Abstract
Haemostasis during any surgical procedure is fundamental for attaining a positive patient outcome. Safe thyroid surgery requires meticulous attention for careful control of bleeding and safe guarding important structures like recurrent laryngeal nerve. Many methods such as ligation and suturing, electro ligation sealing, coagulation, and ultrasonic coagulation have been put to use for achieving haemostasis. The objective of this systemic review was to compare and review the surgical outcomes between harmonic (ultrasonic) scalpel and conventional ligature techniques in performing thyroid surgery. The systematic review was performed in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement and checklist with a total of 11 studies selected for qualitative analysis. The statistical software Review Manager 5.4.1 provided by the Cochrane Collaboration was used for performing the analysis on the two groups. It was concluded that the use of harmonic scalpel for thyroid surgery is useful for reducing operative time, postoperative pain, drainage volume and transient hypocalcemia, hence can be a reliable and a safe tool compared to conventional techniques often used for surgery.
Keywords: Thyroidectomy, Electrocoagulation, Diathermy, Harmonic scalpel, Conventional methods
Introduction
Thyroidectomy is one of the most frequently carried out procedures in head and neck surgery globally. [1, 2]
Thyroid surgery is performed by variety of surgeons ranging from Head & neck surgeon, Endocrine surgeon, Surgical oncologist to General surgeons. Safe thyroid surgery requires meticulous attention to hemostasis and careful control of bleeding while safe guarding important structures like recurrent laryngeal nerb. The thyroid gland has a rich blood supply; prompt hemostasis is crucial to avoid intraoperative bleeding, good visualization of the surgical field to prevent damage to vital structures such as parathyroid glands or laryngeal nerve and to reduce associated post-operative complications. [3]
Hemostasis is a critical factor in determining the frequency of other complications and prolongation of the operative time hence increases the length of hospital stay and costs. [4, 5]
Many methods are currently utilized to maintain surgical hemostasis, such as ligation and suturing (threads, clips, staplers), coagulation (monopolar and bipolar electrocoagulation), ultrasonic coagulation (Ultracision, Harmonic Scalpel®; Ethicon Endo-Surgery, Cincinnati, OH), electro-ligation sealing (LigaSure® Vessel Sealing System; Valleylab, Boulder, CO USA). Electrosurgical devices use heat energy to denature proteins and lateral dispersion of the heat in the surgical field may damage surrounding vital structures. In the recent years research necessitated unraveling new techniques with less thermal spread in an effort reducing intraoperative complications and operative time. Among these instruments we focused our attention on the Harmonic Scalpel® (HS) because this is the oldest and most studied hemostatic device. [2, 6–8].
We did not come across any systematic review or meta-analysis comparing the use of electrocautery and ultrasonic devices; hence we felt the need to perform a systematic review. The objective of this systemic review was to compare surgical outcomes between harmonic scalpel and conventional ligature techniques in performing thyroid surgery.
Methods
This systematic review was performed in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement and checklist [9]. The below mentioned electronic databases were consulted for identification of the primary studies.
Medline (via Pub Med)
Cochrane Library
Embase
For recovery of the primary articles, the search strategy (thyroidectomy OR thyroid surgery) AND (electrocoagulation OR diathermy OR thermocoagulation OR harmonic scalpel OR ultrasonic OR ligation OR conventional methods OR suture techniques) was used. In addition the references of the selected studies and of published reviews were consulted through manual search to select articles that were not included in the electronic searches. The data collected was reviewed separately by all authors.
1191 records were picked from the database out of which 352 articles were screened, of which 315 articles were excluded as they were found out of scope as depicted in the flow chart. Remaining 37 studies were assessed; out of which 11 studies were analyzed since 26 studies did not qualify for further analysis due to improperly randomized.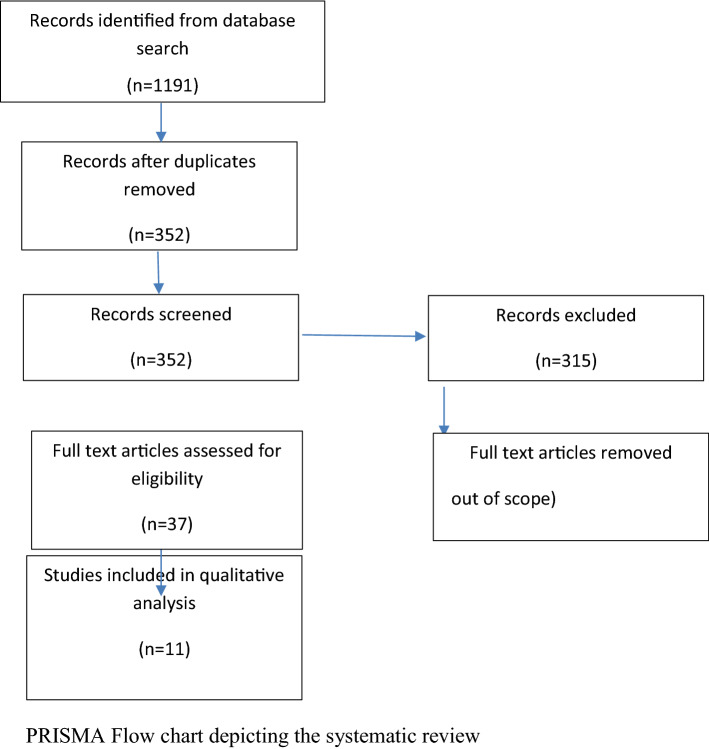
We selected all randomized controlled clinical trials (RCT) comparing use of harmonic scalpel with the conventional ligature technique in patients submitted to thyroidectomy from 2013 to 2020. The studies were selected from the reading of the respective titles and abstracts.
Inclusion Criteria
All Studies included patients aged ≥ 18 years with thyroid gland disease, regardless of the nature of the diagnosis (benign or malignant) that underwent total thyroidectomy.
The intervention group included patients where harmonic scalpel was used while the control group underwent thyroidectomy with conventional ligation.
Exclusion Criteria
Studies using additional procedures or evaluation of ligaSure as surgical technique were excluded.
Parameters analyzed.
The outcomes were based on the following:
Operating time
Intraoperative bleeding volume
Incidences of inferior laryngeal nerve injury (temporary and permanent)
Postoperative hypocalcemia (temporary and permanent)
Post-operative hematoma requiring surgical intervention
The principle meta-analysis compared Harmonic scalpel technique with conventional haemostasis. The statistical software Review Manager 5.4.1 provided by the Cochrane Collaboration was used for performing both analysis.
Mean differences (MD) were used as treatment effect measures for operative times and intraoperative blood loss. Regarding wound complications postoperative hypocalcemia and RLN palsy data were analyzed using Odds Ratio (ORs) with 95% of Confidence Interval (CI). Statistical heterogeneity was tested using χ2 and I2 tests. If heterogeneity was high (I > 50%), the random effects model was performed; otherwise, the fixed-effects model was considered appropriate. Funnel plots were produced to investigate the possibility of publication bias. The selected studies with parameters analyzed are in Table 1
Table 1.
Various studies with analyzed parameters
| Studies | Operat. time | Intrp bld lss | transnt hypocal | Permnt hypocal | Tempry RLN inj | Permnt RLN inj | Postop Haemt | Postop hosp sty |
|---|---|---|---|---|---|---|---|---|
| Yun Fei Duan 2013 | + | + | + | + | + | |||
| Zanghi 2014 | + | + | + | + | + | + | + | |
| Cannizaro 2014 | + | + | + | + | + | + | ||
| Docimo 2015 | + | + | + | + | + | |||
| Karaca 2015 | + | + | + | + | + | + | ||
| Minni 2016 | + | + | + | + | + | |||
| Arslan 2016 | + | + | + | + | + | + | ||
| Aziz 2016 | + | |||||||
| Blanchard 2017 | + | + | + | + | + | + | + | |
| Saim 2018 | + | + | ||||||
| Noori 2018 | + | + | + |
Results
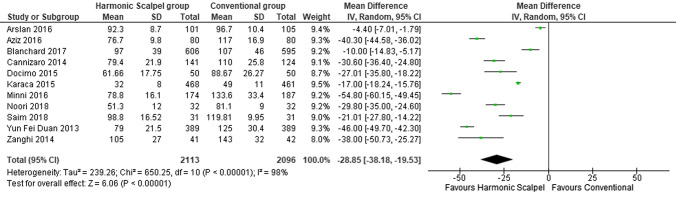
Operating Time (Fig. 1)
Fig. 1.
Forest plot of operative time with Harmonic Scalpel versus conventional haemostasis
Forest plot depicts analysis of operating time differences. The mean reduction in operating time was 28.85 min (95% CI, − 38.18 to − 19.53) resulting from all study estimates.
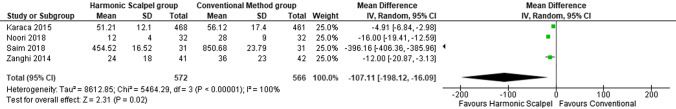
Intraoperative Blood Loss (Fig. 2)
Fig. 2.
Forest plot of intraoperative blood loss with Harmonic Scalpel versus conventional haemostasis
Intraoperative blood loss was reported in 4 studies with mean reduction of 107.11 ml (95% CI, − 198.12 to − 16.09) (Fig. 2), both differences being statistically significant.
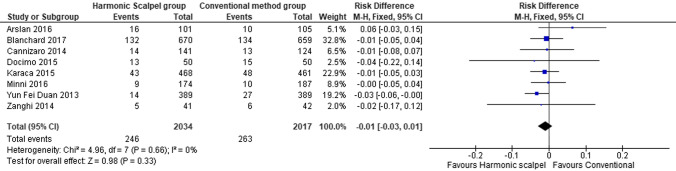
Postoperative Complications (Fig. 3)
Fig. 3.
Forest plot of transient hypocalcaemia with Harmonic Scalpel versus Conventional Haemostasis
8 studies reported transient hypocalcaemia in 246 patients undergoing total thyroidectomy (TT) with harmonic scalpel (HS) while in 263 patients undergone TT with conventional haemostasis (CH). ORs (Odds Ratio) were lower in Harmonic Scalpel group compared to conventional haemostasis (ORs 0.01; 95% CI -0.03 to 0.01) but the difference was statistically not significant (Fig. 3).
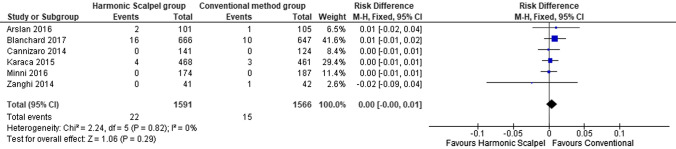
Hypocalcaemia (Fig. 4)
Fig. 4.
Forest plot of permanent hypocalcaemia with Harmonic Scalpel versus Conventional Haemostasis
Permanent hypocalcaemia was reported in 22 patients in HS group and 15 patients in CH group among 8 studies with ORs lower in the HS group (ORs 0.00; 95% CI, -0.00 to 0.01), results were found not to be statistically significant (Fig. 4).
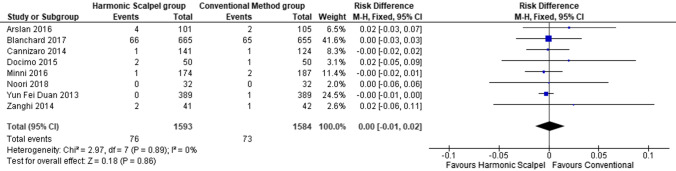
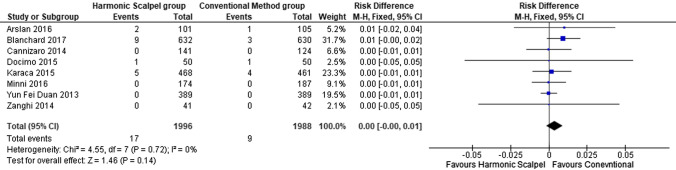
RLN Palsy (Figs. 5 and 6)
Fig. 5.
Forest plot of temporary RLN dysfunction with Harmonic Scalpel versus conventional haemostasis
Fig. 6.
Forest plot of permanent RLN dysfunction with Harmonic Scalpel versus conventional haemostasis
After HS TT, 76 patients experienced transient post-operative RLN palsy and no significant difference was found with CH (ORs 0.00; 95% CI, − 0.01 to 0.02) (Fig. 5). 17 patients reported permanent RLN palsy in the HS group (ORs 0.00; 95% CI, − 0.00 to 0.01), the difference not being statistically significant (Fig. 6).
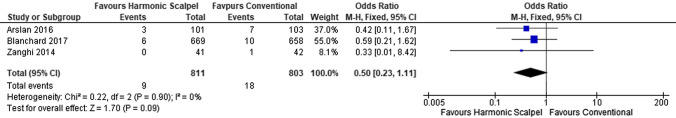
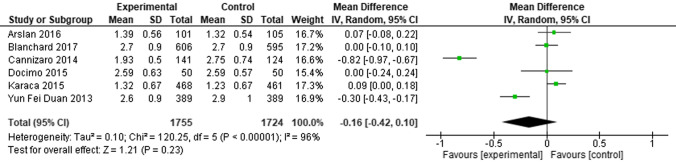
Postoperative Haematoma (Figs. 7 and 8)
Fig. 7.
Forest plot of post-operative hematoma with Harmonic Scalpel versus conventional haemostasis
Fig. 8.
Forest plot of mean post-operative hospital stay with Harmonic Scalpel versus conventional haemostasis
Only 3 studies reported post-operative hematoma, 9 patients in the HS group whereas 18 in the CH group (ORs 0.5; 95% CI, 0.23 to 1.11) but without statistical significance (Fig. 7). Post-operative hospital stay was reported from 6 studies with a statistically significant result favouring the HS group reduction by 0.16 days (95% CI, − 0.42 to 0.10) (Fig. 8).
Discussion
The need for this meta-analysis was felt for appraisal of a new technique with available studies with varying results. This meta-analysis is specifically designed and powered to detect a difference in operative and peri-operative complications and to compare the results of Harmomic scalpel (HS) with conventional hemostasis (CH).
In an attempt to make thyroidectomy safer and more efficient procedure, hemostatic devices were developed with the purpose of achieving adequate hemostasis obviating the need for numerous ligatures which theoretically could save time. One of the most studied is the harmonic scalpel which entails mechanical energy in the form of ultrasonic vibrations (up to 55,000 Hz) that seal blood vessels by breaking the hydrogen and protein bonds of the tissues and vessels and creating endovascular clot [10, 11]. One of the theoretical benefits of using the harmonic scalpel is that it acts at lower temperatures (50–100 °C) resulting in decreased heat transfer to the adjacent tissues, consequently less thermal trauma [10, 11]. Moreover it does not transmit any type of current to the patient [10, 11].
The development of devices such as HS has led to shorter operative time [12]. One explanation for decrease in the surgical time could be due to reduction in time required for the hemostasis of the blood vessels of the thyroid gland whereas experience and expertise of surgeons using these devices could be other reason. The HS combines hemostasis and cutting in a single instrument thus avoiding loss of time when associated with the manipulation with several instruments [12]. The success of thyroid surgery is primarily based on factors, adequate hemostasis to prevent bleeding which could become fatal and to keep the surgical site clean facilitating dissection of tissues while safeguarding vital structures especially recurrent laryngeal nerve and parathyroid glands. Given this premise the results of this review show that there is a statistically significant decrease in intraoperative bleeding volume. However this data didn’t correlate with the reduction of perioperative complications.
It is important to mention the heterogeneity among studies while interpreting the meta-analysis results as certain differences in methodologies may influence the results. The present meta-analysis included 11 studies, all of which were RCTs. Differences in the experience of surgeons and surgical procedures may have affected the surgical outcomes of the thyroid surgery.
Transient hypocalcemia observed after Total thyroidectomy (TT) is believed to be related to traumatization of the parathyroid glands which are intimately related to the thyroid gland sharing its blood supply. We speculate that use of the HS may facilitate dissection of the parathyroid glands in a plane farther away from the parathyroid gland capsule thus reducing the chance of damaging their blood supply, directly or indirectly with either mechanical forces or electrical currents. The incidence of postoperative hypocalcemia was similar in 2 groups by meta-analysis of Cirocchi [6]. There was a reduction in transient hypocalcemia in the meta-analysis of Melck [7] and in permanent hypocalcemia in the meta-analysis of Garas in HS group [8].
The complication of RLN palsy after TT is also an extremely uncommon occurrence. HS has been shown to cause less collateral thermal injury than conventional electrocautery; we would expect to see less Recurrent Laryngeal Nerve Dysfunction (RLND) in the HS group. This meta-analysis showed no significant differences in the RLND. In the previous meta-analysis data about permanent RLN palsy are available only in the analysis of Garas [8] with a higher risk in HS group. It is of fundamental importance using this device judiciously in the vicinity of extremely vital structures such as the RLN [13].
Carlander et al [14] in a recent study showed that HS causes less trauma to adjacent nerve fibers than bipolar electrosurgery, whereas HS may also cause nerve injury at close distances. The potential electrical energy dispersion may cause damage to the surrounding tissue. The temperature of peripheral tissue is dependent upon the distance to the HS blade and the length of time the HS is used. The closer to the activated HS tip and the longer duration of HS use, can result in higher tissue temperature. The tissues are likely to be injured if the temperature increases to a harmful level hence a safety margin to use the HS close to the RLN is required. Jiang et al [15] in their experimental study showed that while activating the HS within 3s, lateral injury of 2 mm tissue thickness occurs and when used close to RLN at setting of level of 3, the activated HS tip should be 2 mm from the nerve and the application duration should be _x0005_ 3 s. Importance of conventional vessel ligation cannot be overemphasized when the hand piece of HS is very close to the RLNs. Permanent nerve injury is a rare complication of TT, this study shows no difference between HS and CH groups in terms of the same.
Patients who underwent HS TT had an earlier pain-free return to normal activity and work. This finding may influence the length of hospital stay and costs; in this meta-analysis there was significant difference with respect to post-operative hospital stay [2].
This meta-analysis has some limitations. A significant heterogeneity across studies for several of pooled analyses was observed. Since clinical and methodological diversity always occur in meta-analysis, a statistical heterogeneity is inevitable [16] and when studies have small sample size or a fewer in number the chi-squared test has low power. On the other hand there are several strengths. First the evidence is based on the meta-analysis of RCTs which is the highest level of evidence (Level I). Secondly a rigorous studies selection with restricted inclusion criteria and a meticulous assessment quality studies are carried out. Furthermore, visual inspection of various forest plots in our study suggests that there is a quite consistency with reference to magnitude and direction of effects.
Conclusion
The results of this meta-analysis showed that HS TT can be a safe, useful and fast alternative to CH TT. The main advantage of this device is that it simplifies the procedure and eliminates the need for clips and suture ligations while also achieving efficient hemostasis. It significantly reduced operative time, blood loss and post-operative hospital stay in HS group compared with the CH. In sutureless open and endoscopic thyroid surgery, the operating space is limited because of the anatomical features of the neck, therefore maintaining a bloodless operating field is essential.
The HS is the device of choice for TT though its inappropriate use may harm surrounding vital structures. In patients undergoing thyroidectomy HS is a reliable and a safe tool. Comparing with CH techniques its use reduces operative time, postoperative pain, drainage volume and transient hypocalcaemia.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Smith RB, Coughlin A. Thyroidectomy hemostasis. Otolaryngol Clin North Am. 2016;49:727–748. doi: 10.1016/j.otc.2016.03.006. [DOI] [PubMed] [Google Scholar]
- 2.Ecker T, Carvalho AL, Choe JH, et al. Hemostasis in thyroid surgery: harmonic scalpel versus other techniques—a meta-analysis. Otolaryngol Head Neck Surg. 2010;143:17–25. doi: 10.1016/j.otohns.2010.03.018. [DOI] [PubMed] [Google Scholar]
- 3.Khafagy A, Abdelnaby I. Total thyroidectomy: ligasure versus clamp & knot technique for intraoperative hemostasis, Egypt. J Ear Nose Throat Allied Sci. 2013;14:59–65. doi: 10.1016/j.ejenta.2013.02.001. [DOI] [Google Scholar]
- 4.Rosato L, Avenia N, Bernante P, De Palma M, Gulino G, Nasi PG, Pelizzo MR, Pezzullo L. Complications of thyroid surgery: analysis of a multicentric study on 14,934 patients operated on in Italy over 5 years. World J Surg. 2004;28:271–276. doi: 10.1007/s00268-003-6903-1. [DOI] [PubMed] [Google Scholar]
- 5.Cannizzaro MA, Bianco SL, Borzì L, Cavallaro A, Buffone A. The use of focus harmonic scalpel compared to conventional haemostasis (knot and tie ligation) for thyroid surgery: a prospective randomized study. Springerplus. 2014;3:639. doi: 10.1186/2193-1801-3-639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cirocchi R, D'Ajello F, Trastulli S, Santoro A, Di Rocco G, Vendettuoli D, Rondelli F, Giannotti D, Sanguinetti A, Minelli L, Redler A, Basoli A, Avenia N. Meta-analysis of thyroidectomy with ultrasonic dissector versus conventional clamp and tie. World J Surg Oncol. 2010;23:8e112. doi: 10.1186/1477-7819-8-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Melck AL, Wiseman SM. Harmonic scalpel compared to conventional hemostasis in thyroid surgery: a meta-analysis of randomized clinical trials. Int J Surg Oncol. 2010;2010:306079. doi: 10.1155/2010/396079.ID396079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Garas G, Okabayashi K, Ashrafian H, Shetty K, Palazzo F, Tolley N, Darzi A, Athanasiou T, Zacharakis E. Which hemostatic device in thyroid surgery? A network meta-analysis of surgical technologies. Thyroid. 2013;23(9):1138–1150. doi: 10.1089/thy.2012.0588. [DOI] [PubMed] [Google Scholar]
- 9.Moher D, Liberati A, Tetzlaff J, Altman DG. The PRISMA group, preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Manouras A, Markogiannakis HE, Kekis PB, Lagoudianakis EE, Fleming B. Novel haemostatic devices in thyroid surgery: electrothermal bipolar vessel sealing system and harmonic scalpel. Expert Rev Med Devices. 2008;5(4):447–466. doi: 10.1586/17434440.5.4.447. [DOI] [PubMed] [Google Scholar]
- 11.Dhepnorrarat RC, Witterick IJ. New technologies in thyroid cancer surgery. Oral Oncol. 2013;49(7):659–664. doi: 10.1016/j.oraloncology.2013.03.445. [DOI] [PubMed] [Google Scholar]
- 12.Pons Y, Gauthier J, Ukkola-Pons E, Clément P, Roguet E, Poncet JL, Conessa C. Comparison of LigaSure vessel sealing system, harmonic scalpel, and conventional hemostasis in total thyroidectomy. Otolaryngol Head Neck Surg. 2009;141(4):496–501. doi: 10.1016/j.otohns.2009.06.745. [DOI] [PubMed] [Google Scholar]
- 13.Ardito G, Revelli L, D'Alatri L, Lerro V, Guidi ML, Ardito F. Revisited anatomy of the recurrent laryngeal nerves. Am J Surg. 2004;187:249–253. doi: 10.1016/j.amjsurg.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 14.Carlander J, Koch C, Brudin L, Nordborg C, Gimm O, Johansson K. Heat production, nerve function, and morphology following nerve close dissection with surgical instruments. World J Surg. 2012;36:1361–1367. doi: 10.1007/s00268-012-1471-x. [DOI] [PubMed] [Google Scholar]
- 15.Jiang Y, Gao B, Zhang X, Zhao J, Chen J, Zhang S, Luo D. Prevention and treatment of recurrent laryngeal nerve injury in thyroid surgery. Int J Clin Exp Med. 2014;7(1):101–107. [PMC free article] [PubMed] [Google Scholar]
- 16.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]