Abstract
Plasma cell dyscrasia is the term used to describe the disorders characterized by neoplastic proliferations of plasma cells with production of immuno globulins. Of all the plasma cell dyscrasias, multiple myeloma is the commonest and clinically important. Multiple myeloma accounts for 1% of all malignancies and 10–20% of all hematologic malignancies. Mostly the patients present with bone pain, pathological fractures, renal insufficiency or infections. Here we present two cases of multiple myeloma with unusual presentations admitted in the otorhinolaryngology department of a tertiary care center. One 50-year old male presented with a mass in the left external auditory canal along with left facial palsy and the other a 45 yr old female, who presented with painful deglutition, multiple mucosal erosion in oral cavity, throat tightness and left side facial pain. Both cases are examined and evaluated and found to have multiple myeloma. They were referred to the Hematology department for further management.
Keywords: Multiple myeloma, Bence jones proteins, Plasma cells, CSOM, Dysphagia, Mband, Lytic bone lesions
Introduction
Plasma cell dyscrasia is the term used to describe the disorders characterized by neoplastic proliferations of plasma cells with production of immuno globulins. Of all the plasma cell dyscrasias, multiple myeloma is the commonest and clinically important. Multiple myeloma accounts for 1% of all malignancies and 10–20% of all hematological malignancies. Mostly the patients present with bone pain, pathological fractures, renal insufficiency or infections [1].
We report two unusual presentation of multiple myeloma, where one presented with Aural mass along with facial palsy and the other with dysphagia and odynophagia. So, it is important to think outside the box when the cause is not obvious, to rule out serious systemic causes.
Case Reports
Case 1
A 58-year-old male patient presented to ENT OPD with complains of left aural mass for 6 months along with discharge from the same ear, swelling in the parotid area for last 3 months and deviation of face to right side for 15 days. The left aural mass was slowly progressive associated with discharge which was mucoid, non foul smelling, not blood tinged and not associated with pain. After that he noticed swelling over parotid area which was not associated with pain. His face deviated to right side for last 15 days.
He was not a known case of pulmonary tuberculosis, hypertension or diabetes mellitus. Patient had undergone coronary bypass surgery 5 years back. History of (h/o) weight loss and anorexia was present. There was no h/o fever or headache or dizziness. There was no history of any tobacco addiction or exposure to radiation.
On examination, a pinkish, soft to firm, non-tender mass was seen occupying the whole left external auditory canal along with discharge. On probing the mass, it was found that the mass was coming from deeper part of external auditory canal with no bleeding on probing. There was a Non-tender firm swelling of size 4 cm × 3 cm × 3 cm over left parotid area not adherent to overlying skin. No neck node was palpable.
There was
Lower Motor Nerve type facial nerve palsy of left side
Nasal examination and tongue movement was normal
Left side Soft palate palsy was present
Gag reflex was diminished
Clinically it was thought to be a case of middle ear malignancy with differential diagnosis of chronic Suppurative Otitis Media (CSOM) with complication. Further evaluation was done by hematological investigations and by imaging studies.
Hematological Findings:
CBC NORMOCYTIC NORMOCHROMIC ANEMIA (Hb-8.2 gm%), NEUTROPHILLIC LEUKOCYTOSIS (82%-15,000/mm3), Total platelet count (TPC)—Within normal limit (WNL)
Serum urea-65 mg/dl (↑), Creatinine 3.1 mg/dl. (↑), RBS-154 mg/dl (↑)
Serum uric acid-12.8 mg/ml (↑)
Low albumin-1.8 gm/dl
Diagnostic laryngeal endoscopy: left vocal cord palsy
Histopathology of aural mass suggested “GRANULATION TISSUE”.
UltraSonoGraphy of ABDOMEN and PELVIS: Bilateral (B/L) medical renal disease Grade 1 and (B/L) mild pleural effusion
CT BRAIN with HRCT Temporal Bone Large expansile isodense lytic lesion involving occipital and left temporal bone with involvement of left middle ear, left external ear encasing left ICA and left IJV with extensions to left side basiocciput, adjacent atlas arch, posterior fossa causing compression of left cerebellar hemisphere & inferiorly extends up to left parotid space and left paraspinal muscles.
Additional multiple lytic lesions noted in calvarium and condyle of mandible.
X ray pelvis showed Multiple punched out lesions
FNAC from parotid swelling: Features Suggestive of Plasmacytoma.
Serum Protein Electrophoresis Gamma Globulin-66.2% (↑) with presence of “Monoclonal M spike”.
Bone marrow study Plasma cells > 66%, hyper cellular, mitoses – present, myeloid: erythroid ratio-4:1, reticulm cells absent, normal leucopoiesis & erythropoiesis.
Thus, a final diagnosis of multiple myeloma was made. Figs. 1, 2, 3, 4.
Fig. 1.

Pinkish firm left aural mass occupying the whole of the EAC
Fig. 2.

Showing multiple punched out lesions in X-Ray skull and pelvis
Fig. 3.
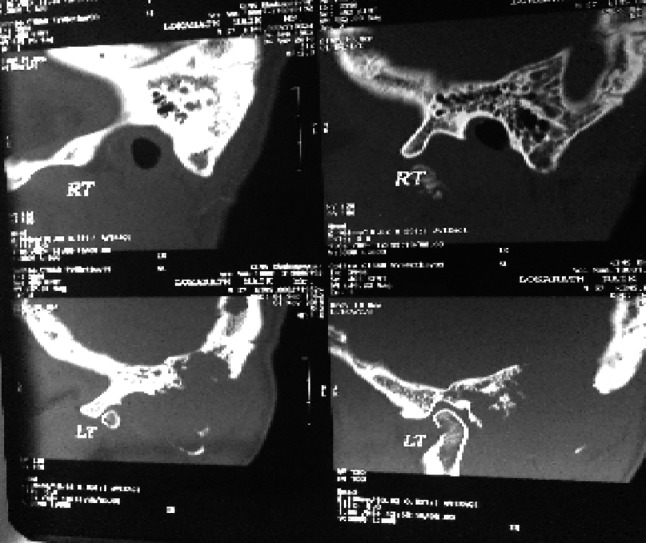
CT scan showing Large expansile isodense lytic lesion involving left temporal bone with involvement of left middle ear and normal right mastoid
Fig. 4.
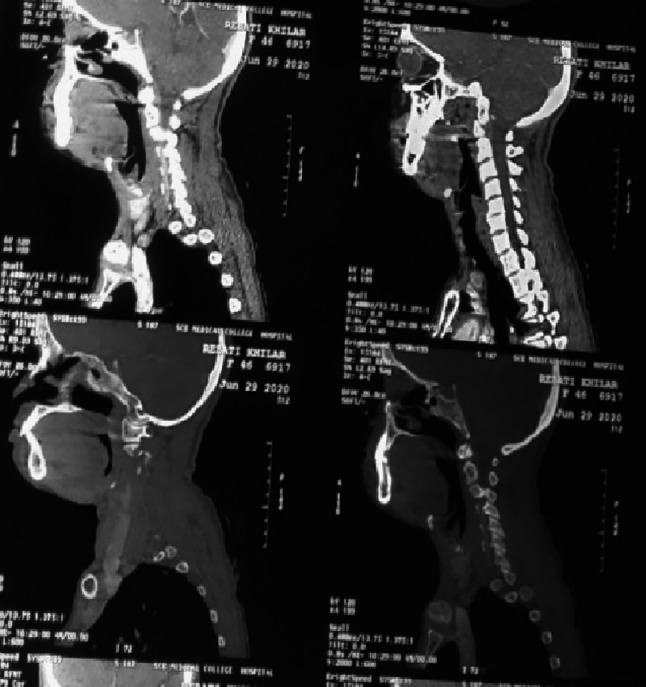
CT Scan showing Multiple well-defined lytic areas in C2, C3 vertebrae body, occipital bone and transverse process of C4, C5
Case 2
A 45-year old female presented to our ENT OPD with chief complains of painful swallowing for last 6 months. She was apparently alright 6 months back. To start with she developed painful swallowing first to liquid then subsequently to solid food. It was associated with throat tightness since then. Also, she developed recurrent aphthous ulcers and left side throat pain intermittently for last 3–4 months. She was not a k/c/o any chronic illness like hypertension/Type 2 Diabetes Mellitus/Pulmonary tuberculosis. There was no history of any tobacco addiction or exposure to radiation. She had history of weight loss and loss of appetite.There was no history of fever, vomiting, cough, ear discharge or hoarseness. She was properly evaluated by clinical, haematological and imaging studies.
On examination—She was found to have multiple mucosal erosion over b/l buccal mucosa.
No cervical lymphadenopathy
Laryngeal crepitus-present
CBC profile shows normocytic normochromic anemia (Hb%-9.2 gm%) with neutrophillic leucocytosis (88%). ESR-50 mm in 1st hr, Serum reticulocyte count − 0.5%, TPC-WNL
C-Reactive Protein was raised
LFT, RFT, TFT, PT, INR, APTT, RA factor (quantitative), Serum CK-MB -WNL
Direct Coombs Test, Indirect Coombs Test-Negative
Urine routine & microscopy examination-Increased pus cells and RBCs
Diagnostic laryngeal endoscopy was normal and Upper GI endoscopy revealed pre-pyloric ulcer. Patient was examined to rule out any systemic disease.
USG ABDOMEN DONE: minimal ascites, left mild hydroureteronephrosis.
ANA profile: negative.
Serum LDH 553 µ/l(250–450).
CECT skull, neck and chest showed bilateral reduced volume of Maxillary and Sphenoid sinus with mucosal thickening and bony hyperostosis. Multiple well-defined lytic areas in C2, C3 vertebral bodies, occipital bone and transverse process of C4, C5, B/L lung Fields- apical patchy fields with mosaic attenuation.
As per CT findings it was provisionally diagnosed as plasma cell disorder like multiple myeloma and was evaluated further.
Urine protein electrophoresis Total proteins-825.60 mg/24 h. (28–141) (Increased globulins concentration 85%).
Serum Protein Electrophoresis Increased gamma globulin with presence of M-Band.
BONE MARROW BIOPSY Presence of Plasma Cells more than 20%, with suppressed erythropoesis and mild depressed leucopoiesis.
Finally, both the patients were diagnosed as Multiple Myeloma.
Discussion
Multiple Myeloma has been recognized since ancient times. The first well-documented case was reported in 1844 by Samuel Solly. The most commonly recognized case is that of Thomas Alexander McBean, a highly respectable tradesman from London in 1850. Mr. McBean excreted a large amount of protein that was described by Henry Bence Jones in the middle of the nineteenth century [2].
The plasma cell disorders are characterized by abnormal proliferation of immunoglobulin-producing cells and result in accumulation of monoclonal immunoglobulin in serum and urine. The group as a whole is known by various synonyms such as plasma cell dyscrasias, paraproteinaemias, dysproteinaemias monoclonal gammopathies Fig. 5.
Fig. 5.
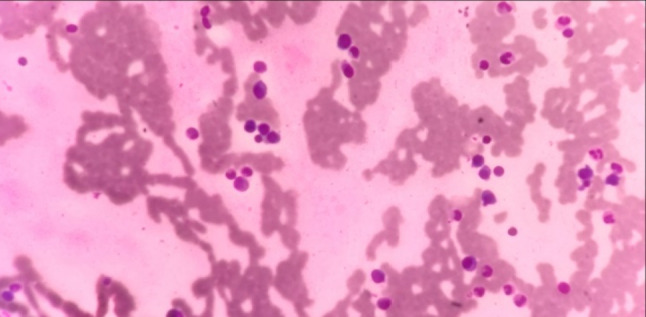
Bone Marrow biopsy Showing Plasma cells
This group consists of six different types, out of which multiple myeloma is one of them.
Multiple myeloma primarily affects the elderly (peak incidence in 5th-6th decades) and increases in incidence with age. It is rare under the age of 40. Myeloma is more common in males than females [3]. One of our female patients is below 50 years.
Mostly the patients present with bone pain, unexplained anemia, pathological fractures, renal insufficiency or infections. The characteristic lytic lesions are due to the increased osteoclastic activity from bone marrow infiltration. Both patients did not present with typical features of Multiple Myeloma. Neoplasms of plasma cells are rare in the head and neck region.
Plasmacytoma is further classified into two groups: osseous and non-osseous (extramedullary) primary lesions. Osseous lesions constitute approximately 70% of all plasmacytomas. They involve primarily marrow-containing bones, with a predilection for the vertebrae, femurs, and pelvis. Of the extramedullary lesions, approximately 80% occur in the head and neck region and frequently involve the upper respiratory tract [4, 5].
At first, they were thought to be a disease with local symptoms only but later systemic involvement was detected. Renal failure occurs in about 25% of patients, while renal pathology occurs in 50% of cases. One of our cases had not developed renal failure.
The differential diagnosis for our cases includes middle ear malignancy, CSOM with complications, recurrent aphthous ulcer, granulomatous disease like tuberculosis, eosinophilic granuloma, autoimmune diseases, as well as multiple myeloma. The median survival is 2 years for Multiple Myeloma after the diagnosis is made.
Conclusion
Our cases had atypical presentations. Only after proper evaluation and investigations, final diagnosis could be made. Patient with multiple myeloma may present to the otolaryngologist with local pathology in head and neck region. But they should be evaluated properly to rule out any systemic cause to reach the final diagnosis. When neurological symptoms similar to those we observed are associated with lesions in cervical vertebral bodies or the petrous bone, multiple myeloma should be considered as the differential diagnosis. Left vocal cord palsy, palatal palsy can be explained due to the lytic lesion involving left temporal bone and occipital bone in skull base. Further clinical, biochemical, and radiological follow-up of such patients is necessary. Both the patients were treated conservatively in our department till final diagnosis of multiple myeloma was made and then referred to Haematology department for further management.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tejinder S. Multiple myeloma and walderstrom macroglobulinemia. Atlas and text of haematology. 3. New Delhi: Avichal Publishing Company; 2010. pp. 353–355. [Google Scholar]
- 2.Robert KA, Moehler T, Goldschmidt H, et al. History of multiple myeloma, multiple myeloma. Berlin: Springer; 2011. pp. 3–23. [Google Scholar]
- 3.Mohan H. Disorders of lymphocytes and lympho reticular tissues textbook of pathology. 6. New Delhi: JP Medical Ltd; 2011. pp. 380–385. [Google Scholar]
- 4.Bolek TW, Marcus RB, Mendenhall NP. Solitary plasmacytoma of bone and soft tissue. Int J Radiat Oncol Biol Phys. 1996;36:329–333. doi: 10.1016/S0360-3016(96)00334-3. [DOI] [PubMed] [Google Scholar]
- 5.Saif MW, Greenberg BR. Dysphagia secondary to a solitary plasmacytoma. Cancer Control J. 1998;5:433–438. doi: 10.1177/107327489800500507. [DOI] [PubMed] [Google Scholar]


