Abstract
Objective
The study aimed to determine the clinical manifestations and epidemiology of extrapulmonary tuberculosis (EPTB) of the head and neck in the otorhinolaryngeal regions. There is an increase in the incidence of EPTB in recent years because of increase in immunocompromised states and development of resistant bacteria. The clinical symptoms and signs of EPTB of the otorhinolaryngeal regions overlap with that of malignancies and other diseases in otorhinolaryngology thereby requiring correct early diagnosis so as to avoid unnecessary surgeries and procedures with initiation of appropriate anti tuberculous treatment under RNTCP.
Study design
Our prospective study was done on 45 patients who attended the ENT OPD at a tertiary care centre in Southern India over a period of 18 months with diagnosed EPTB of the otorhinolaryngeal regions.
Results
The study included 29 (64.4%) patients who presented with cervical lymphadenopathy, 11 (24.4%) patients with tuberculous laryngitis, 3 (6.6%) patients with tuberculous otitis media and 1 each with nasal and oral cavity tuberculosis. In our study 6 (13.3%) patients had co-existing pulmonary tuberculosis, 8 (18%) had diabetes, 5 (11%) had past history of tuberculosis and 7 (16%) had contact with patient with tuberculosis.
Conclusion
A high index of suspicion of EPTB must be kept among patients where (i) the clinical symptoms are out of proportion to the signs, (ii) common treatment fails or (iii) there is persistence or recurrence of symptoms despite therapy. The challenge is in confirming diagnosis which requires histopathological examination (HPE) of the tissue specimen. The timely diagnosis and initiation of anti tuberculous treatment (ATT) as per RNTCP helps in complete recovery thereby reducing morbidity.
Keywords: Extrapulmonary tuberculosis (EPTB), Tuberculous lymphadenopathy, Tuberculous laryngitis, Tuberculous otitis media, Anti tuberculous treatment (ATT)
Introduction
India is the country with highest burden of tuberculosis (TB) and accounts for one fourth of the global tuberculosis burden. The WHO statistics for 2015 gives an estimated incidence of 2.8 million cases of tuberculosis in India out of global incidence of 10.4 million [1]. Tuberculosis (TB) is a chronic granulomatous, infectious and communicable disease caused by Mycobacterium tuberculosis. Tuberculosis affecting other sites—known as extra pulmonary tuberculosis (EPTB) is rarely smear positive. It is generally accepted that the contagious potential of this form is negligible and has therefore never been a priority in the campaigns undertaken by National tuberculosis control programs [2]. The percentage of patients with EPTB (extrapulmonary tuberculosis)in tertiary care hospitals in India is between 30 and 53% while the percentage estimated by national control program in India for HIV negative adults is 15–20% [3]. The Indian branch of Advocacy to Control TB Internationally (ACTION) says the country’s TB control program is failing to take sufficient action to diagnose cases of EPTB [4]. Tertiary care centre’s appear to be an excellent place for medical education & operational research in this regard. This is much needed as HIV-TB co-infection; MDR TB & EPTB continue to be major public health threats.
Tuberculosis of the otorhinolaryngeal region is an uncommon, but not rare, clinical problem. Most physicians do not consider TB in the differential diagnosis of various otorhinolaryngeal symptoms, resulting in misdiagnosis and improper treatment. Symptoms and signs of tuberculosis of this region can mimic malignancy, and; hence, an early diagnosis is essential. With this background a study to know the basic demographics, clinical presentation, diagnostic evaluation & treatment response of extrapulmonary TB in the otorhinolaryngeal regions is felt necessary.
Aim
To determine the clinical presentations & epidemiology of extra pulmonary tuberculosis of head and neck in otorhinolaryngeal areas with assessment of treatment response at 3 months & 6 months after initiation of anti tuberculous treatment (ATT).
Materials and Methods
This study is a prospective study conducted at the Department of ENT, Government Medical College Kozhikode; a tertiary care hospital in Northern Kerala, for a period of 18 months from 01 Jun 2016 to 30 Nov 2017. All patients diagnosed as new cases of extrapulmonary tuberculosis of head & neck region with or without pulmonary tuberculosis who presented to Department of ENT, Govt. Medical College, Kozhikode were included in the study. The patients with FNAC or histopathological examination confirming tuberculosis alone were taken as new cases of extrapulmonary tuberculosis in this study. However patients with relapse or those lost to follow up were excluded from the study.
A complete history including presenting complaints, past history of tuberculosis, co-existing or contact with active pulmonary tuberculosis and any other co-morbidity was obtained. This was followed with clinical examination and relevant investigations including Chest X-ray, sputum AFB, HIV status, diabetic status, tuberculin test, FNAC, histopathological examination and specific investigations; inclusive of otoendoscopy, videolaryngoscopy, pure tone audiometry & diagnostic nasal endoscopy as and when required. After having made the diagnosis the treatment with ATT was given & post treatment outcome was assessed at 3 months and 6 months respectively. The treatment response was assessed clinically in terms of symptomatic improvement and improvement of observed clinical signs.
Results
A total of 45 patients were diagnosed with extrapulmonary tuberculosis of the otorhinolaryngeal regions in our institute during the study period. The study group included patients in the age range of 14–86 years. 34% of patients belonged to the age group of 21–40 years and 31% in the age group of 41–60 years. Of the patients 27 (58%) were males and 18 (42%) were females. Our study included 29 (64.4%) patients who presented with neck swelling, 11 (24.4%) patients with hoarseness of voice, 3 (6.6%)patients with otorrhoea and reduced hearing and 2 (4.4%) others. Among the 2 others, one patient had an ulcer over left side of columella of nose and other one had a growth over dorsum of tongue (Table 1). In our study 6 (13.3%) patients had co-existing pulmonary tuberculosis, 8 (18%) had diabetes, 5 (11%) had past history of tuberculosis and 7 (16%) had contact with patient with tuberculosis.
Table 1.
Age and Sex distribution among the diagnosed cases of EPTB
| Clinical presentation | 0–20 years | 21–40 years | 41–60 years | 61–80 years | > 80 years | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| F | M | F | M | F | M | F | M | F | M | |
| Neck swelling | 2 | 3 | 6 | 6 | 4 | 3 | 0 | 4 | 1 | 0 |
| Otorrhoea | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Hoarseness | 0 | 0 | 0 | 1 | 0 | 5 | 1 | 4 | 0 | 0 |
| Growth over dosrum of tongue | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Ulcer left side of columella | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
Tuberculous Lymphadenopathy
The commonest extrapulmonary tuberculosis manifestation in the otorhinolaryngeal region as seen in our study was tuberculous cervical lymphadenopathy accounting for 29 (64.4%) of the cases. There were 16 males and 13 females. The commonest age group affected was between the second and sixth decade of life. They presented with complaint of neck swelling predominantly involving the neck nodes in the anterior triangle level 3, 4. There were multiple lymph nodes involved in 4 patients. In 11 cases (38%) the posterior triangle lymph nodes were involved. (Fig. 1) 2 patients with past history of tuberculosis, 6 patients with history of tuberculous contact and 5 patients with diabetes mellitus presented with tuberculous lymphadenopathy. FNAC was found to be confirmatory in 27 (93%) patients with cervical lymphadenitis. 2 (7%) patients required lymph node biopsy for confirmation. The size of neck swelling decreased in all 29 patients who presented with tubercular cervical lymphadenitis at 3 months of starting ATT with complete resolution by 6 months.
Fig. 1.
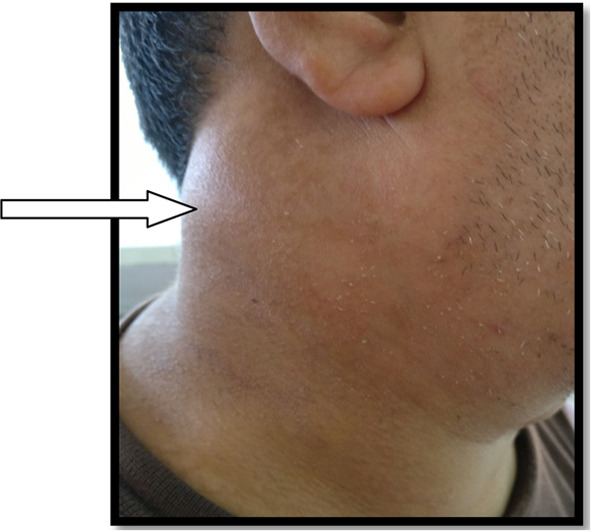
Cervical lymphadenopathy with involvement of the lymph nodes in posterior triangle of neck
Tuberculous Laryngitis
There were 11 (24.4%) cases of tuberculous laryngitis. All cases were above 40 years of age and mostly male patients except for one female patient. The predominant presenting complaint was hoarseness of voice. The 6 patients in our study with pulmonary tuberculosis had hoarseness of voice and were found to be sputum positive. Among patients with laryngitis; two of them had past history of tuberculosis and one had a history of tuberculous contact. The indirect laryngoscopy revealed involvement of posterior part of the glottis which was confirmed with videolaryngoscopy (Fig. 2) and only one patient had involvement of the anterior part of the glottis. A direct laryngoscopy was done to confirm diagnosis and rule out malignancy. There was no evidence of any mass or vocal cord palsy in any of our patients. Histopathological examination of the specimen confirmed diagnosis. Category I ATT was started as per RNTCP guidelines and patients were followed up. VLS findings disappeared in 7 (64%) of patients who presented with hoarseness at 3 months after starting treatment and in 4 of the remaining patients at 6 months. Most of the patients regained their normal voice; one patient had persistent hoarseness even after successful completion of treatment.
Fig. 2.
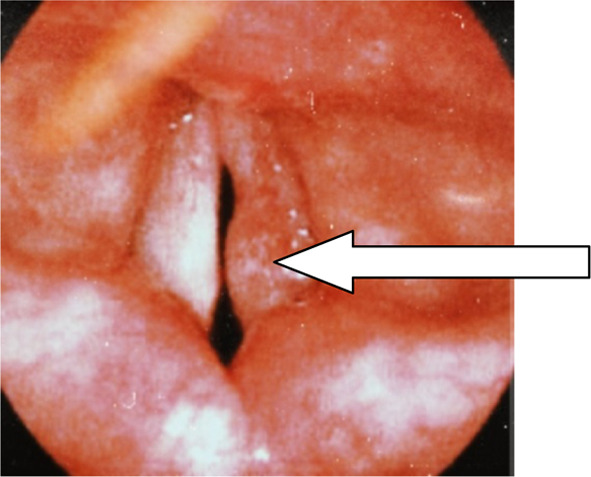
Videolaryngoscopy in a patient with tuberculous laryngitis showing Rt Vocal cord involvement affecting the posterior 2/3rd mainly
Tuberculous Otitis Media
There were 3 cases of tuberculous otitis media. It included 2 females and 1 male patient with all below 25 years of age. Ear discharge was the chief presenting complaint in all cases. There were other complaints like hearing loss and ear ache. Tympanic membrane perforation was present in only one patient. There were pale granulations on the tympanic membrane in the other two cases. None of our patients had facial palsy or other complications. Pure tone audiometry revealed pure conductive loss of 40 dB in two patients with mixed hearing loss in the patient with perforation. All patients had unilateral symptoms and signs. One case also had past history of pulmonary tuberculosis and was treated for same. The biopsy from the granulations removed revealed the diagnosis of TB. Patients were started on category I ATT with improvement in symptoms. However the audiometry remained abnormal in 1 patient who was found to have mixed hearing loss even at 6 months after starting treatment.
Nasal Tuberculosis
There was one case of nasal TB during the period of review. Patient was a 50 year old female who presented to us with a lesion over the nose not responding to treatment and was referred from dermatology department. This patient was on medications for depression and on follow up at psychiatry department. The examination revealed an ulcer on the columella left side with occasional discharge (Fig. 3). The excision biopsy revealed tuberculosis. The patient was started on category I ATT and improvement noted within 4 months of initiation of the treatment.
Fig. 3.

Nasal Tuberculosis—patient presented with ulcer over the left side of the columella
Tuberculosis of Oral Cavity
We had one case of tuberculosis of the oral cavity wherein a 58 year old female patient presented with a lesion noted over the dorsum of tongue on the left side which was increasing in size with irritation on eating. The examination revealed an exophytic lesion over dorsum of tongue with papillae, friable and non tender. The biopsy was done which revealed the diagnosis of tuberculosis. The patient was started on ATT category I and improvement noted at 5 months after initiation of treatment.
The assessment of treatment of the patients with EPTB at 3 and 6 months respectively is as shown in Table 2. The early diagnosis with initiation of treatment with ATT is the basis for recovery from this condition.
Table 2.
Assessment of response to treatment with ATT at 3 and 6 months
| Response to treatment with ATT | TB lymphadenopathy (Total 29 patients) | TB Laryngitis (Total 11 patients) | Tuberculous otitis media (Total 3 patients) | Nasal tuberculosis (1 patient) | Tuberculosis of Oral cavity (1 patient) |
|---|---|---|---|---|---|
| At 3 months | Improvement noted clinically in all 29 patients with decrease in the size of the swelling neck | 7 patients showed improvement both clinically and with VLS findings | 2 patients with conductive hearing loss showed clinical improvement but audiometry showed conductive hearing loss with decrease in AB gap compared to that before treatment. The PTA was normal at 6 months | ||
| At 6 months | Complete resolution in all 29 patients | 4 patients had significant clinical improvement only after 5 months of treatment | 1 patient with mixed hearing loss had improvement in hearing by 5 months but audiometry showed Moderate hearing loss with sensorineural component. The perforation had healed with scarring | Improvement was noted at 4 months of therapy with complete resolution by 6 months | Improvement was noted by 5 months of therapy with complete resolution by 6 months |
| Special features that require mention and due consideration in further studies | However even after resolution of the lesion 1 patient had a change in voice persistent despite therapy | Though clinically patients improved, the improvement in hearing on audiometry was delayed with 1 patient having mixed loss continuing to have abnormal PTA even after 6 months |
Discussion
Tuberculosis affecting the otorhinolaryngeal regions though rare is not uncommon. It is commonly grouped under the non-classified & rare forms of extrapulmonary tuberculosis. One of the reasons for the incorrect estimation of the epidemiology of extrapulmonary tuberculosis (EPTB) is a difference in terminology. Some authors consider extrapulmonary tuberculosis as tuberculosis of any organ, excluding exactly bronchopulmonary lesions whereas others think that the division of the lung and their covering pleura into two separate organs is incorrect and ascribe both organs to pulmonary tuberculosis, and instead of extrapulmonary tuberculosis use the terms extrathoracic tuberculosis (ETTB) or extrarespiratory tuberculosis, which merge the tuberculosis of all organs except thoracic ones [5]. Solovic and colleagues reported that the percentage of extrapulmonary tuberculosis cases among tuberculosis in the EU ranged from 4 to 48%. This difference might be explained by differences in risk factors for extrapulmonary tuberculosis or challenges in diagnosis [6]. Mazza Stalder and colleagues considered that the share of EPTB was increasing; at 20–40%. In 1984 EPTB was a major health problem in Australia, where 24.3% of all new TB notifications were extrapulmonary in origin [7]. The commonest sites of disease were the lymph nodes, urogenital tract, pleura and bone. As most of the patients primarily manifest with pulmonary tuberculosis and receive treatment, it’s only those patients who develop symptoms early or have the symptoms affecting ear, nose and throat without involvement of the lungs that report to the ENT OPD. This could be the reason for the reduced number of cases seen primarily in the ENT OPD as reflected in our study too.
The extrapulmonary tuberculosis of the otorhinolaryngeal regions as in our study is found to affect predominantly individuals in their third-fourth decade of life except for patients presenting with laryngeal tuberculosis. This is mainly because the clinical presentation can mimic a laryngeal malignancy. The male preponderance in our study is similar with results of other studies done in India [8] but contrary to the findings of Mazza Stadler et al. [6] The developed countries with a low disease load have a difference in the demographic profile as noted. The male female ratio obtained in our study is comparable to a study conducted by Antoni Bruzgielewicz et al. [9] which had a male female ratio of 1.43.
The clinical presentation of EPTB affecting the otorhinolaryngeal regions as noted in our study is comparable with a study conducted by Masahiro Oishi et al. [10] in which they studied 47 patients over a period of 10 years and found that 63.8% were cervical lymphadenitis, 25.5% were laryngeal tuberculosis and 4.3% involved middle ear. On analysing the symptoms, all patients had gradual onset and progressive symptoms and average duration was found to be < 6 months in 84.4%. The duration of symptoms in our study is comparable with a study conducted by Pang et al. [11] in which they studied 60 patients over a period of 11 years and found that average duration of symptoms is 4 months. 13.3% had co existing pulmonary tuberculosis, 11% had past history of tuberculosis, and 16% gave history of contact with tuberculosis. 18% of patients were found to have diabetes mellitus. In the study conducted by Antoni Bruzgielewicz et al. [9] 12% of patients gave a history of contact with tuberculosis and 35.6% had chest X ray features suggestive of co existing pulmonary tuberculosis. In another study conducted by Kamath Pandurang et al. [12] 12.8% of patients had HIV infection and 33% had co existing pulmonary tuberculosis. Our study had 6 (13.3%) patients with co-existing pulmonary tuberculosis, 8 (18%) with diabetes, 5 (11%) with past history of tuberculosis and 7 (16%) with history of contact with patient having tuberculosis. No other causes of immunosuppression were found in our study group. It is imperative therefore to follow up patients with pulmonary tuberculosis enabling early diagnosis of EPTB.
Cervical lymphadenopathy the common clinical presentation of EPTB in the otorhinolaryngeal regions; is known to affect the posterior triangle lymphnodes, upper deep cervical group of lymphnodes and the submandibular lymphnodes. The etiology is the dissemination via the blood stream, of bacillary pulmonary foci or from the bacilli gaining entrance via the tonsils, dental or pharyngeal foci. However, any lymph node may be affected. This most prevalent form of TB in the head and neck region presents itself insidiously with a gradual increase in the lymph node and evolution to caseification [13]. No gender difference was found among those suffering from TB in cervical lymph nodes. However, what was verified is that there was greater prevalence in the 35–44 years old age group [14]. The diagnosis was confirmed by USG neck and FNAC neck node. It has been suggested by Chakravorty et al. [8] that the paucibacillary nature of tissue other than sputum compromises the diagnosis rate in TB. In cases where FNAC is inconclusive a biopsy is necessary to confirm diagnosis.
Larynx is one of the organs that can be secondarily affected by TB although in some cases laryngeal TB (LTB) maybe the primary involvement. Tuberculous laryngitis commonly presents as dysphonia, aphonia or pain. There are two theories that attempt to explain its pathogenesis: bronchogenic theory, which is the most accepted, says bronchogenic secretions are responsible for contaminating the larynx through the direct contact of the secretions with the laryngeal mucosa; and hematogenous theory, which says that Mycobacterium tuberculosis reaches the blood and lymph vessels and thus affects the larynx, it being possible for there not to be any pulmonary damage. This is as per reports in literature wherein it has been reported that 1% of cases of PTB have LTB and 100% of cases of LTB have PTB [15]. In our study of the 11 patients with laryngeal TB (LTB); 6 (54.5%) had pulmonary TB (PTB), 2 patients had a past history of TB and 1 patient had history of tuberculosis contact. The most commonly affected site is the region of the vocal folds; the posterior third, followed by the vestibular folds and may involve the epiglottis, the aryepiglottic fold, the arytenoids, the posterior commissure and the subglottis. Indirect laryngoscopy and videolaryngoscopy(VLS) may assist in diagnosis but a direct laryngoscopy is a mandatory investigation of choice to confirm the diagnosis, exclude malignancy and obtain the tissue for HPE.
Tuberculous otitis media (TBOM) is one of the rare clinical presentations of EPTB of head and neck regions. Several theories attempt to explain the infection of the middle ear by TB, but its pathogenesis still remains controversial. It is suggested that routes may be through the bloodstream, by direct extension, from the nasopharynx through the Eustachian tube, via the lymphatic system, externally, by perforation of the tympanic membrane; by direct extension from adjacent structures, the central nervous system, congenital infection (via the placenta) or during passage through the birth canal. Classically it is presented as the triad: painless otorrhea, multiple perforations of the tympanic membrane and peripheral facial palsy; but currently its presentation has become polymorphic. Though the classical description of TBOM has been multiple tympanic membrane perforations in a patient with painless ear discharge and disproportionate sensorineural hearing loss, various studies have reported a whole range of ear findings and different types and severity of hearing loss [16]. In our study all the patients presented with otorrhea and reduced hearing of which one patient had perforation in the tympanic membrane and the other two had granulations in the external auditory canal. The Pure tone audiogram revealed unilateral involvement with moderate conductive hearing loss in two patients and a mixed hearing loss in one patient respectively. The presence of clinical signs disproportionate to the symptoms in any patient with ear complaints must arouse a high index of suspicion of tuberculosis. None of our patients had any complications but among its complications mentioned are the following: peripheral facial paralysis, retro-auricular fistula, labyrinthitis, meningitis, tuberculous osteomyelitis of the petrous pyramid, subperiosteal, cerebral or cerebellar abscess, acute mastoiditis and cellulitis. The diagnosis in these patients is a challenge and HPE of the diseased tissue from the ear is the gold standard for confirming diagnosis. Detection rates of AFB has been reported to be in the order of 5–35% which at best can get to 50% with repeated testing [17]. ATT without surgery can effectively cure TBOM; with surgery required seldom to either deal with complications or unresponsiveness or progression of disease despite treatment. However the improvement in hearing was very marginal and unpredictable. This has also been reported by other studies [16, 17].
Nasal Tuberculosis is a very rare presentation even in countries with a high disease load [18]. The mean age in case series by Kim et al. [19] was 31 years. There is a clear preponderance of females in all reported literature though no reasons have been ascribed for it. The most common symptoms include nasal obstruction and nasal discharge. The less common symptoms include nasal discomfort, presence of a mass, epistaxis, crusting, lacrimation, postnasal drip, recurrent polyps and nasal ulcer. However the commonest feature of nasal tuberculosis is septal involvement with perforation resulting in external nasal deformity. A high index of suspicion is the only key especially since there can be varied differential diagnosis [19, 20]. The patient in our study was a 50 year old female with an ulcer over the collumella and lower part of septum (lt) not responding to treatment and hence referred to the ENT OPD. The biopsy revealed nasal TB and it responded to ATT. ATT is reported to be sufficiently effective in providing complete cure in these patients.
Oral TB another rare form represents only 0.5–1% of the total TB infections. It is more frequent in men than in women appearing mainly in the form of ulcerative lesions [21]. The tongue is the most common site of oral TB [22]. The integrity of the oral mucosa, the cleaning action of the saliva, the presence of oral saprophytes and sub mucosal antibodies represent a natural resistance to the invasion of Mycobacterium tuberculosis [22]. Oral trauma, tooth extraction, inflammatory conditions and poor hygiene represent gateways [21]. Carcinomas have been found coexisting in the same site of the lesion in 3% of patients. In approximately 50%, the oral manifestation of TB led to the diagnosis of systemic infection [21].
The otorhinolaryngeal manifestations of extra pulmonary tuberculosis definitely merit increased awareness among the specialists. There is the need of evaluation of patients being seen in ENT OPD with high index of suspicion especially if condition persists, recurs or does not respond to treatment. The early diagnosis and treatment with ATT helps complete resolution of EPTB. It is imperative to be aware of the extrapulmonary manifestations of tuberculosis likely to be seen in ENT practice which could help avoid unnecessary delay in appropriate diagnosis and enable early initiation of ATT which is not only crucial in treatment but also helps avoid unnecessary treatment options. This knowledge is important to help reduce the medical burden in the general population.
Conclusion
Extrapulmonary tuberculosis of head and neck region though not common; is an entity that requires due consideration. It can affect all age groups and is common in 4th–5th decade of life. It can have varied and atypical presentations that may lead to delay in diagnosis. Otorhinolaryngologists should be aware of the diagnostic challenges in these patients so as to avoid wrong diagnosis and delay in treatment. When the clinical signs are out of proportion to the symptoms in any patient presenting to the ENT OPD there is a need to exclude extrapulmonary tuberculosis (EPTB). Carcinoma may co-exist or confuse the diagnosis in many sites with EPTB in head and neck regions therefore HPE is mandatory. Paucibacillary nature of the specimens obtained may lead to negative culture reports; hence histopathology remains the main stay in diagnosis. A high index of suspicion and pathological examination can lead to early diagnosis and prompt treatment. Role of surgery is limited only in obtaining samples for histopathology. The main stay in treatment is by antitubercular (ATT) treatment according to RNTCP guidelines. If compliant, majority of symptoms decrease by 3 months after starting ATT. A multidisciplinary approach with a team of otorhinolaryngologists, surgeons, chest physicians, microbiologists and pathologists is highly recommended for the efficient management of extrapulmonary tuberculosis.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Nittu Thomas, Email: nittu.mary@gmail.com.
Sapna Sreedharan Nambiar, Email: snambiar25@gmail.com.
P. Muraleedharan Nampoothiri, Email: pmnamboothiri@yahoo.com.
References
- 1.World Health Organisation (2016) WHO/HTM/2016.13.Geneva: World Health Organisation. Global tuberculosis report 2016
- 2.World Health Organisation . Tuberculosis programme: framework for effective tuberculosis control. Geneva: WHO; 1994. [Google Scholar]
- 3.Sharma SK, Mohan A. Extrapulmonary tuberculosis. Indian J Med Res. 2004;120:316–353. [PubMed] [Google Scholar]
- 4.Prakasha SR, Suresh G, D’sa IP, Shetty SS, et al. Mapping the pattern and trends of extrapulmonary tuberculosis. J Glob Infect Dis. 2013;5(2):54–59. doi: 10.4103/0974-777X.112277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kulchavenya E. Extrapulmonary tuberculosis: Are statistical reports accurate? Ther Adv Infect Dis. 2014;2(2):61–70. doi: 10.1177/2049936114528173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Solovic I, Jonsson J, Korzeniewska-Kosela M, Chiotan DI, Pace-Asciak A, Slump E, et al. Challenges in diagnosing extrapulmonary tuberculosis in the European Union, 2011. Eurosurveillance. 2013;18:20432. doi: 10.2807/ese.18.12.20432-en. [DOI] [PubMed] [Google Scholar]
- 7.Mazza-Stalder J, Nicod L, Janssens J. Extrapulmonary tuberculosis. Rev Mal Respir. 2012;29:566578. doi: 10.1016/j.rmr.2011.05.021. [DOI] [PubMed] [Google Scholar]
- 8.Chakravorty S, Sen MK, Tyagi JS. Diagnosis of extrapulmonary tuberculosis by smear, culture, and PCR using universal sample processing technology. J Clin Microbiol. 2005;43(9):4357–4362. doi: 10.1128/JCM.43.9.4357-4362.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bruzgielewicz A, Rzepakowska A, Osuch-Wójcikewicz E, Niemczyk K, Chmielewski R. Tuberculosis of the head and neck—epidemiological and clinical presentation. Arch Med Sci. 2014;6:1160–1166. doi: 10.5114/aoms.2013.34637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oishi M, Okamoto S, Teranishi Y, Yokota C, et al. Clinical study of extrapulmonary head and neck tuberculosis: a single-institute 10-year experience. Int Arch Otorhinolaryngol. 2016;20(1):30–33. doi: 10.1055/s-0035-1565011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pang P, Duan W, Liu S, Bai S, Ma Y, Li R, et al. Clinical study of tuberculosis in the head and neck region—11 years’ experience and a review of the literature. Emerg Microbes Infect. 2018;7:1. doi: 10.1038/s41426-017-0008-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pandurang K. Tuberculosis in the head and neck in India: Down but not yet dead. J Mycobac Dis. 2014;4:2. doi: 10.4172/2161-1068.1000148. [DOI] [Google Scholar]
- 13.Sousa RT, Briglia MFS, Lima LCN, Teixeira LM, Marcião AHR, et al. Frequency of otorhinolaryngologies' manifestations in patients with pulmonary tuberculosis. Int Arch Otorhinolaryngol. 2010;14(2):156–162. [Google Scholar]
- 14.Abebe G, Deribew A, Apers L, Abdissa A, Deribie F, Woldemichael K, et al. Tuberculosis lymphadenitis in Southwest Ethiopia: a community based cross-sectional study. BMC Public Health. 2012;12:504. doi: 10.1186/1471-2458-12-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pino Rivero V, Marcos Garcia M, Gonzalez Palomino A, Trinidad Ruiz G, Pardo Romero G, Pimentel Leo JJ, Blasco Huelva A. Laryngeal tuberculosis masquerading as carcinoma. Report of one case and literature review. An Otorrinolaringol Ibero Am. 2005;32(1):47–53. [PubMed] [Google Scholar]
- 16.Abes GT, Abes FL, Jamir JC. The variable clinical presentation of tuberculosis otitis media and the importance of early detection. Otol Neurotol. 2011;32(4):539–543. doi: 10.1097/MAO.0b013e3182117782. [DOI] [PubMed] [Google Scholar]
- 17.Adhikari P. Tuberculous otitis media: a review of literature. Internet J Otorhinolaryngol. 2009;9(1):7. doi: 10.5580/1b78. [DOI] [Google Scholar]
- 18.Levenson MJ, Ingerman M, Grimes C, Robbett WF. Laryngeal tuberculosis: review of twenty cases. Laryngoscope. 1984;94(8):1094–1097. doi: 10.1288/00005537-198408000-00019. [DOI] [PubMed] [Google Scholar]
- 19.Dixit R, Dave L. Primary nasal tuberculosis. Lung India. 2008;25:102–103. doi: 10.4103/0970-2113.44127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim YM, Kim AY, Park YH, Kim DH, Rha KS. Eight cases of nasal tuberculosis. Otolaryngol Head Neck Surg. 2007;137(3):500–504. doi: 10.1016/j.otohns.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 21.Kakisi OK, Kechagia AS, Kakisis IK, Rafailidis PI, Falagas ME. Tuberculosis of the oral cavity: a systematic review. Eur J Oral Sci. 2010;118:103–109. doi: 10.1111/j.1600-0722.2010.00725.x. [DOI] [PubMed] [Google Scholar]
- 22.Assante LR, Barra E, Bocchino ML, Zuccarini G, Ferrara G, Sanduzzi A. Tuberculosis of the tongue in a patient with rheumatoid arthritis treated with methotrexate andadalimumab. Infez Med. 2014;2:144–148. [PubMed] [Google Scholar]


