Abstract
Background:
Little is known about how local area hospice capacity and staffing levels impact hospice use in urban versus rural areas.
Objectives:
To examine the association between local hospice capacity and staffing levels and hospice use in the context of rural disparities in hospice use, among a sample of patients with metastatic breast cancer.
Design:
A retrospective cohort study using Surveillance Epidemiology End-Results (SEER)—Medicare linked data 2000–2010, Medicare Provider of Service files, and Census 2000 U.S. Zip Code Tabulation Areas files.
Setting:
Use of Medicare-certified hospice programs among older adults with metastatic breast cancer residing in one of the SEER program cancer registries designated by National Cancer Institute in the United States.
Measurements:
Measurements of geographic access to hospices include urban/rural characteristics of patient residence and driving time from the nearest Medicare-certified hospice headquarter. Measurements of local-area hospice capacity and staffing levels include per capita number of Medicare-certified hospice programs and full-time employees among older adults within a predefined radius.
Results:
Among the study population (N = 5418), remote and suburban areas were negatively associated with hospice use. Lower hospice use in remote and suburban areas was associated with fewer per capita number of Medicare-certified hospice program employees in local areas ≥70-minute driving radius (p = 0.0042), while per capita number of Medicare-certified hospice programs in local areas showed no impact.
Conclusion:
For older patients with metastatic breast cancer, availability of hospice staff, rather than driving distance or the number of hospice agencies, may limit hospice use in remote and suburban areas.
Keywords: geographic access, health care workforce, health disparities, hospice capacity, hospice size, rural health
Introduction
Hospice care is an exemplary model of expert medical care, pain and symptom management, and emotional and social support for patients with life-limiting illnesses and their family members. In the United States between the early 2000s and 2010, there was tremendous growth in the hospice care industry, witnessed by increased access to hospice services among patients.1,2 In the last decade, the sustained growth in hospice programs has been driven by for-profit hospice programs, while the number of nonprofit and government-funded hospice programs has slightly decreased.3 Patients enrolled in hospice expanded to 1.61 million, and 51.6% of Medicare decedents used hospice in 2019.4
However, entrenched disparities in hospice use remain in rural and frontier areas.1,5–7 Using National Hospice Survey data, studies on ownership, profitability, and preferred practices showed that urban locations often correlated with for-profit status and bigger sizes of hospice programs, which were shown to be associated with a number of outcomes, including differences in patient diagnosis, length of stay, and hospital utilization.8,9 In addition, variation in hospice use was observed by locations of health centers within an integrated health care system among cancer patients.10 This body of evolving literature suggests that factors at the practice level, such as hospice capacity and trained workforce, care coordination, and how patients, providers, and hospices interact at the local level, might contribute to barriers in access to hospice care.11
There have been scant data regarding how local-area hospice capacity and staffing levels may impact hospice use among patients across broad geographic locations of urban, suburban, rural, and remote areas. Previous studies estimated the extent of shortage of hospice and palliative care workforce based on staffing levels of existing hospice and palliative care programs.12 Because staffing models in hospice and palliative care programs are separate in the United States, more in-depth and nuanced data are critical to meet patient end-of-life care needs, due to economic incentives of reimbursement, inpatient versus home-based care, patient level of dependency, staff activities and workload, and team staff mix.13 Hospice staffing levels and the availability of certified hospice programs can be considered aspects of access to hospice care.
Delivering hospice care in rural and frontier areas is challenging because of long driving times, disconnected downstream communication and information dissemination, sparsely distributed health facilities, and relative isolation in these communities, which add complexities to the stretched daily schedules of health professionals and contribute to high turnover rates in the hospice care workforce.14 These predisposing factors of human resources and professional networks may affect how patients and providers understand end-of-life care, gain experience in when and how to receive hospice benefits, and make goal-concordant treatment decisions.
Understanding how local area hospice capacity and staffing levels within an accessible geographic area exert an influence on hospice use among patients with potential needs for end-of-life care provides actionable opportunities to address modifiable human resource factors in reducing disparities in hospice use, particularly in less urban areas. Therefore, the hypotheses of this study are as follows: (1) a greater per capita number of hospices and hospice staff is associated with increased hospice use in localized geographical areas and (2) per capita number of hospices and hospice staff is associated with more prominent effects on increased hospice use among patients living in rural and remote areas more than their counterparts in urban areas.
Using the zip code-centered driving time to define localized areas, the purpose of this study is to examine how local hospice capacity and staffing levels impacted hospice use in urban versus less-urban neighborhoods among a sample of older adults with metastatic breast cancer in the United States.
Materials and Methods
This is a retrospective cohort study. We followed the STROBE reporting guidelines for observational studies.15
Setting
The clinical setting for this study was the use of Medicare-certified hospice programs among older adults 65 years and older with metastatic breast cancer, who resided in one of the Surveillance Epidemiology End-Results (SEER) program cancer registries designated by National Cancer Institute in the United States.
Data sources
SEER-Medicare linked data 2001–2010 were used to select study population. Data collected at National Cancer Institute SEER cancer registries, also referred to as Patient Entitlement and Diagnosis Summary File, include patient demographics, information about cancer such as date of diagnosis, cancer type, stage, histology, other tumor-related information, and mortality. Medicare Provider of Service files were used to obtain the location and the number of hospice employees for each Medicare-certified hospice. Patient zip codes and census tract-level socioeconomic variables were obtained with permission from the review committee of SEER-Medicare program for this study. The Census 2000 U.S. Gazetteer Files Zip Code Tabulation Areas file was used to obtain the number of older adult populations (65+ years old) residing at each zip code.
Study population
Patients were selected if they were diagnosed with metastatic breast cancer for the first time between 2002 and 2009 and died between 2002 and 2010. The study population included those who were ≥66 years old at diagnosis, had continuous 12-month Medicare coverage before diagnosis to measure the comorbidities, and had continuous 24-month Medicare coverage post-diagnosis or until time of death.16,17
Patients were excluded if they were diagnosed with in situ stage I, II, or III, or unknown breast cancer; had an unknown month of diagnosis; had the date of death before the date of diagnosis; died on the same day of diagnosis or had a nonblank date of death from SEER and a blank date of death from Medicare claims indicating wrong documentation of death; or resided in a zip code outside the residing SEER area. Patients whose driving times were unavailable on Google Maps were also removed in the final analysis. The sample included 5418 patients.
Outcome variable
The outcome variable was whether the patient used any hospice service after being diagnosed with metastatic breast cancer.
Predictor variables
The key independent variables included rural/urban characteristics of the patient residence, driving time from the nearest hospice headquarter to patient residence, per capita number of Medicare-certified hospice programs, and Medicare-certified hospice programs' full-time employees (hereafter referred to as “employees”) among older adults 65+ years old located in an area surrounding the patient residence. Rural/urban continuum codes from Department of Agriculture Economic Research Service, available in the Patient Entitlement and Diagnosis Summary File, is a variable of nine categories that distinguish metropolitan counties by the population size and nonmetropolitan counties by aggregated population size and adjacency to metropolitan areas.
Driving time between zip codes of patient residence and hospice headquarters was calculated using Statistical Analytical Software (SAS) and Google Maps,18 a method described in the study by Carlson et al1 The total number of Medicare-certified hospice programs and their employees was computed within a predetermined driving radius surrounding the patients' residence zip codes—that is, driving times of 25, 50, 60, 70, 80, 90, 100, 110, and 120 minutes—and then divided by the total number of older adults 65+ years old to get per capita number of Medicare-certified hospice programs and employees.
Control variables
Control variables included age, race, marital status, comorbidities, hormone biomarker status, diagnosis year, SEER cancer registry where patients resided, income, and education index at the census tract level. These variables were derived based on the patient utility model originated from Becker's economic approach to human behavior.19
Statistical analysis
We used univariate analyses to describe the distribution of driving time, per capita number of Medicare-certified hospice programs, and per capita number of hospice employees. Chi-square statistics were used to summarize the differences in hospice use across explanatory variables. Multivariate logistic regression models were used to estimate the effects of hospice access on hospice use. The key access variables were added in a stepwise approach. Interaction terms between race and each access variable were added to explore differential effects of local area hospice capacity on hospice care choice among racial/ethnic subgroups. Odds ratios were reported with a 95% confidence interval. The threshold of statistical significance was a two-sided p-value of <0.05.
This study was approved by Rocky Vista University Institutional Review Board as expedited and exempt (IRB No. 2019-0020). All data analyses were conducted using SAS 9.4 (SAS Institute, Inc., Cary, NC).
Results
Patient sociodemographic, geographic, and comorbid characteristics
Among the study population of 5418 patients, 48.73% received hospice care (Table 1). The average age of those who used hospice services was 78.97 years versus 77.05 years among those who did not. Hospice use increased steadily with age, with the lowest utilization rate of 39.23% among patients between 66 and 69 years of age and the highest rate 57.09% among those 85 years of age or older. Over 41% of the patients had one or more comorbidities before the diagnosis of metastatic breast cancer, although the number of comorbidities was not associated with hospice use.
Table 1.
Patient Sociodemographic, Geographic, and Comorbid Characteristics by Hospice Use
| Hospice use | Cases of hospice use (N = 5418) | p | |
|---|---|---|---|
| Characteristics | |||
| Age at diagnosis, years | |||
| 66–69 | 39.23% | 357 | <0.0001 |
| 70–74 | 43.02% | 515 | |
| 75–79 | 48.72% | 588 | |
| 80–84 | 55.12% | 592 | |
| 85 or older | 57.09% | 588 | |
| Race and ethnicitya | |||
| Asian | 31.11% | 42 | <0.0001 |
| Black | 44.61% | 298 | |
| Hispanic | 42.99% | 95 | |
| Non-Hispanic White | 50.25% | 2199 | |
| Marital status | |||
| Ever married | 51.61% | 1520 | <0.0001 |
| Married | 44.05% | 711 | |
| Single | 45.26% | 277 | |
| Unmarried/unknown | 53.44% | 132 | |
| Percentage of low-income residents above median | |||
| No | 48.78% | 2626 | 0.3001 |
| Yes | 40.00% | 14 | |
| No. of comorbiditiesb | |||
| 0 | 48.56% | 1550 | 0.6816 |
| 1 | 49.82% | 565 | |
| 2 | 48.08% | 525 | |
| Patient residencec characteristics | |||
| Metro ≥1M | 47.25% | 1435 | 0.0049 |
| Metro 250K–1M | 51.40% | 514 | |
| Metro ≤250K | 54.70% | 291 | |
| Urban, adjacent to metro >20K | 43.35% | 88 | |
| Urban, not adjacent to metro >20K | 45.37% | 49 | |
| Urban, adjacent to metro <20K | 53.16% | 143 | |
| Urban, not adjacent to metro <20K | 43.16% | 82 | |
| Rural, adjacent to metro <2500 | 54.76% | 23 | |
| Rural, not adjacent to metro <2500 | 40.54% | 15 | |
| State of residenced | |||
| California | 43.77% | 608 | <0.0001 |
| Connecticut | 42.50% | 153 | |
| Detroit | 51.13% | 227 | |
| Georgia | 59.12% | 308 | |
| Hawaii | 34.62% | 18 | |
| Iowa | 63.09% | 188 | |
| Kentucky | 49.02% | 200 | |
| Louisiana | 52.07% | 201 | |
| New Jersey | 45.18% | 502 | |
| New Mexico | 53.40% | 55 | |
| Seattle | 45.93% | 113 | |
| Utah | 67.00% | 67 | |
| Year of diagnosis of breast cancer | |||
| 2002 | 52.04% | 344 | <0.0001 |
| 2003 | 50.15% | 325 | |
| 2004 | 53.19% | 367 | |
| 2005 | 55.64% | 385 | |
| 2006 | 51.97% | 357 | |
| 2007 | 45.06% | 315 | |
| 2008 | 44.99% | 305 | |
| 2009 | 36.50% | 242 | |
Note: α = 0.05. Bolded values indicate statistical significance.
Race: American Indian/Alaska Native (n = 12), or unknown (n = 6) were not reported due to Centers for Medicare & Medicaid Services (CMS) cell size suppression policy. Asian population included Asian, Native Hawaiian, and Pacific Islander.
Comorbidities measured the following chronic conditions: chronic obstruction pulmonary disease, cerebrovascular disease, congestive heart failure, diabetes, dementia, myocardial infarction, peripheral vascular disease, peptic ulcer disease, paralysis, renal disease, rheumatologic disease.
Rural/urban area characteristics of patient residence was based on Area Resource File that is available in the Patient Entitlement and Diagnosis Summary Files (PEDSF) file, including counties of metro areas of 1 million population or more, counties of metro areas of 250,000–1,000,000 population, counties in metro areas of fewer than 250,000 population, counties of urban population of >20,000 population and adjacent to a metro area, counties of urban population of 2,500–19,999 and adjacent to a metro area, counties of urban population of 2,500–19,999 and not adjacent to a metro area, completely rural less than 2,500 urban population and adjacent to a metro area, and completely rural less than 2,500 population and not adjacent to a metro area.
State of residence was cancer registry at the state level or regions included in the Surveillance Epidemiology End-Results (SEER) program funded by the National Cancer Institute to collect cancer statistics in the United States.
Racial and ethnic minority groups, including Asian, Black, and Hispanic, were significantly less likely to use hospice than non-Hispanic Whites. Marital status and area poverty level were not associated with hospice use. About 88.08% of the study population lived in metropolitan or urban areas with populations of at least 20,000. Substantial variation in hospice use existed among SEER registries, with the highest utilization rate of 67.00% in Utah, almost twice the lowest rate of 34.62% in Hawai'i.
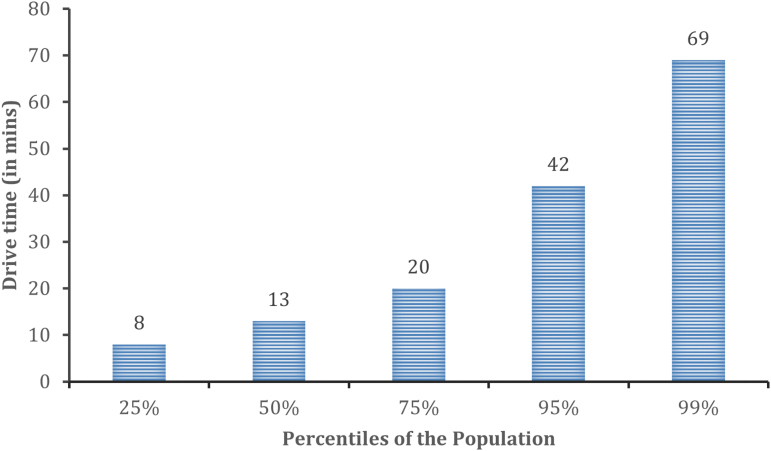
Driving time
Figure 1 shows that half the study population lived within a 13-minute drive of a Medicare-certified hospice program. About 83% of patient residences were within a 25-minute drive from a nearest hospice headquarter office (data not shown). The average driving time was 16 minutes.
FIG. 1.
Time from the nearest hospice headquarter to patient residence.
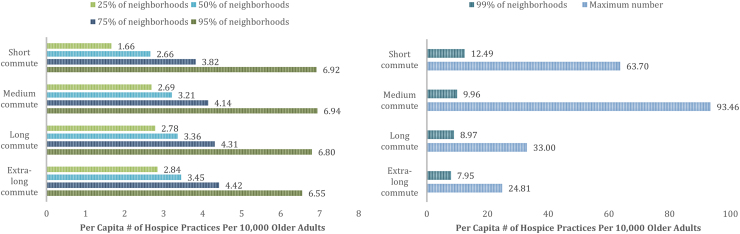
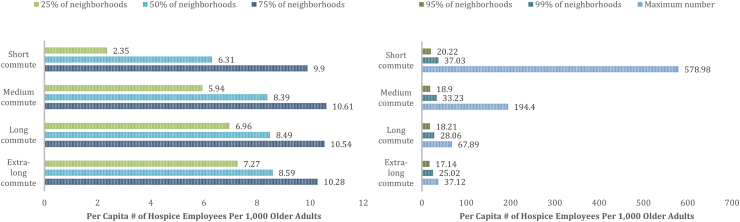
Per capita number of Medicare-certified hospice programs and employees
Figure 2 shows that up to 95% of these communities had comparable coverage in terms of per capita number of Medicare-certified hospice programs. Figure 3 shows that across these communities of different commuting time, staff availability had similar coverage for about 75% of these neighborhoods as indicated by per capita number of employees. Differences of staff availability ranged from 1.32 to 3.08 full-time employees per 1000 older adults comparing short commuting area (25 minutes) to medium (50 minutes), long (70 minutes), and extra-long commuting areas (100 minutes) at the 95th percentile (Fig. 3).
FIG. 2.
Up to 95% of the neighborhoods had comparable number of Medicare-certified hospice practices.
FIG. 3.
Up to 75% of the neighborhoods had comparable number of Medicare-certified hospice employees.
Predictors of use of hospice services
To assess the robustness of the results, we estimated the models based on local areas of driving time, defined as 25, 50, 60, 70, 80, 90, 100, 110, and 120 minutes. The results in Table 2 are estimates from local areas with a 70-minute driving time (results from local areas of 80 to 120 minutes were similar). In Model 1, with rural/urban area codes and other control variables, a statistically significant variation in hospice use was observed among areas defined by the rural/urban continuum codes.
Table 2.
Estimates of Effects of Local Area Hospice Capacity and Rural/Urban Residence on Hospice Use among Older Adults with Metastatic Breast Cancer
| Variable | N | Model 1a | Model 1+driving time | Model 1+driving time No. of hospice practices | Model 1+driving time No. of hospice employees |
|---|---|---|---|---|---|
| Rural/urban area characteristics | 5418 | ||||
| p Value of F-statistics | 0.0090* | 0.02* | 0.0153* | 0.1044 | |
| OR (95% CI) | |||||
| Metro ≥1M | 3037 | Reference | Reference | Reference | Reference |
| Metro 250K–1M | 1000 | 0.971 (0.809–1.165) | 0.978 (0.815–1.174) | 0.979 (0.816–1.175) | 1.017 (0.846–1.223) |
| Metro ≤250K pop. | 532 | 0.965 (0.771–1.208) | 0.966 (0.771–1.210) | 0.967 (0.772–1.212) | 1.049 (0.831–1.323) |
| Urban, adjacent to metro >20K | 203 | 0.692 (0.500–0.958) | 0.708 (0.510–0.982) | 0.717 (0.516–0.995) | 0.756 (0.543–1.052) |
| Urban, not adjacent to metro >20K | 108 | 0.766 (0.482–1.218) | 0.747 (0.465–1.200) | 0.751 (0.468–1.207) | 0.877 (0.538–1.429) |
| Urban, adjacent to metro <20K | 269 | 0.809 (0.597–1.096) | 0.832 (0.612–1.130) | 0.823 (0.605–1.119) | 0.903 (0.661–1.234) |
| Urban, not adjacent to metro <20K | 190 | 0.519 (0.363–0.741) | 0.537 (0.375–0.770) | 0.520 (0.360–0.751) | 0.612 (0.422–0.888) |
| Rural, adjacent to metro <2500 | 42 | 0.865 (0.445–1.679) | 0.929 (0.472–1.827) | 0.905 (0.459–1.785) | 0.989 (0.503–1.947) |
| Rural, not adjacent to metro <2500 | 37 | 0.457 (0.224–0.930) | 0.470 (0.230–0.962) | 0.454 (0.221–0.932) | 0.545 (0.265–1.123) |
| Driving time | |||||
| p Value of χ2-statistics | 0.2892 | 0.3501 | 0.3792 | ||
| Parameter estimate | −0.00136 | −0.00117 | −0.00108 | ||
| OR (95% CI) | 0.999 (0.996–1.001) | 0.999 (0.996–1.001) | 0.999 (0.997–1.001) | ||
| Per capita number of hospices | |||||
| p Value of χ2-statistics | 0.3810 | ||||
| Parameter estimate | 0.0203 | ||||
| OR (95% CI) | 1.021 (0.975–1.068) | ||||
| Per capita number of hospice employees | |||||
| p Value of χ2-statistics | 0.0042* | ||||
| Parameter estimate | 0.0239 | ||||
| OR (95% CI) | 1.024 (1.008–1.041) |
Results were tabulated based on the local area defined as a 70-minute driving time radius. Driving time, rural/urban area characteristics, per capita number of Medicare-certified hospice programs, and per capita number of hospice employees were defined the same as in the Materials and Methods section.
Control variables in the model include patient age, race, comorbidities, marital status, census tract median household income and education level, residence SEER area, and diagnosis year.
Model 1 includes rural/urban characteristics plus control variables.
Significance level at 0.05 level.
CI, confidence interval; OR, odds ratio; SEER, Surveillance Epidemiology End-Results.
Specifically, suburban and rural areas not adjacent to a metropolitan area had lower odds ratios of hospice use compared with metropolitan areas and areas adjacent to a metropolitan area. When adding driving time to Model 1, F-statistics showed that such variation among areas of different levels of rurality remained significant, while driving time was not significantly associated with hospice use at the population level. Correlation analysis showed that Pearson correlation coefficients between per capita number of Medicare-certified hospice programs and employees were 0.5320, 0.5100, and 0.3069 in 25-, 50-, and 100-mile radii, respectively.
Therefore, subsequent models included either of the two hospice access measures due to the multicollinearity. When adding per capita number of Medicare-certified hospice programs, this variable was not associated with hospice use. When adding per capita number of employees, this variable was significantly positively associated with hospice use. The parameter estimate of the variable suggested that the odds ratio of hospice use would increase by 1.024 (i.e., e0.0239), if adding one hospice staff for every thousand older adults 65+ years old in local areas within a 70-minute drive. Moreover, the per capita number of employees was consistently positively associated with hospice use in areas of 80- to 120-minute driving time models.
Effects of interaction terms between race/ethnicity and each access variable and squared terms of each access variable were not statistically significant. In addition, F-statistics of hospice use among SEER registries in all models were significant, suggesting that even after controlling for urban/rural characteristics and geographic access variables, there was still substantial regional variation in hospice use.
Discussion
With an aging population and an increasing burden of serious illnesses, continued increase in patient needs for high-quality end-of-life care is expected. This expectation translates into an increasing demand for palliative and hospice care health professionals, which would further strain the shortage of trained professionals in this specialty area, particularly for underserved areas.
Lower hospice use in suburban and rural areas without a neighboring metro area
Rural residence and driving time represent conceptually different aspects of geographic barriers in access to health care.20 Driving time from the nearest hospice headquarters to patient residence is a proxy measure of physical access to hospice services, indicating how far hospice-care health professionals may need to travel to provide care at patients' homes. Different from driving time, rural residence is a proxy for factors associated with lower use of hospice services in rural areas, including both geographic factors, such as long commutes, and nongeographic factors, such as demographic, socioeconomic, cultural, and environmental variables.21
In some regions, rural communities may be close enough to metropolitan areas that rural residence captures nongeographic factors associated with lower use of hospice services. Suburban and rural areas that are not close to a metropolitan area were associated with lower hospice use. For these older adults with metastatic breast cancer, the lower hospice use was not associated with driving time. These findings suggest that lower hospice use in these areas may be attributed to lack of resources among hospice care health professionals. It is possible that lack of awareness, knowledge, and trust about hospice services among patients in these areas may also contribute to lower hospice use.
Increased hospice capacity associated with more use in local areas >70-minute drive
Local area per capita number of employees was significantly associated with hospice use in areas with driving times of 70 minutes or longer, but the number of Medicare-certified programs was not associated with hospice use in these areas. In areas requiring a 70-minute or longer drive that did not share boundaries with metropolitan areas, more staffing was associated with higher patient volume. Previous studies suggested that larger hospice programs were more likely to admit patients with fewer restrictions, such as patients receiving chemotherapy for both curative and palliative purposes.22 Many small hospices may suggest competition, but fewer larger hospices may improve access through a better array of services, such as monitoring pain and symptoms.8
Increased hospice capacity may be associated with the scale of business, with larger organizations able to admit patients with more costly needs, who then share the costs of care with a larger patient population. Increased hospice capacity may also be associated with specialization, which leads to a broader range of services that are potentially higher quality and may be more adaptable to diverse needs of the patient population.
The integrated interdisciplinary hospice care team is the foundation of individualized and holistic end-of-life care. In suburban and rural areas without neighboring metropolitan areas, there may be fewer health professionals available to collaborate with and to deliver team-based hospice care to patients' homes. More trained health professionals could operate with different expertise and offer their specific skill sets to improve patient access to preferred care. Greater numbers of trained health professionals could also amend gaps in patient care communication that are more prevalent among patients with cancer living in rural areas.23
Study limitations
Our study has several limitations. First, the SEER-Medicare data used in the analysis were not the most recent. Medicare Provider of Services files for 2011 and 2012 were missing key data documented in a recent report on ownership changes in hospice care,24 along with several updates of SEER-Medicare data occurred during the time. Moreover, considering the COVID-19 pandemic and its impact on provider burnout, it is likely that local area hospice staffing differences have been recently exacerbated. Further study on hospice workforce is underway using more recent national data. Second, our study population focused on older adults with metastatic breast cancer and did not include other cancer types or end-stage diseases, and it therefore limits generalizability. Third, not all patients necessarily received home-based hospice care.
Our analysis used driving time between the centroids of patient residence and the nearest Medicare-certified hospice program headquarter as a proxy measure for space and time that hospice staff may need to commute to provide hospice care. Driving mileage may better represent hospice staff efforts to travel from home to home in suburban and rural areas in future studies. Finally, our study did not differentiate the profit status of hospice programs, which has been shown to be negatively associated with admission of older adults with advanced cancer.9
Conclusions
Our study suggests that more research is needed to address suburban and rural communities' needs for end-of-life care that is not adequately met by local hospice and palliative care workforce, compared to urban areas. In suburban and rural areas with fewer hospice and palliative care professionals per capita, innovative delivery strategies leveraging interprofessional teams, telehealth, and technology can be developed to amplify patient-provider/provider-provider communications and reduce barriers in access to end-of-life care among ever-aging adult populations with serious illness.25
Acknowledgments
The authors acknowledge the input from Dr. John Brooks and Dr. Elizabeth Chrischilles during the early stage of the study. Dr. Tae Park, Dr. Mike Zdeb, and Dr. Francis Boscoe offered generous advice and insights into the calculation of driving time. The authors would like to thank Dr. Sharon Bigger, Dr. Peter Teichman, and other readers for their helpful comments on the article. All contributing authors meet the criteria for authorship and approved this version to be published. This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the National Cancer Institute; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database.
The collection of cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute's Surveillance, Epidemiology and End Results Program under contract HHSN261201000140C awarded to the Cancer Prevention Institute of California, contract HHSN261201000035C awarded to the University of Southern California, and contract HHSN261201000034C awarded to the Public Health Institute; and the Centers for Disease Control and Prevention's National Program of Cancer Registries, under agreement # U58DP003862-01 awarded to the California Department of Public Health. The authors acknowledge the efforts of the National Cancer Institute; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database.
Authors' Contributions
S.W. led the conceptualization of the study, data curation, formal analysis, investigation, and writing of the original draft. S.M.F. and J.S.K. provided mentorship and leadership responsibilities for the research activity. All listed authors have made substantial contributions to the interpretation and validation of data for the study. All listed authors have made substantial contributions to revising the draft critically for important intellectual content; approved the final version to be published; and agreed to be accountable for all aspects of the study in ensuring that questions related to the accuracy or integrity of any part of the study are appropriately investigated and resolved.
Disclaimer
The ideas and opinions expressed herein are those of the author(s) and endorsement by the State of California Department of Public Health, the National Cancer Institute, and the Centers for Disease Control and Prevention or their Contractors and Subcontractors is not intended nor should be inferred.
Funding Information
S.W. received a National Research Service Award T32 in Palliative Care and Aging (5T32AG044296) in supporting her time. Expenses of acquiring SEER-Medicare data were partially supported by a start-up from the University of Charleston, WV.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Carlson MD, Bradley EH, Du Q, et al. Geographic access to hospice in the United States. J Palliat Med 2010;13(11):1331–1338; doi: 10.1089/jpm.2010.0209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Meier DE. Increased access to palliative care and hospice services: Opportunities to improve value in health care. Milbank Q 2011;89(3):343–380; doi: 10.1111/j.1468-0009.2011.00632.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Medicare Payment Advisory Commission. March 2022 Report to the Congress: Medicare Payment Policy. Assessing payment adequacy and updating payments: Hospice services. 2022;361–406. Available from: https://www.medpac.gov/document-type/presentation [Last accessed: March 31, 2022]. [Google Scholar]
- 4. National Hospice and Palliative Care Organization. Hospice Facts and Figures: 2021. Edition. Available from: https://www.nhpco.org/wp-content/uploads/NHPCO-Facts-Figures-2021.pdf [Last accessed: July 22, 2021].
- 5. Medicare Payment Advisory Commission. March 2020 Report to the Congress: Medicare Payment Policy. 2020;325–364. Available from: https://www.medpac.gov/wp-content/uploads/import_data/scrape_files/docs/default-source/reports/mar20_entirereport_sec.pdf [Last accessed: September 31 2021].
- 6. Virnig BA, Ma H, Hartman LK, et al. Access to home-based hospice care for rural populations: Identification of areas lacking service. J Palliat Med 2006;9(6):1292–1299; doi: 10.1089/jpm.2006.9.1292 [DOI] [PubMed] [Google Scholar]
- 7. Virnig BA, Moscovice IS, Durham SB, et al. Do rural elders have limited access to Medicare hospice services? J Am Geriatr Soc 2004;52(5):731–735; doi: 10.1111/j.1532-5415.2004.52213.x [DOI] [PubMed] [Google Scholar]
- 8. Aldridge MD, Epstein AJ, Brody AA, et al. The impact of reported hospice preferred practices on hospital utilization at the end of life. Med Care 2016;54(7):657–663; doi: 10.1097/MLR.0000000000000534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wachterman MW, Marcantonio ER, Davis RB, et al. Association of hospice agency profit status with patient diagnosis, location of care, and length of stay. JAMA 2011;305(5):472–479; doi: 10.1001/jama.2011.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Keating NL, Herrinton LJ, Zaslavsky AM, et al. Variations in hospice use among cancer patients. J Natl Cancer Inst 2006;98(15):1053–1059; doi: 10.1093/jnci/djj298 [DOI] [PubMed] [Google Scholar]
- 11. Aldridge MD, Hasselaar J, Garralda E, et al. Education, implementation, and policy barriers to greater integration of palliative care: A literature review. Palliat Med 2016;30(3):224–239; doi: 10.1177/0269216315606645 [DOI] [PubMed] [Google Scholar]
- 12. Lupu D. Estimate of current hospice and palliative medicine physician workforce shortage. J Pain Symptom Manage 2010;40(6):899–911; doi: 10.1016/j.jpainsymman.2010.07.004 [DOI] [PubMed] [Google Scholar]
- 13. Roberts D, Hurst K. Evaluating palliative care ward staffing using bed occupancy, patient dependency, staff activity, service quality and cost data. Palliat Med 2013;27(2):123–130; doi: 10.1177/0269216312447593 [DOI] [PubMed] [Google Scholar]
- 14. Dudley N, Chapman S, Spetz J. Community-based palliative care leader perspectives on staffing, recruitment, and training. J Hosp Palliat Nurs 2018;20(2):146–152; doi: 10.1097/NJH.0000000000000419 [DOI] [PubMed] [Google Scholar]
- 15. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann Intern Med 2007;147(8):573–577; doi: 10.7326/0003-4819-147-8-200710160-00010 [DOI] [PubMed] [Google Scholar]
- 16. Dinan MA, Curtis LH, Setoguchi S, et al. Advanced imaging and hospice use in end-of-life cancer care. Support Care Cancer 2018;26(10):3619–3625; doi: 10.1007/s00520-018-4223-0 [DOI] [PubMed] [Google Scholar]
- 17. Wang SY, Hall J, Pollack CE, et al. Trends in end-of-life cancer care in the Medicare program. J Geriatr Oncol 2016;7(2):116–125; doi: 10.1016/j.jgo.2015.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zdeb M. Driving distance and driving times using SAS and Google Maps. SAS Global Forum. 2010. Available from: https://support.sas.com/resources/papers/proceedings10/050-2010.pdf [Last accessed: September 1, 2019].
- 19. Becker GS. The Economic Approach to Human Behavior. Chicago, IL: University of Chicago Press; 1978. [Google Scholar]
- 20. Tonelli M, Klarenbach S, Rose C, et al. Access to kidney transplantation among remote- and rural-dwelling patients with kidney failure in the United States. JAMA 2009;301(16):1681; doi: 10.1001/jama.2009.545 [DOI] [PubMed] [Google Scholar]
- 21. Wang F, Luo W. Assessing spatial and nonspatial factors for healthcare access: Towards an integrated approach to defining health professional shortage areas. Health Place 2005;11(2):131–146; doi: 10.1016/j.healthplace.2004.02.003 [DOI] [PubMed] [Google Scholar]
- 22. Lorenz KA, Asch SM, Rosenfeld KE, et al. Hospice admission practices: Where does hospice fit in the continuum of care? J Am Geriatr Soc 2004;52(5):725–730; doi: 10.1111/j.1532-5415.2004.52209.x [DOI] [PubMed] [Google Scholar]
- 23. Walling EB, Fiala M, Connolly A, et al. Challenges associated with living remotely from a pediatric cancer center: A qualitative study. J Oncol Pract 2019;15(3):e219–e229; doi: 10.1200/JOP.18.00115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Stevenson D, Krone E, Meneades L, et al. Tracking the impact of ownership changes in hospice care provided to Medicare beneficiaries: Final report. Office of the Assistant Secretary for Planning and Evaluatyion. 2017. Available from: https://aspe.hhs.gov/reports/tracking-impact-ownership-changes-hospice-care-provided-medicare-beneficiaries-final-report-0 [Last accessed: September 31, 2021].
- 25. Purnell TS, Calhoun EA, Golden SH, et al. Achieving health equity: Closing the gaps in health care disparities, interventions, and research. Health Aff (Millwood) 2016;35(8):1410–1415; doi: 10.1377/hlthaff.2016.0158 [DOI] [PubMed] [Google Scholar]