Abstract
Background:
The COVID-19 pandemic overwhelmed health care systems, leading many jurisdictions to reduce surgeries to create capacity (beds and staff) to care for the surge of patients with COVID-19; little is known about the impact of this on patients whose surgery was delayed. The objective of this study was to understand the patient and family/caregiver perspective of having a surgery delayed during the COVID-19 pandemic.
Methods:
Using an interpretative descriptive approach, we conducted interviews between Sept. 20 and Oct. 8, 2021. Adult patients who had their surgery delayed or cancelled during the COVID-19 pandemic in Alberta, Canada, and their family/caregivers were eligible to participate. Trained interviewers conducted semistructured interviews, which were iteratively analyzed by 2 independent reviewers using an inductive approach to thematic content analysis.
Results:
We conducted 16 interviews with 15 patients and 1 family member/caregiver, ranging from 27 to 75 years of age, with a variety of surgical procedures delayed. We identified 4 interconnected themes: individual-level impacts on physical and mental health, family and friends, work and quality of life; system-level factors related to health care resources, communication and perceived accountability within the system; unique issues related to COVID-19 (maintaining health and isolation); and uncertainty about health and timing of surgery.
Interpretation:
Although the decision to delay nonurgent surgeries was made to manage the strain on health care systems, our study illustrates the consequences of these decisions, which were diffuse and consequential. The findings of this study highlight the need to develop and adopt strategies to mitigate the burden of waiting for surgery during and after the COVID-19 pandemic.
COVID-19 was declared a pandemic by the World Health Organization (WHO) in March 2020,1 and health care systems across the globe braced for a potentially large influx of patients with COVID-19 within hospitals. These situations played out in countries such as Italy, where health care systems quickly became overwhelmed. 2 In light of the impact of the pandemic on health care systems globally, many Canadian provinces reallocated health care resources to care for patients with COVID-19 by reducing surgical capacity. Consequently, a staggering number of nonurgent surgeries (surgeries for conditions not immediately threatening life or limb)3 were delayed. For example, early in the COVID-19 pandemic response, Ontario delayed 185 000 surgeries, and the number of delayed surgeries during the fourth wave in Alberta climbed to more than 30 000 — a number that continues to increase at the time of writing (unpublished data, 2021).1,4,5 The effect of delaying nonurgent surgeries in Canada has not been fully explored, but it is estimated that the backlog from just the first wave of COVID-19 in some provinces will take 84 weeks to clear.5
Prepandemic evidence suggests that excessive surgical wait times can lead to poor physical health, increased anxiety, and decreased social interaction, ability to work and overall quality of life.6,7 Factors that mediate the impact of delays in access to surgical care include patient choice in the delay, and the quality and quantity of communication from health care providers. 6,7 It is unclear whether these prepandemic factors (poor physical and mental health, and quality of life) are consistent with the effects of delaying surgery in the context of the COVID-19 pandemic because evidence of the impact of delayed surgeries during COVID-19 is still in its infancy.8 With the continued rise in delayed surgeries, understanding the scope of the personal impact on patients and their daily lives is of critical importance. To address this knowledge gap, we sought to understand the patient and family/caregiver perspective of having a surgery delayed during the COVID-19 pandemic response.
Methods
In this qualitative study, we used an interpretative descriptive approach as the methodological framework, which is aligned with the constructivist and naturalistic orientation of inquiry and aims to understand a phenomenon grounded in the data within a clinic context to apply the findings.9–12 This study was reported according to the Consolidated Criteria for Reporting Qualitative Research.13
This study took place in Alberta from Sept. 14 to Dec. 1, 2021. At the time of writing, Canada had experienced 4 waves of COVID-19.14 In Alberta, wave 1 (early March 2020 to early May 2020) resulted in a reported 30% decrease in surgical capacity, waves 2 and 3 did not result in a strategic decrease in surgical capacity, and wave 4 (September 2021 to the time of writing in November 2021) resulted in all nonurgent surgeries being delayed (only emergent and urgent surgeries performed) with an estimated 60%–70% decrease in surgical capacity.1
Participants
All adult patients (age ≥ 18 yr) and family/caregivers of adult patients in Alberta who had their surgery delayed owing to the COVID-19 pandemic response were eligible to participate.
Recruitment and sample selection
Recruitment occurred between Sept. 14 and Oct. 1, 2021. Recruitment posters were distributed initially through the social media accounts (Twitter, Facebook, Instagram) of the principal investigator (K.M.S.) and subsequently through reposts and local news outlets to allow us to reach patients across broad networks spanning the province of Alberta. Patients with delayed surgeries and their family/caregivers contacted the principal investigator via email or telephone.
Consistent with interpretative descriptive approach, a theoretical sampling strategy was used. We collected data to achieve a purposive sample of anticipated variations in response based on age categories (variety of ages), gender (identify as man, woman, other), type of surgery and geographical location (the health-related zones across the province).10
Data collection
We collected data between Sept. 20 and Oct. 8, 2021, via interviews that were guided by a semistructured interview guide, with prompts to elicit emergent ideas while maintaining focus on the topic (Appendix 1, available at www.cmajopen.ca/content/11/1/E90/suppl/DC1). The interview guide was developed and iteratively refined by the investigators (K.M.S., S.B. and M.E.B.) based on the objective of the study and informed by the methodological framework (interpretive descriptive approach).9 The interview guide was pilot tested among the research team to ensure the questions elicited responses relevant to the objective.
Interviews were conducted virtually (using Zoom or telephone) owing to public health restrictions in Alberta during data collection, and were audio recorded and transcribed. Field notes were included to clarify context, where appropriate. The consenting process occurred before beginning the interviews (Appendix 2, available at www.cmajopen.ca/content/11/1/E90/suppl/DC1). The consent script was sent to participants by email when participants indicated interest in participating, and multiple opportunities were provided to answer the participants’ questions before completing the oral consent process.
Ten interviews were anticipated, but interviews continued until saturation was reached (i.e., no new themes or novel data were identified) and we had recruited patients with varied ages, genders, types of surgery and geographical locations.
Reflexivity
Interviews were conducted by experienced facilitators (C.S., J.K., E.S. and N.J.). The facilitators were female graduate students and a research associate with experience in qualitative methods, but not within the area of surgical care or COVID-19, who volunteered to conduct the interviews. Therefore, there were few assumptions or biases with regard to the results of the study. The facilitators and principal investigator (study team) had formal graduate training in qualitative methods or experiential training in interview facilitation, and had graduate degrees in public health. The study team did not have previous relationships with the participants or their health care providers. The study team experienced the pandemic and the response to the pandemic differently with regard to disruptions to family and work life. None of the members of the study team had surgery or were waiting for surgery during the pandemic, but the senior author is a pediatric surgeon.
Data analysis
Data were managed using NVivo 12.015 and analyzed in keeping with our interpretive descriptive approach by 2 independent reviewers (K.M.S. and C.S.) using thematic content analysis to understand key elements of the patient experience.10–12 An inductive approach was used so that themes were drawn from the data rather than from preexisting sources. Data analysis was iterative, whereby the 2 reviewers coded transcripts and met to compare emerging themes to ensure rigour of the analytic process. Final themes were determined by consensus among reviewers.
To ensure trustworthiness of the findings, the results were first reviewed by the interview facilitators (J.K., E.S. and N.J.). The results were then reviewed and refined by all authors. Finally, 3 participants who agreed, during the interview, to review the findings reviewed the results to ensure trustworthiness of the findings by the participants.
Ethics approval
This study was approved by the University of Calgary Conjoint Health Research Ethics Board (REB20–0753).
Results
We conducted 16 interviews with 15 patients and 1 family member/caregiver between Sept. 20 and Oct. 8, 2021. Saturation was achieved, with no new themes added, after the 13th interview.
The average length of the interviews was 22 minutes. Participants had a mean age of 47 (range 27–75) years, with most (62%) identifying as women. Most participants lived in the 2 largest health system zones (Calgary Zone 56% and Edmonton Zone 38%), with 1 participant living in the South Zone. Correspondingly, surgeries were mostly scheduled in urban centres (75%). The type of surgery scheduled varied considerably and included gynecologic (n = 5), orthopedic (n = 4), gastrointestinal (n = 2), diagnostic, gender reallocation, prostate, neurosurgery and cardiac. Most participants had their surgery delayed during the fourth wave (62%), while (25%) of participants had their surgery delayed during wave 1. Four participants had their surgery completed before the interview (25%) and 12 did not (75%). The 3 participants who reviewed the findings did not suggest changes to the results, and therefore no refinements were made based on their review.
Themes
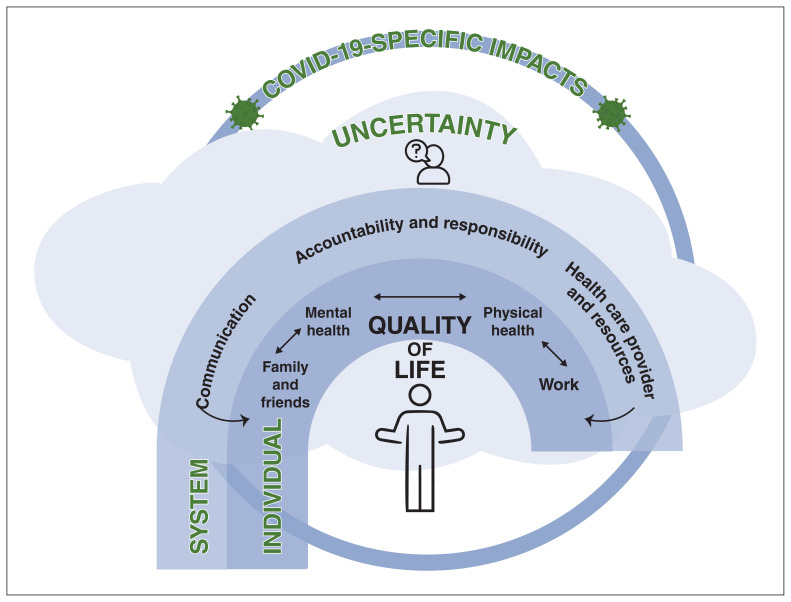
Four overarching themes emerged from the data: individual-level impacts (subthemes included physical health, mental health, family and friends impact, work impact and quality of life), system-level factors (subthemes included communication, health care resources and perceived accountability and responsibility), COVID-19-specific impacts and uncertainty (Figure 1).
Figure 1:
Four interconnected themes were identified by participants. Participants reported several individual-level effects of delaying surgery during the COVID-19 pandemic, including the impact on family and friends, their mental health, their physical health and work. The individual-level subthemes were interrelated (e.g., the impact on family and friends exacerbated the impact on participants’ mental health). Similarly, there were system-level factors, including communication, accountability and responsibility, and health care provider and health care resources that mediated the individual-level impacts. Uncertainty was a cloud that hung over all of the individual-and system-level impacts. Similarly, the COVID-19 pandemic introduced several unique factors that touched many of the themes and subthemes.
Individual-level impacts
Representative quotations for the theme of individual-level impacts on physical and mental health, family and friends, work and quality of life are shown in Table 1.
Table 1:
Quotations representing the theme of individual-level impacts
| Subtheme | Descriptive codes | Exemplar quotations |
|---|---|---|
| Physical health | Pain Discomfort Quality of life Worry |
“ … but you can see the pain on her face when she sits at the table, or whatever, and now she spends as much time lying in bed off her legs and her hip.” [Participant 7A] “So, this delay, basically I’m afraid I can have a heart attack or stroke, at any time. So, it’s been very stressful on me and my [spouse] as well.” [Participant 6] “It seems like I’m getting … my breath is getting shorter. I get tired quicker it seems.” [Participant 6] “This wasn’t like you know, a health life-saving surgery so it’s been, it was fine. Like my fibro [fibromyalgia] probably got worse because of stress.” [Participant 3] “… it’s pretty hard for the ones that are waiting like myself included, it, yeah, kind of, it would be nice to get done because everyday pain; I mean a lot of pain.” [Participant 7B] “I’m now on pain medication every day. Yep. At the moment, I don’t do a whole lot because it hurts too much.” [Participant 15] “I mean, the obvious [impact] is the continued pain. So, what I’m sort of dealing with on a sort of weekly basis is, I’m not sure what causes it, but I’ll get a sharp onset of pain in my abdomen just below my ribs … So, it makes it hard and painful to inhale deeply. So, I find myself short of breath even in with simple tasks like climbing a flight of stairs.” [Participant 14] |
| Mental health | Depression Anxiety Worry Frustration Anger Independence Isolation Uncertainty |
“It’s been a challenge more from the mental health side of things.” [Participant 1] “It’s been a lot of mental strain, because I know the extra is going to be put on the people at work. And my limited activity at home and just the mental stress of having surgery, period. And then the ups and downs of watching the news to see how bad it’s getting, and if it might get cancelled. And then the relief of having a surgery date, and then the immediate crushing that it was cancelled. So, it’s been an extremely emotional toll on me.” [Participant 9] “I mean, just kind of, like, bummed me out. I’ve got body dysphoria; so having boobs was just lousy.” [Participant 3] “In August I had a panic attack … and talked to the doctor there and anyway, since that time I’ve been extremely; I have been quite calm OK … And then they cancel my surgery so that stress level went up again.” [Participant 6] “… and again, like I know for me, like, it’s not so much of an impact in a physical sense, so, like, in that case, no. But, again, the emotional toll makes me sometimes not want to do anything.” [Participant 9] “And we were able to stop and control the prolapse but every day waiting for that flap surgery, and every day waiting for the reversal. I held my breath that my intestine would not truly fall out of my body.” [Participant 11] “So, there’s kind of the stress over that, the stress over wondering if I do have to delay till April. Obviously, there’s a risk that a gallstone can get stuck and cause a lot worse problems. So, there’s that stress.” [Participant 14] “So this delay, basically I’m afraid I can have a heart attack or stroke, at any time. So, it’s been very stressful on me and my wife as well.” [Participant 6] “I did contact my surgeon’s office to find out how much notice I would get ahead of when the surgery was rebooked, because I have arthritis that’s autoimmune. And so of course, when your stress levels go up, the arthritis tends to flare.” [Participant 14] “You worry all the time. You worry about what could happen, what might happen, why it isn’t happening. So, there’s a lot of depression and anxiety involved.” [Participant 12] “I’m going to be diagnosed with depression and I think it was ultimately a result of the delay because you’re so excited you’re counting down the days and then, like I said, just to be told a week before that after you’ve been waiting for so long that it’s not happening, and you don’t know when it’s happening, like, that loss of control and all of those unknowns … Just, like, on a mental health toll it’s impacted my day to day, and wanting to make plans.” [Participant 10] “I think the biggest reason why I wanted to participate is; just again, it’s that emotional toll that it takes on people on a daily basis and I have to assume that the government thought about that, but perhaps they don’t realize the actual toll that it takes on all of these other people’s lives …” [Participant 9] |
| Family and friends | Isolation Independence Burden |
“But it tells you, it shows you the stress. That my constant surgeries and the postponement because of COVID. That my child could see how crucial this was. A teenager. Interviewer: Yeah, it impacts the entire family? Oh, to just an extreme.” [Participant 11] “So he [participant’s father] ended up just, like, rejigging his schedule; looks like he’ll take a different day of work, whenever this actually happens. So, it was just, like, very stressful for a lot of people who had kind of, like, tried to reorganize their life around me.” [Participant 3] “At this point, my son, this is what I really want to stress, this wasn’t just me. I have a 16 [year-old son]. He’s a competitive athlete … and he made the choice to pull out of his training, even COVID-safe because at this point, we’re 2 weeks before my surgery and if anyone’s exposed to COVID I’m not going. So, my whole house shut down. We isolated and shut down completely. So, when you talk about socialization it wasn’t just mine, I had a teenager and a home that it affected.” [Participant 11] “Socialization and relationships that didn’t really … well … apart from in my marriage, I guess. I don’t know if fibroids, if they were affecting my hormone levels. But I did decrease my libido so probably had an impact on my marriage as I was waiting. Not, I don’t know how you think it’s not something you could quantify but that’s just a sense that I got a change that I sensed in myself.” [Participant 4] “Like I’m fortunate, I have a really good husband at home, but I’ve definitely had to rely on him more like even some days it’s hard to want to make dinner, for example, just because it’s so emotionally tolling. So yeah, he’s definitely had to step up, and I’ve definitely relied on friends and family, a lot more, and just talking about everything and more detail, sometimes I feel like a broken record.” [Participant 9] |
| Work | Income Responsibility Identity Burden Insecurity |
“I also have to worry about where is my income coming in, I have to make sure that my mortgage is paid, my bills are paid and I can’t be irresponsible because I don’t want to suffer. I don’t want to suffer due to the fact that COVID and the lack of surgeries and what’s happening is going to affect me in the future, because it will.” [Participant 10] “I have to miss more work because I’m now going to massage therapy once a week and for deep tissue and then physiotherapy. I’m still on modified work duty for my last failed surgery of this. So that continues my work doesn’t know exactly when I’m going to be gone now.” [Participant 15] “My job is quite physical, lifting relatively heavy things. So I’ve had to ask for others’ help with those types of tasks, which is another mental health thing because I don’t like imposing on other people, and I don’t like feeling incompetent.” [Participant 14] “For me, how it affected me was I couldn’t go back to work. I was waiting, like, because of the surgeries I wasn’t well enough. I was constantly waiting. Like for all care, even just support when you have a new appliance, COVID, it affects all of that. When you can’t go into proper clinics, when you know there’s just, it just affected every element. And at this point now, I find myself not employed, because at some point your employers have to move on.” [Participant 11] “Fortunately, I’m able to work from home most days and so when I’m not feeling well, I can kind of step away for my, for my work and just, kind of, focus on me for a bit.” [Participant 9] “I haven’t been able to work as well, which is another factor … I’m going to lose business because of this.” [Participant 9] |
| Quality of life | Physical health Mental health |
“For that, so, from a health perspective it’s been pretty extreme, the delays. Right and you remember within those time periods. When you’re having surgeries that rely upon one successful completion to move to that next stage, to try and move you through … those periods, it affects your nutrition, it affects your sleep, it affects every aspect of your life.” [Participant 11] “I think there’s a line, of course, between life and death. And then there’s a line between a quality of life, where a person is still affected daily. And I think that is just as important as the life and death.” [Participant 12] “But I did decrease my libido so probably had an impact on my marriage as I was waiting. Not, I don’t know how you think it’s not something you could quantify but that’s just a sense that I got a change that I sensed in myself. So that was difficult.” [Participant 4] “I mean I’m functioning, but I spend a lot of time on the couch, right.” [Participant 6] “I have been, I’m not myself by no means. I used to be very active. I’m not as reliable as I once was; I’m cancelling on things constantly because either a) I’ve lost my voice, b) I’m in so much pain I can’t lift anything.” [Participant 10] “Yeah. It’s not urgent, it’s not life threatening. It’s just, it’s quality of life. It really just impacts me at the moment.” [Participant 15] |
Physical health
Nearly all participants identified ongoing physical health issues related to their delayed surgery. Physical ailments ranged from mild (“The fibroids in my uterus were getting larger and causing me to become more uncomfortable”) to pervasive and debilitating (“I have a very difficult time breathing, I have a very difficult time eating”). Several patients described ongoing physical pain and the effects on their daily lives, from modifications to exercise and activities of daily living, to inability to do one’s job effectively or at all, and prolonged use of pain medication to manage the pain.
Issues around the impact of delayed surgeries on physical health consequently led to impacts on mental health, specifically around worry (fear) and anxiety. Uncertainty related to when the surgery would occur and relief of physical health consequences was also expressed by many participants. For example, one participant indicated that they were afraid of having a heart attack due to their illness while waiting for surgery, and that worry about their physical health was having negative mental health impacts on them and their spouse.
Mental health
All participants described an impact on their mental health and this was the most discussed theme. One participant described mental health impacts as their reason for participating in the study, to raise awareness of the “toll” delays in surgery can have on people’s lives.
The impacts on mental health ranged from disappointment to depression and anxiety. Participants expressed a feeling of depression with the delay of surgery and related to navigating the impacts of the delay. Feeling depressed ranged from passive comments of feeling low (“Right now I’m a little depressed … but I keep telling myself let it go”) to newly physician-diagnosed depression. Many participants described anxiety and/or worry that was far reaching and extended beyond physical health (as described above) to concerns about their friends and family, their work and many aspects of their daily life. Many of these feelings of anxiety and/or worry were tied to a loss of control and uncertainty around the plans for their surgery, which are explored in the theme of uncertainty.
Family and friends impact
The impact of delaying surgery extended to family and friends in all cases. This was often related to requiring extra support with activities of daily living (e.g., housework or cooking) or emotional support for physical and mental health challenges directly related to the delayed surgery. Another commonly described impact was related to social relationships where participants cancelled social plans and trips to visit family and friends out of fear of missing a surgery date. Some participants also expressed safety concerns around contracting SARS-CoV-2 or other illness that would compound their existing health issues and prevent them from being able to have surgery.
Several participants also described strains in their relationships, outlining that their partners were stressed and worried about the changes in their physical and mental health, which in turn caused further stress for patients as they waited for surgery. Some participants also described changes to their sexual relationship with their partners because of difficulty with intercourse related to their unresolved health issues.
Work impact
Nearly all participants indicated that their delayed surgery directly affected their professional life. While some described changes in their ability to work, others disclosed losing their employment; for one participant this was described as an important loss to their identity. The theme of uncertainty reemerged when discussing the impact on the participants’ work life — participants felt that because of the uncertainty around surgical resumption they were unable to plan time off for surgery and this would have a downstream impact on work and colleagues. Similarly, participants held off taking vacation before surgery (before the cancellation), which in some cases led to burnout.
Other participants noted that they were unable to do their job normally or that they lost employment due to the physical or mental health impacts of waiting for surgery. This led to concerns about job security, and many endorsed struggles with earning a stable income and financial stress. For example, one participant worried that the small business they own would lose customers because they were not able to work.
Conversely, because of flexible, virtual work environments during the COVID-19 pandemic, some participants highlighted that this allowed them to be able to continue to work while managing their ongoing health issues.
Quality of life
For many participants the culmination of impaired physical and/or mental health, strained social interactions and employment challenges led to poorer quality of life. Interestingly, physical impairments were not always a driving factor; some participants commented that despite being able to physically function, their quality of life still declined. Many patients described their delayed surgery as having an overarching cloud over their lives.
System-level factors
Participants described several system-level factors primarily revolving around access to and communication with the health care system, including their health care providers (Table 2). Furthermore, several participants identified sources of accountability and responsibility for handling of the COVID-19 pandemic, including delayed surgeries, and even provided suggestions for how to manage these delays in the future.
Table 2:
Quotations representing the theme of system-level impacts
| Subtheme | Descriptive codes | Exemplar quotations |
|---|---|---|
| Health care resources | Access Hesitancy |
“Yeah, the only thing that I had to do, which was continuous since I had the catheter first put in, was going every 4 weeks and have it changed … The only thing that changed on that, is that the health unit out here, instead of me going to them, they came to my home to change the catheter.” [Participant 2] “I had a conversation with my doctor, but she just did it over the phone, rather than making me go into the office. I just talked to her about that it is delayed, and you know that I would continue to take pain medication for it, but I have not had to visit any emergency room because of it.” [Participant 8] “I did have an incident where I should … could have gone in but I just decided not to. And yeah, just the waiting around in the emergencies just driving me crazy.” [Participant 10] “And once I was able to walk and talk, they wheeled me out into a hallway in the neuro ward. And I spent 2 weeks outside of a room, in a hallway at [hospital]. That was pretty uncomfortable. I’ve definitely seen what the effects of lack of bed availability looks like.” [Participant 13] |
| Health care provider | Access Communication Responsibility |
“I don’t know about the avoiding delay, but I do definitely think it’s a system and set a cut-off time. For example, if we are a go as of 2:00 pm the day before surgery, we’re not going to cancel it. In other words, not waiting until the last minute to cancel and have a cut-off time the day before. So at least that person isn’t scared to go into the hospital the next morning and being afraid they’re going to be kicked back out.” [Participant 12] “They just said, ‘We’ll just have to wait. We’ve got no idea what a realistic timeline is, and we’ll keep you updated.’ So, I really have no expectations to hearing from them, until they know more. And I don’t really have expectations of things getting better anytime soon.” [Participant 13] “When the surgery was cancelled, I didn’t think to ask, but I also was not instructed what to do in terms of if I’m experiencing particular symptoms, whether that means I should go to the [emergency department], that kind of thing. So, I’ve just been suffering through it on my own, I guess.” [Participant 14] |
| Communication | Policy Government Health care provider Media |
Interviewer: How do you think the people that were making the decisions could do a better job in the future? “I guess they could be more consistent … like they come out and say one thing and then they come out and say another thing. You know.” [Participant 6] “That just speaks to leadership, again, I think it just sent so many false messages, so many confusing messages.” [Participant 11] “And I probably shouldn’t say that, but he’s a bit of a dick. So, the thyroid doctor, he showed no mercy, he showed no kindness, he was just a jackass but his assistant was amazing.” [Participant 10] “I definitely feel like giving more notice that a surgery’s going to be cancelled. Less than 24 hours’ notice is just not enough time for a person. I think it’s more emotionally devastating to be right on the cusp of finally dealing with the situation, and having it cancelled. So, I think giving a more advanced notice of cancellations would’ve been better.” [Participant 12] “I did connect with the oncology clinic and they’ve been super about it, um, but I have nothing but praise for that clinic overall in terms of how they keep you informed and stuff like that so that’s been good.” [Participant 1] “I was impressed, I got a phone call right, like, from the doctor, which it wasn’t just a, like, a nurse or a clinic staff or someone like that. So, it was a personal phone call and she just apologized and said there was nothing she could do, and she would get back in touch with me when she could.” [Participant 5] |
| Accountability and responsibility | Understanding Frustration Anger Communication Vaccination Public policy Government Health care system |
“Overall, this is a massive public policy failure.” [Participant 3] “Well, I mean, I understand that they had to maintain space in the health care system for COVID patients. And be able to create more ICU space, as is necessary, so I totally understand the rationale and thankfully I’m not speaking from the perspective of, say, a brain cancer patient where getting that surgery done now is so, so important. I think my perspective would be different if that were the case, but my surgery was one that could afford to be delayed and I recognize the need for it to have been based on having to keep beds available for those COVID patients.” [Participant 4] “I wish that things with regards to the pandemic had been handled much differently so that, potentially, patients and the hospital staff wouldn’t have been put in this situation.” [Participant 5] “I’m disappointed, but also understanding. Like, I understand the reason needed for it, I understand why the hospitals are not doing surgeries right now. I don’t hold ill will to the health care system.” [Participant 8] Interviewer: Did you think there was alternate options, maybe, like, something else they could have done in your eyes? “I think more restrictions earlier on would definitely be an alternative.” [Participant 8] “Our health care system is suffering, and I feel like the people that are making these decisions might be prioritizing social aspects before medical ones.” [Participant 8] “In my particular surgery, the chances of going to ICU after surgery were nil, very small. And so, I feel like my surgery could have been done, without adding to the ICU problem of being overcrowded. So, I think some of the surgeries that, in a limited quantity, should still have been done.” [Participant 12] |
Note: ICU = intensive care unit.
Health care resources
Several participants indicated that they required additional care or interacted with the health care system, beyond their baseline use, while they were waiting for surgery. This included more frequent visits with their primary care physician (including virtual care visits), consultation with psychologists, regular visits (every 4 weeks) to change a catheter, regular visits with a gastroenterologist for ileostomy (including a day surgery) and visits to the emergency department. Some participants expressed less health care use owing to concerns around contracting SARS-CoV-2 in physician offices or hospitals.
Communication
Discussion around communication focused primarily on communication with participants’ health care providers, specifically how and by whom the delay was communicated. Participants viewed communication as equally positive and negative overall. Negative comments were largely related to short notice of the delay and lack of information when communicating the delay. Participants who perceived communication to be negative expressed more anger and frustration. Conversely, many participants felt they were given sufficient notice about the delay and praised their health care providers for their communication. Participants who reported positive communication indicated that they received timely communication directly from their health care provider (surgeon or surgery clinic rather than the health care system), who demonstrated regret and concern for the patient. Several participants also commented on the effect that positive or negative communication from their health care providers had on their mental health and quality of life.
There were also some concerns raised about communication by the government and media. Specifically, some participants raised concerns that the government and health care system communication categorized these surgeries as “elective.” They voiced that although their condition may not be immediately life-threatening, it was life-altering, and their surgery was far from “elective.”
Perceived accountability and responsibility
When participants were asked what could have been done differently to minimize the impact of the COVID-19 response on surgery patients, discussion frequently deviated to anger and/or frustration about the current situation, specifically, the high number of COVID-19 cases necessitating surge capacity in our hospitals and the resulting decision to delay surgeries.
One participant summarized the overall sentiment of most participants: “I understand it, but I don’t like it.” Anger and frustration with the current situation were frequently associated with uncertainty.
However, other sources of anger and/or frustration were related to responsibility for the COVID-19 situation in our province. Participants frequently cited the government’s handling of the COVID-19 pandemic as the reason for having to delay surgeries. There were also strong feelings of divide toward people who have chosen not to receive the vaccine.
Despite negative views about the current situation, including delaying surgeries, there were also sentiments of understanding, especially regarding the decision to delay surgeries during the first wave of COVID-19, when less was known about the trajectory of the pandemic and when vaccines were not available.
COVID-19-specific factors
Participants highlighted unique factors related to the COVID-19 pandemic that complicated their delayed surgery experience (Table 3). Protecting and maintaining one’s health and isolation were 2 common threads around COVID-19-related impacts.
Table 3:
Quotations representing the theme of COVID-19-specific factors
| Descriptive codes | Exemplar quotations |
|---|---|
| Isolation Uncertainty Health care access Vaccine |
“Um, I think in terms of logistics it’s just been a, more of a preventative, just kind of keeping myself on the safe side at this point in terms of perhaps being a higher risk or maybe that our vaccine didn’t quite give me enough of the boost that I needed or anything like that. But, you know, better safe than sorry at this point.” [Participant 1] “Yeah and, like, I’d already been isolating for like 2 weeks because, like, if you get; if you show up at the hospital with the sniffles, we’re cancelling your surgery. Right. Which is very reasonable. But then it’s like, cool, I’m locked down for 2 weeks. Um, and then it was like, a week out it got cancelled. That was a week of locking down that was kind of wasted.” [Participant 3] “Yeah, obviously with COVID I’m not really going out and socializing so that has been affected.” [Participant 14] “Well, COVID in general has affected the ability to socialize. And the fact that if I’m going to be going into surgery, I can’t take any chance of catching COVID, so socialization is nothing. It’s not there, because you can’t take that chance, because surgery might be around the corner. And you can’t chance possibly being sick and it being cancelled.” [Participant 12] “There have been times that I’ve thought of, about going in, even going into the doctor and stuff. And I’ve been hesitant about doing it … Because of going in, it feels like you’re walking into a germ factory maybe, right now.” [Participant 12] |
Participants expressed concern or challenges with accessing health care services because of the COVID-19 pandemic, but there were also some advantages to accessing care during the pandemic with the advent of virtual care. Some participants indicated hesitation in accessing in-person health care for fear of acquiring SARS-CoV-2 infection in public places. Similarly, the fear of contracting SARS-CoV-2 or other viruses in their vulnerable condition was a great concern. The fear was twofold — they were fearful of becoming severely ill but also fearful of further surgical delays if they were to become ill at a time when a surgery date became available. Their fear of becoming ill resulted in physical isolation and, consequently, psychological isolation for many participants. Moreover, their poor mental health also made socialization (virtual or in person) more challenging.
Uncertainty
Uncertainty about health and surgery resumption had a large impact on participants (Table 4). All participants found that the uncertainty surrounding their surgery and physical health was pervasive and affected many aspects of their life. Uncertainty was described as a loss of control and lack of information about surgery and underlying health. One participant described this loss of control as “being held hostage to what’s happening in the hospital; like … total limbo.”
Table 4:
Quotations representing the theme of uncertainty
| Descriptive codes | Exemplar quotations |
|---|---|
| Worry Anxiety Quality of life Physical health Plan for future |
“… anguish and uncertainty and whatever because of the lack of communication, no answers and no timeline; well, unfortunately it’s, well, you could die before you get your knee replacement, right.” [Participant 7A] “Even the facts of, like, if I was going to go somewhere, right, I would love to make all these plans, but I can’t because I don’t know if I can speak and I don’t know if I can, I don’t know if I can make any kind of future plans, because I’m like, oh, I have to wait for surgery.” [Participant 10] “It delays everything; it puts absolutely everything on hold. I think when I mentioned a cumulative effect for me. Before the Mar. 31, 2021, surgery, which was the reversal. That had been postponed so, then I was postponed for November, scheduled for Mar. 31. We are holding on by a thread in our home to see if I’m even going to get in. Or if things are going to be cancelled because we watch the numbers; everyone’s watching the numbers.” [Participant 11] “I’m at their mercy basically of when, when they’ll get me back in. And just not really being given any sort of alternative option. I mean I don’t know what that would look like, or what I even expect but, yeah, you just kind of feel very left in the dark.” [Participant 9] “… loss of control and all of those unknowns, it’s just hard to comprehend, and I guess just, yeah, plan for your future because I have no idea. So even just, like, on a mental health toll it’s, it’s impacted my day to day and wanting to make plans.” [Participant 9] “It would definitely be to just have that date in mind and just be able to mentally prepare for it. So, it was difficult to not have a date and to just be kind of in limbo and waiting and not knowing both personally and professionally how that was going to be affecting things in my life.” [Participant 4] |
In addition to feelings of uncertainty resulting from the perception of loss of control and being uninformed, uncertainty was also described as a reason for poor mental health. This association was rooted in feelings of anxiety, fear and worry about the unknown consequences of delaying surgery on their physical health and uncertainty about the future.
Uncertainty resulted in poor mental health but also logistic challenges in several areas of life. For example, uncertainty affected planning time off work for surgery and the subsequent recovery. As well, it affected participants’ ability to commit to social activities, engage in family planning and pursue postsecondary education. Uncertainty frequently led to discussion about the impact of the delayed surgery on friends and family, and the participants’ professional lives.
Interpretation
We found that the impact of delaying surgeries to manage the surge of COVID-19 patients was diffuse and consequential on the lives of patients. Four interconnected themes emerged: individual-level impacts (subthemes: physical health, mental health, family and friend impact, work impact, quality of life), system-level factors (subthemes: communication, health care resources, perceived accountability and responsibility), COVID-19-specific factors and uncertainty.
The physical effect of delaying surgery has been illustrated in the prepandemic setting. Exceeding the optimal interval from diagnosis to surgery has been associated with poor outcomes in many diseases.6,7,16–18 For example, delayed cancer surgery results in poor disease-free survival,18–20 and patients with delayed cardiac surgery experience greater morbidity and mortality, and longer hospitalizations, and are more likely to die postoperatively.21,22 Delaying surgeries considered less urgent is associated with an increased cost to patients (e.g., increased pain, decreased quality of life) and the health care system.23–27 Our study confirmed that perceived physical health was compromised by the delays in surgery; however, the physical impact was less prominent and perhaps the driver of more significant effects on participants’ mental health and quality of life.
Distress among patients waiting for surgery has been previously described; however, there is a need for additional research on the burden of delayed surgeries during the COVID-19 pandemic given the unique and unprecedented nature of surgical delays during the pandemic, which was highlighted in our study with the COVID-19-specific factors that mediated the other impacts.28 A recent study of patients waiting for cancer surgery owing to COVID-19-related capacity limits reported similar findings to ours; participants had high levels of distress, stress, anxiety and depression.8 The similarity between our findings and those of Forner and colleagues, 8 despite a small number of participants undergoing cancer surgery in our study, suggests that the experience of waiting for surgery during the COVID-19 pandemic is similar across surgeries. We hypothesize that the unifying characteristic among patients waiting for any type of surgery during the COVID-19 pandemic is uncertainty, specifically, the unpredictability of the pandemic and response. Uncertainty was a prominent theme that arose in our study, and many participants underlined the connection between the uncertainty and the distress and burden this placed on all aspects of their lives. Minimizing uncertainty is challenging in the context of the COVID-19 pandemic because it has been, in and of itself, unpredictable. Our findings highlight that timely, personalized, pragmatic and compassionate 2-way communication between health care providers and patients is needed and may minimize distress in patients waiting for surgery, even if certainty cannot be provided.28–30
In addition to the profound individual-level impacts, there are also effects of delaying nonurgent surgeries on health care systems. A review of reorganization of surgical services during public health emergencies identified downstream consequences of delaying surgery, such as alterations in medical training.31 Additional research is needed to explore other potential effects of delaying nonurgent surgeries on health care systems, such as intensity of resource use while patients are waiting for surgery (e.g., emergency department visits and hospital stays requiring intensive care stay). Mitigating the backlog of surgeries due to the response to COVID-19 by managing surgical waitlists and transforming surgical care is another important area of work to deal with the delayed surgeries. Approaches to decrease wait time and increase efficiency of surgical care to create more capacity, and increase quality, during the COVID-19 pandemic and beyond have been proposed.32–34 These approaches include a single-entry system for surgical referral (i.e., central access and triage model), team-based care, and implementation of guidelines that improve care and care processes.32–34 However, these approaches require system-wide change that takes time and substantial investments to implement, and an even longer time for patients and health care systems to reap the benefits. Focusing on improving the surgery waiting period could minimize the impact of delaying surgery during and after the COVID-19 pandemic. The waiting period is fraught with consequences to patients’ physical and mental health.6 Based on our findings, interventions that support patient mental health are needed during surgery waiting periods. Studies suggest that strategies such as educating patients about the potential mental health consequences of waiting for surgery, regular communication with health care providers and mental health support (e.g., self-management approaches and peer support) could improve the impact of surgical delays on patients’ mental health.28 Our findings support the need and potential utility of these strategies, but future research is needed to explore the critical components for successful strategies and their implementation.
Our study has several strengths. Data collection was continued after we reached thematic saturation to ensure a broad perspective of a varied patient sample, and we used iterative member checking. We captured patient perspectives from diverse backgrounds and clinical areas, and our team engaged in peer debriefing during analysis.
Limitations
Our findings should be interpreted with limitations in mind. Participants were limited to a single province, during the largest wave to date of the COVID-19 pandemic, which may differ from the unique experience with COVID-19 of each province. We did not inquire about the length of patients’ delay, which is a factor that may have affected the participants’ experience. Moreover, although we tried to capture a variety of responses based on age, gender, geographical location and type of surgery, there were few patients who had (or planned to have) surgery at small community hospitals or were undergoing surgery for cancer. The reason for the small number of patients in these categories may be related to the small number of surgeries conducted at small community hospitals and to the fact that cancer surgeries were prioritized in Alberta during disruptions to surgical services. Finally, we chose to recruit patients through social media because recruiting through surgery clinics was challenging owing to limited in-person visits during the pandemic and because we wished to reach patients throughout the province. However, this may have selectively included patients who had strong responses and opinions on the delay of surgeries, which may have skewed our findings.
Conclusion
Our findings illustrate the direct and substantial impact delaying surgery has on patients, specifically the individual-level impacts (subthemes: physical health, mental health, family and friend impact, work impact, quality of life), system-level factors (subthemes: communication, health care resources, perceived accountability and responsibility), COVID-19-specific factors and uncertainty. The interplay between the themes identified in our study suggests it is important to consider all these factors when measuring and developing strategies to mitigate the impact of delaying surgery. During the ongoing COVID-19 pandemic, health care systems have had to make difficult decisions based on incomplete and evolving evidence. While health care system decision-makers anticipated the impact of delaying surgeries on patients, they had little choice owing to strained health care resources. Our study provides evidence of the anticipated impact on patients, which supports the need for investments in mental health, occupational and social supports with clear, personalized and compassionate communication strategies during periods of delay to address all these factors. These investments should be explored to improve surgical care during the COVID-19 pandemic and beyond.
Supplementary Material
Footnotes
Competing interests: Mary Brindle reports a grant from the Canadian Institutes of Health Research to explore how the Surgical Safety Checklist could be improved, a grant from Maternal Newborn Child & Youth to explore the effectiveness of a neonatal Enhanced Recovery After Surgery (ERAS) protocol, honoraria for speaking at Hong Kong University Department of Surgery and the University of Manitoba (both < $1000), an unpaid role on the Data and Safety Monitoring Board for a US randomized controlled trial on ERAS in pediatric patients and an unpaid position as secretary of the ERAS Society. No other competing interests were declared.
This article has been peer reviewed.
Contributors: Khara Sauro was responsible for the conception of the study and study design, supervision of data collection, data analysis and interpretation of the findings, and drafted the manuscript. Mary Brindle contributed substantially to the design and interpretation of the findings and provided critical intellectual contributions to the manuscript. The remaining authors contributed to data collection and analysis, and critically revised the manuscript, therefore providing important intellectual contributions. All authors gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Funding: This work was funded by a grant from the Canadian Institutes of Health Research, awarded to Khara Sauro.
Data sharing: Deidentified data may be made available on reasonable request to the corresponding author.
Supplemental information: For reviewer comments and the original submission of this manuscript, please see www.cmajopen.ca/content/11/1/E90/suppl/DC1.
References
- 1.Timeline: WHO’s COVID-19 response. Geneva: World Health Organization; [accessed 2022 Sept. 12]. Available https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline?gclid=Cj0KCQjw5oiMBhDtARIsAJi0qk2rozzTB4QiPygy20qQDFmw_ULgGDYd7Qj9QX60FvIgQA6aVu-iKkkaAttTEALw_wcB#event-115. [Google Scholar]
- 2.Valenza F, Papagni G, Marchianò A, et al. Response of a comprehensive cancer center to the COVID-19 pandemic: the experience of the Fondazione IRCCS-Istituto Nazionale dei Tumori di Milano. Tumori. 2020 May 4; doi: 10.1177/0300891620923790. 300891620923790. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Prin M, Guglielminotti J, Mtalimanja O, et al. Emergency-to-elective surgery ratio: a global indicator of access to surgical care. World J Surg. 2018;42:1971–80. doi: 10.1007/s00268-017-4415-7. [DOI] [PubMed] [Google Scholar]
- 4.Tam DY, Qiu F, Manoragavan R, et al. The impact of the COVID-19 pandemic on cardiac procedure wait list mortality in Ontario, Canada. Can J Cardiol. 2021 Oct;37(10):1547–1554. doi: 10.1016/j.cjca.2021.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang J, Vahid S, Eberg M, et al. Clearing the surgical backlog caused by COVID-19 in Ontario: a time series modelling study. CMAJ. 2020;192:E1347–56. doi: 10.1503/cmaj.201521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oudhoff JP, Timmermans DRM, Knol DL, et al. Waiting for elective general surgery: impact on health-related quality of life and psychosocial consequences. BMC Public Health. 2007;7:164. doi: 10.1186/1471-2458-7-164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carr T, Teucher U, Mann J, et al. Waiting for surgery from the patient perspective. Psychol Res Behav Manag. 2009;2:107–19. doi: 10.2147/prbm.s7652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Forner D, Murnaghan S, Porter G, et al. Psychosocial distress in adult patients awaiting cancer surgery during the COVID-19 pandemic. Curr Oncol. 2021;28:1867–78. doi: 10.3390/curroncol28030173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hunt MR. Strengths and challenges in the use of interpretive description: reflections arising from a study of the moral experience of health professionals in humanitarian work. Qual Health Res. 2009;19:1284–92. doi: 10.1177/1049732309344612. [DOI] [PubMed] [Google Scholar]
- 10.Thorne S, Kirkham SR, MacDonald-Emes J. Interpretive description: a noncategorical qualitative alternative for developing nursing knowledge. Res Nurs Health. 1997;20:169–77. doi: 10.1002/(sici)1098-240x(199704)20:2<169::aid-nur9>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 11.Thorne S, Kirkham SR, O’Flynn-Magee K. The analytic challenge in interpretive description. Int J Qual Methods. 2004;3:1–11. [Google Scholar]
- 12.Thorne S. Qualitative research for applied practice. 2nd ed. London (UK): Routledge; 2016. [Google Scholar]
- 13.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–57. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- 14.COVID-19 Outbreak update. Ottawa: The Government of Canada; [accessed 2022 Sept. 12]. Available: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection.html?&utm_campaign=gc-hc-sc-coronavirus2021-ao-2021-0005-9834796012&utm_medium=search&utm_source=google_grant-ads-107802327544&utm_content=text-en-434601690164&utm_term=covid. [Google Scholar]
- 15.NVivo 12.0. Doncaster (AU): QSR International; 2021. [Google Scholar]
- 16.Zhao F, Qi N, Zhang C, et al. Impact of surgical wait time on survival in patients with upper urinary tract urothelial carcinoma with hydronephrosis. Front Oncol. 2021;11:698594. doi: 10.3389/fonc.2021.698594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pincus D, Ravi B, Wasserstein D, et al. Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA. 2017;318:1994–2003. doi: 10.1001/jama.2017.17606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deidda S, Elmore U, Rosati R, et al. Association of delayed surgery with oncologic long-term outcomes in patients with locally advanced rectal cancer not responding to preoperative chemoradiation. JAMA Surg. 2021;156:1141–9. doi: 10.1001/jamasurg.2021.4566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heiden BT, Eaton DB, Jr, Engelhardt KE, et al. Analysis of delayed surgical treatment and oncologic outcomes in clinical stage I non-small cell lung cancer. JAMA Netw Open. 2021;4:e2111613. doi: 10.1001/jamanetworkopen.2021.11613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matsuo K, Shimada M, Matsuzaki S, et al. Wait-time for adjuvant radiotherapy and oncologic outcome in early-stage cervical cancer: a treatment implication during the coronavirus pandemic. Eur J Cancer. 2021;148:117–20. doi: 10.1016/j.ejca.2021.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohamed MO, Banerjee A, Clarke S, et al. Impact of COVID-19 on cardiac procedure activity in England and associated 30-day mortality. Eur Heart J Qual Care Clin Outcomes. 2021;7:247–56. doi: 10.1093/ehjqcco/qcaa079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rexius H, Brandrup-Wognsen G, Odén A, et al. Mortality on the waiting list for coronary artery bypass grafting: incidence and risk factors. Ann Thorac Surg. 2004;77:769–74. doi: 10.1016/j.athoracsur.2003.05.007. discussion 74–5. [DOI] [PubMed] [Google Scholar]
- 23.Traylor J, Koelper N, Kim SW, et al. Impact of surgical wait time to hysterectomy for benign gynecologic disease. J Minim Invasive Gynecol. 2021;28:982–90. doi: 10.1016/j.jmig.2020.08.486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Elit LM, O’Leary EM, Pond GR, et al. Impact of wait times on survival for women with uterine cancer. J Clin Oncol. 2014;32:27–33. doi: 10.1200/JCO.2013.51.3671. [DOI] [PubMed] [Google Scholar]
- 25.Berger A, Bozic K, Stacey B, et al. Patterns of pharmacotherapy and health care utilization and costs prior to total hip or total knee replacement in patients with osteoarthritis. Arthritis Rheum. 2011;63:2268–75. doi: 10.1002/art.30417. [DOI] [PubMed] [Google Scholar]
- 26.Mather RC, III, Hug KT, Orlando LA, et al. Economic evaluation of access to musculoskeletal care: the case of waiting for total knee arthroplasty. BMC Musculoskelet Disord. 2014;15:22. doi: 10.1186/1471-2474-15-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Snider MG, MacDonald SJ, Pototschnik R. Waiting times and patient perspectives for total hip and knee arthroplasty in rural and urban Ontario. Can J Surg. 2005;48:355–60. [PMC free article] [PubMed] [Google Scholar]
- 28.Gagliardi AR, Yip CYY, Irish J, et al. The psychological burden of waiting for procedures and patient-centred strategies that could support the mental health of wait-listed patients and caregivers during the COVID-19 pandemic: a scoping review. Health Expect. 2021;24:978–90. doi: 10.1111/hex.13241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Howe LS, Wigmore D, Nelms N, et al. Perioperative family updates reduce anxiety and improve satisfaction: a randomized controlled trial. J Patient Cent Res Rev. 2021;8:107–12. [PMC free article] [PubMed] [Google Scholar]
- 30.Hartlief GA, Niemeijer AS, Lamberts KF, et al. The impact of early information concerning the surgical operations on anxiety in patients with burns. Burns. 2021;47:847–53. doi: 10.1016/j.burns.2020.08.013. [DOI] [PubMed] [Google Scholar]
- 31.O’Rielly C, Ng-Kamstra J, Kania-Richmond A, et al. Surgery & COVID-19: a rapid scoping review of the impact of COVID-19 on surgical services during public health emergencies. BMJ Open. 2021;11:e043966. doi: 10.1136/bmjopen-2020-043966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Urbach DR, Martin D. Confronting the COVID-19 surgery crisis: time for transformational change. CMAJ. 2020;192:E585–6. doi: 10.1503/cmaj.200791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kasivisvanathan R, Tilney HS, Jhanji S, et al. The ‘hub and spoke model’ for the management of surgical patients during the COVID-19 pandemic. Int J Health Plann Manage. 2021;36:1397–406. doi: 10.1002/hpm.3243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ljungqvist O, Nelson G, Demartines N. The post COVID-19 surgical backlog: Now is the time to implement enhanced recovery after surgery (ERAS) World J Surg. 2020;44:3197–8. doi: 10.1007/s00268-020-05734-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.