IMPORTANCE:
Although rapid treatment improves outcomes for patients presenting with sepsis, early detection can be difficult, especially in otherwise healthy adults.
OBJECTIVES:
Using medico-legal data, we aimed to identify areas of focus to assist with early recognition of sepsis.
DESIGN, SETTING, AND PARTICIPANTS:
Retrospective descriptive design. We analyzed closed medico-legal cases involving physicians from a national database repository at the Canadian Medical Protective Association. The study included cases closed between 2011 and 2020 that had documented peer expert criticism of a diagnostic issue related to sepsis or relevant infections.
MAIN OUTCOMES AND MEASURES:
We used univariate statistics to describe patients and physicians and applied published frameworks to classify contributing factors (provider, team, system) and diagnostic pitfalls based on peer expert criticisms.
RESULTS:
Of 162 involved patients, the median age was 53 years (interquartile range [IQR], 34–66 yr) and mortality was 49%. Of 218 implicated physicians, 169 (78%) were from family medicine, emergency medicine, or surgical specialties. Eighty patients (49%) made multiple visits to outpatient care leading up to sepsis recognition/hospitalization (median = two visits; IQR, 2–4). Almost 40% of patients were admitted to the ICU. Deficient assessments, such as failing to consider sepsis or not reassessing the patient prior to discharge, contributed to the majority of cases (81%).
CONCLUSIONS AND RELEVANCE:
Sepsis continues to be a challenging diagnosis for clinicians. Multiple visits to outpatient care may be an early warning sign requiring vigilance in the patient assessment.
Keywords: Canada, delayed diagnosis, infections, malpractice, sepsis
KEY POINTS
Question: Using medico-legal data, what patient characteristics and elements of healthcare contributed to diagnostic delay of sepsis? What potential warning signs for patients at risk of developing severe sepsis could be identified?
Findings: Findings include a relatively high mortality rate (49%). Deficient assessments, including failure to include sepsis in the differential diagnosis, contributed to the majority of cases in our study. Almost half of the patients had multiple visits to outpatient care prior to recognition of sepsis.
Meaning: Medico-legal data may help to identify clues that are overlooked early in the patient course that may result in delayed diagnosis of sepsis.
Sepsis is organ dysfunction caused by a dysregulated host response to infection and is life-threatening (1), with greater risks for people under 1 year old or in higher age groups (2, 3). There were an estimated 11 million sepsis-related deaths worldwide in 2017 (4), and for septic shock, in particular, the mortality rate has decreased very little in recent decades despite advances in sepsis management (5, 6).
Outcomes for patients with sepsis can be improved through the early recognition of sepsis and appropriate management, which may include prompt consultation and admission to ICU (7). Yet early detection can be difficult. Of patients who experience sepsis, the estimated proportion with a missed or delayed diagnosis ranges between 8.2% and 20.8% (8, 9). In an effort to help with early detection, researchers have redefined sepsis (10) and validated criteria for identifying high-risk patients. Other studies have analyzed sepsis care retrospectively to learn from suboptimal outcomes, but their use of billing data (11) or medical charts from a single hospital (12) may have overlooked contextual factors that challenge early detection.
In this study, we analyzed cases featuring diagnostic delays with sepsis or relevant infections from a repository of medico-legal data. Each case had previously undergone independent peer-reviewed scrutiny of the care provided, offering unique insights into physicians’ cognitive processes, personal interactions with teams and patients, and system factors. Our study objectives were to describe the patient characteristics and elements of healthcare associated with diagnostic delays and suggest opportunities for improvement.
MATERIALS AND METHODS
We conducted a retrospective descriptive study of medico-legal cases supported by the Canadian Medical Protective Association (CMPA). Ethical approval for the conduct of this study was provided by the Advarra Institutional Review Board (Approval number: MOD01230759; approval date: February 18, 2022; study title: “The Canadian Medico-legal Landscape: A Mixed Methods Study.” Study procedures followed the regional ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975). The Reporting of studies Conducted using Observational Routinely-collected Data (RECORD) statement (13) guided report writing.
Setting
The CMPA offers medico-legal support, advice, and education to physicians and engages in safe medical care research using medico-legal data. The CMPA has over 105,000 physician members who can contact the Association for advice or support for medico-legal matters.
In this study, each case represented a complaint against a physician in a civil legal, medical regulatory authority (College, equivalent to a state medical board), or hospital matter (defined in Appendix 1, http://links.lww.com/CCX/B128). All cases had been closed by the CMPA between January 1, 2011, and December 31, 2020. Cases were de-identified and reported in aggregate to ensure confidentiality for both patients and healthcare providers.
Data Source
For all closed cases with sufficient information, experienced CMPA nurse-analysts routinely summarize each case file—including the case information, peer expert opinions, and the ruling or final decision—and apply medical coding. These codes represent patient demographic information, health conditions (14), peer expert opinions classified using the CMPA’s published contributing factors framework (15), and patient harm classified using an in-house classification of harms (Appendix 2, http://links.lww.com/CCX/B128). To reduce misclassification, nurse-analysts conduct regular quality assurance reviews of coding electronically and as a group.
Study Population
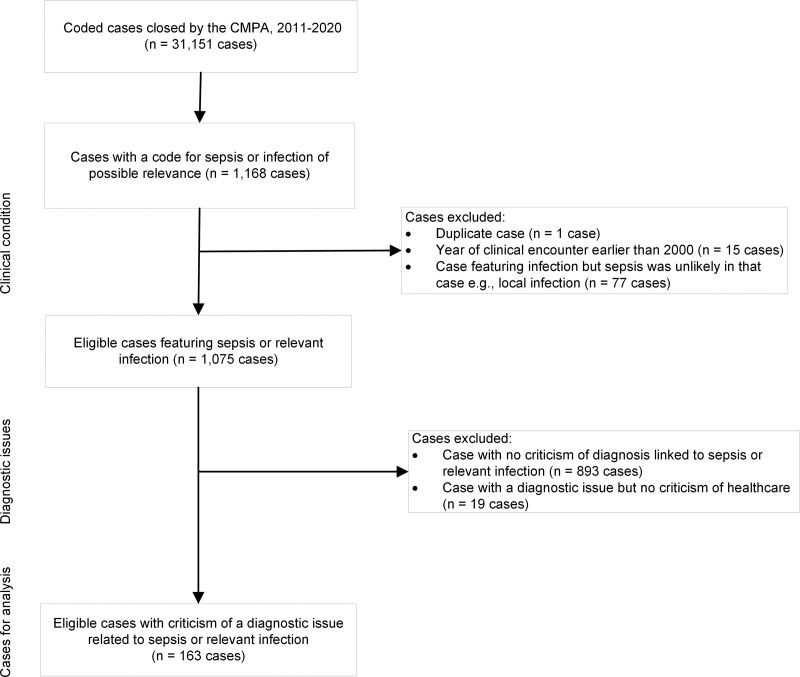
For study inclusion, cases must have been closed by the CMPA between 2011 and 2020 and involved sepsis or relevant infections (defined in Appendix 3, http://links.lww.com/CCX/B128) that were associated with an identified diagnostic delay/failure or wrong diagnosis and had documented peer expert criticism of a provider, team, or system. We identified these cases using International Classification of Diseases, 10th Revision, Canada (ICD-10-CA) codes from the literature (16) and the clinical judgment of coauthors (P.J.F., E.J.B., G.E.G.). Perinatal infections, neonatal infections, and puerperal sepsis were not included. Specific other infections were included (endocarditis, Clostridioides difficile, Staphylococcus aureus, pneumonia) as they may progress to sepsis and addressed our interest in early recognition. For those infections, a nurse-researcher (P.J.F.) reviewed CMPA case summaries and excluded the case if sepsis was unlikely (explained in Appendix 3, http://links.lww.com/CCX/B128). We excluded cases with clinical encounters pre-2000, the approximate year of change in sepsis standard of care (Fig. 1 for study flow chart).
Figure 1.
Study flow chart. See Appendix 3 (http://links.lww.com/CCX/B128) for list of eligible International Classification of Diseases, 10th Revision, Canada codes for sepsis and relevant infections. CMPA = Canadian Medical Protective Association.
Variables
Variables of interest were patient characteristics, location, and specialty of implicated physicians (defined in Appendix 2, http://links.lww.com/CCX/B128) and documented peer expert criticisms (contributing factors). We abstracted the following variables directly from the repository: case type, date of clinical encounter, physician subspecialty, patient gender implied from the medico-legal documentation, patient date of birth, risk factors, harm (Appendix 2, http://links.lww.com/CCX/B128), patient-reported reason for visiting a physician (presenting complaint), and CMPA contributing factors as previously described. We derived the following variables (described in Appendix 4, http://links.lww.com/CCX/B128): number of outpatient visits for the same condition (to a family doctor, emergency department, or walk-in clinic) before sepsis was recognized or patient was admitted to hospital; recent surgery or invasive procedure; geographic location (17, 18); and physician specialty.
Analysis
We calculated frequencies, proportions, and univariate statistics for variables of interest. For brevity, we reported only the most frequent (≥ 10) reasons for visiting physicians and the three most frequent contributing factors attributed to providers, teams, and systems, respectively. We described patient-physician communication breakdowns as in the literature (19). In post hoc analyses, we mapped criticisms of physicians to the Diagnosis Error Evaluation and Research (DEER) taxonomy (20) (Appendix 5, http://links.lww.com/CCX/B128). To apply the DEER taxonomy, a nurse-researcher (P.J.F.) and emergency department physician (E.J.B.) independently reviewed medico-legal case summaries and categorized peer expert criticisms into phases of the diagnostic process. A nurse-clinical-coding specialist (C.M.O.) verified categorizations and discrepancies were resolved by consensus. We used SAS Version 9.4 (SAS Institute Inc., Cary, NC), Microsoft Excel (Microsoft Corporation. Redmond, WA), and a custom data analysis tool in Microsoft Access (Microsoft Corporation) for statistical analyses.
RESULTS
One-hundred sixty-three cases met eligibility criteria: 81 civil legal matters (50%), 75 College matters (46%), and seven hospital matters (4%). These cases involved 162 patients (one patient made two claims). Most clinical encounters happened in large urban population centers (99/163 cases, 61%) (Table 1). Clinical encounters occurred between 2000 and 2020 as civil legal cases may take years to proceed to closure.
TABLE 1.
Physician Characteristics in Canadian Medical Protective Association Medico-Legal Cases (Closed 2011–2020) With Peer Expert Criticism of a Diagnostic Issue Linked to Sepsis or a Relevant Infection, n = 163 Cases
| Characteristics | n (%) |
|---|---|
| Healthcare | |
| Geographic locationa | |
| Large urban population center | 99 (60.7) |
| Medium population center | 19 (11.7) |
| Small population center or rural area | 45 (27.6) |
| Physicians, n = 218 | |
| Specialtyb,c | |
| Family medicine or general practice | 63 (28.9) |
| Subgroup that provided care in the emergency department | 15 (6.9) |
| Emergency medicine | 59 (27.1) |
| Surgical | 47 (21.6) |
| Medical | 39 (17.9) |
| Residency or postgraduate training | 10 (4.6) |
Location of the implicated physician(s) (defined in Appendix 2, http://links.lww.com/CCX/B128) when administering healthcare described in the medico-legal record. Geographic locations are defined using Statistics Canada categories (21, 22) and methods described in Appendix 5 (http://links.lww.com/CCX/B128).
See Appendix 7 (http://links.lww.com/CCX/B128) for physician specialty definitions.
Percent was calculated for 218 implicated physicians (defined in Appendix 2, http://links.lww.com/CCX/B128); 42 of 163 cases (25.8%) involved more than one of these physicians.
While patients spanned all ages (range, 0–90 yr), many (83/162, 51%) were 30–64 years old. The mortality rate of 49% (79/162) varied by age group and was highest among elderly patients (65% for patients 65–79 yr old, 89% for patients ≥ 80 yr; see Appendix 7, http://links.lww.com/CCX/B128). Thirty percent of patients (49/162) experienced severe harm, such as limb amputation due to gangrene or brain damage. Fever was a documented presenting complaint for just 26% of patients (Appendix 4, http://links.lww.com/CCX/B128). Several patients had recent surgeries/invasive procedures (41/162, 25%), of which most were abdominal (31/41, 76%). Almost 40% of patients (63/162) required ICU care during their hospitalization. More detailed patient characteristics can be found in Appendix 7 (http://links.lww.com/CCX/B128).
Nearly half of patients (80 of 162, 49%) made multiple visits to a family physician, walk-in clinic, or emergency department in the time leading up to sepsis recognition/hospitalization. Of those, 75% (60/80) made more than one visit within 72 hours of recognition/hospitalization (e.g., signs or symptoms normalized but later returned). The median number of visits was 2 (interquartile range, 2–4 visits); 13 patients made five or more visits. Among 41 patients with recent surgeries/invasive procedures, a subset was discharged from hospital and later assessed in hospital emergency departments (11 patients) or sought care multiple times (2–4 visits) from family physicians or specialists (nine patients).
A total of 218 physicians were involved in these cases. While the implicated physicians spanned all specialties, the majority (169/218 physicians, 78%) specialized in family medicine, emergency medicine, or surgery (Table 1). Within the surgical group, 30 of 47 physicians (64%) were general surgeons.
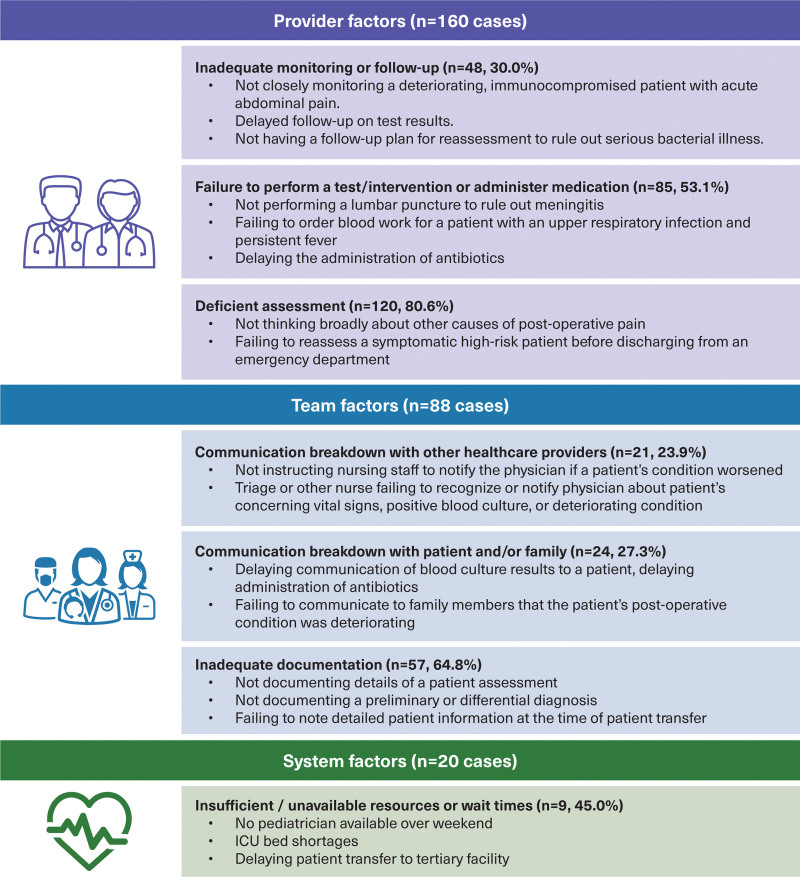
Deficient assessment was the top contributing factor attributed to providers, suggesting problems with information-gathering or considering diagnoses. For example, some physicians failed to reassess symptomatic high-risk patients before discharging from emergency departments (Fig. 2). Also common were physicians failing to perform tests or interventions (e.g., bloodwork) or inadequately monitoring patients. Other notable contributing factors identified in our cases included delays in physicians attending to patients (e.g., not assessing patients in person in a timely manner after handover or consultation) and poor coordination of care that led to delays in diagnostic testing.
Figure 2.
Top factors contributing to 163 medico-legal cases involving physicians; Canadian Medical Protective Association cases closed 2011–2020.
The DEER taxonomy classified 76% of physician pitfalls (123/163 cases; Table 2) in the assessment phase of diagnosis (defined in Appendix 5, http://links.lww.com/CCX/B128), suggesting failures/delays to consider diagnoses, failures/delays to consider or recognize patient urgency or complications, or suboptimal prioritization of diagnoses.
TABLE 2.
Physician-Related Pitfalls in the Diagnostic Processa,b in 163 Medico-Legal Cases Involving Physicians; Canadian Medical Protective Association Cases Closed 2011–2020
| Phase of Diagnostic Process | n (%) | Example From Cases |
|---|---|---|
| Access and presentation | 0 (0) | None |
| History | 31 (19.0) | Failing to question patients in detail about risk factors for infection |
| Not reviewing a medical chart that included abnormal findings by a previous physician | ||
| Physical examination | 66 (40.5) | Not listening to the patient’s chest at any repeat visit for the same health issue |
| Conducting a suboptimal (superficial) examination on a deteriorating patient with concerning vital signs | ||
| Testing | 80 (49.1) | Not conducting a full septic work-up when indicated for a patient under 12 mo old |
| Misinterpreting a postoperative CT image showing the source of infection | ||
| Delaying to follow-up on a positive blood culture after discharging a patient from the emergency department | ||
| Assessment | 123 (75.5) | Wrongly attributing signs or symptoms in adult patients to illicit drugs or prescription medications |
| Not recognizing the signs and symptoms of septic shock thereby delaying treatment | ||
| Failing to consider an alternative diagnosis when the treatment response was not sustained or a patient was deteriorating | ||
| Referral or consultation | 48 (29.4) | Delaying or not requesting a second opinion when the diagnosis was unclear |
| Delaying transfer of a patient with significant signs and symptoms to a tertiary hospital | ||
| Follow-up | 7 (4.3) | Performing no further investigations after the clinical encounter to confirm or rule out a diagnosis |
Each pitfall represents documented peer expert criticisms of a physician’s care in the medico-legal record. A single case may have had multiple pitfalls.
Using the Diagnosis Error Evaluation and Research taxonomy (23) defined in Appendix 6 (http://links.lww.com/CCX/B128).
The top contributing factors attributed to teams were inadequate documentation and communication breakdowns, either between healthcare professionals or between physicians and patients/caregivers (Fig. 2). In the latter scenario (24 cases), peer experts were critical of physicians’ communication: delayed, absent, or incorrect (e.g., communicating diagnostic test results); being disrespectful (e.g., end-of-life communication with family); or not eliciting key information (e.g., from parents of pediatric patients). Peer experts also noted issues with transitions in care, including failures to document detailed patient information when transferring patients to another institution, or failures to provide clear monitoring instructions to nurses (Fig. 2).
The top contributing factors attributed to systems were insufficient/unavailable resources (e.g., pediatric specialist) and extended wait times in emergency departments or patient transfers (Fig. 1).
DISCUSSION
We analyzed 163 closed cases involving physicians and sepsis-related diagnostic issues. We observed a relatively low proportion of known sepsis risk factors such as chronic illness, immune compromising conditions, and extreme age in our population. Of note, just 25% of patients presented with fever. Most physicians implicated in these cases specialized in family medicine, emergency medicine, and surgery. The top factor contributing to sepsis-related diagnostic issues was deficient assessment.
Epidemiological studies suggest that the incidence of severe sepsis is greatest for patients age less than 1 year (5/1,000 patients) or greater than or equal to 85 years (26/1,000 patients) (3). In our dataset, however, 51% of patients were age 30–64 years, which is more consistent with large studies of medical malpractice data (24). The 49% mortality rate in our study exceeded average mortality associated with septic shock (30–40%) (5, 6) and was comparable to 5-year mortality for severe sepsis (55%) (21).
Our findings of frequent deficient assessments, issues with verbal and written communication, and insufficient resources (in the provider, team, system domains, respectively) align with other studies of diagnostic error (20, 22, 25), sepsis care (23,26,27), and medico-legal risk (24). A deficient assessment, the most common contributing factor overall, may reflect cognitive bias—a form of systematic error due to subconscious, intuitive clinical reasoning or mental shortcuts (28). Early screening tools such as quick Sequential Organ Failure Assessment scores (29) have potential to mitigate bias but in order for physicians to apply them, infections need to be in the differential diagnosis. Physicians might also consider cognitive debiasing strategies (30, 31), such as deliberately reflecting (31), using decision support systems (32), and drawing collective intelligence from teams (33) to improve patient assessments.
Multiple visits to outpatient care may be an early warning sign for patients at risk of developing sepsis (11, 34). Studies suggest that multiple outpatient visits are common in the 2 to 3 days (11, 34) or 5 to 7 days (35–37) leading up to sepsis hospitalization. This is consistent with our study, in which half of the patients in our dataset had multiple outpatient visits prior to the diagnosis of sepsis. The literature in this area has been limited to studies without control groups and further research is required, but multiple visits to outpatient care may represent an opportunity for physicians to consider sepsis in an evolving differential diagnosis.
Almost 40% of patients in our series were admitted to the ICU during their hospitalization, and mortality rate was high in this group. Criticism of the care received in the ICU or provided by critical care physicians, however, was uncommon. This underscores the importance of early diagnosis and also suggests that diagnostic issues related to sepsis occur prior to admission to ICU. Despite this, our data offer some potential considerations for critical care specialists. In several of our cases, peer experts were critical of the timeliness of physicians directly assessing patients after handover or consultation. Providers should consider the importance of prompt, in-person assessments of patients to reduce potential delays in ordering appropriate tests or supporting the diagnostic process. Critical care physicians might also consider how best to coordinate the care of patients at increased risk of sepsis with their surgical, emergency department and hospitalist colleagues, as appropriate care and prompt admission to ICU may improve outcomes (7).
Our study has several limitations. Lack of a control or comparator group prevented comparisons that might have generated further insights and context. The ICD-10-CA codes for identifying sepsis conditions (Appendix 3, http://links.lww.com/CCX/B128) differ from those used in other studies (16), which could impact comparisons with other reports. Our list was appropriate, however, given our inclusion of both clinical and microbiological indications of relevance to early sepsis recognition and case-by-case verification by a nurse-researcher. Our results reflect only diagnostic issues reported to the CMPA. To our knowledge, CMPA physician-members seek assistance for nearly all civil legal cases to the CMPA but do not always seek assistance for College and hospital matters. Despite rigorous quality assurance processes in place to assess the quality of the medical coding of our cases, we do not calculate and thus cannot report formal measures of inter-coder reliability, such as a Kappa statistic. We also acknowledge the selective nature of peer expert opinions in civil legal cases and potential for biases (38); some contributing factors were likely undocumented. Finally, our data may underrepresent patient risk factors and outpatient visits since the CMPA’s medical coding generally only captures details of medico-legal relevance.
CONCLUSIONS
This study describes a cohort of medico-legal claims pertaining to patients with missed or delayed diagnoses of sepsis. Adults 30–64 years old were overrepresented in our data, and patient outcomes were severe. Over half of the patients in our sample had multiple visits to outpatient care in the days leading up to their diagnosis with sepsis. Our descriptive analysis of a unique medico-legal dataset suggests that there are challenges remain in recognizing sepsis-related conditions in patients of any age, with or without specific complaints or comorbidities.
ACKNOWLEDGMENTS
We wish to thank Ria De Gorter for project administration; Joanna Zaslow for assisting with the literature review and protocol writing; Allan McDougall for supporting the article revisions; and Qian Yang for providing supervision and resources and facilitating data requests to the Canadian Institute for Health Information. We also thank the Data Capture team in the Department of Safe Medical Care Research at the Canadian Medical Protective Association for medical coding.
Supplementary Material
Footnotes
This study was funded by the Canadian Medical Protective Association.
Parts of this material are based on data and information provided by the Canadian Institute for Health Information. However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors and not necessarily those of the Canadian Institute for Health Information.
Dr. Liu disclosed work for hire. Dr. Bridges received funding from the Canadian Medical Protection Association that provides specialized professional development programs; she disclosed that she is a member of the Scientific Planning Committee at Saegis. All authors disclosed that they are employees of the Canadian Medical Protective Association, a not-for-profit mutual defense organization for physicians, at the time of this study.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
REFERENCES
- 1.Seymour CW, Liu VX, Iwashyna TJ, et al. : Assessment of clinical criteria for sepsis: For the third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016; 315:762–774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Navaneelan T, Alam S, Peters PA, et al. : Deaths Involving Sepsis in Canada. Ottawa, ON, Canada, Statistics Canada, 2016. Contract No.: Catalogue no.82-624-X. Available at: https://www150.statcan.gc.ca/n1/pub/82-624-x/2016001/article/14308-eng.htm. Accessed January 3, 2023 [Google Scholar]
- 3.Angus DC, Linde-Zwirble WT, Lidicker J, et al. : Epidemiology of severe sepsis in the United States: Analysis of incidence, outcome, and associated costs of care. Crit Care Med 2001; 29:1303–1310 [DOI] [PubMed] [Google Scholar]
- 4.Rudd KE, Johnson SC, Agesa KM, et al. : Global, regional, and national sepsis incidence and mortality, 1990-2017: Analysis for the Global Burden of Disease Study. Lancet 2020; 395:200–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bauer M, Gerlach H, Vogelmann T, et al. : Mortality in sepsis and septic shock in Europe, North America and Australia between 2009 and 2019- results from a systematic review and meta-analysis. Crit Care 2020; 24:239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vincent JL, Jones G, David S, et al. : Frequency and mortality of septic shock in Europe and North America: A systematic review and meta-analysis. Crit Care 2019; 23:196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Evans L, Rhodes A, Alhazzani W, et al. : Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Crit Care Med 2021; 49:e1063–ee143 [DOI] [PubMed] [Google Scholar]
- 8.Newman-Toker DE, Wang Z, Zhu Y, et al. : Rate of diagnostic errors and serious misdiagnosis-related harms for major vascular events, infections, and cancers: Toward a national incidence estimate using the “Big Three.” Diagnosis (Berl) 2021; 8:67–84 [DOI] [PubMed] [Google Scholar]
- 9.Cifra CL, Westlund E, Ten Eyck P, et al. : An estimate of missed pediatric sepsis in the emergency department. Diagnosis (Berl) 2021; 8:193–198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Singer M, Deutschman CS, Seymour CW, et al. : The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA 2016; 315:801–810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nassery N, Horberg MA, Rubenstein KB, et al. : Antecedent treat-and-release diagnoses prior to sepsis hospitalization among adult emergency department patients: A look-back analysis employing insurance claims data using Symptom-Disease Pair Analysis of Diagnostic Error (SPADE) methodology. Diagnosis (Berl) 2021; 8:469–478 [DOI] [PubMed] [Google Scholar]
- 12.Filbin MR, Lynch J, Gillingham TD, et al. : Presenting symptoms independently predict mortality in septic shock: Importance of a previously unmeasured confounder. Crit Care Med 2018; 46:1592–1599 [DOI] [PubMed] [Google Scholar]
- 13.Benchimol EI, Smeeth L, Guttmann A, et al. : The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med 2015; 12:e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Canadian Institute for Health Information: Canadian Coding Standards for Version 2018 ICD-10-CA and CCI. Ottawa, ON, Canada, Canadian Institute for Health Information, 2018. Available at: https://secure.cihi.ca/free_products/CodingStandards_v2018_EN.pdf. Accessed January 3, 2023 [Google Scholar]
- 15.McCleery A, Devenny K, Ogilby C, et al. : Using medicolegal data to support safe medical care: A contributing factor coding framework. J Healthc Risk Manag 2019; 38:11–18 [DOI] [PubMed] [Google Scholar]
- 16.Jolley RJ, Quan H, Jetté N, et al. : Validation and optimisation of an ICD-10-coded case definition for sepsis using administrative health data. BMJ Open 2015; 5:e009487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Statistics Canada: Population Centre and Rural Area Classification Ottawa. 2016. Available at https://www.statcan.gc.ca/en/subjects/standard/pcrac/2016/introduction. Accessed January 3, 2023
- 18.Statistics Canada: Population and Dwelling Count Highlight Tables, 2016 Census Ottawa. 2016. Available at https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/hlt-fst/pd-pl/Table.cfm?Lang=Eng&T=703&S=87&O=A. Accessed January 3, 2023
- 19.Gillespie A, Reader TW: The Healthcare Complaints Analysis Tool: Development and reliability testing of a method for service monitoring and organisational learning. BMJ Qual Saf 2016; 25:937–946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schiff GD, Hasan O, Kim S, et al. : Diagnostic error in medicine: Analysis of 583 physician-reported errors. Arch Intern Med 2009; 169:1881–1887 [DOI] [PubMed] [Google Scholar]
- 21.Farrah K, McIntyre L, Doig CJ, et al. : Sepsis-associated mortality, resource use, and healthcare costs: A propensity-matched cohort study. Crit Care Med 2021; 49:215–227 [DOI] [PubMed] [Google Scholar]
- 22.Schnapp BH, Sun JE, Kim JL, et al. : Cognitive error in an academic emergency department. Diagnosis (Berl) 2018; 5:135–142 [DOI] [PubMed] [Google Scholar]
- 23.Matthaeus-Kraemer CT, Thomas-Rueddel DO, Schwarzkopf D, et al. : Crossing the handover chasm: Clinicians’ perceptions of barriers to the early detection and timely management of severe sepsis and septic shock. J Crit Care 2016; 36:85–91 [DOI] [PubMed] [Google Scholar]
- 24.Newman-Toker DE, Schaffer AC, Yu-Moe CW, et al. : Serious misdiagnosis-related harms in malpractice claims: The “Big Three” - vascular events, infections, and cancers. Diagnosis (Berl) 2019; 6:227–240 [DOI] [PubMed] [Google Scholar]
- 25.Okafor N, Payne VL, Chathampally Y, et al. : Using voluntary reports from physicians to learn from diagnostic errors in emergency medicine. Emerg Med J 2016; 33:245–252 [DOI] [PubMed] [Google Scholar]
- 26.Raben DC, Viskum B, Mikkelsen KL, et al. : Application of a non-linear model to understand healthcare processes: Using the functional resonance analysis method on a case study of the early detection of sepsis. Reliab Eng Syst Saf 2018; 177:1–11 [Google Scholar]
- 27.Loots FJ, Smits M, van Steensel C, et al. : Management of sepsis in out-of-hours primary care: A retrospective study of patients admitted to the intensive care unit. BMJ Open 2018; 8:e022832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Croskerry P, Singhal G, Mamede S: Cognitive debiasing 1: Origins of bias and theory of debiasing. BMJ Qual Saf 2013; 22(Suppl 2):ii58–ii64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lane DJ, Wunsch H, Saskin R, et al. : Screening strategies to identify sepsis in the prehospital setting: A validation study. CMAJ 2020; 192:E230–E239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Croskerry P, Singhal G, Mamede S: Cognitive debiasing 2: Impediments to and strategies for change. BMJ Qual Saf 2013; 22(Suppl 2):ii65–ii72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Norman GR, Monteiro SD, Sherbino J, et al. : The causes of errors in clinical reasoning: Cognitive biases, knowledge deficits, and dual process thinking. Acad Med 2017; 92:23–30 [DOI] [PubMed] [Google Scholar]
- 32.Sibbald M, Monteiro S, Sherbino J, et al. : Should electronic differential diagnosis support be used early or late in the diagnostic process? A multicentre experimental study of Isabel. BMJ Qual Saf 2021; 31:426–433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schaller-Paule MA, Steinmetz H, Vollmer FS, et al. : Lessons in clinical reasoning - pitfalls, myths, and pearls: The contribution of faulty data gathering and synthesis to diagnostic error. Diagnosis (Berl) 2021; 8:515–524 [DOI] [PubMed] [Google Scholar]
- 34.Miller HC, Liu VX, Prescott HC: Characteristics and outcomes of clinic visits immediately preceding sepsis hospitalization. Am J Crit Care 2021; 30:135–139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vaillancourt S, Guttmann A, Li Q, et al. : Repeated emergency department visits among children admitted with meningitis or septicemia: A population-based study. Ann Emerg Med 2015; 65:625–632.e3 [DOI] [PubMed] [Google Scholar]
- 36.Fay K, Sapiano MRP, Gokhale R, et al. : Assessment of health care exposures and outcomes in adult patients with sepsis and septic shock. JAMA Netw Open 2020; 3:e206004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Liu VX, Escobar GJ, Chaudhary R, et al. : Healthcare utilization and infection in the week prior to sepsis hospitalization. Crit Care Med 2018; 46:513–516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hugh TB, Tracy GD: Hindsight bias in medicolegal expert reports. Med J Aust 2002; 176:277–278 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.