Abstract
Iatrogenic chyle leak is commonly seen when dissection happens very low in neck. Management of chyle leak is conservative with compression dressing, fat restricted diet, somatostatin analogues. Surgery is required in extreme cases with failure of conservative treatment. This is a retrospective observational study carried out from a prospectively maintained database. A total of 6482 head and neck surgeries with neck dissections were carried out between January 2015 till July 2020 at our tertiary cancer center. Out of which there were 52 cases of chyle leak reported post neck dissection. All details regarding age, sex, primary tumor location, surgery performed, level of nodal dissection performed, details related to chyle leak from beginning day and its progression and management offered. The median age in the study group was 42 years (24–70 years). Chyle leak was most commonly seen on left side (88.5%). Low output leaks(n = 43) resolved within a median period of 9 days (5–13 days) period of conservative management. High output leak (n = 9) had leak resolution within a median period of 12 days (7–19 days). Patients who had received preoperative radiotherapy and who had extra nodal extension in lymph nodes had significantly higher incidence of high output leaks. Chyle leak is a rare but serious complication in head and neck surgery. Timely identification and management is crucial. Conservative management is mainstay. Surgical management is instituted in cases of failure of conservative management.
Keywords: Thoracic duct, Chyle leak, Neck dissection, Head and neck, Somatostatin
Introduction
Chyle leak is a rare complication associated with head and neck surgery. It is a serious complication seen in upto 0.5–1.4% of thyroidectomies and 2–8% of neck dissections [1]. It is more common on left side, but seen upto 25% in right side [1–3]. The fragile anatomy of thoracic duct makes it prone to iatrogenic injury during surgery in neck. The thoracic duct is the largest lymphatic trunk carrying lymph from left side of the body and right side of body below diaphragm. The right adult lymphatic duct carries lymph from right side of thorax, arm and head and neck region.
Iatrogenic chyle leak is commonly seen when dissection happens very low in neck due to metastatic nodes at level IV and in patients with prior history of irradiation [1]. Management of chyle leak in majority of cases are conservative with compression dressing, fat restricted diet, somatostatin analogues. Surgery is required with failure of conservative treatment with either intrathoracic thoracic duct ligation or local exploration with duct closure in neck. There is no defined protocol for management of chyle leak. We share here our experience of 52 cases of post-operative chyle leak.
Materials and Methods
Data Collection
This is a retrospective observational study carried out from a prospectively maintained database. A total of 6482 head and neck surgeries with neck dissections were carried out between January 2015 till July 2020 at our tertiary cancer center. Out of which there were 52 cases of chyle leak reported. All details regarding age, sex, primary tumor location, surgery performed, level of nodal dissection performed, details related to chyle leak from beginning day and its progression and management offered. Histopathology was also noted.
Intraoperative Precaution
All patients of chyle leak were detected post neck dissection. It is a norm to give ventilatory positive pressure to increase the intrathoracic pressure intraoperatively to look for chyle leak or bleeding in all patients undergoing neck dissection. 32 chyle leaks were detected intraoperatively and they were managed with duct identification and suture placement with 4–0 polypropylene or with clip application. Rest 20 patients developed chyle leak without any intraoperative evidence of the same.
Management
Milky white drain output was concluded to be chyle leak. [Fig. 1]. All cases of chyle leak were managed conservatively as part of initial management. Chyle output less than 500 ml/24 h was considered low output and more than 500 ml/24 h was considered high output. Conservative management included closed suction drainage, pressure dressing in the supraclavicular region, fat restricted diet, use of medium chain fatty acid (MCFA) and movement restriction. Subcutaneous octreotide 100ug eight hourly was given in all patients irrespective of drain output. Strict weight charting was done. Failure of chyle leak resolution within 14 days of detection along with persistence of high output and clinical deterioration in the form of weight loss, wound complication and infection were considered failure of conservative management. Three patients with persistent high output chyle leak failed conservative management and thus required VATS thoracic duct ligation [Fig. 2]. There was no mortality reported. All patients completed their adjuvant treatment and were followed up for at least 6 months.
Fig. 1.

Showing Milky white aspirate suggestive of chyle leak
Fig. 2.
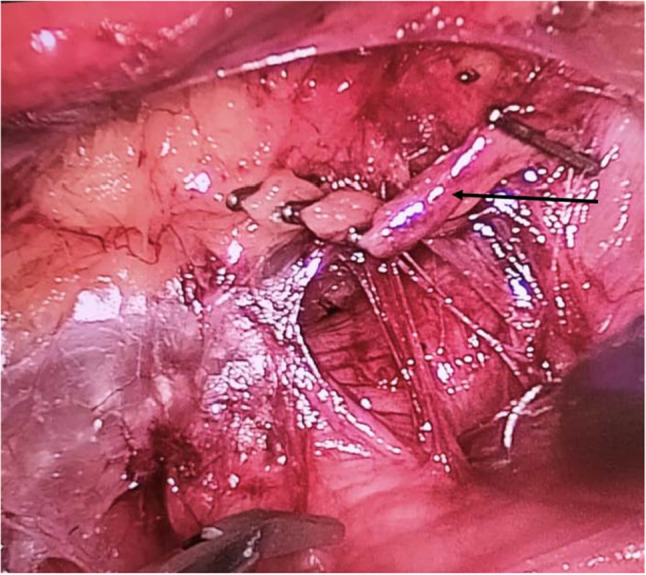
VATS thoracic duct ligation of patients who had failure of conservative management. Arrow points towards thoracic duct which has been clipped
Statistical Analysis
Statistical Analysis was done with IBM SPSS Statistics for Windows, version 25 (IBM Corp., Armonk, N.Y., USA). Demographic assessment was done with descriptive statistics. Categorical variables were compared using chi-square test. P-value of less than 0.05 was considered significant.
Results
A total of 6,482 head and neck surgeries involving neck dissections were performed during the study period and there were reported 52 post-operative chyle leaks. The median age in the study group was 42 years (24–70 years). There were 39(75% males and 13(25%) females. Primary sites for which surgery was performed were oral cavity (90.4%), thyroid (5.8%) and larynx (3.8%). Most common histologies were squamous cell carcinoma (94.2%) followed by papillary thyroid cancer (3.8%) and medullary thyroid cancer (1.9%). All patients had undergone neck dissection. Chyle leak was most commonly seen on left side (88.5%). [Table 1].
Table 1.
Demographic data of the study population
| Parameters | Frequency | |
|---|---|---|
| Median age | 42 years(24–70 years) | |
| Gender | Male | 39(75%) |
| Females | 13(25%) | |
| Side | Left | 46(88.5%) |
| Right | 6(11.5%) | |
| Site | Oral cavity | 47(90.4%) |
| Thyroid | 3(5.8%) | |
| Larynx | 2(3.8%) | |
| Histology | Squamous cell carcinoma | 49(94.2%) |
| Papillary thyroid cancer | 2(3.8%) | |
| Medullary thyroid cancer | 1(1.9%) | |
| Preoperative radiotherapy | Received | 12(23.1%) |
| Not received | 40(76.9%) | |
| Level of Lymph node dissection performed | Level 1,2,3,4,5 | 35(67.3%) |
| Level 1,2,3,4 | 12(26.9%) | |
| Level 2,3,4 | 3(5.8%) | |
| Nodal stage | N0 | 6(11.5%) |
| N1 | 19(36.5%) | |
| N2a | 15(28.8%) | |
| N2b | 4(7.7%) | |
| N3b | 8(15.4%) | |
| Extra-nodal extension | Present | 14(26.9%) |
| Absent | 38(73.1%) | |
All patients after completion of neck dissection were subjected to ventilatory positive pressure intraoperatively to look for chyle leak and bleeding. In 32(61.5%) patients, chyle leak was detected intraoperatively and was identified and ligated with either 4–0 polypropylene simple sutures or clips to confirm stoppage of leak. All patients received conservative management at the very onset of chyle leak detection. Three patients failed conservative management after 14 days with persistence of high output were subjected to VATS thoracic duct ligation. [Fig. 2] There were no mortality. All patients received timely adjuvant treatment within 6 weeks of surgery. Median duration of chyle leak was 9.5 days (5–19 days). Median hospital stay was 14 days (12–32 days). [Table 2].
Table 2.
Details of Chyle leak
| Parameters | Frequency | |
|---|---|---|
| Intraoperatively detected | Detected and fixed | 32(61.5%) |
| Undetected | 20(38.5%) | |
| Output | Low output(< 500 ml/24 h) | 43(82.7%) |
| High output(> 500 ml/24 h) | 9(17.3%) | |
| Wound infection | Yes | 4(7.7%) |
| No | 48(92.3) | |
| Median duration of chyle leak | Low output(< 500 ml/24 h) (n = 43) | 9 days(5–13 days) |
| High output(> 500 ml/24 h) (n = 9) | 12 days(7–19 days) | |
| Median maximum 24 h output of chyle | 250 ml (100–1200 ml/24 h) | |
| Median hospital stay | 14 days(12–32 days) | |
Forty three patients had low output leaks and they all resolved within a median period of 9 days (5–13 days) of conservative management. Nine patients had high output leak, of which 3 required surgical management with VATS thoracic duct ligation and rest 6 patients had resolution of their leak within a median period of 10 days (7–12 days) of conservative management.
Patients who had received preoperative radiotherapy, patients and who had extra nodal extension in lymph nodes were correlated with output (low output and high output) with chi-square test and it was found that.
Out of 12 patients who had received preoperative radiotherapy, 8(66.6%) patients had high output(> 500 ml/24 h) chyle leak (p value = 0.001).
Out of 14 patients who had extra nodal extension, 8(57.1%) patients had high output chyle leak (p value = 0.001).
Discussion and Literature review
Chyle leak after head and neck surgeries is caused by inadvertent injury to thoracic duct during neck dissection. It is a rare and serious complication with incidence upto 1–2.5%. It most commonly occurs on left side [1–3]. Chyle leak can produce severe nutritional, metabolic and immune disability in patients [3].
Anatomy of Thoracic Duct
It begins as cisterna chyli at the level of L2 vertebrae and ascends along the anterior surface of lumbar vertebrae between aorta and azygous vein to enter the thorax via the aortic hiatus in the posterior mediastinum. In the thorax, it ascends on left side posterior to the aortic arch and lateral to esophagus and enters the root of neck where it is bounded anteriorly by the left common carotid artery, vagus nerve and internal jugular vein, medially by esophagus, posteriorly by vertebra and laterally by omohyoid. Here the thoracic duct arches superiorly and laterally, anterior to scalene muscle and phrenic nerve [5]. It courses 3–5 cm above the clavicle and can go as high as the level of thyroid cartilage also [6, 7]. and terminates in Internal jugular vein (46%), confluence of IJV and subclavian vein (32%) or subclavian vein (18%) [4]. The length of an adult thoracic duct is 36–45 cm with an average diameter of 5 mm [8]. The diameter of thoracic duct decreases from abdomen to the thorax and then again increases again in the cervical region reaching upto 1 cm as it empties in large veins in the neck [9]. The diameter can increase with rise in intraabdominal or intrathoracic pressures [1].
Functions of Thoracic Duct
The thoracic duct has a crucial role in fluid balance and return of lymph to systemic circulation. Chyle comprises of lymphatic fluid and chylomicrons. Lymphatic fluid contains protein, white blood cells, electrolytes, fat-soluble vitamins, trace elements, and glucose absorbed from the interstitial fluid, which is then returned to the systemic circulation. Chylomicrons are composed of esterified monoglycerides and fatty acids combined with cholesterol and proteins. These are the breakdown products of long chain fatty acids by bile salts and absorbed into the lymphatic system by lacteals present in the villous region of intestines. Medium chain fatty acids are more water soluble thus absorbed directly into the portal veins not via lacteals [10]. Chyle propagation is multifactorial ranging from muscular action of breathing, smooth muscles in the duct and internal valves preventing back flow. Diet, intestinal function, physical activity and changes in intrathoracic and intraabdominal pressures modulate chyle flow [10]. These principles form the basis of conservative management in chyle leak including fat restricted diet, use of medium chain fatty acid powders and bed restriction.
Pathophysiology of Chyle Leak
Chyle leak in head and neck surgery is mostly iatrogenic due to inadvertent injury during neck dissection. Prior irradiation and presence of large nodal disease makes the surgery more challenging and increases the risk of iatrogenic duct injury [11, 12]. In the current study, it was found that prior irradiation and large nodal burden with extra-nodal extension were significantly associated with high volume chyle leak (p value = 0.001). Early identification of chyle leak and starting its management at the earliest improves result. Consequences of acute large volume chyle leak leads to detrimental effects on nutrition (loss of protein, fat- and fat-soluble vitamins, trace elements), electrolyte imbalance (hyponatremia, hypochloremia and hypoproteinemia) and immunosuppression [1].
Chyle leak can lead to increased wound complication like infection or wound breakdown due to intense inflammatory reaction. Chyle accumulation below the skin flap can decrease tissue perfusion and cause flap necrosis [13]. In some cases, cervical chyle leak can enter the mediastinum and cause chylothorax presenting as shortness of breath [1].
Management
It is customary to check for chyle leak in all patients undergoing neck dissection by either by Valsalva maneuver or by pressing the abdomen and increasing the intraabdominal pressure. If chyle leak is evident then following are the options to be considered.
4–0 polypropylene simple sutures or clip applied to close the duct.
Locoregional flaps with clavicular head of sternocleidomastoid or anterior scalene flap or pectoralis major flap can be used to provide coverage to the surgical bed [14–16].
Sometimes even after identifying and tackling the leak intraoperatively chyle accumulation happens in the neck in the post-operative period as evident in 32 patients in the present study. Chyle leak may not be identified intraoperatively depending on the prolonged fasting status of the patient preoperatively and can manifest postoperatively after feeding starts. Milky cream colored fluid is characteristics [Fig. 1]. Drain fluid triglycerides greater than 100 g/dl, drain fluid triglycerides more than serum triglycerides or presence of chylomicrons in drain fluid confirms the diagnosis of chyle leak [1].
In the post-operative period base on drain output patients are classified into low output(< 500 ml/24 h) and high output(> 500 ml/24 h). Conservative management is administered to all patients first which includes.
Restricted activity and head elevation upto 30–40 degrees. Stool softeners should be administered to reduce intrathoracic and intraabdominal pressures.
Adequate fluid and electrolyte supplementation to prevent hypovolemia.
Fatty diet should be stopped immediately and medium chain fatty acid (MCFA) diet must be started promptly along with multivitamin supplementation. Since MCFA diet bypasses the lymphatic system and gets absorbed directly being water soluble, chyle production decreases thus giving time to heal.
In persistent high output Total parenteral nutrition can be tried since it bypasses the lymphatic system completely thus more effective than MCFA, but it has its own complications related to venous access, metabolic disturbances and high cost [7].
Continuous suction drainage to monitor output and prevent accumulation and pressure dressing are crucial part of management. Vaccum assisted closure of the wound to remove fluid and shrink wound size has promising results but requires further study [17].
We started 100 ug Octreotide, a long acting somatostatin 8 hourly immediately after identifying a chyle leak and advocate to continue 2 days after resolution of chyle leak. If chyle leak persists even after 2 weeks along with nutritional impairment and persistent high output we advocate going for surgical intervention. Somatostatin decreases chyle production via reduction of gastric, pancreatic and intestinal secretions. It causes smooth muscles vasoconstriction in splanchnic and lymphatic vessels to decrease lymph production and lymph flow [17]. Jain et al. reported their experience in 19 patients where all patients were managed with conservative management and octreotide was given for 5–7 days in low and high output chyle leaks [18]. Swanson et al. reported their experience in 12 patients receiving octreotide and their chyle leak resolved in 5.5 days and they administered octreotide for 9 days total [11]. There is no clear-cut guidelines for the duration of octreotide administration. In the current study, there were 43 patients who had low output leaks and they all resolved within a median period of 9 days (5–13 days) period of conservative management. Nine patients had high output leak, of which 3 required surgical management with VATS thoracic duct ligation and rest 6 patients had resolution of their leak within a median period of 10 days (7–12 days) of conservative management.
Use of topical agents like OK-432 or tetracycline has been described to be used at the time of surgery or postoperatively by either drain tube administration or percutaneous injection. Idea is to produce fibrosis and obliterate the surgical field [14, 19]. But this makes neck re exploration difficult. Sclerosants can also injure surrounding structures like phrenic nerve and IJV [20]. Other agents that are producing successful results are Cyanoacrylate adhesives, fibrin glue and polyglactin mesh [21–23].
Surgical management is reserved for patients who fail conservative management. We performed VATS thoracic duct ligation in three patients who had persistent high output leak even after 14 days and along with nutritional impairment in the form of > 5 kgs weight loss in 2 weeks. Surgery was performed via right thoracoscopic approach and thoracic duct was ligated at the supra diaphragmatic hiatus between aorta and azygous vein. Other procedures are.
Local exploration and identification of the leaking duct and talking it with non-absorbable sutures along with local flaps. Problem is difficulty in identifying the leaking duct due to past surgery leading to adhesions and fibrosis.
Percutaneous transabdominal cannulation of thoracic duct at cisterna chyli and lymphography and embolization with coils or adhesives is a safe minimally invasive technique. Reported success rate is 45–70% [17, 24]. If facility is available then this is a good alternative to surgical re-exploration. Problem with this method is it requires expertise, multiple attempts and is time consuming [25].
Conclusion
Chyle leak is a rare but serious complication in head and neck surgery. Timely identification and management are crucial. Conservative management is mainstay but regular monitoring of output and patient response and assessment in terms of immunosuppression, nutritional debilitation and impaired wound healing is essential to identify failure of conservative management at the earliest and initiate surgical ligation to prevent grave complications.
Authors Contribution
Kunal Nandy-Conceptualization, Methodology, Software, Formal Analysis, Writing-original draft, Dipin Jayaprakash-Writing-original draft, Methodology, Shreya Rai-Writing-original draft, Data curation, Validation, Ajay Kumar- Methodology, Software, Formal Analysis, Writing-original draft, Ketul Puj- Methodology, Software, Formal Analysis, Writing-original draft, Umank Tripathi- Writing review and editing and supervision.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration
Conflict of interest
The authors declare that they have no conflict of interest.
Institutional Review Board Approval
Taken.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Delaney SW, Shi H, Shokrani A, Sinha UK (2017) Management of chyle leak after head and neck surgery: review of current treatment strategies. International journal of otolaryngology 2017. [DOI] [PMC free article] [PubMed]
- 2.Langford RJ, Daudia AT, Malins TJ. A morphological study of the thoracic duct at the jugulo-subclavian junction. J Cranio-Maxillofacial Surg. 1999;27(2):100–104. doi: 10.1016/S1010-5182(99)80021-3. [DOI] [PubMed] [Google Scholar]
- 3.Crumley RL, Smith JD. Postoperative chylous fistula prevention and management. Laryngoscope. 1976;86(6):805–813. doi: 10.1288/00005537-197606000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Greenfield J, Gottlieb MI. Variations in the terminal portion of the human thoracic duct. AMA Archives Surg. 1956;73(6):955–959. doi: 10.1001/archsurg.1956.01280060055012. [DOI] [PubMed] [Google Scholar]
- 5.Ammar K, Tubbs RS, Smyth MD, Wellons Iii JC, Blount JP, Salter G, Oakes WJ. Anatomic landmarks for the cervical portion of the thoracic duct. Neurosurgery. 2003;53(6):1385–1388. doi: 10.1227/01.NEU.0000093826.31666.A5. [DOI] [PubMed] [Google Scholar]
- 6.Kwon SS, Falk A, Mitty HA. Thoracic duct injury associated with left internal jugular vein catheterization: anatomic considerations. J Vasc Interv Radiol. 2002;13(3):337–339. doi: 10.1016/S1051-0443(07)61730-8. [DOI] [PubMed] [Google Scholar]
- 7.Hart AK, Greinwald JH, Shaffrey CI, Postma GN. Thoracic duct injury during anterior cervical discectomy: a rare complication: case report. J Neurosurg. 1998;88(1):151–154. doi: 10.3171/jns.1998.88.1.0151. [DOI] [PubMed] [Google Scholar]
- 8.Schünke M, Schulte E, Schumacher U, Ross LM, Lamperti ED (2006) Thieme atlas of anatomy: Neck and internal organs. Thieme.
- 9.Phang K, Bowman M, Phillips A, Windsor J. Review of thoracic duct anatomical variations and clinical implications. Clin Anat. 2014;27(4):637–644. doi: 10.1002/ca.22337. [DOI] [PubMed] [Google Scholar]
- 10.Bach A, Babayan VK. Medium-chain triglycerides: an update. Am J Clin Nutr. 1982;36(5):950–962. doi: 10.1093/ajcn/36.5.950. [DOI] [PubMed] [Google Scholar]
- 11.Swanson MS, Hudson RL, Bhandari N, Sinha UK, Maceri DR, Kokot N. Use of octreotide for the management of chyle fistula following neck dissection. JAMA Otolaryngol-Head Neck Surg. 2015;141(8):723–727. doi: 10.1001/jamaoto.2015.1176. [DOI] [PubMed] [Google Scholar]
- 12.Ahn D, Sohn JH, Jeong JY. Chyle fistula after neck dissection: an 8-year, single-center, prospective study of incidence, clinical features, and treatment. Ann Surg Oncol. 2015;22(3):1000–1006. doi: 10.1245/s10434-015-4822-7. [DOI] [PubMed] [Google Scholar]
- 13.George Broughton II, Janis JE, Attinger CE. The basic science of wound healing. Plast Reconstr Surg. 2006;117(7S):12S–34S. doi: 10.1097/01.prs.0000225430.42531.c2. [DOI] [PubMed] [Google Scholar]
- 14.Ilczyszyn A, Ridha H, Durrani AJ. Management of chyle leak post neck dissection: a case report and literature review. J Plast Reconstr Aesthet Surg. 2011;64(9):e223–e230. doi: 10.1016/j.bjps.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 15.Fitz-Hugh GS, Cowgill R. Chylous fistula: complication of neck dissection. Arch Otolaryngol. 1970;91(6):543–547. doi: 10.1001/archotol.1970.00770040773010. [DOI] [PubMed] [Google Scholar]
- 16.de Gier HH, Balm AJ, Bruning PF, Gregor RT, Hilgers FJ. Systematic approach to the treatment of chylous leakage after neck dissection. Head Neck: J Sci Specialties Head Neck. 1996;18(4):347–351. doi: 10.1002/(SICI)1097-0347(199607/08)18:4<347::AID-HED6>3.0.CO;2-Y. [DOI] [PubMed] [Google Scholar]
- 17.Campisi CC, Boccardo F, Piazza C, Campisi C. Evolution of chylous fistula management after neck dissection. Curr Opin Otolaryngol Head Neck Surg. 2013;21(2):150–156. doi: 10.1097/MOO.0b013e32835e9d97. [DOI] [PubMed] [Google Scholar]
- 18.Jain A, Singh SN, Singhal P, Sharma MP, Grover M. A prospective study on the role of octreotide in management of chyle fistula neck. Laryngoscope. 2015;125(7):1624–1627. doi: 10.1002/lary.25171. [DOI] [PubMed] [Google Scholar]
- 19.Roh JL, Yoon YH, Park CI. Chyle leakage in patients undergoing thyroidectomy plus central neck dissection for differentiated papillary thyroid carcinoma. Ann Surg Oncol. 2008;15(9):2576–2580. doi: 10.1245/s10434-008-0017-9. [DOI] [PubMed] [Google Scholar]
- 20.Kirse DJ, Suen JY, Stern SJ. Phrenic nerve paralysis after doxycycline sclerotherapy for chylous fistula. Otolaryngol-Head Neck Surg. 1997;116(6):680–683. doi: 10.1016/S0194-5998(97)70249-3. [DOI] [PubMed] [Google Scholar]
- 21.Muthusami JC, Raj JP, Gladwin D, Gaikwad P, Sylvester S. Persistent chyle leak following radical neck dissection: a solution that can be the solution. Ann R Coll Surg Engl. 2005;87(5):379. doi: 10.1308/1478708051766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gregor RT. Management of chyle fistulization in association with neck dissection. Otolaryngol-Head Neck Surg. 2000;122(3):434–439. doi: 10.1067/mhn.2000.95229. [DOI] [PubMed] [Google Scholar]
- 23.Anestis N, Christos FC, Ioannis P, Christos I, Lampros P, Stephanos P. Thoracic duct injury due to left subclavicular vein catheterization: a new conservative approach to a chyle fistula using biological glue. Int J Surg Case Rep. 2012;3(7):330–332. doi: 10.1016/j.ijscr.2012.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Polistena A, Monacelli M, Lucchini R, Triola R, Conti C, Avenia S, Barillaro I, Sanguinetti A, Avenia N. Surgical morbidity of cervical lymphadenectomy for thyroid cancer: a retrospective cohort study over 25 years. Int J Surg. 2015;21:128–134. doi: 10.1016/j.ijsu.2015.07.698. [DOI] [PubMed] [Google Scholar]
- 25.Cope C. Diagnosis and treatment of postoperative chyle leakage via percutaneous transabdominal catheterization of the cisterna chyli: a preliminary study. J Vasc Interv Radiol. 1998;9(5):727–734. doi: 10.1016/S1051-0443(98)70382-3. [DOI] [PubMed] [Google Scholar]


