Abstract
Audiologists extend their services to wide range of patients who vary across several factors like age, disease, nutritional status, pharmacological intervention, socioeconomic status and compromised immune systems. This involves direct or indirect contact with patients exposing the clinician to blood, and other bodily fluids which are considered to be potentially infectious substances. Thus infection control activities must be stressed with the goal of reducing or preventing the transmission of nosocomial pathogens to patients and staff. The aim of the study is to provide an in-depth assessment of current infection control strategies and hygienic measures followed among Audiologists in India. An internet based questionnaire survey was done among 172 Audiologists. The questionnaire focused on four domains: demography; knowledge, attitude and practice of infection control and hygienic measures followed in audiology clinic. Majority of the participants had a positive attitude towards infection control practice. Though most of them had an access to gloves (73.3%) and masks (60%), their usage was minimal and restricted to selected procedures. Hand hygienic measures were practiced by 89% of the participants only during few procedures. Irrespective of critical or non-critical instruments, majority of the participants preferred cleaning and disinfecting. Sterilisation of critical instruments was performed only by 30% of the audiologists. Audiologists knowledge and practice of infection control and hygienic measures was found to be inadequate. Specialized training program on infection control strategies should be targeted to the newly graduated and practicing audiologists to ensure patient safety and infection free clinical environment.
Keywords: Infection control, Hand hygiene, Sterilisation, Disinfection, Audiologist
Introduction
Infection prevention and control is a scientific approach and practical solution designed to prevent patients and health care workers from any harm caused by infections [1]. Audiology practice involves and requires a notable degree of direct and indirect patient contact [2–4]. Audiologists use various instruments, devices, probes, specula, ear moulds and hearing aids in their clinical environment which comes into direct or indirect contact with multiple patients and hence, the importance of infection control is paramount. [2, 5, 6] The scope of audiology practice has expanded in the past few years, where audiologists are involved in intraoperative monitoring, handling, insertion and removal of needle electrodes; thereby, placing audiologists at risk for potential exposure to blood and other bodily fluids [7–9].
Audiological services are catered to the need of wide variety of patients’ in different age group, with different underlying disease/condition, socio-economic status and nutritional status [10, 11]. Geriatrics, paediatrics, HIV positive individuals, diabetics, and other population with immune-compromised system are at greater risk of acquiring life threatening serious infections as a result of exposure to ubiquitous microbes [2, 11]. Infection control measures must be implemented by Audiologists to prevent infection spread from the potential sources in audiology clinics [12]. These measures not only involve controlling the exposure between people but also between people and the environment. In order to accomplish this, specific infection control guidelines must be followed in any health care settings to reduce the risk of cross-infection and cross-contamination [2, 13].
Some of the possible infections that spread in audiology clinic includes Acquired Immune Deficiency Syndrome (AIDS), chicken pox, common cold, cytomegalovirus, hepatitis A, hepatitis B, herpes simplex 1, herpes zoster, infectious mononucleosis, infectious meningitis, influenza, measles, mumps, otitis externa, pneumonia, tuberculosis, streptococcus and staphylococcus infection [3, 14, 15]. As audiologists are at risk for exposure to and transmission of various infectious diseases, immunizations/vaccinations are considered to be an effective way in protecting audiologists from infections [3, 4, 7]. Infections caused by measles, mumps, rubella, chicken pox, pertussis, tuberculosis, hepatitis A, hepatitis B, tetanus and influenza are all preventable though vaccination. [10, 15–17].
In India, National Centre for Disease Control [14] and Indian Council of Medical Research [15] has provided guidelines with respect to infection control strategies. These guidelines follow similar protocols as implemented by Centre for Disease Control and Prevention [18]. These universal precautions comprises of five general pronouncements such as use of appropriate personal barriers during various procedures (such as glove and masks), hand hygiene measures, cleaning and disinfecting touch and splash surfaces, sterilizing critical instruments and disposing the waste appropriately [9, 11].
Only few studies have attempted to assess infection control practices in the field of audiology in western countries [10, 13, 19, 20]. It has been reported that majority of the audiologists surveyed were unaware of the potential sources of cross infection caused by various microbes located on audiological instruments including headphones, specula, probe tips and tubes in the clinic [10, 19, 20]. In developing countries like India, there is an increased prevalence of infectious disease and spread of infections is reported to be 2–6 times higher than those reported in developed countries [21, 22]. The extent to which audiologists appreciate the need for infection control and implementation of infection control strategies followed in audiology clinic in India remains unknown. Owing to the vulnerability and existence of different health care provision, facility and resources, it is essential to explore Audiologists knowledge and practice of infection control strategies in India. Therefore, this study aimed to explore the infection control strategies and hygienic measures followed by Audiologists in their clinical set-up.
Materials and Methods
Participants
One hundred and seventy-two currently practicing full time/part time audiologists participated in the study. Audiologists who were not practicing in India at the time of study and students pursuing their bachelor or master’s programme on speech and hearing were excluded from the study.
Procedure
The study was carried out in two phases. Phase 1 of the study involved construction of the questionnaire and phase 2 involved administration of the questionnaire.
Construction of the Questionnaire
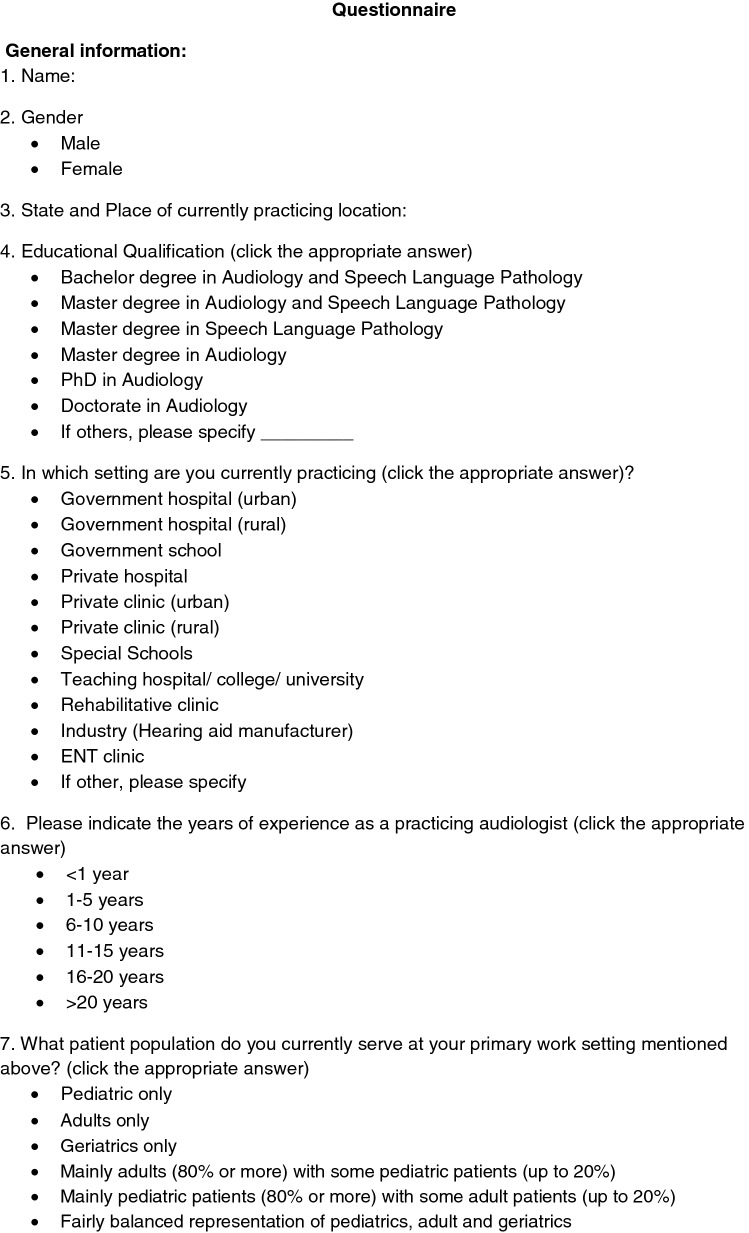
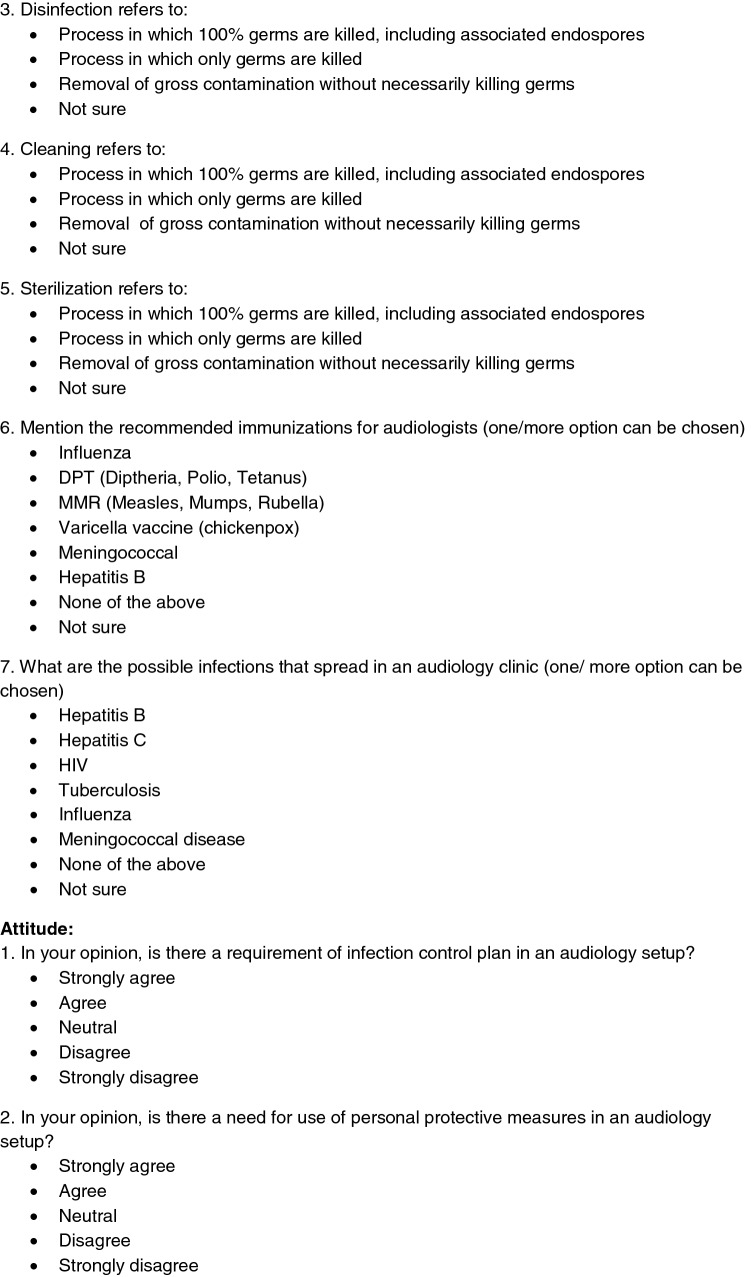
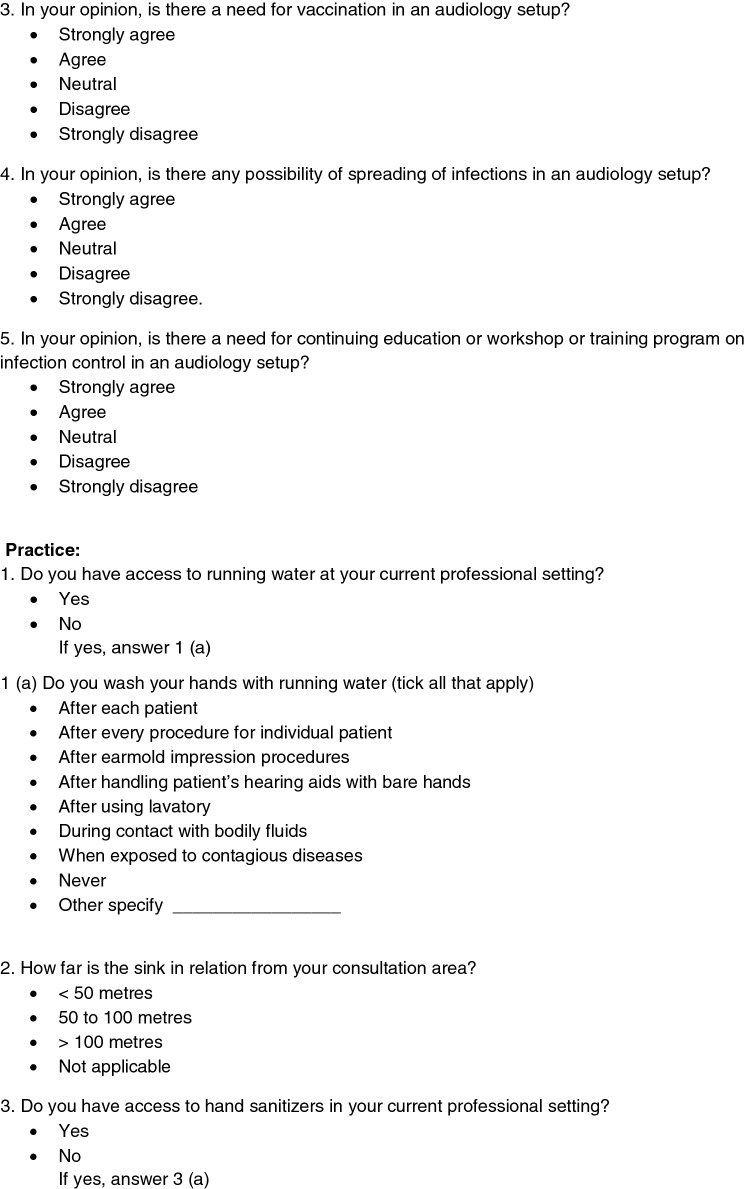
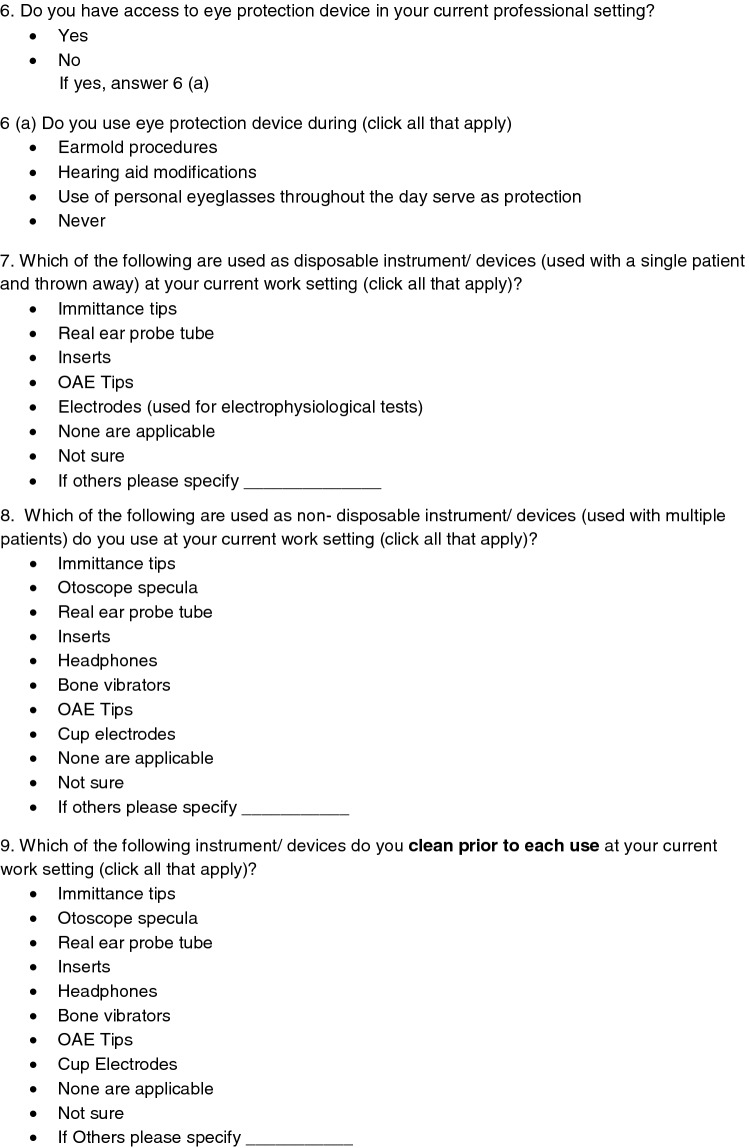
The questionnaire was constructed based on previous literature on infection control [13, 19, 20]. The developed questionnaire comprised of 45 questions under four domains: Domain I dealt with general information, Domain II focused on knowledge on infection control and hygiene measures, Domain III dealt with the attitude for the requirement of infection control and hygiene measures, and Domain IV assessed infection control practices followed in audiology clinic. The questions were verified and validated for its content by 3 audiologists (“Appendix”).
Administration of the Questionnaire
The questionnaire that was content validated was converted to a web version and was launched from a period of November 1, 2018 to 15th January, 2019. This web link was mailed to the Audiologists working in India. Details and purpose of the study were provided along with the inclusion criteria to participate in the study. Participants who met the inclusion criteria and who consent to participate in the study completed the survey. The filled surveys were accessed from server database. Once the data collection was closed the information was downloaded from the website and analysed.
Statistical Analysis
Percentage analysis was done to profile the responses of audiologists for each item. Statistics were calculated using the Statistical Package for the Social Sciences (version 16.0).
Results
The present study aimed to identify the knowledge, attitude and practice of infection control and hygienic measures among Audiologists practicing in India. Results on each domain are presented below:
General Information
Of 172 Audiologists (59.3% female and 40.7% male) who participated in the study, 48.8% had master degree in audiology and speech language pathology, 27.9% had bachelor degree in audiology and speech language pathology, 15.1% had master degree in Audiology, 5.8% had doctorate in Audiology and others had master degree in speech language pathology. More than one-third of participants (33%) reported of working in private audiology clinic and academic institutions, 15.7% in private hospitals, 14% in Government hospital, 9.3% in ENT clinic, 5.8% in rehabilitative clinic and others in hearing aid industries, special school and cochlear implant companies.
Nearly half of the participants (45.9%) had 1–5 years of experience, 21.5% had 6–10 years of experience, 12% had 11–20 years of experience, followed by 20% who had less than 1 year of experience. Around 55.8% of the participants serve a fairly balanced population of paediatrics, adult and geriatrics with the majority of the participants (> 60%) performing pure tone audiometry, immittance audiometry, otoscopy, otoacoustic emission, evoked potentials, dispensing hearing aids and neonatal hearing screening. With respect to the educational experience on infection control, most of the participants (66.3%) did not have any experience related to infection control in audiology clinic.
Knowledge
Agencies Related to Infection Control and Need for Personal Barriers
Only 45.3% of the participants were aware of the agencies related to infection control. Occupational Safety and Health Administration (OSHA) and Food and Drug Administration (FDA) were the two agencies that were familiar to the audiologists. With respect to the personal barriers such as gloves, masks, gowns and eye protection devices, only 9.3% of the participants appreciated the need of all the personal barriers in audiology clinic. More than 60% of the participants appreciated the need for gloves and masks in the clinics.
Terminologies Related to Infection Control
With respect to the terminologies, majority of the participants (80%) were able to identify the definition of term sterilization, followed by cleaning (53%) and disinfection (43%). Around 35% of the participants were not sure of the terminologies related to infection control.
Immunization and Spread of Infections in Audiology Clinic
On assessing participants’ knowledge on immunization and infections that spread in an audiology clinic, more than one-third of the participants (38.4%) were not sure about immunizations that are required/recommended for audiologists. Around 48.3% and 44.2% of participants were aware of the infection spread through tuberculosis and influenza respectively. Only few participants were aware of spread of other infections such as HIV, hepatitis, and meningococcal infections. Almost 29.7% were not sure of the infections that spread in audiology clinic.
Attitude
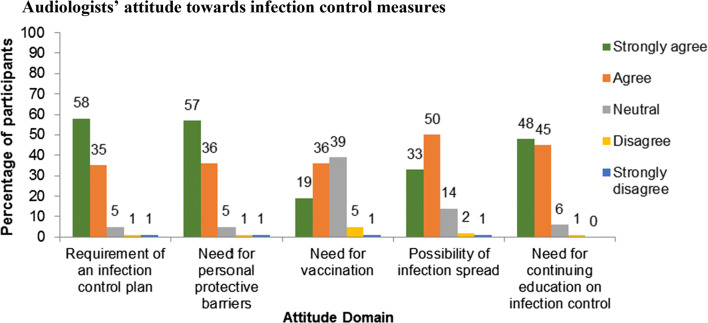
Majority of the participants expressed positive attitude towards the need for infection control measures (Fig. 1). More than one-third of the participants had neutral views towards the need for vaccination.
Fig. 1.
Audiologists’ attitude towards infection control measures
Practice
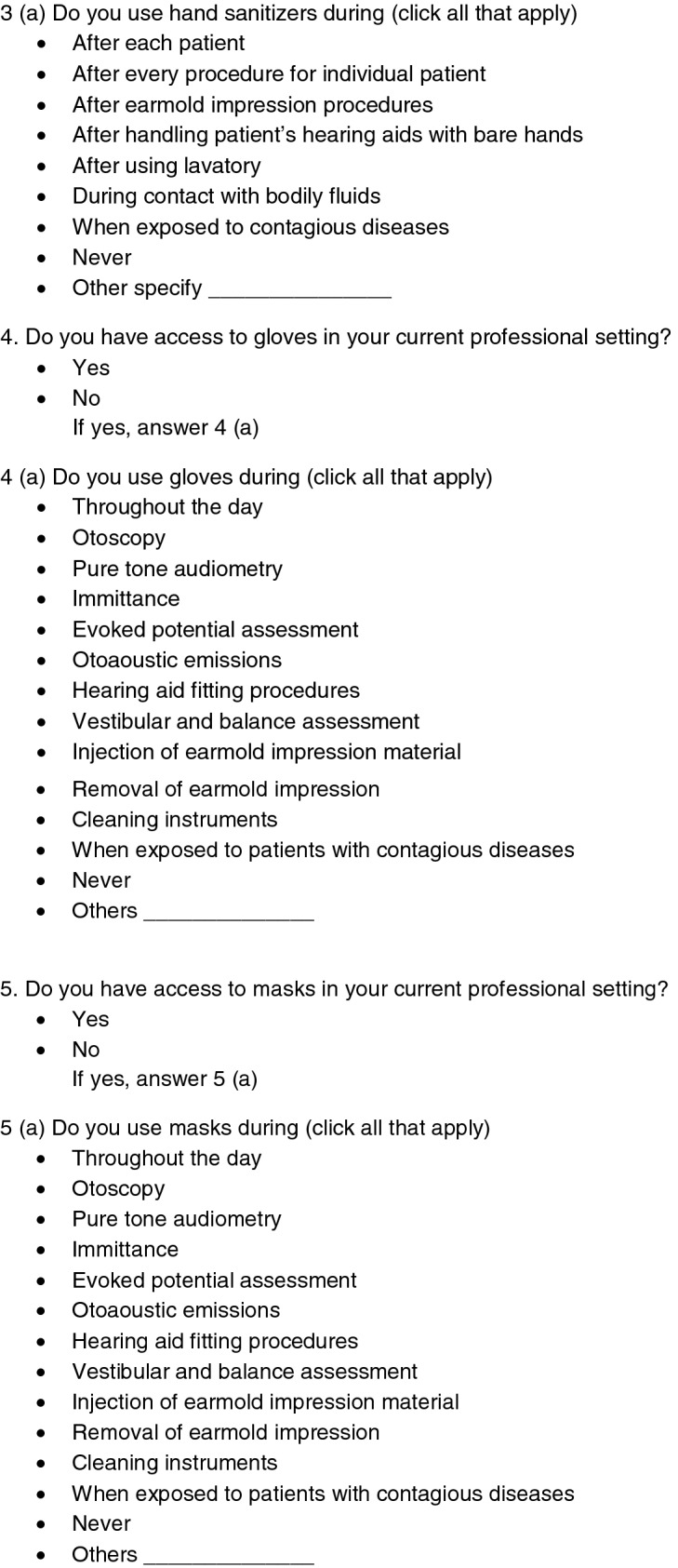
Hand Hygiene Practice
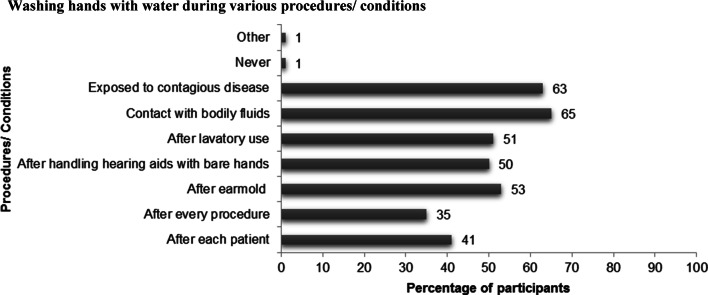
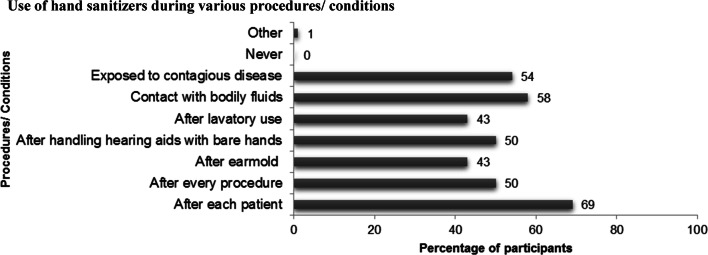
Few participants (11%) reported of no access to the running water and hand sanitizers in their clinics. Majority (89%) of the participants had access to running water and hand sanitizers. However, the hand hygiene practices were not consistently followed in all required and recommended procedures/situations but were reported to follow on certain instances (Figs. 2, 3). Around 65% of the participants reported of washing hands when they are in contact with bodily fluids. Majority (69%) reported of using hand sanitizers after each patient.
Fig. 2.
Washing hands with water during various procedures/conditions
Fig. 3.
Use of hand sanitizers during various procedures/conditions
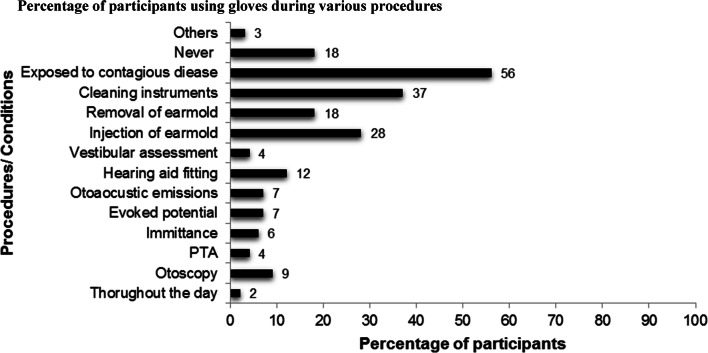
Access and Use of Personal Protective Barriers
Most of the participants (73.3%) had an access to gloves in their work setting. Though majority had access to gloves, it has not been regularly used (Fig. 4). Only 2% of the participants reported of using gloves throughout the day. It was very concerning to know that 18% of them never wore gloves.
Fig. 4.
Percentage of participants using gloves during various procedures
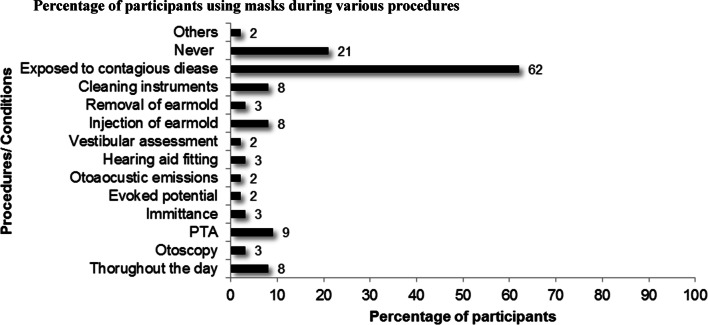
Only 60.5% participants had access to masks in their work setting, of which 21.2% of the participants never used. Percentage of participants who used masks during various procedures/conditions was represented in Fig. 5.
Fig. 5.
Percentage of participants using masks during various procedures
Majority of the participants (91.3%) do not have access to eye protection devices in their work setting. Participants (8.7%) who had access to eye protection devices reported of using it during earmold and hearing aid modification procedures.
Disposables Used in Audiology Clinic
Majority of the participants reported of re-using the accessories that are meant to be disposed after use. Only few participants (36%) disposed electrodes that were used in electrophysiological testing. Less than 20% of the participants disposed insert tips (19.8%), OAE tips (11%), immittance tips (10.5%) and real ear probe tubes (7%).
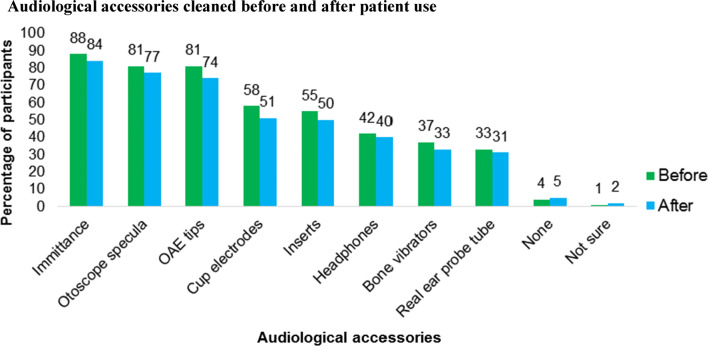
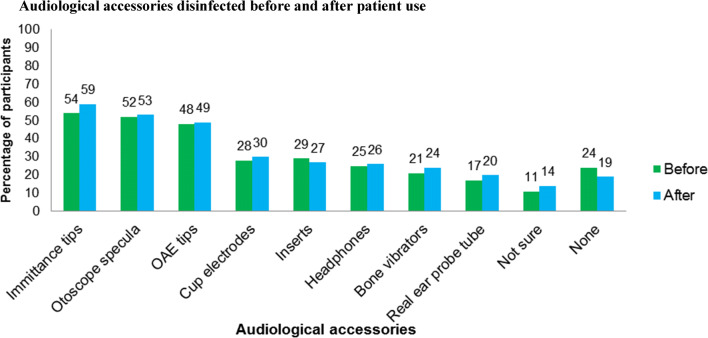
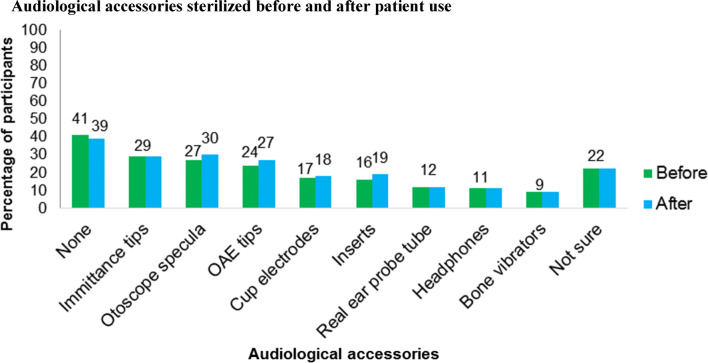
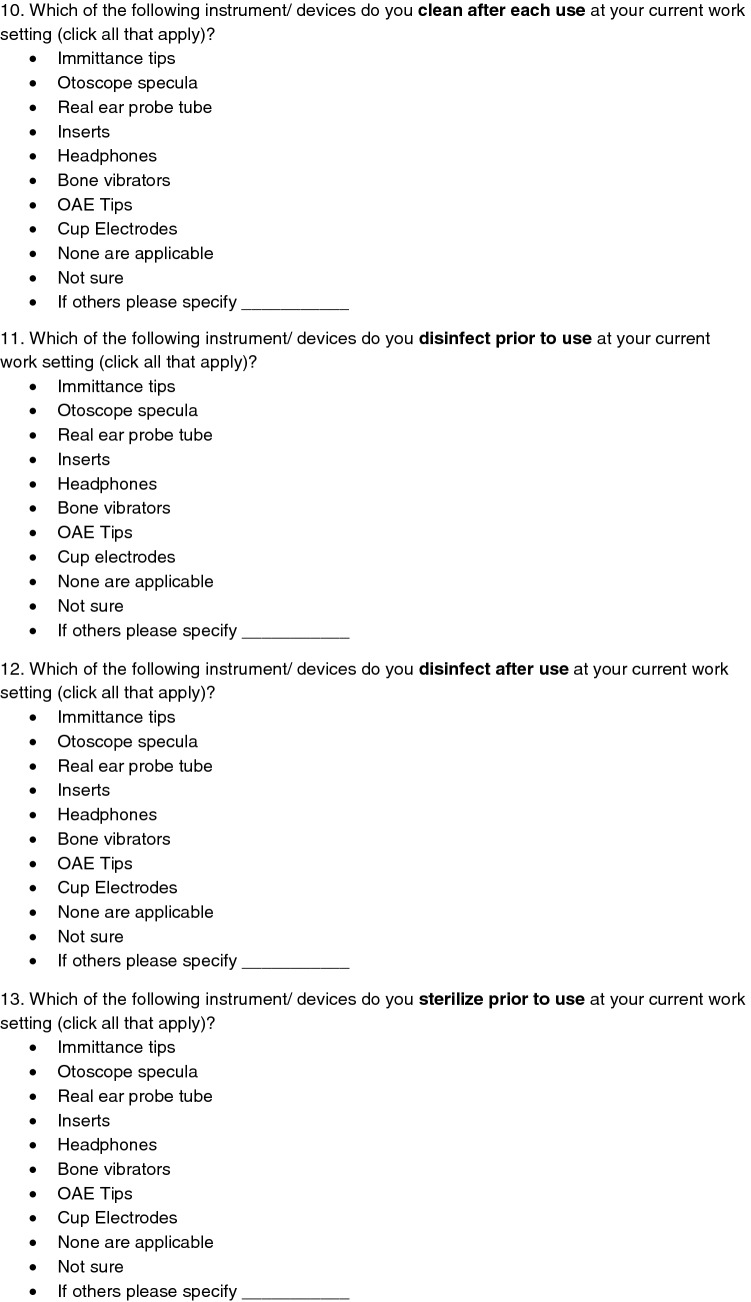
Cleaning, Disinfecting and Sterilizing Audiological Accessories
Majority of the participants used non-disposable transducers such as headphones (88.4%) and bone vibrators (86.6%). However, the cleaning, disinfecting and sterilizing of the same was not adequately practiced by the audiologists. Other non- disposables that were used includes otoscope specula (75%), immittance tips (73.3%), OAE tips (68%), inserts (58.7%), cup electrodes (55.2%) and real ear probe tube (39%). It was appreciated that majority of the participants cleaned and disinfected immittance tips, OAE tips and otoscope specula before and after patient use when compared to that of other accessories that were used in audiology clinic. However, sterilization of these accessories were not adequately practiced. Percentage of participants who clean, disinfect and sterilize accessories before and after use are represented in Figs. 6, 7, 8 respectively.
Fig. 6.
Audiological accessories cleaned before and after patient use
Fig. 7.
Audiological accessories disinfected before and after patient use
Fig. 8.
Audiological accessories sterilized before and after patient use
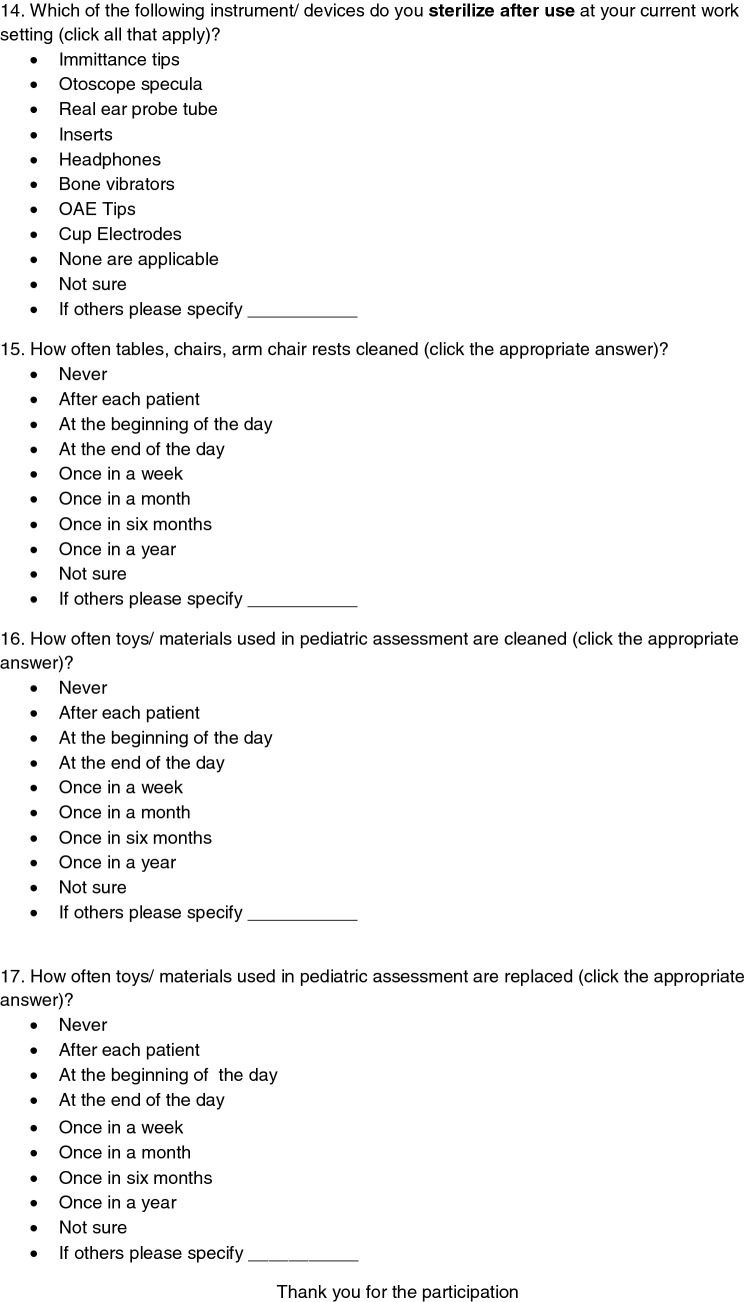
Touch Surfaces and Toys
Half of the participants (50.6%) reported of cleaning touch surfaces at the beginning of the day. It was surprising to know that the toys used in audiology clinic were not cleaned and replaced regularly. Only few participants reported of cleaning toys once in a week (23.8%), once in a month (12%), once in six months and once in a year (< 5%). Only few participants (17%) reported of replacing toys once in a year.
Discussion
Knowledge
Agencies Related to Infection Control and Use of Personal Barriers
In the current study, only 50% of the participants were aware of these agencies related to infection control and only 9% of participants reported that all the personal barriers should be used in audiology clinic. This indicated a lack of knowledge on the agencies related to infection control and need for personal barriers among Audiologists practicing in India. In the curriculum of speech, language pathology and audiology, topics focusing on infection control and regulatory agencies for infection control and hygiene practice should be made mandatory. In addition to this, specialized training program on infection control and hygienic measures should be catered for the newly graduated and also practicing audiologists. There is not much information about these knowledge aspects of audiologists across different countries.
In India, NCDC [14] and ICMR [15] have given guidelines on infection control measures and these are based on OSHA [23] and other agencies such as Joint Commission, Environmental Protection Agency, Food and Drug Administration and Commission on Accreditation of Rehabilitation Facilities [12]. All these regulatory agencies have specific regulations and guidelines on how to minimise the potential spread of disease in workplace. Hence, it is the responsibility of audiologists to legally and ethically uphold the standards put forth by these agencies for infection free clinical environment [10, 13].
Terminologies Related to Infection Control
Knowledge on infection control terminologies should be considered as an important aspect among audiologists as this directs the professionals to follow infection control strategies appropriately and efficiently. In the current study, almost 80% of the participants had adequate knowledge on the term sterilization. Whereas, only 40% and 53% of participants had knowledge of the term disinfection and cleaning respectively. In contrast to the current findings, Burco [13] reported that more than 80% of audiologists practicing in United States correctly identified the term sterilization and almost 70% identified the term disinfection and cleaning. Almost 70% of those participants had reported of attending annual training on infection control which could be the reason for their familiarity with the terminologies [13]. Whereas, in the current study, only 33.7% of the partipants had underwent training on infection control.
Immunizations and Infections that Spread in Audiology Clinic
Immunization is considered to be the single most effective method to prevent transmission of several diseases [7, 16]. In the current study, 20% of audiologists felt the need for Hepatitis B vaccine. Thirty percent of the participants appreciated the need for influenza, MMR and varicella vaccine indicating an insufficient knowledge on the importance of immunizations in majority of the participants. OSHA [23] mandated the need for Hepatitis B Vaccine (HBV) for all the healthcare workers [2]. In addition to Hepatitis B, the other vaccines that were recommended by ICMR [15] include Measles Mumps Rubella (MMR), Tetanus, Varicella, Meningococcal, and Influenza [10, 17].
More than one-fourth of the participants were not sure of the infections that spread in an audiology clinic. ICMR [15] had listed various infections that spread in clinical setup which includes influenza, hepatitis B, tuberculosis and AIDS [4, 10]. It is important to adhere to the immunization recommended by ICMR among healthcare workers to create a safe and infection controlled work setup.
Audiologists who are actively involved in intraoperative monitoring or post -surgical assessments as their mainstay of employment meet the category of 1; audiologists who are involved in handling hearing aids, earmold impressions, cerumen removal, cleaning, disinfecting and sterilizing instruments meet the classification of category 2 and finally audiologist who is an administrator or any front office staff who does not have any patient contact will be classified as category 3 [23]. These categorization of audiologists is not prevailing in India. It has been recommended that HBV must be made available to all category 1 and 2 workers free of charge [24, 25]. This vaccine administration details has to be placed in the infection control plan records of every clinic [23]. Since, there is a dearth of literature on audiologists’ knowledge on various infections that spread in an audiology clinic and vaccinations recommended for audiologists both in India and other countries, comparisons could not be made with the current study.
Attitude
Majority of the participants agreed on the need for infection control plan, use of personal protective barriers in audiology clinic and need for continuing education on infection control. Audiologists did not have positive attitude towards need for vaccination. This could be due to the fact that in India, people do not prefer immunization [26]. They believe that it may affect the natural immunity and may kill the body’s own ability to fight against infections [27]. It is important to highlight that they are at high risk of contracting the disease themselves, which can in turn lead to spread of disease to their vulnerable patients, compromising patient safety [28]. Globally, there is not much information available related to immunization among audiologists. Practicing audiologists should serve as role models who can influence their peers/students to get vaccinated. This may in turn improve the quality of patient care. For all these reasons, one could see immunization as a duty of professionalism and an ethical responsibility [4].
Practice
Hand Hygiene Measures
Hand hygiene measures such as washing hands with running water and use of hand sanitizers is considered to be the most critical measure for infection control program [4, 12]. It was interesting to know that 90% of the participants have access to running water and hand sanitizers in their clinical setup which is similar to the results obtained from studies done in South Africa [19] and United States [13]. It was surprising to know that hand hygiene procedures were followed only during few procedures and conditions. Similarly, Burco [13] and Amlani [20] also had reported that accessibility did not correspond to the practice of hand hygiene procedures. Even though, the clear benefits of hand washing have been proven in many healthcare settings, the lack of consistent hand washing practices remains a worldwide issue [29]. Thus, monitoring of hand hygiene is a key component in improving infection control processes and its compliance in clinical setup.
Personal Protective Barriers
Personal barriers that are of major importance in audiology clinic includes gloves, disposable masks and eye protection devices [30]. In the current study, though gloves were accessible to 70% of the participants only less than 40% of them wore gloves when exposed to patients with contagious disease, ear mould procedures and while cleaning audiological instrument. This is similar to the results obtained in South Africa [19] and United States [13] where the use of personal protection barrier is less among audiologists. Audiologists must be aware that the earmold, hearing aids and audiological accessories may be contaminated with cerumen or other microorganisms, which may increase the possibility of cross contamination and disease spread when proper infection control procedures were not utilized [9, 31].
Most of the participants in the current study had reported the availability of masks in audiology clinics and majority reported of unavailability of eye protection devices. Safety glasses and masks were not adequately used during any of the audiological procedures. The findings of the current study is in line with Burco [13]. Use of masks should be encouraged during any audiological procedures to prevent clinicians from acquiring airborne microbial transmission [10]. Eye protection devices along with mask protect the conjunctiva of the eyes from particles generated from buffing/grinding wheels during earmold making [2]. Both the availability and use of eye protection devices has to be improved in audiology clinics and the need for the same has to be highlighted.
Disposables
Most audiologists did not dispose objects used in audiology clinic which were considered as disposables. Many participants continue using insert tips, electrodes, and real ear tubes for multiple patients which may contribute to the spread of infections. This could be due to the limited resources, and funding that are made available in health care systems in India [22, 32].
Cleaning, Disinfecting and Sterilizing Audiological Accessories
Certain audiological equipment are considered as non-disposables, which can be used with multiple patients after cleaning and disinfecting or sterilizing [10, 11, 30]. These are classified as critical/semi-critical and non-critical equipment based on patient contact. Critical/Semi critical equipment includes immittance tips, OAE tips, and otoscope specula. Non-critical equipment includes headphones, bone vibrators and cup electrodes [3, 33]. Critical equipment should be cleaned and sterilized whereas, non-critical equipment should be cleaned and disinfected regularly [3, 33]. Majority of the participants disinfected critical equipment before and after patient use which is not recommended to be done as it may change the property and nature of the objects that has been disinfected [10]. Very few participants practiced disinfecting non-critical instruments appropriately. Similar study done in United States [13] also indicated that only half of the participants follow the procedures of cleaning, disinfecting and sterilizing immittance and OAE probe tips, otoscope specula indicating a poor practice of infection control measures [13]. Ehlert [19] reported that over half (54%) of the audiologists reported of disinfecting mechanical equipment and 34% did not disinfect their equipment which creates the risk of cross-contamination in their patients [19]. Sterilization which should be followed for critical equipment were followed adequately by most of the participants before and after patient use [11]. However in the current study some participants also reported of sterilizing non-critical equipment which is not appropriate as these equipment should be cleaned and disinfected rather than sterilizing them [3, 19].
From the practice of cleaning, disinfecting and sterilizing audiological objects, it is evident from the current study that participants practice these methods inappropriately and knowledge on the application of the same is inadequate. This may further lead to an increased risk of transmission of infections in the clinical environment and also leads to equipment damage. Despite of having knowledge on spread of infections, disinfection and sterilisation of equipment are often overlooked. National guidelines for disinfection and sterilisation of individual audiological equipment and accessories should be made available in each audiological suite. A protocol should also be established for frequency of disinfection and to monitor its efficacy and compliance.
Cleaning Touch Surfaces and Toys
Touch surfaces such as tables, chairs and door handles serve as a potential source of indirect spread of infectious agents [4, 7]. These surfaces should be cleaned regularly and routinely. It is necessary to clean touch surfaces following each patient appointment [5, 10]. In addition to these surfaces, toys are also considered to be the carrier for various infections as they come in contact with patient during paediatric assessment procedures [2, 10].
The results of the current study show that majority of the audiologists did not felt the need to disinfect toys and touch surfaces in audiology clinics. This could be because they were not aware that toys can also contribute to infection spread in audiology clinic to the clinicians and from clinician to patient and vice versa if they are not cleaned and replaced regularly. Similar findings were reported by Ehlert [19], who had reported that only one-third of the respondents disinfected touch surfaces and toys when there were visible contaminations. Burco [13] had reported very few participants disinfected touch surfaces. However, the reported figures are not acceptable according to professional infection control guidelines [34].
Toys used for conditioning audiometry and for reinforcement should be disinfected daily as children put them in their mouth and saliva is a fertile source of bacteria [35, 36]. Increased patient load was quoted as one of the reasons for inadequate practice of cleaning touch surfaces [37, 38].
Professionals should commit themselves to basic ethical principles such as non-maleficence, trust, autonomy, and social responsibility and these should be considered as essentials in audiology practice.
Conclusion
Thus, the findings on infection control measures and hygienic practice among audiologists in India, provide valuable first-time information from this part of the world. Results from this study identified areas of concern with respect to cross infection. Audiologists are obligated to ensure that current standard practices incorporate infection control procedures as outlined by the national regulatory agencies for infection control. To establish patient safety and infection free environment, the following steps should be implemented:
Specialized training program on infection control and hygienic measures should be targeted on newly graduated and practicing audiologists.
Written infection control guidelines should be made available in every clinical setting.
Inclusion of infection control measures in undergraduate/postgraduate curriculum.
Review of infection control and annual training programs.
Audiologists must be professionally and socially responsible in their efforts to control spread of infections within the context of their clinical setting, thereby assuring infection free clinical environment. Future research can focus on reporting micro-organisms that exist on various audiological equipment/accessories used in clinics. This will further aid in creating awareness towards infection control among audiologists.
Appendix
Author contributions
Chandralekha Meenakshi Sundaram: Formulation of methodology, investigation, formal analysis, data curation, writing original draft, resources. Jayashree Seethapathy: Conceptualization, design of methodology, supervision, feedback, manuscript writing and editing.
Funding
Not applicable.
Compliance with the Ethical Standards
Conflict of interest
There is no conflict of interest.
Ethical Approval
The study was approved by the Institutional Ethics Committee, Sri Ramachandra Institute of Higher Education and Research (Deemed to be University) (REF: CSP/18/AUG/72/224).
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization (2019) Infection prevention and control (Internet). https://www.who.int/gpsc/ipc/en. Cited 24 Sep 2019
- 2.Kemp RJ, Bankaitis AU (2000) Infection control in audiology. Audiology online [Internet]. http://www.audiologyonline.com/articles/infection-control-in-audiology-1299. Cited 9 Apr 2018
- 3.The Canadian Interorganizational Group for Speech Language Pathology and Audiology (2000) Infection prevention and control guidelines for audiology [Internet]. https://canadianaudiology.ca/wp-content/uploads/2016/11/Infection-Prevention-and-Control-Guidelines-for-Audiology.pdf. Cited 9 Apr 2018
- 4.Kemp RJ, Roeser RJ. Infection control for audiologists. Semin Hear. 1998;19(2):195–204. doi: 10.1055/s-0028-1082968. [DOI] [Google Scholar]
- 5.Katz J, Chasin M, English K, Hood LJ, Tillery KL, editors. Handbook of clinical audiology. 7. Philadelphia: Wolters Kluwer Health; 2015. [Google Scholar]
- 6.American Speech and Hearing Association (2007) Infection control in audiology [Internet]. https://www.asha.org/aud/infection-control/. Cited 14 Jan 2019
- 7.Roeser RJ, Kemp RJ, Ballachanda B. Control and prevention of disease transmission in audiology practice. Am J Audiol. 1996;5(1):74–82. doi: 10.1044/1059-0889.0501.74. [DOI] [Google Scholar]
- 8.Easwar V, Boothalingam S, Chundu S, Manchaiah VKC, Ismail SM. Audiological practice in India: an internet-based survey of audiologists. Indian J Otolaryngol Head Neck Surg. 2013;65:S636–S644. doi: 10.1007/s12070-013-0674-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bankaitis AU (2012) Infection control part II: what audiologists need to do [Internet]. https://www.audiologyonline.com/articles/infection-control-part-ii-what-779. Cited 14 Jan 2019
- 10.Clark JG, Kemp RJ, Bankaitis AU. Infection control in audiological practice. Audiol Today. 2003;15(5):12–19. [Google Scholar]
- 11.Bankaitis AU, Kemp RJ (2010) ABC’ s of infection control [Internet]. https://ihsinfo.org/IhsV2/Ceus/pdf/FINAL_WEB_108929_1.pdf. Cited 8 Jul 2018
- 12.Hosford-Dunn H, Roeser RJ, Valente M. Audiology: practice management. 2. New York: Thieme Medical Publishers Inc.; 2008. [Google Scholar]
- 13.Burco A (2007) Current infection control trends in audiology [Internet]. http://digitalcommons.wustl.edu/pacs_capstones/287/. Cited 1 Apr 2019
- 14.National Centre for Disease Control [Internet]. c2016 [cited 2019 Jan 12]. https://ncdc.gov.in/WriteReadData/l892s/File571.pdf
- 15.Indian Council of Medical Research [Internet] (2016) https://www.icmr.nic.in/sites/default/files/guidelines/Hospital_Infection_controlguidelines.pdf. Cited 6 Jan 2019
- 16.Vaccine-preventable diseases and vaccines [Internet] (2019) https://www.who.int/ith/ITH-Chapter6.pdf. Cited 27 Sep 2019
- 17.Recommended Vaccines for Healthcare Workers [Internet] (2016). https://www.cdc.gov/vaccines/adults/rec-vac/hcw.html. Cited 17 Aug 2019
- 18.Centre for Disease Control and Prevention [Internet] (1996) http://www.cdc.gov/ncidod/dhqp/bp_universal_precautions.html. Cited 8 Oct 2018
- 19.Ehlert K, Naude AM. Infection prevention and control measures currently applied in South African audiology. S Afr J Commun Disord. 2014;61(1):1–10. doi: 10.4102/sajcd.v61i1.55. [DOI] [PubMed] [Google Scholar]
- 20.Amlani AM. Current trends and future needs for practices in audiologic infection control. J Am Acad Audiol. 1999;10(3):151–159. doi: 10.1055/s-0042-1748474. [DOI] [Google Scholar]
- 21.Swaminathan S, Prasad J, Dhariwal AC, Guleria R, Misra MC, Malhotra R, Mathur P, Walia K, Gupta S, Sharma A, Ohri V, Jain S, Gupta N, Laserson K, Malpiedi P, Velayudhan A, Park B, Srikantiah P. Strengthening infection prevention and control and systematic surveillance of healthcare associated infections in India. BMJ. 2017;358:59–62. doi: 10.1136/bmj.j3768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Raka L, Mulliqi-osmani G (2011) Infection control in developing world. Infection control—updates, pp 65–78
- 23.Occupational Safety and Health Administration [Internet] (2010). https://www.osha.gov/laws-regs/federalregister/2010-05-06. Cited 8 Apr 2019
- 24.Bankaitis AU (2014) Infection control—what to do and how to do it [Internet]. https://www.audiologyonline.com/articles/infection-control-what-to-do-12953. Cited 26 Sep 2019
- 25.Infectious Diseases SER Background Stetement [Internet] (2012). https://www.osha.gov/dsg/id/OSHA-2010-0003-0239.pdf. Cited 26 Sep 2019
- 26.Handy LK, Maroudi S, Powell M, Nfila B, Moser C, Japa I, et al. The impact of access to immunization information on vaccine acceptance in three countries. PLoS ONE. 2017;12(8):e0180759. doi: 10.1371/journal.pone.0180759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ozisik L, Tanriover MD, Altınel S, Unal S. Vaccinating healthcare workers: level of implementation, barriers and proposal for evidence-based policies in Turkey. Hum Vaccines Immunother. 2017;13(5):1198–1206. doi: 10.1080/21645515.2016.1269992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maltezou H, Poland G. Immunization of health-care providers: necessity and public health policies. Healthcare. 2016;4(3):47. doi: 10.3390/healthcare4030047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Allegranzi B, Pittet D. Role of hand hygiene in healthcare-associated infection prevention. J Hosp Infect. 2009;73(4):305–315. doi: 10.1016/j.jhin.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 30.Camacho L (2012) Infection control: best clinical practices [Internet]. https://www.audiologyonline.com/articles/infection-control-best-clinical-practices-6926. Cited 23 Mar 2019
- 31.Bankaitis AU. Hearing aids: Lick’em and Stick’em. Audiol Today. 2005;17(6):2–3. [Google Scholar]
- 32.Dang A, Likhar N, Alok U. Importance of economic evaluation in health care: an Indian perspective. Value Health Reg Issues. 2016;9:78–83. doi: 10.1016/j.vhri.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 33.Cohen MR, Mccollough TD. Infection control protocols for audiologists. Am J Audiol. 1996;5(1):20–22. doi: 10.1044/1059-0889.0501.20. [DOI] [Google Scholar]
- 34.The South African Speech-Language-Hearing Association Ethics and Standards Committee (2017) Practice guidelines for audiologists and speech-language therapists in early communication intervention [Internet]. https://www.saslha.co.za/Content/Documents/Guidelines_for_Early_Communication_Intervention_2017.pdf. Cited 26 Sep 2019
- 35.Avila-Aguero ML, German G, Paris MM, Herrera JF. Toys in a pediatric hospital: are they a bacterial source? Am J Infect Control. 2004;32(5):287–290. doi: 10.1016/j.ajic.2003.10.018. [DOI] [PubMed] [Google Scholar]
- 36.Merriman E, Corwin P, Ikram R. Toys are a potential source of cross-infection in general practitioners’ waiting rooms. Br J Gen Pract. 2002;52(475):138–140. [PMC free article] [PubMed] [Google Scholar]
- 37.Sanju HK, Choudhury M, Kumar A (2017) The status of audiology in India [Internet]. https://hearinghealthmatters.org/hearinginternational/2017/status-audiology-india/. Cited 25 Sep 2019
- 38.Leas BF, Sullivan N, Han JH, Pegues DA, Kaczmarek JL, Umscheid CA (2015) Environmental cleaning for the prevention of healthcare-associated infections [Internet]. https://www.ncbi.nlm.nih.gov/books/NBK311016/. Cited 25 Sep 2019 [PubMed]