Abstract
Extensive clinical and experimental evidence suggests that macrophages play a crucial role in cancer immunotherapy. Cluster of differentiation (CD) 47, which is found on both healthy and malignant cells, regulates macrophage-mediated phagocytosis by sending a "don't eat me" signal to the signal regulatory protein alpha (SIRPα) receptor. Increasing evidence demonstrates that blocking CD47 interaction with SIRPα can enhance cancer cell clearance by macrophages. Additionally, inhibition of CD47/SIRPα interaction can increase antigen cross-presentation, leading to T-cell priming and an activated adaptive antitumor immune response. Therefore, inhibiting CD47/SIRPα axis has a significant impact on tumor immunotherapy. Studies on CD47 monoclonal antibodies are at the forefront of research, and impressive results have been obtained. Nevertheless, hematotoxicity, especially anemia, has become the most common adverse effect of the CD47 monoclonal antibody. More specific targeted drugs (i.e., bispecific antibodies, SIRPα/Fc fusion protein antibodies, and small-molecule inhibitors) have been developed to reduce hematotoxicity. Here, we review the present usage of CD47 antagonists for the treatment of lymphomas and hematologic neoplasms from the perspectives of structure, function, and clinical trials, including a comprehensive overview of the drugs in development.
Keywords: CD47, SIRPα, Targeted therapies, Clinical trials, Immunotherapy
Background
Structure, Expression, and function of CD47/SIRPα
Cancer treatment targeting immune checkpoints like programmed cell death receptor-1 (PD-1)/ Programmed cell death ligand-1 (PD-L1) has raised significant interest. Recently, pharmaceutical communities have shifted their attention to the development of new anti-cancer medicines that target innate immunity checkpoints, such as the immune checkpoint of macrophages: a cluster of differentiation (CD) 47/signal regulatory protein alpha (SIRPα) pathway.
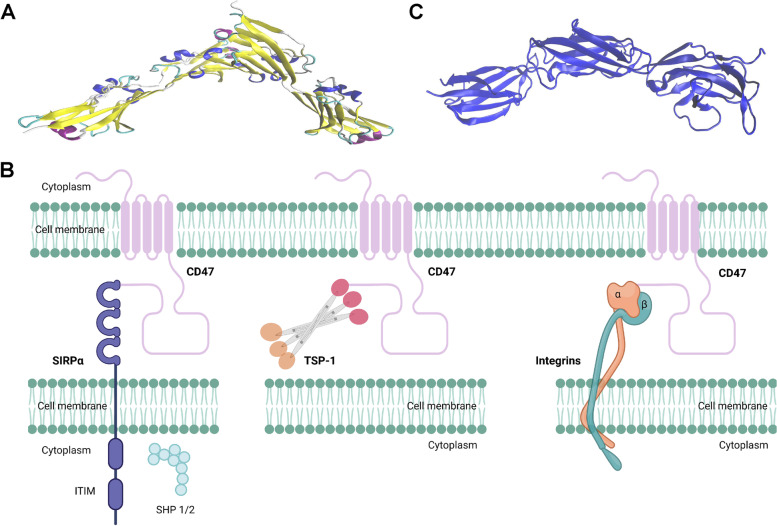
CD47, formerly known as integrin-associated protein, is a 50 kDa plasma membrane molecule. CD47 is composed of an extracellular variable region that interacts with corresponding ligands (Fig. 1A), a transmembrane region comprised of highly hydrophobic transmembrane segments, and a hydrophilic carboxy-terminal intracellular region [1].
Fig. 1.
Overall structures of CD47, SIRPα and CD47 complex. A Structure of the ectodomain of human CD47 (PDB#2VSC). B Interaction of CD47 with three major ligands (SIRPα, TSP-1 and integrin). The figure was created by Biorender.com. C Complete extracellular region of human SIRPα (PDB#2WNG). The structures were reconstructed using VMD software. Abbreviations: CD47, cluster of differentiation 47; IgSF, immunoglobulin superfamily; ITIM, immunoreceptor tyrosine-based inhibitory motif; SHPS-1/2, protein tyrosine phosphatase substrate-1/2; SIRPα, signal-regulatory protein α; TSP-1: thrombospondin-1
CD47 was firstly found as a transmembrane protein of red blood cells (RBCs). Current evidence indicates that CD47 is widely expressed in various normal human cell types, as well as in the membrane of different cancer cell types. In oncology study, CD47 was initially discovered as a tumor antigen in human ovarian cancer, and later was found overexpressed in various lymphomas and hematological tumors, such as non-Hodgkin's lymphomas (NHL) [2], T-cell lymphoma [3], acute myeloid leukemia (AML) and myelodysplastic syndrome (MDS) [4].
CD47 is capable of interacting with a variety of extracellular ligands, including SIRPα, thrombospondin-1 (TSP-1), integrins (α2β1, α4β1, α5β1, and α6β1), SIRPγ, CD36 and CD95, as well as with various intracellular ligands, such as the Gi proteins and Bcl-2/adenovirus E1B 19-kDa interacting protein 3 [1, 5]. Among these ligands, SIRPα, TSP-1 and integrins have been mostly studied (Fig. 1B).
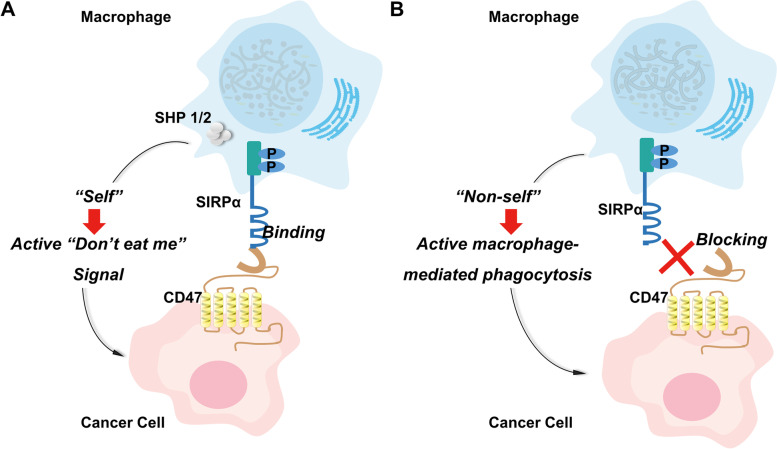
SIRPα is a member of the receptor family of signal regulatory proteins (SIRP) which involves five members (SIRPα, SIRPβ1, SIRPγ, SIRPβ2, and SIRPδ) encoded by a gene cluster located on chromosome 20p13 [6]. Among the family members, SIRPα is composed of an intracellular domain containing an immunoreceptor tyrosine-based inhibitor motif (ITIM), a transmembrane-spanning region, and three extracellular immunoglobulin superfamily domains (Fig. 1C). When CD47 binds to SIRPα, ITIM in the cytoplasmic tail of SIRPα is phosphorylated. Phosphatases including Src homology phosphatase (SHP)-1 and SHP-2, are then recruited and activated (Fig. 1C). CD47 is capable of distinguishing self or non-self cells via attaching to SIRPα which are mainly expressed on myeloid cells (monocytes, granulocytes, dendritic cells, and particularly macrophages [7–9]). When CD47 binds to SIRPα, the "don't eat me" signal is activated, inhibiting macrophage-mediated phagocytosis (Fig. 2) [10, 11].
Fig. 2.
Macrophages distinguish between “self” or “non-self” by binding to SIRPα transmembrane protein on macrophage to form the CD47/SIRPα signaling complex. A CD47 expressed on cancer cell membrane binds to SIRPɑ on macrophage cell membrane to activate the “Don’t eat me” signal and block macrophage phagocytosis of cancer cells. B Blocking CD47-SIRPɑ interaction between cancer cell and macrophage induces phagocytosis by macrophage. Abbreviation: CD47, cluster of differentiation 47; SIRPα, signal-regulatory protein α
TSP-1, which belongs to a thrombospondin family of five secreted glycoproteins, has a high binding affinity to CD47 at picomolar concentrations [12]. The interaction occurs via the C-terminal domain of TSP-1, and plays an important role in maintaining vascular tone, blood pressure, and modulating cardiac response [13]. In addition, several integrins are capable of interacting with CD47. For example, α5β1 is involved in chondrocyte mechanotransduction by binding to CD47 [14]. Dysregulation of αVβ3 and CD47 signaling leads to joint inflammation, cartilage destruction, and progression of osteoarthritis [15].
Function and mechanism of CD47/SIRPα axis in tumor cells
CD47 expression is significantly elevated in leukemic cancer cells and supports these cells in evading phagocytosis by macrophages [16]. Numerous studies have indicated that CD47 is critical for treatment, prognosis, and diagnosis of a variety of malignancies, in which the most notable function of the CD47/SIRPα axis regards cancer therapy.
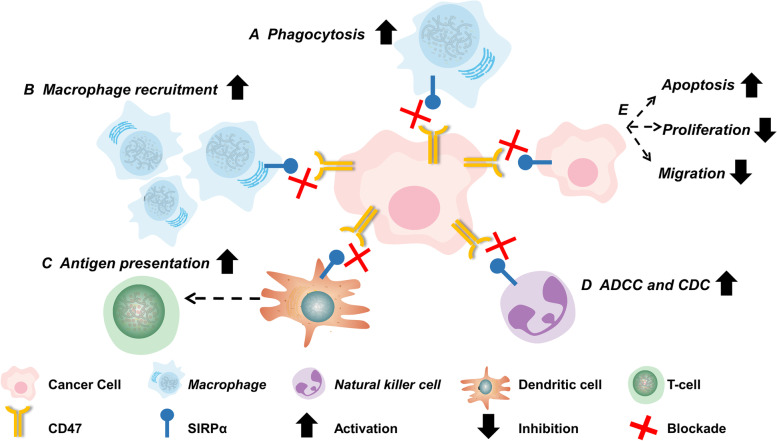
Recent research has shown that the CD47/SIRPα axis controls the destiny of tumor cells. Inhibiting the axis is able to enhance macrophage phagocytosis of tumor cells. So far five primary mechanisms of the CD47/SIRPα axis have been discovered (Fig. 3). Firstly, suppression of the CD47-SIRPα interaction results in macrophage phagocytosis of tumor cells. Full activation of macrophages requires two conditions: blockade of the CD47 "don't eat me" signal, and activation of the Fc receptor "eat me" signal. The presence of either can only provide a limited macrophage activation [17]. Secondly, blocking the CD47/SIRPα axis can transform tumor-associated macrophages into an antitumor state, and increase tumor macrophage recruitment [18, 19]. Thirdly, inhibition of the SIRPα/CD47 axis promotes phagocytosis by dendritic cells and subsequent antigen presentation to CD8 + T-cells, hence inducing an adaptive antitumor immune response [20, 21]. Moreover, CD47 antagonists destroy tumor cells utilizing natural killer cell-mediated antibody-dependent cytotoxicity (ADCC) and complement-dependent cytotoxicity (CDC) [22, 23]. Lastly, CD47 antagonists can promote tumor cell death [24, 25], reduce tumor cell proliferation [26–28], and prevent tumor cell migration [29, 30].
Fig. 3.
Inhibiting CD47/SIRPα axis regulates the fate of cancer cells. Inhibiting the CD47/SIRPα axis can (A) directly enhance phagocytosis of macrophages to tumor cells; B transform tumor-associated macrophages into an antitumor state and increase the recruitment of macrophages in tumors; C promote phagocytosis by dendritic cells and antigen presentation to CD8 + T-cells; (D) destroy tumor cells by natural killer cell-mediated ADCC and CDC; E increase tumor cell death, inhibit tumor cell proliferation, and prevent tumor cell migration. Abbreviation: CD47, cluster of differentiation 47; SIRPα, signal-regulatory protein α; ACDD: antibody-dependent cellular cytotoxicity; CDC: complement-dependent cytotoxicity
Additionally, CD47 can be used as a prognostic marker in a variety of cancers. High CD47 expression has been demonstrated to correlate with a poor outcome in AML [16], chronic myelogenous leukemia [31], NHL [32] and some solid tumors (e.g., breast cancer, renal cell carcinoma, non-small cell lung cancer, thyroid cancer [33], etc.).
Aside from the implications mentioned above in tumor treatment and prognosis, CD47 has been implicated to aid the diagnosis of non-small cell lung cancer [34], renal cell tumors, and hematological tumors [33].
Clinical development of CD47/SIRPα antibodies
In the past decade, patent applications for CD47 antagonists have increased steadily, reaching a high in 2019. The top five licensing authorities (the United States, the World Intellectual Property Organization, the European Patent Office, Japan, and China) hold a large number of CD47 antagonist patents (> 67% of all patents), in which numerous of them have entered clinical trials. Currently, CD47 antagonists are primarily classified into five categories: (1) CD47 monoclonal antibody; (2) CD47-targeted bispecific antibody; (3) SIRPα/Fc fusion protein antibody, (4) CD47 small-molecule inhibitor, and (5) CD47 antibody–drug conjugate. Since no clinical trials on CD47 small-molecule inhibitors or antibody–drug conjugates for hematologic malignancies are publicly available, only the first three categories will be discussed.
Recent clinical investigations employing CD47 monoclonal antibodies have produced excellent results. Anemia and thrombocytopenia are the most common adverse events (AEs) associated with CD47 monoclonal antibodies [35]. This is due to the fact that erythrocytes and platelets express CD47; CD47 monoclonal antibodies can attack them either through direct binding or through activation of NK cells and macrophages via Fc-mediated ADCC or CDC [36].
To reduce toxicity and improve treatment efficacy, researchers have developed CD47-targeted bispecific antibodies and the SIRPα/Fc fusion protein antibodies. The synergistic effect of bispecific antibodies targeting CD47 and other tumor antigens can potentially increase the safety and efficacy of treatment by targeting tumor cells preferentially [37].
SIRPα/Fc fusion protein antibodies are able to destroy CD47/SIRPα binding to decrease the CD47 "don't eat me" signal and generate an activating prophagocytic signal via Fc receptors [3, 32, 38]. Since SIRPα is not expressed on human blood cells, SIRPα/Fc fusion protein antibodies display negligible binding to RBCs or blood platelets, distinguishing them from anti-CD47 monoclonal antibodies [39].
The CD47/SIRPα axis has been identified as a potential future immunotherapeutic target for hematological malignancies. Here, we provide a summary of CD47 antagonist clinical research frontiers in treating lymphomas and hematological malignancies. All clinical research and trial information was gathered from the PubMed database, Researchgate database, the US national clinical trials registry (NCT) system www.clinicaltrials.gov and the China drug trials registry (CTR) system www.chinadrugtrials.org.cn.
CD47 antagonist in lymphomas treatment
Currently, twenty-three CD47 antagonists are available in clinical trials for the treatment of lymphomas (Table 1). A list of CD47 antagonists with published clinical data is shown (Table 2).
Table 1.
CD47 antagonists currently entering clinical trials for treatment of lymphomas
| Drug Name |
Other Name | Companies | Target-based Actions | Drug Classification | Indications | US Highest Phase | Chinese Highest Phase | NCT | CTR |
|---|---|---|---|---|---|---|---|---|---|
| CC-90002 | INBRX-103 | Bristol-Myers Squibb Company | CD47 antagonist | anti-CD47 monoclonal antibody | Non-Hodgkin lymphoma | Phase I | / | NCT02641002 | / |
| GenSci-059 | GenSci-059 | GeneScience Pharmaceuticals Co Ltd | CD47 antagonist | anti-CD47 monoclonal antibody | Lymphoma | Phase I | / | NCT05221385 | / |
| IMC-002 | 3D-197 | ImmuneOncia Therapeutics LLC | CD47 antagonist | anti-CD47 monoclonal antibody | Lymphoma | Phase I | / | NCT04306224 | / |
| Lemzoparlimab | TJ011133; TJC4 | I-Mab Bio-Tech (Tianjin) Co., Ltd | CD47 antagonist | anti-CD47 monoclonal antibody | Lymphoma | Phase I | / | NCT03934814 | / |
| CD20 positive lymphoma | / | Phase I | / | CTR20210313 | |||||
| Letaplimab | IBI-188 | Innovent Biologics Inc | CD47 antagonist | anti-CD47 monoclonal antibody | Lymphoma | Phase I | Phase I | NCT03717103, NCT03763149, NCT04861948 | CTR20182140 |
| Ligufalimab | AK117 | Akeso Biopharma Inc | CD47 antagonist | anti-CD47 monoclonal antibody | Lymphoma | Phase I | Phase I | NCT04728334, NCT04349969 | CTR20202684 |
| Magrolimab | Hu5F9-G4 | Gilead Sciences | CD47 antagonist | anti-CD47 monoclonal antibody | Non-Hodgkin lymphoma | Phase II | / | / | |
| Classic Hodgkin lymphoma | Phase II | / | NCT04788043 | / | |||||
| T-Cell lymphoma | Phase II | / | NCT04541017 | / | |||||
| MIL-95 | CM-312 | KeyMed Biosciences Co Ltd | CD47 antagonist | anti-CD47 monoclonal antibody | Lymphoma | Phase I | Phase I | NCT04651348 | CTR20201108 |
| SHR-1603 | SHR-1603 | Jiangsu Hengrui Medicine Co Ltd | CD47 antagonist | anti-CD47 monoclonal antibody | Lymphoma | Phase I | Phase I | NCT03722186 | CTR20181964 |
| ZL-1201 | ZL-1201 | Zai Lab Limited | CD47 antagonist | anti-CD47 monoclonal antibody | Lymphoma | Phase I | Phase I | NCT04257617 | CTR20210973 |
| BAT-7104 | BAT-7101 | Bio-Thera Solutions Ltd | CD47 antagonist; Programmed cell death ligand 1 inhibitor | bispecific antibody | Lymphoma | Phase I | / | CTR20220098 | |
| HX-009 | HX-009–5 | HanX Biopharmaceuticals Inc | CD47 antagonist; Programmed cell death protein 1 inhibitor | bispecific antibody | Lymphoma | Phase II | Phase II | NCT05189093 | CTR20213391 |
| IBI-322 | IBI-322 | Innovent Biologics Inc | CD47 antagonist; Programmed cell death ligand 1 inhibitor | bispecific antibody | Lymphoma | Phase I | / | NCT04338659 | / |
| IMM-0306 | IMM-0306 | ImmuneOnco Biopharm Co Ltd | B-lymphocyte antigen CD20 modulator; CD47 antagonist; Immunoglobulin gamma Fc receptor agonist | bispecific antibody | CD20-positive B-cell non-Hodgkin's lymphoma | Phase I | / | NCT04746131 | CTR20192612 |
| JMT-601 | CPO-107 | Shanghai JMT-Bio Inc | B-lymphocyte antigen CD20 modulator; CD47 antagonist | bispecific antibody | CD20 positive B-cell non-Hodgkin's lymphoma | Phase II | Phase II | NCT04853329 | CTR20211365 |
| SG-12473 | SG-12473 | Hangzhou Sumgen Biotechnology Co Ltd | CD47 antagonist; Programmed cell death ligand 1 inhibitor | bispecific antibody | Lymphoma | / | Phase I | / | CTR20211029 |
| TG-1801 | NI-1701 | TG Therapeutics Inc | B-lymphocyte antigen CD19 modulator; CD47 antagonist; Immunoglobulin Fc receptor agonist | bispecific antibody | B-Cell Lymphoma | Phase I | / | NCT03804996, NCT04806035 | / |
| XL-114 | AU-341; AU7R-104; AUR-104 | Exelixis Inc | Bcl-10 protein modulator; CD47 antagonist; Caspase recruitment domain protein 11 modulator; Epidermal fatty acid binding protein inhibitor | bispecific antibody | Non-Hodgkin lymphoma | Phase I | / | NCT05144347 | / |
| Evorpacept | ALX-148 | ALX Oncology | SIRPα-Fc fusion protein,SIRPα/CD47 blocker | SIRPα/Fc fusion protein antibody | B-cell Non-Hodgkin Lymphoma | Phase II | / | NCT05025800, NCT03013218 | / |
| IMM-01 | IMM-01 | ImmuneOnco Biopharm Co Ltd | CD47 antagonist | SIRPα/Fc fusion protein antibody | Hodgkin's lymphoma, B-cell non-Hodgkin lymphoma; NK/T-cell lymphoma | / | Phase II | / | CTR20212227 |
| IMM-01 | IMM-01 | ImmuneOnco Biopharm Co Ltd | CD47 antagonist | SIRPα/Fc fusion protein antibody | Lymphoma | / | Phase II | / | CTR20191531 |
| TTI-621 | TTI-621 | Trillium Therapeutics Inc | CD47 antagonist; Immunoglobulin gamma Fc receptor agonist | SIRPα/Fc fusion protein antibody | Mycosis fungoides | Phase I | / | NCT02890368 | / |
| TTI-622 | TTI-622 | Trillium Therapeutics Inc | CD47 antagonist; Immunoglobulin gamma Fc receptor agonist | SIRPα/Fc fusion protein antibody | Lymphoma | Phase I | / | NCT03530683 | / |
| RRx-001 | RRx-001 | EpiCentrx Inc | CD47 antagonist; DNA methyltransferase inhibitor; Epigen modulator; Programmed cell death ligand 1 inhibitor; Tyrosine phosphatase substrate 1 inhibitor | small-molecule inhibitor | Lymphoma | Phase I | / | NCT01359982, NCT02096341, NCT02518958 | / |
Table 2.
Published results of clinical trials on the use of CD47 antagonists in lymphomas
| Drug Name | NCT Number | Sponsor | Protocol | Indication Detail | Enroll-ment | Age/Race/Healthy Volunteers | Phase | Status | Start Date | Design | Endpoint Types | Efficacy Results | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ALX148 | NCT03013218 | ALX Oncology | ALX148 | advanced malignancy and non-Hodgkin lymphoma | 25 (ALX148 monotherapy per week); 11 (ALX148 monotherapy at the highest dose of 30 mg/kg once every other week) | Adults (18 and over) | Phase I | No longer recruiting | 2017–01-06 | Interventional; Treatment; Non-Randomized; Open Label; Single Group Assignment | Safety; Efficacy; Pharmacokinetics; Pharmacodynamics | SD: 27% (ALX148 monotherapy per week), 18% (ALX148 monotherapy at the highest dose of 30 mg/kg once every other week) | [40] |
| ALX148 | NCT03013218 | ALX Oncology | ALX148; rituximab | Patients with relapsed or refractory CD20-positive B-cell NHL | 33 | Adults (18 and over) | Phase I | No longer recruiting | 2017–01-06 | Interventional; Treatment; Non-Randomized; Open Label; Single Group Assignment | Safety; Efficacy; Pharmacokinetics; Pharmacodynamics | ORR: 45% | [40] |
| TJ011133 | NCT03934814 | I-Mab Bio-Tech (Tianjin) Co., Ltd | lemzoparlimab; rituximab | R/R patients with CD20 positive Non-Hodgkin’s Lymphoma | 8 | Adults (18 and over) | Phase I | Recruiting | 2019–04-16 | Interventional; Treatment; Non-Randomized; Open Label; Single Group Assignment | Safety; Efficacy; Pharmacokinetics; Pharmacodynamics | ORR: 57% | [41] |
| IBI-188 | NCT03763149 | Innovent Biologics Inc | letaplimab | advanced/refractory solid tumors or lymphoma | 20 | Adults (18 and over) | Phase I | Completed | 2019–02-19 | Interventional; Treatment; Open Label; Single Group Assignment | Safety; Efficacy; Pharmacokinetics; Pharmacodynamics | / | [42] |
| Hu5F9-G4 | NCT02953509 | Forty Seven Inc; Gilead Sciences Inc | Hu5F9-G4; rituximab | Relapsed/Refractory B-cell Non-Hodgkin's Lymphoma | 22 | Adults (18 and over) | Phase I/II | No longer recruiting | 2016–11-21 | Interventional; Treatment; Non-Randomized; Open Label; Single Group Assignment | Safety; Efficacy; Pharmacokinetics; Pharmacodynamics | ORR: 50% | [43] |
| TTI-621 | NCT02663518 | Trillium Therapeutics Inc | TTI-621 | T-Cell Lymphoma | 64 | Adults (18 and over) | Phase I | No longer recruiting | 2016–01-01 | Interventional; Treatment; Non-Randomized; Open Label; Parallel Assignment | Safety; Efficacy; Pharmacokinetics; Pharmacodynamics | ORR (CTCL): 19%; ORR (PTCL): 18% | [44] |
| TTI-621 | NCT02663518 | Trillium Therapeutics Inc |
1. TTI-621; rituximab 2. TTI-621 |
DLBCL | 35 | Adults (18 and over) | Phase I | No longer recruiting | 2016–01-01 | Interventional; Treatment; Non-Randomized; Open Label; Parallel Assignment | Safety; Efficacy; Pharmacokinetics; Pharmacodynamics | ORR: 21% vs 29% (TTI-621 plus rituximab vs TTI-621 monotherapy) | [44] |
| TTI-621 | NCT02890368 | Trillium Therapeutics Inc | TTI-621 | Relapsed/Refractory Mycosis Fungoides and Sézary Syndrome | 35 | Adults (18 and over) | Phase I | Terminated | 2016–09-01 | Interventional; Treatment; Non-Randomized; Open Label; Parallel Assignment | Safety; Efficacy; Pharmacokinetics; Pharmacodynamics | ≥ 50% reduction in CAILS score: 34% | [45] |
| TTI-622 | NCT03530683 | Trillium Therapeutics Inc | TTI-622 | patients with advanced relapsed or refractory lymphoma | 42 | Adults (18 and over) | Phase I | Recruiting | 2018–05-01 | Interventional; Treatment; Non-Randomized; Open Label | Safety; Efficacy; Pharmacokinetics; Pharmacodynamics | ORR: 33% | [46, 47] |
CD47 monoclonal antibodies
CC-90002
CC-90002 is the first generation of humanized IgG4 anti-CD47 antibody entering clinical research. CC-90002 plus rituximab (an anti-CD20 monoclonal antibody) demonstrated tolerability and modest clinical activity in the heavily pretreated relapsed/refractory (R/R) NHL patients [48]. AEs were predominantly Grade 1/2, and the most frequent Grade 3/4 AEs were neutropenia (38%) and thrombocytopenia (21%). Twenty-four subjects were treated, one subject attained a stable complete response rate (CR), two subjects achieved partial response (PR), and three subjects achieved stable disease (SD). Although the fact that the current data suggest further investigation of CC-90002 in conjunction with rituximab for the treatment of NHL, no Phase II clinical studies have been conducted.
Hu5F9-G4
Hu5F9-G4 (5F9), also known as magrolimab, is a humanized monoclonal IgG4 antibody that was independently developed by Stanford University Forty Seven (Stanford, CA, USA) [49]. 5F9 not only inhibits CD47 signaling, which increases macrophage phagocytosis, but also stimulates ADCC [50]. Studies have demonstrated that 5F9 was more effective in combination with other antibodies than alone in the treatment of non-Hodgkin lymphoma [1, 43, 51, 52].
A phase Ib study (NCT02953509) assessed the safety and efficacy of 5F9 in combination with rituximab in 22 patients with R/R lymphoma (15 with DLBCL and 7 with FL) [43]. According to this study, CD47 receptors were present on more than 90% of peripheral blood cells. The overall response rate (ORR) and complete response rate (CR) were 50% and 36%, respectively. ORR and CR rates for DLBCL patients were 40% (6/15) and 33% (5/15), respectively. The ORR and CR for patients with a diagnosis of FL were 71% (5/7) and 43% (3/7), respectively. Anemia was the most prevalent AE, occurring in around 42% of patients, while all were manageable. To treat anemia, priming doses of 1 mg/kg 5F9 and maintenance doses of 30 mg/kg every week (QW) were administered. This study demonstrates that the combination of 5F9 and rituximab is effective in patients with R/R DLBCL or FL without a considerable risk of AEs.
In 2018, the Food and Drug Administration (FDA) approved 5F9 for the treatment of two types of R/R B-cell NHL (DLBCL and FL). Ongoing clinical trials involve the combination of 5F9 and rituximab (NCT03527147), the BTK inhibitor acalabrutinib (NCT03527147), mogamulizumab (NCT04541017), and pabolizumab (NCT04788043).
TJ011133 (TJC4, lemzoparlimab)
TJ011133 (TJC4, also known as lemzoparlimab) is a therapeutic anti-CD47 IgG4 antibody of the next generation investigated by I-Mab Biopharma (Beijing, China). TJ011133 has a unique binding epitope and an RBC/platelet sparing characteristic; therefore it does not produce substantial hematologic toxicity and does not require priming doses like 5F9 [49].
Eight R/R patients with CD20-positive NHL who had received at least two prior lines of therapy were included in a Phase Ib research (NCT03934814) [41]. TJ011133 was administered intravenously at doses of 20 or 30 mg/kg weekly with rituximab. All treatment-related AEs were grade 1 or 2 except for one patient who reported Grade 3 treatment-related AEs. CD47 receptor occupancy was 80% and 90% in those who received 20 mg/kg and 30 mg/kg of TJ011133, respectively. The assessable efficacy of seven individuals showed an ORR of 57% (three CR, one PR and the rest SD). The combo therapy demonstrated therapeutic effectiveness for individuals with R/R NHL. In addition, no priming dose was required for TJ011133 in this clinical research.
AK117 (Ligufalimab)
AK117 is a novel humanized IgG4 monoclonal antibody with a unique structure. Due to the unique conformation of AK117/CD47 complex, AK117 has no hemagglutination effect. A phase I clinical trial of AK117 revealed that it was well-tolerated up to 45 mg/kg per week in participants with no dose-limiting toxicity events and no hematological treatment-related AEs. As a result, AK117 does not need a lower 'priming' dose to prevent anemia. The CD47 receptor occupancy of AK117 on T cells in peripheral blood of participants reached and sustained at 100% at a dose of 3 mg/kg alone, with complete and lasting receptor occupancy in peripheral blood found at ≥ 10 mg/kg. AK117 has an excellent safety profile in clinical applications. A series of clinical trials of AK117 alone or in combination with multiple agents (e.g., rituximab) are ongoing for the treatment of a variety of hematologic malignancies [53].
CD47-targeted bispecific antibodies
CD47/CD20-targeted bispecific antibodies
IMM0306
Both in vivo and in vitro experiments confirmed that comparing with CD47 monoclonal antibodies, anti-CD47/CD20 bispecific antibodies showed better binding preference to tumor cells and more potent anti-lymphoma activity [54, 55]. Researchers suggest that anti-CD47/CD20 bispecific antibodies might be viable candidates for clinical trials, in which IMM0306 was the first of these to report preclinical results.
IMM0306 is a fusion protein of CD20 monoclonal antibody with CD47 binding domain of SIRPα. It exerts excellent cancer killing efficacy by activating both macrophages and NK cells via blockade of CD47-SIRPα interaction and FcɣR engagement by simultaneously binding to CD47 and CD20 of B cells. Extensive in vitro analysis revealed that IMM0306 had a strong affinity for a variety of hematologic malignant cells. Concerning the usage safety, IMM0306 has no binding activity on human RBCs. IMM0306 showed stronger ADCC activity and lower CDC activity in various hematologic malignancy cells when compared to rituximab, possibly due to the fact that the Fc segment of the recombinant protein in IMM0306 is IgG1. Application of IMM0306 in treating tumor-implanted SCID mice significantly inhibited tumor growth. Furthermore, in a lymphoma orthotopic model, IMM0306 paired with lenalidomide outperformed any single medicine or rituximab combination with lenalidomide in terms of therapeutic impact [17]. IMM0306 is being tested in two phase I clinical trials in patients with R/R CD20-positive B-cell NHL (NCT04746131 and CTR20192612).
CD47/CD19-targeted bispecific antibody
TG-1801 (NI-1701)
TG-1801 is an investigational first-in-class, bispecific anti-CD47/CD19 monoclonal antibody. TG-1801 has exhibited a potent capability to induce ADCP and ADCC in malignant B-cell lines and primary tumor B-cells from patients with ALL, CLL, and different subtypes of NHL in preclinical studies [56]. TG-1801 combined with rituximab was observed to have a stronger tumor-killing synergy than applying rituximab alone [36]. TG-1801 was also confirmed to be compatible with rituximab [57] and umbalixib (a phosphatidylinositol 3-kinase δ inhibitor) [57, 58] for the treatment of B-cell NHL and CLL.
TG-1801 is currently being evaluated in two phase I trials (NCT03804996 and NCT04806035) to evaluate its safety and efficacy in treating patients with B-cell lymphoma and CLL. No clinical data on TG-1801 have been reported so far.
SIRPα/Fc fusion protein antibodies
TTI-621 (SIRPα-IgG1 Fc)
TTI-621 is a fusion protein developed from the CD47 binding domain of human SIRPα linked to the Fc region of human IgG1. It is intended to improve phagocytosis and anti-cancer activity of macrophages by preventing CD47-SIRPα interaction between malignant cells and macrophages through Fc receptors engagement [45]. In preclinical studies, TTI-621 was shown to enhance macrophage phagocytosis of various malignant cells and decreased the growth of AML and B-cell lymphoma in xenografts. Besides, TTI-621 also displayed low binding affinity to human erythrocytes [3].
NCT02663518 is the First-in-human (FIH) phase I study in patients with R/R lymphoma [3]. This study aimed to evaluate the safety and efficacy of TTI-621 as a monotherapy or combination with rituximab or nivolumab. The MTD of the TTI-621 single-drug and the combined groups were 0.2 and 0.1 mg/kg, respectively. No death happened as a result of treatment-related adverse events, and only 37% of the patients experienced adverse events (AEs) of grade 3 or higher. Twenty percent of patients experienced thrombocytopenia, which was reversible and often cleared within one week. At the highest dose evaluated (0.5 mg/kg), the systemic exposure of TTI-621 showed dose-dependent without a plateau. The receptor occupancy rate was 34% and 66% at 0.2 and 0.5 mg/kg groups, respectively. Furthermore, single TTI-621 dosages up to 0.5 mg/kg did not increase the incidence of thrombocytopenia as compared to the 0.2 mg/kg group. The ORRs for TTI-621 monotherapy and TTI-621 plus rituximab for DLBCL were 29% (2/7) and 21% (5/24), respectively. The ORR for TTI-621 monotherapy in T-cell NHL was 25% (8/32). Updated results from clinical study NCT02663518 showed that TTI-621 demonstrated ORR in 14/71 (20%) NHL patients, including those with cutaneous T-cell lymphoma (n = 42, one CR, seven PR), peripheral T-cell lymphoma (n = 22, two CR, two PR), and DLBCL (n= 7, one CR, one PR) [44].
Another phase I clinical trial (NCT02890368) confirmed that topically administered TTI-621 was tolerated and had systemic and local antitumor activity in patients with R/R fungal disease and Sezary syndrome [45]. TTI621 was administered intralesionally to 35 individuals. The maximum assessed dosing regimen in this trial was 10 mg, and the MTD was not met. Although 25 (71%) individuals experienced treatment-related adverse events, they were all grade 1 or 2. During the trial, the Composite Assessment of Index Lesion Severity (CAILS) scores were reduced in 26 (90%) of the 29 patients, with CAILS score reductions of 50% or more in 10 (34%) of the patients. The median time to respond for the nine patients with a CAILS response on TTI-621 monotherapy was 45 days (95% CI 17–66). Even single injections reduced CAILs scores, and lesions adjacent to the injection site in eight patients showed decreases. Continuing monotherapy with TTI-621 induced further reductions in CAILS scores up to 100%. Nevertheless, the efficacy of TTI-621 in combination with pegylated interferon alpha-2a or a PD-1/PD-L1 inhibitor appearred poor in the trial.
In conclusion, TTI-621 is well-tolerated and can be used as monotherapy in patients with R/R NHL and combined with rituximab in patients with R/R B cell- NHL.
TTI-622 (SIRPα/IgG4 Fc)
Like TTI-621, TTI-622 is a soluble SIRPα/Fc variant protein containing an IgG4 Fc tail. TTI-622 resulted in a statistically significant tumor growth reduction and improved survival in both early and delayed treatment in DLBCL xenograft tumor model. TTI-622 monotherapy showed partial tumor growth inhibition in Burkitt lymphoma and in MM xenograft models. Additionally, the therapeutic effect was further enhanced when TTI-622 was combined with daratumumab (an anti-CD38 antibody). Importantly, TTI-622 does not bind to human RBCs [46, 47].
The data above supports the clinical evaluation of TTI-622 in combination with other antitumor antibodies in hematological malignancies patients. There is an ongoing multicenter, phase I dose-escalation and expansion trial of TTI-622 (NCT03530683). TTI-622 was given to 42 individuals with R/R lymphoma at weekly doses ranging from 0.05 to 18 mg/kg. Treatment-related AEs have occurred in 20 (47%) patients, and most AEs have been Grade 1 or 2 and reversible. Related AEs of Grade ≥ 3 intensity has occurred in 7 (16.7%) patients. No significant dose relationship was observed between the AEs. Preliminary pharmacokinetics data indicated a dose-dependent increase in exposure after single and repeated TTI-622 infusions. According to pharmacodynamics results, end-of-infusion CD47 receptor occupancy is greater than 60% at 2 mg/kg doses. Objective responses occurred in 33% (9/27) of response-evaluable patients at doses ranging from 0.8 to 18 mg/kg. Of the nine patients, two achieved CR (one in DLBCL and one in cutaneous T-cell lymphoma—mycosis fungoides), and seven achieved PR (two in cutaneous T-cell lymphoma, two in peripheral T-cell lymphoma, two in DLBCL, and one in FL) [46, 47].
Based on these preliminary results, TTI-622 is currently being evaluated in various combination regimens in ongoing studies.
ALX148
ALX148 (also known as evorpacept) is a new CD47-blocking molecule produced by connecting a modified SIRPα D1 domain to an inactive human IgG1 Fc. ALX148 exhibits a high affinity for CD47 in many species, inhibits wild-type SIRPα binding, and promotes tumor cell phagocytosis by macrophages. ALX148 had little effect on normal blood cells in experiments with rodents and NHPs. In addition, ALX148 enhanced anti-cancer activity of obinutuzumab and rituximab (both anti-CD20 antibodies) in carcinogenesis murine xenograft models employing human lymphoma (Z138 and Raji) cell lines [59].
Preliminary activity in combination with rituximab was observed in R/R CD20-positive B-cell NHL patients with no curative treatment. Thirty-three patients were enrolled in a phase I clinical trial (NCT03013218) aiming to evaluate the effects of different dosages of ALX148 in conjunction with rituximab. A total of eleven patients received ALX148 (15 mg/kg QW) in combination with rituximab and 63.6% of them achieved ORR (three CR and four PR). In the fully enrolled safety cohorts, no Dose-limiting toxicities (DLTs) have been reported, and the MTD of ALX148 combined with rituximab had yet to be reached. There have been no reports of dose-limiting toxicities (DLTs), and the MTD of ALX148 combined with rituximab had not yet been reached. No treatment-related fatality was documented, and 16/33 patients experienced low-grade AEs [40].
IMM01
IMM01 is a recombinant human SIRPα IgG1 fusion protein that has strong dual-functional anti-tumor activity through phagocytosis with improved potency upon N-glycosylation removal [10]. IMM01 exhibits promising preclinical characteristics regarding its link between receptor occupancy, tumor exposure and efficacy. Moreover, IMM01 shows a unique property of weak human erythrocyte conjugation to avoid severe hemolysis [60].
Preliminary results of an FIH phase I study (CTR1900024904) in patients with R/R lymphoma revealed that 14 patients with R/R lymphoma who had failed standard therapies received IMM01 monotherapy [60]. No DLTs were detected at a dose up to 1 mg/kg. Most treatment-related side effects were grade 1 or 2, but one patient had a grade 3 temporary platelet count decrease after two hours of drug implication, which returned to baseline 24 to 48 h after the initial infusion. The ORR was 14.3% (one CR and one PR), and two patients had verified SD. According to the research, IMM01 demonstrated an outstanding preclinical safety, tolerability, and prospective antitumor effectiveness at dose up to 1.0 mg/kg.
CD47 antagonist in the treatment of hematological tumors
There are currently 17 CD47 antagonists being tested for the treatment of hematological tumors in clinical trials (Table 3). CD47 antagonists with published clinical data are listed in Table 4.
Table 3.
CD47 antagonists currently entering clinical trials for treatment of hematological tumors
| Drug Name |
Other Name | Companies | Target-based Actions | Drug Classification | Indications | US Highest Phase | Chinese Highest Phase | NCT | CTR |
|---|---|---|---|---|---|---|---|---|---|
| AO-176 | AO-104 | Arch Oncology | CD47 antagonist | anti-CD47 monoclonal antibody | Multiple myeloma | Phase II | / | NCT04445701 | / |
| CC-90002 | INBRX-103 | Celgene Corp | CD47 antagonist | anti-CD47 monoclonal antibody | Acute myeloid leukaemia | Phase I | / | NCT02367196 | / |
| Myelodysplastic syndrome | Phase I | / | NCT02367196 | / | |||||
| GenSci-059 | GenSci-059 | GeneScience Pharmaceuticals Co Ltd | CD47 antagonist | anti-CD47 monoclonal antibody | Acute myeloid leukaemia | Phase I | / | NCT05263271 | / |
| Myelodysplastic syndrome | Phase I | NCT05263271 | / | ||||||
| Lemzoparlimab | TJ011133; TJC4 | I-Mab Bio-Tech (Tianjin) Co., Ltd | CD47 antagonist | anti-CD47 monoclonal antibody | Acute myeloid leukaemia | Phase II | Phase II | NCT04202003, NCT04912063 | CTR20210555, CTR20192522 |
| Myelodysplastic syndrome | Phase II | Phase III | NCT04202003, NCT04912063 |
CTR20210555, CTR20192522, CTR20230090 |
|||||
| Multiple Myeloma | Phase I | / | NCT04895410 | / | |||||
| Letaplimab | IBI-188 | Innovent Biologics Inc | CD47 antagonist | anti-CD47 monoclonal antibody | Acute myeloid leukaemia | Phase II | Phase II | NCT04485052 | CTR20200938 |
| Myelodysplastic syndrome | Phase I | Phase III | NCT04511975, NCT04485065 | CTR20201039 | |||||
| Ligufalimab | AK117 | Akeso Biopharma Inc | CD47 antagonist | anti-CD47 monoclonal antibody | Acute myeloid leukaemia | Phase II | Phase II | NCT04980885 | CTR20211305 |
| Myelodysplastic syndrome | Phase II | Phase II | NCT04900350 | CTR20210825 | |||||
| Magrolimab | Hu5F9-G4 | Gilead Sciences | CD47 antagonist | anti-CD47 monoclonal antibody | Myelodysplastic syndrome | Phase III | / | NCT04313881, NCT03527147 | / |
| Acute myeloid leukaemia | Phase III | / | NCT05263271, NCT04435691, NCT03248479, NCT03922477, NCT02678338 | / | |||||
| Myelodysplastic syndrome | Phase II | / | NCT05263271, NCT03248479, NCT02678338 | / | |||||
| ZL-1201 | ZL-1201 | Zai Lab Limited | CD47 antagonist | anti-CD47 monoclonal antibody | hematologic malignancies | Phase I | Phase I | NCT04257617 | CTR20210973 |
| IBI-322 | IBI-322 | Innovent Biologics Inc | CD47 antagonist; Programmed cell death ligand 1 inhibitor | bispecific antibody | Hematological neoplasm | Phase I | Phase I | NCT04795128 | CTR20210385 |
| Myeloid leukemia | Phase I | Phase I | NCT05148442 | CTR20213120 | |||||
| SIRPa-Fc-CD40L | SL-172154 | Shattuck Labs Inc | CD40 ligand receptor agonist; CD47 antagonist | bispecific antibody | Acute myeloid leukaemia | Phase I | NCT05275439 | / | |
| Myelodysplastic syndrome | Phase I | NCT05275439 | / | ||||||
| TG-1801 | NI-1701 | TG Therapeutics Inc | B-lymphocyte antigen CD19 modulator; CD47 antagonist; Immunoglobulin Fc receptor agonist | bispecific antibody | Chronic lymphocytic leukemia | Phase I | / | NCT04806035 | / |
| XL-114 | AU-341; AU7R-104; AUR-104 | Exelixis Inc | Bcl-10 protein modulator; CD47 antagonist; Caspase recruitment domain protein 11 modulator; Epidermal fatty acid binding protein inhibitor | bispecific antibody | Chronic lymphocytic leukemia | Phase I | / | NCT05144347 | / |
| DSP-107 | DSP-107 | KAHR Medical Ltd | CD47 antagonist; CDw137 agonist | SIRPα/Fc fusion protein antibody | Acute myeloid leukaemia | Phase I | / | NCT04937166 | / |
| Myelodysplastic syndrome | Phase I | NCT04937166 | / | ||||||
| Chronic myelomonocytic leukemia | Phase I | / | NCT04937166 | / | |||||
| Evorpacept | ALX-148 | ALX Oncology | SIRPα-Fc fusion protein,SIRPα/CD47 blocker | SIRPα/Fc fusion protein antibody | Acute myeloid leukaemia | Phase II | / | NCT04755244 | / |
| Myelodysplastic syndrome | Phase II | / | NCT04417517 | / | |||||
| IMM-01 | IMM-01 | ImmuneOnco Biopharm Co Ltd | CD47 antagonist | SIRPα/Fc fusion protein antibody | Acute myeloid leukaemia | Phase II | Phase II | NCT05140811 | CTR20212227, CTR20212519 |
| Myelodysplastic syndrome | Phase II | Phase II | NCT05140811 | CTR20212227, CTR20212519 | |||||
| Multiple myeloma | / | Phase II | / | CTR20212227 | |||||
| TTI-621 | TTI-621 | Trillium Therapeutics Inc | CD47 antagonist; Immunoglobulin gamma Fc receptor agonist | SIRPα/Fc fusion protein antibody | Multiple myeloma | Phase I | NCT05139225 | / | |
| Hematological neoplasm | Phase II | / | NCT02663518 | / | |||||
| TTI-622 | TTI-622 | Trillium Therapeutics Inc | CD47 antagonist; Immunoglobulin gamma Fc receptor agonist | SIRPα/Fc fusion protein antibody | Acute myelogenous leukemia | Phase I | / | NCT03530683 | / |
| Multiple myeloma | Phase I | / | NCT03530683, NCT05139225 | / | |||||
| Multiple myeloma | Phase I | / | NCT03530683 | / |
Table 4.
Published results of clinical trials on the use of CD47 antagonists in hematological tumors
| Drug Name | NCT Number | Sponsor | Protocol | Indication Detail | Enroll-ment | Age/Race/Healthy Volunteers | Phase | Status | Start Date | Design | Endpoint Types | Efficacy Results | Ref |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CC-90002 | NCT02641002 | Celgene Corp | CC-90002 | Subjects With AML and High-Risk MDS | 28 | Adults (18 and over) | Phase I | Terminted | 2016/3/1 | Interventional; Treatment; Open Label; Single Group Assignment | Safety; Efficacy; Pharmacokinetics | terminated (preliminary monotherapy data did not offer a sufficiently encouraging profile for further dose escalation/expansion) | [61] |
| TJ011133 | NCT04202003 | I-Mab Biopharma Co Ltd | TJ011133 | r/r AML/MDS | 5 | Adults (18–79 years) | Phase I | Recruiting | 2020/3/25 | Interventional; Treatment; Non-Randomized; Open Label; Single Group Assignment | Efficacy | 20% achieved morphologic leukemia-free state | [62] |
| Hu5F9-G4 | NCT03248479 | Gilead Sciences Inc | Hu5F9-G4; AZA | untreated AML/MDS | 68 | Adults (18 and over) | Phase I | Recruiting | 2017/9/8 | Interventional; Treatment; Non-Randomized; Open Label; Parallel Assignment | Safety; Efficacy; Pharmacokinetics | ORR: 79%; CR/CRi: 56% | [63] |
| Hu5F9-G4 | NCT04435691 | MD Anderson Cancer Center | Hu5F9-G4; AZA; VEN | Patients (pts) with Newly Diagnosed AML | 23 | Adults (18 and over) | Phase I/II | Recruiting | 2020/7/28 | Interventional; Treatment; Open Label; Single Group Assignment | Safety; Efficacy | CR/CRi: 100% | [64] |
| Hu5F9-G4 | NCT04435691 | MD Anderson Cancer Center | Hu5F9-G4; AZA; VEN | Patients (pts) with R/R-post-VEN failure AML | 13 | Adults (18 and over) | Phase I/II | Recruiting | 2020/7/28 | Interventional; Treatment; Open Label; Single Group Assignment | Safety; Efficacy | CR/CRi: 27% | [64] |
| Hu5F9-G4 | NCT04435691 | MD Anderson Cancer Center | Hu5F9-G4; AZA; VEN | Patients (pts) with R/R-VEN naive AML | 8 | Adults (18 and over) | Phase I/II | Recruiting | 2020/7/28 | Interventional; Treatment; Open Label; Single Group Assignment | Safety; Efficacy | CR/CRi: 63% | [64] |
CD47 monoclonal antibodies
CC-90002
Although the potential efficacy of CC-90002 in various hematologic malignancies has been demonstrated preclinically [65], a phase I study of patients with R/R AML and MDS (NCT02641002) was terminated due to lack of monotherapy activity and evidence of anti-drug antibodies [61]. In that study, no objective response was observed in any of the enrolled 28 patients (24 patients with AML and 4 with MDS). Of the 15 efficacy-evaluable patients with AML, 14 (93.3%) were classified as having treatment failure; of the 3 efficacy-evaluable patients with MDS, 1 (33.3%) was classified as having treatment failure; the remaining patients achieved the best overall response of SD. Hematologic improvements in MDS were not observed in any of the patient. The reason may be that replacing IgG1 with IgG4 significantly weakened the killing ability of CD47 monoclonal antibodies against tumor cells. At present, the research of CC-90002 in hematological malignancies is not continued.
Hu5F9-G4
Preclinical research has demonstrated powerful 5F9 anti-activity in various hematologic malignancies, particularly in AML and MDS [66]. In patients with AML/MDS, 5F9 binds to more than 99% of CD47 receptors in peripheral blood and about 90% in bone marrow [67]. In a clinical trial (NCT03248479), 53% (8/15) untreated AML/MDS patients had a CR or CR with incomplete count recovery (CRi) to 5F9 + azacitidine (AZA) (5/10 in AML and 3/5 in MDS) [63]. In another clinical research (NCT04778397), 56% (10/34) AML patients achieved CR/CRi to 5F9 + AZA [68]. This phase Ib trial also indicated that TP53 mutations were present in 65% of the 34 AML patients examined for efficacy, and that the CR/CRi rate was greater in patients bearing TP53 mutations [68]. Another study included 44 patients (23 newly diagnosed, 8 R/R prior to Venetoclax (VEN)-naïve, and 13 R/R-post-VEN failure). Although the onset of anaemia appears early, it can be alleviated. The CR/CRi rate in the remaining newly diagnosed patients was 100% (15/15), with a CR rate of 87% (13/15). Besides, 7/8 newly diagnosed patients with TP53-mutations were evaluated with a CR/CRi in 100% (7/7) and CR in 86% (6/7). In R/R prior VEN-naïve AML, the CR/CRi rate was 63% (5/8), with median overall survival (OS) not reached (range 1.2–9.7). In R/R prior VEN failure AML the CR/CRi rate was 27% (3/13) with med OS 3.1 (range 0.9–6.5) [64]. Anemia is still the most common AEs of 5F9 during the treatment of hematological tumors. AML patients have decreased hemoglobin and increased blood transfusion demand during 5F9 treatment [69].
In 2019, 5F9 was granted fast-track designation by the FDA for AML/MDS treatment and orphan drug designation by the FDA and European Medicines Agency for AML treatment. However, Gilead Sciences Inc. announced in 2022 that the FDA had placed a partial clinical hold on studies evaluating the combination of 5F9 plus AZA due to an apparent imbalance in investigator-reported suspected unexpected severe adverse reactions between study arms. It is gratifying that the FDA removed the partial clinical hold after reviewing the comprehensive safety data from each trial in 2022. Studies impacted by the action include NCT04313881 (Phase III, MDS), NCT04778397 (Phase III, AML), NCT05079230 (Phase III, MDS), NCT03248479 (Phase Ib, MDS), and NCT04778410 (Phase II, myeloid malignancies and only the AZA combination cohorts). Clinical studies on MDS/AML include NCT03922477 (plus Atezolizumab), NCT04435691 (plus AZA and VEN), NCT04892446(plus daratumumab, plus pomalidomide and dexamethasone, plus bortezomib and dexamethasone). Except for AZA, the combination of 5F9 and other drugs is also undergoing clinical trials. Clinical studies on MDS/AML include NCT03922477 (plus Atezolizumab), NCT04435691 (plus AZA and VEN), NCT04892446 (plus daratumumab, plus pomalidomide and dexamethasone, plus bortezomib and dexamethasone).
IBI-188 (Letaplimab)
Studies evaluating the safety and efficacy of IBI-188 in combination with AZA for the treatment of newly diagnosed middle- and high-risk MDS and AML are currently underway in both China and the United States. Notably, IBI-188 in conjunction with AZA for the treatment of hematologic disorders in China is undergoing Phase III clinical trials. Other Phase I trials include Letaplimab in combination with rituximab in advanced lymphoma (NCT03717103), with AZA in AML (NCT04485052), and with AZA in newly diagnosed higher-risk MDS (NCT04485065).
TJ011133 (TJC4, Lemzoparlimab)
TJ011133 is now being tested in patients with R/R AML or MDS in a phase I trial (NCT04202003). Four out of five patients had treatment-related AEs. Only one AE was of Grade 3, while the rest were of Grades 1–2. No DLTs or MTDs were detected up to a weekly dose of 10 mg/kg. The average receptor occupancy on peripheral T cells was 74%, 82%, and 84%, respectively, for 1, 3, and 10 mg/kg. One main refractory AML patient attained morphologic leukemia-free status following two cycles of 1 mg/kg TJ011133 therapy [62]. TJ011133 in combination with AZA has been approved for a phase III clinical trial in the treatment of primary higher risk MDS.
Challenges and future perspectives of CD47/SIRPα immune checkpoint for tumors
Challenges
CD47 antagonists have shown some promise results in preclinical and clinical studies for treating hematologic tumors and lymphomas. For the foreseeable future, CD47/SIRPα will one day become an equally promising immunotherapy as PD-1/PD-L1. In order to reach the full potential of CD47/SIRPα immune checkpoint-based immunotherapy, further studies are necessary. Currently, Hu5F9-G4, ALX-148 and TJ011133 are undergoing Phase III clinical studies, and it is anticipated that these medications will be the first to file marketing applications for new drugs.
However, the development of CD47 monoclonal antibodies still faces three major challenges: therapeutic effectiveness, safety concerns, and lack of published data. CD47 is widely expressed in normal cells, this implies that substantial dosages or frequent administration may be necessary to achieve effective therapeutic CD47 blockage. Preclinical studies have shown that 40–60% CD47 receptor occupancy is required for the induction of phagocytosis [51]. However, extra caution is required given that large doses or frequent administration may result in treatment-related adverse effects. Besides, when tumor cells express both SIRPα and TSP-1 which inhibit the CD47-SIRPα interaction [70], the effective dose of CD47 antagonist may need to be modified. Additionally, sufficient macrophage activation requires triggering of Fc receptors, hence proper human IgG should be chosen [17]. Even though human IgG1 works better to stimulate macrophages, it also causes immune cells to attack RBCs. Therefore, most companies have chosen to develop human IgG4-type antibodies, which significantly lower the antitumor activity [71]. Moreover, CD47-targeted bispecific antibodies only act on particular tumor types, therefore malignancies must be identified and classified to determine the most effective treatment. So far, most clinical trials on CD47 antagonists are in phase I and II, implying that optimal dosage of dual antibodies requires further investigation.
Hematotoxicity, particularly anemia, is the most frequent adverse effect of CD47 inhibitors. Even if there is evidence of promising antitumor efficacy, CD47 antagonists are associated with anemia since RBCs express a substantial amount of CD47. Additionally, activating certain epitopes on the Ig variable structural region of CD47 has been reported to induce fast T cell apoptosis and depletion [72]. Application of CD47 antagonists may also cause other safety issues, for example, unexpected immunological problems may occur as most immune cells express CD47; inhibiting SIRPα may produce nervous system malfunction, such as aberrant synaptic pruning in microglia neurodegeneration, since SIRPα is highly expressed in central and peripheral nervous system cells [13, 73]. Finally, due to the sequence similarities of SIRP family, CD47 may cross-react with other SIRPs, resulting in unintended side effects. CD47 has been found to bind to SIRPγ and positively regulate human T cell activation and proliferation [5]. Use of CD47 inhibitors may result in T-cell function suppression, which deserves further investigation in the future.
Last but not least, there is a lack of published data on the affinity of CD47 antagonists for checkpoint binding, either with pure CD47 and SIRPα protein or on appropriate human cells, hindering more insightful analysis on this topic.
Future perspectives
In order to increase the efficacy and safety of CD47 antagonists, the following strategies of antagonist development may emerge in the future (Fig. 4): (1) Using the strategy of CD47 antagonist prime and maintenance dosing (e.g., 5F9 and IBI-188); (2) Modifying the drug structure of CD47 monoclonal antibody (e.g., AO-176, TJ011133, SRF231, and AK117); (3) Fusion protein of CD47/SIRPa combining with different antibodies, such as CD20, CD19, could be of a promising strategy in the immunotherapy targeting CD47/SIRPa axis (e.g., IMM0306, NI-1701) [17, 74]; (4) Development of SIRPα/Fc fusion protein antibodies; (5) Development of small-molecule inhibitors (e.g., RRX-001, QPCTL antibodies); (6) Introduction of new drug delivery methods (e.g., CD47 nanobody [55], plasmid vector [75], and CD47/SIRPα blocking peptide [76]); (7) Since binding of CD47 to SIRPγ enables T cell activation and proliferation [5], blockade of SIRPα-CD47 interaction while preserving SIRPγ binding to CD47 may be a strategy for cancer immunotherapy (e.g., SIRP-1 and SIRP-2) [77]; (8) SIRPα engages with CD47 in either cis or trans behavior in different scenarios. SIRPα expressed in macrophages exhibits trans binding to CD47 that are expressed in other types of ‘self’ cells, leading to local SIRPα accumulation and inhibition of ‘self’cell engulfment including the tumor cells [35, 78]. On the other hand, CD47 expressed on macrophages has the potential to modulate phagocytosis through a cis interaction with SIRPα that is also expressed on macrophages. Blockade of the cis CD47-SIRPα interaction could result in hyper phagocytosis [79]. Therefore, extra consideration needs to be taken in the development of CD47 antagonists as they may lead to different clinical outcomes; (9) Improvement of the tumor selectivity of CD47 antagonists may also be a future strategy (e.g., a PH-dependent CD47 antibody) [80].
Fig. 4.
Future strategies for developing CD47 antagonists. Abbreviation: CD47, cluster of differentiation 47; SIRP, signal-regulatory protein
In conclusion, given that CD47 antagonists enable cancer cells to escape macrophage-mediated phagocytosis, inhibiting the CD47/SIRPα axis is a potential cancer treatment strategy. A deeper understanding of the mechanisms and processes by which tumor cells avoid immune clearance and improving CD47 antagonist administration routes would contribute to developing effective and safe antitumor medicines. The latest clinical research advances and detailed information were presented in tables to aid the readers for quick search of the contents of interest.
Acknowledgements
We thank the members of You’s lab for helpful discussions.
Abbreviations
- ADCC
Antibody-dependent cell-mediated cytotoxicity
- AE
Adverse event
- ALL
Acute lymphoblastic leukemia
- AML
Acute myeloid leukemia
- AZA
Azacitidine
- CAILS
Composite assessment of index lesion severity
- CD
Cluster of differentiation
- CDC
Complement-dependent cytotoxicity
- CLL
Chronic lymphocytic leukemia
- CR
Complete response rate
- CRi
CR with incomplete blood count recovery
- CTR
The China drug trials registry
- DLBCL
Diffuse large B cell lymphoma
- DLT
Dose-limiting toxicity
- FDA
Food and Drug Administration
- FIH
First-in-human
- FL
Follicular lymphoma
- ITIM
Immunoreceptor tyrosine-based inhibitor motif
- MDS
Myelodysplastic syndrome
- MM
Multiple myeloma
- MTD
Maximum tolerated dose
- NCT
The US national clinical trials registry
- NHL
Non-Hodgkin lymphoma
- NHP
Non-human primate
- ORR
Overall response rate
- OS
Overall survival
- PD-1
Programmed cell death receptor-1
- PD-L1
Programmed cell death ligand-1
- PR
Partial response
- QPCTL
Glutaminyl-peptide cyclotransferase-like
- QW
Every week
- R/R
Relapsed/refractory
- RBC
Red blood cells
- SD
Stable disease
- SHP
Src homology phosphatase
- SIRP
Signal regulatory protein
- SIRPα
Signal regulatory protein alpha
- TSP-1
Thrombospondin-1
- VEN
Venetoclax
Authors’ contributions
HY1 and YX contributed equally to the work. HY2 conceived the hypothesis, and revised the manuscript. HY1 and YX did the literature search and wrote the manuscript. HY1 and HY2 prepared the tables and figures. The authors read and approved the final manuscript.
Funding
This study was supported by the National Natural Science Foundation of China (82203844, 82203213, 81911530169), Basic and Applied Basic Research Project of Guangdong Province (2020A1515111201), and University Special Innovative Research Program of the Department of Education of Guangdong Province (2020KQNCX073).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Ethical Approval is not applicable. This paper has not been published elsewhere in whole or in part. All authors have read and approved the content, and agree to submit it for consideration for publication.
Consent for publication
Consent for publication is not applicable in this research.
Competing interests
The authors declare no competing interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Hua Yang and Yang Xun contributed equally to this work.
References
- 1.Eladl E, Tremblay-LeMay R, Rastgoo N, Musani R, Chen W, Liu A, Chang H. Role of CD47 in Hematological Malignancies. J Hematol Oncol. 2020;13(1):96. doi: 10.1186/s13045-020-00930-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chao MP, Tang C, Pachynski RK, Chin R, Majeti R, Weissman IL. Extranodal dissemination of non-Hodgkin lymphoma requires CD47 and is inhibited by anti-CD47 antibody therapy. Blood. 2011;118(18):4890–4901. doi: 10.1182/blood-2011-02-338020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ansell SM, Maris MB, Lesokhin AM, Chen RW, Flinn IW, Sawas A, Minden MD, Villa D, Percival M-EM, Advani AS et al. Phase I Study of the CD47 Blocker TTI-621 in Patients with Relapsed or Refractory Hematologic Malignancies. Clin Cancer Res. 2021;27(8):2190–9. [DOI] [PubMed]
- 4.Pang WW, Pluvinage JV, Price EA, Sridhar K, Arber DA, Greenberg PL, Schrier SL, Park CY, Weissman IL. Hematopoietic stem cell and progenitor cell mechanisms in myelodysplastic syndromes. Proc Natl Acad Sci U S A. 2013;110(8):3011–3016. doi: 10.1073/pnas.1222861110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piccio L, Vermi W, Boles KS, Fuchs A, Strader CA, Facchetti F, Cella M, Colonna M. Adhesion of human T cells to antigen-presenting cells through SIRPbeta2-CD47 interaction costimulates T-cell proliferation. Blood. 2005;105(6):2421–2427. doi: 10.1182/blood-2004-07-2823. [DOI] [PubMed] [Google Scholar]
- 6.Kharitonenkov A, Chen Z, Sures I, Wang H, Schilling J, Ullrich A. A family of proteins that inhibit signalling through tyrosine kinase receptors. Nature. 1997;386(6621):181–186. doi: 10.1038/386181a0. [DOI] [PubMed] [Google Scholar]
- 7.Adams S, van der Laan LJ, Vernon-Wilson E. Renardel de Lavalette C, Döpp EA, Dijkstra CD, Simmons DL, van den Berg TK: Signal-regulatory protein is selectively expressed by myeloid and neuronal cells. J Immunol. 1998;161(4):1853–1859. [PubMed] [Google Scholar]
- 8.Veillette A, Thibaudeau E, Latour S. High expression of inhibitory receptor SHPS-1 and its association with protein-tyrosine phosphatase SHP-1 in macrophages. J Biol Chem. 1998;273(35):22719–22728. doi: 10.1074/jbc.273.35.22719. [DOI] [PubMed] [Google Scholar]
- 9.Seiffert M, Cant C, Chen Z, Rappold I, Brugger W, Kanz L, Brown EJ, Ullrich A, Bühring HJ. Human signal-regulatory protein is expressed on normal, but not on subsets of leukemic myeloid cells and mediates cellular adhesion involving its counterreceptor CD47. Blood. 1999;94(11):3633–3643. [PubMed] [Google Scholar]
- 10.Yu J, Li S, Chen D, Liu D, Guo H, Yang C, Zhang W, Zhang L, Zhao G, Tu X et al. Crystal Structure of Human CD47 in Complex with Engineered SIRPα.D1(N80A). Molecules. 2022;27(17):5574. [DOI] [PMC free article] [PubMed]
- 11.Li W, Wang F, Guo R, Bian Z, Song Y. Targeting macrophages in hematological malignancies: recent advances and future directions. J Hematol Oncol. 2022;15(1):110. doi: 10.1186/s13045-022-01328-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kale A, Rogers NM, Ghimire K. Thrombospondin-1 CD47 Signalling: From Mechanisms to Medicine. Int J Mol Sci. 2021;22(8):4062. [DOI] [PMC free article] [PubMed]
- 13.Rogers NM, Sharifi-Sanjani M, Csányi G, Pagano PJ, Isenberg JS. Thrombospondin-1 and CD47 regulation of cardiac, pulmonary and vascular responses in health and disease. Matrix Biol. 2014;37:92–101. doi: 10.1016/j.matbio.2014.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Orazizadeh M, Lee HS, Groenendijk B, Sadler SJ, Wright MO, Lindberg FP, Salter DM. CD47 associates with alpha 5 integrin and regulates responses of human articular chondrocytes to mechanical stimulation in an in vitro model. Arthritis Res Ther. 2008;10(1):R4. doi: 10.1186/ar2350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Q, Onuma K, Liu C, Wong H, Bloom MS, Elliott EE, Cao RR, Hu N, Lingampalli N, Sharpe O et al. Dysregulated integrin αVβ3 and CD47 signaling promotes joint inflammation, cartilage breakdown, and progression of osteoarthritis. JCI Insight. 2019;4(18):e128616. [DOI] [PMC free article] [PubMed]
- 16.Majeti R, Chao MP, Alizadeh AA, Pang WW, Jaiswal S, Gibbs KD, Jr, van Rooijen N, Weissman IL. CD47 is an adverse prognostic factor and therapeutic antibody target on human acute myeloid leukemia stem cells. Cell. 2009;138(2):286–299. doi: 10.1016/j.cell.2009.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yu J, Li S, Chen D, Liu D, Guo H, Yang C, Zhang W, Zhang L, Zhao G, Tu X et al. IMM0306, a fusion protein of CD20 mAb with the CD47 binding domain of SIRPα, exerts excellent cancer killing efficacy by activating both macrophages and NK cells via blockade of CD47-SIRPα interaction and FcɣR engagement by simultaneously binding to CD47 and CD20 of B cells. Leukemia. 2022. Epub ahead of print. [DOI] [PMC free article] [PubMed]
- 18.Weiskopf K, Jahchan NS, Schnorr PJ, Cristea S, Ring AM, Maute RL, Volkmer AK, Volkmer JP, Liu J, Lim JS, et al. CD47-blocking immunotherapies stimulate macrophage-mediated destruction of small-cell lung cancer. J Clin Investig. 2016;126(7):2610–2620. doi: 10.1172/JCI81603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang M, Hutter G, Kahn SA, Azad TD, Gholamin S, Xu CY, Liu J, Achrol AS, Richard C, Sommerkamp P, et al. Anti-CD47 Treatment Stimulates Phagocytosis of Glioblastoma by M1 and M2 Polarized Macrophages and Promotes M1 Polarized Macrophages In Vivo. PLoS ONE. 2016;11(4):e0153550. doi: 10.1371/journal.pone.0153550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tseng D, Volkmer JP, Willingham SB, Contreras-Trujillo H, Fathman JW, Fernhoff NB, Seita J, Inlay MA, Weiskopf K, Miyanishi M, et al. Anti-CD47 antibody-mediated phagocytosis of cancer by macrophages primes an effective antitumor T-cell response. Proc Natl Acad Sci USA. 2013;110(27):11103–11108. doi: 10.1073/pnas.1305569110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Soto-Pantoja DR, Terabe M, Ghosh A, Ridnour LA, DeGraff WG, Wink DA, Berzofsky JA, Roberts DD. CD47 in the tumor microenvironment limits cooperation between antitumor T-cell immunity and radiotherapy. Can Res. 2014;74(23):6771–6783. doi: 10.1158/0008-5472.CAN-14-0037-T. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhao XW, van Beek EM, Schornagel K, Van der Maaden H, Van Houdt M, Otten MA, Finetti P, Van Egmond M, Matozaki T, Kraal G, et al. CD47-signal regulatory protein-α (SIRPα) interactions form a barrier for antibody-mediated tumor cell destruction. Proc Natl Acad Sci USA. 2011;108(45):18342–18347. doi: 10.1073/pnas.1106550108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saumet A, Slimane MB, Lanotte M, Lawler J, Dubernard V. Type 3 repeat/C-terminal domain of thrombospondin-1 triggers caspase-independent cell death through CD47/alphavbeta3 in promyelocytic leukemia NB4 cells. Blood. 2005;106(2):658–667. doi: 10.1182/blood-2004-09-3585. [DOI] [PubMed] [Google Scholar]
- 24.Song G, Yang L. Inhibited CD47 gene affects the clearance of acute myelogenous leukemia stem cells. J Cell Biochem. 2019;120(6):10303–10309. doi: 10.1002/jcb.28314. [DOI] [PubMed] [Google Scholar]
- 25.Kikuchi Y, Uno S, Kinoshita Y, Yoshimura Y, Iida S, Wakahara Y, Tsuchiya M, Yamada-Okabe H, Fukushima N. Apoptosis inducing bivalent single-chain antibody fragments against CD47 showed antitumor potency for multiple myeloma. Leuk Res. 2005;29(4):445–450. doi: 10.1016/j.leukres.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 26.Boukhari A, Alhosin M, Bronner C, Sagini K, Truchot C, Sick E, Schini-Kerth VB, André P, Mély Y, Mousli M, et al. CD47 activation-induced UHRF1 over-expression is associated with silencing of tumor suppressor gene p16INK4A in glioblastoma cells. Anticancer Res. 2015;35(1):149–157. [PubMed] [Google Scholar]
- 27.Zhang JF, Hua R, Liu DJ, Liu W, Huo YM, Sun YW. Effect of CD74 on the prognosis of patients with resectable pancreatic cancer. Hepatobiliary Pancreat Dis Int. 2014;13(1):81–86. doi: 10.1016/s1499-3872(14)60011-4. [DOI] [PubMed] [Google Scholar]
- 28.Piccione EC, Juarez S, Tseng S, Liu J, Stafford M, Narayanan C, Wang L, Weiskopf K, Majeti R. SIRPα-Antibody Fusion Proteins Selectively Bind and Eliminate Dual Antigen-Expressing Tumor Cells. Clin Cancer Res. 2016;22(20):5109–5119. doi: 10.1158/1078-0432.CCR-15-2503. [DOI] [PubMed] [Google Scholar]
- 29.Xu JF, Pan XH, Zhang SJ, Zhao C, Qiu BS, Gu HF, Hong JF, Cao L, Chen Y, Xia B, et al. CD47 blockade inhibits tumor progression human osteosarcoma in xenograft models. Oncotarget. 2015;6(27):23662–23670. doi: 10.18632/oncotarget.4282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu J, Li Z, Yang Z, Guo L, Zhang Y, Deng H, Wang C, Feng M. A Glutamine-Rich Carrier Efficiently Delivers Anti-CD47 siRNA Driven by a "Glutamine Trap" To Inhibit Lung Cancer Cell Growth. Mol Pharm. 2018;15(8):3032–3045. doi: 10.1021/acs.molpharmaceut.8b00076. [DOI] [PubMed] [Google Scholar]
- 31.Russ A, Hua AB, Montfort WR, Rahman B, Riaz IB, Khalid MU, Carew JS, Nawrocki ST, Persky D, Anwer F. Blocking "don't eat me" signal of CD47-SIRPα in hematological malignancies, an in-depth review. Blood Rev. 2018;32(6):480–489. doi: 10.1016/j.blre.2018.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang W, Huang Q, Xiao W, Zhao Y, Pi J, Xu H, Zhao H, Xu J, Evans CE, Jin H. Advances in Anti-Tumor Treatments Targeting the CD47/SIRPα Axis. Front Immunol. 2020;11:18. [DOI] [PMC free article] [PubMed]
- 33.Lu Q, Chen X, Wang S, Lu Y, Yang C, Jiang G. Potential New Cancer Immunotherapy: Anti-CD47-SIRPα Antibodies. Onco Targets Ther. 2020;13:9323–9331. doi: 10.2147/OTT.S249822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Catalán R, Orozco-Morales M, Hernández-Pedro NY, Guijosa A, Colín-González AL, Ávila-Moreno F, Arrieta O. CD47-SIRPα Axis as a Biomarker and Therapeutic Target in Cancer: Current Perspectives and Future Challenges in Nonsmall Cell Lung Cancer. J Immunol Res. 2020;2020:9435030. doi: 10.1155/2020/9435030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oldenborg PA, Zheleznyak A, Fang YF, Lagenaur CF, Gresham HD, Lindberg FP. Role of CD47 as a marker of self on red blood cells. Science. 2000;288(5473):2051–2054. doi: 10.1126/science.288.5473.2051. [DOI] [PubMed] [Google Scholar]
- 36.Buatois V, Johnson Z, Salgado-Pires S, Papaioannou A, Hatterer E, Chauchet X, Richard F, Barba L, Daubeuf B, Cons L, et al. Preclinical Development of a Bispecific Antibody that Safely and Effectively Targets CD19 and CD47 for the Treatment of B-Cell Lymphoma and Leukemia. Mol Cancer Ther. 2018;17(8):1739–1751. doi: 10.1158/1535-7163.MCT-17-1095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang Y, Yang Z, Yang Y. Potential Role of CD47-Directed Bispecific Antibodies in Cancer Immunotherapy. Front Immunol. 2021;12:686031. doi: 10.3389/fimmu.2021.686031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Theocharides AP, Jin L, Cheng PY, Prasolava TK, Malko AV, Ho JM, Poeppl AG, van Rooijen N, Minden MD, Danska JS, et al. Disruption of SIRPα signaling in macrophages eliminates human acute myeloid leukemia stem cells in xenografts. J Exp Med. 2012;209(10):1883–1899. doi: 10.1084/jem.20120502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Petrova PS, Viller NN, Wong M, Pang X, Lin GH, Dodge K, Chai V, Chen H, Lee V, House V, et al. TTI-621 (SIRPαFc): A CD47-Blocking Innate Immune Checkpoint Inhibitor with Broad Antitumor Activity and Minimal Erythrocyte Binding. Clin Cancer Res. 2017;23(4):1068–1079. doi: 10.1158/1078-0432.CCR-16-1700. [DOI] [PubMed] [Google Scholar]
- 40.Kim T, Lakhani N, Gainor J, Kamdar M, Fanning P, Squifflet P, Jin F, Forgie A, Wan H, Pons J, et al. ALX148, a CD47 Blocker, in combination with rituximab in patients with non-hodgkin lymphoma. Blood. 2020;136:13–14. [Google Scholar]
- 41.Mehta A, Harb W, Xu C, Meng Y, Lee L, Yuan V, Wang Z, Song P, Shen J, Gopal A. Lemzoparlimab, a Differentiated Anti-CD47 Antibody in Combination with Rituximab in Relapsed and Refractory Non-Hodgkin's Lymphoma: Initial Clinical Results. Blood. 2021;138:3542–3542. [Google Scholar]
- 42.Lakhani N, Orloff M, Fu S, Liu Y, Wang Y, Zhou H, Lin K, Liu F, Yan S, Patnaik A. 295 First-in-human Phase I trial of IBI188, an anti-CD47 targeting monoclonal antibody, in patients with advanced solid tumors and lymphomas. J Immunother Cancer. 2020;8:A322–A322. [Google Scholar]
- 43.Advani R, Flinn I, Popplewell L, Forero A, Bartlett NL, Ghosh N, Kline J, Roschewski M, LaCasce A, Collins GP, et al. CD47 Blockade by Hu5F9-G4 and Rituximab in Non-Hodgkin's Lymphoma. N Engl J Med. 2018;379(18):1711–1721. doi: 10.1056/NEJMoa1807315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Horwitz S, Foran J, Maris M, Lue J, Sawas A, Okada C, Feldman T, Mei M, Flinn I, Villa D, et al. Updates from Ongoing, First-in-Human Phase 1 Dose Escalation and Expansion Study of TTI-621, a Novel Biologic Targeting CD47, in Patients with Relapsed or Refractory Hematologic Malignancies. Blood. 2021;138:2448–2448. [Google Scholar]
- 45.Querfeld C, Thompson JA, Taylor MH, DeSimone JA, Zain JM, Shustov AR, Johns C, McCann S, Lin GHY, Petrova PS, et al. Intralesional TTI-621, a novel biologic targeting the innate immune checkpoint CD47, in patients with relapsed or refractory mycosis fungoides or Sézary syndrome: a multicentre, phase 1 study. Lancet Haematology. 2021;8(11):e808–e817. doi: 10.1016/S2352-3026(21)00271-4. [DOI] [PubMed] [Google Scholar]
- 46.Patel K, Ramchandren R, Maris M, Lesokhin A, Keudell G, Cheson B, Zonder J, Seymour E, Catalano T, Lin G, et al. Investigational CD47-Blocker TTI-622 shows single-agent activity in patients with advanced relapsed or refractory lymphoma: update from the ongoing first-in-human dose escalation study. Blood. 2020;136:46–47. [Google Scholar]
- 47.Patel K, Zonder J, Sano D, Maris M, Lesokhin A, Keudell G, Lai C, Ramchandren R, Catalano T, Lin G, et al. CD47-Blocker TTI-622 shows single-agent activity in patients with advanced relapsed or refractory lymphoma: update from the ongoing first-in-human dose escalation study. Blood. 2021;138:3560–3560. [Google Scholar]
- 48.Abrisqueta P, Sancho J-M, Cordoba R, Persky D, Andreadis C, Huntington S, Carpìo C, Giles D, Wei X, Li Y, et al. Anti-CD47 Antibody, CC-90002, in Combination with Rituximab in Subjects with Relapsed and/or Refractory Non-Hodgkin Lymphoma (R/R NHL) Blood. 2019;134:4089–4089. [Google Scholar]
- 49.Meng Z, Wang Z, Guo B, Cao W, Shen H. TJC4, a Differentiated Anti-CD47 Antibody with Novel Epitope and RBC Sparing Properties. Blood. 2019;134:4063–4063. [Google Scholar]
- 50.Gholamin S, Mitra S, Feroze A, Liu J, Kahn S, Zhang M, Esparza R, Richard C, Ramaswamy V, Remke M, et al. Disrupting the CD47-SIRPα anti-phagocytic axis by a humanized anti-CD47 antibody is an efficacious treatment for malignant pediatric brain tumors. Scie Transl Med. 2017;9:eaaf2968. doi: 10.1126/scitranslmed.aaf2968. [DOI] [PubMed] [Google Scholar]
- 51.Liu J, Wang L, Zhao F, Tseng S, Narayanan C, Shura L, Willingham S, Howard M, Prohaska S, Volkmer J, et al. Pre-Clinical Development of a Humanized Anti-CD47 Antibody with Anti-Cancer Therapeutic Potential. PLoS ONE. 2015;10(9):e0137345. doi: 10.1371/journal.pone.0137345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chao MP, Alizadeh AA, Tang C, Myklebust JH, Varghese B, Gill S, Jan M, Cha AC, Chan CK, Tan BT, et al. Anti-CD47 antibody synergizes with rituximab to promote phagocytosis and eradicate non-Hodgkin lymphoma. Cell. 2010;142(5):699–713. doi: 10.1016/j.cell.2010.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Qu T, Zhong T, Pang X, Huang Z, Jin C, Wang ZM, Li B, Xia Y. Ligufalimab, a novel anti-CD47 antibody with no hemagglutination demonstrates both monotherapy and combo antitumor activity. J Immunother Cancer. 2022;10(11):e005517. [DOI] [PMC free article] [PubMed]
- 54.Piccione EC, Juarez S, Liu J, Tseng S, Ryan CE, Narayanan C, Wang L, Weiskopf K, Majeti R. A bispecific antibody targeting CD47 and CD20 selectively binds and eliminates dual antigen expressing lymphoma cells. mAbs. 2015;7(5):946–956. doi: 10.1080/19420862.2015.1062192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ma L, Zhu M, Gai J, Li G, Chang Q, Qiao P, Cao L, Chen W, Zhang S, Wan Y. Preclinical development of a novel CD47 nanobody with less toxicity and enhanced anti-cancer therapeutic potential. J Nanobiotechnol. 2020;18(1):12. doi: 10.1186/s12951-020-0571-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dheilly E, Moine V, Broyer L, Salgado-Pires S, Johnson Z, Papaioannou A, Cons L, Calloud S, Majocchi S, Nelson R, et al. Selective Blockade of the Ubiquitous Checkpoint Receptor CD47 Is Enabled by Dual-Targeting Bispecific Antibodies. Mol Ther. 2017;25(2):523–533. doi: 10.1016/j.ymthe.2016.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lunning M, Vose J, Nastoupil L, Fowler N, Burger JA, Wierda WG, Schreeder MT, Siddiqi T, Flowers CR, Cohen JB, et al. Ublituximab and umbralisib in relapsed/refractory B-cell non-Hodgkin lymphoma and chronic lymphocytic leukemia. Blood. 2019;134(21):1811–1820. doi: 10.1182/blood.2019002118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Normant E, Ribeiro ML, Reyes D, Miskin HP, Sportelli P, Weiss MS, Bosch F, Roue G: The Novel Bispecific CD47-CD19 antibody TG-1801 potentiates The Activity Of Ublituximab-Umbralisib (U2) DRUG combination in preclinical models of B-NHL. 2019, 37(S2):322–323.
- 59.Kauder SE, Kuo TC, Harrabi O, Chen A, Sangalang E, Doyle L, Rocha SS, Bollini S, Han B, Sim J, et al. ALX148 blocks CD47 and enhances innate and adaptive antitumor immunity with a favorable safety profile. PLoS ONE. 2018;13(8):e0201832. doi: 10.1371/journal.pone.0201832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sun M, Qi J, Zheng W, Song L, Jiang B, Wang Z, Huang C, Tian W, Qiu L. Preliminary results of a first-in-human phase I dtudy of IMM01, SIRPα Fc protein in patients with relapsed or refractory lymphoma. J Clin Oncol. 2021;39:2550–2550. [Google Scholar]
- 61.Zeidan AM, DeAngelo DJ, Palmer J, Seet CS, Tallman MS, Wei X, Raymon H, Sriraman P, Kopytek S, Bewersdorf JP, et al. Phase 1 study of anti-CD47 monoclonal antibody CC-90002 in patients with relapsed/refractory acute myeloid leukemia and high-risk myelodysplastic syndromes. Ann Hematol. 2022;101(3):557–569. doi: 10.1007/s00277-021-04734-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Qi J, Li J, Jiang B, Jiang B, Liu H, Cao X, Zhang M, Meng Y, Ma X, Jia Y, et al. A Phase I/IIa study of lemzoparlimab, a monoclonal antibody targeting cd47, in patients with relapsed and/or refractory acute myeloid leukemia (AML) and myelodysplastic syndrome (mds): initial phase i results. Blood. 2020;136:30–31. [Google Scholar]
- 63.Sallman D, Donnellan W, Asch A, Lee D, Malki M, Marcucci G, Pollyea D, Kambhampati S, Komrokji R, Elk J, et al. The first-in-class anti-CD47 antibody Hu5F9-G4 is active and well tolerated alone or with azacitidine in AML and MDS patients: Initial phase 1b results. J Clin Oncol. 2019;37:7009–7009. [Google Scholar]
- 64.Daver N, Konopleva M, Maiti A, Kadia T, Dinardo C, Loghavi S, Pemmaraju N, Jabbour E, Montalbán Bravo G, Tang G, et al. Phase i/ii study of azacitidine (aza) with venetoclax (ven) and magrolimab (magro) in patients (pts) with newly diagnosed older/unfit or high-risk acute myeloid leukemia (aml) and relapsed/refractory (R/R) AML. Blood. 2021;138:371–371. [Google Scholar]
- 65.Narla RK, Modi H, Bauer D, Abbasian M, Leisten J, Piccotti JR, Kopytek S, Eckelman BP, Deveraux Q, Timmer J et al. Modulation of CD47-SIRPα innate immune checkpoint axis with Fc-function detuned anti-CD47 therapeutic antibody. Cancer Immunol Immunother. 2022;71(2):473–89. [DOI] [PMC free article] [PubMed]
- 66.Chao MP, Takimoto CH, Feng DD, McKenna K, Gip P, Liu J, Volkmer JP, Weissman IL, Majeti R. Therapeutic targeting of the macrophage immune checkpoint cd47 in myeloid malignancies. Front Oncol. 2019;9:1380. doi: 10.3389/fonc.2019.01380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Agoram B, Jin C, Maute R, Takimoto C, Chao M, Sallman D. Pharmacokinetic (PK)-pharamcodynamic (PD) analysis and receptor occupancy data to support every other week maintenance dosing of magrolimab in combination with azacitidine in MDS/AML patients. J Clin Oncol. 2020;38:e15098–e15098. [Google Scholar]
- 68.Sallman D, Asch A, Kambhampati S, Malki M, Zeidner J, Donnellan W, Lee D, Vyas P, Jeyakumar D, Mannis G, et al. AML-196: the first-in-class anti-cd47 antibody magrolimab in combination with azacitidine is well tolerated and effective in aml patients: phase 1b results. Clin Lymphoma Myeloma Leuk. 2021;21:S290. [Google Scholar]
- 69.Brierley CK, Staves J, Roberts C, Johnson H, Vyas P, Goodnough LT, Murphy MF. The effects of monoclonal anti-CD47 on RBCs, compatibility testing, and transfusion requirements in refractory acute myeloid leukemia. Transfusion. 2019;59(7):2248–2254. doi: 10.1111/trf.15397. [DOI] [PubMed] [Google Scholar]
- 70.Isenberg JS, Annis DS, Pendrak ML, Ptaszynska M, Frazier WA, Mosher DF, Roberts DD. Differential interactions of thrombospondin-1, -2, and -4 with CD47 and effects on cGMP signaling and ischemic injury responses. J Biol Chem. 2009;284(2):1116–1125. doi: 10.1074/jbc.M804860200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pietsch EC, Dong J, Cardoso R, Zhang X, Chin D, Hawkins R, Dinh T, Zhou M, Strake B, Feng PH, et al. Anti-leukemic activity and tolerability of anti-human CD47 monoclonal antibodies. Blood Cancer J. 2017;7(2):e536. doi: 10.1038/bcj.2017.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Pettersen RD, Hestdal K, Olafsen MK, Lie SO, Lindberg FP. CD47 signals T cell death. J of immunol(Baltimore, Md : 1950) 1999;162(12):7031–7040. [PubMed] [Google Scholar]
- 73.Ding X, Wang J, Huang M, Chen Z, Liu J, Zhang Q, Zhang C, Xiang Y, Zen K, Li L. Loss of microglial SIRPα promotes synaptic pruning in preclinical models of neurodegeneration. Nat Commun. 2021;12(1):2030. doi: 10.1038/s41467-021-22301-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ni H, Cao L, Wu Z, Wang L, Zhou S, Guo X, Gao Y, Jing H, Wu M, Liu Y, et al. Combined strategies for effective cancer immunotherapy with a novel anti-CD47 monoclonal antibody. Cancer Immunol Immunother. 2022;71(2):353–363. doi: 10.1007/s00262-021-02989-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Billerhart M, Schönhofer M, Schueffl H, Polzer W, Pichler J, Decker S, Taschauer A, Maier J, Anton M, Eckmann S, et al. CD47-targeted cancer immunogene therapy: Secreted SIRPα-Fc fusion protein eradicates tumors by macrophage and NK cell activation. Molecular therapy oncolytics. 2021;23:192–204. doi: 10.1016/j.omto.2021.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Wang H, Sun Y, Zhou X, Chen C, Jiao L, Li W, Gou S, Li Y, Du J, Chen G et al. CD47/SIRPα blocking peptide identification and synergistic effect with irradiation for cancer immunotherapy. J Immunother Cancer. 2020;8(2):e000905. [DOI] [PMC free article] [PubMed]
- 77.Andrejeva G, Capoccia BJ, Hiebsch RR, Donio MJ, Darwech IM, Puro RJ, Pereira DS. Novel SIRPα Antibodies That Induce Single-Agent Phagocytosis of Tumor Cells while Preserving T Cells. J Immunol. 2021;206(4):712–721. doi: 10.4049/jimmunol.2001019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Weiskopf K, Ring AM, Ho CC, Volkmer JP, Levin AM, Volkmer AK, Ozkan E, Fernhoff NB, van de Rijn M, Weissman IL, et al. Engineered SIRPα variants as immunotherapeutic adjuvants to anticancer antibodies. Science. 2013;341(6141):88–91. doi: 10.1126/science.1238856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Hayes BH, Tsai RK, Dooling LJ, Kadu S, Lee JY, Pantano D, Rodriguez PL, Subramanian S, Shin JW, Discher DE. Macrophages show higher levels of engulfment after disruption of cis interactions between CD47 and the checkpoint receptor SIRPα. J Cell Sci. 2020;133(5):jcs237800. [DOI] [PMC free article] [PubMed]
- 80.Li Y, Liu J, Chen W, Wang W, Yang F, Liu X, Sheng Y, Du K, He M, Lyu X, et al. A pH-dependent anti-CD47 antibody that selectively targets solid tumors and improves therapeutic efficacy and safety. J Hematol Oncol. 2023;16(1):2. doi: 10.1186/s13045-023-01399-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.