Abstract
To compare radiofrequency and electrocauterization in reducing the degree of postoperative pain in pediatric patients undergoing tonsillectomy. A double-blind, parallel-group, randomized controlled trial. Pediatric patients with indications for tonsillectomy were randomized to receive either tonsillectomy with radiofrequency or electrocautery. Also recorded were intraoperative blood loss, duration of the surgery, length of hospital stays, and complications from the surgery. Forty pediatric patients participated in the study; 20 were randomized to each group. The participants’ ages ranged from 3 to 14 years old, and 65% were male. The overall postoperative pain scale score during the early postoperative period was lower in the radiofrequency group compared to the electrocautery group (mean difference − 1.37 (95%CI − 1.72, − 0.12); p < 0.001). Also, the mean pain scale scores at 6 h, 1, and 2 days were significantly lower in the radiofrequency group. Intraoperative blood loss and length of hospital stay in the radiofrequency group were also significantly lower than in the electrocautery group, whereas the duration of the surgery and complication rate were not different between the two groups. Pediatric tonsillectomy using radiofrequency ablation could reduce the severity of early postoperative pain, intraoperative blood loss, and length of hospital stay compared to tonsillectomy with electrocautery. Therefore, tonsillectomy with radiofrequency may be considered a safe and effective operative option.
Trial registration Thai Clinical Trials Registry (TCTR-20210303007), 03-March-2021.
Keywords: Pediatrics, Tonsillectomy, Radiofrequency, Electrocautery
Introduction
Tonsillectomy is a common operation in otolaryngology, especially in pediatric patients. Its indication includes a history of recurrent throat infection and obstructive sleep apnea (OSA) diagnosed by polysomnography (PSG) [1]. The operation can be performed using various methods, such as standard surgery, in which the tonsils are removed from the tonsillar capsule (cold dissection), and other more advanced techniques, such as electrocautery, laser dissection, radiofrequency ablation, harmonic scalpel, and coblation [2].
Electrocautery is one of the popular surgical procedures because it could shorten the operative time and reduce intraoperative blood loss [3, 4]. However, this technique requires a large amount of heat to be released under the temperature between 400 °C and 600 °C, which may result in excessive postoperative pain and prolonged recovery time [3].
On the other hand, tonsillectomy using radiofrequency radiation involves radiofrequency energy in the range between 0.01 and 300 MHz, which emits a lower amount of heat than electrocauterization. Also, the temperature is much lower at between 40 °C and 70 °C, thus reducing the risk of injury to nearby tissues and the degree of postoperative pain [5]. Previous studies in adult patients have shown that tonsillectomy performed with the radiofrequency technique could reduce the severity of postoperative pain [6], reduce intraoperative blood loss [7], shorten the operative time, and reduce the recovery time [8] in comparison with other surgical techniques. However, to the best of our knowledge, there has been no randomized controlled trials comparing radiofrequency ablation with electrocauterization in pediatric patients. Consequently, we conducted this randomized controlled trial to compare the efficacy in terms of the degree of postoperative pain between tonsillectomy performed with radiofrequency radiation and electrocauterization in pediatric patients requiring tonsillectomy.
Materials and Methods
Study Design and Setting
This single-center, double-blind, parallel-group, randomized controlled trial was conducted at the Otolaryngology Department, HRH Princess Maha Chakri Sirindhorn Medical Center, Nakorn Nayok, Thailand, from January 1 to December 31, 2020. The hospital is a large tertiary university hospital with over 10,000 otolaryngology outpatient visits, and approximately 800 otolaryngology operations annually. The Human Ethics Committee of Srinakharinwirot University approved the study (SWUEC-129/61F). Informed consent was obtained from all the participants’ legal guardians before their inclusion into the trial. We registered the trial in the Thai Clinical Trials Registry (TCTR-20210303007).
Participants
Included participants were pediatric patients aged 3 to 14 years old with at least one of the following indications for tonsillectomy; (1) a history of at least 7 episodes of throat infection in the past year, or at least 5 episodes per year for 2 years, or at least 3 episodes per year for 3 years, with ≥ 1 of the following symptoms documented in the medical record in each episode: fever > 38.3 °C, cervical adenopathy, exudative tonsil, and positive test for group A beta-hemolytic streptococcus; (2) a history of recurrent throat infection not meeting the above criteria with ≥ 1 of the following history: multiple allergies or intolerance to antibiotics, Periodic Fever Aphthous stomatitis Pharyngitis and Adenitis (PFAPA), > 1 episode of peritonsillar abscess; and (3) OSA diagnosed by PSG [1].
Excluded participants were those with contraindications to surgery or anesthesia, morbid obesity, a preoperative PSG test result of severe OSA, a history of an allergic reaction to pain relievers (acetaminophen and ibuprofen), previous adenotonsillectomy, craniofacial abnormalities, cardiac dysfunction, pulmonary abnormalities, or coagulopathies.
Randomization
After obtaining informed consent, enrolled patients were randomized in a 1:1 ratio to receive tonsillectomy either with radiofrequency or electrocautery. Computer-generated block randomization was performed with a block size of four. The sequence was concealed with sequential-numbered sealed opaque envelopes. The participants were not aware of the allocated assignments except the surgeons.
Study Process
History taking, physical examination, and laboratory testing, including complete blood count, prothrombin time, partial thromboplastin time, international nationalized ratio, and chest radiography, were performed in all participants before the surgery as per the standard procedure of our hospital.
All operations were performed by same otolaryngologists who was skilled in both surgical technique (AT). All the study participants were operated under general anesthesia with endotracheal intubation. Basic surgical procedures were similarly delivered to all participants. They were placed in the Rose position with their mouth opened using a McIvor retractor. Tonsillectomy was performed by conventional extra-capsular dissection method. Different instruments were obtained to amputate the membrane and tissue between the tonsils and the tonsillar bed. In the group that received radiofrequency, To-bite™ bipolar tonsillectomy forceps and CURIS® (Sutter, Tullastraße, Freiburg, Germany) radiofrequency generator were applied. Whereas in the group that received electrocautery, bipolar coagulation forceps and a ValleyLab Force Triad™ (Convidien, Boulder, Colorado, USA) electrosurgical unit were employed. Adenoidectomy was routinely performed in all patients with adenoid curette. All participants in both groups also received a single dose of 0.5 mg/kg intravenous dexamethasone intraoperatively. The operation time were recorded from the first incision to remove McIvor retractor. The intraoperative blood loss was recorded from suction and cotton balls.
After the surgery, all the participants received intravenous maintenance fluid based on their body weight on the first day and oral amoxicillin/clavulanic acid syrup (amoxicillin 40 mg/kg/day) for 7 days. Also, a clear liquid diet was maintained during the first 2 weeks. In case of hypersensitivity to penicillin, 40 mg/kg/day of erythromycin was instead prescribed. For pain control, 15 mg/kg/dose of acetaminophen (maximum 75 mg/kg/day or 4,000 mg/day) was delivered every 4 h in combination with 10 mg/kg/day of ibuprofen every 6 h (maximum 40 mg/kg/day or 1,200 mg/day). If the patient had severe persistent pain, 1 mcg/kg/dose of fentanyl could be given every 1 h (maximum 25 mcg/dose). All the participants also received intravenous dexamethasone 0.5 mg/kg every 8 h for 24 h after the surgery.
Study Objectives
The primary objective was postoperative pain assessed with the Wong-Baker FACES pain rating scale, a reliable and widely-used scale for assessing the severity of pain in children aged at least 3 years old [9]. The secondary outcomes were the operative time, intraoperative blood loss, length of hospital stay and postoperative complications.
Data Collection
We recorded participants’ demographics (sex, age, weight, height, body mass index, comorbidities, and history of drug allergy) and their physical examination results, including the size of the tonsils and adenoids and indications for surgery. During the surgery, we collected the operative time, intraoperative blood loss, and intraoperative complications. After the surgery, a physician, who was blinded to the surgical technique performed and independent of the surgeons, assessed each participant’s pain scale at 6 h, 1, 2, 7, and 14 days. Also recorded were any extra dosages of pain relievers required by the study participants, length of hospital stay, any complications related to the surgery, and the pathology report.
Statistical Analyses
The sample size was calculated according to the formula recommended by Frison and Pocock [10]. Based on the previous studies [11, 12], we estimated that the average pain scale score of the radiofrequency and electrocautery group was 2.0–2.6 (standard deviation (SD) 0.9–1.2) and 3.0–4.0 (SD 1.0–1.5), respectively. Therefore, a sample of twenty participants per group was considered sufficiently large to indicate clinically meaningful differences with 87.10% power and a 5% significance level.
Descriptive statistics were obtained to present participants’ baseline demographics. We compared categorical data using the Chi-squared test or the Fisher’s Exact test as appropriate. While continuous data were compared using the independent t-test.
Pain scale scores at each time-point are presented as mean and SD. For the primary analysis, the overall mean pain scale scores between the two groups at all time-points were compared using generalized estimating equations (GEE) adjusted for the baseline measurements of that group, age, and sex. While the mean difference at each time-point was analyzed using multiple linear regression. Results are reported as mean differences, and 95% confidence interval (95%CI). The Mann–Whitney U test was employed to compare intraoperative blood loss, the operative time, and length of hospital stay. A p-value of less than 0.05 was considered statistically significant. All statistical analyses and the sample size calculation were performed using STATA version 14.0 (College Station, TX).
Results
Characteristics of Participants
During January 1 and December 31, 2020, a total of 44 eligible patients underwent tonsillectomy. Three patients were excluded due to concomitant severe OSA, and one patient declined to participate. Consequently, 40 patients were enrolled in the study. Twenty participants were assigned to receive tonsillectomy with radiofrequency, and another twenty were randomized to receive tonsillectomy with electrocautery (Fig. 1). All randomized patients were analyzed, and there were no missing data in the study.
Fig. 1.
Participant flowchart
The participants' age ranged from 3 to 14 years old. There were 26 males and 14 females. Both groups had similar characteristics regarding sex, age, body mass index, and tonsil and adenoids sizes (Table 1).
Table 1.
Demographic data
| Radiofrequency n = 20 | Electrocautery n = 20 | p-value | |
|---|---|---|---|
| Age (year) | 7.30 ± 2.43 | 5.95 ± 2.14 | 0.070a |
| Sex | 0.741b | ||
| Male | 12 | 14 | |
| Female | 8 | 6 | |
| BMI (kg/m2) | 19.07 ± 4.39 | 19.22 ± 3.78 | 0.914a |
| Tonsil grade | 0.699c | ||
| Grade 1 | 0 | 1 | |
| Grade 2 | 8 | 5 | |
| Grade 3 | 8 | 9 | |
| Grade 4 | 4 | 5 | |
| Adenoid size (%) | 60.00 ± 19.19 | 69.50 ± 10.50 | 0.060a |
| Indication for surgery | 0.917b | ||
| Recurrent tonsillitis | 12 | 10 | |
| Obstructive sleep apnea | 8 | 10 |
Data presented as count or mean (standard deviation)
aIndependent t-test
bChi-square test
cFisher's exact test
Postoperative Pain
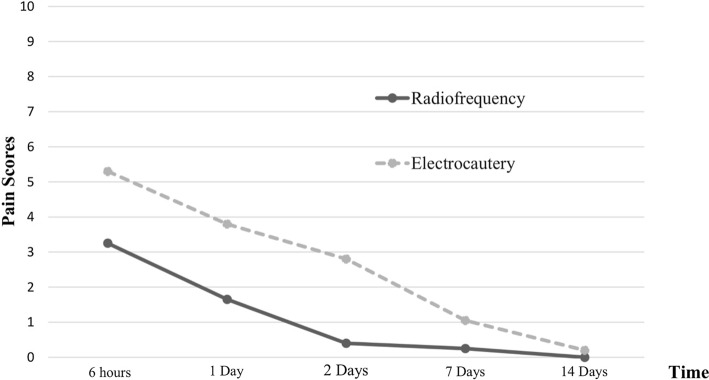
Patients in the radiofrequency group had an overall lower level of early postoperative pain compared to those in the electrocautery group (mean difference − 1.37 points), which is statistically significant (95%CI − 1.72, − 0.12, p < 0.001). The mean ± SD pain scale scores of the radiofrequency group at 6 h, 1 day, and 2 days postoperative were 3.25 ± 0.97, 1.65 ± 0.93, and 0.40 ± 0.60, respectively. While the pain scale scores of the electrocautery group were higher at 5.30 ± 1.30, 3.80 ± 0.83, and 2.80 ± 0.70 points at 6 h, 1 day, and 2 days, respectively. The differences were statistically significant in favor of the radiofrequency group at all time-points (mean difference at 6 h post-operation − 2.16 (95%CI − 2.92, − 1.39), p < 0.001; mean difference at 1 day post-operation − 0.91 (95%CI − 1.37, − 0.45), p < 0.001; mean difference at 2 days post-operation − 1.84 (95%CI − 2.36, − 1.31), p < 0.001).
At 7 and 14 days in outpatient visit, postoperative pain were not different between the groups. Results on the pain scale scores are presented in Table 2 and Fig. 2. Only a small number of participants required an additional dosage of pain relievers other than the standard acetaminophen and ibuprofen regimen in the protocol. One patient in the radiofrequency group and two patients in the electrosurgical group had fentanyl prescribed.
Table 2.
Postoperative pain scale scores
| Pain scale scores | Radiofrequency | Electrocautery | Mean difference | 95% CI | p-value |
|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | ||||
| 6 h | 3.25 ± 0.97 | 5.30 ± 1.30 | − 2.16 | − 2.92, − 1.39 | < 0.001a |
| 1 day | 1.65 ± 0.93 | 3.80 ± 0.83 | − 0.91 | − 1.37, − 0.45 | < 0.001a |
| 2 days | 0.40 ± 0.60 | 2.80 ± 0.70 | − 1.84 | − 2.36, − 1.31 | < 0.001a |
| Overall early post-operative period | N/A | N/A | − 1.37 | − 1.72, − 0.12 | < 0.001b |
| 7 days | 0.25 ± 0.55 | 1.05 ± 1.05 | − 0.26 | − 1.01, 0.48 | 0.475a |
| 14 days | 0 | 0.20 ± 0.62 | − 0.34 | − 0.74, 0.06 | 0.094a |
SD Standard deviation, CI Confidence Interval
aAnalyzed with multiple linear regression
bAnalyzed with generalized estimating equations
Fig. 2.
Postoperative pain scores
Intraoperative Time, Intraoperative Blood Loss, and Hospital Length of Stay
The mean ± SD volume of intraoperative blood loss was 28.75 ± 16.37 ml in the radiofrequency group and 46.00 ± 24.20 ml in the electrocautery group. The radiofrequrncy group had significantly lower degree of intraoperative blood loss than the electrocautery group (p = 0.010) (Table 3). Nonetheless, the radiofrequency group were operated for approximately 54.4 ± 18.61 min, similar to the electrocautery group, who were under the operation for approximately 60.45 ± 15.18 min (p = 0.057). However, the participants who underwent radiofrequency had a significantly shorter length of stay in the hospital than those underwent electrocautery (hospital length of stay 4.25 ± 2.88 days versus 5.05 ± 3.17 days, respectively, p = 0.024) (Table 3).
Table 3.
Intraoperative blood loss, operative time and length of stay
| Mean ± SD | Median | Median difference | 95% CI | p-valuea | |
|---|---|---|---|---|---|
| Blood loss (ml) | |||||
| Radiofrequency | 28.75 ± 16.37 | 25 | 20.00 | 5.00, 30.00 | 0.010 |
| Electrocautery | 46.00 ± 24.20 | 45 | |||
| Operative time (min) | |||||
| Radiofrequency | 54.40 ± 18.61 | 50 | 10.00 | 0.00, 15.00 | 0.057 |
| Electrocautery | 60.45 ± 15.18 | 60 | |||
| Length of stay (days) | |||||
| Radiofrequency | 4.25 ± 2.88 | 3 | 1.00 | 0.00, 2.00 | 0.024 |
| Electrocautery | 5.05 ± 3.17 | 5 |
SD Standard deviation, CI confidence Interval
aAnalyzed with the Mann–Whitney U test
Bleeding After Surgery and Other Postoperative Complications
There was no postoperative bleeding or complications associated with both the surgical interventions in all of the participants.
Pathology Results
All the participants' pathology results reported chronic hypertrophic tonsillitis.
Disscussion
This single-center, double-blind, parallel-group, randomized controlled trial found that tonsillectomy performed under radiofrequency could result in a lower degree of early post-operative pain than tonsillectomy using electrocauterization in pediatric patients. Moreover, the novel surgical technique could decrease intraoperative blood loss and shorten hospital length of stay compared to the surgery using electrocautery with a similar negligible complication rate.
Tonsillectomy has long been one of the most common otolaryngology surgical procedures in pediatric patients. It is indicated in patients with recurrent tonsillitis or chronic tonsillar hypertrophy with OSA. Because these conditions result in enlarged tonsils obstructing the upper airway, removing the tonsils is thereby required.
There is currently a wide range of surgical instruments and techniques developed to improve the effectiveness of the treatment and reduce the complications secondary to former surgical procedures. One of the innovative techniques is radiofrequency, which emits less heat and lower energy than electrocauterization, thus reducing the risk of injury to nearby tissues [11, 13]. It also helps to reduce pain and bleeding after the surgery [11, 13]. Several studies have compared tonsillectomy using different instruments and techniques, but those studies have been primarily conducted in adults [6], with only a few studies in children. Consequently, the authors conducted this randomized controlled trial to compare the efficacy in terms of postoperative pain between pediatric patients receiving tonsillectomy performed using radiofrequency and those who underwent tonsillectomy with electrocauterization.
The present study demonstrated that the participants in the radiofrequency group had significantly lower severity of postoperative pain than the electrocautery group during the early postoperative period. The pain scale scores of the radiofrequency group were also significantly lower than that of the electrocautery group at all early postoperative time-points assessed, which are 6 h, 1 day, and 2 days. However, the pain levels between the two groups measured at 7 and 14 days postoperatively were not significantly different, although the mean pain scale scores were lower in the radiofrequency group at both the time-points. This is in line with the results of the other two non-randomized studies conducted by Hall et al. [11]. and Morinière et al. [14]. Both studies compared the level of postoperative pain between pediatric patients receiving tonsillectomy with radiofrequency and tonsillectomy with electrocautery. They both found that patients who received radiofrequency experienced less severe postoperative pain than those who received the other intervention. Moreover, the results of the present study are consistent with a meta-analysis by Lee et al. [6] that pooled 11 randomized controlled trials conducted in adult patients and found that radiofrequency resulted in a lower degree of postoperative pain than electrocautery. The meta-analysis reported significant differences during the early postoperative period within 2 days post-operation and non-statistically significant differences on day 7 and day 14, consistent with the results of the present study. Similarly, a previous study by Kumar et al. [15] reported a lower degree of pain in pediatric patients after tonsillectomy with radiofrequency compared to that with the traditional surgical technique.
Furthermore, the present study found that radiofrequency could lead to a lower degree of intraoperative blood loss compared with electrocautery. This result is discordant with the findings of Hall et al. [11], who conducted a non-randomized study comparing the two types of surgery in pediatric patients and reported an undifferent amount of intraoperative blood loss between the two surgical methods. However, the results of the present study were concordant with a pediatric study by Ragab et al. [16] and an adult study by Nemati et al. [7] Both studies found that radiofrequency could significantly reduce blood loss compared to the standard surgical procedures.
In the present study, the operative time of the two surgical procedures was not significantly different. This is consistent with a non-randomized study by Morinière et al. [14], who compared the two surgical techniques in pediatric patients and found no between-group difference regarding the intraoperative time. However, in Ragab et al.’s study involving adult patients [8], it was evident that the use of radiofrequency was less time-consuming than electrocautery. Nonetheless, it is important to note that the operative time of the radiofrequency group in the present study was similar to the duration reported in Ragab et al.’s study.
Nevertheless, the length of hospital stay in the radiofrequency group was significantly shorter than in the electrocautery group. In the present study, the participants were under consideration for discharge once they had retained their eating ability and had fully recovered from all other disabling symptoms. Furthermore, short hospital stays diminished the hospital cost in our setting. In terms of the patients’ recovery time in the radiofrequency group, our study result is similar to the finding of Businco et al. [12], who found that the recovery time was significantly lower in the radiofrequency group than in the traditional surgery group. Also, the results of Ragab et al.’s study [8], reported a shortened incubation time with regards to wound healing following radiofrequency surgery. Additionally, Aksoy et al. [17] demonstrated that wound healing was significantly better after radiofrequency compared with electrocautery.
During the overall duration of the present study, no patients experienced postoperative bleeding. The safety profile of radiofrequency has been previously proposed by Morinière et al. [14] and Hegazy et al. [18], both of whom stated that the implementation of radiofrequency in pediatric tonsillectomy is safe. However, a study by Sunnergren et al. [19] involving 1602 pediatric patients in Sweden found a small incidence of post-tonsillectomy bleeding (1.2%) under radiofrequency. Nonetheless, this incidence rate is considered small compared to the average overall incidence of bleeding after tonsillectomy of any methods, which was approximately 3.3% [20].
The present study has some limitations. First, the primary outcome was the degree of pain, which is a subjective outcome that could have suffered from possible unreliable and inaccurate results due to the complexity in the measurement and evaluation. In particular, the accurate level of pain in pediatric patients is challenging to assess and achieve. Further studies should emphasize on evaluating individual results for pediatric patients of different age ranges using an appropriate measurement tool according to each age range. This may help differentiate levels of pain more accurately. Moreover, this study was a single-center study, which may limit the generalizability of its findings because patients or conditions unique to a particular institution may reduce the relevance when extrapolated to other sites. Further multi-center trials are required to evaluate the effects of the interventions in other populations.
In conclusion, pediatric tonsillectomy using radiofrequency ablation could reduce the severity of early postoperative pain compared to tonsillectomy with electrocauterization. Also, it could reduce intraoperative blood loss and length of hospital stay without complication. Therefore, it may be considered a safe and effective surgical option for pediatric patients who required tonsillectomy.
Acknowledgements
The authors would like to acknowledge the assistance of Kitasarawut Khancharee, Ph.D., who provided statistical analyses plan, conducted the analyses and supervised their interpretation. We would also like to acknowledge all the physicians, nurses, nursing assistants in the otolaryngology department, and all who have assisted this work. Also, the study is dedicated to the patients who participated.
Abbreviations
- CI
Confidence interval
- GEE
Generalized estimating equations
- MHz
Megahertz
- OSA
Obstructive sleep apnea
- PFAPA
Periodic fever aphthous stomatitis pharyngitis and adenitis
- PSG
Polysomnography
- SD
Standard deviation
- USA
United States of America
Authors' Contributions
AT was also responsible for the study design, data collection, analyses and drafted the manuscript. PW conceived the main research idea, developed the study design, collected the data, drafted the manuscript, and edited the manuscript in consultation with AT. All authors read and approved the final manuscript.
Funding
This study was supported by a research grant from HRH Princess Maha Chakri Sirindhorn Medical Center, Faculty of Medicine, Srinakharinwirot University (Grant No.153/2563).
Availability of Data and Materials
The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethics Approval
The Human Ethics Committee of Srinakharinwirot University approved the study (SWUEC-129/61F).
Informed Consent
Informed consent was obtained from all the participants’ legal guardians before their inclusion into the trial.
Consent for Publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Mitchell RB, Archer SM, Ishman SL, Rosenfeld RM, Coles S, Finestone SA, et al. Clinical practice gvuideline: tonsillectomy in children. Otolaryngol Head Neck Surg. 2019;160(1_suppl):S1–S42. doi: 10.1177/0194599818801757. [DOI] [PubMed] [Google Scholar]
- 2.Spektor Z, Kay DJ, Mandell DL. Prospective comparative study of pulsed-electron avalanche knife (PEAK) and bipolar radiofrequency ablation (coblation) pediatric tonsillectomy and adenoidectomy. Am J Otolaryngol. 2016;37(6):528–533. doi: 10.1016/j.amjoto.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Roje Z, Racic G, Kardum G, Selimovic M. Is the systemic inflammatory reaction to surgery responsible for post-operative pain after tonsillectomy, and is it "technique-related"? Wien Klin Wochenschr. 2011;123(15):479–484. doi: 10.1007/s00508-011-0020-1. [DOI] [PubMed] [Google Scholar]
- 4.Tay HL. Post-operative morbidity in electrodissection tonsillectomy. J Laryngol Otol. 1995;109(3):209–211. doi: 10.1017/s0022215100129718. [DOI] [PubMed] [Google Scholar]
- 5.Littlefield PD, Hall DJ, Holtel MR. Radiofrequency excision versus monopolar electrosurgical excision for tonsillectomy. Otolaryngol Head Neck Surg. 2005;133(1):51–54. doi: 10.1016/j.otohns.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 6.Lee YC, Hsin LJ, Lin WN, Fang TJ, Tsai YT, Luo CM. Adolescents and adults undergoing temperature-controlled surgical instruments vs electrocautery in tonsillectomy: a aystematic review and meta-analysis of randomized clinical trials. JAMA Otolaryngol Head Neck Surg. 2020;146(4):339–346. doi: 10.1001/jamaoto.2019.4605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nemati S, Banan R, Kousha A. Bipolar radiofrequency tonsillotomy compared with traditional cold dissection tonsillectomy in adults with recurrent tonsillitis. Otolaryngol Head Neck Surg. 2010;143(1):42–47. doi: 10.1016/j.otohns.2010.03.031. [DOI] [PubMed] [Google Scholar]
- 8.Ragab SM. Six years of evidence-based adult dissection tonsillectomy with ultrasonic scalpel, bipolar electrocautery, bipolar radiofrequency or 'cold steel' dissection. J Laryngol Otol. 2012;126(10):1056–1062. doi: 10.1017/S0022215112002022. [DOI] [PubMed] [Google Scholar]
- 9.Wong DL, Baker CM. Pain in children: comparison of assessment scales. Pediatr Nurs. 1988;14(1):9–17. [PubMed] [Google Scholar]
- 10.Frison L, Pocock SJ. Repeated measures in clinical trials: analysis using mean summary statistics and its implications for design. Stat Med. 1992;11(13):1685–1704. doi: 10.1002/sim.4780111304. [DOI] [PubMed] [Google Scholar]
- 11.Hall DJ, Littlefield PD, Birkmire-Peters DP, Holtel MR. Radiofrequency ablation versus electrocautery in tonsillectomy. Otolaryngol Head Neck Surg. 2004;130(3):300–305. doi: 10.1016/j.otohns.2003.09.024. [DOI] [PubMed] [Google Scholar]
- 12.Businco LDR, Tirelli GC. Paediatric tonsillectomy: radiofrequency-based plasma dissection compared to cold dissection with sutures. Acta Otorhinolaryngol Ital. 2008;28(2):67–72. [PMC free article] [PubMed] [Google Scholar]
- 13.Stoker KE, Don DM, Kang DR, Haupert MS, Magit A, Madgy DN. Pediatric total tonsillectomy using coblation compared to conventional electrosurgery: a prospective, controlled single-blind study. Otolaryngol Head Neck Surg. 2004;130(6):666–675. doi: 10.1016/j.otohns.2004.02.012. [DOI] [PubMed] [Google Scholar]
- 14.Morinière S, Roux A, Bakhos D, Trijolet JP, Pondaven S, Pinlong E, et al. Radiofrequency tonsillotomy versus bipolar scissors tonsillectomy for the treatment of OSAS in children: a prospective study. Eur Ann Otorhinolaryngol Head Neck Dis. 2013;130(2):67–72. doi: 10.1016/j.anorl.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 15.Kumar S, Padiyar BV, Rai AK. Cold dissection tonsillectomy and radiofrequency tonsil ablation: a prospective comparative study. Dubai Med J. 2018;1(1–4):6–12. doi: 10.1159/000493513. [DOI] [Google Scholar]
- 16.Ragab SM. Bipolar radiofrequency dissection tonsillectomy: a prospective randomized trial. Otolaryngol Head Neck Surg. 2005;133(6):961–965. doi: 10.1016/j.otohns.2005.07.037. [DOI] [PubMed] [Google Scholar]
- 17.Aksoy F, Ozturan O, Veyseller B, Yildirim YS, Demirhan H. Comparison of radiofrequency and monopolar electrocautery tonsillectomy. J Laryngol Otol. 2010;124(2):180–184. doi: 10.1017/S0022215109991642. [DOI] [PubMed] [Google Scholar]
- 18.Hegazy HM, Albirmawy OA, Kaka AH, Behiry AS. Pilot comparison between potassium titanyl phosphate laser and bipolar radiofrequency in paediatric tonsillectomy. J Laryngol Otol. 2008;122(4):369–373. doi: 10.1017/S0022215107008328. [DOI] [PubMed] [Google Scholar]
- 19.Sunnergren O, Hemlin C, Ericsson E, Hessén-Söderman AC, Hultcrantz E, Odhagen E, et al. Radiofrequency tonsillotomy in Sweden 2009–2012. Eur Arch Otorhinolaryngol. 2014;271(6):1823–1827. doi: 10.1007/s00405-013-2867-4. [DOI] [PubMed] [Google Scholar]
- 20.Krishna P, Lee D. Post-tonsillectomy bleeding: a meta-analysis. Laryngoscope. 2001;111(8):1358–1361. doi: 10.1097/00005537-200108000-00008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.