Abstract
Arthrocentesis is a simple minimally invasive procedure with less risk of complications and significant benefits in patients with internal derangement of temporomandibular joint. Here we report a study on four patients to evaluate the efficacy of arthrocentesis in the treatment of internal derangement of temporomandibular joint.
Keywords: Temporomandibular joint, Internal derangement, Arthrocentesis
Introduction
Arthrocentesis is a method of flushing out the temporomandibular joint (TMJ) by placing needles into the upper joint compartment using local anesthesia or sedation. The process is referred to as lysis or lavage and can produce good therapeutic outcomes in patients with restricted mouth opening due to either an anchored disc phenomenon or a non-reducing disc displacement [1]. It has low morbidity, few risks and low cost compared to other TMJ surgical interventions, and may be conducted under local anesthesia in an outpatient setting [2, 3].
Patients with TMJ disorder may present with a cluster of joint and muscle disorders characterized primarily by pain, joint sounds and irregular or deviating jaw. Clinical trials suggested splint therapy, arthrocentesis, arthroscopic lysis and lavage and arthrotomy to be effective on TMJ related signs and symptoms in terms of therapy [4].
Internal derangement (ID) of the TMJ is characterized by displacement of the intra-articular disc, resulting in clicking and popping sounds. These conditions may be painless or may be associated with pain, especially during function. The most common causes are trauma, which results in an immediate displacement of the disc, or chronic parafunction, resulting in degenerative changes causing increased friction and gradual disc displacement (arthro1). The study aims to evaluate the efficacy of arthrocentesis in the treatment of ID of TMJ in 4 patients.
Case Report
A total number of 4 patients reported in department of Oral and Maxillofacial Surgery, Chandra Dental College and Hospital, Lucknow (U.P) with the chief complaint of pain and clicking in the TMJ. Out of 4 patients there were 2 males and 2 females. These patients presented with significant pain and limitation of mouth opening. Three patients were diagnosed with painful clicking and one was diagnosed with closed lock either due to a displaced disc or anchored disc phenomenon. All the patients reported for the previous treatment with pain killers and conservative treatment in the form of occlusal splint for one month period, which failed to relieve the symptoms. An OPG was taken (Figs. 1, 2, 3, 4) which showed slight forward displacement, beginning of deformity of disc, thickening of posterior edge of disc in painful patients. However, there was no hard tissue change was noted in closed lock patient. Preoperative maximal interincisal opening (MIO) and pain score in the form of visual analogue scale (VAS) ranging from 1 to 10 was recorded.
Fig. 1.

OPG patient 1
Fig. 2.

OPG patient 2
Fig. 3.

OPG patient 3
Fig. 4.

OPG patient 4
Technique
All these patients with failed conservative treatment were subjected for TMJ arthrocentesis. Under aseptic conditions arthrocentesis was performed in the superior joint space of all 4 patients. A line is drawn from the lateral canthus to the most posterior and central point on the tragus (Halmlund-Hellsing Line). The posterior line of entry is located along the canthotragal line 10 mm from the middle of the tragus and 2 mm below the canthotragal line. This is the approximate area of the maximum concavity of the glenoid fossa. The anterior point of entry is placed 10 mm further along the canthotragal line and 10 mm below it, which indicates the site of the eminence f the TMJ. Through one needle Ringer’s lactate is injected into the superior joint space while the second needle acts as an outflow portal for the lavage of joint cavity (Figs. 5, 6, 7, 8). Post operative care included NSAIDS, physical therapy and soft diet. Patients with the habit of bruxism and clenching were instructed for the placement of occlusal splints. All the patients were followed up for 6 months and there was no abnormality reported.
Fig. 5.

Lavage of joint space patient 1
Fig. 6.

Lavage of joint space patient 2
Fig. 7.
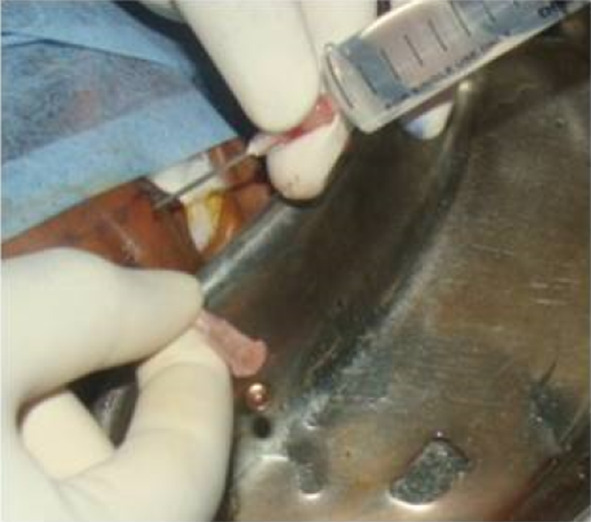
Lavage of joint space patient 3
Fig. 8.

Lavage of joint space patient 4
Discussion
The currently adopted technique to perform arthrocentesis of the TMJ provides a double access to the joint space. Such an access is performed by taking as indicator, the Halmlund Line and consists of the positioning of two 19-G needles within a small virtual cavity [1]. This method is consistent with method which is used in our study. Clinical evidences support regarding disc displacement in TMJ internal derangement.
There are suggestions that a change in the position of the disc is not a primary factor in TMJ pain and dysfunction but alterations in joint pressure, biochemical substances, and constituents of the synovial fliud may lead to clicking and derangement of the TMJ. Inflammatory cells and inflammatory mediators including arachidonic acid metabolites and cytokines were also been demonstrated in symptomatic patients with TMJ problem [2]. Proteins involved in inflammation such as haptoglobin, ceruloplasmin, compliment C3 and fibrinogen aswell as collagen and IgG and IgM are found in synovial fluid of painful TMJs. Lipid pain mediators such as prostaglandin D2, E2, F2a, 6-Keto, F; thromboxane 2a, prostacyclin and leukotriene B4, and platelet activating factor which accumulate in the inflamed synovial fluid and their presence is correlated with synovitis. These protein and lipid moieties act on nerve ending of the synovial membrane and provoke nociception [3, 4].
Arthrocentesis is the recent surgical approach for the internal derangement of the TMJ. Many cases of the anterior displacement of the disc or closed lock that did’nt improve with medical treatment were treated with surgical repositioning of the disc and arthroplasty of the mandibular fossa. Arthrocentesis has an intermediate place between the medical and the surgical forms of treatment [3]. There are no longitudinal studies to compare the success of this technique but studies suggests that arthrocentesis is an efficient method with relatively high success rate. This is consistent with our study as all the patients had improvement in symptoms related to the intrarticular derangement and increased mandibular movement. It is a first line procedure for acute and chronic closed lock of the TMJ. It is minimally invasive, effective ad has minimal potential complications [4].
The orthopedic literature includes its use for the symptomatic relief of pain in patients with traumatic synovitis, emarthrosis, arthritides, pseudogout, lupus erythematosis, and septic arthritis. Development of arthrocentesis for the TMJ was a natural consequence of the success with arthroscopic lysis and lavage for the treatment of limited mandibular movement. It is understood to include lavage of the upper joint space, hydraulic pressure and manipulation to release adhesions, or the anchored disc phenomenon or the suction cup effect and improve motion and the therapeutic injection of a steroid [4]. On some occasions, the procedure also includes inserting a blunt instrument inside the joint. The instrument is used in a sweeping motion to remove tissue adhesion bands and to dislodge a disc that is stuck in front of the condyle (ball) inside of the joint. If jaw pain goes away after arthrocentesis, the surgery was a success. If pain does not subside more invasive procedures are probably necessary [5, 8, 9].
The technique of arthrocentesis reported in the literature itself varies considerably. A number of irrigating solutions have been used in varying quantities and at different pressures. Intra operatively, the jaw has been manipulated to increase the mouth opening and inn addition, various medications, splint therapy and physical therapy have also shown improvement [11], which is similar in our study also.
According to Monge-Gil F et al. in their review of 14 studies the average age of the patients was 34.3 years and the average duration of the lock was 12.8 months which was consistent with the age of the patients in our study (23–34 years). It was concluded that age and duration of the lock should be considered as indicators for predicting the result of this type of procedure [6].
Murakami et al. found that arthrocentesis was more effective in the treatment of TMJ closed lock while Goudot et al. found the arthroscopy was more effective in improving mouth opening. However, both are not without risks. Damage to facial and auriculotemporal nerves, perforation of the external auditory canal and tympanic membrane and breach of the base of skull have been reported in arthroscopy. Transient facial nerve paralysis caused by local anaethesia, swelling of the preauricular area due to fluid extravasation may result from arthrocentesis. No such complication was encountered with the patients reported in this study [7].
Conclusion
Arthrocentesis is a simple and minimally invasive procedure. Lavage of superior joint space with saline exerts its effects through its ability to eliminate joint effusion thus reducing the symptoms. These observations make this technique as a line of treatment for patients with TMJ internal derangements.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Vikas Kumar, Email: drvikaslko@gmail.com.
Ambrish Kaushal, Email: ambrishkaushal@rediffmail.com.
Devesh Tiwari, Email: deveshomfs@gmail.com.
Syed Mohd Ahmad, Email: dr_ahmad123@yahoo.co.in.
References
- 1.Nardini LG, Manfredini D, Ferronato N. Arthrocentesis of the temporomandibular joint: a proposal for a single needle technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:83–86. doi: 10.1016/j.tripleo.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 2.Neeli AS, Umerani M, Katrashetti SM, Baliga S. arhrocentesis for the treatment of internal derangement of the temporomandibular joint. J Maxillofac Oral Surg. 2010;9(4):350–354. doi: 10.1007/s12663-010-0155-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vasconcelas BC, Do Egito NRVB, Roch NS. temporomandibular joint arthrocentesis: evaluation of results and review of the literature. Rev Bras Otorrinolanringol. 2006;72(4):634–638. doi: 10.1590/S0034-72992006000500009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Matsa S, Kumar Raja VBK, Bhalerao S, Sekhar S. temporomandibular joint arthrocentesis for closed lock-a prospective analysis of 10 consecutive cases. SRM Univ J Dental Sci. 2010;1(3):225–229. [Google Scholar]
- 5.Norman N, Purcell TMJ (xxxx) Arthrocentesis, arthroscopy and lavage. Therapy in motion-Physical therapy with a personal touch; www.therapyinmotion.net.
- 6.Monje-Gil F, Nitzan D, Garcia RG. Temporomandibular joint arthrocentesis-review of the literature. Med Oral Patol Oral Cir Bucal. 2012;17(4):e57–81. doi: 10.4317/medoral.17670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tan DBP, Krishnaswamy G. A retrospective study of temporomandibular joint internal derangement treated with arthrocentesis and arthroscopy. Proc Singapore Healthcare. 2012;21(1):73–78. doi: 10.1177/201010581202100112. [DOI] [Google Scholar]
- 8.Manfredini D, Rancitelli D, Guarda-Nardini L. arthrocentesis in temporomandibular joint inflammatory-degenerative disease: a randomized and controlled trial. Zeitschrift fur Kraniomandibulare Funktion. 2011;3(1):41–46. [Google Scholar]
- 9.Shinohara EH, Pardo-Kaba SC, Martini MZ, Horikawa FK. single puncture for TMJ arthrocentesis: an effective technique for hydraulic distension of the superior joint space. Natl J Maxillofacial Surg. 2012;3(1):96–97. doi: 10.4103/0975-5950.102177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Samiee A, Sabzerou D, Edalatpajouh F, Clark GT, Ram S. temporomandibular joint infection with corticosteroid and local anaesthetic for limited mouth opening. J Oral Sci. 2011;3(3):321–325. doi: 10.2334/josnusd.53.321. [DOI] [PubMed] [Google Scholar]
- 11.Ethunandan M, Wilson AW. temporomandibular joint arthrocentesis-more questions and answers. J Oral Maxillofac Surg. 2006;64:952–955. doi: 10.1016/j.joms.2006.02.012. [DOI] [PubMed] [Google Scholar]


