Abstract
Sino-nasal organized hematoma (OH) is an uncommon, benign condition of the sinuses. It mimics neoplasm in its clinical presentation as well on imaging appearance. Careful evaluation of the clinical history and imaging features is essential to avoid misdiagnosis. We present an interesting case of sino-nasal organizing hematoma in a 26-year-old male patient, masquerading as sino-nasal neoplasm.
Keywords: Sino nasal, Organizing hematoma, Magnetic resonance imaging, Maxillary sinus
Introduction
Sino-nasal organized hematoma is an uncommon, non-neoplastic benign condition of the sinuses. It primarily involves the maxillary sinus and is generally located in the medial antral wall near the sinus ostium, extending into the nasal cavity or orbit through smooth dehiscence of sinus walls. It can be mistaken for sino-nasal neoplasm clinically due to its locally aggressive features. It can result from any cause of sinus haemorrhage with hematoma formation which later organizes through fibrosis and neo-vascularization. [1–3]
Case Report
A 26-year-old man presented with one-year history of recurrent nasal bleeding, right sided nasal obstruction and cheek swelling. He had no antecedent history of trauma or sinus surgery. Also, there was no significant past medical history or anticoagulant drug use. General examination was normal. On nasal endoscopy, a large polypoid pedunculated mass was seen arising from the posteromedial wall of right maxillary sinus, obstructing the nasal cavity. The middle and inferior turbinates and nasal septum were deviated to the left.
Non-contrast Computed tomography (CT) scans of paranasal sinuses showed expansion and heterogeneous opacification of the right maxillary sinus. Patchy hyper-dense areas were seen centrally with peripheral hypo-dense areas (Fig. 1a). The uncinate process was demineralized. Smooth scalloping of the anterior and posterolateral sinus walls was also seen. The nasal septum was deviated towards left (Fig. 1b). Post contrast study showed central frond like enhancement (Fig. 1c).Magnetic resonance (MR) imaging showed a well circumscribed lesion with smooth margins, showing heterogeneous, predominantly hyper intense signal intensity with thin peripheral hypo intense rim on T2 weighted sequence (Fig. 2a) and intermediate signal intensity on T1 weighted sequence (Fig. 2b). The lesion was bulging into the nasal cavity through smooth dehiscence of the naso-antral wall (Fig. 2a). On Post gadolinium T1 fat saturated sequence, the lesion showed nodular enhancement in the central part (Fig. 2c). Mucosal thickening was seen in rest of the sinus cavity (Fig. 2a).
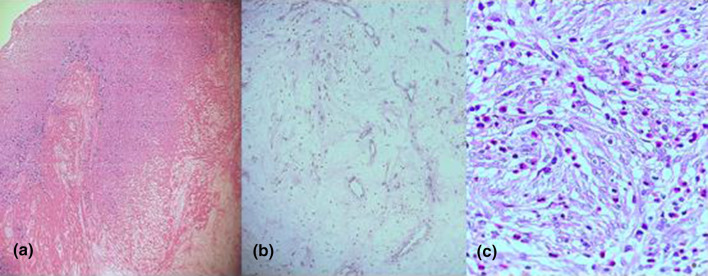
Fig. 1.
a Axial non contrast scan obtained in soft tissue window settings show expansile heterogeneous opacification of the right maxillary sinus bulging into the middle meatus through dehiscence of medial sinus wall. Notice the hypodense mucosal thickening separating lesion from sinus wall (Blue arrow). b Axial contrast enhanced scan obtained in bone window settings shows smooth remodelling of the posterior sinus wall. The spheno-palatine foramen and pterygo-maxillary fissure (white arrow) are normal c Coronal contrast enhanced scan in soft tissue window settings shows nodular enhancement in the centre of the lesion (orange arrow)
Fig. 2.

a Coronal T2 weighted MR image shows a well defined mass centred in the right maxillary sinus showing heterogeneous hyper intense signal intensity with peripheral hypo intense rim(blue arrow). The lesion is surrounded by high signal intensity thickened mucosa. Obstructed secretions are noted in the ethmoid air cells(black arrow). Axial a) Non contrast enhanced T1 image shows intermediate signal intensity with in the lesion b Contrast enhanced T1 FS MR images show central nodular enhancement in the lesion (orange arrow)
On further investigation, no bleeding diathesis was found in the patient.
Patient underwent endoscopic resection of the mass through antrostomy under general anaesthesia. The mass was friable and greyish brown in colour. On microscopic examination, the lesion showed fibrinous matrix with numerous thin walled vascular channels and inflammatory infiltrates composed of lymphocytes, plasma cells and eosinophils (Fig. 3). No lining epithelium was seen. The radiological and histo-pathological findings were consistent with organized hematoma.
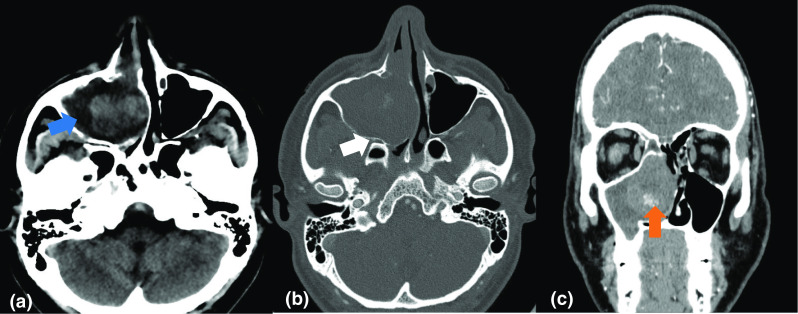
Fig. 3.
Pathological photomicrograph a revealing a lesion consisting of numerous red blood cells mixed with neovascularization and granulation tissue. Low–power field, magnification × 40;Hematoxylin and eosin stain.b Matrix of hyalinised collagen and blood vessels c showing Fibrosis with new vascular endotheliocytes, inflammatory cells and fibrocytes. High-power field, magnification × 200
Discussion
Sino-nasal hematoma was first reported by Ozahn et al. in a patient with von Willebrand disease [4]. Its pathogenesis is not fully understood. Various causes, such as trauma, surgery, bleeding diatheses, underlying hemorrhagic lesion or inflammatory erosion of an arterial wall.
in fungal infections can lead to accumulation of blood in the maxillary sinus. Due to its large size, maxillary sinus is prone to negative pressure which favours accumulation of large amount of blood. Decreased ventilation and poor drainage predispose to the formation of a fibrous capsule which prevents resorption of hematoma and stimulates neo-vascularization. Neovascularization leads to repeated intra-capsular bleed resulting in progressive expansion and bony remodelling / dehiscence of sinus walls. [1, 2, 5, 6]
Recurrent episode of epistaxis is the most common clinical presentation. [1, 6] Other symptoms include cheek swelling and nasal obstruction due to gradual enlargement of the lesion. [7] It affects all age groups ranging from 11 to 78 years and almost twice as common in males as females [4, 7–10]. It occurs in patients with and without a bleeding diathesis.
The CT appearance of sino-nasal OH are non specific. [1, 4, 5, 7] They commonly present as large mass causing expansion of the maxillary sinus with bony erosion and heterogeneous high attenuation on pre-contrast CT scans [2, 6, 9, 11]. Varying degrees of patchy heterogeneous enhancement is usually found within the lesion on contrast enhanced scans [2]. In a clinico-radiological series, MR was found to be superior to CT for determining the margin and extent of the lesion [12]. Due to the higher soft tissue contrast resolution, MR imaging is better in showing internal characteristics of the lesion and differentiating lesion margin from surrounding mucosal inflammatory thickening due to chronic obstruction [10]. Our case demonstrated the classical T2 hypointense peripheral rim sign, first described by Song et al., which corresponded histologically with an attenuated fibrous pseudocapsule [9]. Central frond like/nodular enhancement on both post contrast CT and MRI suggests the neovascularization process associated with the lesion and is similar to description in literature [7, 9, 10].
Radiological differential diagnoses of sino nasal organizing hematoma include mucocele, fungus ball, inflammatory polyp, cholesterol granuloma, inverted papilloma, hemangioma, and carcinoma. [2, 8, 9] Differentiation from mucocele, fungus ball, inflammatory polyp, and cholesterol granuloma can be done by administering contrast as these conditions do not usually enhance. Inverted papilloma primarily involves the nasal cavity and shows the characteristic convoluted cerebriform pattern on T2- or enhanced T1-weighted MR images. [10, 13] Sino nasal hemangioma, especially the cavernous type, is the closest radiological and clinical differential. Some authors have suggested the possible pathologic similarity of haemangioma and sino nasal OH. However, others have refuted the theory based on the difference in the size of vascular channels in these entities. [9] Sino nasal carcinoma are associated with bony destruction and invasion of adjacent structures, in contrast to smooth bony remodelling/erosion of the sinus walls in organizing hematoma. [2]
Treatment Approach
Correct preoperative diagnosis is important for determining the correct surgical approach. Unlike malignant lesions, Sino nasal OH is usually curative with complete surgical resection by minimally invasive surgery (endoscopic sinus surgery or Caldwell-Luc operation) with extremely low recurrence rates. [2, 6, 9]
Conclusions
Sino nasal organizing hematoma can mimic malignant neoplasms due to its locally aggressive behaviour with a tendency to cause bone dehiscence and sino-nasal expansion. Careful evaluation of imaging features can help in correct pre-operative diagnosis. Characteristic findings on CT/MRI such as sino-nasal expansion, smooth bone dehiscence, heterogeneous signal intensity and a peripheral rim of hypo intensity on T2-weighted MR sequence, and nodular or frond like central enhancement on contrast-enhanced CT and MR images, favours the diagnosis of sino-nasal hematoma over other benign and malignant sino nasal neoplasms.
Acknowledgements
We acknowledge the contribution of Dr Naina, Histo-pathologist for giving her clinical inputs into the case.
Declarations
Conflicts of interest
The authors declare that they do not have any conflict of interest.
Ethical Approval
Our institutional review board has given ethical clearance.
Informed Consent
Written informed consent was taken from the patient for publication.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Lee BJ, Park HJ, Heo SC. Organized hematoma of the maxillary sinus. Acta Otolaryngol. 2003;123(7):869–872. doi: 10.1080/00016480310002492. [DOI] [PubMed] [Google Scholar]
- 2.Lee HK, Smoker WR, Lee BJ, Kim SJ, Cho KJ. Organized hematoma of the maxillary sinus: CT findings. AJR Am J Roentgenol. 2007;188(4):W370–W373. doi: 10.2214/AJR.05.1479. [DOI] [PubMed] [Google Scholar]
- 3.Choi SJ, Seo ST, Rha KS, Kim YM. Sinonasal organized hematoma:clinical features of seventeen cases and a systematic review. Laryngoscope. 2015;125:2027–2033. doi: 10.1002/lary.25200. [DOI] [PubMed] [Google Scholar]
- 4.Ozhan S, Arac M, Isik S, et al. Pseudotumor of the maxillary sinus in a patient with von Willebrand's disease. AJR Am J Radiol. 1996;166:950–951. doi: 10.2214/ajr.166.4.8610579. [DOI] [PubMed] [Google Scholar]
- 5.Tabaee A, Kacker A. Hematoma of the maxillary sinus presenting as a mass–a case report and review of literature. Int J Pediatr Otorhinolaryngol. 2002;65:153–157. doi: 10.1016/S0165-5876(02)00148-9. [DOI] [PubMed] [Google Scholar]
- 6.Yoon TM, Kim JH, Cho YB. Three cases of organized hematoma of the maxillary sinus. Eur Arch Otorhinolaryngol. 2006;263:823–826. doi: 10.1007/s00405-006-0064-4. [DOI] [PubMed] [Google Scholar]
- 7.Yagisawa M, Ishitoya J, Tsukuda M. Hematoma-like mass of the maxillary sinus. Acta Otolaryngol. 2006;126:277–281. doi: 10.1080/00016480500316746. [DOI] [PubMed] [Google Scholar]
- 8.Unlu HH, Mutlu C, Ayhan S, et al. Organized hematoma of the maxillary sinus mimicking tumor.Auris Nasus Larynx 2001;28:253–55 [DOI] [PubMed]
- 9.Song HM, Jang YJ, Chung Y-S, et al. Organizing hematoma of the maxillary sinus. Otolaryngol Head Neck Surg. 2007;136:616–620. doi: 10.1016/j.otohns.2006.10.033. [DOI] [PubMed] [Google Scholar]
- 10.Kim EY, Kim HJ, Chung SK, et al. Sinonasal organized hematoma: CT and MR imaging findings. AJNR Am J Neuroradiol. 2008;29(6):1204–1208. doi: 10.3174/ajnr.A1042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nishiguchi T, Nakamura A, Mochizuki K, Tokuhara Y, Yamane H, Inoue Y. Expansile organized maxillary sinus hematoma: MR and CT findings and review of literature. AJNR Am J Neuroradiol. 2007;28(7):1375–1377. doi: 10.3174/ajnr.A0629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ojiri H, Ujita M, Tada S, et al. Potentially distinctive features of sinonasal inverted papilloma on MR imaging. AJR Am J Roentgenol. 2000;175:465–468. doi: 10.2214/ajr.175.2.1750465. [DOI] [PubMed] [Google Scholar]
- 13.Jeon TY, Kim HJ, Chung SK, et al. Sinonasal inverted papilloma: value of convoluted cerebriform pattern on MR imaging. AJNR Am J Neuroradiol. 2008;29(8):1556–1560. doi: 10.3174/ajnr.A1128. [DOI] [PMC free article] [PubMed] [Google Scholar]