Abstract
Benign schwannoma is a slow growing encapsulated tumor arising from the sheath of Schwann, The majority had extra-cranial localization. We report in this review three cases of a rare extra cranial localization of benign schwannoma in the trachea, frontal sinus and intraparotid facial nerve. The first case diagnosed in a 10-years-old boy, presented with a painless, slow growing mass evolving for three years in the left parotidic region, total conservative parotidectomy was done. The second case concerned a 38-years-old, was admitted to the emergency department with acute inspiratory dyspnea, endoscopic exploration revealed a polylobed tracheal tumor, complete tumor excision was done endoscopically. The third case was about a 33 years old patient, presented a gradually enlarging frontal swelling associated with headache and left nasal obstruction, the endoscopic examination revealed a gray pinkish, smooth and firm soft tissue mass occupying the entire left nasal cavity, CT scan and MRI were requested to assess the characteristics and extent of the tumor, The surgical intervention combined two approaches: trans facial through a mid-frontal incision, and endonasal one. Histopathological examination confirmed the diagnosis of benign schwannoma in all these cases.
Keywords: Benign schwannoma, Intraparotid facial nerve, Frontal sinus, Trachea
Introduction
Benign schwannoma is a slow growing encapsulated tumor arising from the sheath of Schwann.
About 25–45% of all the extracranial schwannomas have been reported in the head and neck region [1]. Three cases of rare extra cranial schwannomas presented in the Department of ENT, Mohamed VI university hospital during the period 2010–2021. These presented in the trachea, frontal sinus and intraparotid facial nerve and are being reported and discussed.
Case 1
A 10-year-old boy with no medical hystory, presented with a slow growing, painless mass of three years evolution in the left parotidic region. Physical examination revealed a well-defined, approximately 3 cm/2 cm sized, smooth, mobile mass (Fig. 1). Facial and other cranial nerve examinations revealed no abnormalities. CT scan showed a well-defined mass of the left parotid, lobulated, homogenous, with mild enhancement in the center and multiple small lymph nodes (Fig. 2). The results of the routine blood investigations were normal.
Fig. 1.

Photograph showing a mass of the left parotid
Fig. 2.
Axial and coronal CT scan: Homogenous and well defined mass of the left parotid gland and measuring 44.6 mm × 59.3 mm
Total conservative parotidectomy was done. Intraoperatively, the mass was well encapsulated and involved the superficial lobe of the parotid. The trunk and main branches of the facial nerve were preserved. The mass was dissected and removed without difficulty (Fig. 3). Histopathological examination confirmed the diagnosis of a benign schwannoma. Microscopically, the tumor consisted of palisading spindle cells with immunohistochemical expression of the S-100 (Fig. 4). Facial nerve functions were normal after the operation, and no recurrence was encountered within a 3 years follow-up.
Fig. 3.
Photograph showing the resected tumor
Fig. 4.

Tumor exhibiting cellular and hypocellular areas. The cellular area shows nuclear palisading around the fibrillar cellular processes and myxoid hypocellular area
Case 2
A 38-year-old patient, followed for 2 years for asthma, put on bronchodilators and inhaled corticosteroids. The patient was admitted to the emergency department with acute high inspiratory dyspnea. Endoscopic exploration revealed polylobed tracheal tumor.
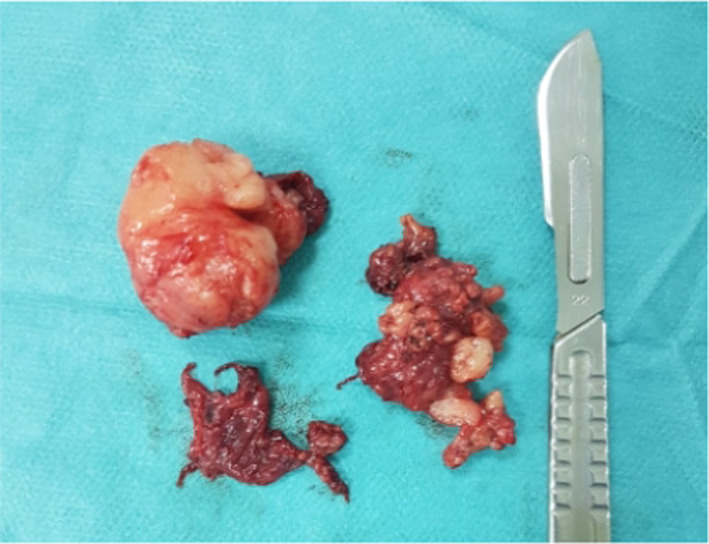
Magnetic resonance imaging revealed a roughly oval and polylobed intratracheal process measuring 18/32/19 mm, which does not enhance after injection of contrast product (Fig. 5). Under cover of a primary tracheostomy, complete tumor excision was done endoscopically (Fig. 6). Histopathological examination confirmed the diagnosis of a benign schwannoma. No adjuvant treatment has been recommended for complete resection. The surveillance did not note a recurrence after 5 years of surveillance.
Fig. 5.
Axial and sagittal MRI scan showing a roughly oval, polylobed tracheal process
Fig. 6.

Photograph showing the resected tumor
Case 3
A 33 years old patient, without no prior pathological history, presented for 18 months a gradually enlarging frontal swelling associated for the last 9 of those 18 months with headache and left nasal obstruction, without any sign fever or general state alteration. Endoscopic examination revealed a gray pinkish, smooth, firm, and soft tissue mass occupying the entire left nasal cavity arriving at the edge of the inferior turbinate and bulging into the nasopharynx (Fig. 7), the contralateral nasal cavity appeared normal. The rest of the physical examination shows a frontal, firm, slightly painful, non-mobile, and well-defined swelling without any endobuccal expression or cervical adenopathy. The ophthalmologic and neurologic examinations were unremarkable.
Fig. 7.

Endoscopic view of the tumor
CT scan and MRI showed an isodensed, T2 isointense, T1 hypointense, with heterogeneous enhanced postcontrast mass of both frontal sinuses, the left anterior ethmoidal sinus and the left nasal cavity, extended anteriorly to the frontal soft tissue and posteriorly to the endocranial (Fig. 8). This process caused bone destruction of the frontal sinus’s anterior and posterior wall, anterior cranial fossa and the interior wall of the left orbit.
Fig. 8.
Coronal T2 MRI showing orbital and endocranium extension of the tumor (A), sagittal T1 MRI showcasing endocranium extension (B), axial gadolinium-enhances T1 weighted MRI showing endocranium extension (C)
The histologic and immunohistochemical studies of an endoscopic biopsy revealed a tumoral proliferation of spindle cell with regular elongated nuclei, without any nuclear atypia with intense PS-100 expression abling the schwannoma diagnosis figure.
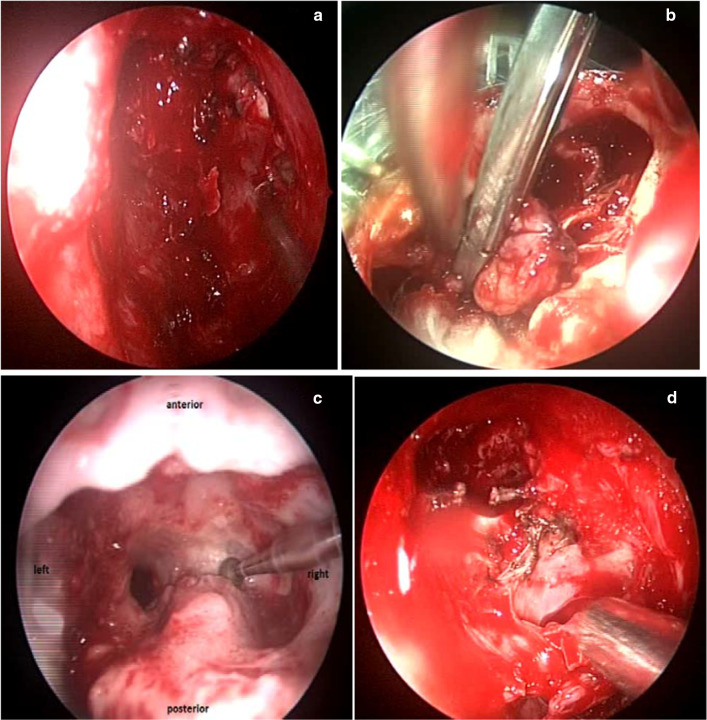
The chirurgical intervention combined two approaches, external one; trans facial; through a mid-frontal incision, and endonasal one. The complete resection of the mass, that extends to the endocranial extradural level and left orbit, was performed with an endonasal frontal sinus drainage defining a Draf III. Reconstruction of the skull base was carried out by septal cartilage, abdominal fat, biological glue and Surgicel (Fig. 9). The anatomopathological study of the mass confirmed the diagnosis.
Fig. 9.
perioperative view of endoscopic resection of tumor(A), perioperative view of tumor resection by external approach(B), frontal endoscopic view of Draf III procedure(C), perioperative view of the reconstruction of skull base (D)
Postoperatively, the patient did present a diplopia without any signs of meningitis or cerebrospinal fluid rhinorrhoea.
Discussion
Schwannoma is a slow growing encapsulated tumor arising from the sheath of Schwann.These neoplasms can develop at any age, but peak in incidence between the 3rd and 6th decades and there is no gender and race predilection [2].
Intraparotid facial nerve schwannomas, are very rare in childhood [3, 4].The clinical manifestations of intra parotid facial nerve schwannomas are not specific and radiological diagnosis is difficult. Marchioni et al. concluded that there are no definitive radiological features for intra-parotid facial nerve schwannoma [5].
intra-parotid facial nerve schwannomas are classified on 4 types according to its position on the facial nerve. Type A: tumors can be removed without sacrificing the facial nerve. Type B: tumors can be resected with partial sacrifice of the peripheral branches of facial nerve or their distal divisions.Type C:tumors require sacrificing the main trunk of the facial nerve for their resection, while type D tumors require sacrificing the trunk and its main divisions to be resected [5]. The prognosis of schwannomas is excellent if surgical excision was complete.
Tracheal schwannomas are extremely rare. They represent less than 0.2% of tracheobronchial tumors [6]. They occur in adults around the age of 50, with a female predominance [7]. In most cases, diagnosis may be delayed because of the insidious and non-specific symptoms [8]. Clinical manifestations depend on the site, the size and the degree of obstruction of the tumor. An asthmatic symptomatology is classically described, which can go as far as respiratory distress [9]. CT scan and bronchoscopy are usually used to confirm the diagnosis and to evaluate the tumor extension [10]. Bronchoscope is important in the diagnosis of primary tracheal tumors, it can facilitate the location of tumor and give instructive information for both intubation and surgery.
Treatment of primary tracheal schwannoma now includes surgery and bronchoscopic resection. However, it is concerned that bronchoscopic resection was associated with high rate of residual tumor, a rate of 46.2% was reported [11].
Frontal sinus schwannoma is uncommon. This disease affects subjects from age range of 14 to 81 years with an average age of 40 years old [12]. The clinical/radiological aspects of this disease are not specific and may mimic different differential diagnoses such as esthesioneuroblastoma or olfactory meningioma [13].
The main reported signs are nasal obstruction, headache, olfactory disorder such as hyposmia and anosmia. [14]. On CT scan the typical appearance of these tumors is marked by calcifications or bone destruction, [12] while on MRI they were often appreared in iso or hypo signal T1 and hypersignal T2 with heterogeneous enhancement after the injection of gadolinium [15].
The anatomopathological and immunohistochemical studies allow the diagnoses; revealing a proliferation of spindle-shaped cells, with small nuclei gathered in a cell population either in order called Antoni A or sometimes in disorder called Antoni B, with a positive immunostaining for the S-100 protein [16].
The treatment is based on the complete surgical resection; the partial one is performed when the tumor adheres to noble neurovascular structures. The external bicoronal approach was once the most used procedure for the resection of tumors invading the anterior level of the skull base. Nowadays, the use of the endoscopic approach combined with less invasive external route is more frequent [17]
Conclusion
Schwannomas of the head and neck are uncommon tumours that arise from any peripheral, cranial or autonomic nerve. They usually present insidiously and thus are often diagnosed incorrectly or after lengthy delays. Surgical excision is the treatment of choice.
Declarations
Conflicts of interest
The authors declare that they have no conflicts of interest in relationship with this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Salemis NS, Karameris A, Gourgiotis S, et al. Large intraparotid facial nerve schwannoma: case report and review of the literature. Int J Oral Maxillofac Surg. 2008;37:679–681. doi: 10.1016/j.ijom.2008.01.018. [DOI] [PubMed] [Google Scholar]
- 2.Shah HK, Kantharia C, Shenoy AS. Intraparotid facial nerve schwannoma. J Postgrad Med. 1997;43:14. [PubMed] [Google Scholar]
- 3.Saravakos P, Papapetropoulos N, Genopoulou SV, et al. Intraparotid facial nerve schwannoma in a 12-year-old child report of a case and review of the literature. Int J Pediatric Otorhinolaryngol Extra. 2015;10:45–48. doi: 10.1016/j.pedex.2015.03.004. [DOI] [Google Scholar]
- 4.Khilnani AK, Thaddanee R, Parmar B, et al. Intraparotid schwannoma: A rare case report. Int J App BasicMed Res. 2015;5:154–6. doi: 10.4103/2229-516X.157176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marchioni D, AlicandriCiufelli M, Presutti L. Intraparotid facial nerve schwannoma: literature review and classification proposal. J LaryngolOtol. 2007;121:707–712. doi: 10.1017/S0022215107006937. [DOI] [PubMed] [Google Scholar]
- 6.Macchiarini P. Primary tracheal tumours. Lancet Oncol. 2006;7:83–91. doi: 10.1016/S1470-2045(05)70541-6. [DOI] [PubMed] [Google Scholar]
- 7.Ge X, Han F, Guan W, et al. Optimal treatment for primary benign Intratracheal Schwannoma: a case report and review of the literature. Oncol Lett. 2015;10:2273–2276. doi: 10.3892/ol.2015.3521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chávez-Fernández DA, Zúñiga-Garza E, López-Saucedo RA. Primary tracheal schwannoma resected in a Turner syndrome patient: a case report. J Surg Case Rep. 2020;2020(10):rjaa430. doi: 10.1093/jscr/rjaa430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Munira A, Kinshuck AJ, Rouhani M, Sandison A, Sandhu GS. The surgical management of recurrent tracheal schwannoma. AME Case Rep. 2018;2:16. doi: 10.21037/acr.2018.04.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen H, Zhang K, Bai M, Li H, Zhang J, Gu L, et al. Recurrent transmural tracheal schwannoma resected by videoassisted thoracoscopic window resection: a case report. Medicine. 2019;98:e18180. doi: 10.1097/MD.0000000000018180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kasahara K, Fukuoka K, Konishi M, et al. Two cases of endobronchial neurilemmoma and review of the literature in Japan. Intern Med. 2003;42:1215–1218. doi: 10.2169/internalmedicine.42.1215. [DOI] [PubMed] [Google Scholar]
- 12.Hu J, Bao YY, Cheng K, et al. Computed tomography and pathological findings of five nasal neurilemmomas. Head Neck Oncol. 2012;4:26. doi: 10.1186/1758-3284-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sunaryo PL, et al. Schwannomas of the sinonasal tract and anterior skull base: a systematic review of 94 cases. Am J Rhinol Allergy. 2014;28(1):39–49. doi: 10.2500/ajra.2014.28.3978. [DOI] [PubMed] [Google Scholar]
- 14.Jawad J, Mandura R, Alhatem H. Neurilemmoma of fronto-ethmoid paranasal sinuses: aggressive anterior skull base destructing tumor—a case report. J Surg Case Rep. 2020;2020(12):rjaa469. doi: 10.1093/jscr/rjaa469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wanamaker JR, Wanamaker HH, Kotton B. Schwannomas of the nose and paranasal sinuses. Am J Rhinol. 1993;7:59–65. doi: 10.2500/105065893781976465. [DOI] [Google Scholar]
- 16.Gencarelli J, et al. Atypical presentation of sinonasal cellular schwannoma: a nonsolitary mass with osseous, orbital, and intracranial invasion. J Neurol Surg Rep. 2014;75(1):e144–e148. doi: 10.1055/s-0034-1376424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blake DM, et al. Endoscopic endonasal resection of sinonasal and anterior skull base schwannomas. J Clin Neurosci. 2014;21(8):1419–1423. doi: 10.1016/j.jocn.2014.03.007. [DOI] [PubMed] [Google Scholar]