Abstract
Objectives:
To assess trends in timing of mortality among patients with septic shock.
Design:
Retrospective cohort study.
Setting:
Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project’s National Inpatient Sample, 1994–2014.
Patients:
Hospitalized adults (≥ 18 yr) with International Classification of Diseases, 9th Edition, Clinical Modification codes consistent with septic shock; secondary analysis: adults with International Classification of Diseases, 9th Edition, Clinical Modification codes consistent with acute respiratory failure receiving invasive mechanical ventilation and patients with both septic shock and acute respiratory failure receiving invasive mechanical ventilation.
Interventions:
None.
Measurements and Main Results:
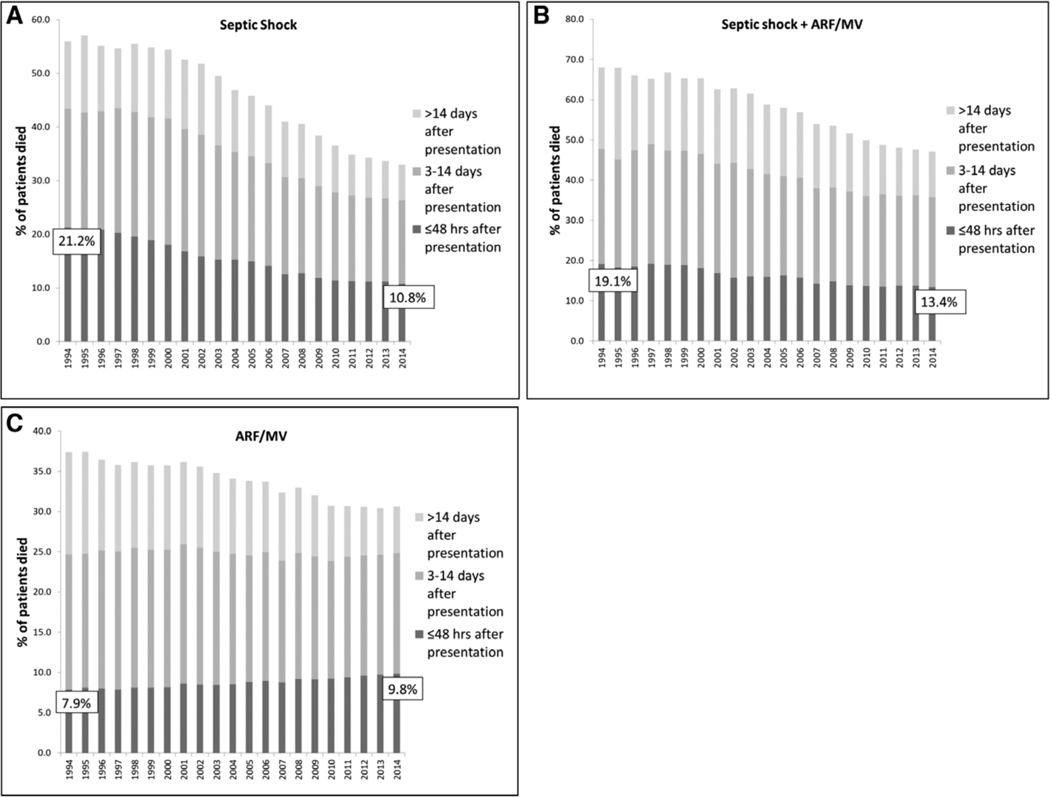
From 1994 to 2014, 48-hour mortality rates decreased among patients with septic shock (21.2% to 10.8%) and septic shock with acute respiratory failure receiving invasive mechanical ventilation (19.1% to 13.4%) but increased among patients with acute respiratory failure receiving invasive mechanical ventilation (7.9% to 9.8%; p value for all trends, < 0.001). Three-to-14-day mortality decreased among patients with septic shock (22.1% to 15.5%), septic shock with acute respiratory failure receiving invasive mechanical ventilation (28.7% to 22.4%) and acute respiratory failure receiving invasive mechanical ventilation (16.8% to 15.0%; p value for all trends, < 0.001). Mortality after 14 days decreased among all groups (septic shock: 12.6% to 6.7%; septic shock with acute respiratory failure receiving invasive mechanical ventilation: 20.3% to 11.3%; and acute respiratory failure receiving invasive mechanical ventilation: 12.7% to 5.8%; p value for all trends, < 0.001). Cox proportional hazard ratio for declining risk in mortality per year (adjusted for patient and hospital characteristics) was 0.96 (95% CI, 0.96–0.96) for septic shock, 0.97 (0.97–0.97) for acute respiratory failure receiving invasive mechanical ventilation and septic shock, and 0.99 (0.99–0.99) for acute respiratory failure receiving invasive mechanical ventilation.
Conclusions:
Septic shock 48-hour, 3–14-day and greater than 14-day mortality declined markedly over two decades; in contrast, patients with acute respiratory failure only experienced marked decreases in greater than 14-day in-hospital mortality rates.
Keywords: acute respiratory failure, mechanical ventilation, mortality, sepsis, septic shock
Analyses of trends in septic shock outcomes have focused on reductions in 28–30-day or in-hospital mortality, largely attributed to improvements in time-sensitive sepsis recognition and treatment (1, 2). However, emerging evidence suggests that risk factors associated with “early” versus “late” death during septic shock differ, with early deaths primarily attributable to multiple organ failure due to infection, and late deaths more strongly associated with comorbidity, ICU-acquired complications, or end-of-life decisions (3, 4). Evaluating trends in the “timing” of sepsis mortality may inform how improvement efforts affected different stages of critical illness due septic shock, and direct future efforts. Because premorbid conditions, ICU-acquired complications, and end-of-life decisions are generally not targets of septic shock resuscitation improvement initiatives, we hypothesized that the largest reductions in septic shock mortality over time would be seen in early deaths, as compared with changes in critical illness mortality independent of sepsis initiatives, where we expected reductions in mortality at later time points.
MATERIALS AND METHODS
We used the Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project’s National Inpatient Sample, 1994–2014, a longitudinal, random, 20% stratified sample of all nonfederal U.S. acute care hospitalizations (5, 6). Using survey-weighted methods, we identified hospitalized adults (≥ 18 yr) with primary or secondary International Classification of Diseases, 9th Edition, Clinical Modification (ICD-9-CM) diagnosis codes consistent with septic shock (i.e., the presence of both severe sepsis and shock) (7, 8) (supplement, Supplemental Digital Content 1, http://links.lww.com/CCM/E858) and evaluated trends in annual population-standardized incidence and 48-hour mortality, 3–14-day mortality, and greater than 14-day mortality (from day of admission). Among patients with septic shock, the association between year of admission and time to death within 30 days was also analyzed using Cox proportional hazards regression, adjusting for factors with potential to confound associations of interest, including patient characteristics (age, sex, race, primary insurance payer, median zip code income, Elixhauser comorbidities [9], type of critical illness [8], and type of acute organ failure [7]) and hospital characteristics (bed size, location/teaching status, U.S. region). To understand how trends in mortality during critical illness changed over time separate from changes to sepsis care, we conducted secondary analyses in patients with acute respiratory failure receiving invasive mechanical ventilation (ARF/MV) without septic shock, as well as in patients with both ARF/MV and septic shock. To better characterize patients who might have had septic shock and ARF/MV at admission, we conducted sensitivity analyses in cohorts with sepsis or ARF codes as primary diagnoses only. Statistical testing was two-tailed, performed with α equals to 0.05 with SAS 9.4 (SAS Institute. Cary, NC). The Beth Israel Deaconess Medical Center Institutional Review Board deemed the study exempt from review.
RESULTS
From 1994 to 2014, population-standardized incidence increased for septic shock (11.6 to 142.8 per 100,000), ARF/MV (102.6 to 232.0 per 100,000), and septic shock with ARF/MV (3.2 to 59.0 per 100,000; p value for all trends, < 0.001). Forty-eight–hour mortality rates decreased among patients with septic shock (21.2% to 10.8%) (Fig. 1) and septic shock with ARF/MV (19.1% to 13.4%) but increased among patients with ARF/MV (7.9% to 9.8%; p value for all trends, < 0.001). Three-to-14–day mortality decreased among patients with septic shock (22.1% to 15.5%), septic shock with ARF/MV (28.7% to 22.4%) and ARF/MV (16.8% to 15.0%; p value for all trends, < 0.001). Mortality after 14 days decreased among all groups (septic shock: 12.6% to 6.7%; septic shock with ARF/MV: 20.3% to 11.3%; and ARF/MV: 12.7% to 5.8%; p value for all trends, < 0.001). Cox proportional hazard ratio for declining risk in mortality per year (adjusted for patient and hospital characteristics) was 0.96 (95% CI, 0.96–0.96) for septic shock, 0.97 (0.97–0.97) for ARF/MV and septic shock, and 0.99 (0.99–0.99) for ARF/MV. Sensitivity analyses restricted to sepsis or ARF as primary diagnoses showed similar results as primary analyses, with decreasing 48-hour septic shock mortality (27.2% to 12.9%) and increasing 48-hour ARF/MV mortality (4.9% to 6.0%); 3–14-day and greater than 14-day mortality decreased in both groups.
Figure 1.
Rates in 48-hr mortality, 3–14-d mortality, and greater than 14-d mortality have all declined over time in patients with septic shock (A), and to a lesser degree, in patients with both septic shock and acute respiratory failure receiving invasive mechanical ventilation (ARF/MV) (B). By contrast, only 3–14-d mortality, and greater than 14-d mortality have decreased in patients with ARF/MV, while 48-hr mortality has increased (C). Forty-eight–hr mortality rates in 1994 and 2014 are shown for each cohort.
DISCUSSION
Over two decades of observation, septic shock case-fatality declined markedly across 48-hour, 3–14-day and greater than 14-day mortality, whereas patients with ARF only experienced marked decreases in greater than 14-day in-hospital mortality rates.
Although other analyses have reported on trends in 28–30-day or in-hospital mortality (1, 2), few other studies have investigated epidemiological trends in the timing of death during critical illness in the United States. Our study extends the findings of Kaukonen et al (2), who found uniform decreases in mortality in a cohort with severe sepsis in Australia and New Zealand across all hospital lengths of stay. Because prior studies suggested that early deaths after septic shock were attributable to multiple organ failure related to infection, it is plausible that improvements in 48-hour and 3–14-day mortality were consequences of pre-hospital or intra-hospital sepsis-specific initiatives implemented in the past two decades, many of which focused on earlier recognition of sepsis or initiation of therapy (4, 10). However, mortality later in the hospital stay following septic shock is less likely modified by sepsis-specific initiatives, and reasons for improved greater than 14-day mortality may be more complex. We hypothesize that reductions in later in-hospital mortality in both the septic shock and ARF/MV groups may be due to general ICU quality improvement initiatives (e.g., Awakening and Breathing Coordination, Delirium Monitoring and Management, and Early Mobility bundles [11], ventilator-associated pneumonia-prevention bundles [12]), which may only begin to show effects after weeks, rather than days; this may help explain why only greater than 14-day mortality improved markedly in the ARF/MV group. Additionally, earlier hospital transfer to long-term acute care hospitals and/or increased discharge to hospice over time (13, 14) may shift deaths out of hospital without meaningfully changing overall mortality. Our results should be considered hypothesis-generating and warrant confirmatory studies to explore the mechanisms by which sepsis-specific and/or general ICU quality initiatives impacted mortality timing, or whether certain subgroups of patients with septic shock have been differentially affected over time.
Our study has limitations. First, we relied on the use of ICD-9-CM coding to identify patients with septic shock and patients with ARF/MV. However, the codes we used to identify severe sepsis and MV have been validated previously and shown to have strong positive predictive values (7, 15). Although prior studies have noted that coding sensitivity for sepsis as a principal diagnosis increased with time (14), use of secondary and primary diagnosis (as in our primary analysis) with MV procedure codes (as in our septic shock with ARF/MV group) has been shown to mitigate effects of changes in coding sensitivity on mortality trends (7, 16). Additionally, analyses of granular medical records have also shown that although coding for sepsis increased over time, there was no difference in clinical characteristics of patients receiving sepsis codes (illness severity, as evidenced by vasopressor use and lactate levels, as well as confirmatory evidence of sepsis, were stable over time) (17). Thus, the observed rise in background incidence is presumed to be due to increased—but accurate—coding and decreasing thresholds of illness severity used for septic shock ICD-9-CM codes are unlikely to explain our findings. However, as trends in illness severity for ARF/MV remains poorly characterized (18), it is possible that the lack of improvement in the ARF/MV cohort is due to increasing illness severity. Second, we could not identify time of onset of septic shock or ARF/MV precisely. However, a sensitivity analysis including patients with sepsis or ARF codes as primary diagnoses likely to be present at admission showed similar results. Finally, we did not perform analyses adjusting for changes in source of sepsis over time, which could account for changes in mortality timing; this possibility could be pursued in further studies.
In conclusion, although sepsis initiatives have placed particular emphasis on the early and aggressive management of an initial infection, sepsis mortality rates have improved across both early and later follow-up times. Similar improvements in early mortality were not observed for critically ill patients with ARF/MV. Further work is needed to determine the roles that changes in coding and discharge patterns, sepsis-specific initiatives, and/or general quality improvement initiatives may have played in observed mortality reductions.
Supplementary Material
Acknowledgments
Dr. Law received funding from National Institutes of Health (NIH)/National Institute on Aging (1F32AG058352). Dr. Stevens received funding from Agency for Healthcare Research and Quality (5K08HS024288) and Doris Duke Charitable Foundation. Dr. Walkey received funding from NIH/National Heart, Lung, and Blood Institute (1R01HL136660 and 1R01HL139751) and Boston University School of Medicine Department of Medicine Career Investment Award.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
REFERENCES
- 1.Stevenson EK, Rubenstein AR, Radin GT, et al. : Two decades of mortality trends among patients with severe sepsis: A comparative meta-analysis*. Crit Care Med 2014; 42:625–631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaukonen KM, Bailey M, Suzuki S, et al. : Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000–2012. JAMA 2014; 311:1308–1316 [DOI] [PubMed] [Google Scholar]
- 3.Iwashyna TJ, Hodgson CL, Pilcher D, et al. : Timing of onset and burden of persistent critical illness in Australia and New Zealand: A retrospective, population-based, observational study. Lancet Respir Med 2016; 4:566–573 [DOI] [PubMed] [Google Scholar]
- 4.Daviaud F, Grimaldi D, Dechartres A, et al. : Timing and causes of death in septic shock. Ann Intensive Care 2015; 5:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Geriatrics Society Ethics Committee, Clinical Practice, Models of Care Committee: American Geriatrics Society feeding tubes in advanced dementia position statement. J Am Geriatr Soc 2014; 62:1590–1593 [DOI] [PubMed] [Google Scholar]
- 6.Healthcare Cost and Utilization Project (HCUP): HCUP Nationwide Inpatient Sample (NIS). 2012–2014. Rockville, MD, Agency for Healthcare Research and Quality. 2018. Available at: http://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed July 1, 2019 [Google Scholar]
- 7.Martin GS, Mannino DM, Eaton S, et al. : The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med 2003; 348:1546–1554 [DOI] [PubMed] [Google Scholar]
- 8.Ehlenbach WJ, Hough CL, Crane PK, et al. : Association between acute care and critical illness hospitalization and cognitive function in older adults. JAMA 2010; 303:763–770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Healthcare Cost and Utilization Project (HCUP): HCUP Comorbidity Software. Rockville, MD, Agency for Healthcare Research and Quality, 2008. Available at: www.hcup-us.ahrq.gov/toolssoftware/comorbidity/comorbidity.jsp. Accessed January 15, 2018 [Google Scholar]
- 10.Levy MM, Evans LE, Rhodes A: The surviving sepsis campaign bundle: 2018 update. Crit Care Med 2018; 46:997–1000 [DOI] [PubMed] [Google Scholar]
- 11.Boehm LM, Vasilevskis EE, Dietrich MS, et al. : Organizational domains and variation in attitudes of intensive care providers toward the ABCDE bundle. Am J Crit Care 2017; 26:e18–e28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klompas M: What is new in the prevention of nosocomial pneumonia in the ICU? Curr Opin Crit Care 2017; 23:378–384 [DOI] [PubMed] [Google Scholar]
- 13.Mehta AB, Syeda SN, Bajpayee L, et al. : Trends in tracheostomy for mechanically ventilated patients in the United States, 1993–2012. Am J Respir Crit Care Med 2015; 192:446–454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rhee C, Dantes R, Epstein L, et al. ; CDC Prevention Epicenter Program: Incidence and trends of sepsis in US hospitals using clinical vs claims data, 2009–2014. JAMA 2017; 318:1241–1249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kerlin MP, Weissman GE, Wonneberger KA, et al. : Validation of administrative definitions of invasive mechanical ventilation across 30 intensive care units. Am J Respir Crit Care Med 2016; 194:1548–1552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Walkey AJ, Lagu T, Lindenauer PK: Trends in sepsis and infection sources in the United States. A population-based study. Ann Am Thorac Soc 2015; 12:216–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Law A, Klompas M; CDC Prevention Epicenters: Are clinical characteristics of patients with sepsis codes changing over time? Infect Control Hosp Epidemiol 2015; 36:1364–1366 [DOI] [PubMed] [Google Scholar]
- 18.Pham T, Rubenfeld GD: Fifty years of research in ARDS. The epidemiology of acute respiratory distress syndrome. A 50th birthday review. Am J Respir Crit Care Med 2017; 195:860–870 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.