Purpose of review
To highlight progress in glaucoma therapy challenging the traditional medication-first approach and present evidence supporting early standalone surgery in the era of micro-invasive glaucoma surgery (MIGS).
Recent findings
Medical therapy is limited by well documented poor adherence that compromises the quality of intraocular pressure reduction. Results from modern clinical trials demonstrate advantages of selective laser trabeculoplasty and MIGS procedures in terms of both IOP control and progression risk.
Summary
The MIGS options for pseudophakic or precataractous patients are limited by regulatory rules that require the performance of some procedures only at the time of cataract surgery. These include the iStent/iStent Inject and the Hydrus implants. Nonbleb-forming procedures currently available for standalone use in eyes with mild–moderate primary open-angle glaucoma include gonioscopy-assisted transluminal trabeculotomy (which lowers IOP by 28-61% and medication use by 38–73% in various studies), trabecular ablation with the Trabectome (23–39% and 21–43%, respectively), excisional goniotomy with the Kahook Dual Blade (15–36% and 15–40%, respectively), ab interno canaloplasty (35% and 57%, respectively), and combined canaloplasty and trabeculotomy using the OMNI system (39–40% and 64–73%, respectively). For patients who would benefit from early standalone surgery, these procedures offer meaningful reductions in both IOP and medication burden.
Keywords: glaucoma, micro-invasive glaucoma surgery, standalone
INTRODUCTION
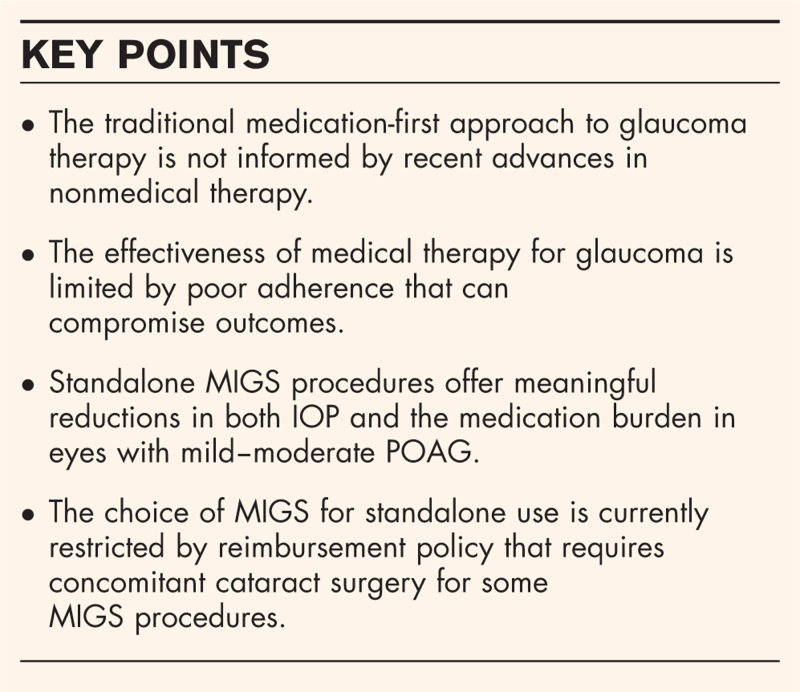
The traditional approach to glaucoma therapy – topical medications as first line followed if needed by laser and then surgery, all with the goal of lowering intraocular pressure (IOP) – has been largely unchanged for over 150 years [1]. The development of a family of procedures –collectively called micro-invasive glaucoma surgery (MIGS) – addresses an unmet need for a procedure for patients with mild-to-moderate glaucoma who would benefit from early surgical management but whose therapeutic target does not justify the risks of traditional procedures such as trabeculectomy or tube-shunt implantation [2–5]. The indications for MIGS include reduction of IOP, reduction of the medication burden, or a combination of both. In general, standalone procedures are more often performed with the goal of IOP reduction, while procedures combined with cataract surgery are more likely to be performed with the goal of medication reduction. Because as of this moment, trabecular MIGS stents are approved for use only in combination with cataract surgery and most payors will not reimburse for their standalone use, some MIGS stents are not available to patients who require standalone surgery for IOP reduction. Further, the benefits of medication reduction as a goal for surgical intervention should not be underestimated, given the significant and myriad limitations of medical therapy. This article will review the limitations of the current glaucoma treatment paradigm and make a case for earlier use of standalone MIGS for modern glaucoma management.
Box 1.
no caption available
CHALLENGING THE CURRENT GLAUCOMA TREATMENT PARADIGM
Medications, laser therapy, and surgical procedures have all been shown to effectively reduce the risk of glaucoma progression [6–10]. The order in which they are traditionally deployed reflects the relative risks and benefits of each option: medications effectively lower IOP with low risk, while traditional surgery delivers maximal IOP reduction but carries significantly higher risk of potentially sight-threatening complications. This treatment paradigm does not reflect modern therapeutic innovations or our expanding awareness of their strengths and limitations, as described below.
Medications are not as effective in the real world as we are led to believe based on clinical trial efficacy outcomes. Topical solutions and suspensions of medications – and fixed combinations thereof – can effectively and safely lower IOP, but these treatment options are not without significant limitations, the most important of which relate to a trio of inter-related factors: adherence, tolerability, and toxicity. Patterns and contributors to nonadherence with glaucoma therapy have been comprehensively described [11–14]. More than half of patients are nonadherent with therapy after 3–4 years of treatment [15,16], and at a cost: nonadherent patients are more likely than adherent patients to experience disease progression [17,18]. Among other factors, nonadherence has been linked to forgetfulness, the cost of therapy, and the disincentive of side effects [11–14]. Side effects of glaucoma medications can range from the cosmetic (e.g. conjunctival hyperemia with prostaglandin analogue therapy [19]) to the minor (such as transient stinging upon instillation) to the more significant [such as prostaglandin-associated periorbitopathy (PAP)]. PAP is a syndrome of gradual onset characterized by eyelash changes that include lengthening, thickening, and/or darkening, hyperpigmentation of the iris and periorbital skin, vellus hair growth, potentially irreversible deepening of the upper eyelid sulcus (DUES), periorbital fat loss, ptosis, and enophthalmos [20–23]. PAP is cosmetically displeasing, and DUES and orbital fat loss in particular may also complicate future ocular surgery because of globe retroplacement into the orbit in the supine position. Recently, prostaglandin analogues have been shown to be associated with a very high prevalence of meibomian gland dysfunction, which is seen in up to 92% of patients using a prostaglandin analogue [24]. In addition to active ingredients, some excipient ingredients have also been associated with ocular surface toxicity. The most important contributor to ocular toxicity is benzalkonium chloride (BAK), a preservative found in ∼70% of all ophthalmic formulations [25,26]. BAK is linked to multiple cytotoxic effects on ocular surface cells [27,28,29▪] resulting in significant signs and/or symptoms of ocular surface disease (OSD) in 30–70% of patients using topical therapy [30–36]. The likelihood of developing OSD doubles with each additional BAK-containing eye drop prescribed [33]. OSD symptoms can disincentivize adherence, leading to poor disease control and the addition of more medications in a vicious cycle.
Laser therapy – once a stopgap between maximal medical therapy and surgery – has evolved to a safe, well tolerated, and repeatable form that can offer long-term disease control when used as primary therapy [9,37▪▪]. Several studies have compared primary trabeculoplasty to primary medical therapy in a direct challenge to the medications-first paradigm [8,9,38]. Among these, both the Glaucoma Laser Trial (using argon laser trabeculoplasty) and the Laser in Glaucoma and Ocular Hypertension Trial [using selective laser trabeculoplasty (SLT)] demonstrated better visual field outcomes in laser-first eyes compared with medications-first eye therapy [8,39], and there is early evidence that a paradigm shift to primary SLT is underway [40]. Further, the prospective, multicenter COAST trial (Clarifying the Optimal Application of SLT Therapy), supported by the US National Institutes of Health, is actively enrolling newly diagnosed and treatment-naive patients with mild–moderate primary open-angle glaucoma (POAG) or high-risk ocular hypertension to evaluate the optimal use of primary SLT to prolong medication-free survival [41▪▪].
The glaucoma surgical landscape has evolved substantially in the past decade. As far back as the 1990s, primary surgery was evaluated in the Moorfields Primary Therapy Trial (MPTT) [42] and the Collaborative Initial Glaucoma Treatment Study (CIGTS) [7], the former of which demonstrated better visual field outcomes in the laser and surgery groups compared with the medication group. In more modern times, MIGS procedures have begun to replace traditional procedures for surgeons around the world, with consistent reductions in rates of trabeculectomy with commensurate increases in rates of MIGS procedures in the United States [43▪,44▪], Germany [45▪], France [46], Australia [47], and Japan [48]. MIGS procedures are generally somewhat less effective than traditional filtering procedures but have a more favorable safety profile, positioning them well for early deployment in patients with mild-to-moderate disease and modest treatment goals [2–5].
Together, these observations illustrate that the long-held practice of starting with medications and reserving surgery as a last resort does not reflect the efficacy and safety of modern therapies and may not represent the optimal treatment of glaucoma today.
EXPANDING THE ROLE FOR STANDALONE MICRO-INVASIVE GLAUCOMA SURGERY
Minimizing or eliminating the requirement to self-administer topical medications is a desirable goal for most patients. Freedom from (or a reduced need for) drop therapy offers numerous advantages. The most significant of these is that nonadherence can be eliminated or, where adjunctive drop therapy is still necessary, of less risk. Nonadherence increases the risk of glaucoma progression, so by extension, eliminating nonadherence may improve long-term outcomes [17–18]. The ongoing side effects of topical therapy can also be avoided, including the development of preservative-related OSD. OSD comorbid to glaucoma adversely affects quality of life [49,50], and the use of BAK-preserved medications adversely affects quality of life more than BAK-free medications [51,52]. MIGS improves the signs, symptoms, and severity of OSD in patients using topical medications preoperatively [53]. Further, the MPTT demonstrated that surgery more effectively prevented visual field progression than medical therapy [42] (although this was not confirmed in CIGTS [7]). Also, there are intuitive, intangible benefits of a drop-free treatment regimen. Self-administration of one or more drops per day from one or more bottles (and many glaucoma patients require more than one medication for adequate disease control [54–55]) is a hassle. It is time-consuming, exposes patients to instillational side effects once or more daily, and further, it is a daily reminder of the presence of a potentially vision-threatening condition for which the benefits of therapy are imperceptible to patients. The impact of this ‘hassle factor’ on quality of life is difficult to measure, as there are no validated instruments designed to measure the impact of glaucoma treatment on quality of life. This shortcoming was underscored by the LiGHT study's inability to demonstrate a quality-of-life benefit to SLT over medical therapy [9] when intuitively one should exist. Such an instrument – and specific to vision-related quality of life in MIGS patients – is in development in response to a recognized unmet need for such a tool [56,57]. However, there are some limited data on the relationship between MIGS and quality of life. MIGS has been associated with higher patient satisfaction and quality of life compared with trabeculectomy [58]. Recently, an analysis of data from the trabecular micro-bypass (iStent Inject, Glaukos) demonstrated a higher proportion of patients with improved quality of life (using the general Vision Function Questionnaire VFQ-25) following combined phacoemulsification and implant surgery versus phacoemulsification alone, supporting the benefit of MIGS on quality of life; this improvement in quality of life was associated with being medication-free [59▪▪].
One potential benefit to employing a procedure to control IOP compared with a pharmaceutical therapy may be a better quality of IOP reduction. Pharmaceutical IOP reduction is inherently variable, with fairly wide peaks and troughs for most agents shortly following and preceding dosing, respectively. Additionally, not all eye drops work well in the habitual nocturnal period [60,61]. Data from the GEMINI study demonstrated that combined canaloplasty and trabeculotomy with the OMNI (Sight Sciences) reduced IOP fluctuations in addition to lowering IOP 12 months postoperatively [62▪]. Compliance with topical therapy is inherently worse than laser or MIGS. In the LiGHT study, there were fewer rapid progressors and fewer patients requiring major glaucoma surgery in the laser group, despite similar IOP measurements as drop-treated eyes at study visits [39]. In the 3-year HORIZON study, placement of the Hydrus (Ivantis) with cataract surgery demonstrated a significant difference in the risk of secondary glaucoma surgery at 3 years compared with cataract surgery alone, despite the IOPs in both groups being treated to roughly the same level [63▪▪]. It is notable that eyes undergoing cataract extraction alone required more medications than those undergoing Hydrus placement with cataract extraction. Therefore, a growing literature supports these findings that IOP-lowering procedures may do a better job of reducing glaucoma progression and/or secondary surgical intervention than medically treated eyes.
These benefits of early surgery have not been sufficient to justify the early use of traditional procedures such as trabeculectomy or tube-shunts, but the emergence of MIGS procedures has tipped the risk–benefit scale in favor of early surgery to afford the aforementioned benefits of early surgery to patients who otherwise would not be considered appropriate surgical candidates. MIGS were designed with safety in mind. The initial characterization of the MIGS family of procedures consisted of five key features that would support their use early in the treatment cascade: an ab interno approach, minimally traumatic to the target tissues, at least modest efficacy compared with traditional procedures, greater safety than traditional procedures, and rapid visual recovery with minimal impact on quality of life [64].
Despite the rapid and widespread adoption of MIGS (a >400% increase in utilization in the United States from 2013 to 2018 [43▪]), evidence suggests that they remain broadly underutilized. An estimated 18% of more than 21 000 eyes undergoing cataract surgery in a multilocation managed care practice had comorbid glaucoma [65]. Given that approximately 3.8 million cataract surgeries are performed annually in the United States [66], an estimated 684 000 eyes with glaucoma undergo cataract surgery annually. In 2018, only ∼40 000 MIGS procedures were performed in patients with a glaucoma diagnosis [43▪]. By extension, therefore, there are many, many pseudophakic patients with glaucoma who do not undergo MIGS at the time of cataract surgery and who might benefit from MIGS at a later date.
The MIGS options for these pseudophakic patients are limited. Several MIGS procedures – including the most commonly performed iStent/iStent Inject (Glaukos) implantation – are restricted by the labeled indication (in the United States) to use in conjunction with cataract surgery and are not covered by most payors as standalone surgery, rendering them effectively unavailable for pseudophakic patients with glaucoma in whom surgery would be of value. These differential indications have significant implications for access to surgery, as the vast majority of iStent implantations are performed by comprehensive (primarily cataract) surgeons, while most standalone procedures are performed by glaucoma specialists [44▪]. As of this writing, the only nonbleb-based MIGS procedures reimbursable as standalone procedures for mild-to-moderate glaucoma include various forms of trabeculotomy, goniotomy, and canaloplasty. There are two bleb-based MIGS procedures [the Xen 45 gel stent (Allergan) and PreserFlo microshunt (Santen/Glaukos)] indicated for refractory glaucomas (the latter not yet approved in the United States). Of note the iStent infinite, similar to the iStent inject except that three stents are implanted rather than two, was recently cleared in the United States for standalone use in refractory glaucoma. These devices are not considered herein as the focus of this article is early surgery for patients with mild–moderate glaucoma.
OUTCOMES OF STANDALONE MICRO-INVASIVE GLAUCOMA SURGERY
Multiple studies have evaluated the outcomes of trabeculotomy, goniotomy, and/or canaloplasty as standalone procedures for glaucoma. In addition, limited data are available on outcomes of standalone implantation of trabecular micro-bypass and Schlemm's canal implants that are approved for standalone use in some global markets (but not in the United States). Results of these studies are discussed here and summarized in Table 1 below.
Table 1.
Summary of efficacy outcomes of standalone micro-invasive glaucoma surgery procedures
| Procedure | Mean IOP reductions | Mean medication reductions |
| GATT | ||
| POAG [67–70] | 32–44% | 38–72% |
| Secondary OAG [67,69–73,74▪,75▪] | 28–68% | 49–86% |
| Refractory glaucoma [74▪,76,77▪] | 40–51% | 38–73% |
| Trabectome [81–86] | 23–39% | 21–43% |
| Excisional goniotomy (KDB) [88–91,92▪] | 15–36% | 15–40% |
| ABiC [94–96] | 25–40% | 46–79% |
| OMNI [100–102,103▪] | 27–40% | 35–73% |
IOP, intraocular pressure.
GATT, gonioscopy-assisted transluminal trabeculotomy, POAG, primary open-angle glaucoma, OAG, open-angle glaucoma, KDB, Kahook dual blade, ABiC, ab-interno canaloplasty.
Ab interno trabeculotomy
The ab interno trabeculotomy procedure has been described using either an illuminated or nonilluminated microcatheter. GATT describes a procedure in which a tip-illuminated microcatheter (iTrack, Nova Eye Medical, Kent Town, SA, Australia) is threaded through Schlemm's canal via an ab interno approach, advanced the full 360°, then cheese-wired to perform a complete trabeculotomy [67]. In retrospective standalone studies with follow-up of 6–24 months, mean IOP reductions of 32–44% were reported in eyes with primary open-angle glaucoma [67–70], of 28–68% in eyes with secondary open-angle glaucomas [67,69–73,74▪,75▪] and of 40–51% in eyes with prior failed glaucoma surgery [74▪,76,77▪]; respective mean reductions in medication use ranged from 38 to 72%, 49 to 86%, and 38 to 73%. These large differences between studies are likely attributable to differences in patient characteristics, therapeutic goals (IOP versus medication reduction), and follow-up durations. TRAB360 (now part of the OMNI system, Sight Sciences, Menlo Park, CA, USA) is similar to the GATT procedure except that a nonilluminated microcatheter – blue in color to aid visualization during passage – is utilized to perform the trabeculotomy. In a pair of retrospective studies of 5–12 months duration, mean IOP reductions of 31–32% and medication reductions of 35–82% have been reported in standalone cases [78,79].
Trabecular ablation
The Trabectome (MicroSurgical Technology, Redmond, WA, USA) utilizes an electrocautery handpiece to ablate a sector (typically less than 120 degrees) of trabecular meshwork [80]. A meta-analysis reported mean IOP reduction of 39% among six studies with follow-up ranging from 12 to 60 months [81]; mean medication reductions among the included studies ranged from 21 to 43% [82–85]. A more recent prospective study reported mean IOP reduction of 23% and medication reduction of 7%. A global registry study of greater than 5000 cases reported mean IOP reduction at 90 months of 29% with medication reduction of 38% [86]. These large data sets include both standalone cases and those combined with cataract surgery.
Excisional goniotomy
Excisional goniotomy is performed with the Kahook Dual Blade (New World Medical, Rancho Cucamonga, CA, USA), a disposable instrument incorporating a ramp that elevates and stretches the trabecular meshwork leading to two parallel blades that excise a strip of meshwork typically of 120° or less [87]. As a standalone procedure in prospective and retrospective studies of 6–24 months duration, mean IOP reductions of 15–36% and mean medication reductions of 15–40% were reported [88–91,92▪]. These large ranges likely represent differences between samples in the dual indications for MIGS: IOP reduction versus medication reduction. In a single retrospective study that conducted a subgroup analysis of eyes with high-baseline versus low-baseline IOP (with the assumption that high-IOP eyes sought IOP reduction and low-IOP eyes sought medication reduction), mean IOP reduction in high-IOP eyes was 46% and mean medication reduction in low-IOP eyes was 36% [89].
Canaloplasty
Ab interno canaloplasty is an evolution of suture canaloplasty, an ab externo procedure that included both viscodilation of Schlemm's canal and the placement of a 360° tension suture within the canal [93], that now consists of an ab interno procedure of viscodilation and mechanical dilation of the canal but without a retained tension suture [94]. Ab interno canaloplasty (ABiC) utilizes the iTrack tip-illuminated microcatheter to cannulate Schlemm's canal and dispense ophthalmic viscosurgical device (OVD) throughout its circumference upon withdrawal. In studies of ab interno canaloplasty with the iTrack, mean IOP reductions at 1 year ranged from 25 to 40% and medication reductions from 46 to 79%, with generally insignificant differences between standalone and combined cases [94–96]. The VISCO360 procedure (performed with a nonilluminated blue-colored microcatheter that is now part of the OMNI system, Sight Sciences) has been evaluated in a retrospective analysis of eyes with high-baseline (≥18 mmHg) or low-baseline (<18 mmHg) IOP [97]. Mean IOP reduction was 41% in high-IOP eyes and unchanged in low-IOP eyes, and both groups demonstrated an 89% reduction in medication use at 12 months. Similar data with longer follow-up have been published for the OMNI system when used for canaloplasty only, with significant mean IOP and medication reductions of 36 and 32% at 18 months [98].
Combined viscodilation and trabeculotomy
The OMNI surgical system (Sight Sciences) incorporates the historical TRAB360 and VISCO360 procedures into an integrated platform that facilitates up to a 360° mechanical canaloplasty and viscodilation of Schlemm's canal and the collector channel openings followed by up to a 360° trabeculotomy, if desired [99]. In studies of standalone procedures, mean IOP reductions of 27–40% and mean medication reductions of 48–73% were seen with follow-up ranging from 12 to 24 months [100–102]. In subgroup analysis, eyes with high baseline IOP (>18 mmHg) demonstrated mean IOP reduction of 28% and medication reduction of 29%, while low-baseline IOP eyes (≤18 mmHg) demonstrated mean IOP reduction of 11% and medication reduction of 35% [103▪].
Trabecular meshwork and Schlemm's canal implants
A recent meta-analysis of standalone trabecular micro-bypass (iStent, Glaukos, San Clemente, CA, USA) implantation reported a mean IOP reduction of 31% at 6–12 months and remained consistent (30.4–32.9%) through up to 60 months of follow-up [104▪▪]. The COMPARE study (included in the iStent meta-analysis) was a prospective, randomized comparison of two first-generation iStents versus a single Schlemm's canal microstent (Hydrus, Alcon, Fort Worth, TX, USA) as standalone procedures in eyes with open-angle glaucoma [105]. At 12 months, mean IOP reductions were 5 and 9% in the iStent and Hydrus groups, respectively, and medication reductions were 37 and 64%, respectively. In a prospective, nonrandomized comparison of standalone Hydrus to SLT in eyes with medically uncontrolled POAG, mean IOP reductions at 12 months were 26% for the Hydrus and 31% for SLT and medication reductions were 39 and 20%, respectively [106]. Of note, neither of these devices is approved in the United States for standalone use and must be paired with cataract extraction.
CONCLUSION
Benefits of early surgery for glaucoma include the elimination of nonadherence to topical medical therapy with better disease control, avoidance of medication-related side effects, and freedom from the hassles of daily self-dosing. The family of MIGS procedures represents an array of surgical options for patients with mild-to-moderate open-angle glaucoma whose therapeutic goals would otherwise not justify the risk profile of traditional filtering procedures. For pseudophakic patients, the MIGS options are limited in the United States and some other global markets by regulatory policy that precludes standalone surgery for common procedures such as iStent implantation that must be combined with cataract surgery. For these patients who would benefit from early surgery, the options include various forms of trabeculotomy (GATT, Trabectome), goniotomy (excisional goniotomy with the KDB), canaloplasty (ABiC or OMNI), or a combination of these (trabeculotomy and viscodilation with the OMNI system). Data from studies of standalone surgery support the use of these procedures for patients with mild–moderate open-angle glaucoma.
Acknowledgements
Assistance in the drafting of this manuscript was provided by Tony Realini, Hypotony Holdings, LLC.
Financial support and sponsorship
Sight Sciences provided funding for medical writing support and publication costs.
Conflicts of interest
N.R. serves as a consultant to the following companies: Alderya, Avellino, Aerie Pharmaceuticals; Alcon Vision, Alimera Sciences, Allergan/AbbVie, Bausch + Lomb, Beaver-Visitec International, Belkin, CATS, Carl Zeiss Meditec, CATS, Dompe, Ellex, ELIOS Vision Inc, Equinox, Eyepoint Pharmaceuticals, Glaukos, Iridex, IrisVision, Kala Pharmaceuticals, Lumenis, New World Medical, Novartis, Ocular Science, Ocular Therapeutix, Omeros, Reichert, Santen, Shire, Sight Sciences, Spyglass, Tarsus, Thea, TearClear, and ViaLase.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Realini T. A history of glaucoma pharmacology. Optom Vis Sci 2011; 88:36–38. [DOI] [PubMed] [Google Scholar]
- 2.Richter GM, Coleman AL. Minimally invasive glaucoma surgery: current status and future prospects. Clin Ophthalmol 2016; 10:189–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lavia C, Dallorto L, Maule M, et al. Minimally-invasive glaucoma surgeries (MIGS) for open angle glaucoma: a systematic review and meta-analysis. PLoS ONE 2017; 12:e0183142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ansari E. An update on implants for minimally invasive glaucoma surgery (MIGS). Ophthalmol Ther 2017; 6:233–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fellman RL, Mattox C, Singh K, et al. American Glaucoma Society Position Paper: microinvasive glaucoma surgery. Ophthalmol Glaucoma 2020; 3:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol 2002; 120:1268–1279. [DOI] [PubMed] [Google Scholar]
- 7.Lichter PR, Musch DC, Gillespie BW, et al. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology 2001; 108:1943–1953. [DOI] [PubMed] [Google Scholar]
- 8.Glaucoma Laser Trial Research Group. The Glaucoma Laser Trial (GLT) and Glaucoma Laser Trial Follow-Up Study: 7. Results. Am J Ophthalmol 1995; 120:718–731. [DOI] [PubMed] [Google Scholar]
- 9.Gazzard G, Konstantakopoulou E, Garway-Heath D, et al. LiGHT Trial Study Group. Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): a multicentre randomised controlled trial. Lancet 2019; 393:1505–1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.AGIS Study Group. The Advanced Glaucoma Intervention Study (AGIS): 4. Comparison of treatment outcomes within race. Seven-year results. Ophthalmology 1998; 105:1146–1164. [DOI] [PubMed] [Google Scholar]
- 11.Tsai JC. A comprehensive perspective on patient adherence to topical glaucoma therapy. Ophthalmology 2009; 116: (11 suppl): S30–536. [DOI] [PubMed] [Google Scholar]
- 12.Newman-Casey PA, Dayno M, Robin AL. Systematic review of educational interventions to improve glaucoma medication adherence: an update in 2015. Expert Rev Ophthalmol 2016; 11:5–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Newman-Casey PA, Robin AL, Blachley T, et al. The most common barriers to glaucoma medication adherence: a cross-sectional survey. Ophthalmology 2015; 122:1308–1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsai JC. Medication adherence in glaucoma: approaches for optimizing patient compliance. Curr Opin Ophthalmol 2006; 17:190–195. [DOI] [PubMed] [Google Scholar]
- 15.Nordstrom BL, Friedman DS, Mozaffari E, et al. Persistence and adherence with topical glaucoma therapy. Am J Ophthalmol 2005; 140:598–606. [DOI] [PubMed] [Google Scholar]
- 16.Newman-Casey PA, Blachley T, Lee PP, et al. Patterns of glaucoma medication adherence over four years of follow-up. Ophthalmology 2015; 122:2010–2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sleath B, Blalock S, Covert D, et al. The relationship between glaucoma medication adherence, eye drop technique, and visual field defect severity. Ophthalmology 2011; 118:2398–2402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newman-Casey PA, Niziol LM, Gillespie BW, et al. The association between medication adherence and visual field progression in the Collaborative Initial Glaucoma Treatment Study. Ophthalmology 2020; 127:477–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parrish RK, Palmberg P, Sheu WP. XLT Study Group. A comparison of latanoprost, bimatoprost, and travoprost in patients with elevated intraocular pressure: a 12-week, randomized, masked-evaluator multicenter study. Am J Ophthalmol 2003; 135:688–703. [DOI] [PubMed] [Google Scholar]
- 20.Tan J, Berke S. Latanoprost-induced prostaglandin-associated periorbitopathy. Optom Vis Sci 2013; 90:e245–e247. [DOI] [PubMed] [Google Scholar]
- 21.Rabinowitz MP, Katz LJ, Moster MR, et al. Unilateral prostaglandin-associated periorbitopathy: a syndrome involving upper eyelid retraction distinguishable from the aging sunken eyelid. Ophthal Plast Reconstr Surg 2015; 31:373–378. [DOI] [PubMed] [Google Scholar]
- 22.Zhang F, Liao S, Liu K, Duan XC. Prostaglandin-associated periorbitopathy. Zhonghua Yan Ke Za Zhi 2017; 53:637–640. [DOI] [PubMed] [Google Scholar]
- 23.Yip IYM, Ramasamy B. Unilateral orbital fat change. BMJ Case Rep 2018; 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mocan MC, Uzunosmanoglu E, Kocabeyoglu S, et al. The association of chronic topical prostaglandin analog use with meibomian gland dysfunction. J Glaucoma 2016; 25:770–774. [DOI] [PubMed] [Google Scholar]
- 25.Freeman PD, Kahook MY. Preservatives in topical ophthalmic medications: historical and clinical perspectives. Expert Rev Ophthalmol 2009; 4:59–64. [Google Scholar]
- 26.Broadway DC, Grierson I, O’Brien C, Hitchings RA. Adverse effects of topical antiglaucoma medication. II. The outcome of filtration surgery. Arch Ophthalmol 1994; 112:1446–1454. [DOI] [PubMed] [Google Scholar]
- 27.Baudouin C, Labbe A, Liang H, et al. Preservatives in eyedrops: the good, the bad and the ugly. Prog Retin Eye Res 2010; 29:312–334. [DOI] [PubMed] [Google Scholar]
- 28.Baudouin C. Side effects of antiglaucomatous drugs on the ocular surface. Curr Opin Ophthalmol 1996; 7:80–86. [DOI] [PubMed] [Google Scholar]
- 29▪.Goldstein MH, Silva FQ, Blender N, et al. Ocular benzalkonium chloride exposure: problems and solutions. Eye (Lond) 2022; 36:361–368. [DOI] [PMC free article] [PubMed] [Google Scholar]; The authors review the myriad consequences of chronic (and acute) exposure to the preservative BAK and offer solutions to reduce or avoid BAK exposure, including the use of therapies formulated with non-BAK preservatives, preservative-free formulations, sustained release drug delivery platforms, and nonpharmacological therapies.
- 30.Labbe A, Terry O, Brasnu E, et al. Tear film osmolarity in patients treated for glaucoma or ocular hypertension. Cornea 2012; 31:994–999. [DOI] [PubMed] [Google Scholar]
- 31.O’Hare F, Ghosh S, Lamoureux E, et al. Prevalence of signs and symptoms of ocular surface disease in individuals treated and not treated with glaucoma medication. Clin Exp Ophthalmol 2012; 40:675–681. [DOI] [PubMed] [Google Scholar]
- 32.Valente C, Iester M, Corsi E, Rolando M. Symptoms and signs of tear film dysfunction in glaucomatous patients. J Ocul Pharmacol Ther 2011; 27:281–285. [DOI] [PubMed] [Google Scholar]
- 33.Leung EW, Medeiros FA, Weinreb RN. Prevalence of ocular surface disease in glaucoma patients. J Glaucoma 2008; 17:350–355. [DOI] [PubMed] [Google Scholar]
- 34.Fechtner RD, Godfrey DG, Budenz D, et al. Prevalence of ocular surface complaints in patients with glaucoma using topical intraocular pressure-lowering medications. Cornea 2010; 29:618–621. [DOI] [PubMed] [Google Scholar]
- 35.Rossi GC, Pasinetti GM, Scudeller L, et al. Risk factors to develop ocular surface disease in treated glaucoma or ocular hypertension patients. Eur J Ophthalmol 2013; 23:296–302. [DOI] [PubMed] [Google Scholar]
- 36.Skalicky SE, Goldberg I, McCluskey P. Ocular surface disease and quality of life in patients with glaucoma. Am J Ophthalmol 2012; 53:1–9e2. [DOI] [PubMed] [Google Scholar]
- 37▪▪.Realini T, Shillingford-Ricketts H, Burt D, Balasubramani GK. Long-term outcomes of selective laser trabeculoplasty for open-angle glaucoma in the caribbean. Am J Ophthalmol 2021; 232:83–89. [DOI] [PMC free article] [PubMed] [Google Scholar]; In what may be the longest prospective study of SLT reported to date, more than 70% of Afro-Caribbean patients treated with SLT as primary or replacement therapy (and repeated as needed) for POAG remained medication-free after 94 months of follow-up. Given that people of African descent have the highest risk of glaucoma and glaucoma vision loss, SLT could be a powerful tool in the management of POAG in this population.
- 38.Katz LJ, Steinmann WC, Kabir A, et al. Selective laser trabeculoplasty versus medical therapy as initial treatment of glaucoma: a prospective, randomized trial. J Glaucoma 2012; 21:460–468. [DOI] [PubMed] [Google Scholar]
- 39.Wright DM, Konstantakopoulou E, Montesano G, et al. Laser in Glaucoma and Ocular Hypertension Trial (LiGHT) Study Group. Visual field outcomes from the multicenter, randomized controlled Laser in Glaucoma and Ocular Hypertension Trial (LiGHT). Ophthalmology 2020; 127:1313–1321. [DOI] [PubMed] [Google Scholar]
- 40.Bonafede L, Sanvicente CT, Hark LA, et al. Beliefs and attitudes of ophthalmologists regarding SLT as first line therapy for glaucoma. J Glaucoma 2020; 29:851–856. [DOI] [PubMed] [Google Scholar]
- 41▪▪.Realini T, Gazzard G, Latina M, Kass M. Low-energy selective laser trabeculoplasty repeated annually: rationale for the COAST Trial. J Glaucoma 2021; 30:545–551. [DOI] [PMC free article] [PubMed] [Google Scholar]; As an extension of the results of reference [37▪▪], the authors propose an evidence-based strategy for optimizing SLT delivery to maximize long-term medication-free IOP control. This strategy is the subject of an ongoing multicenter clinical trial supported by the US National Institutes of Health.
- 42.Migdal C, Gregory W, Hitchings R. Long-term functional outcome after early surgery compared with laser and medicine in open-angle glaucoma. Ophthalmology 1994; 101:1651–1656. [DOI] [PubMed] [Google Scholar]
- 43▪.Yang SA, Mitchell W, Hall N, et al. Trends and usage patterns of minimally invasive glaucoma surgery in the United States: IRIS(R) registry analysis 2013-2018. Ophthalmol Glaucoma 2021; 4:558–568. [DOI] [PubMed] [Google Scholar]; This database study from the IRIS registry illustrates the evolution of practice patterns for the management of glaucoma, with MIGS procedures becoming more common in recent years.
- 44▪.Rathi S, Andrews CA, Greenfield DS, Stein JD. Trends in glaucoma surgeries performed by glaucoma subspecialists versus nonsubspecialists on Medicare beneficiaries from 2008 through 2016. Ophthalmology 2021; 128:30–38. [DOI] [PMC free article] [PubMed] [Google Scholar]; As might be expected, procedures that require combination with cataract surgery are more commonly performed by comprehensive ophthalmologists, while standalone surgeries are more likely to be performed by glaucoma specialists.
- 45▪.Luebke J, Boehringer D, Anton A, et al. Trends in surgical glaucoma treatment in Germany between 2006 and 2018. Clin Epidemiol 2021; 13:581–592. [DOI] [PMC free article] [PubMed] [Google Scholar]; This database study demonstrated a reduction in the performance of trabeculectomy with a commensurate rise in performance of MIGS procedures in Germany.
- 46.Bron AM, Mariet AS, Benzenine E, et al. Trends in operating room-based glaucoma procedures in France from 2005 to 2014: a nationwide study. Br J Ophthalmol 2017; 101:1500–1504. [DOI] [PubMed] [Google Scholar]
- 47.Newman AR, Andrew NH. Changes in Australian practice patterns for glaucoma management. Clin Exp Ophthalmol 2019; 47:571–580. [DOI] [PubMed] [Google Scholar]
- 48.Iwasaki K, Arimura S, Takamura Y, Inatani M. Clinical practice preferences for glaucoma surgery in Japan: a survey of Japan Glaucoma Society specialists. Jpn J Ophthalmol 2020; 64:385–391. [DOI] [PubMed] [Google Scholar]
- 49.Rossi GC, Tinelli C, Pasinetti GM, et al. Dry eye syndrome-related quality of life in glaucoma patients. Eur J Ophthalmol 2009; 19:572–579. [DOI] [PubMed] [Google Scholar]
- 50.Rossi GC, Pasinetti GM, Scudeller L, Bianchi PE. Ocular surface disease and glaucoma: how to evaluate impact on quality of life. J Ocul Pharmacol Ther 2013; 29:390–394. [DOI] [PubMed] [Google Scholar]
- 51.Kumar S, Singh T, Ichhpujani P, et al. Correlation of ocular surface disease and quality of life in Indian glaucoma patients: BAC-preserved versus BAC-free travoprost. Turk J Ophthalmol 2020; 50:75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hommer A, Kimmich F. Switching patients from preserved prostaglandin-analog monotherapy to preservative-free tafluprost. Clin Ophthalmol 2011; 5:623–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schweitzer JA, Hauser WH, Ibach M, et al. Prospective interventional cohort study of ocular surface disease changes in eyes after trabecular micro-bypass stent(s) implantation (iStent or iStent inject) with phacoemulsification. Ophthalmol Ther 2020; 9:941–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120:701–713. [DOI] [PubMed] [Google Scholar]
- 55.Lam BL, Zheng DD, Davila EP, et al. Trends in glaucoma medication expenditure: Medical Expenditure Panel Survey 2001-2006. Arch Ophthalmol 2011; 129:1345–1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cui QN, Hays RD, Tarver ME, et al. Vision-targeted health-related quality-of-life survey for evaluating minimally invasive glaucoma surgery. Am J Ophthalmol 2021; 229:145–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Le JT, Viswanathan S, Tarver ME, et al. Assessment of the incorporation of patient-centric outcomes in studies of minimally invasive glaucoma surgical devices. JAMA Ophthalmol 2016; 134:1054–1056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Klink T, Sauer J, Korber NJ, et al. Quality of life following glaucoma surgery: canaloplasty versus trabeculectomy. Clin Ophthalmol 2015; 9:7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59▪▪.Samuelson TW, Singh IP, Williamson BK, et al. Quality of life in primary open-angle glaucoma and cataract: an analysis of VFQ-25 and OSDI from the iStent inject pivotal trial. Am J Ophthalmol 2021; 229:220–229. [DOI] [PubMed] [Google Scholar]; This post hoc analysis of data from the iStent Inject pivotal trial demonstrated that combined cataract surgery and MIGS resulted in greater reductions in the medication burden and greater improvement in QoL than cataract surgery alone.
- 60.Liu JH, Medeiros FA, Slight JR, Weinreb RN. Comparing diurnal and nocturnal effects of brinzolamide and timolol on intraocular pressure in patients receiving latanoprost monotherapy. Ophthalmology 2009; 116:449–454. [DOI] [PubMed] [Google Scholar]
- 61.Liu JH, Kripke DF, Weinreb RN. Comparison of the nocturnal effects of once-daily timolol and latanoprost on intraocular pressure. Am J Ophthalmol 2004; 138:389–395. [DOI] [PubMed] [Google Scholar]
- 62▪.Pyfer MF, Gallardo M, Flowers BE, et al. Suppression of diurnal (8am-4pm) IOP fluctuations with minimally invasive glaucoma surgery: an analysis of data from the prospective, multicenter, single-arm GEMINI Study. Clin Ophthalmol 2021; 15:3931–3938. [DOI] [PMC free article] [PubMed] [Google Scholar]; This post hoc analysis of data from a prospective study demonstrated that MIGS (combined trabeculotomy and viscocanaloplasty in this case) reduced diurnal IOP fluctuations significantly over time.
- 63▪▪.Ahmed IIK, Rhee DJ, Jones J, et al. HORIZON Investigators. Three-year findings of the HORIZON Trial: a Schlemm canal microstent for pressure reduction in primary open-angle glaucoma and cataract. Ophthalmology 2021; 128:857–865. [DOI] [PubMed] [Google Scholar]; This pivotal trial with 3-year follow-up characterized the long-tern efficacy and safety of the Schlemm canal microstent, reporting 73% surgical success with combined surgery versus 48% for phacoemulsification alone.
- 64.Saheb H, Ahmed II. Micro-invasive glaucoma surgery: current perspectives and future directions. Curr Opin Ophthalmol 2012; 23:96–104. [DOI] [PubMed] [Google Scholar]
- 65.Ianchulev T, Litoff D, Ellinger D, et al. Office-based cataract surgery: population health outcomes study of more than 21 000 cases in the United States. Ophthalmology 2016; 123:723–728. [DOI] [PubMed] [Google Scholar]
- 66. iData Research. Available at: https://idataresearch.com/over-3-8-million-cataract-surgeries-performed-every-year/. [Accessed 17 October 2020] [Google Scholar]
- 67.Grover DS, Godfrey DG, Smith O, et al. Gonioscopy-assisted transluminal trabeculotomy, ab interno trabeculotomy: technique report and preliminary results. Ophthalmology 2014; 121:855–861. [DOI] [PubMed] [Google Scholar]
- 68.Rahmatnejad K, Pruzan NL, Amanullah S, et al. Surgical outcomes of gonioscopy-assisted transluminal trabeculotomy (GATT) in patients with open-angle glaucoma. J Glaucoma 2017; 26:1137–1143. [DOI] [PubMed] [Google Scholar]
- 69.Grover DS, Smith O, Fellman RL, et al. Gonioscopy-assisted transluminal trabeculotomy: an ab interno circumferential trabeculotomy: 24 months follow-up. J Glaucoma 2018; 27:393–401. [DOI] [PubMed] [Google Scholar]
- 70.Aktas Z, Ozmen MC, Atalay HT, Ucgul AY. Evaluation of episcleral venous fluid wave during gonioscopy assisted transluminal trabeculotomy in patients with advanced glaucoma. Eye (Lond) 2019; 33:668–673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Parikh DA, Mellen PL, Kang T, et al. Gonioscopy-assisted transluminal trabeculotomy for the treatment of glaucoma in uveitic eyes. Ocul Immunol Inflamm 2022; 1–7. [DOI] [PubMed] [Google Scholar]
- 72.Vez S, Muller L, Bochmann F. Surgical outcomes of gonioscopy-assisted transluminal trabeculotomy (GATT) in patients with open-angle glaucoma - a retrospective case series. Klin Monbl Augenheilkd 2021; 238:391–395. [DOI] [PubMed] [Google Scholar]
- 73.Aktas Z, Ucgul AY, Ozdek S, Boluk CE. Outcomes of gonioscopy-assisted transluminal trabeculotomy in vitrectomized patients with secondary glaucoma after silicone oil removal. J Glaucoma 2021; 30:e114–e118. [DOI] [PubMed] [Google Scholar]
- 74▪.Fontana L, De Maria M, Caristia A, et al. Comparison of gonioscopy-assisted transluminal trabeculotomy versus trabeculectomy with mitomycin C in patients with open-angle glaucoma. J Glaucoma 2021; 30:101–108. [DOI] [PubMed] [Google Scholar]; This retrospective cohort study demonstrated greater IOP reductions with trabeculectomy over GATT but comparable reductions in medication burden between groups.
- 75▪.Smith OU, Butler MR, Grover DS, et al. Twenty-four-month outcome of gonioscopy-assisted transluminal trabeculotomy (GATT) in eyes with prior corneal transplant surgery. J Glaucoma 2022; 31:54–59. [DOI] [PubMed] [Google Scholar]; This retrospective analysis reported substantial reductions in both IOP and medication use after GATT in hard-to-manage eyes with secondary open-angle glaucoma arising from prior corneal transplant surgery.
- 76.Grover DS, Godfrey DG, Smith O, et al. Outcomes of gonioscopy-assisted transluminal trabeculotomy (GATT) in eyes with prior incisional glaucoma surgery. J Glaucoma 2017; 26:41–45. [DOI] [PubMed] [Google Scholar]
- 77▪.Faria BM, Daga FB, Reboucas-Santos V, et al. Gonioscopy-assisted transluminal trabeculotomy (GATT) outcomes in eyes with open-angle glaucoma resistant to maximum treatment. Arq Bras Oftalmol 2021; 84:587–593. [DOI] [PubMed] [Google Scholar]; This retrospective study reported that GATT reduced both IOP and the need for medications in eyes with OAG that were incompletely controlled using maximal tolerated medical therapy (3+ medications).
- 78.Sarkisian S, Allan EJ, Ding K. New way for ab interno trabeculotomy: initial results. American Society of Cataract and Refractive Surgery Annual Meeting San Diego, CA. 2015. [Google Scholar]
- 79.Sarkisian SR, Mathews B, Ding K, et al. 360 degrees ab-interno trabeculotomy in refractory primary open-angle glaucoma. Clin Ophthalmol 2019; 13:161–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Minckler DS, Baerveldt G, Alfaro MR, Francis BA. Clinical results with the Trabectome for treatment of open-angle glaucoma. Ophthalmology 2005; 112:962–967. [DOI] [PubMed] [Google Scholar]
- 81.Kaplowitz K, Bussel II, Honkanen R, et al. Review and meta-analysis of ab-interno trabeculectomy outcomes. Br J Ophthalmol 2016; 100:594–600. [DOI] [PubMed] [Google Scholar]
- 82.Ting JL, Damji KF, Stiles MC. Trabectome Study Group. Ab interno trabeculectomy: outcomes in exfoliation versus primary open-angle glaucoma. J Cataract Refract Surg 2012; 38:315–323. [DOI] [PubMed] [Google Scholar]
- 83.Maeda M, Watanabe M, Ichikawa K. Evaluation of trabectome in open-angle glaucoma. J Glaucoma 2013; 22:205–208. [DOI] [PubMed] [Google Scholar]
- 84.Ahuja Y, Ma Khin Pyi S, Malihi M, et al. Clinical results of ab interno trabeculotomy using the Trabectome for open-angle glaucoma: the Mayo Clinic series in Rochester, Minnesota. Am J Ophthalmol 2013; 156:927.e2–935.e2. [DOI] [PubMed] [Google Scholar]
- 85.Minckler D, Mosaed S, Dustin L, Ms BF. Trabectome Study Group. Trabectome (trabeculectomy-internal approach): additional experience and extended follow-up. Trans Am Ophthalmol Soc 2008; 106:149–159. [PMC free article] [PubMed] [Google Scholar]
- 86.Mosaed S. The first decade of global Trabectome outcomes. Eur Ophthal Rev 2014; 8:113–119. [Google Scholar]
- 87.Seibold LK, Soohoo JR, Ammar DA, Kahook MY. Preclinical investigation of ab interno trabeculectomy using a novel dual-blade device. Am J Ophthalmol 2013; 155:524.e2–529.e2. [DOI] [PubMed] [Google Scholar]
- 88.Salinas L, Chaudhary A, Berdahl JP, et al. Goniotomy using the Kahook Dual Blade in severe and refractory glaucoma: 6-month outcomes. J Glaucoma 2018; 27:849–855. [DOI] [PubMed] [Google Scholar]
- 89.Berdahl JP, Gallardo MJ, ElMallah MK, et al. Six-month outcomes of goniotomy performed with the Kahook Dual Blade as a stand-alone glaucoma procedure. Adv Ther 2018; 35:2093–2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.ElMallah MK, Berdahl JP, Williamson BK, et al. Twelve-month outcomes of stand-alone excisional goniotomy in mild to severe glaucoma. Clin Ophthalmol 2020; 14:1891–1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sieck EG, Epstein RS, Kennedy JB, et al. Outcomes of Kahook Dual Blade goniotomy with and without phacoemulsification cataract extraction. Ophthalmology Glaucoma 2018; 1:75–81. [DOI] [PubMed] [Google Scholar]
- 92▪.Arnljots TS, Economou MA. Kahook Dual Blade goniotomy vs iStent inject: long-term results in patients with open-angle glaucoma. Clin Ophthalmol 2021; 15:541–550. [DOI] [PMC free article] [PubMed] [Google Scholar]; With approximately 2 years of mean follow-up, eyes in this retrospective analysis, both procedures lowered IOP well in combination with cataract surgery, but only goniotomy (and not iStent) lowered IOP as a standalone procedure.
- 93.Lewis RA, von Wolff K, Tetz M, et al. Canaloplasty: circumferential viscodilation and tensioning of Schlemm's canal using a flexible microcatheter for the treatment of open-angle glaucoma in adults Interim clinical study analysis. J Cataract Refract Surg 2007; 33:1217–1226. [DOI] [PubMed] [Google Scholar]
- 94.Gallardo MJ, Supnet RA, Ahmed IIK. Viscodilation of Schlemm's canal for the reduction of IOP via an ab-interno approach. Clin Ophthalmol 2018; 12:2149–2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Gillmann K, Aref A, Niegowski LJ, Baumgartner JM. Combined ab interno viscocanaloplasty (ABiC) in open-angle glaucoma: 12-month outcomes. Int Ophthalmol 2021; 41:3295–3301. [DOI] [PubMed] [Google Scholar]
- 96.Gallardo MJ, Supnet RA, Ahmed IIK. Circumferential viscodilation of Schlemm's canal for open-angle glaucoma: ab-interno vs ab-externo canaloplasty with tensioning suture. Clin Ophthalmol 2018; 12:2493–2498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ondrejka S, Korber N. 360 degrees ab-interno Schlemm's canal viscodilation in primary open-angle glaucoma. Clin Ophthalmol 2019; 13:1235–1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hughes T, Traynor M. Clinical results of ab interno canaloplasty in patients with open-angle glaucoma. Clin Ophthalmol 2020; 14:3641–3650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Dickerson JE, Dhamdhere K. Combined circumferential canaloplasty and trabeculotomy ab interno with the OMNI Surgical System. Front Ophthalmol 2021; 1:106–115. [Google Scholar]
- 100.Grabska-Liberek I, Duda P, Rogowska M, et al. 12-month interim results of a prospective study of patients with mild to moderate open-angle glaucoma undergoing combined viscodilation of Schlemm's canal and collector channels and 360 degrees trabeculotomy as a standalone procedure or combined with cataract surgery. Eur J Ophthalmol 2022; 32:309–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Klabe K, Kaymak H. Standalone trabeculotomy and viscodilation of Schlemm's Canal and collector channels in open-angle glaucoma using the OMNI Surgical System: 24-month outcomes. Clin Ophthalmol 2021; 15:3121–3129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Toneatto G, Zeppieri M, Papa V, et al. 360 degrees ab-interno Schlemm's canal viscodilation with OMNI viscosurgical systems for open-angle glaucoma-midterm results. J Clin Med 2022; 11:259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103▪.Vold SD, Williamson BK, Hirsch L, et al. Canaloplasty and trabeculotomy with the OMNI System in pseudophakic patients with open-angle glaucoma: the ROMEO study. Ophthalmol Glaucoma 2021; 4:173–181. [DOI] [PubMed] [Google Scholar]; In this multicenter retrospective analysis, pseudophakic eyes undergoing standalone canaloplasty and trabeculotomy achieved significant reductions in IOP and/or medication use stratified by baseline IOP.
- 104▪▪.Healey PR, Clement CI, Kerr NM, et al. Standalone iStent trabecular micro-bypass glaucoma surgery: a systematic review and meta-analysis. J Glaucoma 2021; 30:606–620. [DOI] [PubMed] [Google Scholar]; Given little data on standalone iStent use, this meta-analysis provides the best evidence to date on its use when not combined with cataract surgery.
- 105.Ahmed IIK, Fea A, Au L, et al. COMPARE Investigators. A prospective randomized trial comparing Hydrus and iStent microinvasive glaucoma surgery implants for standalone treatment of open-angle glaucoma: the COMPARE study. Ophthalmology 2020; 127:52–61. [DOI] [PubMed] [Google Scholar]
- 106.Fea AM, Ahmed II, Lavia C, et al. Hydrus microstent compared to selective laser trabeculoplasty in primary open angle glaucoma: one year results. Clin Exp Ophthalmol 2017; 45:120–127. [DOI] [PubMed] [Google Scholar]