Abstract
Pleomorphic adenoma (PA) is the most common benign salivary gland neoplasm. Metastasising PA (MPA) is a rare subtype which is histologically and molecularly indistinguishable from the tumor in the primary location that often occurs after multiple recurrences.We herein report a case of 29 year female who underwent right parotidectomy for PA 15 years ago which was followed by history of recurrences and now presenting with MPA involving ipsilateral lymph nodes.
Keywords: Pleomorphic adenoma, Recurrent, Metastasising
Introduction
Pleomorphic adenoma (PA) is the most common benign salivary gland tumor, accounting for 60% of all salivary gland tumors. PA mainly involves parotid gland followed by submandibular gland, soft and hard palate, nasal septum and tongue and has a female predilection. MPA is a rare subtype, the etiology of which remains incompletely understood and the histological appearance, is indistinguishable from a benign PA, thus at great variance with its clinically malignant behaviour. The three common sites of MPA are bone, lung and cervical lymph nodes. Other reported sites include kidney, skin, liver, brain and rarely sinus, retroperitoneum, abdominal wall, pharynx, mediastinum and breast [1, 2].
Complete meticulous excision of the primary lesion may reduce the likelihood of distant spread [3].
Case Report
A 29 year female who underwent right total parotidectomy for a PA 15 years ago with revision surgeries for multiple recurrences, latest being 8 years ago, now presented with a painful hard swelling in right neck of 3 months duration. PET CT performed revealed a mild soft tissue thickening in the parotid bed and metabolically active enlarged right cervical lymph nodes (Fig. 1). FNAC from parotid region and cervical node was done. The patient underwent right cervical lymphadenectomy which included level 1–4 and EJV nodes, the histopathologic examination of which showed PA in the parotid bed and in the lymph nodes (Fig. 2).
Fig. 1.
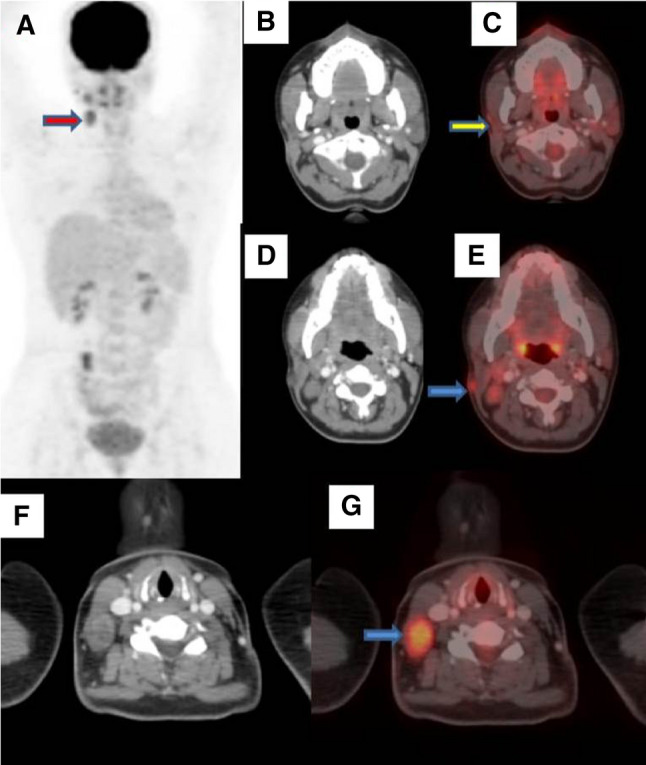
a MIP image with red arrow showing metastatic nodes; c Fused image showing post operative site with yellow arrow; e and g Blue arrow in fused image showing metastatic nodes and b, d and f showing corresponding CT image respectively
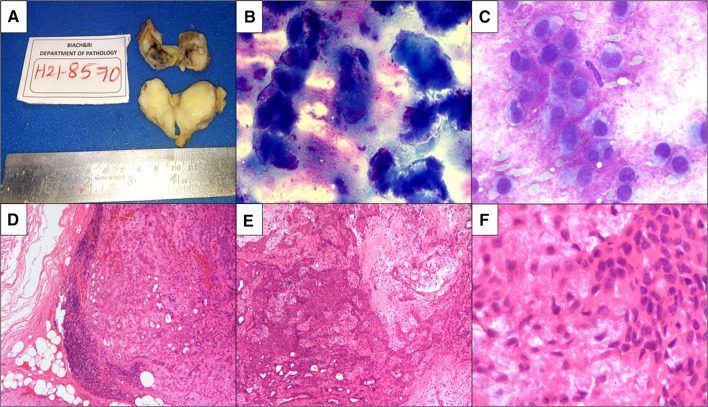
Fig. 2.
a Gross image: The deposit over sternocleidomastoid and lymph node cut section shows a grey white glistening relatively well circumscribed mass; b, c FNAC: Highly cellular smears showing clusters of epithelial cells admixed with metachromatic fibrillary myxoid stroma. Epithelial cells in clusters, trabeculae with round to oval nuclei with minimal cytoplasm myoepithelial cells admixed with metachromatic stroma; d, e, f H&E: lymph nodes show lesion arranged as acini, tubules, nests and cribriform structures with abundant intervening chondromyxoid stroma
Discussion
Pleomorphic adenoma is a benign tumor with high propensity to recur and metastasize when the excision is incomplete. There is often a long time interval between primary PA and detection of metastasis ranging from 1.5 to 55 years [1, 2].PA has clinical features, such as distant metastases and malignant transformation, which are inconsistent with the benign phenotype in local sites. When metastasis of PA occurs, its benign phenotype is preserved [4].
On histology the primary salivary gland tumour as well as the metaststic site shows mixture of benign appearing epithelial and mesenchymal components of PA. Cellular atypia and mitoses are not seen and immunohistochemically Ki-67 proliferation index is low supporting benign histology. Thus no histological features can reliably predict metastasis [2, 5].
Main treatment of PA is meticulous tumor resection with adequate margin. It is documented in literature that surgical manipulation and incomplete removal of tumour lead to tumor cell dislodgement and vascular implantation, and eventually a hematogenous spread associated with local recurrence and distant metastasis [3].
Fusion genes, such as Pleomorphic Adenoma Gene 1(PLAG1) and High Mobility Group A2 (HMGA2) have been reported to be involved in the pathogenesis [3, 6].Transcriptomic analysis has revealed that HMGA2 gene is necessary and sufficient for TGF-β-induced epithelial mesenchymal transition, a major factor in tumor invasiveness and metastasis [7].
Due to long interval between PA resection and detection of MPA it is advisable that patients with incomplete excision or surgical spillage or local recurrence have a long term follow up. A poor prognostic factor includes multiple metastases, which are deemed invariably fatal. It may be impossible to determine which of the locally recurrent PA lesions have the potential to give rise to MPA and therefore, an investigation of a locally recurrent PA should include a search for distant metastases. Hence, whole body PET-CT can be considered as most suitable investigation of choice [2–4].
Literature review of MPA shows 40% of patients die with disease, 47% live free of disease and 13% live with disease [8].
Conclusion
Pleomorphic adenoma can metastasize years after initial disease and can be associated with local recurrences. Development of metastases in the initial 10 years after surgery and presence of metastases in multiple sites, independently predict poor survival.Understanding tumorigenesis of PA with in depth multiomics on large number of cases may help in development of targeted therapy which could make these tumours dormant enabling prevention of metastases and aggressive behaviour.
Declarations
Conflict of interest
No conflicts of interest to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Daphne Fonseca, Email: daf_doc_2005@hotmail.com.
Sahithi Shilpa Arya, Email: shannuarya@gmail.com.
Suseela Kodandapani, Email: suseela.kpani@gmail.com.
Anita Chandini, Email: anita.chandini@gmail.com.
Samatha Kurapati, Email: samathakurapati@gmail.com.
Chandrasekhara Rao, Email: drlmcsraos@gmail.com.
Tejonath Gadepalli, Email: tejonathg@gmail.com.
Zakir Ali, Email: anezak@gmail.com.
References
- 1.Koyama M, Terauchi T, Koizumi M, Tanaka H, Sato Y. Metastasizing pleomorphic adenoma in the multiple organs: a case report on FDG-PET/CT imaging. Medicine (Baltimore) 2018;97(23):e11077. doi: 10.1097/MD.0000000000011077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knight J, Ratnasingham K. Metastasising pleomorphic adenoma: systematic review. Int J Surg. 2015;19:137–145. doi: 10.1016/j.ijsu.2015.04.084. [DOI] [PubMed] [Google Scholar]
- 3.Nouraei SAR, Ferguson MS, Clarke PM, et al. Metastasizing pleomorphic salivary adenoma. Arch Otolaryngol Head Neck Surg. 2006;132(7):788–793. doi: 10.1001/archotol.132.7.788. [DOI] [PubMed] [Google Scholar]
- 4.Iida Y, Serizawa M, Mukaigawa T, Kamijo T, Nakajima T, Asakura K, Kusuhara M, Yamaguchi K, Onitsuka T. Molecular profile of a pleomorphic adenoma of the hard palate: a case report. Medicine (Baltimore) 2020;99(29):e21207. doi: 10.1097/MD.0000000000021207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohan BP, Letha V, Pothen L, Bhat S. Metastasizing pleomorphic adenoma of parotid presenting as a huge renal mass. Indian J Pathol Microbiol. 2018;61:456–457. doi: 10.4103/IJPM.IJPM_111_17. [DOI] [PubMed] [Google Scholar]
- 6.Kumuş O, Ikiz AO, Sarıoglu S, Erdag TK. Recurrent parotid pleomorphic adenomas: our clinical experience. Turk Arch Otorhinolaryngol. 2016;54(3):112–117. doi: 10.5152/tao.2016.1802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thuaultş S, Valcourt V, Petersen M, Manfioletti G, Heldin CH, Moustakas A. Transforming growth factor-beta employs HMGA2 to elicit epithelial-mesenchymal transition. J Cell Biol. 2006;174(2):175–183. doi: 10.1083/jcb.200512110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Soteldo J, Aranaga N. Metastasizing pleomorphic adenoma of the parotid gland. Ecancer. 2017;15(11):758. doi: 10.3332/ecancer.2017.758. [DOI] [PMC free article] [PubMed] [Google Scholar]