Abstract
Middle meningeal artery embolization (MMAE) for chronic subdural hematoma (CSDH) is a novel, minimally invasive treatment. The indications and treatment practices for MMAE are variable and remain controversial. This study aimed to evaluate a strategy involving sequential MMAE after burr hole surgery for treating recurrent CSDH. We performed a retrospective analysis of data from consecutive patients who had undergone MMAE using liquid embolic agents within approximately 2 weeks after burr hole surgery for recurrent CSDH from September 2020 to March 2022. We analyzed patient characteristics, procedural details, CSDH recurrence after MMAE, surgical rescue, and complications. Six of the nine patients who underwent MMAE for CSDH recurrence were male, and the median age was 85 (range, 70-94) years. Five of the nine patients were being administered antithrombotic agents. The median duration between the burr hole surgery and MMAE procedure was 10 (range, 3-25) days. Anterior and posterior convexity branches were targeted for embolization using low-concentration N-butyl cyanoacrylate (NBCA), and the abnormal vascular networks with a cotton wool appearance disappeared after embolization in all cases. The NBCA distribution was observed by high-resolution computed tomography during the procedure; in three of nine cases, the NBCA penetrated not only the MMA but also the inner membrane. No recurrence, surgical rescue, or complications were observed in any patient during the median follow-up period of 3 months. As a minimally invasive treatment for recurrent CSDH, sequential MMAE after burr hole surgery may be a safe and effective option for preventing recurrence.
Keywords: chronic subdural hematoma, middle meningeal artery, embolization, burr hole surgery, recurrence
Introduction
Chronic subdural hematoma (CSDH) has become a common disease, especially in the elderly, and the frequency with which it occurs is predicted to increase further due to the aging population and the prevalent use of antithrombotic agents.1,2) CSDH is projected to become the most common neurosurgical disease by 2030 in the United States.2) Treatment for CSDH has traditionally involved burr hole surgery, with an outcome known to be generally favorable.3) However, CSDH recurrence is a possible complication after burr hole surgery, with a recurrence rate of 5%-30%.4-7) The use of anticoagulants, especially in elderly patients, is a known risk factor for CSDH recurrence.8,9)
Middle meningeal artery embolization (MMAE) for CSDH is a novel, minimally invasive treatment that is reportedly effective in preventing recurrence, and there has been an exponential increase in MMAE procedures in recent years in the United States.10-12) On the other hand, established methodologies for the treatment of CSDH are lacking, and the indications for MMAE and the treatment practices are variable and remain controversial.13,14) This study aimed to evaluate the safety and efficacy of sequential MMAE after burr hole surgery for preventing recurrence in consecutive patients treated for CSDH at our institution.
Material and Methods
Participants and study design
We performed a retrospective analysis of data collected from consecutive patients who had undergone MMAE for CSDH recurrence from September 2020 to March 2022. We first performed a burr hole surgery again to treat the recurrent CSDH and planned a subsequent MMAE procedure to be performed within a period of approximately 2 weeks. CSDH recurrence was defined as an increase of hematoma width on follow-up computed tomography (CT) compared with the postoperative CT after the first burr hole surgery, with accompanying symptoms that included headache, gait instability, focal motor weakness, and altered mental status. We also collected patients' characteristic data, such as age, sex, history of head trauma, and use of antithrombotic agents. We analyzed the timing of MMAE, details of the embolization procedures, resulting complications, recurrence after MMAE, and surgical rescue, which was defined as the requirement for burr hole surgery due to recurrent or persistent hematoma. The recurrence after MMAE was assessed by CT at 1, 3, and 6 months after the procedure. This study was approved by the institutional ethics committee (approval number 2-148; March 11, 2021). Written informed consent was obtained from each participant or his or her legal representative.
Endovascular procedure
Under local anesthesia, a 5-Fr guiding sheath was inserted into the right femoral artery and guided into the common carotid artery. Under systemic heparinization, a 3.4-Fr distal access catheter was inserted into the external carotid artery. After guiding the distal access catheter to a location close to the foramen spinosum, a 1.3-Fr flow-guided microcatheter was navigated into the middle meningeal artery (MMA) using a guidewire (0.010 inches). Anterior and posterior convexity branches were targeted for embolization. In the anterior branch, MMA angiography was performed to detect the absence of anastomosis with the ophthalmic artery. The microcatheter was positioned above the orbital roof to minimize the risk of embolization of the ophthalmic artery. In the posterior convexity branch, the microcatheter was positioned sufficiently distal to the foramen spinosum to minimize the risk of embolization of the petrosal branch, which feeds the vessel to the facial nerve. Both branches were embolized using heated 16.7% N-butyl cyanoacrylate (NBCA) mixed with lipiodol. After embolization, we performed high-resolution CT (HRCT) to visualize the distribution of the NBCA. After the procedure, the patients underwent observation in the general ward and were assessed for neurological symptoms. The subsequent day, CT was performed, and the patients were discharged, either returning home or being sent to a rehabilitation hospital. Postoperative CT was also performed at 1, 3, and 6 months after the procedure, when possible.
Results
A total of 103 CSDHs in 87 patients were treated in burr hole surgery, and the recurrence rate after burr hole surgery was 8.7% (9 patients). Table 1 summarizes the characteristics of the nine patients who underwent sequential MMAE after burr hole surgery for the treatment of CSDH recurrence. Six of the nine patients were male, and the median age was 85 (range, 70-94) years. Five of the nine patients were being administered antithrombotic agents. The median maximum width of hematoma before burr hole surgery was 30 (range, 22-39) mm, and all patients exhibited symptoms associated with hematoma. The median duration of time between the burr hole surgery and MMAE procedure was 10 (range, 3-25) days. Anterior and posterior convexity branches were targeted for embolization, and abnormal vascular networks with a cotton wool appearance were observed in all cases. Both branches were embolized using 16.7% NBCA. The median volume of NBCA administered in the anterior branch was 0.1 (range, 0.02-0.17) mL; in the posterior convexity branch, the median volume administered was 0.08 (range, 0.02-0.17) mL. The abnormal vascular networks were confirmed to have disappeared after embolization. The distribution of the NBCA was observed by HRCT during the procedure, and the NBCA penetrated not only the MMA but also the inner membrane in three of the nine cases. No complications such as visual field defects, alterations in visual acuity, or facial paralysis associated with MMAE were observed in any of the patients. The median follow-up duration was 103 (range, 9-185) days, during which no recurrence or surgical rescue was observed in any patient.
Table 1.
Patients’ demographic and clinical characteristics
| Case no. | Age (years) | Sex | History of head trauma | Antithrombotic agents administered | Symptoms | Duration between surgery and MMAE (days) | Complications | Recurrence | Follow-up period (days) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 92 | M | + | − | Altered mental status | 3 | − | − | 9 |
| 2 | 83 | F | − | Anticoagulant therapy | Gait instability | 9 | − | − | 95 |
| 3 | 77 | M | + | DAPT | Gait instability | 13 | − | − | 111 |
| 4 | 87 | M | + | − | Gait instability | 10 | − | − | 185 |
| 5 | 94 | M | + | − | Altered mental status | 25 | − | − | 13 |
| 6 | 81 | F | + | Antiplatelet therapy | Focal motor weakness | 8 | − | − | 178 |
| 7 | 93 | M | + | Antiplatelet therapy | Gait instability | 7 | − | − | 175 |
| 8 | 70 | M | + | DAPT | Headache | 10 | − | − | 25 |
| 9 | 85 | F | + | − | Focal motor weakness | 13 | − | − | 28 |
Abbreviations: DAPT, dual antiplatelet therapy; F, female; M, male; MMAE, middle meningeal artery embolization
Case presentation (case 6)
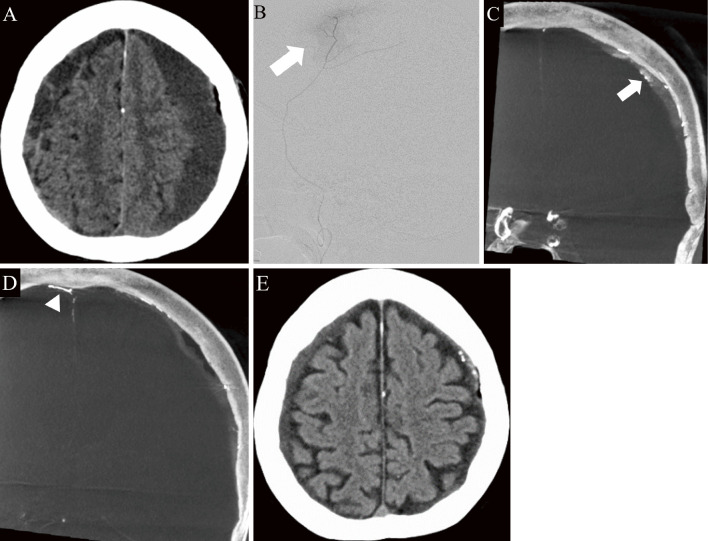
An 81-year-old female presented with right hemiplegia and aphasia 2 weeks after experiencing head trauma. She had been receiving an antiplatelet agent for the treatment of coronary artery disease. CT examination revealed bilateral CSDH. Therefore, a burr hole surgery was performed for left CSDH, after which the right hemiplegia and aphasia improved, and she was discharged the following day. However, the symptoms of right hemiplegia reappeared 2 weeks later, and CSDH recurrence was confirmed by CT (Fig. 1A). We performed another burr hole surgery and a left MMAE procedure was conducted 8 days later. The MMA angiography revealed abnormal staining, with a cotton wool appearance (Fig. 1B), and the anterior and posterior convexity branches were embolized with 16.7% NBCA. HRCT revealed that the NBCA penetrated not only the treated MMA but also the inner membrane and contralateral MMA (Fig. 1C, D). We confirmed that not only the left but also the right hematoma had been reduced through follow-up CT examinations performed 1 and 3 months after the procedure (Fig. 1E).
Fig. 1.
Imaging findings of an 81-year-old female who presented with right hemiplegia and aphasia 2 weeks after head trauma (case 6).
A: Computed tomography (CT) image indicating the recurrence of left chronic subdural hematoma (CSDH).
B: Super-selective angiogram (lateral view) of the anterior branch showing an abnormal cotton wool appearance (white arrow).
C and D: High-resolution CT (coronal view) showing that the N-butyl cyanoacrylate (NBCA) penetrated not only the treated middle meningeal artery (MMA) but also the inner membrane (white arrow) and contralateral MMA (arrowhead).
E: CT performed 3 months postembolization showing the resolution of not only the left subdural hematoma but also the right subdural hematoma.
Discussion
In this study, we analyzed data from nine cases in which MMAE was performed using liquid embolic agents within 2 weeks following burr hole surgery for the treatment of recurrent CSDH. No complications, recurrence, or surgical rescue was observed in any of the patients. MMAE for CSDH is an emerging minimally invasive procedure that has the potential to reduce the need for further surgical intervention.10-14) In a previous meta-analysis that included 718 MMAE cases, MMAE was associated with lower rates of CSDH recurrence (P = 0.02, odds ratio: 0.15, 95% confidence interval: 0.03-0.75) and surgical rescue (P = 0.003, odds ratio: 0.21, 95% confidence interval: 0.07-0.58) compared to those associated with conventional management.13) Since the first report of MMAE in 2000, the number of reports involving the use of MMAE for the treatment of CSDH has been increasing.11,12,15)
However, the indications for MMAE are variable.13) In this study, we evaluated and presented data from consecutive cases who underwent MMAE after burr hole surgery for all CSDH recurrences, a treatment strategy that has not been previously reported. Initially, there were some reports involving MMAE, all of which were targeted only at groups that were at high risk of recurrence after burr hole surgery.15-20) In recent years, however, the safety of MMAE has been established, and there have been published reports describing prophylactic MMAE performed immediately after the first burr hole surgery, as well as upfront MMAE as an alternative to the first burr hole surgery.21-24) The indications for MMAE remain controversial, and it is important to define appropriate patient selection criteria. The treatment strategy for symptomatic CSDH recurrence has generally involved a repeated burr hole surgery. However, patients treated with anticoagulant therapy, especially the elderly, have an increased risk of CSDH recurrence even after burr hole surgery.8,9) Sequential MMAE after burr hole surgery could be an effective option for minimizing CSDH recurrence to avoid the need to undergo repeated burr hole surgeries.
One of the advantages of this strategy is that it facilitates the early resumption of antithrombotic agents, although the timing of MMAE is also controversial. In this study, we performed sequential MMAE following burr hole surgery for CSDH recurrence, with a median duration of 10 days between the second burr hole surgery and the MMAE procedure. CSDH recurrence after burr hole surgery often occurs within about 1 month. Therefore, we first planned another burr hole surgery for CSDH recurrence and subsequently performed MMAE within a period of approximately 2 weeks, which appeared to be an appropriate timeframe for ensuring a good outcome.
Polyvinyl alcohol particles are an embolic material commonly selected for MMAE.10,17,24) In this study, however, we selected heated low-concentration NBCA as a liquid embolic material.25-28) NBCA is a fast-acting liquid adhesive that polymerizes upon contact with anions in the blood; this can result in shorter operating times, which can be advantageous when used under local anesthesia, especially in elderly patients.29) The use of low-concentration NBCA prevents the adhesion of the microcatheter tip to the vessel wall, allowing for long-term injection and safer embolization. The addition of lipiodol to adjust to the low-concentration NBCA also improves visibility at the time of embolization. Another advantage of using NBCA is that its penetration can be confirmed by CT. In some cases, postembolization HRCT showed that the NBCA penetrated not only the MMA but also the inner membrane (Fig. 1C).
Regarding embolized blood vessels, some studies have reported that it is important to embolize both the anterior and posterior convexity branches to achieve extensive devascularization in MMAE.30) The anterior and posterior convexity branches are often involved in a hematoma. In angiographic anatomical analysis of the MMA, three groups have been used to classify the dominance of the anterior or posterior convexity branch. The dominance of the anterior branch was observed in a minority of MMAs (41%), whereas posterior dominance or codominance was observed in 59% of cases.30) In this study, the posterior dominance or codominance was observed in five of nine patients. We performed embolization of both branches, and no recurrence requiring surgical rescue was observed in this study.
In terms of complications, in the anterior branch, it is important to evaluate the potential for anastomoses with the orbital branch. The microcatheter should be positioned above the orbital roof in a lateral position to minimize the risk of embolization of the ophthalmic artery. In the posterior convexity branch, it is important for the microcatheter to be positioned sufficiently distal to the foramen spinosum to minimize the risk of embolization of the petrosal branch, which feeds the vessel to the facial nerve. In a previous study, the posterior convexity branch presented a proximal origin at 36%; therefore, in such cases, one must pay particular attention to bifurcation of the petrosal branch.30)
This study had several limitations. For example, it included a small number of cases, it was retrospective in nature, and it relied on data from a single center. Another limitation was the relatively short follow-up period. Further studies with a larger cohort and a long-term follow-up period are necessary to confirm the present findings.
As a minimally invasive treatment for recurrent CSDH, sequential MMAE using NBCA performed within 2 weeks after burr hole surgery may be a safe and effective option to prevent recurrence, although further studies with larger sample sizes and long-term follow-up periods are required.
Conflicts of Interest Disclosure
The authors declare no competing interests.
References
- 1).Sahyouni R, Goshtasbi K, Mahmoodi A, Tran DK, Chen JW: Chronic subdural hematoma: A historical and clinical perspective. World Neurosurg 108: 948-953, 2017 [DOI] [PubMed] [Google Scholar]
- 2).Balser D, Farooq S, Mehmood T, Reyes M, Samadani U: Actual and projected incidence rates for chronic subdural hematomas in United States Veterans Administration and civilian populations. J Neurosurg 123: 1209-1215, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3).Feghali J, Yang W, Huang J: Updates in chronic subdural hematoma: Epidemiology, etiology, pathogenesis, treatment, and outcome. World Neurosurg 141: 339-345, 2020 [DOI] [PubMed] [Google Scholar]
- 4).Santarius T, Kirkpatrick PJ, Ganesan D, et al. : Use of drains versus no drains after burr-hole evacuation of chronic subdural haematoma: A randomised controlled trial. Lancet 374: 1067-1073, 2009 [DOI] [PubMed] [Google Scholar]
- 5).Tsutsumi K, Maeda K, Iijima A, et al. : The relationship of preoperative magnetic resonance imaging findings and closed system drainage in the recurrence of chronic subdural hematoma. J Neurosurg 87: 870-875, 1997 [DOI] [PubMed] [Google Scholar]
- 6).Toi H, Kinoshita K, Hirai S, et al. : Present epidemiology of chronic subdural hematoma in Japan: Analysis of 63,358 cases recorded in a national administrative database. J Neurosurg 128: 222-228, 2018 [DOI] [PubMed] [Google Scholar]
- 7).Hirai S, Yagi K, Hara K, et al. : Postoperative recurrence of chronic subdural hematoma is more frequent in patients with blood type A. J Neurosurg 135: 1-5, 2021 [DOI] [PubMed] [Google Scholar]
- 8).Nathan S, Goodarzi Z, Jette N, Gallagher C, Holroyd-Leduc J: Anticoagulant and antiplatelet use in seniors with chronic subdural hematoma: Systematic review. Neurology 88: 1889-1893, 2017 [DOI] [PubMed] [Google Scholar]
- 9).Zhang P, Li Y, Huang J, et al. : Chronic subdural haematoma in antithrombotic cohorts: Characteristics, surgical outcomes, and recurrence. Br J Neurosurg 34: 408-415, 2020 [DOI] [PubMed] [Google Scholar]
- 10).Ban SP, Hwang G, Byoun HS, et al. : Middle meningeal artery embolization for chronic subdural hematoma. Radiology 286: 992-999, 2018 [DOI] [PubMed] [Google Scholar]
- 11).Dicpinigaitis AJ, Al-Mufti F, Cooper JB, et al. : Nationwide trends in middle meningeal artery embolization for treatment of chronic subdural hematoma: A population-based analysis of utilization and short-term outcomes. J Clin Neurosci 94: 70-75, 2021 [DOI] [PubMed] [Google Scholar]
- 12).Nia AM, Srinivasan VM, Lall RR, Kan P: Middle meningeal artery embolization for chronic subdural hematoma: A national database study of 191 patients in the United States. World Neurosurg 153: e300-e307, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13).Ironside N, Nguyen C, Do Q, et al. : Middle meningeal artery embolization for chronic subdural hematoma: A systematic review and meta-analysis. J Neurointerv Surg 13: 951-957, 2021 [DOI] [PubMed] [Google Scholar]
- 14).Shotar E, Meyblum L, Premat K, et al. : Middle meningeal artery embolization reduces the post-operative recurrence rate of at-risk chronic subdural hematoma. J Neurointerv Surg 12: 1209-1213, 2020 [DOI] [PubMed] [Google Scholar]
- 15).Mandai S, Sakurai M, Matsumoto Y: Middle meningeal artery embolization for refractory chronic subdural hematoma. Case report. J Neurosurg 93: 686-688, 2000 [DOI] [PubMed] [Google Scholar]
- 16).Mino M, Nishimura S, Hori E, et al. : Efficacy of middle meningeal artery embolization in the treatment of refractory chronic subdural hematoma. Surg Neurol Int 1: 78, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17).Kim E: Embolization therapy for refractory hemorrhage in patients with chronic subdural hematomas. World Neurosurg 101: 520-527, 2017 [DOI] [PubMed] [Google Scholar]
- 18).Hashimoto T, Ohashi T, Watanabe D, et al. : Usefulness of embolization of the middle meningeal artery for refractory chronic subdural hematomas. Surg Neurol Int 4: 104, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19).Chihara H, Imamura H, Ogura T, et al. : Recurrence of a refractory chronic subdural hematoma after middle meningeal artery embolization that required craniotomy. NMC Case Rep J 1: 1-5, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20).Okuma Y, Hirotsune N, Sato Y, et al. : Midterm follow-up of patients with middle meningeal artery embolization in intractable chronic subdural hematoma. World Neurosurg 126: e671-e678, 2019 [DOI] [PubMed] [Google Scholar]
- 21).Schwarz J, Carnevale JA, Goldberg JL, et al. : Perioperative prophylactic middle meningeal artery embolization for chronic subdural hematoma: A series of 44 cases. J Neurosurg 21: 1-9, 2021 [DOI] [PubMed] [Google Scholar]
- 22).Gomez-Paz S, Akamatsu Y, Salem MM, et al. : Upfront middle meningeal artery embolization for treatment of chronic subdural hematomas in patients with or without midline shift. Interv Neuroradiol 27: 571-576, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23).Khorasanizadeh M, Chang YM, Enriquez-Marulanda A, et al. : Morphological changes in chronic subdural hematomas following upfront middle meningeal artery embolization: Sequence, timing, and association with outcomes. J Neurosurg 26: 1-14, 2021 [DOI] [PubMed] [Google Scholar]
- 24).Link TW, Boddu S, Paine SM, Kamel H, Knopman J: Middle meningeal artery embolization for chronic subdural hematoma: A series of 60 cases. Neurosurgery 85: 801-807, 2019 [DOI] [PubMed] [Google Scholar]
- 25).Nakagawa I, Park HS, Kotsugi M, et al. : Enhanced hematoma membrane on DynaCT images During middle meningeal artery embolization for persistently recurrent chronic subdural hematoma. World Neurosurg 126: e473-e479, 2019 [DOI] [PubMed] [Google Scholar]
- 26).Matsumoto H, Hanayama H, Okada T, et al. : Which surgical procedure is effective for refractory chronic subdural hematoma? Analysis of our surgical procedures and literature review. J Clin Neurosci 49: 40-47, 2018 [DOI] [PubMed] [Google Scholar]
- 27).Yajima H, Kanaya H, Ogino M, Ueki K, Kim P: Middle meningeal artery embolization for chronic subdural hematoma with high risk of recurrence: A single institution experience. Clin Neurol Neurosurg 197: 106097, 2020 [DOI] [PubMed] [Google Scholar]
- 28).Saito H, Tanaka M, Hadeishi H: Angiogenesis in the septum and inner membrane of refractory chronic subdural hematomas: Consideration of findings after middle meningeal artery embolization with low-concentration n-butyl-2-cyanoacrylate. NMC Case Rep J 6: 105-110, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29).Shapiro M, Walker M, Carroll KT, et al. : Neuroanatomy of cranial dural vessels: Implications for subdural hematoma embolization. J Neurointerv Surg 13: 471-477, 2021 [DOI] [PubMed] [Google Scholar]
- 30).Shotar E, Premat K, Lenck S, et al. : Angiographic anatomy of the middle meningeal artery in relation to chronic subdural hematoma embolization. Clin Neuroradiol 32: 57-67, 2022 [DOI] [PubMed] [Google Scholar]