Abstract
Background:
Different sets of barriers have been identified to explain the difficulties in the access and availability of opioid analgesics in palliative care, particularly in low- and middle-income countries, including Latin America.
Objective:
To validate a structured questionnaire for the access to opioid medicines and to investigate the perception of health professionals regarding access barriers to opioid analgesics in 17 countries of the Latin American Region.
Design:
Survey to identify the domains and barriers of access to opioid medicines according to health professionals, including physicians, nurses, and pharmacists affiliated to institutions that provide palliative care in Latin America between August 2019 and October 2020.
Results:
We analyzed responses from 426 health professionals. The median age was 44 years old (ranging from 23 to 73 years) with an average experience in palliative care of 10 years (range: 1–35), 71.8% were women, and 49.8% were affiliated to specialized health care facilities of urban areas (94.6%). The main barriers perceived to be extremely relevant by the respondents were “belief that patients can develop addiction” and “financial limitations of patients” for the patient's domain and the “appropriate education, instruction, and training of professionals” for health professional's domain.
Conclusions:
It is necessary to develop strategies to strengthen less-developed health systems of the region to review legal frameworks, ensure integrated palliative care systems, and deploy multidisciplinary strategies for sensitizing, training, and raising the awareness of patients, caregivers and, particularly, health professionals regarding appropriate prescription and rational use of opioid analgesics.
Keywords: analgesics opioid, essential medicines, health services accessibility, Latin America, opioid epidemic, palliative care
Introduction
Palliative care is part of the core components of the human right to health and universal health coverage because it ensures comprehensive care and contributes to relieving the suffering associated with advanced illness.1
Every year, ∼56.8 million people require palliative care, of whom about 80% are adults living in low- and middle-income countries.2,3 By 2060, the need for palliative care may double due to the aging of the population, the increased incidence of noncommunicable chronic diseases, and the health emergency caused by COVID-19.3 In 2014, the World Health Assembly, invited the member states to strengthen palliative care in their countries, including strategies to ensure availability and accessibility to opioid analgesics and essential medicines.4
Aggregate data on opioid consumption showed that the United States and Canada consumed ∼82% of the whole reported opioid consumption in the Region of the Americas. Therefore, a high contrast emerges between suggesting a potential overuse in high-income countries and a severe underuse in less wealthy countries of the Region.2,5–7
In Latin America, it is estimated that over 3.5 million people may require palliative care and pain relief, but only 7.6% will receive it.5,6 However, the distributed opioid morphine equivalent (DOME) also shows geographical variability: while countries such as Chile and Argentina report higher consumption (26.3 and 17.1 DOME/per capita, respectively), countries such as Venezuela, Bolivia, and Honduras report alarmingly low figures (0.2, 0.9, and 1.0 DOME/per capita, respectively).7,8
Different sets of barriers have been identified to explain the existing complications in the access and availability of opioid analgesics,3,7,9 including certain public policies, restrictive laws and regulations, an exaggerated fear of addiction, insufficient training of health professionals, and the lack of political support.3,8,10 Additionally, components associated with behaviors, knowledge, and practices of health professionals providing palliative care have also been described as barriers.11,12
For the abovementioned reasons and in accordance with WHO (World Health Organization) and PAHO (Pan American Health Organization) global and regional resolutions on palliative care,13 this work aims to investigate the concerning barriers of access to opioid analgesics by health professionals in 17 countries of the Latin American region to provide the basis on which to build strategies to overcome the identified barriers.
Materials and Methods
This study included the design and validation of a structured questionnaire as a tool to identify domains and barriers of access to opioid medicines, intended for health professionals experienced in providing palliative care in Argentina, Bolivia, Chile, Colombia, Costa Rica, Ecuador, El Salvador, Guatemala, Honduras, Mexico, Nicaragua, Panama, Paraguay, Peru, Dominican Republic, Uruguay, and Venezuela.
The study was approved by the Pan American Health Organization Ethics Review Committee. The study protocol is available for consultation upon request.
Questionnaire design
To develop the survey questionnaire, a literature review was carried out based on a search in the following databases: Medline. EMBASE, SCOPUS, WHOLIS, Scielo, Cochrane Pain, Palliative and Supportive Care, and Cochrane Central in March 2017.
Questions from previously implemented and validated questionnaires found in the literature were included,7,9,14 as well as questions regarding the context of the Latin American region, for a total of 40 questions. The questionnaire was divided into three sections: (1) sociodemographic data of participants; (2) information on the opioid analgesic treatments used; and (3) situation regarding the access to opioid analgesics and palliative care, including barriers and solutions. Acknowledging the cultural and linguistical differences among Latin American countries and to avoid misunderstandings, the questionnaire included technical terms and key words common to all health professionals.
The questionnaire validation process concerning coverage, relevance, and clarity characteristics was carried out with the consensus of nine experts from seven countries of the region (Mexico, Panama, Colombia, Costa Rica, Ecuador, El Salvador, and Paraguay) Despite the fact that the number of experts is not established for this kind of validations, many studies include a minimum of 8–10 participants.15,16
The selection of the nine participants for the consensus was made by convenience, considering the following inclusion criteria: (1) Health professionals, including physicians, nurses, and pharmacists; (2) affiliated to institutions that provide palliative care in Latin America in the last five years; and (3) minimum experience of five years on palliative care/attention. Additionally, one expert with profile and experience as an editor was invited to the validation, to evaluate the appearance of the instrument in terms of clarity, understandability, and cultural specificities of the questionnaire. The experts were contacted by e-mail and the validation process was carried out in REDCap, an electronic data collection tool.17,18
The validation process enabled adjustment of the wording of questions and restructuring of the three sections of the questionnaire. A copy of the original questionnaire is included as Supplementary Material S1.
Survey design and participators
The questionnaire was applied between August 2019 and October 2020 to health professionals, including physicians, nurses, and pharmacists with the following inclusion criteria: (1) affiliated to institutions that provide palliative care in Latin America, (2) provided palliative care/attention in the last three years, and (3) voluntarily accepted to participate. Participants were identified through PAHO local offices, Ministries, or Secretariats of Health; palliative care or pain relief associations; and palliative care hospital programs of participating countries. Participants were contacted and invited to answer the survey by e-mail and the link to access the informed consent and questionnaire was sent afterward.
Questionnaire answers were collected and managed using REDCap,17,18 with regular follow-up and e-mail reminders sent to the participants every two weeks.
Analysis
A descriptive analysis of sociodemographic characteristics (sections 1 and 2 of the questionnaire) was made using summary measures and frequency distribution tables, depending on the level of measurement of each characteristic. The program used for data statistical analysis was Stata 17.0.
For data analysis, answers were stratified according to the following geographic zones (subregions):
Southern Cone: Argentina, Uruguay, Paraguay, and Chile.
Andean Region: Colombia, Peru, Ecuador, Bolivia, and Venezuela.
Central America and the Caribbean: Costa Rica, Guatemala, El Salvador, Honduras, Nicaragua, Panama, and Dominican Republic.
North America: Mexico.
The questions in section 3: Situation of the access to opioid analgesics and palliative care were structured as barriers to access and classified in three different domains according to the literature reviewed: barriers related to patients, barriers related to health professionals, and barriers related to the health system. Likewise, classifications according to types of barriers were considered to ease analysis and discussion.
For the selected questions, 95% confidence intervals were constructed for the proportion of individuals reporting that item as a barrier to access.
Based on estimated proportions, barriers were classified into quartiles: those with a proportion higher than 75% were considered extremely relevant and those with a proportion between 50% and 75% were considered highly relevant. A traffic-light system was proposed to facilitate the readability of relevance levels.
A statistical analysis was performed using the chi-square test to identify possible differences in responses (with 95% of confidence) and based on five criteria: differences by gender, age group, profession, years of experience, and institution.
Possible solutions to overcome the identified barriers to access were categorized as proposed by The Lancet Commission on Palliative Care and Pain Relief.5 One of the authors categorized each solution within the established options and this classification was reviewed independently by a second author (Table 1).
Table 1.
Categorization of Solutions
| Category | Refers to solutions, including |
|---|---|
| Priority setting |
 Establishment of public policies related to palliative care Establishment of public policies related to palliative care Political will Political will Creation of communication campaigns for the general public. Creation of communication campaigns for the general public. |
| Planning |
 Development or strengthening of plans and programs for palliative care Development or strengthening of plans and programs for palliative care Development or strengthening of clinical practice guidelines Development or strengthening of clinical practice guidelines Inclusion of essential medicines for palliative care in national lists Inclusion of essential medicines for palliative care in national lists |
| Regulatory aspects |
 Creation or amendment of laws, standards, and regulations regarding palliative care Creation or amendment of laws, standards, and regulations regarding palliative care Establishment of sanctions Establishment of sanctions |
| Monitoring and assessment of performance |
 Follow-up, assessment, and control of the implementation of national palliative care programs and plans Follow-up, assessment, and control of the implementation of national palliative care programs and plans |
| Intersectoral support |
 Proposals to connect all the involved players in the provision of palliative care Proposals to connect all the involved players in the provision of palliative care |
| Funding |
 Inclusion of palliative care interventions in the chart of essential or free services of the country Inclusion of palliative care interventions in the chart of essential or free services of the country Guarantee budget or investment for providing palliative care Guarantee budget or investment for providing palliative care Establishment of purchase agreements and enough purchases to satisfy the demand for opioid medicines. Establishment of purchase agreements and enough purchases to satisfy the demand for opioid medicines. |
| Strengthening of distribution and delivery |
 Inclusion of palliative care and pain treatment at all levels of care Inclusion of palliative care and pain treatment at all levels of care Implementation of quality assurance measures Implementation of quality assurance measures Adequate supply chain Adequate supply chain |
| Strengthening of human resources |
 Training of health professionals Training of health professionals Increase reserve of trained health care professionals Increase reserve of trained health care professionals |
| Information & research |
 Incorporation of palliative care follow-up indicators Incorporation of palliative care follow-up indicators Funding of palliative care research Funding of palliative care research |
Results
Sample description
A total of 874 health professionals were invited to answer the questionnaire. As of October 2020, 426 surveys (48.7%) were collected. Of the total respondents, 71.8% were women and 28.2% men; average age was 44 years old (ranging from 23 to 73 years). The type of institutions where professionals worked was mainly specialized health care facilities (49.8%); the institutions were primarily located in urban areas (94.6%); and the countries with the highest proportion of answers were Chile (11.74%), Colombia (11.74%), and Mexico (11.27%). Most respondents were palliative care specialized physicians (49.4%), and their average experience in palliative care was 10 years (range: 1–35) (Table 2). Information about the prescribed opioid analgesics is annexed as Supplementary Material S2. From the 426 total respondents, 306 (72%) provided complete responses to all 40 questions of the survey. The maximum number of unanswered key questions was 4.
Table 2.
Sociodemographic Characteristics of Participants
| Country of origin | Argentina | 7.3% (31) | Mexico | 11.3% (48) |
| Bolivia | 4.2% (18) | Nicaragua | 1.4% (6) | |
| Chile | 11.7% (50) | Panama | 4.7% (20) | |
| Colombia | 11.7% (50) | Paraguay | 3.1% (13) | |
| Costa Rica | 7.3% (31) | Peru | 5.4% (23) | |
| Ecuador | 6.8% (29) | Dominican Rep. | 3.3% (14) | |
| El Salvador | 3.5% (15) | Uruguay | 5.4% (23) | |
| Guatemala | 3.1% (13) | Venezuela | 7.0% (30) | |
| Honduras | 2.8% (12) | |||
| Gender | Female | 71.8% (306) | ||
| Male | 28. 2% (120) | |||
| Age | 23–33 Years | 12.2% (52) | ||
| 34–43 Years | 44.1% (188) | |||
| 44–53 Years | 24.2% (103) | |||
| 54–63 Years | 15.7% (67) | |||
| 64–73 Years | 3.8% (16) | |||
| Facility | Primary health care level | 8.9% (38) | ||
| Secondary health care level | 12.4% (53) | |||
| Tertiary health care level | 24.2% (103) | |||
| Specialized health care | 49.3% (210) | |||
| Othersa | 4.2% (18) | |||
| No answer | 0.94% (4) | |||
| Geographic area of the institution | Urban | 94.6% (403) | ||
| Rural | 5.4% (23) | |||
| Profession/medical specialty | Nursing | 12.9% (55) | ||
| Pharmacy | 4.2% (18) | |||
| General/family practice | 9.8% (42) | |||
| Medicine specialized in palliative care | 49.3% (210) | |||
| Specialized medicineb | 23.5% (100) | |||
| No answer | 0.23% (1) | |||
| Years of experience | 1–5 | 33.3% (142) | ||
| 6–10 | 29.3% (125) | |||
| 11–15 | 18.3% (78) | |||
| 16–20 | 10.6% (45) | |||
| 21–25 | 4.5% (19) | |||
| 26–30 | 2.8% (12) | |||
| 31–35 | 0.5% (2) | |||
| No answer | 0.7% (3) | |||
Description of Others: Private institution, academy, home care, nonprofit foundations, health management, ministry of public health.
Description of specialties: family medicine, internal medicine, oncology, hematological oncology, geriatrics, pediatrics, radiotherapy, surgery, anesthesiology, pain management, nephrology.
Barriers of access related to patients
The barriers of access identified as extremely relevant at the regional level were those related to cultural and social aspects concerning pain treatments, specifically, patients' beliefs that the consumption of opioids may be addictive, as well as financial limitations for their procurement. The highly relevant barriers were the fear of experiencing adverse effects, the reluctance of patients and caregivers to be prescribed opioid medicines, in addition to difficult geographical access, and difficult or extremely difficult procurement of medicines (Table 3).
Table 3.
Barriers of Access Related to Patients
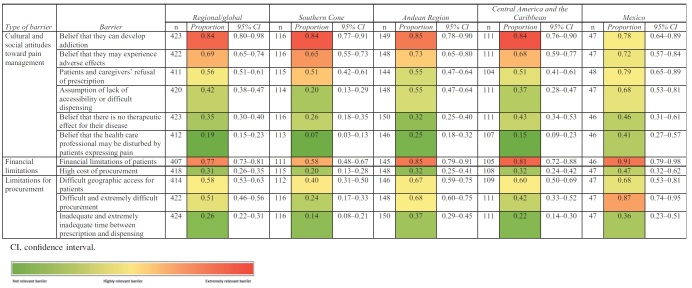
|
Barriers of access related to health professionals
The extremely relevant barriers identified at regional level were those associated with the lack of trained professionals, inadequate education, lack of training regarding opioid prescription, and inadequate assessment of pain, fear of dependence, and reluctance to prescribing (Table 4).
Table 4.
Barriers Related to Health Professionals
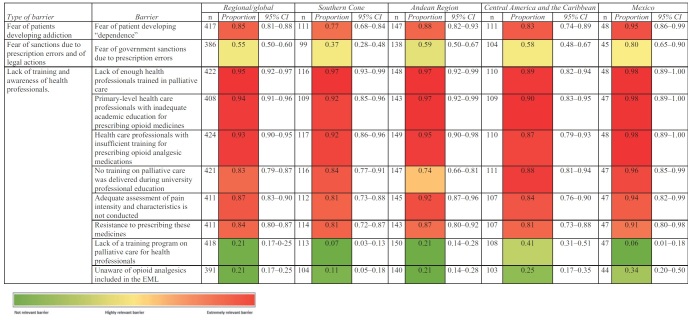
|
At a subregional level, the fear of government sanctions due to prescription errors was reported as extremely relevant, particularly in Mexico, and as highly relevant in the Andean Region and in Central America and the Caribbean. In the Southern Cone, this was not reported as relevant. Except in this case, global results for this domain were, in general, common to all the analyzed subregions.
Barriers of access related to the health care system
All the subregions reported the lack of campaigns to raise awareness and educate the population on the rational use of opioid analgesics as extremely relevant barriers, as well as the limited geographic access for the purchase of opioid medicines (Table 5). Some of the most important highly relevant barriers at regional level were lack of availability at the dispensing establishment; inadequate supply chain and inventory management; shortage of opioid medicines in the market; lack of public policies supporting the provision of palliative care; and local or national regulations restricting accessibility.
Table 5.
Barriers Related to the Health System
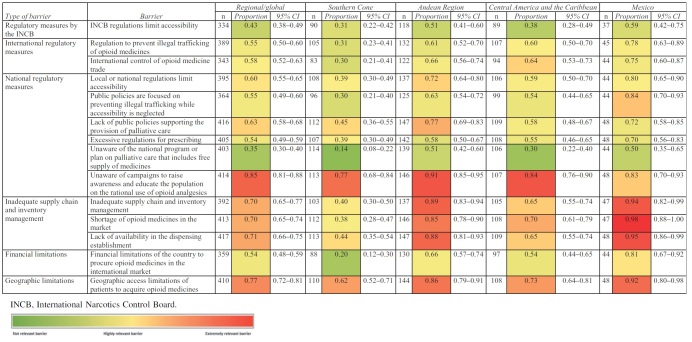
|
Analysis by subregions
Mexico is the subregion that reported most of the barriers as extremely relevant (21/37) and six barriers as highly relevant (6/37). It was also the subregion that reported the greatest number of extremely relevant barriers in the domain associated to the health system.
The Andean subregion reported the second highest number of extremely relevant (14/37) or highly relevant barriers (13/37). Most extremely relevant barriers are those related to health professionals and inadequate supply chain and inventory management. This subregion was the only one that reported the absence of public policies supporting the provision of palliative care as an extremely relevant barrier (77%). Additional highly relevant barriers in regional results were related to the health system.
In the Central America and Caribbean subregion, extremely relevant barriers (10/37) fell mostly in the domain of health professionals. Highly relevant barriers (15/37) reported were particularly associated with the health system. In this subregion, the “Difficult and extremely difficult procurement” barrier was reported as 40%, lower than in other subregions.
The Southern Cone reported the lowest number of barriers in the extremely (9/37) or highly relevant (3/37) categories. Extremely relevant barriers were almost exclusively in the domain associated with health professionals. Compared with the other subregions, two barriers were less reported: fear of government sanctions due to prescription errors (37%) and financial limitations of patients for procurement (58%). For the domain of barriers related to the health system, “not acquainted with campaigns to raise awareness and educate the population on the rational use of opioid analgesics” was the only barrier reported as extremely relevant (77%).
For the statistical analysis performed, among the categories included, age group and profession held the most significative differences, 34.15% and 48.57%, respectively.
Potential solutions
Figure 1 shows the categories of solutions identified. In general, it can be observed that solutions are mainly categorized according to aspects related to strengthening human resources, strengthening medicine supply chains, establishing or setting priorities, and regulatory aspects.
FIG. 1.
Categorization of solutions.
Discussion
This is the first study carried out in Latin America providing results derived from a structured questionnaire for diagnosing barriers of access to opioid analgesics from the health care professionals' perspective.
The barriers herein identified in relation to the lack of education and communication strategies for patients, professionals, and other stakeholders have already been described by the WHO and the International Narcotics Control Board (INCB) as one of the challenges to be overcome to strengthen palliative care and access to opioid medicines.19,20
Health professionals consider the barriers related to cultural and social attitudes of patients and caregivers toward pain management to be extremely and highly relevant aspects, particularly the belief that these medicines may cause adverse effects and addiction. This situation has already been described in the literature as an obstacle for the appropriate use of opioid medicines.12,21
Regarding the “fear of developing addiction,” this barrier was consistently reported among the regions evaluated (above 70% within prescribers), showing an important awareness about the possibility of this undesirable outcome. An additional evaluation would be required to assess to what extent this might also contribute to prescription restrictions of opioids. The barriers to access identified for the health professionals' domain, according to the respondents' perception, are those that need more urgent intervention. Similar research conducted in other regions is consistent with this study regarding inadequate knowledge, skills, and training of health professionals on the use of opioid analgesics.9,11,22 WHO states that palliative care should be available at all levels of health care.2 Therefore, strengthening the education of all human resources involved in palliative care is crucial, particularly at the level of primary care, where palliative care specialists tend to be lacking.
According to the respondents, there is no adequate education on palliative care during undergraduate education, which is confirmed by the information of the Atlas of Palliative Care in Latin America, which reports that only 15% of medical schools offer palliative care as a separate subject.8
Eight of the 19 countries recognize palliative medicine as a specialty and, also, postgraduate programs exist such as degrees, master's degrees, and courses in several countries.8 However, the participants perceive a lack of health professionals trained in palliative care. This means that, in spite of the efforts, specialists are still insufficient.23
Regarding barriers related to the health system, one of the barriers to access identified as extremely relevant is the lack of knowledge about campaigns to raise awareness and educate the population on the rational use of opioid analgesics. This finding is in line with the conclusions reached for the domains associated to patients and health professionals.
Another barrier characterized as extremely relevant concerns the geographic limitations that make access to opioid analgesics difficult or impossible. This barrier is characteristic of low- and middle-income countries where rural and remote areas are more common.24 Improving this aspect also implies integrating palliative care into the primary health care level.25
National and international regulatory measures and inadequate supply chains have also been defined as relevant barriers. These results add to previous studies conducted in the region describing regulatory barriers such as excessive restrictions for prescribing and dispensing as well as limited availability.7 Establishing palliative care as a priority of the public health policy and research agenda, turning restrictive national regulations into standards, plans, and programs focused on patients' needs may help overcome these barriers.24
The relevance of barriers to access related to the health system presents greater differences among subregions. These differences may be due to the large variability in economic and social aspects and, therefore, in the development of palliative care in Latin America.7 Most countries analyzed in this study have limitations to guarantee the inclusion of palliative care in the health care system. Just a few countries (e.g., Chile, Costa Rica, Uruguay, among others), have made significant advances in this process.6,26,27
Regarding the 35 barriers reported, almost half of the comparisons by profession were statistically significant. The proportion of participant nurses and pharmacists was significantly lower. These differences could be explained based on the academic, educational, and professional background of the individuals surveyed. Physicians, nurses, and pharmacists are a very heterogeneous group of people with different training, experience, and roles regarding patient's care; therefore, their perception about access to opioids may be different.11
The proposals made by the interviewed health professionals are consistent with the public health approach for the development of palliative care based on 4 components: education, availability, implementation, and public policy.21,28,29
Limitations
The nonrandom selection of participants and the response rate may affect the representativeness of the results in this study. Nevertheless, the response rate of 47% achieved in the present study is above the expected for online surveys and could be a result of the follow-up strategy.30,31 Response rates for similar previously published studies in the same context, potentially allowing comparisons, were not identified.
Data were not collected from the population that did not agree to participate; hence, it is not possible to assess the differences in their profiles, in comparison to the respondents. This may represent a possible source of selection bias. Additionally, most of the professionals who participated in the survey work in urban areas, which, in general, have better access to opioid analgesics. It is possible that professionals from rural or remote areas may perceive additional barriers or others having an even higher intensity.
The relevance established for the barriers may be subjective and their potential interventions will mainly depend on the perspective and the needs of each of the parties involved in the provision of palliative care, available resources, and the priorities of public health policies.
Conclusions
The main barriers of access to opioid analgesics perceived by health professionals are related to the lack of knowledge, skills, and training of health professionals, patients, and other parties involved in the provision of palliative care. At the same time, aspects concerning geographic limitations and restrictive regulatory aspects are highlighted.
It is necessary to develop strategies that allow strengthening the less developed health care systems of the region to review regulatory frameworks, ensure integrated palliative care systems, and establish multidisciplinary strategies that enable sensitizing, training, and raising awareness of patients, caregivers and, particularly, health professionals.
Supplementary Material
Acknowledgments
The authors wish to express their special gratitude to the Asociación Latinoamericana de Cuidados Paliativos (ALCP) and the following national associations and health professionals for their help in contacting respondents:
Colombia: Observatorio Colombiano de Cuidados Paliativos.
Argentina: Dr. Nicolas Dawidowicz and Dr. Roberto Daniel Wenk.
Guatemala: Dr. Marisol Bustamante and Dr. Silvia Rivas de Verdugo.
Bolivia: Dr. Mirna García Burgoa—Asociación Alianza Boliviana de Cuidados Paliativos and Els Van Hoecke—SENTEC.
Mexico: Dr. Uria Guevara, Dr. Anahí Cristina Dreser, Dr. Luis Saucedo, and Dr. Celina Castañeda
Costa Rica: Dr. Andrea Medina—ASOPALLIUM, Dr. María José Morales—ASOPALLIUM, Dr. Nuria Montero, and Dr. Andrea Rodríguez Hernández.
Venezuela: Dr. Tulio Wladimir Gonzalez Coronel.
Ecuador: Dr. Tatiana Fernández—Asociación Ecuatoriana de Cuidados Paliativos (AECP).
Chile: Dr. Alfredo Rodriguez, Dr. Marcela Barrier, Lea Derio.
Panama: Dr. Bruna Chin, Dr. Milagros Cubilla, Dr. Nisla Camaño-Asociación Panameña de Cuidados Paliativos.
The team thanks all the health professionals who participated in this study as well as the focal points of PAHO/WHO national offices for their support in the referral of contacts.
Authors' Contributions
All authors participated in the concept, methodology, validation, formal analysis, investigation, writing, and/or revision of the article.
Disclaimer/License
R. R.-C., J.F., A.P., S.L., and J.L.C. are a staff members of the Pan American Health Organization (PAHO). The author alone is responsible for the views expressed in this publication, and they do not necessarily represent the decisions or policies of the PAHO. In any reproduction of this article, there should not be any suggestion that PAHO, or this article endorse any specific organization or products.
Funding Information
Regular budget of the Pan American Health Organization/World Health Organization.
Author Disclosure Statement
No competing financial interests exist.
Supplementary Material
References
- 1. Pereira Arana I: El abordaje de la atención en salud desde un enfoque de derechos humanos (The approach to health care from a human rights perspective). Bogotá, DC: De Justicia, 2016. Report No.: 26. [Google Scholar]
- 2. Organización Mundial de la Salud: Cuidados Paliativos (World Health Organization: Palliative Care) [Online]: 2020 [cited Septiembre 25, 2021. https://www.who.int/es/news-room/fact-sheets/detail/palliative-care (Last accessed September 15, 2021).
- 3. Worldwide Hospice Palliative Care Alliance: Global Atlas of Palliative Care, Segunda edición. Londres: Reino Unido, 2020 [Google Scholar]
- 4. Asamblea Mundial de la Salud: Strengthening of palliative care as a component of comprehensive care throughout the life course. Resolución 2014, Document Number WHA67.19. [Google Scholar]
- 5. Knaul F, Farmer P, Krakauer E, et al. : Alleviating the access abyss in palliative care and pain relief—An imperative of universal health coverage: The Lancet Commission report. Lancet 2018;391:1391–1454. [DOI] [PubMed] [Google Scholar]
- 6. Pastrana T, and De Lima L: Palliative care in Latin America: Are we making any progress?. J Pain Symptom Manage 2021. [DOI] [PubMed] [Google Scholar]
- 7. Cleary J, De Lima L, Eisenchlas J, et al. : Formulary availability and regulatory barriers to accessibility of opioids for cancer pain in Latin America and the Caribbean: A report from the Global Opioid Policy Initiative (GOPI). Ann Oncol 2013;24 Suppl 11:xi41–xi50. [DOI] [PubMed] [Google Scholar]
- 8. Pastrana T, De Lima L, Sánchez-Cárdenas M, et al. : Atlas de Cuidados Paliativos en Latinoamérica 2020 (Atlas of Palliative Care in Latin America 2020), 2nd ed. Houston: IAHPC Press, 2021. [Google Scholar]
- 9. Berterame S, Erthal J, Thomas J, et al. : Use of and barriers to access to opioid analgesics: A worldwide, regional, and national study. Lancet 2016;387:1644–1656. [DOI] [PubMed] [Google Scholar]
- 10. Leon MX, De Lima L, Florez S, et al. : Improving availability of and access to opioids in Colombia: Description and preliminary results of an Action Plan for the Country. J Pain Symptom Manage 2009;38:758–766. [DOI] [PubMed] [Google Scholar]
- 11. Hyun JJ, Yeol K, Kyung AK, et al. : Knowledge, practices, and perceived barriers regarding cancer pain management among physicians and nurses in Korea: A Nationwide Multicenter Survey. PLoS One 2014;9:e105900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kwon JH: Overcoming barriers in cancer pain management. J Clin Oncol 2014;32:1727–1733. [DOI] [PubMed] [Google Scholar]
- 13. Organización Panamericana de la Salud: Strategy for Universal Access to Health. Washington, DC, 2014. [Google Scholar]
- 14. Lima L, Pastrana T, Radburch L, et al. : Cross-sectional pilot study to monitor the availability, dispensed prices, and affordability of opioids around the globe. J Pain Symptom Manage 2014;48:649–659.e1. [DOI] [PubMed] [Google Scholar]
- 15. Ogbeifun E, and Agwa-Ejon J: The Delphi technique: A credible research methodology. Proceedings of the 2016 International Conference on Industrial Engineering and Operations Management. Kuala Lumpur, Malaysia, March 8–10, 2016. [Google Scholar]
- 16. Hsu CC, Sandford BA: The Delphi technique: Making sense of consensus. Pract Assess Res Eval 2007;12:1–8. [Google Scholar]
- 17. Harris P, Taylor R, Thielke R, et al. : Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Harris P, Taylor R, Minor B, et al. ; REDCap Consortium. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Organización Mundial de la Salud: Strengthening of Palliative Care as a Component of Integrated Treatment Throughout the Life Course—Report by the Secretariat. Executive Board. Session 134th, 2013. Report No.: Item 9.4. [Google Scholar]
- 20. Junta Internacional de Fiscalización de Estupefacientes. Progresos en lo que respecta a garantizar el acceso adecuado a sustancias sujetas a fiscalización internacional para fines médicos y científicos (International Narcotics Control Board. Progress in ensuring adequate access to internationally controlled substances for medical and scientific purposes). Viena: Naciones Unidas, 2019. [Google Scholar]
- 21. Hawley P: Barriers to Access to Palliative Care. Palliat Care 2017;10:1178224216688887; doi: 10.1177/1178224216688887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Vranken MJ, Linge-Dahl L, Mantel-Teeuwisse AK, et al. : The perception of barriers concerning opioid medicines: A survey examining differences between policy makers, healthcare professionals and other stakeholders. Palliat Med 2020;34:493–503. [DOI] [PubMed] [Google Scholar]
- 23. Pastrana T, De Lima L, and Stoltenberg M, HP: Palliative medicine specialization in Latin America: A comparative analysis. J Pain Symptom Manage 2021;62:960–967. [DOI] [PubMed] [Google Scholar]
- 24. Abu-Odah H, Molassiotis A, and Liu J: Challenges on the provision of palliative care for patients with cancer in low- and middle-income countries: A systematic review of reviews. BMC Palliat Care 2020;19:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Recoche K, Lee S, O'Connor M, et al. : Building palliative care capacity in rural health: A collaborative approach. Aust Nurs Midwifery J 2014;21:38. [PubMed] [Google Scholar]
- 26. Lynch T, Connor S, and Clark D: Mapping levels of palliative care development: A global update. J Pain Symptom Manage 2013;45:1094–1106. [DOI] [PubMed] [Google Scholar]
- 27. Unit TEI: The 2015 Quality of Death Index Ranking Palliative Care Across the World. London: The Economist Intelligence Unit Limited, 2015. [Google Scholar]
- 28. Stjernswärd J, Foley K, and Ferris F: The public health strategy for palliative care. J Pain Symptom Manage 2007;33:486–493. [DOI] [PubMed] [Google Scholar]
- 29. Zuccaro S, Vellucci R, Sarzi-Puttini P, et al. : Barriers to pain management: Focus on opioid therapy. Clin Drug Investig 2012;32(Suppl 1):11–19. [DOI] [PubMed] [Google Scholar]
- 30. Nair CS, and Adams P: Survey platform: A factor influencing online survey delivery and response rate. Qual Higher Educ 2009;15:291–296. [Google Scholar]
- 31. Deutskens E, de Ruyter K, MW, and Oosterveld P: Response rate and response quality of Internet-Based Surveys: An experimental study. Market Lett 2004;15:21–36. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



