Abstract
Inherent to the cancer disease trajectory are heightened risks for a plethora of comorbid diagnoses. As the treatment landscape for oncology therapeutics continues to rapidly advance, patients are living longer and potentially experiencing more symptoms requiring rapid assessment. Prompt assessment and intervention for cancer or cancer treatment-related symptoms is imperative to achieve patient comfort and obtain the best overall patient outcomes. Traditionally, these patients were frequently referred to the emergency department (ED) when same-day clinic appointments were not obtainable. In order to decrease ED utilization and provide same-day urgent care for oncology patients, the Abramson Cancer Center established an advanced practice provider–led Oncology Evaluation Center where cancer patients are able to receive same-day assessment, symptom relief, and ultimately prevent unnecessary ED visits.
There was an estimated 1.9 million cancer cases diagnosed and 609,360 cancer-related deaths in 2022 in the United States (American Cancer Society, 2022). Cancer treatment advances have expanded through the years to more complex regimens and novel therapies with diverse mechanisms of action and unique side-effect profiles. These advances have resulted in people with cancer living longer. The trends in 5-year relative survival for all types of cancer have increased from 49% in 1975 to 67% in 2016 (National Cancer Institute, 2017).
Throughout the cancer treatment trajectory, patients continue to seek emergent care outside the practices of their primary oncology teams. Patients with cancer account for more than 4.5 million emergency department (ED) visits annually. This value is likely underestimated as data gathered were based on ED diagnostic codes as opposed to oncology diagnostic codes (Rui et al., 2015; Rivera et al., 2017). Several studies suggest that lung cancer, non-colorectal gastrointestinal cancer, and breast cancer account for the most frequent oncology diagnoses seen in the ED (Barbera et al., 2010; Bozdemir et al., 2009; Mayer et al., 2011; McKenzie et al., 2010; Sivendran et al., 2016).
ONCOLOGY CARE AND THE ED LANDSCAPE
The role of emergency medicine in the care of oncology patients has typically been to address febrile neutropenia, thrombosis, tumor lysis syndrome, or hypercalcemia, among other cancer- or cancer treatment–related symptoms (Caterino et al., 2019). Symptom-driven complaints such as pain, dyspnea, nausea, and constipation are typically the most common issues for cancer patients presenting to the ED (Caterino et al., 2019). There are multiple studies that have captured the most prevalent reasons patients with cancer have visited the ED. Hsu and colleagues (2018) performed a data analysis evaluating the common oncology-related symptoms of patients who sought ED care utilizing the National Hospital Ambulatory Medical Care Survey (NHAMCS). The NHAMCS is a national probability sample of outpatient and ED visits across the United States and is managed by the National Center for Health Statistics (NCHS). A review of the NHAMCS data from 2012 through 2014 identified the chief complaints for oncology patients included nausea, vomiting, shortness of breath, and chest pain (Hsu et al., 2018). These symptom reports parallel findings from several other studies. Additional chief complaints from cancer patients visiting the ED include abdominal pain, dyspnea, malaise, and fever (Barbera et al., 2010; Bozdemir et al., 2009; Mayer et al., 2011; McKenzie et al., 2010).
Overcrowding of EDs across the country inflict prolonged wait times for patients when many are at their most vulnerable. For the immunocompromised oncology patient, the potential exposures in this environment can be medically altering. Data from the Centers for Medicare and Medicaid Services reported in 2016 that median ED wait times had wide variability across states, ranging from a 14-minute wait time in Colorado to a 143-minute wait time in Georgia (Groeger et al., 2019).
In many circumstances, a viable alternative to ED visits by oncology patients is evaluation through an urgent care center (UCC). The establishment of UCCs has been shown to decrease ED visits to upwards of 48% (Corwin et al, 2016). Advanced practice providers (APPs) in oncology have an established skill set to provide a comprehensive assessment, establishment of differential diagnosis, confirmation of diagnosis, and management. As such, we believe that APPs utilized in an oncology care UCC are the ideal provider to meet the patient's needs while minimizing ED visits and/or admissions to the hospital. This article demonstrates this hypothesis through a clinical case review and descriptive analysis of patients seen over 4 years at one oncology APP-led UCC.
ED-ONCOLOGY CLINICAL SCENARIO
JM is a 64-year-old man with stage IV non–small cell lung cancer (NSCLC). He called his medical oncologist's office on a Tuesday afternoon at 1:00 pm. He spoke with the triage nurse reporting that for the past 24 to 48 hours he developed worsening shortness of breath and a dry cough. He denied fever, chest pain, and hemoptysis. He stated that his breathing was worse with exertion. The triage nurse provided this assessment to his primary oncology provider who recommended that JM present to the ED for evaluation.
Upon arrival to the ED at 3:00 pm, JM's vital signs were a blood pressure of 108/65 mmHg, heart rate of 99 beats per minute, pulse oximetry on room air of 96%, temperature of 98.8°F, and respiratory rate of 20 breaths per minute. He was taken back for evaluation by the ED physician within 3 hours. Following assessment, he had blood work drawn and CT imaging of the chest with contrast pulmonary embolus protocol completed. The CT scan results confirmed pulmonary embolism.
JM was admitted to the ED observation unit for monitoring and initiation of anticoagulation therapy. He was discharged in less than 48 hours on low-molecular-weight heparin (LMWH).
CONCEPTION OF THE ONCOLOGY EVALUATION CENTER
Clinical cases like JM's raises the question of whether there is a safe and effective way to diagnose and treat oncology-related symptoms without utilizing the ED. The Abramson Cancer Center (ACC) at the Hospital of the University of Pennsylvania (HUP) realized the unmet urgent care needs of oncology patients were due to a variety of variables including, but not limited to, consistent overcrowding of the ED. The APPs and their collaborating physicians are well equipped to triage, evaluate, and treat cancer or cancer-treatment related symptoms on an outpatient basis. However, their clinic schedule is typically at capacity and limits the ability to accommodate same-day symptom management appointments. Additionally, if treatment assessment and intervention required urgent radiology imaging or infusion services, these departments are generally booked and unable to accept add-on requests.
Given these challenges, a small task force was developed consisting of outpatient oncology APPs, physicians, and administrators from the cancer service line to determine if it was feasible to establish a same-day urgent care in the outpatient setting. The initial goals for the UCC were to: (1) decrease overall hospital admissions, (2) decrease the number of patients sent to the ED from home without any outpatient evaluation, (3) increase the number of direct admissions from clinic as opposed to ED visits, and (4) increase the number of outpatient APP visits and infusion visits. The proposed logistics included having clinic space in or adjacent to the infusion area, designated rooms for infusion, clinic hours extending until 7:00 pm, and streamlined access to radiology.
Initially, there were five diagnoses recognized by the task force that were ideal for assessment and management in the UCC: (1) pulmonary embolism, (2) febrile neutropenia, (3) uncomplicated dehydration, (4) uncomplicated shortness of breath, and (5) pain management. These were chosen based on the chief complaints of patients who were previously referred to the ED and ultimately diagnosed, treated, and discharged in less than 24 hours.
To substantiate evaluation of patients with symptoms of shortness of breath and fever, evidence-based clinical guidelines were presented to the task force supporting outpatient management for pulmonary embolism and febrile neutropenia. Stratification tools for the management of PE, including the Pulmonary Embolism Severity Index and the Hestia criteria were reviewed (Aujesky et al., 2005; Aujesky et al., 2011; Lankett et al., 2012; Lee & Levine, 2003). Both models used a points or leveling system to classify the level of risk from a pulmonary embolism to determine if anticoagulation therapy could safely be initiated in the out-patient setting. Other factors impacting the initiation of outpatient anticoagulation included: (1) insurance readily approving medications (such as LMWH), (2) patient or caregiver ability to administer the medication, and (3) nearby availability of a tertiary care center if their respiratory status deteriorated. Risk scoring models such as the Talcott score and the Multidisciplinary Association of Supportive Care in Cancer (MASCC) score are reliable tools to assess the risk for complication due to febrile neutropenia. If patients were considered low risk, they could potentially be managed out-patient with oral antibiotic therapy (Klastersky et al., 2000, 2006).
There were a multitude of administrative considerations to address in order to establish a UCC, including proper billing, location space, staff allotment, and collaboration with radiology leadership to prioritize urgent diagnostic imaging tests such as ultrasounds, CT, and Doppler studies. Once these administrative concerns were situated and logistics secured a UCC, the Oncology Evaluation Center (OEC), was opened in November 2016 at the ACC at HUP. The goal of the OEC is to streamline care in an efficacious and real-time manner while decreasing ED visits by oncology patients.
OEC OVERVIEW
The OEC staff is comprised of two APPs, two registered nurses (RNs), an oncology pharmacist, and a certified nursing assistant (CNA) who also functions in a scheduling capacity. The APPs in the OEC have an expansive collaborative agreement that includes all of the practicing physicians within medical oncology in the ACC. The OEC provides urgent, same-day appointments for established ACC oncology patients who experience new or uncontrolled symptoms related to their cancer or cancer treatments. Symptoms addressed include but are not limited to, nausea, vomiting, constipation, diarrhea, dehydration, pain, neutropenic fever, other infections, acute deep vein thrombosis, pulmonary embolism, hypercalcemia of malignancy, and acute kidney injury. There are six dedicated infusion chairs in the OEC for administration of hydration, blood products, antibiotics, antiemetics, pain medications, and more as needed.
METHOD OF REFERRAL TO OEC
Patients are referred to the OEC by their primary oncology team after triage to determine eligibility. To be seen in the OEC, the patient must have an oncology diagnosis being managed by a medical oncologist from the ACC. Patients are not eligible for the OEC if they exhibit life-threatening symptoms, have severe mental status changes, have significant bleeding, or are suffering from head trauma or marked respiratory distress. The OEC APP will review the referral for appropriateness. The patient will then receive a phone call from the OEC scheduler to schedule an appointment.
Upon arrival, the patient is evaluated by the APP in the designated clinic space. Based on this assessment, the patient's plan could include laboratory work, radiographic imaging, or infusion services, as indicated. There are three potential dispositions from the OEC, which are to home, ED, or a direct admission to HUP. The determination of a patient being transferred to the ED as opposed to direct admission is contingent on the patient's status and hospital bed capacity.
OEC UTILIZATION
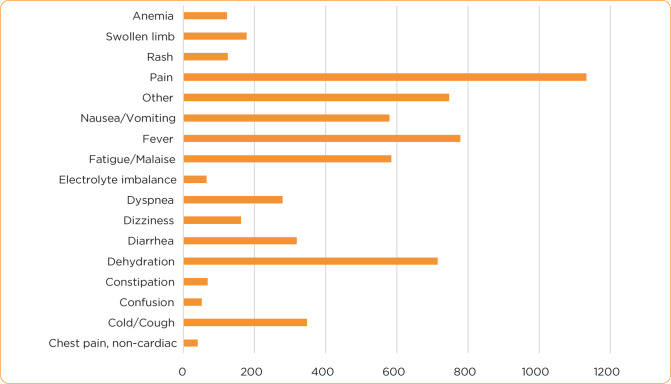
Since the OEC's inception, data have been collected on utilization, diagnosis, chief complaints, and dispositions. From November 2016 through November 2020, a total of 4,474 patients have been evaluated. Of these patients, 81% (n = 3,642) were discharged to home while only 15% (n = 665) were sent to the emergency department and 4% (n = 167) were directly admitted to the hospital (Figure 1). The most common chief complaints requiring assessment in the OEC are chest pain (non-cardiac), cough, mild confusion, constipation, dehydration, diarrhea, dyspnea, electrolyte imbalance, fatigue, fever, nausea or vomiting, pain, rash, swollen limb, and anemia (Figure 2). The three symptoms most frequently evaluated are pain, fever, and dehydration. Patients with hematologic malignancies were the predominant referrals to the OEC, followed by gastrointestinal and thoracic oncology diagnoses (Figure 3). Next, we will revisit the case of JM after the establishment of the OEC to highlight the benefits of the OEC in contrast to JM's ED visit described previously.
Figure 1.

Oncology Evaluation Center patient dispositions.
Figure 2.
Oncology Evaluation Center chief complaints.
Figure 3.
Disease-specific utilization of the Oncology Evaluation Center.
OEC CLINICAL SCENARIO
JM called his medical oncologist's office on a Tuesday afternoon at 1:00 pm. He spoke with the triage nurse reporting that for the past 24 to 48 hours he developed worsening shortness of breath and a dry cough. He denied fever, chest pain, or hemoptysis. He stated that his breathing is worse with exertion. The triage nurse provided this assessment to his primary oncology provider who recommended that JM be evaluated in the OEC.
Once referred to the OEC, the OEC APP reviewed his chart and requested that JM be scheduled for evaluation. The OEC medical assistant called JM and scheduled his appointment for 3:00 pm. Upon arrival to the OEC, JM's vital signs were a blood pressure of 108/65 mmHg, heart rate of 99 beats per minute, pulse oximetry on room air of 96%, temperature of 98.8°F, and respiratory rate of 20 breaths per minute. The APP completed a review of systems, updated medical history, and physical assessment. The APP ordered stat labs and a stat CT chest with contrast pulmonary embolus protocol to assess for the differential diagnoses of pneumonia, pulmonary embolism, pleural effusion, pneumonitis from treatment, or a chronic obstructive pulmonary disease flare. The APP receives a call from the reading radiologist to discusses the imaging findings of pulmonary embolism.
Based on JM's clinical assessment findings of low-risk Hestia scoring, unremarkable lab results, and stable vital signs and reliability, the APP concluded that JM did not require admission and prescribed LMWH. The OEC registered nurse educated JM on subcutaneous injection, and he demonstrated appropriate technique with the first dose administration. The APP confirmed with the outpatient hospital pharmacy that JM's insurance covered the LMWH and the co-pay was acceptable. JM was given written discharge instructions on the new medication, risks of bleeding, what to do if his condition worsens, and when to schedule a follow-up appointment with his primary oncology provider. JM verbalized understanding of his plan and was discharged home.
SENTINEL ADVANCEMENTS
A foundational goal of the OEC was achieved based on 81% of patients being discharged home. To build on this success, a partnership with the ED and their observation unit (OU) was developed for OEC patients, with completed medical evaluation and diagnosis, requiring a less than 48-hour stay.
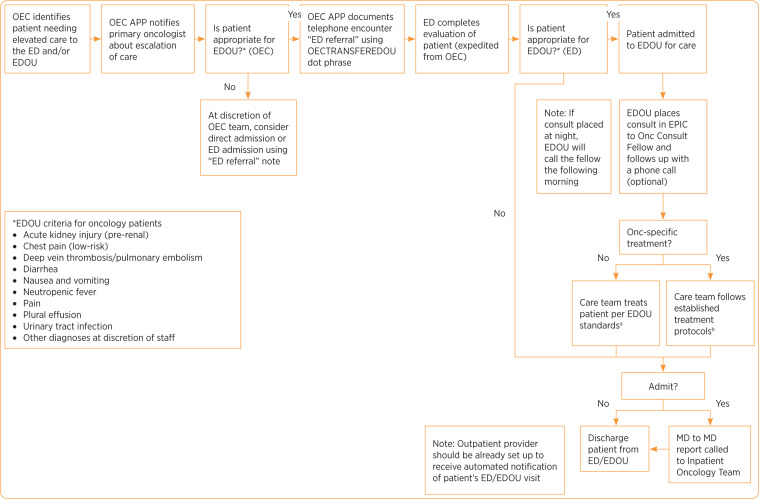
In 2018, a phase I oncology-EDOU partner-ship was operationalized. Criteria for referral to the EDOU from the OEC were established to include only solid tumor oncology patients. Diagnoses to be considered for admission to the EDOU included cancer-associated pain, deep vein thrombosis or pulmonary embolism, uncontrolled nausea or vomiting, neutropenic fever, diarrhea, acute kidney injury, pleural effusions, low-risk chest pain, and urinary tract infection. The referral process for the EDOU is initiated by the OEC APP once a confirmatory diagnosis is determined. The OEC APP will call the EDOU APP to confirm appropriateness and availability. Collaboratively, the providers will establish a treatment plan and transfer the patient to the ED. Once an ED provider performs a preliminary clinical review, the patient is then transitioned to the EDOU. An algorithm for this process was developed and is comprehensively summarized in Figure 4. From July 2018 through December 2019, 32 patients had successfully transitioned from the OEC to the EDOU. The start of the COVID-19 pandemic in January 2020 has unfortunately necessitated that this program be placed on hold.
Figure 4.
Emergency Department Observation Unit Pathway for Oncology Patients. Algorithm developed by Erin Lightheart, MBA, CSSBB, PNP, and Abbey C. Walsh, MSN, RN, OCN. OEC = Oncology Evaluation Center; ED = emergency department; EDOU = emergency department observation unit; APP = advanced practice provider
aAKI (pre-renal), chest pain (low-risk), pleural effusion, urinary tract infection, and other at discretion of staff.
bFever, pain, diarrhea, nausea and vomiting, and DVT/PE.
Patients with sickle cell disease are a population of benign hematology that have been under-served by the medical community (Lanzkron et al., 2021). Historically, pain management of vasoocclusive crisis has been a challenge for healthcare providers. In April 2018, the OEC collaborated with the benign hematologists to establish a pathway for early onset outpatient pain management to decrease ED visits and increase patient satisfaction. The same-day appointment availability within the OEC enables prompt establishment of symptomatic care. Pain plans are individualized and are developed with input from a multidisciplinary team, including the patient's primary hematology providers, clinical pharmacist, and the OEC APP.
Influenced by the successful accomplishments of the OEC, other disease teams were motivated to establish a similar framework to address high-risk, non-oncology ambulatory patients who require urgent, same-day evaluations. Examples of these patient populations include but are not limited to solid organ transplant, cardiology, pulmonology, renal, and endocrinology. An APP-led symptom management service (SMS) clinic was developed in March 2019. The OEC shares their clinical and infusion space with SMS providers.
FUTURE DIRECTIONS
The opening of the OEC has served as a catalyst for the development of new programs to address unmet needs of diverse patient groups. Moving forward, consideration of extended hours, week-end referrals, and incorporation of patient satisfaction surveys to further advance quality care are being considered.
CONCLUSIONS
The ACC at HUP is a National Cancer Institute–designated cancer center that sees over 500 patients a day. As a result, many oncology patients are sent to the ED due to the inability to schedule same-day appointments with their primary medical oncologists or APP providers. In 2016, the ACC established the OEC to provide same-day urgent evaluations. In the past 5 years, 4,474 patients have been evaluated in the OEC. We identified pain, fever, and dehydration as the three presenting symptoms most frequently evaluated in the OEC. Interestingly, this contradicts the literature citing pain, dyspnea, nausea, and constipation as the most common chief complaints presenting to the ED. Of these patients, 3,642 were discharged to home. The OEC data capture a 4% direct admission disposition. We recognize this low percentage relates to patients' stability and/or inpatient bed availability. These factors likely contributed to the 15% transferred to the ED. Based on these results, we believe that the availability of an APP-run OEC significantly decreases ED visits by oncology patients. Furthermore, the OEC pilot was established as a standard of care at ACC, has expanded its patients served, and has been used as a model for other APP-led UCCs.
Footnotes
The authors have no conflicts of interest to disclose.
References
- American Cancer Society. (2022). Cancer Facts and Figures 2022. https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2022.html
- Aujesky, D., Obrosky, D. S., Stone, R. A., Auble, T. E., Perrier, A., Cornuz, J.,…Fine, M. J. (2005). Derivation and validation of a prognostic model for pulmonary embolism. American Journal of Respiratory and Critical Care Medicine, 172(8), 1041–1046. 10.1164/rccm.200506-862oc [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aujesky, D., Roy, P.-M., Verschuren, F., Righini, M., Oster-walder, J., Egloff, M.,…Yealy, D. M. (2011). Outpatient versus inpatient treatment for patients with acute pulmonary embolism: An international, open-label, randomised, non-inferiority trial. Lancet, 378(9785), 41–48. 10.1016/s0140-6736(11)60824-6 [DOI] [PubMed] [Google Scholar]
- Barbera, L., Taylor, C., & Dudgeon, D. (2010). Why do patients with cancer visit the emergency department near the end of life? Canadian Medical Association Journal, 182(6), 563–568. 10.1503/cmaj.091187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bozdemir, N., Eray, O., Eken, C., Senol, Y., Artac, M. & Samur, M. (2009). Demographics, clinical presentations and outcomes of cancer patients admitted to the emergency department. Turkish Journal of Medical Sciences, 39(2), 235–240. [Google Scholar]
- Caterino, J. M., Adler, D., Durham, D. D., Yeung, S.-C. J., Hudson, M. F., Bastani, A.,…Venkat, A. (2019). Analysis of diagnoses, symptoms, medications, and admissions among patients with cancer presenting to emergency departments. JAMA Network Open, 2(3), e190979. 10.1001/jamanetworkopen.2019.0979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corwin, G., Parker, D., & Brown, J. (2016). Site of treatment for non-urgent conditions by Medicare beneficiaries: Is there a role for urgent care centers? The American Journal of Medicine, 129(9), 966–973. 10.1016/j.amjmed.2016.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groeger, L., Tigas, M., & Wei, S. (2019). ER Inspector. Pro-Publica. https://projects.propublica.org/emergency/.
- Hsu, J., Donnelly, J. P., Moore, J. X., Meneses, K., Williams, G., & Wang, H. E. (2018). National characteristics of emergency department visits by patients with cancer in the United States. The American Journal of Emergency Medicine, 36(11), 2038–2043. 10.1016/j.ajem.2018.03.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klastersky, J., Paesmans, M., Georgala, A., Muanza, F., Plehiers, B., Dubreucq, L.,…Barette, M. (2006). Outpatient oral antibiotics for febrile neutropenic cancer patients using a score predictive for complications. Journal of Clinical Oncology, 24(25), 4129–4134. 10.1200/jco.2005.03.9909 [DOI] [PubMed] [Google Scholar]
- Klastersky, J., Paesmans, M., Rubenstein, E. B., Boyer, M., Elting, L., Feld, R.,…Talcott, J. (2000). The Multinational Association for Supportive Care in Cancer Risk Index: A Multinational Scoring System for Identifying Low-Risk Febrile Neutropenic Cancer Patients. Journal of Clinical Oncology, 18(16), 3038–3051. 10.1200/jco.2000.18.16.3038 [DOI] [PubMed] [Google Scholar]
- Lankeit, M., Gómez, V., Wagner, C., Aujesky, D., Recio, M., Briongos, S.,…Jiménez, D. (2012). A strategy combining imaging and laboratory biomarkers in comparison with a simplified clinical score for risk stratification of patients with acute pulmonary embolism. Chest, 141(4), 916–922. 10.1378/chest.11-1355 [DOI] [PubMed] [Google Scholar]
- Lanzkron, S., Little, J., Wang, H., Field, J. J., Shows, J. R., Haywood, C.,…Abu Al Hamayel, N. (2021). Treatment of acute pain in adults with sickle cell disease in an infusion center versus the emergency department. Annals of Internal Medicine, 174(9), 1207–1213. 10.7326/m20-7171 [DOI] [PubMed] [Google Scholar]
- Lee, A. Y. Y., & Levine, M. N. (2003). Venous thromboembolism and cancer: Risks and outcomes. Circulation, 107(23_suppl_1). 10.1161/01.cir.0000078466.72504.ac [DOI] [PubMed] [Google Scholar]
- Mayer, D. K., Travers, D., Wyss, A., Leak, A., & Waller, A. (2011). Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. Journal of Clinical Oncology, 29(19), 2683–2688. 10.1200/jco.2010.34.2816 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie, H., Hayes, L., White, K., Cox, K., Fethney, J., Boughton, M., & Dunn, J. (2010). Chemotherapy outpatients' unplanned presentations to hospital: a retrospective study. Supportive Care in Cancer, 19(7), 963–969. 10.1007/s00520-010-0913-y [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. (2017). SEER cancer statistics review, 1975-2017. https://seer.cancer.gov/archive/csr/1975_2017/
- Rivera, D. R., Gallicchio, L., Brown, J., Liu, B., Kyriacou, D. N., & Shelburne, N. (2017). Trends in adult cancer–related emergency department utilization. JAMA Oncology, 3(10), e172450. 10.1001/jamaoncol.2017.2450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rui, P. K. K. (2015). National Hospital Ambulatory Medical Care Survey: 2015 emergency department summary tables. https://www.cdc.gov/nchs/data/nhamcs/web_tables/2015_ed_webtables.pdf.
- Sivendran, S., Holliday, R., Guittar, R., Cox, C., & Newport, K. (2016). The impact of a nurse practitioner-led symptom clinic on emergency department use in cancer patients. Journal of Community and Supportive Oncology, 14(6), 268–272. 10.12788/jcso.0227 [DOI] [Google Scholar]
- Talcott, J. A., Finberg, R., Mayer, R. J., & Goldman, L. (2022). The medical course of cancer patients with fever and neutropenia. Clinical identification of a low-risk sub-group at presentation. Archives of Internal Medicine, 148(12), 2561–2568. https://pubmed.ncbi.nlm.nih.gov/3196123/ [PubMed] [Google Scholar]