Abstract
Objective:
To evaluate changes in insulin pump use over two decades in a national U.S. sample.
Research Design and Methods:
We used data from the SEARCH for Diabetes in Youth study to perform a serial cross-sectional analysis to evaluate changes in insulin pump use in participants <20 years old with type 1 diabetes by race/ethnicity and markers of socioeconomic status across four time periods between 2001 and 2019. Multivariable generalized estimating equations were used to assess insulin pump use. Temporal changes by subgroup were assessed through interactions.
Results:
Insulin pump use increased from 31.7% to 58.8%, but the disparities seen in pump use persisted and were unchanged across subgroups over time. Odds ratio for insulin pump use in Hispanic (0.57, confidence interval [95% CI] 0.45–0.73), Black (0.28, 95% CI 0.22–0.37), and Other race (0.49, 95% CI 0.32–0.76) participants were significantly lower than White participants. Those with ≤high school degree (0.39, 95% CI 0.31–0.47) and some college (0.68, 95% CI 0.58–0.79) had lower use compared to those with ≥bachelor's degree. Those with public insurance (0.84, 95% CI 0.70–1.00) had lower use than those with private insurance. Those with an annual household income <$25K (0.43, 95% CI 0.35–0.53), $25K–$49K (0.52, 95% CI 0.43–0.63), and $50K–$74K (0.79, 95% CI 0.66–0.94) had lower use compared to those with income ≥$75,000.
Conclusion:
Over the past two decades, there was no improvement in the racial, ethnic, and socioeconomic inequities in insulin pump use, despite an overall increase in use. Studies that evaluate barriers or test interventions to improve technology access are needed to address these persistent inequities.
Keywords: Type 1 diabetes, Insulin pump, Socioeconomic status, Insurance coverage, Diabetes disparities
Introduction
The use of insulin pumps in the management of type 1 diabetes (T1D) has been associated with improved glycemic control,1 diabetes-related quality of life,2 treatment satisfaction,2 and lower diabetes distress.3,4 While the literature has demonstrated the value of diabetes technology, numerous cross-sectional studies also show consistent inequities in real-world access to these technologies.5–14 In 2009, the SEARCH for Diabetes in Youth study noted disparities in insulin pump use by race/ethnicity, reporting the use in those of Hispanic ethnicity to be half of those who identified as Non-Hispanic and White (NHW). In those who were Non-Hispanic and Black (NHB) or Asian, pump use was one-fifth of those who were NHW.
Furthermore, most insulin pump users were from families with annual household income >$50,000, who had parental education at the college level and beyond, and who had private health insurance.11 Many subsequent cross-sectional studies have confirmed these socioeconomic disparities in pump use.5–7,9 The literature also now demonstrates that racial and ethnic disparities persist independent of socioeconomic status and glycemic control.6,7,15
Over the past 20 years, as the prevalence of insulin pump use continues to rise16–18 in the setting of advances in technology, a wider range of available devices, and improvements in insurance coverage,19 it is important to evaluate whether these improvements in overall access to insulin pump technology have mitigated versus contributed to disparities in insulin pump use seen in racial-ethnic minorities and those of lower socioeconomic status. Still, there are little data in the United States evaluating this. To this end, the T1D Exchange is the only U.S. study that has described changes in insulin pump use over time, but the analysis spanned ∼8 years and did not report changes in racial-ethnic groups.20 This T1D Exchange study also used a composite measure of socioeconomic status, which does not allow for assessment of changes by specific individual-level socioeconomic factors such as education, income, and medical insurance status and type.
In this study, we used data from the population-based SEARCH for Diabetes in Youth study to evaluate temporal trends across almost 20 years of insulin pump technology use in youth with T1D in the United States, specifically evaluating changes in inequities between racial-ethnic groups and those who are socioeconomically disadvantaged by income, education, and medical insurance.
Research Design and Methods
SEARCH for diabetes in youth
The SEARCH for Diabetes in Youth Study was a multicenter, observational, population-based longitudinal cohort study of youth with diabetes. A detailed description of the SEARCH study methods has previously been published elsewhere.21,22 SEARCH study sites included Ohio, Colorado, Hawaii, South Carolina, and Washington, one site in Southern California, and Indian Health Service participants from Navajo Nation. Local IRBs at each of the clinical sites and at the SEARCH for Diabetes Coordinating Center provided Human Subjects approval for study implementation.
SEARCH included registry and cohort components. The registry study identified incident and prevalent cases of diabetes in children and young adults <20 years of age through the surveillance of a nationally representative sample of ∼6% of the U.S. population in this age range. Diabetes type was confirmed upon entry of the study by abstracting data from medical records or through provider referrals. The cohort component was developed to longitudinally assess diabetes complications, quality of and barriers to care, among other outcomes.22
The SEARCH 3 cohort study occurred during 2011–2015 and was developed by recruiting incident cases with at least 5 years of diabetes duration and prior participation in a SEARCH in-person visit. The SEARCH 4 cohort study occurred during 2016–2019 and followed a subset of the SEARCH 3 cohort (all with type 2 diabetes, all T1D who are racial-ethnic minorities, and a random sample of patients who were NHW with T1D) for an in-person visit and also incident cases from 2012, which had a registry baseline visit in SEARCH 3. The remainder of the SEARCH 3 cohort was invited to complete a survey only.
Data
We completed a serial cross-sectional analysis of all SEARCH participants with T1D who had data on insulin pump use in at least one of the following periods: Period 1 (2001–2005), Period 2 (2006–2010), Period 3 (2011–2015), and Period 4 (2016–2019). We included data acquired from both registry and cohort visits.
Data on sociodemographic and health measures were collected through the last participant surveys administered during each time period. For children <18 years, some components of the self-report surveys were completed by parents. The primary outcome of interest was insulin pump use. Patients were asked, “How do you take your insulin?” Those who responded to the multiple-choice answer with “pump only” or “pump and injections” were identified as pump users. This question was an addition to the initial SEARCH questionnaire in period 1 and so pump use may have not been ascertained in some of the enrollees during this period. Other measures included clinic site, age at diagnosis, body mass index, HbA1c, gender, age at visit, duration of diabetes, race and ethnicity, parental educational attainment, annual household income, and type of health insurance.
Race and ethnicity were summarized as Hispanic, Non-Hispanic and Black (NHB), Non-Hispanic and White (NHW), and Other races and Non-Hispanic (Other NH), which included Asian, Pacific Islander, American Indian, and other races and Non-Hispanic. For health insurance type, Medicaid, Medicare, and State or Federally funded health insurance programs were considered Public Insurance. Those who noted to have private-through work or purchased individually were considered to have Private insurance; all other insurance types (e.g., military, school based, tribe/Indian Health Services, unknown type) were categorized as Other Insurance.
Statistical analysis
Participant demographic and health characteristics were summarized using descriptive statistics. The frequency of pump use in each period was compared across levels of sociodemographic characteristics and health outcomes using chi-square tests for categorical variables and t-tests (or Mann–Whitney test, as appropriate) for continuous variables.
Multiple imputation of missing data was performed for household income, health insurance status, and education level, assuming a missing at random process using the fully conditional specification.23,24 Twenty imputed datasets were generated. Multivariable generalized estimating equations with a binomial distribution and a log link function were used to assess temporal trends in the probability of insulin pump use, accounting for repeated measures within individuals in each imputed dataset. Results were then combined to provide single parameter estimates for each predictor accounting for the missing data imputation.25,26 All models adjusted for age, gender, clinic, duration of diabetes, and separate models were run, which included interactions between periods and each of the four primary predictors: participant race/ethnicity, insurance type, income, and education. Model-based predicted marginal probability of pump use over time was calculated for each primary predictor.
SAS version 9.4 (SAS Institute, Cary, NC) was used for all analyses. An a priori alpha ≤0.05 was used to assess statistically significant differences between groups.
Results
Our study population included a total of 690 youth and young adults with T1D in 2001–2005, 1706 in 2006–2010, 2385 in 2011–2015, and 2257 in 2016–2019. The demographic characteristics of this population are described in Table 1. There was an increase in insulin pump users across all subgroups such that the prevalence of insulin pump users during this time increased from 31.7% in 2001–2005, to 48% in 2006–2010, 54.2% in 2011–2015, and 58.8% in 2016–2019. The odds ratio (OR) for pump use in 2016–2019 was 6.6-fold higher than pump use in 2001–2005 (P < 0.001).
Table 1.
Sample Characteristics
| Pump use | 2001–2005 |
2006–2010 |
2011–2015 |
2016–2019 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| User |
Nonuser |
P | User |
Nonuser |
P | User |
Nonuser |
P | User |
Nonuser |
P | |
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |||||
| Total, N | 187 (27) | 503 (73) | — | 769 (45) | 937 (55) | — | 1293 (54) | 1092 (46) | — | 1326 (59) | 931 (41) | — |
| Age at visita | 12 (8, 14) | 11 (7, 14) | 0.300 | 14 (10, 17) | 15 (11, 18) | 0.000 | 16 (13, 20) | 19 (15, 22) | 0.000 | 20 (17, 24) | 22 (19, 25) | <0.001 |
| Age at diagnosisa | 9 (6, 12) | 9 (5, 12) | 0.710 | 8 (5, 12) | 12 (6.3, 13) | 0.000 | 8 (5, 11) | 11 (7, 13) | 0.000 | 9 (5, 12) | 11 (8, 14) | <0.001 |
| Body mass index | 25 (22, 28) | 25 (23, 30) | 0.500 | 26 (23, 29) | 25 (22, 29) | 0.200 | 25 (22, 28) | 25 (22, 29) | 0.610 | 25 (22, 28) | 25 (22, 29) | 0.090 |
| A1C | 7.7 (7.2, 8.6) | 8.2 (7.5, 9.0) | <0.001 | 8.2 (7.4, 9.0) | 8.8 (7.8, 10.1) | <0.001 | 8.5 (7.7, 9.5) | 9.4 (8.2, 11.0) | <0.001 | 8.5 (7.5, 9.6) | 9.2 (7.8, 11.1) | <0.001 |
| Female | 81 (43) | 238 (47) | 0.350 | 386 (50) | 449 (48) | 0.350 | 669 (52) | 535 (49) | 0.180 | 703 (53) | 470 (51) | 0.240 |
| Clinic site | ||||||||||||
| SC | 43 (23) | 62 (12) | <0.001 | 163 (21) | 195 (21) | <0.001 | 251 (19) | 244 (22) | <0.001 | 224 (17) | 218 (23) | <0.001 |
| OH | 58 (31) | 67 (13) | 182 (24) | 124 (13) | 270 (21) | 168 (15) | 260 (20) | 144 (16) | ||||
| CO | 47 (25) | 192 (38) | 256 (33) | 274 (29) | 452 (35) | 318 (29) | 515 (39) | 252 (27) | ||||
| CA | 7 (4) | 33 (7) | 34 (4) | 151 (16) | 75 (6) | 175 (16) | 96 (7) | 178 (19) | ||||
| WA | 32 (17) | 149 (30) | 134 (17) | 193 (21) | 245 (19) | 187 (17) | 231 (17) | 139 (15) | ||||
| Race/ethnicity | ||||||||||||
| NHB | 3 (3) | 52 (10) | <0.001 | 34 (4) | 149 (16) | <0.001 | 64 (5) | 195 (18) | <0.001 | 76 (6) | 184 (20) | <0.001 |
| Hispanic | 5 (5) | 57 (11) | 38 (5) | 144 (15) | 99 (8) | 186 (17) | 123 (9) | 176 (19) | ||||
| Other NH | 1 (1) | 20 (4) | 10 (1) | 28 (3) | 27 (2) | 31 (3) | 32 (2) | 38 (4) | ||||
| NHW | 178 (95) | 374 (74) | 686 (89) | 616 (66) | 1103 (85) | 679 (62) | 1095 (83) | 532 (57) | ||||
| Parental education | ||||||||||||
| Did not graduate high school | 0 (0) | 24 (5) | <0.001 | 3 (0) | 53 (6) | <0.001 | 15 (1) | 74 (7) | <0.001 | 16 (1) | 73 (8) | |
| High school graduate | 14 (8) | 72 (14) | 63 (8) | 172 (18) | 84 (6) | 186 (17) | 119 (9) | 176 (19) | ||||
| Some college/AA degree | 55 (29) | 184 (37) | 211 (27) | 339 (36) | 378 (29) | 390 (36) | 321 (24) | 257 (28) | ||||
| Bachelor's degree or more | 118 (63) | 219 (44) | 486 (63) | 349 (37) | 810 (63) | 404 (37) | 815 (61) | 349 (37) | ||||
| Unknown | 0 (0) | 24 (5) | 3 (0) | 53 (6) | 15 (1) | 74 (7) | 16 (1) | 73 (8) | ||||
| Income | ||||||||||||
| <$25K | 16 (9) | 117 (23) | <0.001 | 99 (13) | 186 (20) | <0.001 | 173 (13) | 212 (19) | <0.001 | 187 (14) | 181 (19) | <0.001 |
| $25K–$49K | 51 (27) | 97 (19) | 129 (17) | 152 (16) | 214 (17) | 150 (14) | 187 (14) | 97 (10) | ||||
| $50K–$74K | 97 (52) | 172 (34) | 432 (56) | 285 (30) | 624 (48) | 246 (23) | 533 (40) | 184 (20) | ||||
| $75K+ | 11 (6) | 78 (16) | 44 (6) | 156 (17) | 127 (10) | 238 (22) | 129 (10) | 186 (20) | ||||
| Unknown | 12 (6) | 34 (7) | 61 (8) | 137 (15) | 151 (12) | 232 (21) | 249 (19) | 247 (27) | ||||
| Heath insurance | ||||||||||||
| Public | 14 (8) | 110 (22) | <0.001 | 83 (11) | 231 (25) | <0.001 | 199 (15) | 301 (28) | <0.001 | 166 (12) | 169 (18) | <0.001 |
| Private | 170 (91) | 375 (75) | 665 (86) | 645 (69) | 1028 (80) | 642 (59) | 1069 (81) | 604 (65) | ||||
| Other | 3 (2) | 6 (1) | 13 (2) | 16 (2) | 56 (4) | 62 (6) | 57 (4) | 65 (7) | ||||
| None | 0 (0) | 6 (1) | 7 (1) | 33 (4) | 7 (0) | 68 (6) | 11 (1) | 59 (6) | ||||
| Unknown | 14 (8) | 110 (22) | 83 (11) | 231 (25) | 199 (15) | 301 (28) | 166 (12) | 169 (18) | ||||
Median and interquartile range (IQR) are reported.
CA, California; CO, Colorado; NHB, Non-Hispanic and Black; NHW, Non-Hispanic and White; OH, Ohio; Other NH, Other race and Non-Hispanic; SC, South Carolina; WA, Washington.
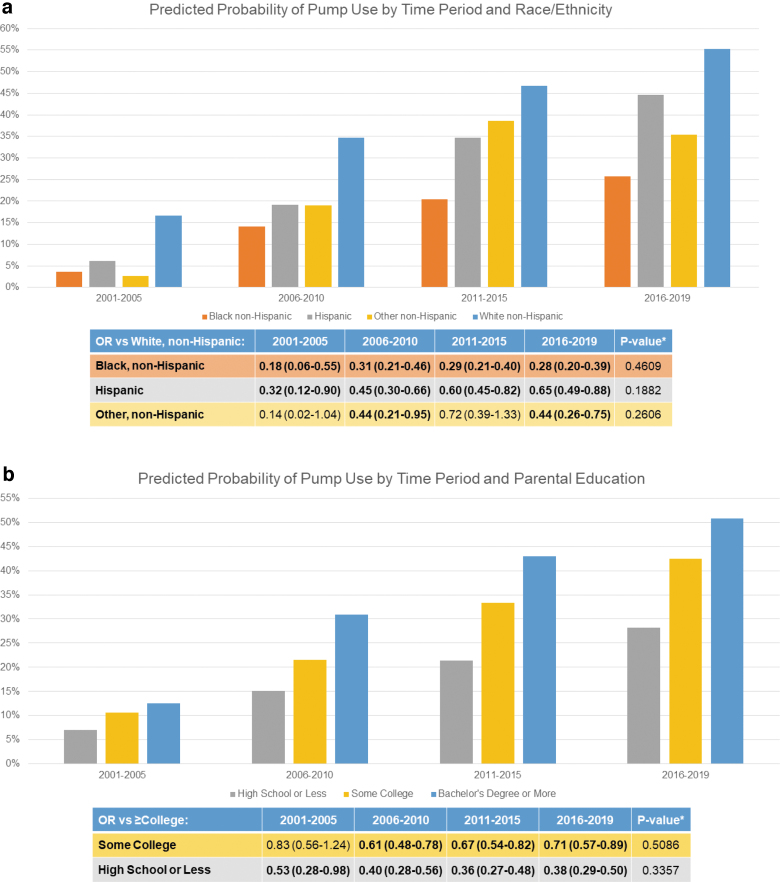
Race/ethnicity
NHW participants had the highest prevalence of pump use. In 2016–2019, 67% of NHW, 41% of Hispanic, 29% of NHB, and 46% of Other NH participants were pump users. Across all years, compared to NHW, the OR for Hispanic (OR 0.57 confidence interval [95% CI] 0.45–0.73), NHB participants (OR 0.28 95% CI 0.22–0.37), and those of Other NH (OR 0.49 [0.32–0.76]) had the lower prevalences of pump use at all time points (Table 2). When compared to NHW participants, there was no significant change over time in pump use in any of the racial and ethnic groups (P = 0.18, P = 0.46, P = 0.26) (Fig. 1).
Table 2.
Adjusted Odds for Insulin Pump Use Across All Years
| OR | 95% CI | P | ||
|---|---|---|---|---|
| Age at visit in years | 0.92 | 0.91 | 0.94 | <0.0001 |
| Diabetes duration in years | 1.08 | 1.05 | 1.11 | <0.0001 |
| Sex | ||||
| Male | 1.00 | Reference | ||
| Female | 1.21 | 1.06 | 1.39 | 0.006 |
| Clinic site | ||||
| SC | 1.39 | 1.11 | 1.75 | 0.004 |
| OH | 1.69 | 1.35 | 2.11 | <0.0001 |
| CO | 1.23 | 1.01 | 1.49 | 0.038 |
| CA | 0.54 | 0.40 | 0.73 | <0.0001 |
| WA | 1.00 | Reference | ||
| Race and ethnicity | ||||
| NHB | 0.28 | 0.22 | 0.37 | <0.0001 |
| Hispanic | 0.57 | 0.45 | 0.73 | <0.0001 |
| Other NH | 0.49 | 0.32 | 0.76 | 0.001 |
| NHW | 1.00 | Reference | ||
| Parental education | ||||
| Did not graduate/high school graduate | 0.39 | 0.31 | 0.47 | <0.0001 |
| Some college/associate's degree | 0.68 | 0.58 | 0.79 | <0.0001 |
| Bachelor's degree or more | 1.00 | Reference | ||
| Insurance | ||||
| Public | 0.84 | 0.70 | 1.00 | 0.050 |
| Private | 1.00 | Reference | ||
| Other/none | 0.58 | 0.45 | 0.74 | <0.0001 |
| Income | ||||
| <$25K | 0.43 | 0.35 | 0.53 | <0.0001 |
| $25K–$49K | 0.52 | 0.43 | 0.63 | <0.0001 |
| $50K–$74K | 0.79 | 0.66 | 0.94 | 0.008 |
| $75K+ | 1.00 | Reference | ||
| Unknown/refuse | 0.52 | 0.44 | 0.62 | <0.0001 |
| Time/SEARCH phase | ||||
| 2001–2005 | 1.00 | Reference | ||
| 2006–2010 | 2.75 | 2.23 | 3.39 | <0.0001 |
| 2011–2015 | 4.70 | 3.62 | 6.10 | <0.0001 |
| 2016–2019 | 6.62 | 4.73 | 9.26 | <0.0001 |
CA, California; CI, confidence interval; CO, Colorado; NHB, Non-Hispanic and Black; NHW, Non-Hispanic and White; OH, Ohio; OR; odds ratio; Other NH, Other race and Non-Hispanic; SC, South Carolina; WA, Washington.
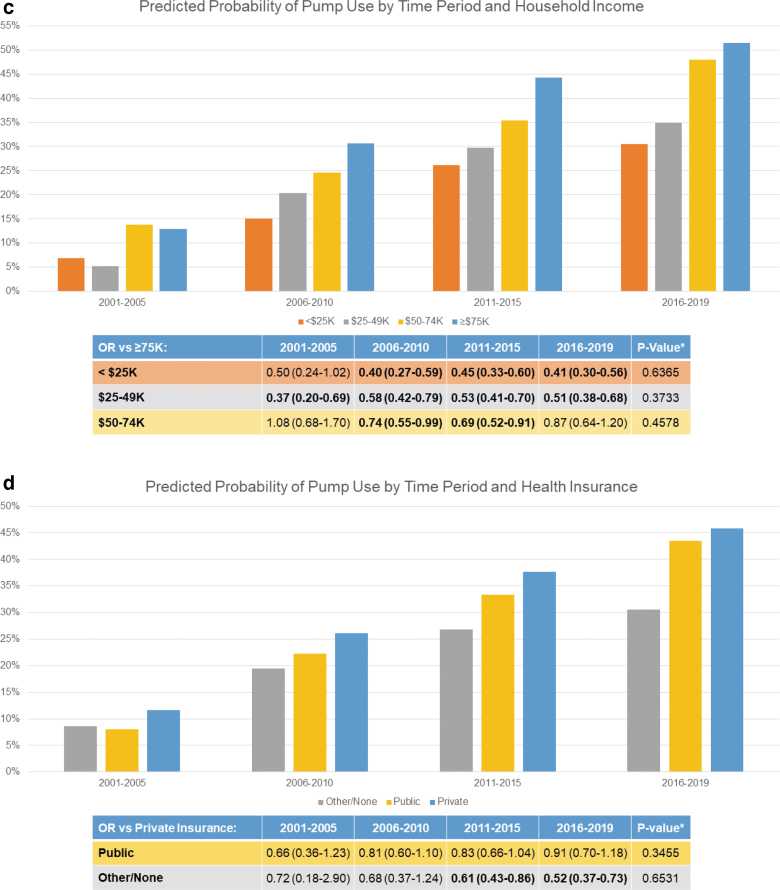
FIG. 1.
Adjusted predicted marginal probabilities and odds ratio for pump use over time by our subgroups of interest. (a) Race/ethnicity, (b) Parental Education, (c) Household Income and (d) Health Insurance. Figures show adjusted marginal prevalence (column graph) and adjusted odds ratio (table) for insulin pump use by patient characteristics and year. *p-Value for statistically significant differences in prevalence for pump use between period 1 (2001–2005) and period 4 (2016–2019) is noted in the table.
Education
Participants whose parents had lower educational attainment had a lower prevalence of insulin pump use, such that those whose parents did not graduate high school had the lowest pump use at all time periods. In 2016–2019, insulin pump use was reported in 70% of those with bachelor's degree or more, 56% with some college, 40% with high school degree and 18% of those without High school education. Across all years, compared to those whose parents had a bachelor's degree or more, participants whose parents had a high school degree or less and college/associate degree had an OR of 0.40 (95% CI 0.31–0.47) and 0.68 (95% CI 0.58–0.79), respectively. When compared to participants with parents with a bachelor's degree or higher, there was no significant change in the OR of pump use by educational group over time (P = 0.34 and P = 0.51).
Income
Lower income groups had lower pump use at all time periods. In 2016–2019, insulin pump use occurred in 74% of those with a household income greater than $75,000, 66% with $50,000–$74,999, 51% with $25,000–$49,999 and 41% with less than $25,000. Across all years, the OR for pump use in those with an annual household income <$25,000, $25,000–$49,999, and $50,000–$74,999 was OR 0.43 (95% CI 0.35–0.53), OR 0.52 (95% CI 0.43–0.63), and OR 0.79 (95% CI 0.66–0.94), respectively, compared to those with an annual household income ≥$75,000. The difference in odds for insulin pump use for those of lower income groups compared to those with income ≥$75,000 was no different in 2001–2005 when compared to 2016–2019 (P = 0.63, 0.37, and 0.46, respectively).
Health insurance
Those with public health insurance had a lower prevalence of insulin pump use at all time points compared to private health insurance across time. In 2016–2019, insulin pump use occurred in 64% of those with private and 50% with public insurance. Across all years, participants with public health insurance had an OR of 0.84 (95% CI 0.70–1.00) for insulin pump use compared to those with private health insurance, although this association was not significant. The difference in odds for insulin pump use for those with public health insurance compared to private insurance was no different in 2001–2005 than it was in 2016–2019 (P = 0.35).
Discussion
In this study spanning nearly two decades, we found that, while insulin pump use for T1D management has increased within all racial-ethnic and socioeconomic groups, there has been no significant change in the disparities that exist between the historically most advantaged and disadvantaged groups. Our study is consistent with the T1D Exchange study, which found no change in disparity of insulin pump use by a composite socioeconomic status measure between 2010–2012 and 2016–2018.20 Our study was the first to evaluate the change over time in racial and ethnic disparities and report the change within specific socioeconomic groups in a national U.S. cohort.
Since the first reports of these disparities in the early 2000s, studies have attempted to explore potential causes. This study demonstrated lower insulin pump use in racial-ethnic minoritized groups, with the lowest in those who were Black Non-Hispanic, even after adjusting for socioeconomic status, consistent with the literature.5–11,27
Recent studies suggest that a potential driver of these disparities may be related to challenges surrounding provider bias and poor physician-patient communication. Interviews with young adults with T1D who were Hispanic and NHB have revealed that many participants were never offered diabetes technology, despite having diabetes for many years.28 They also reported a lack of shared decision-making regarding technology initiation. We know from other studies that providers often rely on their personal opinions to guide who they will recommend diabetes technology to. Fredette et al reported that 70% of providers reported using personal guidelines to select patients for insulin pump use rather than written insulin pump guidelines29
Lawton et al surveyed providers' notions of insulin pump candidacy before a randomized clinical trial of hybrid closed-loop (HCL) insulin pump.30 They found that providers held strong assumptions about the types of patients who would use technology effectively (e.g., well-educated patients, technologically savvy, from close-knit families). Interestingly, after the trial, upon interview, most providers realized that their notions of good candidacy for diabetes technology did not predict success with the HCL pump during the trial. Providers then concluded that patient attributes cannot be used as a pre-selection criterion and that ideally all individuals should be given an opportunity to try new technology.30
In addition to provider barriers, financial barriers play an important role in socioeconomic disparities as health insurance coverage and out-of-pocket cost associated with insulin pump use remain variable and significant barriers to many.31–33 Messer et al found that financial barriers were the most frequently cited barrier to device use among participants. Insurance coverage issues were reported in 41.6% of participants, and cost of supplies and cost of the device were reported in 45.7% and 47.0% of participants, respectively.31
There are limited studies that have evaluated interventions to address the disparities in insulin pump use. A culturally sensitive study of shared medical appointments for Latino youth with T1D resulted in a significant increase in diabetes technology use over the 2-year study period, and a decrease in HBA1c among younger children.34 Several additional potential approaches to addressing these disparities have been suggested in the literature, yet data for their efficacy are lacking.
Approaches or strategies include interventions to improve providers' awareness of unconscious biases, developing a standardized pathway to diabetes technology use to minimize opportunity for provider bias.27,30 It has been recommended that providers improve availability of diabetes technology materials in lower literacy levels, and consider the use of decision aids to educate patients and facilitate shared decision making between the patient and providers,35,36 in addition to culturally sensitive approaches to communication. Decision support tools should specifically include exercises to help patients clarify values and estimate the costs of obtaining and using various types of diabetes technology.37 Studies are needed that evaluate the effectiveness of these and other potential approaches to diminish the persisting disparities noted across the past two decades.
A limitation of this study is that much of the SEARCH data are self-reported through questionnaires and so there is a potential for recall bias, although this may be less likely for key variables such as insulin pump use. Also, we were unable to capture any change in insulin pump use that occurred between visits. Although the surveillance population of SEARCH for incident diabetes was similar to the U.S. Census with regard to race and ethnicity, income, and education, recruitment of participants was based out of five centers in the United States, and so by nature, the participants of this study will not be representative of all youth with diabetes in the United States.
Second, although SEARCH was strategic in recruiting individuals from underrepresented social, racial, and ethnic identities into the cohort study, there were small counts of participants in some groups, especially in earlier years of this study, which may limit generalizability, and as in most studies, there is still likely a selection bias favoring more affluent participants regarding enrollment and retention.38 Consequently, it is possible that the disparities described in this study actually underestimate the magnitude of inequities that exist in the larger population of youth with diabetes.
Although we accounted for potential cofounding due to the correlation between sociodemographic factors, we were unable to evaluate how various combination of factors contribute to the likelihood of pump use. Nonetheless, the SEARCH study is the largest and most diverse diabetes study in youth in the United States, and thus a reasonable data source with which to evaluate this research question. These findings may be explored further in other data sources, including clinical registries, clinical databases, and administrative datasets.
Conclusion
Over the past two decades, there have been few improvements in the racial and ethnic, as well as socioeconomic disparities in utilization of insulin pumps for T1D management in youth and young adults, despite evidence to support their benefits. As recent studies seek to uncover potential drivers of these disparities, additional studies are now needed to test interventions to improve technology access and promote effective use over time.
Acknowledgments
The SEARCH for Diabetes in Youth Study is indebted to the many youth and their families, and their health care providers, whose participation made this study possible. We would like to acknowledge Scott Isom for the data extraction. We wish to also acknowledge the generous funding support from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) K23DK132482 (PI: Everett), L40DK129996 (PI: Everett), and K01DK116932 (PI: Wisk), NIH National Heart, Lung, and Blood Institute (NHLBI) K01 HL130413 (Wright), and National Center for Advancing Translational Sciences, National Institutes of Health KL2TR002490 (Kahkosa).
Authors' Contributions
E.M.E. conceptualized and designed study, interpreted the data, drafted the initial article, and reviewed and revised the article. D.W. contributed to the interpretation of data, the initial draft, and revision of the article. A.W. and J.D. were responsible for the data analysis. C.P. was this study's SEARCH PI and contributed to revision of the article. A.D.L., A.B., A.R.K., R.B., J.M., and E.M.-D. contributed to the revision of the article. L.E.W. contributed to the design of the study, analysis, and interpretation of the data, and reviewed and revised the article. All authors approved the final article as submitted and agree to be accountable for all aspects of the work.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the National Institute of Diabetes and Digestive and Kidney Diseases.
Role of the Funder/Sponsor
The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of data; preparation, review, or approval of the article; and decision to submit the article for publication.
Author Disclosure Statement
No competing financial interests exist.
Funding Information
The SEARCH for Diabetes in Youth Cohort Study (1R01DK127208-01 and 1UC4DK108173) is funded by the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases and supported by the Centers for Disease Control and Prevention. The Population Based Registry of Diabetes in Youth Study (1U18DP006131, U18DP006133, U18DP006134, U18DP006136, U18DP006138, and U18DP006139) is funded by the Centers for Disease Control and Prevention (DP-15-002) and supported by the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases.
References
- 1. Bergenstal RM, Tamborlane WV, Ahmann A, et al. Effectiveness of sensor-augmented insulin-pump therapy in type 1 diabetes. N Engl J Med 2010;363(4):311–320; doi: 10.1056/NEJMoa1002853 [DOI] [PubMed] [Google Scholar]
- 2. Rubin RR, Peyrot M; STAR 3 Study Group. Health-related quality of life and treatment satisfaction in the sensor-augmented pump therapy for A1C reduction 3 (STAR 3) trial. Diabetes Technol Ther 2012;14(2):143–151; doi: 10.1089/dia.2011.0162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Polonsky WH, Hessler D, Layne JE, et al. Impact of the Omnipod® insulin management system on quality of life: A survey of current users. Diabetes Technol Ther 2016;18(10):664–670; doi: 10.1089/dia.2016.0239 [DOI] [PubMed] [Google Scholar]
- 4. Mueller-Godeffroy E, Vonthein R, Ludwig-Seibold C, et al. Psychosocial benefits of insulin pump therapy in children with diabetes type 1 and their families: The Pumpkin Multicenter Randomized Controlled Trial. Pediatr Diabetes 2018;19(8):1471–1480; doi: 10.1111/pedi.12777 [DOI] [PubMed] [Google Scholar]
- 5. Sheikh K, Bartz SK, Lyons SK, et al. Diabetes device use and glycemic control among youth with type 1 diabetes: A single-center, cross-sectional study. J Diabetes Res 2018;2018(5162162):1–6; doi: 10.1155/2018/5162162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. O'Connor MR, Carlin K, Coker T, et al. Disparities in insulin pump therapy persist in youth with type 1 diabetes despite rising overall pump use rates. J Pediatr Nurs 2019;44:16–21; doi: 10.1016/j.pedn.2018.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Commissariat PV, Boyle CT, Miller KM, et al. Insulin pump use in young children with type 1 diabetes: Sociodemographic factors and parent-reported barriers. Diabetes Technol Ther 2017;19(6):363–369; doi: 10.1089/dia.2016.0375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Willi SM, Miller KM, DiMeglio LA, et al. Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics 2015;135(3):424–434; doi: 10.1542/peds.2014-1774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lin MH, Connor CG, Ruedy KJ, et al. Race, socioeconomic status, and treatment center are associated with insulin pump therapy in youth in the first year following diagnosis of type 1 diabetes. Diabetes Technol Ther 2013;15(11):929–934; doi: 10.1089/dia.2013.0132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lado JJ, Lipman TH. Racial and ethnic disparities in the incidence, treatment, and outcomes of youth with type 1 diabetes. Endocrinol Metab Clin North Am 2016;45(2):453–461; doi: 10.1016/J.ECL.2016.01.002 [DOI] [PubMed] [Google Scholar]
- 11. Paris CA, Imperatore G, Klingensmith G, et al. Predictors of insulin regimens and impact on outcomes in youth with type 1 diabetes: The SEARCH for Diabetes in Youth Study. J Pediatr 2009;155(2):183–189.e1; doi: 10.1016/j.jpeds.2009.01.063 [DOI] [PubMed] [Google Scholar]
- 12. Wong JC, Foster NC, Maahs DM, et al. Real-time continuous glucose monitoring among participants in the T1D Exchange Clinic Registry. Diabetes Care 2014;37(10):2702–2709; doi: 10.2337/dc14-0303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Foster NC, Beck RW, Miller KM, et al. State of type 1 diabetes management and outcomes from the T1D exchange in 2016–2018. Diabetes Technol Ther 2019;21(2); doi: 10.1089/dia.2018.0384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Majidi S, Ebekozien O, Noor N, et al. Inequities in health outcomes in children and adults with type 1 diabetes: Data from the T1D exchange quality improvement collaborative. Clin Diabetes 2021;39(3):278–283; doi: 10.2337/CD21-0028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kahkoska AR, Pokaprakarn T, Rumay Alexander G, et al. The impact of racial and ethnic health disparities in diabetes management on clinical outcomes: A reinforcement learning analysis of health inequity among youth and young adults in the SEARCH for diabetes in youth study. Diabetes Care 2022;45(1):108–118; doi: 10.2337/DC21-0496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Van Den Boom L, Karges B, Auzanneau M, et al. Temporal trends and contemporary use of insulin pump therapy and glucose monitoring among children, adolescents, and adults with type 1 diabetes between 1995 and 2017. Diabetes Care 2019;42(11):2050–2056; doi: 10.2337/dc19-0345 [DOI] [PubMed] [Google Scholar]
- 17. Miller KM, Foster NC, Beck RW, et al. Current state of type 1 diabetes treatment in the U.S.: Updated data from the T1D Exchange Clinic Registry. Diabetes Care 2015;38(6):971–978; doi: 10.2337/dc15-0078 [DOI] [PubMed] [Google Scholar]
- 18. Abdullah N, Pesterfield C, Elleri D, et al. Management of insulin pump therapy in children with type 1 diabetes. Arch Dis Child Educ Pract Ed 2014;99(5):214–220; doi: 10.1136/archdischild-2013-304501 [DOI] [PubMed] [Google Scholar]
- 19. Dickson V. CMS Expands Medicare Coverage of Diabetes Devices. 2018. Available from: https://www.modernhealthcare.com/article/20180109/NEWS/180109913/cms-expands-medicare-coverage-of-diabetes-devices [Last accessed: August 12, 2020]. [Google Scholar]
- 20. Addala A, Auzanneau M, Miller K, et al. A decade of disparities in diabetes technology use and HbA1c in pediatric type 1 diabetes: A transatlantic comparison HbA1c was higher in participants with lower SES. Diabetes Care 2010; doi: 10.2337/dc20-0257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hamman RF, Bell RA, Dabelea D, et al. The SEARCH for diabetes in youth study: rationale, findings, and future directions. Diabetes Care 2014;37:3336–3344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. SEARCH for Diabetes in Youth. SEARCH PHASE 3 Protocol. 2010. https://www.searchfordiabetes.org/docs/SEARCH_Phase_3_Protocols.pdf
- 23. Van Buuren S, Boshuizen HC, Knook DL. Multiple imputation of missing blood pressure covariates in survival analysis. Stat Med 1998;18:681–694; doi: 10.1002/(SICI)1097-0258(19990330)18:6 [DOI] [PubMed] [Google Scholar]
- 24. Van Buuren S, Brand JPL, Groothuis-Oudshoorn CGM, et al. Fully conditional specification in multivariate imputation. J Stat Comput Simul 2007;76(12):1049–1064; doi: 10.1080/10629360600810434 [DOI] [Google Scholar]
- 25. Donald B. Rubin. Multiple Imputation for Nonresponse in Surveys. John Wiley & Sons: New York; 1987. [Google Scholar]
- 26. Allison PD. Missing Data. SAGE Publications, Inc: Thousand Oaks; 2001. [Google Scholar]
- 27. Agarwal S, Schechter C, Gonzalez J, et al. Racial-ethnic disparities in diabetes technology use among young adults with type 1 diabetes. Diabetes Technol Ther 2020;23(4):306–313; doi: 10.1089/dia.2020.0338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Agarwal S, Crespo-Ramos G, Long JA, et al. “I Didn't Really Have a Choice”: Qualitative analysis of racial-ethnic disparities in diabetes technology use among young adults with type 1 diabetes. Diabetes Technol Ther 2021;23(9):616–622; doi: 10.1089/DIA.2021.0075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fredette ME, Zonfrillo MR, Park S, et al. Self-reported insulin pump prescribing practices in pediatric type 1 diabetes. Pediatr Diabetes 2021;22(5):758–765; doi: 10.1111/PEDI.13213 [DOI] [PubMed] [Google Scholar]
- 30. Lawton J, Kimbell B, Rankin D, et al. Health Professionals' views about who would benefit from using a closed-loop system: A qualitative study. Diabet Med 2020;37(6):1030–1037; doi: 10.1111/DME.14252 [DOI] [PubMed] [Google Scholar]
- 31. Messer LH, Tanenbaum ML, Cook PF, et al. Cost, hassle, and on-body experience: Barriers to diabetes device use in adolescents and potential intervention targets. Diabetes Technol Ther 2020;22(10):760–767; doi: 10.1089/dia.2019.0509 [DOI] [PubMed] [Google Scholar]
- 32. Everett EM, Wisk LE. Relationships between socioeconomic status, insurance coverage for diabetes technology and adverse health in patients with type 1 diabetes. J Diabetes Sci Technol 2022;16(4):825–833; doi: 10.1177/19322968211050649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Merjaneh L, Pihoker C, Divers J, et al. Out of pocket diabetes-related medical expenses for adolescents and young adults with type 1 diabetes: The SEARCH for Diabetes in Youth Study. Diabetes Care 2019;42(11):e172–e174; doi: 10.2337/DC19-0577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Pascual AB, Pyle L, Nieto J, et al. Novel, culturally sensitive, shared medical appointment model for hispanic pediatric type 1 diabetes patients. Pediatr Diabetes 2019;20(4):468–473; doi: 10.1111/PEDI.12852 [DOI] [PubMed] [Google Scholar]
- 35. Lawson ML, Shephard AL, Feenstra B, et al. Decision coaching using a patient decision aid for youth and parents considering insulin delivery methods for type 1 diabetes: A pre/post study. BMC Pediatr 2020;20(1):1–8; doi: 10.1186/S12887-019-1898-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Wysocki T, James L, Milkes A, et al. Electronically verified use of internet-based, multimedia decision aids by adolescents with type 1 diabetes and their caregivers. MDM Policy Pract 2018;3(1):2381468318769857; doi: 10.1177/2381468318769857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Witteman HO, Ndjaboue R, Vaisson G, et al. Clarifying values: An updated and expanded systematic review and meta-analysis. Med Decis Making 2021;41(7):801–820; doi: 10.1177/0272989X211037946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ejiogu N, Norbeck JH, Mason MA, et al. Recruitment and retention strategies for minority or poor clinical research participants: Lessons from the healthy aging in neighborhoods of diversity across the life span study. Gerontologist 2011;51(Suppl. 1):S33; doi: 10.1093/geront/gnr027 [DOI] [PMC free article] [PubMed] [Google Scholar]