Abstract
Osteitis fibrosa cystica (OFC) is a skeletal disease related to long standing, end-stage hyperparathyroidism. However, nowadays hypercalcemia due to primary or secondary hyperparathyroidism can often be detected early by laboratory screening and imaging modalities; consequentially the frequency of osteitis fibrosa cystica has drastically declined. OFC, also termed as Brown tumor, can mimic primary bone tumors clinically, which often leads to misdiagnosis and inappropriate management. Moreover due to its rarity, it is usually not considered initially in the differential diagnosis of bony tumors. Case presentation: This is the case of a 19-year-old female, who presented with pain over the left ankle region for 3 months. The biochemical screening revealed a picture consistent with primary hyperparathyroidism and the radiologically proven to be left inferior parathyroid adenoma. She underwent excision of the primary parathyroid adenoma, and gradual regression of symptoms was noted postoperatively. Osteitis fibrosa cystica is a rare manifestation of hyperparathtyroidism, which has become a forgotten entity lately due to early identification of hypercalcaemia by modern techniques. A delay in the diagnosis of parathyroid adenoma results in manifestations that can be avoided. The diagnosis of OFC requires a high degree of clinical suspicion. When hypersecretion of PTH is corrected, spontaneous regression of the lesion is expected.
Keywords: Osetitis fibrosa cystica, Brown tumor, Parathyroid adenoma, Hyperparathyroidism, Case report
Background
Primary hyperparathyroidism is characterized by excessive secretion of parathyroid hormone (PTH). This can be due to parathyroid adenoma (~80–85%), parathyroid carcinoma, or hereditary factors [1] The symptoms of the disease include pathological bone fractures, peptic ulcers, kidney stones, and weight loss, which are attributable to the underlying hypercalcemia. Long-standing and end-stage hyperparathyroidism leads to osteitis fibrosa cystica (OFC), also called a Brown tumor. However, due to the advent of highly sensitive laboratory assays and multimodal imaging techniques, hypercalcemia can be picked up in its initial stages without having its full-blown effect, which has reduced the incidence of OFC to less than 2%. It is more common amongst women and between the 5 and 6th decades [2] Due to raised serum PTH levels, there is increased osteoclastic activity, resulting in infiltration by macrophages and fibrovascular tissue deposition. Brown tumors are the foci of these inflammatory areas. These are difficult to distinguish from true malignancy [3] The initial evaluation of a patient with symptomatic primary hyperparathyroidism includes measuring the serum calcium and PTH levels. The etiopathogenesis of OFC is still unclear. It can be a combination of diagnostic delay and low vitamin D/calcium stores. As OFC is rare in younger age groups, we are here presenting a case of 19 years old female suffering from parathyroid adenoma with OFC.
Case Presentation
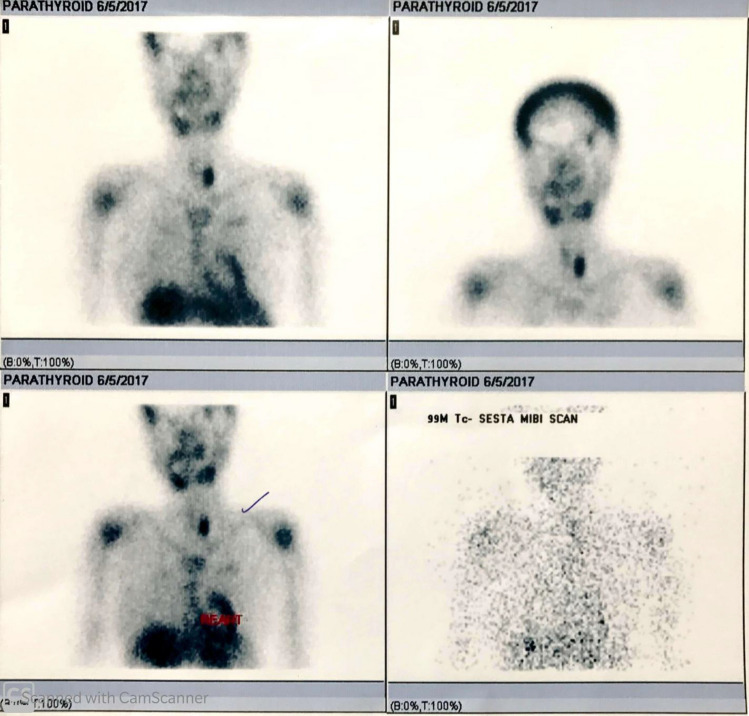
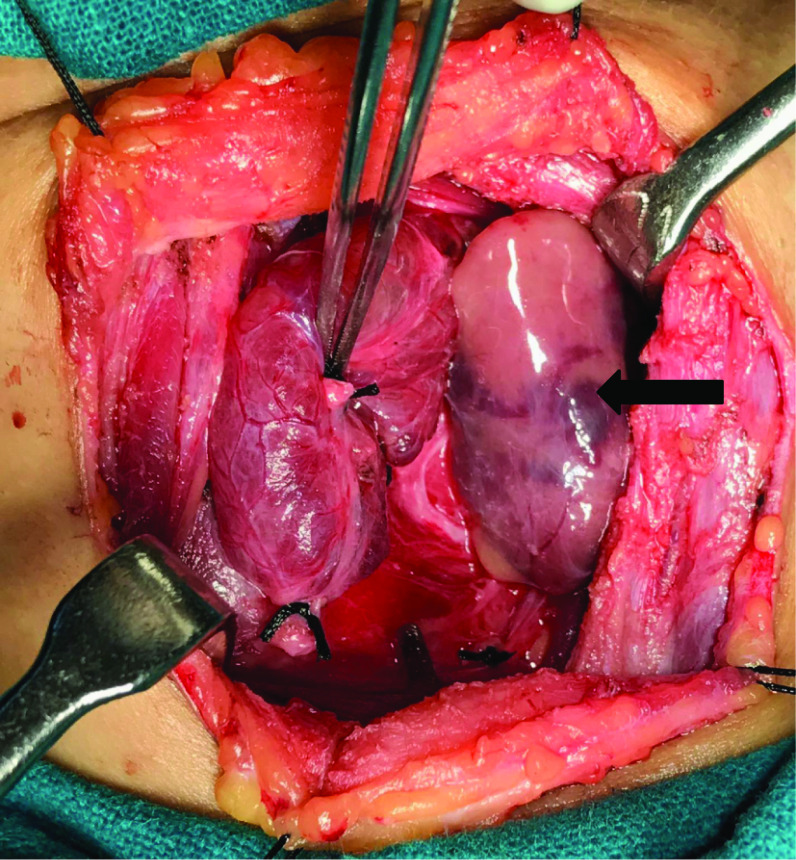
A 19 years old female presented to the orthopedic department with complaints of pain over the left ankle for 3 months. It was insidious in onset, continuous in nature, moderate in intensity, relieved with medication, associated with generalized body aches. There was no history of any other joint pain or swelling, neck swelling, trauma, any other ENT related complaints. Past, personal and family histories were insignificant. Treatment history was unremarkable. General, as well as systemic examinations, were within normal limits. Routine blood investigations of the patient were done, which revealed raised serum calcium (11.8 mg/dl) and PTH levels (967.7 pg/ml). She was then provisionally diagnosed with primary hyperparathyroidism (PHPT) and subsequently transferred to the ENT department for further management. Radiological investigations were done. X-ray of the left leg with the ankle (lateral view) showed lytic lesions at distal ends of tibia and fibula (Fig. 1). X-ray left hand (anteroposterior view) was suggestive of subperiosteal changes along the radial aspect of distal phalanges (Fig. 2). X-ray skull (lateral view) revealed sclerotic areas giving typical "salt and pepper" appearance (Fig. 3). Magnetic Resonance Imaging (MRI) of the left ankle with a leg was suggestive of a well-defined cystic lesion in the distal diaphysis of the tibia (Fig. 4). Ultrasonography of the neck revealed a well defined hypoechoic nodule of size 2.8 X 3.0 cm adjacent to the lower pole of the left thyroid lobe, likely left inferior parathyroid mass. Non-contrast computed tomography (NCCT) scan of the neck revealed a hypodense nodule abutting the lower pole of the left lobe of thyroid. Tc99m-sestamibi scan of the neck showed a hyperactive parathyroid nodule near the inferior pole of left lobe of thyroid (Fig. 5). With the help of clinical findings, hematological and radiological investigations, a diagnosis of left inferior parathyroid adenoma was reached. We did not face any diagnostic challenges throughout. Differential diagnoses for parathyroid adenoma can be metastatic carcinoma, non-Hodgkin's lymphoma, enchondroma, or osteomyelitis. The patient underwent excision of left inferior parathyroid adenoma under general anesthesia (Fig. 6 shows intraoperative findings). The resected specimen was sent for histopathological examination. During the postoperative period, voice was normal. On the second postoperative day, serum calcium level returned to 9.5 mg/dl (within normal limits). However, the patient developed hypocalcemia on the fourth postoperative day and was managed conservatively with oral calcium supplements. PTH level was measured on the second postoperative day which was within normal limits (11.3 pg/ml). Histopathology of the specimen revealed parathyroid adenoma. The patient followed up 2 weeks after the surgery and serum calcium level was measured which was 9.3 mg/dl. PTH level was 19.6 pg/ml. The patient was followed up every month for 6 months and attained complete relief clinically and her biochemically parameters were within normal limits.
Fig. 1.

X-ray left leg with the ankle (lateral view) showing lytic lesions at distal ends of tibia and fibula
Fig. 2.

X-ray left hand (anteroposterior view) suggestive of subperiosteal changes along the radial aspect of distal phalanges
Fig. 3.

X-ray skull (lateral view) showing sclerotic areas giving typical "salt and pepper" appearance
Fig. 4.
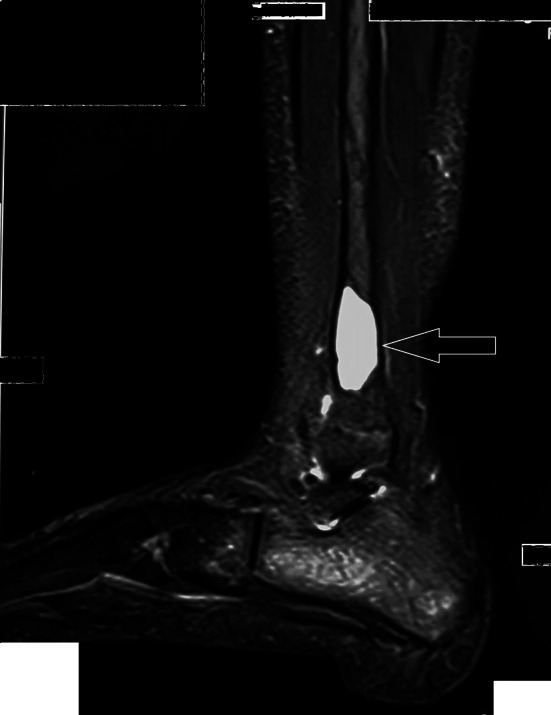
MRI of left ankle with leg suggestive of a well defined cystic lesion in the distal diaphysis of the tibia
Fig. 5.
Tc99m-sestamibi scan of the neck showing hyperactive parathyroid nodule near the inferior pole of the left lobe of the thyroid
Fig. 6.
Intra-operative picture showing left inferior parathyroid adenoma
Discussion
OFC, first described in the nineteenth century, can be regarded as a manifestation of a fully scaled hyperparathyroidism. It typically presents with "pain in bones, renal stones, abdominal groans and psychic overtones."[2] The serum calcium, PTH levels, and serum alkaline phosphatase are usually raised. Due to the ever-decreasing incidence of OFC as a consequence of early picking up of hypercalcemia, OFC presents a diagnostic dilemma, both clinically and radiologically. It often leads to initial mismanagement if a high index of suspicion is not maintained by the treating physician. In developing countries, however, these types of equipment for early pickup are still sparsely available, thus OFC still exists there [4] In the case of OFC, plain radiographs typically depict bone resorption and that of the skull shows classical "salt and pepper" appearance. Distal phalanges show the earliest X-ray changes. Brown tumors can be identified as cysts lined by osteoclasts and blood pigments. These can be identified with nuclear imaging modalities such as the Sestamibi scan [4] The most important way to distinguish these skeletal manifestations of advanced primary hyperparathyroidism from malignancy is by biochemical analysis. PTH will be markedly elevated in primary hyperparathyroidism. In the hypercalcemia of malignancy, such elevation of PTH levels is virtually never seen.
The treatment of underlying PHPT is the first step followed by the management of OFC. Depending upon the severity of disease and symptoms, treatment options can range from hydration to surgical excision of PHPT [5] If left undiagnosed, OFC can lead to severe osteopenia, severe osteoporosis, severe bone aches, and diffuse pathological fractures. This can restrict the patient to complete bed rest. Patients with hyperparathyroidism-induced osteoporosis may be considered for treatment with alendronate or raloxifene. Although no medical treatment has been approved for primary hyperparathyroidism, calcimimetics may reduce serum calcium and PTH levels. Finally, percutaneous alcohol ablation of the parathyroid gland may be a suitable treatment for patients who are unwilling or unable to undergo parathyroidectomy. Nevertheless, in socially isolated persons and populations with suboptimal medical facilities, OFC should remain an important differential for osteolytic bone lesions.3
Younger age and short duration of symptoms in this patient served as a diagnostic challenge, which could have led to misdiagnosis and mismanagement ultimately resulting in worse outcomes. Fortunately, serum calcium and PTH levels followed by radiological and nuclear imaging were done. Finally, a rare diagnosis of OFC was reached and managed successfully.
Conclusion
Osteitis fibrosa cystica is a rare manifestation of hyperparathyroidism, which has become a forgotten entity due to early identification of hypercalcemia by modern techniques, which prevents the florid effect of hyperparathyroidism. A delay in the diagnosis of parathyroid adenoma results in manifestations that can be avoided. The diagnosis of OFC requires a high degree of clinical suspicion. When hypersecretion of PTH is corrected, spontaneous regression of the lesion is expected.
Abbreviations
- OFC
Osteitis fibrosa cystica
- PTH
Parathyroid hormone
- HPT
Hyperparathyroidism
- PHPT
Primary hyperparathyroidism
- ENT
Ear, nose and throat
- MRI
Magnetic resonance imaging
- NCCT
Non contrast computed tomography
Funding
None.
Compliance with ethical standards
Conflicts of interest
None.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Vaibhav Saini, Email: drvaibhavsaini@gmail.com.
Nitin Gupta, Email: nitinent123@gmail.com.
Ankur Mohan, Email: doctorocks@gmail.com.
Vikasdeep Gupta, Email: vdgupta88@gmail.com.
Kartik Kolluru, Email: log2kk92@yahoo.com.
References
- 1.Kearns AE, Thompson GB. Medical and surgical management of hyperparathyroidism. Mayo Clin Proc. 2002;77(1):87–91. doi: 10.4065/77.1.87. [DOI] [PubMed] [Google Scholar]
- 2.Murray JF. Primer on the Metabolic Bone Diseases and Disorders of Mineral Metabolism. 2. New York: Raven Press; 1993. [Google Scholar]
- 3.Lee J, Matthew J, Warwick H, Stephen R (2017) Osteolytic lesions: osteitis fibrosa cystica in the setting of severe primary hyperparathyroidism. BMJ Case Rep Published Online 10.1136/bcr-2017-220603 [DOI] [PMC free article] [PubMed]
- 4.Bilezikian JP, Meng X, Yifan SS, Silverberg SJ. Primary hyperparathyroidism in women: a tale of two cities—New York and Beijing. Int J Fertil Women’s Med. 2000;45(2):158–165. [PubMed] [Google Scholar]
- 5.Rubin MR, Livolsi LA, Bandeira F, Caldas G, Bilezikian JP. Clinical case seminar: Tc99m-sestamibi uptake in osteitis fibrosa cystica simulating metastatic bone disease. J Clin Endocrinol Metab. 2001;86(11):5138–5141. doi: 10.1210/jcem.86.11.7994. [DOI] [PubMed] [Google Scholar]