Abstract
The efficiency in the management of patients with suspected malignant lesions represents the main objective of the oncology of head and neck. Flexible nasopahyngolaryngoscopy with working channel allows to quickly and safely assess and obtain histological samples of this type of lesion. Our objective is to describe the usefulness of this technique in lesions suggestive of malignancy in terms of efficiency, sensitivity and specificity. A retrospective study was carried out over a period of time from December 2014 to December 2019, including patients biopsied with flexible fibroscopy of lesions of debut suspected of malignancy. Here we assess the location of the lesion, the histological results, the diagnostic time and the epidemiological variables. 104 patients were included in the study. More than half of the lesions, 55.2% (57), were located in the larynx; 57.7% (60) resulted positive for malignancy in the flexible fiberscope biopsy; 19.2% (20) were taken to the operating room to get biopsied under general anesthesia resulting in 7.4% (14) positive for malignancy, which shows a sensitivity of the test of 81%. In our sample, a diagnostic time of 15 days was obtained. Considering our results, the few complications and the revised literature, flexible fiberscope biopsy with working channel is an efficient procedure for the management of oncological patients of head and neck.
Keywords: Flexible endoscopic biopsy, Local anesthesia, Head and neck neoplasms, Diagnostic time
Introduction
Spain is one of the countries with the highest incidence of head and neck cancer in the world so that in 2018 around 3600 patients died. It’s estimated 12.000 new cases in 2020 [1]. Which is the seventh most common cause worldwide with a predominant male involvement (3–1) and a usual age of presentation between 50 and 60 years. In particular, cancer at the laryngeal level represents the area with the highest incidence worldwide of 2.3 cases per 100,000 inhabitants/year [2].
In recent years, health expenditure in Spain has been reduced as a result of crisis and post-economic crisis. In particular, in interventionist matters, there is a trend towards outpatient treatment of diagnostic and therapeutic procedures, with the aim of saving money for the system. In our specialty, one such procedure is the flexible fiberscope biopsy that allows diagnosing lesions suspected of malignancy in a rapid, non-invasive and reproducible way. Numerous studies describe the few complications, the ability to reproduce and the advantages in terms of cost-effectiveness [3, 4]. Therefore, this not only represents an improvement in the economic aspect, but also in clinical and prognostic ones, by reducing the time of diagnosis and, consequently, the time of initiation of treatment, crucial in any oncological pathology.
Traditionally, until the introduction of advances in medical technology, biopsies of pharyngeal or laryngeal lesions were performed by indirect laryngoscopy or direct laryngoscopy under general anesthesia. The introduction of the direct pharyngoscopy-laryngoscopy with flexible fiberscope with working channels allowed a correct exploration and visualization of suspicious lesions, obtaining a sample of the lesion more effectively, which will then be histologically analyzed for differential diagnosis [5].
Our objective in this paper is to define the diagnostic usefulness of biopsy by flexible fibroscopy in lesions suspected of malignancy, and also describe the anatomical location of these lesions in our hospital, comparing it to the need to perform an intraoperative biopsy under general anesthesia to reach a definitive diagnosis, in terms of efficiency, sensitivity and specificity. Clinical-epidemiological characteristics, tolerance and cost-effectiveness are evaluated to define the usefulness of this procedure in the diagnosis of cancer in the otorhinolaryngology sphere.
Materials and Methods
We carried out a cross-sectional, retrospective, descriptive and observational study of patients attending the Hospital Universitario de Gran Canaria Doctor Negrín (third level hospital), whose healthcare area covers the North of the island of Gran Canaria (341,391 inhabitants). The study was based in those inhabitants presenting lesions suspected of early malignancy in the otorhinolaryngology field. The patients were offered a biopsy with channel fibroscopy for diagnostic confirmation. The analysis is carried out in the period from December 2014 to December 2019. All patients were recorded, examined and biopsied; with prior informed consent, by an otorhinolaryngology service area specialist. The Ethical Research Committee of our hospital accepted the study.
The corresponding clinical histories were reviewed, collecting epidemiological, clinical and surgical variables (Table 1). After the first examination in which the suspected lesion is treated, the patients are referred to a second consultation for the biopsy using channel fibroscopy.
Table 1.
Epidemiological, clinical and surgical variables
| Variables | ||
|---|---|---|
| Epidemiological | Clinical | Surgical |
| Number of clinical history | Lesion location | Surgical biopsy size |
| Consultation year | Biopsy with fiberscope | Pathological and surgical anatomy |
| Patient’s sex | Diagnostic | Surgical location of the Injury |
| Patient’s age | Size of channel fiberscope biopsy | |
| First appointment date | Pathological anatomy of channel fiberscope | |
| Biopsy date | Toxic habits: smoking, drinking alcohol… | |
| Surgery date | Use of antiaggregating or anticoagulant medication | |
| Date the pathological anatomy report was written | Medical background | |
The technique used to perform the biopsy was flexible fibroscopy with working channel. It is done in a consultation that has a stop car, with two otolaryngologists accompanied by specialized nursing staff. The sitting patient is monitored, recording oxygen saturation, blood pressure and heart rate. An Olympus CV-70 Video Processor is used to display images on HDTV and has NBI technology with working channel. We use topical anesthesia applying Xilonibsa (lidocaine) spray for nasal passages and oral cavity and instillations of Lidocaine 200 mg/10 ml through the fiberscope channel. We perform an endoscopic scan for the location of the lesion and proceed to biopsy, being guided by NBI in case it is not visible at the macroscopic level. We maintain a surveillance time of between 15 and 30 min for control of possible immediate complications secondary to the procedure. Lesions with negative or inconclusive results, but still suspicious of malignancy, are derived to biopsy in surgery under general anesthesia.
The statistical analysis was performed with SPSS 20.0 (IBM). The dependent variable will be the positive result for malignancy. Quantitative variables are shown with mean and standard deviation, with 95% confidence intervals. The qualitative variables are shown in percentages. Pearson’s Chi Square was used to check the association of these variables; to compare stockings, we used t for Student; and non-parametric test like the Mann–Whitney’s U to compare medians. For statistical tests an error α 0,05 is established.
Results
A total of 104 patients with suspected malignant lesions were included in the study. The average age is 62.8 years and the sex distribution is predominantly male with a representation of 83.7% (87). 83.7% (87) of them were smokers and 54% (56) used to drink alcohol, and all drinkers were also smokers.
Regarding the distribution by anatomical areas, the region with the highest location of suspicious lesions was the larynx, representing 55.2% (57); followed by nasopharynx, 21% (22); then hypopharynx, 12.4% (13): and, finally, oropharynx, 11.4% (12).
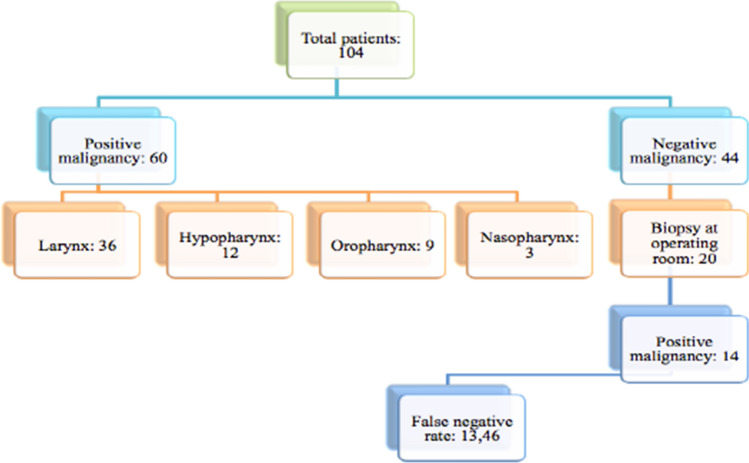
In the anatomical-pathological result of the biopsies, 57.7% (60) were positive and 42.3% (44) were negative for malignancy. 20 of those 44 who had a negative result, had to be taken to the operating room for biopsy under direct laryngoscopy due to the persistence of suspicious lesion, and 14 of them tested positive for malignancy, implying a false-negative rate of 13,46. (Fig. 1).
Fig. 1.
Clinical results
The area distribution of these malignant results was: 60% (36) in the larynx (24 supraglottic, 11 glotic and 1 with subglottic involvement), 20% (12) in the hypopharynx, 15% (9) oropharynx and 5% (3) in nasopharynx.
A total of 91.4% (67) of all malignancy positive patients had a histological sample compatible with epidermoid carcinoma.
These results allow us to obtain a sensitivity of the test of 81% and a specificity of 100%. The positive predictive value is 100% and the negative predictive value is 68.1%. (Table 2).
Table 2.
Contingency table
| Positive biopsy | Negative biopsy | Total | |
|---|---|---|---|
| Carcinoma | 60 | 14 | 74 |
| Non carcinoma | 0 | 30 | 30 |
| Total | 60 | 44 | 104 |
The mean size of the biopsy sample obtained by channel fibroscopy is 0.4 cm. We found no statistically significant relationship between the sample size and the positivity for malignancy [OR 1.26 (IC95% 0.57–2.77)].
The time from the first consultation until we performed the biopsy was 6.5 days on average and the anatomopathological result after the biopsy was 15 days on average.
Discussion
In case of lesions suspected of malignancy, an appropriate management of the patient in the most efficient possible way will allow to obtain good diagnostic results and therapeutic optimization. The strides in medical engineering with the current devices of flexible videoendoscopy with high-definition fiber optic and NBI technology allow very comprehensive and accurate studies of the lesions to be biopsied. The visual analysis of the endoscopic examination must be meticulous and unhurried, always searching for abnormal areas reflected with a change of coloration, abnormal vascular pattern, suspicious appearance of the mucosa or alteration of mobility. As early as 1992, Haughey et al. described the use of routine endoscopy in the protocols for detecting synchronous or metachronic tumors in head and neck neoplasms [6].
Other later studies describe the few or rare complications this technique implies. Wellenstein et al. published in May 2017 a sample of 201 biopsies. They present there the complications derived from these types of procedures organizing them according to the classification of surgical complications of Clavien-Dindo, with 1.99% of complication, describing the presence of a case of laryngospasm, a previous epistaxis, a laryngeal bleeding and a subglottic edema [7]. In our case, we do not register any complications, although some procedures are more laborious than others, technically speaking, mainly related to the location of the lesion, the anatomical characteristics of each patient and the tolerance to the technique.
The most important features of the application of this procedure are the capacity to reproduce and the advantages in terms of cost-effectiveness. The economic impact is always to be considered when making therapeutic decisions, because it is really conditioning. Taking American health system as a referent, both Marcus et al. and Naidu et al. publish very significant economic results, with few complications and with differences up to $6,000 per procedure between taking a canal fiberscope biopsy or direct laryngoscopy under general anesthesia [3, 4].
Taking the National Health System into account, both Castillo Farias et al.and Saga et al. show annual benefits between the comparisons of both techniques [8, 9]. According to our data, we have managed to ensure that 86,5% (90) of patients do not require an operating procedure; thereby contributing to a reduction in health expenditure and avoiding those possible complications of general anesthesia.
The pre-biopsy examination, guided by the patient’s symptoms and sustained by endoscopic vision, confirms the larynx is the first area of suspicious lesions, as described by Wellenstein et al. and Zalvan et al. in their studies [7–10], as well as nasopharynx represents the ENT zone less frequently. The diagnostic confirmation offered by the biopsy shows results that remember to what was found in the literature; more than half of the patients tested positive for malignancy. As we can see in our case study, 57.7% of patients biopsied with channel fibroscopy confirmed the initial diagnostic suspicion of malignancy. Cohen et al.published a percentage of 38.2%, while Saga et al.published a percentage of 65.5% [9–11].
Carrying out a comparative studies in terms of histological results between performing the procedure with channel fiberscope and the “gold standard” test, such as biopsy under general anesthesia, have been the objectives of other authors. In the case of Zalvan et al. the positive results for malignancy were similar in both procedures, finding 54% of malignancies by endoscopy biopsy and 50% by laryngeal microsurgery [10].
If we consider the anatomopathological results after the biopsy, our diagnosed suspicions confirm the organ of the larynx as the first area with malignant lesions; emphasizing supraglottis as the most affected location.
The obtained data show 81% of diagnostic sensitivity of the test, equal to that found in the study of Castillo Farias et al.(81%) and somewhat above those found in the studies of Saga et al.and Cohen et al. which showed 73% and 70.6% respectively [8, 9, 11].
The diagnostic quality of the biopsied tissue has generated a number of false negatives, in some cases due to submucosal location of the sample and this should be taken into account. The persistent suspicion of malignancy, despite a negative histological result, makes us perform the test under general anesthesia using direct laryngoscopy with the idea of deepening the tissue to biopsy and obtaining samples of larger size. In our series there seems to be no statistically significant relationship with the positivity for malignancy and the size of the sample biopsied by channel fiberscope,
The main objectives in the management of the oncology of head and neck are avoiding delays between the appearance of the clinic, the speed in the diagnosis and, therefore, the application of the treatment. Laryngeal neoplasms, especially glottic neoplasms, are usually the first ones to manifest though dysphonia; however, nasopharyngeal, hypopharyngeal, and nasosinusal neoplasms are clinically expressed at more advanced stages. The advantages of being able to perform biopsies with the channel fiberscope on the same day of clinical suspicion, after exploration, offers a progress in the obvious diagnostic time that in our study, resulted in 6,5 days from the time the lesion is seen until the biopsy is obtained and 15 days from the time the lesion is seen until the definitive histological result is obtained. On the other side, Lee et al.offer a diagnostic time of 7.5 days compared to 23 days if the biopsy is performed intraoperatively [12].
Conclusions
Based on our results we see that the larynx continues to represent the area with the highest rate of suspicious lesions and with the highest percentage of positive results for malignancy.
The values obtained in terms of sensitivity and specificity demonstrate the usefulness of biopsy by means of flexible fiberscope, which together with cost-effectiveness, the few complications generated and the revised literature place this procedure in a very efficient test for the diagnosis of suspicious head and neck injuries.
Funding
Not applicable.
Declarations
Conflict of interest
All authors declared that they have no conflict interest.
Statement of Financial Interest
The authors have no financial interest to declare in relation to the content of this article.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sociedad Española de Oncología Médica (SEOM). Las Cifras del Cáncer en España. (2020). Seom.org
- 2.Rettig EM, D’Souza G. Epidemiology of head and neck cancer. Surg Oncol Clin N Am. 2015;24(3):379–396. doi: 10.1016/j.soc.2015.03.001. [DOI] [PubMed] [Google Scholar]
- 3.Naidu H, Noordzij JP, Samim A, et al. Comparison of efficacy, safety, and cost-effectiveness of in-office cup forcep biopsies versus operating room biopsies for laryngopharyngeal tumors. J Voice. 2012;26(5):604–606. doi: 10.1016/j.jvoice.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 4.Marcus S, Timen M, Dion GR, et al. Cost analysis of channeled, distal chip laryngoscope for in-office laryngopharyngeal biopsies. J Voice. 2018 doi: 10.1016/j.jvoice.2018.01.011. [DOI] [PubMed] [Google Scholar]
- 5.Brook CB, Platt MP, Russell K, et al. Time to competency, reliability of flexible transnasal laryngoscopy by training level: a pilot study. Otolaryn Head Neck. 2015;152(5):843–850. doi: 10.1177/0194599815572792. [DOI] [PubMed] [Google Scholar]
- 6.Haughey BH, Arfken CL, Gates GA, Harvey J. Meta-analysis of second malignant tumors in head and neck cancer: the case for an endoscopic screening protocol. Annal Otol Rhinol Laryngol. 1992;101(2):105–112. doi: 10.1177/000348949210100201. [DOI] [PubMed] [Google Scholar]
- 7.Wellenstein DJ, de Witt JK, Schutte HW, et al. Safety of flexible endoscopic biopsy of the pharynx and larynx under topical anesthesia. Eur Arch Otorhinolaryngol. 2017;274(9):3471–3476. doi: 10.1007/s00405-017-4647-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Castillo Farías F, Cobeta I, Souviron R, et al. In-office cup biopsy and laryngeal cytology versus operating room biopsy for the diagnosis of pharyngolaryngeal tumors: efficacy and cost-effectiveness. Head Neck. 2014;37(10):1483–1487. doi: 10.1002/hed.23781. [DOI] [PubMed] [Google Scholar]
- 9.Saga C, Olalde M, Larruskain E, et al. Aplicación de la biopsia por endoscopia flexible en el diagnóstico de la patología tumoral en otorrinolaringología. Acta Otorrinolaringol Esp. 2018;69(1):18–24. doi: 10.1016/j.otorri.2017.04.009. [DOI] [PubMed] [Google Scholar]
- 10.Zalvan CH, Brown DJ, Oiseth SJ, Roark RM. Comparison of trans-nasal laryngoscopic office based biopsy of laryngopharyngeal lesions with traditional operative biopsy. Eur Arch Otorhinolaryngol. 2013;270(9):2509–2513. doi: 10.1007/s00405-013-2507-z. [DOI] [PubMed] [Google Scholar]
- 11.Cohen JT, Benyamini L. transnasal flexible fiberoptic in-office laryngeal biopsies—Our experience with 117 patients with suspicious lesions. Rambam Maimonides Med J. 2014;5(2):e0011. doi: 10.5041/rmmj.10145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee F, Smith KA, Chandarana S, et al. An evaluation of in-office flexible fiber-optic biopsies for laryngopharyngeal lesions. J Otolaryngol Head Neck Surg. 2018 doi: 10.1186/s40463-018-0275-x. [DOI] [PMC free article] [PubMed] [Google Scholar]