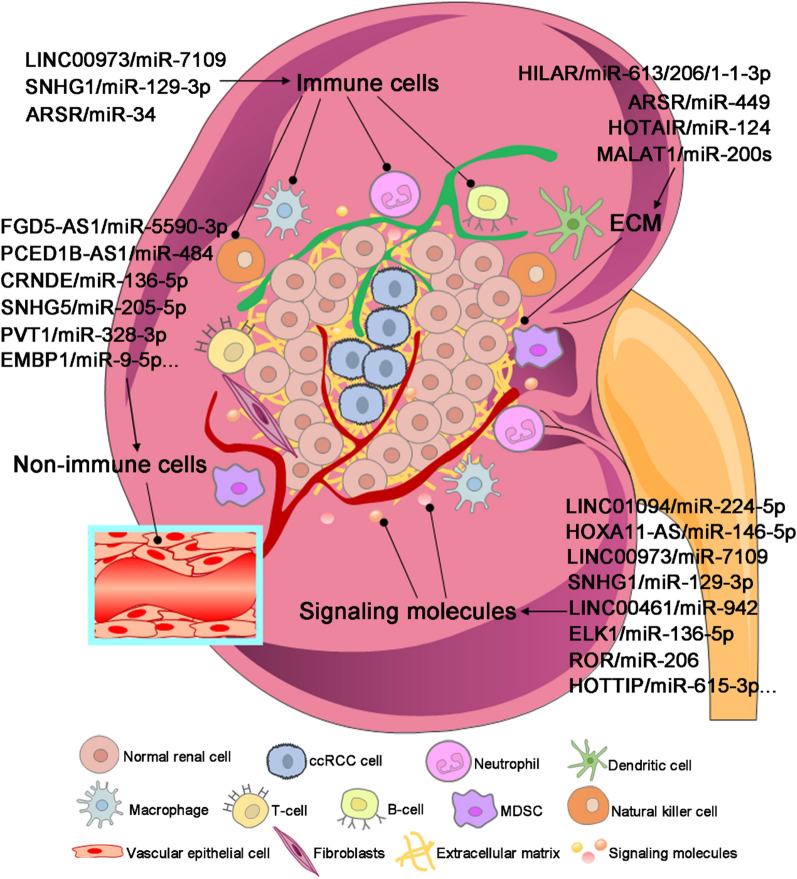
LncRNA/miRNA/mRNA axis in the tumor microenvironment of ccRCC
To date, it is still difficult to eradicate the malignant tumors because they are located in the dynamic tumor microenvironment (TME), which can sustain the nutrient demand of tumor cells and help them escape from the directly killing of immune cells. Hence, TME is vital for tumor formation, growth, angiogenesis, metastasis, and influences therapeutic efficacy of drugs [193]. There are many components in the TME, which can be divided into immune cells, non-immune cells, extracellular matrix (ECM) and signaling molecules (Fig. 3). As tumor cells have close communication with the surrounding TME, targeting the components in the TME is currently a research interest for tumor therapies. In recent years, numerous studies have revealed that lncRNA and miRNA network performs an important role in modulating the TME of ccRCC (Fig. 4).
Fig. 3.
Schematic diagram of TME components. TME consists of immune cells, non-immune cells, extracellular matrix (ECM) and signaling molecules. a Immune cells in the TME are composed of macrophages, neutrophils, myeloid-derived suppressor cells (MDSCs), T-cells, B-cells, natural killer cells and dendritic cells. b Non-immune cells in the TME mainly include vascular epithelial cells, endothelial cells, fibroblasts, adipocytes, glial cells, stellate cells and smooth muscle cells. c ECM refers to the microenvironment supporting the survival and growth of tumor cells, which consists of collagen, elastin fibrils, proteinases, proteoglycans (PGs), glycoproteins, glycosaminoglycans (GAGs) and exosomes. d Signaling molecules in the TME include cytokines (e.g. IL2), growth factors (e.g. VEGF) and degradation and remodeling enzymes (e.g. MMPs)
Fig. 4.
LncRNA/miRNA/mRNA axis in the TME of ccRCC. LncRNA/miRNA/mRNA axis plays a vital role in regulating the TME of ccRCC, such as immune cells, non-immune cells, ECM, and signaling molecules; therefore, the alteration of this network has a significant effect on the initiation and progression of ccRCC
As a modulator of immune cells
Tumor immunotherapies aim to increase the responses of immune cells, which have already become a hotspot for recent studies. Immune escape is helpful for the growth and metastasis of tumor cells, and decreases the responses to immunotherapy, eventually leading to the poor prognosis of patients [194]. Immune cells in the TME consist of macrophages, neutrophils, dendritic cells, B cells, T cells and other immune cells [195]. Many studies have confirmed that immune cells are pivotal in the progression of ccRCC (Fig. 4) [59, 97, 100]. Siglec-15 is an immunosuppressive molecule, which inhibits antigen-specific T cell reactions in vivo and in vitro, and plays an important role in the TME [196]. One study reported that lncRNA LINC00973 was upregulated in Siglec-15 positive ccRCC, which could induce the expression of Siglec-15 by sponging miR-7109, then enhance the tumor immune suppression. Moreover, overexpression of Siglec-15 in ccRCC cells could significantly inhibit the secretion of IL-2 by Jurkat cells [59]. IL-2 deficiency led to a defect in the homeostasis of CD25+ CD4+ regulatory T cells and T lymphocytes, which was closely associated with the initiation of autoimmune diseases [197]. Tian et al. have identified that lncRNA SNHG1 was highly expressed in ccRCC, which could enhance the immune escape of ccRCC cells via binding with miR-129‐3p increase the expression of STAT3 [97]. On the other hand, silencing of SNHG1 could increase the secretion of immune-related factors, such as IFN-γ, TNF-α and IL-2. Moreover, knockdown of SNHG1 in ccRCC mice could substantially increase the infiltration of CD8+ T cells, and prolong the overall survival of ccRCC mice [97]. Similarly, lncARSR was upregulated in ccRCC and could promote M2 polarization of macrophages by activating the STAT3 signal pathway. Its high expression in ccRCC mice could elevate the levels of CD206 and Ki67 [198]. Additionally, lncARSR acts as a ceRNA of miR34/miR449, which could upregulate the expression of AXL and c-MET to facilitate the progression of ccRCC [183].
As a modulator of non-immune cells
Epithelial cells are one subtype of the non-immune cells in the TME, which are the most important components in the EMT process for tumor metastasis. In the EMT process, epithelial cells acquire the mesenchymal and fiber-like characteristics, then decrease their intracellular adhesion and increase their metastasis and invasion abilities, eventually transforming into mesenchymal cells to further facilitate tumor metastasis [199]. Studies have shown that lncRNA/miRNA/mRNA axis can influence the EMT process by regulating the epithelial cells (Fig. 4) [55, 62, 64]. Yang et al. have revealed that lncRNA FGD5-AS1 was upregulated in metastatic ccRCC patients. High expression of FGD5-AS1 could promote the migration, invasion and EMT process of ccRCC cells by absorbing miR-5590-3p, thereby activating the ERK/AKT signaling pathway. Otherwise, silencing of FGD5-AS1 or miR-5520-3p could lead to the increase of E-cadherin and decrease of Vimentin [64]. A recent study reported that lncRNA CDKN2B-AS1/miR-141 axis could inhibit the migration, invasion and EMT process of ccRCC cells via reducing the expression of Cyclin D1 and Cyclin D2 [62]. Importantly, the downregulation of Cyclin D could promote the protein degradation of Ras-related C3 botulinum toxin substrate 1 (RAC1) and p-Paxillin. RAC1 is a member of the Rho family of small G proteins, and its activation can influence many cellular processes, such as cytoskeleton reconstruction, cell adhesion and cell apoptosis [200]. Moreover, RAC1 is closely correlated with tumor differentiation, stage and metastasis of ccRCC [201]. Paxillin is a multifunctional cytoskeletal protein that is involved in cell adhesion and highly phosphorylated in the tumor tissues and cells. It has been demonstrated that Paxillin plays an important role in tumor metastasis, which can recruit signaling molecules involved in cell movement and adhesion [202]. Additionally, lncRNA CRNDE expression was considerably elevated in the ccRCC tissues than that in the normal controls, which could promote tumor metastasis by sponging miR-136-5p to activate the EMT process [55].
As a modulator of ECM
ECM functions as a crucial factor in the crosstalk between tumor and TME. It is a complex system that is composed of many components, including exosomes, collagen, proteinases, glycoproteins, elastin fibrils, glycosaminoglycans and proteoglycans [203]. Among the components in ECM, exosome is a direct signal transmission between tumor cells and TME, which is beneficial for tumor growth and metastasis. Studies have shown that tumor cells can coordinate different cell behaviors to escape the killing by secreting exosomes to ECM (Fig. 4) [44, 198, 204–206]. These secreted exosomes contain numerous information, such as nucleic acids (lncRNAs, miRNAs), growth factors, proteins and lipids, which can be transferred from the donor to the recipient cells [207]. Recently, many studies have focused on the identification of the differential lncRNAs and miRNAs in the exosomes, which may be potential important substances for understanding the mechanism of tumor immune escape.
Jagged1, a ligand of Notch, which can influence cell apoptosis through regulating the Notch signaling pathway [208]. LncHILAR was down-regulated in ccRCC and transmitted by exosomes, whose function was a ceRNA for miR-613, miR-206 and miR-1-1-3p to enhance the expression of Jagged1. Under the hypoxic condition, lncHILAR transferred by exosomes could significantly enhance the invasive abilities of ccRCC cells [44]. LncARSR was highly expressed in ccRCC-derived exosomes, which contributes to the secretion of cytokines, macrophage phagocytosis and angiogenesis [198]. Moreover, lncARSR acted as a ceRNA of miR34/miR449, leading to the elevated expression of AXL and c-MET [183]. Jin et al. have found that lncRNA MALAT1 in exosomes was an important medium for the communication between ccRCC cells and ECM. Exosomes carrying MALAT1 could accelerate the cell viability, migration, invasion and EMT process by inhibiting the activation of transcription factor ETS1 and TFCP2L1 [204]. Additionally, MALAT1 also exerted as a ceRNA by sponging miR-200 s, miR-194-5p and miR-362-3p to induce the expression of ZEB2, ACVR2B and G3BP1 [10, 36, 37]. LncRNA HOTAIR could be released from the tumor cells via exosomes, then transmitted to the endothelial cells to promote tumor angiogenesis [205]. In ccRCC cells, HOTAIR could upregulate the expression of ST8 alpha-N-acetyl-neuraminidase alpha-2,8-sialyltransferase 4 (ST8SIA4) by binding with miR-124 [103]. ST8SIA4 is a member of glycosyltransferase family 29, which is involved in the synthesis of polysialic acid, a modulator of the adhesive properties of neural cell adhesion molecule [209]. In ccRCC cell lines and tissues, ST8SIA4 was significantly upregulated, and its high expression could promote the proliferation and metastasis of ccRCC cells in vitro and in vivo [103, 210]. A recent study has reported that lncRNA IGFL2-AS1 can be packaged into extracellular vesicles (EVs), thereby transmitting the information of sunitinib resistance to other sunitinib-sensitive RCC cells [206]. Meanwhile, IGFL2-AS1 also exerted its function as a tumor promoter by regulating miR-802/cAMP-regulated phosphoprotein 19 (ARPP19) axis [211].
As a modulator of signaling molecules: growth factors
Growth factors are another subtype of transmitters in the crosstalk between tumor cells and TME. Tumor cells maintain their growth by absorbing the essential nutrition from the surrounding blood vessels; thus, angiogenesis is necessary for the initiation and progression of different tumors [212]. Angiogenic growth factors, such as VEGF, PDGF and fibroblast growth factor 2 (FGF2), interact with their receptors to activate the downstream signaling pathways to regulate angiogenesis [8]. It has been reported that lncRNAs and miRNAs have an interaction with multiple angiogenic growth factors, which can influence ccRCC angiogenesis by regulating their expressions (Fig. 4) [45, 77, 85, 94, 107]. VEGF was overexpressed in ccRCC, which could stimulate the formation of blood vessels through the VHL-HIF pathway [213]. The high level of VEGF in the serum was negatively correlated with the tumor stage, pathological grade and overall survival of ccRCC patients [214]. LncRNA ROR was significantly up-regulated in ccRCC cells and tissues, which could promote cell proliferation, migration and angiogenesis by regulating miR-206/VEGF axis, thereby facilitating the progression of ccRCC [85]. LncRNA TUG1 was highly increased in ccRCC and acted as a ceRNA sponging miR-299-3p to induce the expression of VEGFA to promote tumor angiogenesis. Knockdown of TUG1 could inhibit the proliferation, migration and angiogenesis of ccRCC cells in vitro, and similar results were obtained in ccRCC xenograft mice [45]. Placental growth factor (PGF) is a member of the VEGF subfamily, which cooperates with VEGF to promote the formation of blood vessels [215]. PGF amount was greatly increased in the serum samples of ccRCC patients, and its high level was notably related to the poor prognosis of ccRCC [216]. LncRNA ARAP1-AS1 could induce the expression of PGF by sponging miR-361-3p, and promote the proliferation, wound healing and invasion of ccRCC cells [107]. FGF2 is a hematopoietic growth factor that positively regulates the hematopoietic function of various cells, including stromal cells, hematopoietic progenitor cells and blood cells [217]. LncRNA PCGEM1 level was elevated in ccRCC cells, which could promote the proliferation and metastasis of ccRCC cells by binding with miR-433-3p to upregulate FGF2 [77]. Insulin-like growth factor 2 (IGF-2) participates in the regulation of TME by enhancing the anti-inflammatory properties of macrophages. Also, IGF-2 regulates the angiogenesis of vascular endothelial cells, leading to the activation of fibroblasts [218]. LncRNA HOTTIP functioned as a ceRNA for miR-615-3p, which could boost the expression of IGF-2. Moreover, HOTTIP was significantly up-regulated in ccRCC, and its elevated expression is negatively correlated with the OS and DFS of ccRCC patients [94].
As a modulator of signaling molecules: degradation and remodeling enzyme
Matrix metalloproteinases (MMPs) is a large family of zinc-binding proteins, which has been discovered by at least 26 members of this family. Members in the MMP family have the ability to degrade the extracellular matrix and basal membranes; therefore, the alteration of MMPs expression is closely associated with cell differentiation, angiogenesis, extracellular matrix remodeling and metastasis. Studies have found that MMPs can be regulated by various factors, such as hormones, growth factors, cytokines [219]. Currently, lncRNAs and miRNAs also have been demonstrated that they can regulate the expression of many MMP members, then influence the progression of different tumors (Fig. 4) [56, 61, 181]. For example, lncRNA HOXA11-AS could regulate MMP16 by sponging miR-146b-5p, which could promote the proliferation and invasion of ccRCC cells [61]. MMP16 is a membrane protein that is localized in fibroblasts, which is responsible for the degradation of various ECM components and acceleration of the EMT process [220]. Moreover, HOXA11-AS was upregulated in ccRCC tissues and cells, and its high expression was positively correlated with the clinical stage, tumor stage and lymphatic metastasis of ccRCC [61]. MMP2 and MMP7 were found to be increased in ccRCC, and were positively associated with tumor metastasis, pathological grade and clinical stage [221]. Jiang et al. have found that silencing of LINC01094 in ccRCC cells could inhibit the expression of MMP2 and MMP7, then prevent the EMT process [56]. Additionally, LINC01094 acted as a ceRNA of miR-224-5p to induce the expression of chondroitin sulfate synthase 1 (CHSY1), which could enhance the malignant behavior of ccRCC cells. CHSY1 exerts the antagonistic ability for cell apoptosis, and promotes tumor progression by regulating the NF-κB or caspase-3/7 signaling pathway [222]. MMP9 is an important component for the remodeling of extracellular matrix, which plays a critical role in tumor metastasis and progression [223]. It has been reported that MMP9 has an impact on the biological functions of monocytes and related differential cells, and its expression was elevated in ccRCC patients with high abundance of monocytes [224]. LINC00461 was highly expressed in ccRCC cells, and acted as a ceRNA for miRNA-942 to influence the survival of ccRCC patients [181]. Notably, overexpression of miR-942 in metastatic ccRCC cells could promote the secretion of MMP9 and VEGF, which could enhance sunitinib resistance of endothelial cells [225].
Conclusions
Extensive evidence has revealed that lncRNAs and miRNAs are involved in the diagnosis, prognosis, and drug therapy of ccRCC. Understanding the interaction between lncRNA and miRNA network and TME enables us to deeply understand the initiation, development and drug resistance of ccRCC. Nevertheless, the role of lncRNA/miRNA/mRNA axis in the TME of ccRCC remains poorly understood. Hence, in this review, we mainly focus on the biological function of lncRNA/miRNA/mRNA axis in the progression of ccRCC, then discuss how lncRNA/miRNA/mRNA axis regulate the immune cells, non-immune cells, ECM, growth factors, degradation and remodeling enzymes in TME, and finally highlight their potential application as novel biomarkers and therapeutic targets for ccRCC.
MiRNA can bind to the 3’UTR of target mRNAs, while lncRNA act as a sponge of miRNA to prevent the binding between miRNA and mRNA, which can be defined as lncRNA/miRNA/mRNA regulatory network. LncRNA/miRNA/mRNA axis can regulate the gene expression and signal transduction, and play a critical role in transmitting the information between tumor cells and the surrounding TME, thereby influencing the progression of ccRCC. During the initiation and development of ccRCC, lncRNAs have a bidirectional regulatory function of tumor cells, which combine with oncogenic miRNAs will result in tumor inhibition, and interact with suppressive miRNAs will promote tumor progression. Since lncRNAs and miRNAs are stable in the serum, urine, tissues, and they can directly reflect the characteristics of tumor cells; therefore, lncRNAs and miRNAs can become diagnostic and predictive biomarkers of ccRCC. More importantly, lncRNA/miRNA/mRNA axis has a close interaction with the cellular and non-cellular components in the TME of ccRCC, which can influence the cell proliferation, apoptosis, migration, invasion, angiogenesis, EMT process, and immune responses. The interaction between the components in TME and lncRNA/miRNA/mRNA axis will significantly influence the survival, prognosis and drug sensitivity of ccRCC patients.
To date, most studies remain focus on the role of lncRNA/miRNA/mRNA axis in promoting or inhibiting the progression of ccRCC, and little evidence regarding the lncRNA/miRNA/mRNA axis in regulating the crosstalk between ccRCC cells and TME. Moreover, little information has been presented for the clinical application of lncRNA/miRNA/mRNA axis in ccRCC. Therefore, it is necessary to clarify the clinical significance of the lncRNA/miRNA/mRNA axis in the future. First, the delivery of lncRNAs or miRNAs to ccRCC cells needs to be explored to improve the efficacy of drug therapy. Second, the regulation of lncRNAs or miRNAs to overcome the immune escape in ccRCC cells. Third, the evaluation of the doses and pharmacokinetics of lncRNA-based therapies. In conclusion, further studies of lncRNA/miRNA/mRNA axis will provide more information and novel insights to understand the pathogenesis of ccRCC, which will help us better predict the diagnosis and prognosis of ccRCC.
Abbreviations
- RCC
Renal cell carcinoma
- ccRCC
Clear renal cell carcinoma
- lncRNA
Long non-coding RNA
- miRNA
MicroRNA
- mRNA
Messenger RNA
- pRCC
Papillary RCC
- chRCC
Chromophobe RCC
- TME
Tumor microenvironment
- VHL
Von Hippel-Lindau
- HIF
Hypoxia-inducible factor
- VEGF
Vascular endothelial growth factor
- PDGF
Platelet-derived growth factor
- mTOR
Mammalian target of rapamycin
- VEGFR
Vascular endothelial growth factor receptor
- PDGFR
Platelet-derived growth factor receptor
- ncRNA
Non-coding RNA
- sncRNA
Small non-coding RNA
- 3ʹUTR
3ʹUntranslated regions
- FAM193B
Family with sequence similarity 193 member B
- ERK
Extracellular signal-regulated kinase
- OS
Overall survival
- ceRNA
Competing endogenous RNA
- TBX15
T-box transcription factor 15
- DFS
Disease-free survival
- ZEB2
Zinc finger E-box binding homeobox 2
- DNA
Deoxyribo nucleic acid
- ACVR2B
Activin receptor type 2B
- G3BP1
Ras-GTPase-activating SH3-domain-binding protein 1
- DARS
Aspartyl-tRNA synthetase
- XIAP
X-linked inhibitor of apoptosis protein
- DKK1
Dickkopf-1
- TIMP2
Tissue inhibitor of metalloproteinase-2
- TNM
Tumor-node-metastasis
- ASS1
Argininosuccinate synthetase 1
- GSK-3β
Glycogen synthase kinase-3β
- AUC
ROC curve
- AR
Androgen receptor
- HIF-2α
Hypoxia-inducible factor-2α
- TGF-β
Transforming growth factor-beta
- YY1
Yin Yang-1
- FOXO1
Forkhead box protein O1
- ECM
Extracellular matrix
- IFN-γ
Interferon-γ
- TNF-α
Tumor necrosis factor-α
- IL-2
Interleukin-2
- EMT
Epithelial mesenchymal transition
- RAC1
Rac family small GTPase 1
- EV
Extracellular vesicle
- TFCP2L1
Transcription factor CP2-like 1
- ST8SIA4
α-2,8-Sialyltransferase 4
- FGF2
Fibroblast growth factor 2
- PGF
Placental growth factor
- IGF-2
Insulin-like growth factor 2
- CHSY1
Chondroitin sulfate synthase 1
- ADAMTS9-AS2
ADAMTS9 antisense RNA 2
- AJCC
American Joint Committee on Cancer
- AKT
Protein kinase B
- ARAP1-AS1
ARAP1 antisense RNA 1
- CADM1-AS1
CADM1 antisense RNA 1
- CDKN2B-AS1
CDKN2B antisense RNA 1
- c-MET
C-mesenchymal-epithelial transition factor
- CRNDE
Colorectal neoplasia differentially expressed
- DARS-AS1
Aspartyl-tRNA synthetase antisense RNA 1
- FGD5-AS1
FGD5 antisense RNA 1
- GAS5
Growth arrest-specific transcript 5
- GIHCG
Gradually increased during hepatocarcinogenesis
- HIF-1α
Hypoxia inducible factor-1α
- HOTAIR
HOX transcript antisense intergenic RNA
- HOTTIP
HOXA transcript at the distal tip
- HOXA11-AS
HOXA11 antisense RNA
- IL-6
Interleukin-6
- KIF9-AS1
KIF9 antisense RNA 1
- lncARSR
Long noncoding RNA ARSR
- lncHILAR
Hypoxia-induced long non-coding RNA associated with RCC
- MALAT1
Metastasis-associated lung adenocarcinoma transcript 1
- MAPK
Mitogen-activated protein kinase
- MMP
Matrix metalloproteinase
- NBAT1
Neuroblastoma associated transcript 1
- PANDAR
Promoter of CDKN1A antisense DNA damage activated RNA
- PCGEM1
Prostate cancer gene expression marker 1
- p-ERK
Phosphorylated extracellular signal-regulated kinases
- PI3K
Phosphatidylinositol 3-kinase
- PTENP1
Phosphatase and tensin homolog pseudogene 1
- PVT1
Plasmacytoma variant translocation 1
- RNA
Ribonucleic acid
- ROR
Regulator of reprogramming
- SNHG
Small nucleolar RNA host gene
- SARCC
Suppressing androgen receptor in renal cell carcinoma
- SOX
Sex-determining region Y-box
- SRC
Proto-oncogene tyrosine-protein kinase SRC
- STAT3
Signal transducer and activator of transcription 3
- TCL6
T-cell leukemia/lymphoma 6
- TUG1
Taurine upregulated gene 1
- VEGFA
Vascular endothelial growth factor A
- UBE2C
Ubiquitin-mediated proteolysis genes
- ARPP19
CAMP-regulated phosphoprotein 19
Author contributions
QZ wrote the manuscript. HR prepared the tables and figures. LG prepared the figures. WZ and PH critically reviewed and edited the manuscript. FS decided the topic of the manuscript and conceptualized the review. All the authors read and approved the final manuscript.
Funding
This study was supported by grants from the Zhejiang Province Natural Science Foundation of China (No. LYY21H310009 and No. LQ20H310005), National Natural Science Foundation of China (No. 82003853), Medical and Health Research Program of Zhejiang (No. 2021KY046 and No. 2022KY047), and Leading Talent of “Ten Thousand Plan”—National High-Level Talents Special Support Plan and the Science Technology Plan Project of Zhejiang Province (No. 2020R52029).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare that there are no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Feifeng Song, Email: songfeifeng@hmc.edu.cn.
Ping Huang, Email: huangping@hmc.edu.cn.
References
- 1.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7–33. doi: 10.3322/caac.21708. [DOI] [PubMed] [Google Scholar]
- 2.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3.Bahadoram S, Davoodi M, Hassanzadeh S, Bahadoram M, Barahman M, Mafakher L. Renal cell carcinoma: an overview of the epidemiology, diagnosis, and treatment. G Ital Nefrol. 2022;39(3):1. [PubMed] [Google Scholar]
- 4.Liu X, Hao Y, Yu W, Yang X, Luo X, Zhao J, Li J, Hu X, Li L, et al. Long non-coding RNA emergence during renal cell carcinoma tumorigenesis. Cellular Physiol Biochem. 2018;47(2):735–746. doi: 10.1159/000490026. [DOI] [PubMed] [Google Scholar]
- 5.Motzer R, Jonasch E, Agarwal N, Bhayani S, Bro W, Chang S, Choueiri T, Costello B, Derweesh I, Fishman M, et al. Kidney cancer, version 2 2017, NCCN clinical practice guidelines in oncology. J National Comprehen Cancer Net. 2017;15(6):804–834. doi: 10.6004/jnccn.2017.0100. [DOI] [PubMed] [Google Scholar]
- 6.Gilbert NJAU. Surgical treatment of pulmonary metastases in metastatic renal cell carcinoma. Aktuelle Urologie. 2020;51(3):271–274. doi: 10.1055/a-1140-5623. [DOI] [PubMed] [Google Scholar]
- 7.Weaver C, Bin Satter K, Richardson KP, Tran LKH, Tran PMH, Purohit S. Diagnostic and prognostic biomarkers in renal clear cell carcinoma. Biomedicines. 2022;10(11):2953. doi: 10.3390/biomedicines10112953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lai Y, Zhao Z, Zeng T, Liang X, Chen D, Duan X, Zeng G, Wu WJ. Crosstalk between VEGFR and other receptor tyrosine kinases for TKI therapy of metastatic renal cell carcinoma. Cancer Cell Int. 2018;18(1):9. doi: 10.1186/s12935-018-0530-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dell'Atti L, Bianchi N, Aguiari G. New therapeutic interventions for kidney carcinoma: looking to the future. Cancers. 2022 doi: 10.3390/cancers14153616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiao H, Tang K, Liu P, Chen K, Hu J, Zeng J, Xiao W, Yu G, Yao W, Zhou H, et al. LncRNA MALAT1 functions as a competing endogenous RNA to regulate ZEB2 expression by sponging miR-200s in clear cell kidney carcinoma. Oncotarget. 2015;6(35):38005–38015. doi: 10.18632/oncotarget.5357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xue S, Wang S, Li J, Guan H, Jiang S, Guo Y, Li Q. LncRNA NBAT1 suppresses cell proliferation and migration via miR-346/GSK-3beta axis in renal carcinoma. IUBMB Life. 2019;71(11):1720–1728. doi: 10.1002/iub.2111. [DOI] [PubMed] [Google Scholar]
- 12.Kulkarni P, Dasgupta P, Hashimoto Y, Shiina M, Shahryari V, Tabatabai ZL, Yamamura S, Tanaka Y, Saini S, Dahiya R, et al. A lncRNA TCL6-miR-155 interaction regulates the Src-Akt-EMT network to mediate kidney cancer progression and metastasis. Cancer Res. 2021;81(6):1500–1512. doi: 10.1158/0008-5472.CAN-20-0832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yan H, Bu P. Non-coding RNA in cancer. Essays Biochem. 2021;65(4):625–639. doi: 10.1042/EBC20200032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dykes IM, Emanueli C. Transcriptional and post-transcriptional gene regulation by long non-coding RNA. Genomics Proteomics Bioinform. 2017;15(3):177–186. doi: 10.1016/j.gpb.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chi Y, Wang D, Wang J, Yu W, Yang J. Long non-coding RNA in the pathogenesis of cancers. Cells. 2019;8(9):1015. doi: 10.3390/cells8091015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Matsumoto A, Pasut A, Matsumoto M, Yamashita R, Fung J, Monteleone E, Saghatelian A, Nakayama KI, Clohessy JG, Pandolfi PP. mTORC1 and muscle regeneration are regulated by the LINC00961-encoded SPAR polypeptide. Nature. 2017;541(7636):228–232. doi: 10.1038/nature21034. [DOI] [PubMed] [Google Scholar]
- 17.Lim LP, Lau NC, Garrett-Engele P, Grimson A, Schelter JM, Castle J, Bartel DP, Linsley PS, Johnson JM. Microarray analysis shows that some microRNAs downregulate large numbers of target mRNAs. Nature. 2005;433(7027):769–773. doi: 10.1038/nature03315. [DOI] [PubMed] [Google Scholar]
- 18.Khashkhashi Moghadam S, Bakhshinejad B, Khalafizadeh A, Mahmud Hussen B, Babashah S. Non-coding RNA-associated competitive endogenous RNA regulatory networks: Novel diagnostic and therapeutic opportunities for hepatocellular carcinoma. J Cell Mol Med. 2022;26(2):287–305. doi: 10.1111/jcmm.17126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brooks R, Monzy J, Aaron B, Zhang X, Kossenkov A, Hayden J, Keeney F, Speicher DW, Zhang L, Dang CV. Circadian lncRNA ADIRF-AS1 binds PBAF and regulates renal clear cell tumorigenesis. Cell Rep. 2022;41(3):111514. doi: 10.1016/j.celrep.2022.111514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhang S, Huangfu H, Zhao Q, Li Y, Wu L. Downregulation of long noncoding RNA HCP5/miR-216a-5p/ZEB1 axis inhibits the malignant biological function of laryngeal squamous cell carcinoma cells. Front Immunol. 2022;13:1022677. doi: 10.3389/fimmu.2022.1022677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Song EL, Xing L, Wang L, Song WT, Li DB, Wang Y, Gu YW, Liu MM, Ni WJ, Zhang P, et al. LncRNA ADAMTS9-AS2 inhibits cell proliferation and decreases chemoresistance in clear cell renal cell carcinoma via the miR-27a-3p/FOXO1 axis. Aging. 2019;11(15):5705–5725. doi: 10.18632/aging.102154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jin Y, Huang R, Xia Y, Huang C, Qiu F, Pu J, He X, Zhao X. Long noncoding RNA KIF9-AS1 regulates transforming growth factor-beta and autophagy signaling to enhance renal cell carcinoma chemoresistance via microRNA-497-5p. DNA Cell Biol. 2020;39(7):1096–1103. doi: 10.1089/dna.2020.5453. [DOI] [PubMed] [Google Scholar]
- 23.Fernandes JCR, Acuna SM, Aoki JI, Floeter-Winter LM, Muxel SM. Long non-coding RNAs in the regulation of gene expression: physiology and disease. Noncoding RNA. 2019;5(1):17. doi: 10.3390/ncrna5010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shi T, Morishita A, Kobara H, Masaki T. The role of long non-coding RNA and microRNA networks in hepatocellular carcinoma and its tumor microenvironment. Int J Mol Sci. 2021;22(19):10630. doi: 10.3390/ijms221910630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sebastian-delaCruz M, Gonzalez-Moro I, Olazagoitia-Garmendia A, Castellanos-Rubio A. Santin IJN-cR: the role of lncRNAs in gene expression regulation through mRNA stabilization. Non-coding RNA. 2021 doi: 10.3390/ncrna7010003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qiao X, Hou G, He Y, Song D, An Y, Altawil A, Zhou X, Wang Q, Kang J, Yin Y. The novel regulatory role of the lncRNA-miRNA-mRNA Axis in chronic inflammatory airway diseases. Front Mol Biosci. 2022;9:927549. doi: 10.3389/fmolb.2022.927549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xie G, Zheng X, Zheng Z, Wu R, Yao Z, Huang W, Sun F, Mu X, Wu K, Zheng J. The ceRNA PVT1 inhibits proliferation of ccRCC cells by sponging miR-328-3p to elevate FAM193B expression. Aging. 2021;13(17):21712–21728. doi: 10.18632/aging.203514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miricescu D, Balan DG, Tulin A, Stiru O, Vacaroiu IA, Mihai DA, Popa CC, Papacocea RI, Enyedi M, Sorin NA, et al. PI3K/AKT/mTOR signalling pathway involvement in renal cell carcinoma pathogenesis (review) Exp Ther Med. 2021;21(5):540. doi: 10.3892/etm.2021.9972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chen X, Yang Y, Cao Y, Wu C, Wu S, Su Z, Jin H, Wang D, Zhang G, Fan W, et al. lncRNA PVT1 identified as an independent biomarker for prognosis surveillance of solid tumors based on transcriptome data and meta-analysis. Cancer Manag Res. 2018;10:2711–2727. doi: 10.2147/CMAR.S166260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zheng Z, Chen Z, Zhong Q, Zhu D, Xie Y, Shangguan W, Xie W. CircPVT1 promotes progression in clear cell renal cell carcinoma by sponging miR-145-5p and regulating TBX15 expression. Cancer Sci. 2021;112(4):1443–1456. doi: 10.1111/cas.14814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ren Y, Huang W, Weng G, Cui P, Liang H, Li Y. LncRNA PVT1 promotes proliferation, invasion and epithelial-mesenchymal transition of renal cell carcinoma cells through downregulation of miR-16-5p. Onco Targets Ther. 2019;12:2563–2575. doi: 10.2147/OTT.S190239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fang Y, Wei J, Cao J, Zhao H, Liao B, Qiu S, Wang D, Luo J, Chen W. Protein expression of ZEB2 in renal cell carcinoma and its prognostic significance in patient survival. PLoS ONE. 2013;8(5):e62558. doi: 10.1371/journal.pone.0062558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen Z, Zhang J, Zhang Z, Feng Z, Wei J, Lu J, Fang Y, Liang Y, Cen J, Pan Y, et al. The putative tumor suppressor microRNA-30a-5p modulates clear cell renal cell carcinoma aggressiveness through repression of ZEB2. Cell Death Dis. 2017;8(6):e2859. doi: 10.1038/cddis.2017.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chen XF, Guo JF, Xu JF, Yin SH, Cao WL. MiRNA-206 inhibits proliferation of renal clear cell carcinoma by targeting ZEB2. Eur Rev Med Pharmacol Sci. 2019;23(18):7826–7834. doi: 10.26355/eurrev_201909_18992. [DOI] [PubMed] [Google Scholar]
- 35.Zhang HM, Yang FQ, Chen SJ, Che J, Zheng JH. Upregulation of long non-coding RNA MALAT1 correlates with tumor progression and poor prognosis in clear cell renal cell carcinoma. Tumour Biol. 2015;36(4):2947–2955. doi: 10.1007/s13277-014-2925-6. [DOI] [PubMed] [Google Scholar]
- 36.Ye Y, Zhang F, Chen Q, Huang Z, Li M. LncRNA MALAT1 modified progression of clear cell kidney carcinoma (KIRC) by regulation of miR-194-5p/ACVR2B signaling. Mol Carcinog. 2019;58(2):279–292. doi: 10.1002/mc.22926. [DOI] [PubMed] [Google Scholar]
- 37.Wang Z, Chang X, Zhu G, Gao X, Chang L. Depletion of lncRNA MALAT1 inhibited sunitinib resistance through regulating miR-362-3p-mediated G3BP1 in renal cell carcinoma. Cell Cycle. 2020;19(16):2054–2062. doi: 10.1080/15384101.2020.1792667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang Y, Fu D, Chen Y, Su J, Wang Y, Li X, Zhai W, Niu Y, Yue D, Geng H. G3BP1 promotes tumor progression and metastasis through IL-6/G3BP1/STAT3 signaling axis in renal cell carcinomas. Cell Death Dis. 2018;9(5):501. doi: 10.1038/s41419-018-0504-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jiao M, Guo H, Chen Y, Li L, Zhang L. DARS-AS1 promotes clear cell renal cell carcinoma by sequestering miR-194-5p to up-regulate DARS. Biomed Pharmacother. 2020;128:110323. doi: 10.1016/j.biopha.2020.110323. [DOI] [PubMed] [Google Scholar]
- 40.Zhu SY, Zou HC, Gao MM, Chen YX, Xu M, Qin XH. LncRNA GIHCG promoted the proliferation and migration of renal cell carcinoma through regulating miR-499a-5p/XIAP axis. Transl Oncol. 2022;20:101356. doi: 10.1016/j.tranon.2022.101356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Deng H, Huang C, Wang Y, Jiang H, Peng S, Zhao X. LINC00511 promotes the malignant phenotype of clear cell renal cell carcinoma by sponging microRNA-625 and thereby increasing cyclin D1 expression. Aging. 2019;11(16):5975–5991. doi: 10.18632/aging.102156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen Z, Zhang M, Lu Y, Ding T, Liu Z, Liu Y, Zhou Z, Wang L. Overexpressed lncRNA FTX promotes the cell viability, proliferation, migration and invasion of renal cell carcinoma via FTX/miR-4429/UBE2C axis. Oncol Rep. 2022 doi: 10.3892/or.2022.8378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yang T, Zhou H, Liu P, Yan L, Yao W, Chen K, Zeng J, Li H, Hu J, Xu H, et al. lncRNA PVT1 and its splicing variant function as competing endogenous RNA to regulate clear cell renal cell carcinoma progression. Oncotarget. 2017;8(49):85353–85367. doi: 10.18632/oncotarget.19743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hu G, Ma J, Zhang J, Chen Y, Liu H, Huang Y, Zheng J, Xu Y, Xue W, Zhai W. Hypoxia-induced lncHILAR promotes renal cancer metastasis via ceRNA for the miR-613/206/ 1-1-3p/Jagged-1/Notch/CXCR4 signaling pathway. Mol Ther. 2021;29(10):2979–2994. doi: 10.1016/j.ymthe.2021.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 45.Li Y, Zheng D, Pan L, Dai Y, Cai S, Zhao L, Zhu H. Knockdown of TUG1 by shRNA inhibited renal cell carcinoma formation by miR-299-3p/VEGF axis in vitro and in vivo. Eur J Pharmacol. 2019;860:172536. doi: 10.1016/j.ejphar.2019.172536. [DOI] [PubMed] [Google Scholar]
- 46.Liu S, Yang Y, Wang W, Pan X. Long noncoding RNA TUG1 promotes cell proliferation and migration of renal cell carcinoma via regulation of YAP. J Cell Biochem. 2018;119(12):9694–9706. doi: 10.1002/jcb.27284. [DOI] [PubMed] [Google Scholar]
- 47.Lv D, Xiang Y, Yang Q, Yao J, Dong Q. Long non-coding RNA TUG1 promotes cell proliferation and inhibits cell apoptosis, autophagy in clear cell renal cell carcinoma via MiR-31-5p/FLOT1 axis. Onco Targets Ther. 2020;13:5857–5868. doi: 10.2147/OTT.S254634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yang Y, Sun DM, Yu JF, Zhang M, Yi C, Yang R, Dan BH, Li AJ. Long noncoding RNA TUG1 promotes renal cell carcinoma cell proliferation, migration and invasion by downregulating microRNA196a. Mol Med Rep. 2018;18(6):5791–5798. doi: 10.3892/mmr.2018.9608. [DOI] [PubMed] [Google Scholar]
- 49.Zhang W, Lu Y, Shi H, Li X, Zhang Z, Deng X, Yang Y, Wan B. LncRNA ITGB2-AS1 promotes the progression of clear cell renal cell carcinoma by modulating miR-328-5p/HMGA1 axis. Hum Cell. 2021;34(5):1545–1557. doi: 10.1007/s13577-021-00563-7. [DOI] [PubMed] [Google Scholar]
- 50.Wang LN, Zhu XQ, Song XS, Xu Y. Long noncoding RNA lung cancer associated transcript 1 promotes proliferation and invasion of clear cell renal cell carcinoma cells by negatively regulating miR-495-3p. J Cell Biochem. 2018;119(9):7599–7609. doi: 10.1002/jcb.27099. [DOI] [PubMed] [Google Scholar]
- 51.Wang X, Ou H, Zhou L, Liu H, Liu X, Zhang H. Long non-coding RNA LUCAT1 promotes the progression of clear cell renal cell carcinoma via the microRNA-375/YAP1 axis. Exp Ther Med. 2021;22(1):754. doi: 10.3892/etm.2021.10186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Shan G, Huang T, Tang T. Long non-coding RNA MEG8 induced by PLAG1 promotes clear cell renal cell carcinoma through the miR-495-3p/G3BP1 axis. Pathol Res Pract. 2022;229:153734. doi: 10.1016/j.prp.2021.153734. [DOI] [PubMed] [Google Scholar]
- 53.Wang K, Jin W, Song Y, Fei X. LncRNA RP11–436H11 5, functioning as a competitive endogenous RNA, upregulates BCL-W expression by sponging miR-335–5p and promotes proliferation and invasion in renal cell carcinoma. Mol Cancer. 2017;16(1):166. doi: 10.1186/s12943-017-0735-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Qin J, Zhu T, Wu W, Chen H, He Y. Long non-coding RNA PCED1B-AS1 promotes the progression of clear cell renal cell carcinoma through miR-484/ZEB1 axis. Onco Targets Ther. 2021;14:393–402. doi: 10.2147/OTT.S270149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhang Y, Lan X, Wang Y, Liu C, Cui T. CRNDE mediates the viability and epithelial-mesenchymal transition of renal cell carcinoma via miR-136-5p. J Recept Signal Transduct Res. 2021;41(3):234–244. doi: 10.1080/10799893.2020.1805629. [DOI] [PubMed] [Google Scholar]
- 56.Jiang Y, Zhang H, Li W, Yan Y, Yao X, Gu W. FOXM1-activated LINC01094 promotes clear cell renal cell carcinoma development via MicroRNA 224–5p/CHSY1. Mol Cell Biol. 2020 doi: 10.1128/MCB.00357-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Xu H, Wang X, Wu J, Ji H, Chen Z, Guo H, Hou J. Long non-coding RNA LINC01094 promotes the development of clear cell renal cell carcinoma by upregulating SLC2A3 via MicroRNA-184. Front Genet. 2020;11:562967. doi: 10.3389/fgene.2020.562967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ju X, Sun Y, Zhang F, Wei X, Wang Z, He X. Long non-coding RNA LINC02747 promotes the proliferation of clear cell renal cell carcinoma by inhibiting miR-608 and activating TFE3. Front Oncol. 2020;10:573789. doi: 10.3389/fonc.2020.573789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liu Y, Li X, Zhang C, Zhang H, Huang Y. LINC00973 is involved in cancer immune suppression through positive regulation of Siglec-15 in clear-cell renal cell carcinoma. Cancer Sci. 2020;111(10):3693–3704. doi: 10.1111/cas.14611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Jiang Y, Zhang H, Li W, Yan Y, Yao X, Gu W. LINC01426 contributes to clear cell renal cell carcinoma progression by modulating CTBP1/miR-423-5p/FOXM1 axis via interacting with IGF2BP1. J Cell Physiol. 2021;236(1):427–439. doi: 10.1002/jcp.29871. [DOI] [PubMed] [Google Scholar]
- 61.Yang FQ, Zhang JQ, Jin JJ, Yang CY, Zhang WJ, Zhang HM, Zheng JH, Weng ZM. HOXA11-AS promotes the growth and invasion of renal cancer by sponging miR-146b-5p to upregulate MMP16 expression. J Cell Physiol. 2018;233(12):9611–9619. doi: 10.1002/jcp.26864. [DOI] [PubMed] [Google Scholar]
- 62.Dasgupta P, Kulkarni P, Majid S, Hashimoto Y, Shiina M, Shahryari V, Bhat NS, Tabatabai L, Yamamura S, Saini S, et al. LncRNA CDKN2B-AS1/miR-141/cyclin D network regulates tumor progression and metastasis of renal cell carcinoma. Cell Death Dis. 2020;11(8):660. doi: 10.1038/s41419-020-02877-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Na XY, Hu XQ, Zhao Y, Hu CH, Shang XS. LncRNA DNAJC3-AS1 functions as oncogene in renal cell carcinoma via regulation of the miR-27a-3p/PRDM14 axis. Eur Rev Med Pharmacol Sci. 2021;25(3):1291–1301. doi: 10.26355/eurrev_202102_24833. [DOI] [PubMed] [Google Scholar]
- 64.Yang Y, Dong MH, Hu HM, Min QH, Xiao L. LncRNA FGD5-AS1/miR-5590-3p axis facilitates the proliferation and metastasis of renal cell carcinoma through ERK/AKT signalling. Eur Rev Med Pharmacol Sci. 2020;24(17):8756–8766. doi: 10.26355/eurrev_202009_22814. [DOI] [PubMed] [Google Scholar]
- 65.Yang Y, Gong P, Yao D, Xue D, He X. LncRNA HCG18 promotes clear cell renal cell carcinoma progression by targeting miR-152-3p to upregulate RAB14. Cancer Manag Res. 2021;13:2287–2294. doi: 10.2147/CMAR.S298649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Xu C, Liang H, Zhou J, Wang Y, Liu S, Wang X, Su L, Kang X. lncRNA small nucleolar RNA host gene 12 promotes renal cell carcinoma progression by modulating the miR200c5p/collagen type XI alpha1 chain pathway. Mol Med Rep. 2020;22(5):3677–3686. doi: 10.3892/mmr.2020.11490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yu H, Liu J, Zhang Z, Zhu Y, Bi J, Kong C. SNHG12 promotes carcinogenesis of human renal cell cancer via functioning as a competing endogenous RNA and sponging miR-30a-3p. J Cell Mol Med. 2021;25(10):4696–4708. doi: 10.1111/jcmm.16417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wu Z, Chen D, Wang K, Cao C, Xu X. Long non-coding RNA SNHG12 functions as a competing endogenous RNA to regulate MDM4 expression by sponging miR-129-5p in clear cell renal cell carcinoma. Front Oncol. 2019;9:1260. doi: 10.3389/fonc.2019.01260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Xiang W, Lv L, Zhou G, Wu W, Yuan J, Zhang C, Jiang G. The lncRNA SNHG5-mediated miR-205-5p downregulation contributes to the progression of clear cell renal cell carcinoma by targeting ZEB1. Cancer Med. 2020;9(12):4251–4264. doi: 10.1002/cam4.3052. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 70.Li WZ, Zou Y, Song ZY, Wei ZW, Chen G, Cai QL, Wang Z. Long non-coding RNA SNHG5 affects the invasion and apoptosis of renal cell carcinoma by regulating the miR-363-3p-twist1 interaction. Am J Transl Res. 2020;12(2):697–707. [PMC free article] [PubMed] [Google Scholar]
- 71.Wang R, Zheng B, Liu H, Wan X. Long non-coding RNA PCAT1 drives clear cell renal cell carcinoma by upregulating YAP via sponging miR-656 and miR-539. Cell Cycle. 2020;19(10):1122–1131. doi: 10.1080/15384101.2020.1748949. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 72.He H, Wang N, Yi X, Tang C, Wang D. Long non-coding RNA H19 regulates E2F1 expression by competitively sponging endogenous miR-29a-3p in clear cell renal cell carcinoma. Cell Biosci. 2017;7:65. doi: 10.1186/s13578-017-0193-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhou Y, Zhang Z, Wo M, Xu W. The long non-coding RNA NNT-AS1 promotes clear cell renal cell carcinoma progression via regulation of the miR-137/ Y-box binding protein 1 axis. Bioengineered. 2021;12(1):8994–9005. doi: 10.1080/21655979.2021.1992330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hao JF, Chen P, Li HY, Li YJ, Zhang YL. Effects of LncRNA HCP5/miR-214-3p/MAPK1 molecular network on renal cell carcinoma cells. Cancer Manag Res. 2020;12:13347–13356. doi: 10.2147/CMAR.S274426. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 75.Zhang YJ, Lu C. Long non-coding RNA HCP5 promotes proliferation and metastasis of clear cell renal cell carcinoma via targeting miR-140-5p/IGF1R pathway. Eur Rev Med Pharmacol Sci. 2020;24(6):2965–2975. doi: 10.26355/eurrev_202003_20661. [DOI] [PubMed] [Google Scholar]
- 76.Zhu K, Miao C, Tian Y, Qin Z, Xue J, Xia J, Zhu S, Xu A, Yang J, Wang Z. lncRNA MIR4435-2HG promoted clear cell renal cell carcinoma malignant progression via miR-513a-5p/KLF6 axis. J Cell Mol Med. 2020;24(17):10013–10026. doi: 10.1111/jcmm.15609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cai X, Zhang X, Mo L, Zhu J, Yu H. LncRNA PCGEM1 promotes renal carcinoma progression by targeting miR-433-3p to regulate FGF2 expression. Cancer Biomark. 2020;27(4):493–504. doi: 10.3233/CBM-190669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang H, Li W, Gu W, Yan Y, Yao X, Zheng J. MALAT1 accelerates the development and progression of renal cell carcinoma by decreasing the expression of miR-203 and promoting the expression of BIRC5. Cell Prolif. 2019;52(5):e12640. doi: 10.1111/cpr.12640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hirata H, Hinoda Y, Shahryari V, Deng G, Nakajima K, Tabatabai ZL, Ishii N, Dahiya R. Long noncoding RNA MALAT1 promotes aggressive renal cell carcinoma through Ezh2 and interacts with miR-205. Cancer Res. 2015;75(7):1322–1331. doi: 10.1158/0008-5472.CAN-14-2931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jiang LT, Wan CH, Guo QH, Yang SJ, Wu JD, Cai J. Long noncoding RNA metastasis-associated lung adenocarcinoma transcript 1 (MALAT1) promotes renal cell carcinoma progression via sponging miRNA-429. Med Sci Monit. 2018;24:1794–1801. doi: 10.12659/MSM.909450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kulkarni P, Dasgupta P, Bhat NS, Shahryari V, Shiina M, Hashimoto Y, Majid S, Deng G, Saini S, Tabatabai ZL, et al. Elevated miR-182-5p associates with renal cancer cell mitotic arrest through diminished MALAT-1 expression. Mol Cancer Res. 2018;16(11):1750–1760. doi: 10.1158/1541-7786.MCR-17-0762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhou L, Ye J, Wen F, Yu H. Identification of novel prognostic signatures for clear cell renal cell carcinoma based on ceRNA network construction and immune infiltration analysis. Dis Markers. 2022;2022:4033583. doi: 10.1155/2022/4033583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Guo R, Zou B, Liang Y, Bian J, Xu J, Zhou Q, Zhang C, Chen T, Yang M, Wang H, et al. LncRNA RCAT1 promotes tumor progression and metastasis via miR-214-5p/E2F2 axis in renal cell carcinoma. Cell Death Dis. 2021;12(7):689. doi: 10.1038/s41419-021-03955-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Hu Z, Li L, Cheng P, Liu Q, Zheng X, Peng F, Zhang Q. lncRNA MSC-AS1 activates Wnt/beta-catenin signaling pathway to modulate cell proliferation and migration in kidney renal clear cell carcinoma via miR-3924/WNT5A. J Cell Biochem. 2020;121(10):4085–4093. doi: 10.1002/jcb.29594. [DOI] [PubMed] [Google Scholar]
- 85.Shi J, Zhang D, Zhong Z, Zhang W. lncRNA ROR promotes the progression of renal cell carcinoma through the miR206/VEGF axis. Mol Med Rep. 2019;20(4):3782–3792. doi: 10.3892/mmr.2019.10636. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 86.Dong D, Mu Z, Wei N, Sun M, Wang W, Xin N, Shao Y, Zhao C. Long non-coding RNA ZFAS1 promotes proliferation and metastasis of clear cell renal cell carcinoma via targeting miR-10a/SKA1 pathway. Biomed Pharmacother. 2019;111:917–925. doi: 10.1016/j.biopha.2018.12.143. [DOI] [PubMed] [Google Scholar]
- 87.Zhang C, Qu Y, Xiao H, Xiao W, Liu J, Gao Y, Li M, Liu J. LncRNA SNHG3 promotes clear cell renal cell carcinoma proliferation and migration by upregulating TOP2A. Exp Cell Res. 2019;384(1):111595. doi: 10.1016/j.yexcr.2019.111595. [DOI] [PubMed] [Google Scholar]
- 88.Xu Z, Ye J, Bao P, Wu Q, Xie F, Li P. Long non-coding RNA SNHG3 promotes the progression of clear cell renal cell carcinoma via regulating BIRC5 expression. Transl Cancer Res. 2021;10(10):4502–4513. doi: 10.21037/tcr-21-1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wu J, Dong G, Liu T, Zhang S, Sun L, Liang W. LncRNA SNHG17 promotes tumor progression and predicts poor survival in human renal cell carcinoma via sponging miR-328-3p. Aging. 2021;13(17):21232–21250. doi: 10.18632/aging.203440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Lu Y, Liu WG, Lu JH, Liu ZJ, Li HB, Liu GJ, She HY, Li GY, Shi XH. LncRNA UCA1 promotes renal cell carcinoma proliferation through epigenetically repressing p21 expression and negatively regulating miR-495. Tumour Biol. 2017;39(5):1010428317701632. doi: 10.1177/1010428317701632. [DOI] [PubMed] [Google Scholar]
- 91.Wang W, Hu W, Wang Y, An Y, Song L, Shang P, Yue Z. Long non-coding RNA UCA1 promotes malignant phenotypes of renal cancer cells by modulating the miR-182-5p/DLL4 axis as a ceRNA. Mol Cancer. 2020;19(1):18. doi: 10.1186/s12943-020-1132-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wu C, Zhang J. 2020. Long non-conding RNA LOXL1-AS1 sponges miR-589–5p to up-regulate CBX5 expression in renal cell carcinoma. Biosci Rep. [DOI] [PMC free article] [PubMed]
- 93.Zhu Y, Yang Z, Chen H, Pan Y, Gong L, Chen F, Jin X, Wen S, Li Y, Chen G. lncRNAHIF1A-AS2 promotes renal carcinoma cell proliferation and migration via miR-130a-5p/ERBB2 pathway. Onco Targets Ther. 2020;13:9807–9820. doi: 10.2147/OTT.S260191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Wang Q, Wu G, Zhang Z, Tang Q, Zheng W, Chen X, Chen F, Li Q, Che X. Long non-coding RNA HOTTIP promotes renal cell carcinoma progression through the regulation of the miR-615/IGF-2 pathway. Int J Oncol. 2018;53(5):2278–2288. doi: 10.3892/ijo.2018.4539. [DOI] [PubMed] [Google Scholar]
- 95.Zhang J, Jin S, Xiao W, Zhu X, Jia C, Lin Z. Long noncoding RNA LINC00641 promotes renal cell carcinoma progression via sponging microRNA-340-5p. Cancer Cell Int. 2021;21(1):210. doi: 10.1186/s12935-021-01895-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Zhao S, Wang Y, Luo M, Cui W, Zhou X, Miao L. Long noncoding RNA small nucleolar RNA Host Gene 1 (SNHG1) promotes renal cell carcinoma progression and metastasis by negatively regulating miR-137. Med Sci Monit. 2018;24:3824–3831. doi: 10.12659/MSM.910866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Tian P, Wei JX, Li J, Ren JK, Yang JJ. LncRNA SNHG1 regulates immune escape of renal cell carcinoma by targeting miR-129-3p to activate STAT3 and PD-L1. Cell Biol Int. 2021;45(7):1546–1560. doi: 10.1002/cbin.11595. [DOI] [PubMed] [Google Scholar]
- 98.Ye ZH, Gui DW, Wang XY, Wang J, Fu JL. LncRNA SNHG1 promotes renal cell carcinoma progression through regulation of HMGA2 via sponging miR-103a. J Clin Lab Anal. 2022;36(6):e24422. doi: 10.1002/jcla.24422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zhai X, Wu Y, Wang Z, Zhao D, Li H, Chong T, Zhao J. Long noncoding RNA LINC01133 promotes the malignant behaviors of renal cell carcinoma by regulating the miR-30b-5p/Rab3D axis. Cell Transplant. 2020;29:963689720964413. doi: 10.1177/0963689720964413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hong Q, Li O, Zheng W, Xiao WZ, Zhang L, Wu D, Cai GY, He JC, Chen XM. LncRNA HOTAIR regulates HIF-1alpha/AXL signaling through inhibition of miR-217 in renal cell carcinoma. Cell Death Dis. 2017;8(5):e2772. doi: 10.1038/cddis.2017.181. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 101.Ding J, Yeh CR, Sun Y, Lin C, Chou J, Ou Z, Chang C, Qi J, Yeh S. Estrogen receptor beta promotes renal cell carcinoma progression via regulating LncRNA HOTAIR-miR-138/200c/204/217 associated CeRNA network. Oncogene. 2018;37(37):5037–5053. doi: 10.1038/s41388-018-0175-6. [DOI] [PubMed] [Google Scholar]
- 102.Dasgupta P, Kulkarni P, Majid S, Shahryari V, Hashimoto Y, Bhat NS, Shiina M, Deng G, Saini S, Tabatabai ZL, et al. MicroRNA-203 inhibits long noncoding RNA HOTAIR and regulates tumorigenesis through epithelial-to-mesenchymal transition pathway in renal cell carcinoma. Mol Cancer Ther. 2018;17(5):1061–1069. doi: 10.1158/1535-7163.MCT-17-0925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pan Y, Wu Y, Hu J, Shan Y, Ma J, Ma H, Qi X, Jia L. Long noncoding RNA HOTAIR promotes renal cell carcinoma malignancy through alpha-2, 8-sialyltransferase 4 by sponging microRNA-124. Cell Prolif. 2018;51(6):e12507. doi: 10.1111/cpr.12507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Chiyomaru T, Fukuhara S, Saini S, Majid S, Deng G, Shahryari V, Chang I, Tanaka Y, Enokida H, Nakagawa M, et al. Long non-coding RNA HOTAIR is targeted and regulated by miR-141 in human cancer cells. J Biol Chem. 2014;289(18):12550–12565. doi: 10.1074/jbc.M113.488593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yang X, Zhang Y, Fan H. Downregulation of SBF2-AS1 functions as a tumor suppressor in clear cell renal cell carcinoma by inhibiting miR-338-3p-targeted ETS1. Cancer Gene Ther. 2021;28(7–8):813–827. doi: 10.1038/s41417-020-0197-4. [DOI] [PubMed] [Google Scholar]
- 106.Qu Y, Xiao H, Xiao W, Xiong Z, Hu W, Gao Y, Ru Z, Wang C, Bao L, Wang K, et al. Upregulation of MIAT regulates LOXL2 expression by competitively binding MiR-29c in clear cell renal cell carcinoma. Cell Physiol Biochem. 2018;48(3):1075–1087. doi: 10.1159/000491974. [DOI] [PubMed] [Google Scholar]
- 107.Zhong L, Zhong X. Long non-coding RNA ARAP1-AS1 contributes to cell proliferation and migration in clear cell renal cell carcinoma via the miR-361-3p/placental growth factor axis. Bioengineered. 2021;12(1):6629–6642. doi: 10.1080/21655979.2021.1975019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Tao M, Zhou Y, Jin Y, Pu J. Blocking lncRNA MIR155HG/miR-155-5p/-3p inhibits proliferation, invasion and migration of clear cell renal cell carcinoma. Pathol Res Pract. 2020;216(2):152803. doi: 10.1016/j.prp.2019.152803. [DOI] [PubMed] [Google Scholar]
- 109.Huang T, Wang X, Yang X, Ji J, Wang Q, Yue X, Dong Z. Long non-coding RNA DUXAP8 enhances renal cell carcinoma progression via downregulating miR-126. Med Sci Monit. 2018;24:7340–7347. doi: 10.12659/MSM.910054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Cheng T, Shuang W, Ye D, Zhang W, Yang Z, Fang W, Xu H, Gu M, Xu W, Guan C. SNHG16 promotes cell proliferation and inhibits cell apoptosis via regulation of the miR-1303-p/STARD9 axis in clear cell renal cell carcinoma. Cell Signal. 2021;84:110013. doi: 10.1016/j.cellsig.2021.110013. [DOI] [PubMed] [Google Scholar]
- 111.Zeng X, Hu Z, Ke X, Tang H, Wu B, Wei X, Liu Z. Long noncoding RNA DLX6-AS1 promotes renal cell carcinoma progression via miR-26a/PTEN axis. Cell Cycle. 2017;16(22):2212–2219. doi: 10.1080/15384101.2017.1361072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Hong Y, Yuan Z, Huang R, Wu Z, Li Y. The long noncoding RNA EMBP1 inhibits the tumor suppressor miR-9-5p and promotes renal cell carcinoma tumorigenesis. Nefrologia. 2020;40(4):429–439. doi: 10.1016/j.nefro.2019.12.004. [DOI] [PubMed] [Google Scholar]
- 113.Han C, Xu B, Zhou L, Li L, Lu C, Yu GP, Liu YS. LINC02738 participates in the development of kidney cancer through the miR-20b/Sox4 Axis. Onco Targets Ther. 2020;13:10185–10196. doi: 10.2147/OTT.S262046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wang S, Yang X, Xie W, Fu S, Chen Q, Li Z, Zhang Z, Sun T, Gong B, Ma M. LncRNA GAPLINC promotes renal cell cancer tumorigenesis by targeting the miR-135b-5p/CSF1 axis. Front Oncol. 2021;11:718532. doi: 10.3389/fonc.2021.718532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Wu J, Liu T, Sun L, Zhang S, Dong G. Long noncoding RNA SNHG4 promotes renal cell carcinoma tumorigenesis and invasion by acting as ceRNA to sponge miR-204-5p and upregulate RUNX2. Cancer Cell Int. 2020;20:514. doi: 10.1186/s12935-020-01606-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lin K, Chen H, Su C, Zhu H, Lai C, Shi Y. Long non-coding RNA TTN-AS1 serves as a competing endogenous rna of mir-195 to facilitate clear cell renal cell carcinoma progression. Cancer Manag Res. 2020;12:3091–3097. doi: 10.2147/CMAR.S249456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Zhang G, Liu SL, Yi WT, Dong YP, Wan YX. Long noncoding RNA ZFPM2-AS1 regulates renal cell carcinoma progression via miR-130a-3p/ESCO2. Kaohsiung J Med Sci. 2022 doi: 10.1002/kjm2.12527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Li YZ, Zhu HC, Du Y, Zhao HC, Wang L. Silencing lncRNA SLC16A1-AS1 induced ferroptosis in renal cell carcinoma through miR-143-3p/SLC7A11 signaling. Technol Cancer Res Treat. 2022;21:15330338221077803. doi: 10.1177/15330338221077803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Liu Q, Lei C. LINC01232 serves as a novel biomarker and promotes tumour progression by sponging miR-204-5p and upregulating RAB22A in clear cell renal cell carcinoma. Ann Med. 2021;53(1):2153–2164. doi: 10.1080/07853890.2021.2001563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Wang D, Zhu X, Siqin B, Ren C, Yi F. Long non-coding RNA CYTOR modulates cancer progression through miR-136-5p/MAT2B axis in renal cell carcinoma. Toxicol Appl Pharmacol. 2022;447:116067. doi: 10.1016/j.taap.2022.116067. [DOI] [PubMed] [Google Scholar]
- 121.Luo Y, Liu F, Yan C, Qu W, Zhu L, Guo Z, Zhou F, Zhang W. Long non-coding RNA CASC19 sponges microRNA-532 and promotes oncogenicity of clear cell renal cell carcinoma by increasing ETS1 expression. Cancer Manag Res. 2020;12:2195–2207. doi: 10.2147/CMAR.S242472. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 122.Ye Z, Duan J, Wang L, Ji Y, Qiao B. LncRNA-LET inhibits cell growth of clear cell renal cell carcinoma by regulating miR-373-3p. Cancer Cell Int. 2019;19:311. doi: 10.1186/s12935-019-1008-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chu HY, Chen Z, Wang L, Zhang ZK, Tan X, Liu S, Zhang BT, Lu A, Yu Y, Zhang G. Dickkopf-1: a promising target for cancer immunotherapy. Front Immunol. 2021;12:658097. doi: 10.3389/fimmu.2021.658097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Xu Q, Krause M, Samoylenko A, Vainio S. Wnt signaling in renal cell carcinoma. Cancers. 2016 doi: 10.3390/cancers8060057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Seo DW, Li H, Guedez L, Wingfield PT, Diaz T, Salloum R, Wei BY, Stetler-Stevenson WG. TIMP-2 mediated inhibition of angiogenesis: an MMP-independent mechanism. Cell. 2003;114(2):171–180. doi: 10.1016/s0092-8674(03)00551-8. [DOI] [PubMed] [Google Scholar]
- 126.Lu GJ, Dong YQ, Zhang QM, Di WY, Jiao LY, Gao QZ, Zhang CG. miRNA-221 promotes proliferation, migration and invasion by targeting TIMP2 in renal cell carcinoma. Int J Clin Exp Pathol. 2015;8(5):5224–5229. [PMC free article] [PubMed] [Google Scholar]
- 127.Wei D, Zhang G, Zhu Z, Zheng Y, Yan F, Pan C, Wang Z, Li X, Wang F, Meng P, et al. Nobiletin inhibits cell viability via the SRC/AKT/STAT3/YY1AP1 pathway in human renal carcinoma cells. Front Pharmacol. 2019;10:690. doi: 10.3389/fphar.2019.00690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Zeng J, Li Y, Wang Y, Xie G, Feng Q, Yang Y, Feng J. lncRNA 00312 attenuates cell proliferation and invasion and promotes apoptosis in renal cell carcinoma via miR-34a-5p/ASS1 axis. Oxid Med Cell Longev. 2020;2020:5737289. doi: 10.1155/2020/5737289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Liu L, Pang X, Shang W, Xie H, Feng Y, Feng G. Long non-coding RNA GAS5 sensitizes renal cell carcinoma to sorafenib via miR-21/SOX5 pathway. Cell Cycle. 2019;18(3):257–263. doi: 10.1080/15384101.2018.1475826. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 130.Qi Y, Ma Y, Peng Z, Wang L, Li L, Tang Y, He J, Zheng J. Long noncoding RNA PENG upregulates PDZK1 expression by sponging miR-15b to suppress clear cell renal cell carcinoma cell proliferation. Oncogene. 2020;39(22):4404–4420. doi: 10.1038/s41388-020-1297-1. [DOI] [PubMed] [Google Scholar]
- 131.He H, Dai J, Zhuo R, Zhao J, Wang H, Sun F, Zhu Y, Xu D. Study on the mechanism behind lncRNA MEG3 affecting clear cell renal cell carcinoma by regulating miR-7/RASL11B signaling. J Cell Physiol. 2018;233(12):9503–9515. doi: 10.1002/jcp.26849. [DOI] [PubMed] [Google Scholar]
- 132.Zhang R, Zhang W, Xu B, Lv C, Hou J, Zhang G. Long intergenic non-coding RNA 1939 eliminates proliferation and migration of human renal cell carcinoma (RCC) cells by down-regulation of miR-154. Artif Cells Nanomed Biotechnol. 2020;48(1):695–702. doi: 10.1080/21691401.2020.1725024. [DOI] [PubMed] [Google Scholar]
- 133.Wang J, Zou Y, Du B, Li W, Yu G, Li L, Zhou L, Gu X, Song S, Liu Y, et al. SNP-mediated lncRNA-ENTPD3-AS1 upregulation suppresses renal cell carcinoma via miR-155/HIF-1alpha signaling. Cell Death Dis. 2021;12(7):672. doi: 10.1038/s41419-021-03958-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sun K, Jia Z, Duan R, Yan Z, Jin Z, Yan L, Li Q, Yang J. Long non-coding RNA XIST regulates miR-106b-5p/P21 axis to suppress tumor progression in renal cell carcinoma. Biochem Biophys Res Commun. 2019;510(3):416–420. doi: 10.1016/j.bbrc.2019.01.116. [DOI] [PubMed] [Google Scholar]
- 135.Li M, Yin B, Chen M, Peng J, Mu X, Deng Z, Xiao J, Li W, Fan J. Downregulation of the lncRNA ASB16-AS1 decreases LARP1 expression and promotes clear cell renal cell carcinoma progression via miR-185-5p/miR-214-3p. Front Oncol. 2020;10:617105. doi: 10.3389/fonc.2020.617105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Liu Y, Wang J, Shou Y, Xu W, Huang Z, Xu J, Chen K, Liu J, Liu D, Liang H, et al. Restoring the epigenetically silenced lncRNA COL18A1-AS1 represses ccRCC progression by lipid browning via miR-1286/KLF12 axis. Cell Death Dis. 2022;13(7):578. doi: 10.1038/s41419-022-04996-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.He ZH, Qin XH, Zhang XL, Yi JW, Han JY. Long noncoding RNA GIHCG is a potential diagnostic and prognostic biomarker and therapeutic target for renal cell carcinoma. Eur Rev Med Pharmacol Sci. 2018;22(1):46–54. doi: 10.26355/eurrev_201801_14099. [DOI] [PubMed] [Google Scholar]
- 138.Wu Y, Wang YQ, Weng WW, Zhang QY, Yang XQ, Gan HL, Yang YS, Zhang PP, Sun MH, Xu MD, et al. A serum-circulating long noncoding RNA signature can discriminate between patients with clear cell renal cell carcinoma and healthy controls. Oncogenesis. 2016;5:e192. doi: 10.1038/oncsis.2015.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Wang G, Zhang ZJ, Jian WG, Liu PH, Xue W, Wang TD, Meng YY, Yuan C, Li HM, Yu YP, et al. Novel long noncoding RNA OTUD6B-AS1 indicates poor prognosis and inhibits clear cell renal cell carcinoma proliferation via the Wnt/beta-catenin signaling pathway. Mol Cancer. 2019;18(1):15. doi: 10.1186/s12943-019-0942-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Yao J, Chen Y, Wang Y, Liu S, Yuan X, Pan F, Geng P. Decreased expression of a novel lncRNA CADM1-AS1 is associated with poor prognosis in patients with clear cell renal cell carcinomas. Int J Clin Exp Pathol. 2014;7(6):2758–2767. [PMC free article] [PubMed] [Google Scholar]
- 141.Qian M, Zheng JL, Kang N, Su YL. Down-regulation of long noncoding RNA PGM5-AS1 correlates with tumor progression and predicts poor prognosis in clear cell renal cell carcinoma. Eur Rev Med Pharmacol Sci. 2019;23(24):10685–10690. doi: 10.26355/eurrev_201912_19767. [DOI] [PubMed] [Google Scholar]
- 142.Su H, Sun T, Wang H, Shi G, Zhang H, Sun F, Ye D. Decreased TCL6 expression is associated with poor prognosis in patients with clear cell renal cell carcinoma. Oncotarget. 2017;8(4):5789–5799. doi: 10.18632/oncotarget.11011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Cheng G, Li M, Ma X, Nan F, Zhang L, Yan Z, Li H, Zhang G, Han Y, Xie L, et al. Systematic analysis of microRNA biomarkers for diagnosis, prognosis, and therapy in patients with clear cell renal cell carcinoma. Front Oncol. 2020;10:543817. doi: 10.3389/fonc.2020.543817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Iwamoto H, Kanda Y, Sejima T, Osaki M, Okada F, Takenaka A. Serum miR-210 as a potential biomarker of early clear cell renal cell carcinoma. Int J Oncol. 2014;44(1):53–58. doi: 10.3892/ijo.2013.2169. [DOI] [PubMed] [Google Scholar]
- 145.Fedorko M, Stanik M, Iliev R, Redova-Lojova M, Machackova T, Svoboda M, Pacik D, Dolezel J, Slaby O. Combination of MiR-378 and MiR-210 serum levels enables sensitive detection of renal cell carcinoma. Int J Mol Sci. 2015;16(10):23382–23389. doi: 10.3390/ijms161023382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Redova M, Poprach A, Nekvindova J, Iliev R, Radova L, Lakomy R, Svoboda M, Vyzula R, Slaby O. Circulating miR-378 and miR-451 in serum are potential biomarkers for renal cell carcinoma. J Transl Med. 2012;10:55. doi: 10.1186/1479-5876-10-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Faragalla H, Youssef YM, Scorilas A, Khalil B, White NM, Mejia-Guerrero S, Khella H, Jewett MA, Evans A, Lichner Z, et al. The clinical utility of miR-21 as a diagnostic and prognostic marker for renal cell carcinoma. J Mol Diagn. 2012;14(4):385–392. doi: 10.1016/j.jmoldx.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 148.Yadav S, Khandelwal M, Seth A, Saini AK, Dogra PN, Sharma A. Serum microRNA expression profiling: potential diagnostic implications of a panel of serum microRNAs for clear cell renal cell cancer. Urology. 2017;104:64–69. doi: 10.1016/j.urology.2017.03.013. [DOI] [PubMed] [Google Scholar]
- 149.Sun C, Zhou Z, Shi H, Li F, Zhang G. Identification of long noncoding RNA APOC1P1 as an oncogene in clear cell renal cell carcinoma. Dis Markers. 2019;2019:2814058. doi: 10.1155/2019/2814058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Ellinger J, Alam J, Rothenburg J, Deng M, Schmidt D, Syring I, Miersch H, Perner S, Muller SC. The long non-coding RNA lnc-ZNF180-2 is a prognostic biomarker in patients with clear cell renal cell carcinoma. Am J Cancer Res. 2015;5(9):2799–2807. [PMC free article] [PubMed] [Google Scholar]
- 151.Blondeau JJ, Deng M, Syring I, Schrodter S, Schmidt D, Perner S, Muller SC, Ellinger J. Identification of novel long non-coding RNAs in clear cell renal cell carcinoma. Clin Epigenetics. 2015;7:10. doi: 10.1186/s13148-015-0047-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Cox A, Tolkach Y, Kristiansen G, Ritter M, Ellinger J. The lncRNA Fer1L4 is an adverse prognostic parameter in clear-cell renal-cell carcinoma. Clin Transl Oncol. 2020;22(9):1524–1531. doi: 10.1007/s12094-020-02291-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Huang G, Li X, Chen Z, Wang J, Zhang C, Chen X, Peng X, Liu K, Zhao L, Lai Y, et al. A Three-microRNA panel in serum: serving as a potential diagnostic biomarker for renal cell carcinoma. Pathol Oncol Res. 2020;26(4):2425–2434. doi: 10.1007/s12253-020-00842-y. [DOI] [PubMed] [Google Scholar]
- 154.Shiomi E, Sugai T, Ishida K, Osakabe M, Tsuyukubo T, Kato Y, Takata R, Obara W. Analysis of expression patterns of microRNAS that are closely associated with renal carcinogenesis. Front Oncol. 2019;9:431. doi: 10.3389/fonc.2019.00431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Bhat NS, Colden M, Dar AA, Saini S, Arora P, Shahryari V, Yamamura S, Tanaka Y, Kato T, Majid S, et al. MicroRNA-720 Regulates E-cadherin-alphaE-catenin complex and promotes renal cell carcinoma. Mol Cancer Ther. 2017;16(12):2840–2848. doi: 10.1158/1535-7163.MCT-17-0400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Chen X, Ruan A, Wang X, Han W, Wang R, Lou N, Ruan H, Qiu B, Yang H, Zhang X. miR-129-3p, as a diagnostic and prognostic biomarker for renal cell carcinoma, attenuates cell migration and invasion via downregulating multiple metastasis-related genes. J Cancer Res Clin Oncol. 2014;140(8):1295–1304. doi: 10.1007/s00432-014-1690-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Lokeshwar SD, Talukder A, Yates TJ, Hennig MJP, Garcia-Roig M, Lahorewala SS, Mullani NN, Klaassen Z, Kava BR, Manoharan M, et al. Molecular characterization of renal cell carcinoma: a potential three-microrna prognostic signature. Cancer Epidemiol Biomarkers Prev. 2018;27(4):464–472. doi: 10.1158/1055-9965.EPI-17-0700. [DOI] [PubMed] [Google Scholar]
- 158.Peng X, Pan X, Liu K, Zhang C, Zhao L, Li H, Guan X, Xu W, Xu J, Zhang F, et al. miR-142-3p as a novel biomarker for predicting poor prognosis in renal cell carcinoma patients after surgery. Int J Biol Markers. 2019;34(3):302–308. doi: 10.1177/1724600819866456. [DOI] [PubMed] [Google Scholar]
- 159.Fedorko M, Pacik D, Wasserbauer R, Juracek J, Varga G, Ghazal M, Nussir MI. MicroRNAs in the pathogenesis of renal cell carcinoma and their diagnostic and prognostic utility as cancer biomarkers. Int J Biol Markers. 2016;31(1):e26–37. doi: 10.5301/jbm.5000174. [DOI] [PubMed] [Google Scholar]
- 160.Xie J, Zhong Y, Chen R, Li G, Luo Y, Yang J, Sun Z, Liu Y, Liu P, Wang N, et al. Serum long non-coding RNA LINC00887 as a potential biomarker for diagnosis of renal cell carcinoma. FEBS Open Bio. 2020;10(9):1802–1809. doi: 10.1002/2211-5463.12930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Heinemann FG, Tolkach Y, Deng M, Schmidt D, Perner S, Kristiansen G, Muller SC, Ellinger J. Serum miR-122-5p and miR-206 expression: non-invasive prognostic biomarkers for renal cell carcinoma. Clin Epigenetics. 2018;10:11. doi: 10.1186/s13148-018-0444-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Kowalik CG, Palmer DA, Sullivan TB, Teebagy PA, Dugan JM, Libertino JA, Burks EJ, Canes D, Rieger-Christ KM. Profiling microRNA from nephrectomy and biopsy specimens: predictors of progression and survival in clear cell renal cell carcinoma. BJU Int. 2017;120(3):428–440. doi: 10.1111/bju.13886. [DOI] [PubMed] [Google Scholar]
- 163.Chen X, Li R, Li X, Peng X, Zhang C, Liu K, Huang G, Lai Y. Identification of a four-microRNA panel in serum for screening renal cell carcinoma. Pathol Res Pract. 2021;227:153625. doi: 10.1016/j.prp.2021.153625. [DOI] [PubMed] [Google Scholar]
- 164.Wulfken LM, Moritz R, Ohlmann C, Holdenrieder S, Jung V, Becker F, Herrmann E, Walgenbach-Brunagel G, von Ruecker A, Muller SC, et al. MicroRNAs in renal cell carcinoma: diagnostic implications of serum miR-1233 levels. PLoS ONE. 2011;6(9):e25787. doi: 10.1371/journal.pone.0025787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Zhang W, Ni M, Su Y, Wang H, Zhu S, Zhao A, Li G. MicroRNAs in serum exosomes as potential biomarkers in clear-cell renal cell carcinoma. Eur Urol Focus. 2018;4(3):412–419. doi: 10.1016/j.euf.2016.09.007. [DOI] [PubMed] [Google Scholar]
- 166.Zhao A, Li G, Peoc'h M, Genin C, Gigante M. Serum miR-210 as a novel biomarker for molecular diagnosis of clear cell renal cell carcinoma. Exp Mol Pathol. 2013;94(1):115–120. doi: 10.1016/j.yexmp.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 167.Wang X, Wang T, Chen C, Wu Z, Bai P, Li S, Chen B, Liu R, Zhang K, Li W, et al. Serum exosomal miR-210 as a potential biomarker for clear cell renal cell carcinoma. J Cell Biochem. 2018 doi: 10.1002/jcb.27347. [DOI] [PubMed] [Google Scholar]
- 168.Yang Q, Liu J, Liang Y, Wang C, Han J, Zhu L, Yuan S, Sun Q, Zhang H. Correlation between serum level of miRNA-106a expression with clinicopathological characteristics and prognosis of patients with renal cell carcinoma. Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 2021;38(7):652–655. doi: 10.3760/cma.j.cn511374-20200430-00317. [DOI] [PubMed] [Google Scholar]
- 169.Mytsyk Y, Dosenko V, Borys Y, Kucher A, Gazdikova K, Busselberg D, Caprnda M, Kruzliak P, Farooqi AA, Lubov M. MicroRNA-15a expression measured in urine samples as a potential biomarker of renal cell carcinoma. Int Urol Nephrol. 2018;50(5):851–859. doi: 10.1007/s11255-018-1841-x. [DOI] [PubMed] [Google Scholar]
- 170.Outeiro-Pinho G, Barros-Silva D, Aznar E, Sousa AI, Vieira-Coimbra M, Oliveira J, Goncalves CS, Costa BM, Junker K, Henrique R, et al. MicroRNA-30a-5p(me): a novel diagnostic and prognostic biomarker for clear cell renal cell carcinoma in tissue and urine samples. J Exp Clin Cancer Res. 2020;39(1):98. doi: 10.1186/s13046-020-01600-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Shi L, Wang M, Li H, You P. MicroRNAs in body fluids: a more promising biomarker for clear cell renal cell carcinoma. Cancer Manag Res. 2021;13:7663–7675. doi: 10.2147/CMAR.S330881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Song S, Long M, Yu G, Cheng Y, Yang Q, Liu J, Wang Y, Sheng J, Wang L, Wang Z, et al. Urinary exosome miR-30c-5p as a biomarker of clear cell renal cell carcinoma that inhibits progression by targeting HSPA5. J Cell Mol Med. 2019;23(10):6755–6765. doi: 10.1111/jcmm.14553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Cochetti G, Cari L, Nocentini G, Maula V, Suvieri C, Cagnani R, Rossi De Vermandois JA, Mearini E. Detection of urinary miRNAs for diagnosis of clear cell renal cell carcinoma. Sci Rep. 2020;10(1):21290. doi: 10.1038/s41598-020-77774-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Fedorko M, Juracek J, Stanik M, Svoboda M, Poprach A, Buchler T, Pacik D, Dolezel J, Slaby O. Detection of let-7 miRNAs in urine supernatant as potential diagnostic approach in non-metastatic clear-cell renal cell carcinoma. Biochem Med. 2017;27(2):411–417. doi: 10.11613/BM.2017.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Cochetti G, Cari L, Maula V, Cagnani R, Paladini A, Del Zingaro M, Nocentini G, Mearini E. Validation in an independent cohort of MiR-122, MiR-1271, and MiR-15b as urinary biomarkers for the potential early diagnosis of clear cell renal cell carcinoma. Cancers. 2022;14(5):1112. doi: 10.3390/cancers14051112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Dias F, Teixeira AL, Ferreira M, Adem B, Bastos N, Vieira J, Fernandes M, Sequeira MI, Mauricio J, Lobo F, et al. Plasmatic miR-210, miR-221 and miR-1233 profile: potential liquid biopsies candidates for renal cell carcinoma. Oncotarget. 2017;8(61):103315–103326. doi: 10.18632/oncotarget.21733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Xiao CT, Lai WJ, Zhu WA, Wang H. MicroRNA derived from circulating exosomes as noninvasive biomarkers for diagnosing renal cell carcinoma. Onco Targets Ther. 2020;13:10765–10774. doi: 10.2147/OTT.S271606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Lou N, Ruan AM, Qiu B, Bao L, Xu YC, Zhao Y, Sun RL, Zhang ST, Xu GH, Ruan HL, et al. miR-144–3p as a novel plasma diagnostic biomarker for clear cell renal cell carcinoma. Urol Oncol. 2017;35(1):36. doi: 10.1016/j.urolonc.2016.07.012. [DOI] [PubMed] [Google Scholar]
- 179.Hsieh JJ, Purdue MP, Signoretti S, Swanton C, Albiges L, Schmidinger M, Heng DY, Larkin J, Ficarra V. Renal cell carcinoma. Nat Rev Dis Primers. 2017;3:17009. doi: 10.1038/nrdp.2017.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Makhov P, Joshi S, Ghatalia P, Kutikov A, Uzzo RG, Kolenko VM. Resistance to systemic therapies in clear cell renal cell carcinoma: mechanisms and management strategies. Mol Cancer Ther. 2018;17(7):1355–1364. doi: 10.1158/1535-7163.MCT-17-1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Chen Y, He J, Su C, Wang H, Chen Y, Guo W, Li Y, Ding G. LINC00461 affects the survival of patients with renal cell carcinoma by acting as a competing endogenous RNA for microRNA942. Oncol Rep. 2019;42(5):1924–1934. doi: 10.3892/or.2019.7311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Zhai W, Sun Y, Guo C, Hu G, Wang M, Zheng J, Lin W, Huang Q, Li G, Zheng J, et al. LncRNA-SARCC suppresses renal cell carcinoma (RCC) progression via altering the androgen receptor(AR)/miRNA-143-3p signals. Cell Death Differ. 2017;24(9):1502–1517. doi: 10.1038/cdd.2017.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Qu L, Ding J, Chen C, Wu ZJ, Liu B, Gao Y, Chen W, Liu F, Sun W, Li XF, et al. Exosome-transmitted lncARSR promotes sunitinib resistance in renal cancer by acting as a competing endogenous RNA. Cancer Cell. 2016;29(5):653–668. doi: 10.1016/j.ccell.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 184.Li D, Li C, Chen Y, Teng L, Cao Y, Wang W, Pan H, Xu Y, Yang D. LncRNA HOTAIR induces sunitinib resistance in renal cancer by acting as a competing endogenous RNA to regulate autophagy of renal cells. Cancer Cell Int. 2020;20:338. doi: 10.1186/s12935-020-01419-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Zhou X, Zeng B, Li Y, Wang H, Zhang X. LINC02532 contributes to radiosensitivity in clear cell renal cell carcinoma through the miR-654–5p/YY1 Axis. Molecules. 2021 doi: 10.3390/molecules26227040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Li W, Yang D, Zhang Y, Zhao S, Li D, Liu M. Long noncoding RNA PLK1S1 was associated with renal cell carcinoma progression by interacting with microRNA653 and altering CXC chemokine receptor 5 expression. Oncol Rep. 2020;44(5):1985–1996. doi: 10.3892/or.2020.7742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Liu F, Chen N, Gong Y, Xiao R, Wang W, Pan Z. The long non-coding RNA NEAT1 enhances epithelial-to-mesenchymal transition and chemoresistance via the miR-34a/c-Met axis in renal cell carcinoma. Oncotarget. 2017;8(38):62927–62938. doi: 10.18632/oncotarget.17757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Zhai W, Sun Y, Jiang M, Wang M, Gasiewicz TA, Zheng J, Chang C. Differential regulation of LncRNA-SARCC suppresses VHL-mutant RCC cell proliferation yet promotes VHL-normal RCC cell proliferation via modulating androgen receptor/HIF-2alpha/C-MYC axis under hypoxia. Oncogene. 2016;35(37):4866–4880. doi: 10.1038/onc.2016.19. [DOI] [PubMed] [Google Scholar]
- 189.Grimm D, Bauer J, Wise P, Kruger M, Simonsen U, Wehland M, Infanger M, Corydon TJ. The role of SOX family members in solid tumours and metastasis. Semin Cancer Biol. 2020;67(Pt 1):122–153. doi: 10.1016/j.semcancer.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 190.Zhao L, Li R, Qiu JZ, Yu JB, Cao Y, Yuan RT. YY1-mediated PTEN dephosphorylation antagonizes IR-induced DNA repair contributing to tongue squamous cell carcinoma radiosensitization. Mol Cell Probes. 2020;53:101577. doi: 10.1016/j.mcp.2020.101577. [DOI] [PubMed] [Google Scholar]
- 191.Ide H, Mizushima T, Jiang G, Goto T, Nagata Y, Teramoto Y, Inoue S, Li Y, Kashiwagi E, Baras AS, et al. FOXO1 as a tumor suppressor inactivated via AR/ERbeta signals in urothelial cells. Endocr Relat Cancer. 2020;27(4):231–244. doi: 10.1530/ERC-20-0004. [DOI] [PubMed] [Google Scholar]
- 192.Gan B, Lim C, Chu G, Hua S, Ding Z, Collins M, Hu J, Jiang S, Fletcher-Sananikone E, Zhuang L, et al. FoxOs enforce a progression checkpoint to constrain mTORC1-activated renal tumorigenesis. Cancer Cell. 2010;18(5):472–484. doi: 10.1016/j.ccr.2010.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Quail DF, Joyce JA. Microenvironmental regulation of tumor progression and metastasis. Nat Med. 2013;19(11):1423–1437. doi: 10.1038/nm.3394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Jian Y, Yang K, Sun X, Zhao J, Huang K, Aldanakh A, Xu Z, Wu H, Xu Q, Zhang L, et al. Current advance of immune evasion mechanisms and emerging immunotherapies in renal cell carcinoma. Front Immunol. 2021;12:639636. doi: 10.3389/fimmu.2021.639636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Hinshaw DC, Shevde LA. The tumor microenvironment innately modulates cancer progression. Cancer Res. 2019;79(18):4557–4566. doi: 10.1158/0008-5472.CAN-18-3962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Wang J, Sun J, Liu LN, Flies DB, Nie X, Toki M, Zhang J, Song C, Zarr M, Zhou X, et al. Siglec-15 as an immune suppressor and potential target for normalization cancer immunotherapy. Nat Med. 2019;25(4):656–666. doi: 10.1038/s41591-019-0374-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Setoguchi R, Hori S, Takahashi T, Sakaguchi S. Homeostatic maintenance of natural Foxp3(+) CD25(+) CD4(+) regulatory T cells by interleukin (IL)-2 and induction of autoimmune disease by IL-2 neutralization. J Exp Med. 2005;201(5):723–735. doi: 10.1084/jem.20041982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Zhang W, Zheng X, Yu Y, Zheng L, Lan J, Wu Y, Liu H, Zhao A, Huang H, Chen W. Renal cell carcinoma-derived exosomes deliver lncARSR to induce macrophage polarization and promote tumor progression via STAT3 pathway. Int J Biol Sci. 2022;18(8):3209–3222. doi: 10.7150/ijbs.70289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Noubissi Nzeteu GA, Geismann C, Arlt A, Hoogwater FJH, Nijkamp MW, Meyer NH, Bockhorn M. Role of epithelial-to-mesenchymal transition for the generation of circulating tumors cells and cancer cell dissemination. Cancers. 2022 doi: 10.3390/cancers14225483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Lane J, Martin TA, Mansel RE, Jiang WG. The expression and prognostic value of the guanine nucleotide exchange factors (GEFs) Trio, Vav1 and TIAM-1 in human breast cancer. Int Semin Surg Oncol. 2008;5:23. doi: 10.1186/1477-7800-5-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Shan G, Tang T, Qian H, Xia Y. Expression of Tiam1 and Rac1 proteins in renal cell carcinoma and its clinical-pathological features. Int J Clin Exp Pathol. 2017;10(11):11114–11121. [PMC free article] [PubMed] [Google Scholar]
- 202.Lopez-Colome AM, Lee-Rivera I, Benavides-Hidalgo R, Lopez E. Paxillin: a crossroad in pathological cell migration. J Hematol Oncol. 2017;10(1):50. doi: 10.1186/s13045-017-0418-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Najafi M, Farhood B, Mortezaee K. Extracellular matrix (ECM) stiffness and degradation as cancer drivers. J Cell Biochem. 2019;120(3):2782–2790. doi: 10.1002/jcb.27681. [DOI] [PubMed] [Google Scholar]
- 204.Jin C, Shi L, Li K, Liu W, Qiu Y, Zhao Y, Zhao B, Li Z, Li Y, Zhu Q. Mechanism of tumor-derived extracellular vesicles in regulating renal cell carcinoma progression by the delivery of MALAT1. Oncol Rep. 2021;46(3):1. doi: 10.3892/or.2021.8138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Botti G, Scognamiglio G, Aquino G, Liguori G, Cantile M. HOTAIRLncRNA in tumor microenvironment: what role? Int J Mol Sci. 2019;20(9):2278. doi: 10.3390/ijms20092279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Pan Y, Lu X, Shu G, Cen J, Lu J, Zhou M, Huang K, Dong J, Li J, Lin H, et al. Extracellular vesicle-mediated transfer of LncRNA IGFL2-AS1 confers sunitinib resistance in renal cell carcinoma. Cancer Res. 2023;83(1):103–116. doi: 10.1158/0008-5472.CAN-21-3432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Wortzel I, Dror S, Kenific CM, Lyden D. Exosome-mediated metastasis: communication from a distance. Dev Cell. 2019;49(3):347–360. doi: 10.1016/j.devcel.2019.04.011. [DOI] [PubMed] [Google Scholar]
- 208.Wu K, Zhang L, Lin Y, Yang K, Cheng Y. Inhibition of gamma-secretase induces G2/M arrest and triggers apoptosis in renal cell carcinoma. Oncol Lett. 2014;8(1):55–61. doi: 10.3892/ol.2014.2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Moe GR, Steirer LM, Lee JA, Shivakumar A, Bolanos AD. A cancer-unique glycan: de-N-acetyl polysialic acid (dPSA) linked to cell surface nucleolin depends on re-expression of the fetal polysialyltransferase ST8SIA2 gene. J Exp Clin Cancer Res. 2021;40(1):293. doi: 10.1186/s13046-021-02099-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Liu L, Du X, Fang J, Zhao J, Guo Y, Zhao Y, Zou C, Yan X, Li W. Development of an interferon gamma response-related signature for prediction of survival in clear cell renal cell carcinoma. J Inflamm Res. 2021;14:4969–4985. doi: 10.2147/JIR.S334041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Ma Y, Liu Y, Pu Y, Cui M, Mao Z, Li Z, He L, Wu M, Wang J. LncRNA IGFL2-AS1 functions as a ceRNA in regulating ARPP19 through competitive binding to miR-802 in gastric cancer. Mol Carcinogen. 2020;59(3):311–322. doi: 10.1002/mc.23155. [DOI] [PubMed] [Google Scholar]
- 212.Meng D, Jia R, Yuan S, Wei M, Bao X, Zhu C, Wang W, Li Z. Research progress on the circRNA-mediated regulation of tumor angiogenesis through ceRNA mechanisms (Review) Oncol Rep. 2023;49(1):1. doi: 10.3892/or.2022.8449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Ghafouri-Fard S, Shoorei H, Mohaqiq M, Taheri M. Non-coding RNAs regulate angiogenic processes. Vascul Pharmacol. 2020;133–134:106778. doi: 10.1016/j.vph.2020.106778. [DOI] [PubMed] [Google Scholar]
- 214.Jacobsen J, Rasmuson T, Grankvist K, Ljungberg B. Vascular endothelial growth factor as prognostic factor in renal cell carcinoma. J Urol. 2000;163(1):343–347. [PubMed] [Google Scholar]
- 215.Levine RJ, Maynard SE, Qian C, Lim KH, England LJ, Yu KF, Schisterman EF, Thadhani R, Sachs BP, Epstein FH, et al. Circulating angiogenic factors and the risk of preeclampsia. N Engl J Med. 2004;350(7):672–683. doi: 10.1056/NEJMoa031884. [DOI] [PubMed] [Google Scholar]
- 216.Cechova M, Chocholaty M, Babjuk M, Zima T, Havlova K, Koldova M, Schmidt M, Kalousova M. Diagnostic and prognostic value of placental growth factor serum concentration in clear cell renal cell carcinoma. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2021;165(4):375–379. doi: 10.5507/bp.2021.003. [DOI] [PubMed] [Google Scholar]
- 217.Faitova J. Fibroblast growth factor-2. Cesk Fysiol. 2004;53(3):92–101. [PubMed] [Google Scholar]
- 218.Adamek A, Kasprzak A. Insulin-like growth factor (IGF) system in liver diseases. Int J Mol Sci. 2018 doi: 10.3390/ijms19051308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Wang X, Khalil RA. Matrix metalloproteinases, vascular remodeling, and vascular disease. Adv Pharmacol. 2018;81:241–330. doi: 10.1016/bs.apha.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Scheau C, Badarau IA, Costache R, Caruntu C, Mihai GL, Didilescu AC, Constantin C, Neagu M. The role of matrix metalloproteinases in the epithelial-mesenchymal transition of hepatocellular carcinoma. Anal Cell Pathol. 2019;2019:9423907. doi: 10.1155/2019/9423907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Zhang Q, Han Q, Yang Z, Ni Y, Agbana YL, Bai H, Yi Z, Yi X, Kuang Y, Zhu Y. G6PD facilitates clear cell renal cell carcinoma invasion by enhancing MMP2 expression through ROSMAPK axis pathway. Int J Oncol. 2020;57(1):197–212. doi: 10.3892/ijo.2020.5041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Zeng L, Qian J, Luo X, Zhou A, Zhang Z, Fang Q. CHSY1 promoted proliferation and suppressed apoptosis in colorectal cancer through regulation of the NFkappaB and/or caspase-3/7 signaling pathway. Oncol Lett. 2018;16(5):6140–6146. doi: 10.3892/ol.2018.9385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Hamidi AA, Khalili-Tanha G, Nasrpour Navaei Z, Moghbeli M. Long non-coding RNAs as the critical regulators of epithelial mesenchymal transition in colorectal tumor cells: an overview. Cancer Cell Int. 2022;22(1):71. doi: 10.1186/s12935-022-02501-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Augoff K, Hryniewicz-Jankowska A, Tabola R, Stach K. MMP9: a tough target for targeted therapy for cancer. Cancers. 2022 doi: 10.3390/cancers14071847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Prior C, Perez-Gracia JL, Garcia-Donas J, Rodriguez-Antona C, Guruceaga E, Esteban E, Suarez C, Castellano D, del Alba AG, Lozano MD, et al. Identification of tissue microRNAs predictive of sunitinib activity in patients with metastatic renal cell carcinoma. PLoS ONE. 2014;9(1):e86263. doi: 10.1371/journal.pone.0086263. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Wu C, Zhang J. 2020. Long non-conding RNA LOXL1-AS1 sponges miR-589–5p to up-regulate CBX5 expression in renal cell carcinoma. Biosci Rep. [DOI] [PMC free article] [PubMed]
Data Availability Statement
Not applicable.