Purpose of review
Indirect calorimetry is increasingly recommended to guide energy delivery in the ICU. This review aims to provide a critical overview of current literature in support of these recommendations.
Recent findings
There is insufficient evidence to ascertain a mortality benefit from indirect calorimetry-guided energy delivery. However, large variations in energy expenditure during critical illness pose a risk for significant under- and overfeeding if indirect calorimetry is not routinely used.
Summary
Even in the absence of demonstrable clinical benefits, there is a strong physiological rationale in favor of performing indirect calorimetry. Measurements can be prioritized in complex patients and should be repeated during prolonged ICU stay.
Keywords: critical illness, energy expenditure, indirect calorimetry, metabolism
INTRODUCTION
Indirect calorimetry (IC) is recommended in major critical care societal guidelines largely because of the poor agreement between estimated and measured resting energy expenditure (mREE) [1,2▪]. The technique has been in use for over 40 years as a method to assess mREE and substrate oxidation in hospitalized patients [3]. However, routine application of indirect calorimetry remains far from ubiquitous in the modern ICU, and there is still debate over the clinical utility of indirect calorimetry [4].
The main purpose of this review is to address the question whether indirect calorimetry should be the standard for determining energy expenditure in the ICU, or preferentially used in a subset of complex patients. We also aim to summarize recent publications on energy metabolism during critical illness and highlight novel applications of indirect calorimetry in this setting.
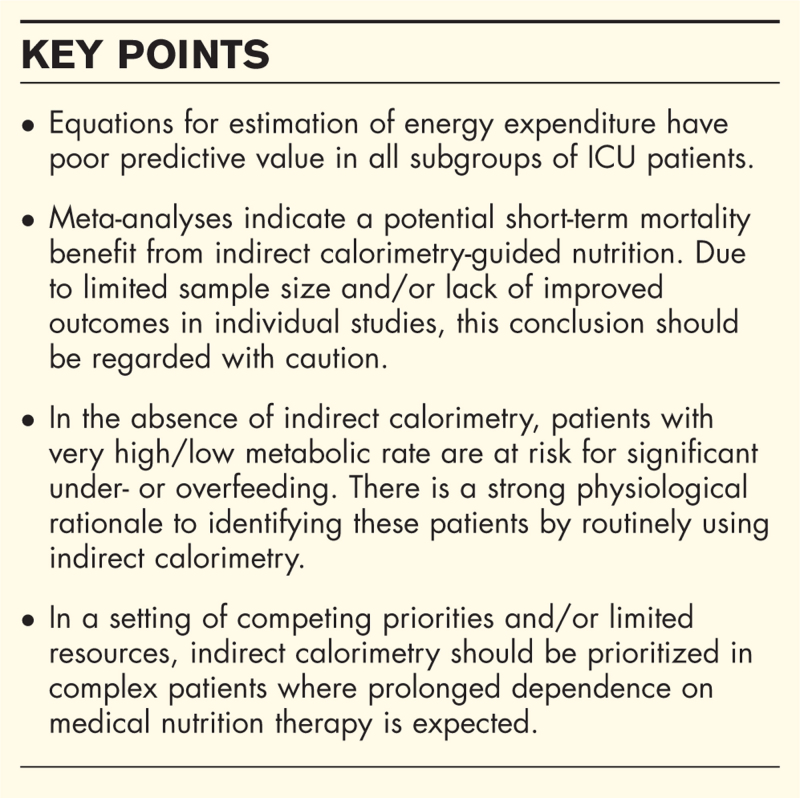
Box 1.
no caption available
AVAILABILITY AND BARRIERS TO USE
Despite being recommended for guiding energy delivery, indirect calorimetry is not available in all ICUs. In an international audit of nutrition practices in mechanically ventilated critically ill patients between 2007 and 2009, 37 of 7872 patients (0.5%) had energy targets determined using indirect calorimetry [5]. In a more recent survey of critical care dietitians in Australia and New Zealand, 13 of 63 respondents (21%) reported having access to indirect calorimetry in their ICU [6]. Although availability of indirect calorimetry is likely to have increased over the past decade, contemporary data is lacking [4].
Also, the use of indirect calorimetry is not possible in all patients. For VO2 and VCO2 to accurately reflect substrate oxidation, it is essential that clinicians are aware of the inherent limitations of indirect calorimetry [2▪]. Technical exclusions to measurement during mechanical ventilation include but are not limited to leaks in the ventilator circuit, high extrinsic PEEP and/or FiO2 support. Measurements may also be limited in spontaneously breathing patients who require noninvasive ventilation or supplemental oxygen, patients with delirium and those with multidrug resistant organisms [7,8].
Lastly, the use of indirect calorimetry requires training to ensure accurate use and interpretation of measurements, funding for consumables/device maintenance and time to complete measurements and adapt nutrition therapy accordingly [4,8]. Prioritizing the completion of measurements can be difficult in light of competing clinician priorities and in periods of low staff availability or high patient loads.
ESTIMATED VERSUS MEASURED ENERGY EXPENDITURE
Indirect calorimetry is recommended as the reference method to determine mREE in critical care nutrition practice guidelines [1]. One of the main arguments in favor of using indirect calorimetry stems from the imprecision of predictive equations in estimating mREE. Over the course of ICU admission, this can result in substantial underfeeding or overfeeding. Data describing the accuracy and/or bias of predictive equations continues to be published in various ICU populations including surgical [9,10], trauma [11,12], medical [13] and mixed [14,15] critically ill patients, reinforcing the poor predictive value of equations. Unsurprisingly, the last few years have also seen an increase in the number of publications describing mREE in patients with SARS-CoV-2 infection [16▪,17,18▪]. Energy expenditure data in these articles is conflicting and agreement with predictive equations is poor. Further, Rousseau et al. provide one of the first reports of mREE in 55 patients discharged from the ICU following an at least 7-day admission, comparing mREE to the Harris–Benedict, Penn-State and 30 kcal/kg/day weight-based equation [19▪▪]. Indirect calorimetry measurements were completed 4 (3–6) days following ICU discharge, with mREE equivalent to 23 (19–24) kcal/kg/day. The Harris–Benedict and 30 kcal/kg/day overestimated mREE at the group level, and all equations displayed wide 95% limits of agreement when compared with mREE. Data on mREE in the post-ICU period is scarce, with further studies warranted to guide nutrition therapy following ICU discharge.
DOES ROUTINE USE OF INDIRECT CALORIMETRY IMPROVE OUTCOMES?
Three systematic reviews and meta-analyses of randomized controlled clinical trials (RCTs) on indirect calorimetry-guided energy delivery have been completed within the last year [20▪▪,21▪,22]. One of these reviews (Pertzov et al., four studies, n = 1052 participants) compared trials where energy delivery was greater than 80% of mREE in the intervention and less than 80% of estimated or mREE in the control. Of note, in the second-largest trial included in the analysis, indirect calorimetry was only performed in two-thirds of patients and only on one occasion [23]. The remaining two reviews [Duan et al., eight studies, n = 991 participants and Heyland et al., nine studies, n = 1176 participants) included all trials where indirect calorimetry was used to guide energy delivery in the intervention and predictive equations were used in the control group.
Meta-analyses by Pertzov et al. and Duan et al. reported a lower 28-day all-cause mortality [risk ratio (RR) 0.79, 95% confidence interval (CI) 0.63–0.99] and short-term mortality (RR 0.77, 95% CI 0.60–0.98) in favor of the intervention group, respectively. Conversely, Heyland et al. found no difference in overall mortality (RR 0.84, 95% CI 0.68–1.04). No other differences were reported in outcome measures including duration of mechanical ventilation, nosocomial infection rate, ICU and hospital length of stay [20▪▪,21▪,22]. In our opinion, the conclusion that use of indirect calorimetry can decrease mortality should be interpreted with caution, for several reasons:
-
(1)
All trials included are either small or intermediate size.
-
(2)
None of the individual trials demonstrate a mortality benefit.
-
(3)
Analysis of mortality at different timepoints led to differing conclusions.
-
(4)
In the largest trial with a trend towards benefit included in the meta-analyses of Pertzov and Duan, mortality data is inconsistent over time [24].
-
(5)
There is no consistent benefit to other patient-centered outcomes, which could explain the mechanism by which indirect calorimetry-guided isocaloric energy delivery would reduce mortality.
-
(6)
The mean increase in energy delivery to patients with indirect calorimetry-guided nutrition was approximately 20%. As highlighted in a recent review on underfeeding in critical illness, five major RCTs on energy targets in the ICU failed to demonstrate either benefit or harm over a wide range of energy provision in the acute phase of critical illness [25]. Although it can be argued that personalized energy delivery avoids potential harms from underfeeding or overfeeding to a greater extent than predictive equations, it is unlikely that it would confer a mortality benefit undetected in other RCTs.
THE CLINICAL RELEVANCE OF ENERGY BALANCE
As the majority of large RCTs fail to demonstrate a mortality benefit in various areas of ICU research, it is unlikely that further RCTs on indirect calorimetry-guided nutrition will provide a clear signal of benefit in this regard [26]. However, avoiding prolonged periods of underfeeding or overfeeding may have other benefits beyond measurable reductions in mortality or morbidity. This section will explore potential clinical implications of measuring energy expenditure using indirect calorimetry and directions for future research.
What is the true incidence of hyper/hypometabolism in the ICU?
A barrier to determining the importance of energy balance on outcomes is the identification of ICU patients who will accumulate substantial energy deficits when predictive equations are used instead of indirect calorimetry. In particular, this would concern patients with pronounced hypermetabolism (REE >30 kcal/kg/day) and a prolonged ICU stay. The true incidence and temporal pattern of hypermetabolism is difficult to discern from the literature, as 1) the majority of publications describing the distribution of mREE are small retrospective studies, 2) data is often presented as means ± standard deviation without standardization to body weight, obscuring the incidence of outliers, and 3) indirect calorimetry measurements are usually completed at one timepoint with the day of measurement often omitted.
Several recent publications indicate that a mREE of greater than 30 kcal/kg/day is not uncommon. A retrospective study of 105 mixed medical/surgical ICU patients reported mREE and oxygen delivery in the early phase of critical illness [27▪]. Median mREE was 20–25 kcal/kg ideal body weight (IBW), but a substantial number of observations exceeded 30 kcal/kg/day (with the 95th percentile approaching 50 kcal/kg/day). mREE was more variable in elderly patients (≥65 years of age). Of interest, nine observations of very low mREE values were reported (≤10.5 kcal/kg IBW/day). Although five patients with profoundly low metabolism died, four cases with an mREE of 9.5–10.5 kcal/kg/day in conjunction with low cardiac index survived to day 28 (T. Ebihara, personal communication, 23 September 2022). A similar pattern of hypermetabolic/hypometabolic outliers is found in other studies [28–30]. These examples clearly illustrate a problem with reserving indirect calorimetry for select occasions. As outliers in mREE cannot be predicted, they will often go undetected in the absence of routine measurements, posing a significant risk of underfeeding or overfeeding.
Temporal changes in energy expenditure during critical illness
Consideration to temporal changes in mREE during ICU stay is also essential. This is of greatest relevance in patients with persistent critical illness, where the use of a single mREE value to guide energy delivery may result in substantial underfeeding or overfeeding if metabolic needs vary over time. During the COVID-19 pandemic, several observational studies of longitudinal mREE measurements in ICU patients with SARS-CoV-2 have been performed [16▪,17,18▪,31]. Results range from moderate–high to low–normal metabolic rate in patients with an ICU length of stay greater than 2 weeks. A potential interpretation is that even in homogenous cohorts with respect to age, acute disease and comorbidities, it is hard to draw any general conclusions about trends in mREE.
Energy balance and body composition in ICU nutrition trials
Avoiding prolonged periods of underfeeding may have other benefits beyond measurable reductions in mortality or morbidity. A negative energy balance will inevitably result in some degree of muscle loss over time. In healthy overweight subjects, a 20% calorie restriction over 12–14 weeks led to a 3% reduction in appendicular lean body mass [32]. As muscle catabolism is accelerated during critical illness, any additional muscle loss from prolonged underfeeding may have a detrimental impact on muscle structure, function and recovery [33].
Only a handful of small studies have investigated the effect of additional energy delivery on body composition. An observational study by Fetterplace et al.[34] found an association between cumulative energy deficits and loss of fat free mass using bioimpedance spectroscopy. In contrast, a more recent study of 32 ICU patients did not find any correlation between muscle loss derived from computer tomography scans and energy delivery [35]. The nearly completed Intensive Nutrition In Critically Ill Adults (INTENT) trial [36▪], randomizing patients to an individualized and intensive whole hospital intervention, including dedicated post-ICU dietician follow-up, also includes a nested substudy of 80 patients with weekly measurements of bioimpedance spectroscopy and muscle ultrasound (NCT04896515). Although not a trial of indirect calorimetry-guided feeding, the results will shed further light on the importance of cumulative energy balance for prevention of muscle wasting.
Future trials of indirect calorimetry-guided energy delivery should consider the recent consensus statement on core outcomes in trials of nutritional and metabolic interventions in critical illness: physical function, nutritional status (encompassing an evaluation of muscle mass), muscle/nerve function and body composition were all considered ‘essential’ or ‘recommended’ domains at 30/90 days postrandomization [37▪▪].
RCTs will not provide (all) the answers
Based on our current knowledge, exposing patients with persistent hypermetabolism to prolonged underfeeding in the setting of a clinical trial would be unethical. Further physiological and observational studies are, therefore, needed to elucidate the impact of energy deficits on protein catabolism. A recent study by Sundström Rehal et al.[38] investigated the effect of half-dose versus full-dose enteral nutrition on protein kinetics in ICU patients. Although whole-body protein balance improved during full enteral feeding, inference about the effects on muscle protein is limited by a small sample size, the single-pool model used, and fixed ratios of calories and protein administered. Tracer studies using a two-pool or three-pool model to investigate lower limb protein balance while only manipulating energy delivery could be of value to address the importance of personalized nutrition in hypermetabolic states. The relative importance of endogenous energy substrates in different phases of critical illness could also be explored using stable isotope dilution techniques.
A multicenter observational study (NCT05124860) to clarify trends in mREE and associated characteristics in persistent critical illness is currently ongoing.
OTHER POTENTIAL APPLICATIONS OF INDIRECT CALORIMETRY
Recent publications also highlight potential applications of indirect calorimetry beyond the assessment of mREE and guidance of energy delivery. During critical illness, tissue hypoxia may arise from insufficient oxygen delivery or impaired oxygen utilization [39]. Indirect calorimetry may have a role to evaluate the adequacy of cellular respiration in shock states.
Hoeyer-Nielsen et al.[40] investigated the association between VO2 and survival in a retrospective cohort of 48 mechanically ventilated septic patients with continuous gas exchange monitoring. They found a lower VO2 : lactate ratio and a decrease in VCO2 over time in nonsurvivors [40]. These results are partially in line with a prospective observational study by Hirayama et al. In 34 septic patients, a 120 min indirect calorimetry measurement was performed within 24 h of tracheal intubation. VO2 and VCO2 decreased over time in all nonsurvivors (n = 8), whereas lactate concentrations increased [41]. In a large retrospective cohort of cardiac surgery patients, Veraar et al.[42▪] also found an association between prolonged postoperative hypometabolism and mortality. These publications indicate that gas exchange measurements may be used as a prognostic marker in various forms of critical illness, or as a tool to identify patients with impaired cellular metabolism. Larger prospective studies are required to determine the utility of indirect calorimetry in this regard.
Continuous monitoring with indirect calorimetry may also be used for assessment of rapid dynamic changes in oxygen delivery and metabolism. In an intriguing feasibility study of critical care rehabilitation, van den Oever et al.[43▪▪] performed indirect calorimetry during active in-bed cycling in seven mechanically ventilated patients. Using VO2 and VCO2 in conjunction with vital signs, factors limiting exercise tolerance could be identified in a majority of patients. The authors also highlight the potential utility of ergometry in difficult weaning from invasive ventilation.
Currently, research on dynamic changes in energy metabolism is limited by the use of indirect calorimetry as a standalone device. A more widespread integration of gas exchange modules into ventilators or other patient monitors will hopefully facilitate work in this field.
A PRAGMATIC APPROACH TO INDIRECT CALORIMETRY
It is unlikely that future trials will demonstrate a mortality benefit from routine use of indirect calorimetry during critical illness. However, this holds true for almost any monitoring tool in the ICU. Despite potential barriers to indirect calorimetry in clinical practice, we believe there is a strong physiological rationale to measure energy expenditure in critically ill patients who require medical nutrition therapy for a prolonged period of time. It is reasonable to avoid significant underfeeding or overfeeding even in the absence of evidence for improved outcomes. As mREE during critical illness is highly variable and difficult to predict, indirect calorimetry is a valuable tool to achieve this goal. Table 1 provides a pragmatic approach to using indirect calorimetry in the ICU.
Table 1.
Pragmatic approach to using indirect calorimetry in the ICU
| A conservative estimate of energy expenditure (20 kcal/kg/day or similar) and routine use of hypocaloric feeding (not exceeding 70% of energy expenditure) should be used to guide energy delivery in the early acute phase of critical illness. Indirect calorimetry can be considered in priority patient groups if resources are available, to identify significant hypometabolism and avoid early overfeeding. |
| Indirect calorimetry should be prioritized in select patient groups to identify significant hypometabolism or hypermetabolism including (but not limited to): • Patients likely to remain mechanically ventilated/require medical nutrition therapy for at least 5 to 7 days. • Patients where body composition (e.g. obesity), old age or clinical conditions (e.g. major burn injury) make estimation of energy expenditure challenging. |
| Indirect calorimetry should be repeated every 3-4 days if possible (weekly at a minimum), or following significant changes in clinical state of patients. |
CONCLUSION
Indirect calorimetry is recommended for guiding energy delivery in critically ill patients. Data on whether indirect calorimetry improves outcomes remains inconclusive and barriers to use prohibit application in all patients. In the absence of definitive evidence, repeat indirect calorimetry measurements should be considered in patients likely to have prolonged ICU admissions and those where estimation of energy expenditure is challenging, to minimize underfeeding and overfeeding. Indirect calorimetry may also have potential applications beyond the measurement of energy expenditure and is an area for future research.
To address the question in the title of this review: we propose that indirect calorimetry should be a part of routine care, in specific situations.
Acknowledgements
The authors would like to thank Takeshi Ebihara for sharing additional data from his research.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Noyahr JK, Tatucu-Babet OA, Chapple LS, et al. Methodological rigor and transparency in clinical practice guidelines for nutrition care in critically ill adults: a systematic review using the AGREE II and AGREE-REX Tools. Nutrients 2022; 14:2603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2▪.Moonen HPFX, Beckers KJH, van Zanten ARH. Energy expenditure and indirect calorimetry in critical illness and convalescence: current evidence and practical considerations. J Intensive Care 2021; 9:8. [DOI] [PMC free article] [PubMed] [Google Scholar]; A well written and extensive narrative review on energy metabolism and indirect calorimetry during critical illness.
- 3.Kinney JM. Indirect calorimetry in malnutrition: nutritional assessment or therapeutic reference? JPEN J Parenter Enteral Nutr 1987; 11: (5 Suppl): 90S–94S. [DOI] [PubMed] [Google Scholar]
- 4.McClave SA, Omer E. Point-counterpoint: indirect calorimetry is not necessary for optimal nutrition therapy in critical illness. Nutr Clin Pract 2021; 36:268–274. [DOI] [PubMed] [Google Scholar]
- 5.Heyland DK, Cahill N, Day AG. Optimal amount of calories for critically ill patients: depends on how you slice the cake!. Crit Care Med 2011; 39:2619–2626. [DOI] [PubMed] [Google Scholar]
- 6.Lambell KJ, Miller EGS Tatucu-Babet##OA, et al. Nutrition management of obese critically ill adults: asurvey of critical care dietitians in Australia and New Zealand. Aust Crit Care 2021; 34:3–8. [DOI] [PubMed] [Google Scholar]
- 7.Achamrah N, Delsoglio M, De Waele E, et al. Indirect calorimetry: the 6 main issues. Clin Nutr 2021; 40:4–14. [DOI] [PubMed] [Google Scholar]
- 8.De Waele E, van Zanten ARH. Routine use of indirect calorimetry in critically ill patients: pros and cons. Crit Care 2022; 26:123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ruan H, Tang Q, Yang Q, et al. Resting energy expenditure early after cardiac surgery and validity of predictive equations: a prospective observational study. Ann Nutr Metab 2021; 77:271–278. [DOI] [PubMed] [Google Scholar]
- 10.Lee SJ, Lee HJ, Jung YJ, et al. Comparison of measured energy expenditure using indirect calorimetry vs predictive equations for liver transplant recipients. JPEN J Parenter Enteral Nutr 2021; 45:761–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu S, Iqbal S, Giroux M, et al. Penn State equation versus indirect calorimetry for nutritional assessment in patients with traumatic brain injury. Can J Surg 2022; 65:E320–E325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pelekhaty SL, Ramirez CL, Massetti JM, et al. Measured vs predicted energy expenditure in mechanically ventilated adults with acute, traumatic spinal cord injuries. Nutr Clin Pract 2021; 36:464–471. [DOI] [PubMed] [Google Scholar]
- 13.Hölzel C, Weidhase L, Petros S. The effect of age and body mass index on energy expenditure of critically ill medical patients. Eur J Clin Nutr 2021; 75:464–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oliveira ACDS, de Oliveira CC, de Jesus MT, et al. Comparison of equations to predict energy requirements with indirect calorimetry in hospitalized patients. JPEN J Parenter Enteral Nutr 2021; 45:1491–1497. [DOI] [PubMed] [Google Scholar]
- 15.Kamel AY, Robayo L, Liang D, et al. Estimated vs measured energy expenditure in ventilated surgical-trauma critically ill patients. JPEN J Parenter Enteral Nutr 2022; 46:1431–1440. [DOI] [PubMed] [Google Scholar]
- 16▪.Niederer LE, Miller H, Haines KL, et al. Prolonged progressive hypermetabolism during COVID-19 hospitalization undetected by common predictive energy equations. Clin Nutr ESPEN 2021; 45:341–350. [DOI] [PMC free article] [PubMed] [Google Scholar]; Important observational study of longitudinal mREE in ICU patients with COVID-19, demonstrating a sustained increase in mREE over time in this cohort.
- 17.Lakenman PLM, van der Hoven B, Schuijs JM, et al. Energy expenditure and feeding practices and tolerance during the acute and late phase of critically ill COVID-19 patients. Clin Nutr ESPEN 2021; 43:383–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18▪.von Renesse J, von Bonin S, Held HC, et al. Energy requirements of long-term ventilated COVID-19 patients with resolved SARS-CoV-2 infection. Clin Nutr ESPEN 2021; 44:211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]; Another observational study of longitudinal mREE in critically ill COVID-19 patients, which did not find a persisting hypermetabolism several weeks after ICU admission.
- 19▪▪.Rousseau AF, Fadeur M, Colson C, Misset B. Measured energy expenditure using indirect calorimetry in post-intensive care unit hospitalized survivors: a comparison with predictive equations. Nutrients 2022; 14:3981. [DOI] [PMC free article] [PubMed] [Google Scholar]; To our knowledge, the only observational study of mREE in post-ICU patients. An important contribution to a field which requires more research.
- 20▪▪.Duan JY, Zheng WH, Zhou H, et al. Energy delivery guided by indirect calorimetry in critically ill patients: a systematic review and meta-analysis. Crit Care 2021; 25:88. [DOI] [PMC free article] [PubMed] [Google Scholar]; An updated systematic review and meta-analysis on trials of indirect calorimetry-guided energy delivery.
- 21▪.Pertzov B, Bar-Yoseph H, Menndel Y, et al. The effect of indirect calorimetry guided isocaloric nutrition on mortality in critically ill patients-a systematic review and meta-analysis. Eur J Clin Nutr 2022; 76:5–15. [DOI] [PubMed] [Google Scholar]; Another updated systematic review and meta-analysis of indirect calorimetry-guided energy delivery.
- 22. Heyland DK, LZ-Y, Lew CCH, et al. Nutritional prescription: use of indirect calorimetry vs. predictive equations. 2021: Critical Care Nutrition.com. [Google Scholar]
- 23.Heidegger CP, Berger MM, Graf S, et al. Optimisation of energy provision with supplemental parenteral nutrition in critically ill patients: a randomised controlled clinical trial. Lancet 2013; 381:385–393. [DOI] [PubMed] [Google Scholar]
- 24.Casaer MP, Van den Berghe G, Gunst J. Indirect calorimetry: a faithful guide for nutrition therapy, or a fascinating research tool? Clin Nutr 2021; 40:651. [DOI] [PubMed] [Google Scholar]
- 25.Tatucu-Babet OA, Ridley EJ. How much underfeeding can the critically ill adult patient tolerate? J Intensive Med 2022; 2:69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Veldhoen RA, Howes D, Maslove DM. Is mortality a useful primary end point for critical care trials? Chest 2020; 158:206–211. [DOI] [PubMed] [Google Scholar]
- 27▪.Ebihara T, Shimizu K, Ojima M, et al. Energy expenditure and oxygen uptake kinetics in critically ill elderly patients. JPEN J Parenter Enteral Nutr 2022; 46:75–82. [DOI] [PubMed] [Google Scholar]; A comparatively large cohort of ICU patients with early REE measurements, demonstrating a large variability and high and low outliers particularly in elderly patients.
- 28.Wewalka M, Schneeweiss M, Haselwanter P, et al. Age-dependent differences in energy metabolism in the acute phase of critical illness. Nutrition 2022; 101:111684. [DOI] [PubMed] [Google Scholar]
- 29.Israfilov E, Kir S. Comparison of energy expenditure in mechanically ventilated septic shock patients in acute and recovery periods via indirect calorimetry. JPEN J Parenter Enteral Nutr 2021; 45:1523–1531. [DOI] [PubMed] [Google Scholar]
- 30.Occhiali E, Urli M, Pressat-Laffouilhère T, et al. Dynamic metabolic changes measured by indirect calorimetry during the early phase of septic shock: a prospective observational pilot study. Eur J Clin Nutr 2022; 76:693–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Karayiannis D, Maragkouti A, Mikropoulos T, et al. Neuromuscular blockade administration is associated with altered energy expenditure in critically ill intubated patients with COVID-19. Clin Nutr 2021; S0261-5614(21)00259-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weiss EP, Jordan RC, Frese EM, et al. Effects of weight loss on lean mass, strength, bone, and aerobic capacity. Med Sci Sports Exerc 2017; 49:206–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chapple LS, Parry SM, Schaller SJ. Attenuating muscle mass loss in critical illness: the role of nutrition and exercise. Curr Osteoporos Rep 2022; 20:290–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fetterplace K, Beach LJ, MacIsaac C, et al. Associations between nutritional energy delivery, bioimpedance spectroscopy and functional outcomes in survivors of critical illness. J Hum Nutr Diet 2019; 32:702–712. [DOI] [PubMed] [Google Scholar]
- 35.Lambell KJ, Goh GS, Tierney AC, et al. Marked losses of computed tomography-derived skeletal muscle area and density over the first month of a critical illness are not associated with energy and protein delivery. Nutrition 2021; 82:111061. [DOI] [PubMed] [Google Scholar]
- 36▪.Ridley EJ, Bailey M, Chapman M, et al. Protocol summary and statistical analysis plan for Intensive Nutrition Therapy comparEd to usual care iN criTically ill adults (INTENT): a phase II randomised controlled trial. BMJ Open 2022; 12:e050153. [DOI] [PMC free article] [PubMed] [Google Scholar]; An ongoing trial of a whole hospital nutritional intervention in ICU patients. Substudies will include longitudinal analysis of body composition.
- 37▪▪.Davies TW, van Gassel RJJ, van de Poll M, et al. Core outcome measures for clinical effectiveness trials of nutritional and metabolic interventions in critical illness: an international modified Delphi consensus study evaluation (CONCISE). Crit Care 2022; 26:240. [DOI] [PMC free article] [PubMed] [Google Scholar]; A consensus statement on core outcome measures in trials of nutrition/metabolic interventions in critically ill patients, endorsed by patients, clinicians, and researchers in the field.
- 38.Sundström Rehal M, Liebau F, Wernerman J, Rooyackers O. Whole-body protein kinetics in critically ill patients during 50 or 100% energy provision by enteral nutrition: a randomized cross-over study. PLoS One 2020; 15:e0240045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vincent JL, De Backer D. Oxygen transport-the oxygen delivery controversy. Intensive Care Med 2024; 30:1990–1996. [DOI] [PubMed] [Google Scholar]
- 40.Hoeyer-Nielsen AK, Holmberg MJ, Grossestreuer AV, et al. Association between the oxygen consumption: lactate ratio and survival in critically ill patients with sepsis. Shock 2021; 55:775–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hirayama I, Asada T, Yamamoto M, et al. Changes in carbon dioxide production and oxygen uptake evaluated using indirect calorimetry in mechanically ventilated patients with sepsis. Crit Care 2021; 25:416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42▪.Veraar C, Fischer A, Bernardi MH, et al. Absent metabolic transition from the early to the late period in non-survivors post cardiac surgery. Nutrients 2022; 14: [DOI] [PMC free article] [PubMed] [Google Scholar]; A retrospective observational study of cardiothoracic ICU patients, indicating that a persisting low metabolic rate may be of negative prognostic importance.
- 43▪▪.van den Oever HLA, Kök M, Oosterwegel A, et al. Feasibility of critical care ergometry: exercise data of patients on mechanical ventilation analyzed as nine-panel plots. Physiol Rep 2022; 10:e15213. [DOI] [PMC free article] [PubMed] [Google Scholar]; An interesting feasibility study investigating the potential utility of critical care ergometry during physiotherapy.