Abstract
Endoscopes have revolutionized the field of otology for the past two decades due to its minimally invasive technique and improved visualization. The advantage of endoscope during surgery for middle ear cholesteatoma both for diagnosing and aiding in removal of residual disease from the hidden areas and the resulting lower recurrence rates have been proven in the past by many authors. But the feasibility of totally endoscopic ear surgery and its surgical and patient related outcomes are yet to be explored in detail. We conducted this systematic review and meta-analysis to compare the surgical and patient related outcomes between totally endoscopic and microscopic technique in cases of acquired middle ear cholesteatoma. This meta-analysis has been conducted as per Preferred Reporting Items for Systematic Reviews and Meta-analysis guidelines. Search engines used to identify the eligible articles were Pubmed, Web of Science, Cochrane Library, Virtual Health Library databases. The studies that compared the outcomes of microscopic and endoscopic techniques in case of acquired middle ear cholesteatoma and with more than 10 patients were included. Outcomes like recurrence, residual disease, graft uptake rate, audiological outcome, conversion rate, pain score, surgery duration, complications and quality of life outcomes were compared.The quality of the included studies was assessed by Methodological Index for Non-randomized studies criteria in case of non-randomized studies and by means of Cochrane Risk of Bias Tool in case of randomized controlled studies. A random effects model was used to calculate pooled estimates. The ODDS ratio and 95% confidence interval were calculated. The heterogeneity among the studies was represented by the Q statistic and Higgins I2 statistic. The test for overall effect was calculated by Z test and a p value of < 0.05 was considered as statistically significant. 11 studies were included in this meta-analysis. Out of 11 included studies, 4 were prospectively designed and 7 were retrospective studies. The overall effect showed recurrence rate (Z:2.69, P:0.007) was lower among endoscopic technique. Post-operative pain was less among the endoscopic technique and there was no difference between the groups with respect to surgical duration. Although endoscopic technique showed lower residual rate and post-operative vertigo with better graft success rate among the individual studies, the overall analysis showed that the difference was not statistically significant. Endoscope has been an invaluable tool in the cholesteatoma surgery over the past 20 years due to its excellent optics and minimally invasive technique. Evaluation of the present data available in the literature reveals that both the techniques have similar outcomes except for a definite advantage of endoscopic technique in reducing the recurrence and post-operative discomfort.
Keywords: Cholesteatoma, Endoscopic, Totally endoscopic ear surgery (TEES), Middle ear cholesteatoma, Chronic otitis media (COM), Squamous disease
Introduction
Endoscopes have revolutionized the field of otology for the past two decades due to its minimally invasive technique and improved visualization [1]. The utility of endoscope in cases of middle ear cholesteatoma has come a long way. Endoscopes were initially used as a diagnostic tool to inspect the hidden areas that were inaccessible to microscope in order to find the residual cholesteatoma during surgery. Later endoscopes were used as an adjunct to microscopes to aid in the dissection of cholesteatoma in the difficult to reach areas [1, 2]. At present totally endoscopic ear surgeries (TEES) have been performed in cases of middle ear cholesteatoma.
The advantage of endoscope during surgery for middle ear cholesteatoma both for diagnosing and aiding in removal of residual disease from the hidden areas and the resulting lower recurrence rates have been proven in the past by many authors. But the feasibility of TEES and its surgical and patient related outcomes are yet to be explored in detail. We conducted this systematic review and meta-analysis to compare the surgical and patient related outcomes between totally endoscopic and microscopic technique in cases of acquired middle ear cholesteatoma.
Material and Methods
Search Criteria
This meta-analysis has been conducted as per Preferred Reporting Items for Systematic Reviews and Meta-analysis guidelines (PRISMA) [3]. Search engines used to identify the eligible articles were Pubmed, Web of Science, Cochrane Library, Virtual Health Library (VHL) databases. The period of search was from January 1st 2000 to December 31st 2020. The MeSH terms or phrases used for literature search were microscop*, endoscop*, cholesteatoma, middle ear cholesteatoma, chronic otitis media squamous disease, chronic otitis media unsafe type, chronic otitis media squamous type. The references of all the eligible articles were manually checked to identify the missed out studies.
Only comparative articles published in English that evaluated and compared the outcomes of microscopic and endoscopic techniques for acquired middle ear cholesteatoma were selected.
Selection Criteria
The titles and abstracts of the selected articles were scanned by two authors independently. In case of any discrepancies or disputes, the decision of the third investigator (senior author) was finalized. Full text of the selected articles was thoroughly studied and the duplicate studies were excluded and the most recent study with sufficient and complete data was included. The authors of the articles with incomplete data were not contacted to procure the unpublished data and those articles were excluded.
Inclusion and Exclusion Criteria
The studies that compared the outcomes of microscopic (MES) and endoscopic (EES) techniques in case of acquired middle ear cholesteatoma and with more than 10 patients were included. Both adult and pediatric study populations were included in this study. As per Cohen et al. [4] classification of endoscopic ear surgery, class 0 and 1 has been included in the microscopic ear surgery group and class 3 (TEES) has been included in the endoscopic ear surgery group. The articles in which class 2 and 3 have been published, the results of class 3 have been extracted. If the results of class 2 and 3 have been combined in the particular study, the article was excluded from the study. The results of congenital cholesteatoma were excluded and the studies in which the congenital cholesteatoma and acquired cholesteatoma among pediatric populations were not distinguished were excluded. The articles with atleast one or more defined outcomes like recurrence, residual disease, graft uptake rate, audiological outcome, conversion rate, pain score, surgery duration, complications and quality of life outcomes were included.
Abstracts, letters, editorials, reviews, expert opinion and animal studies were excluded. Studies with duplicated or insufficient data or studies with combined results of EES 2 and 3, congenital cholesteatoma data and studies without full text availability were excluded.
Data Extraction
The included studies were scanned by 2 independent authors for first author, publication year, study design, study population, number of patients, follow up period, surgical approach, outcome measures like recurrence, residual disease, graft uptake rate, audiological outcome, pre-operative ossicular status, stage or extent of the disease, conversion rate, pain score, surgery duration, complications and quality of life outcomes.
Quality Assessment
The quality of the included studies was assessed by Methodological Index for Non-randomized studies (MINORS) criteria [5] in case of non-randomized studies and by means of Cochrane Risk of Bias Tool in case of randomized controlled studies [6]. MINORS criteria includes 12 separate items for comparative studies and each item is scored as 0 (unreported), 1 (reported but not complete) and 2 (reported and complete) with total maximum score of 24.
Statistical Analysis
The data was extracted and analyzed using the software package Review Manager 5.4 (RevMan 5.4, The Cochrane Collaboration, Oxford, United Kingdom). A random effects model was used to calculate pooled estimates. The ODDS ratio (OR) and 95% confidence interval (CI) were calculated. Continuous outcomes were presented as the weighted mean difference (WMD) and 95% confidence interval. The heterogeneity among the studies was represented by the Q statistic and Higgins I2 statistic. For Q statistic heterogeneity was considered if p < 0.1. The heterogeneity of a certain outcome in the included studies was determined as low (I2 < 25%), moderate (I2 = 25–50%) or high (I2 < 50%). All statistical tests were two-sided. The test for overall effect was calculated by Z test and a p value of < 0.05 was considered as statistically significant. Funnel plot was used to assess the possible publication bias if there were more than three included studies for a particular outcome. Eggers’s test and rank correlation analysis were also done to determine publication bias.
Results
Selection of Included Studies
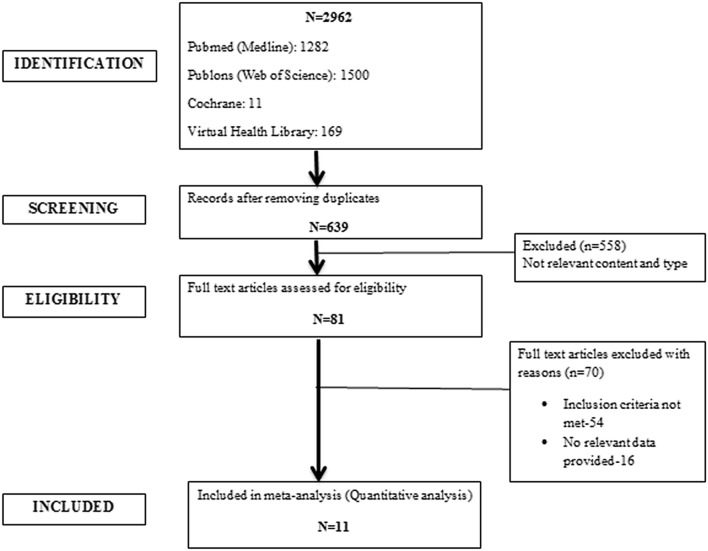
Total of 2962 articles were found on the initial search and 2323 articles were excluded after scanning the titles for duplicate studies. 639 abstracts were assessed and 558 studies were eliminated for non-relevant content and type. Full texts of 81 articles were examined and finally 11 studies were included in the meta-analysis [7–17]. The flow diagram for selection of included studies is depicted in Fig. 1.
Fig. 1.
Flowchart depicting the selection of included studies
Characteristics of Included Studies
Out of 11 included studies, 4 were prospectively designed and 7 were retrospective studies. 10 studies were original articles and one is a randomized controlled trial (RCT). The articles were published from January 1st 2000 to December 31st 2020 and in English language. Total of 872 ears were included in the meta-analysis of which 441 were operated by microscopic technique and 431 ears were operated by totally endoscopic ear surgery (TEES). The characteristics of the included studies are depicted in Table 1.
Table 1.
Characteristics of included studies
| No | Author | Year | Country | Type | No. of patients | Population | Follow-up (months) | Primary outcomes | Secondary outcomes | |
|---|---|---|---|---|---|---|---|---|---|---|
| EES | MES | |||||||||
| 1 | DIXON [7] | 2020 | CANADA | Prospective | 65 | 112 | Pediatric | 24 | Residual | Stage |
| 2 | DAS [8] | 2019 | INDIA | Prospective | 39 | 39 | Adult | 12 | Recurrance Graft success | MESVI, Audiological, post-op pain |
| 3 | BAE [9] | 2019 | KOREA | Retrospective | 10 | 10 | Adult | 29.4 | Recurrance Residual | Audiological, surgical time |
| 4 | GHADEROSHI [10] | 2017 | USA | Retrospective | 12 | 6 | Pediatric | 31.2 | Recurrance Residual | Audiological, surgical time |
| 5 | GLIKSON [11] | 2019 | ISRAEL | Retrospective | 30 | 19 | Pediatric | > 12 | Recurrance Residual | Audiological, complications |
| 6 | HUNTER [12] | 2016 | USA | Retrospective | 8 | 47 | Pediatric | 18.8 | Recurrance Residual | Audiological, surgical time |
| 7 | KAHEKATA [13] | 2018 | JAPAN | Prospective | 106 | 55 | Adult | – | Post-op pain | – |
| 8 | KILEEN [14] | 2019 | USA | Retrospective | 35 | 30 | Adult | 49.7-MES 18-EES | Recurrance Residual | Audiological, surgical time Conversion rate Extent of disease |
| 9 | MAGLIULO [15] | 2018 | ITALY | Prospective | 40 | 40 | Adult | 12.3 | Recurrance | Complications |
| 10 | MARCHIONI [16] | 2015 | ITALY | Retrospective | 31 | 28 | Pediatric | 36 | Recurrance Residual | Stage Audiological, Complications |
| 11 | PRESUTTI [17] | 2018 | ITALY | Retrospective | 55 | 55 | Adult | 29.7 | Recurrance | Location of disease Graft success |
Quality of Included Studies
The 10 original articles were subjected to quality assessment by MINORS criteria and the mean total score was 15.1 (12–20). All the 10 studies were of moderate to good quality (Table 2). One RCT included was subjected to Cochrane risk of bias tool for quality assessment (Table 3). The selection bias by means of random sequence generation and allocation concealment was of low risk and also reporting bias was of low risk. The other sources of bias were unclear.
Table 2.
Minors Scoring For The Original Articles Included
| No | Author | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | 7 | Q8 | Q9 | Q10 | Q11 | Q12 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | DIXON | 2 | 2 | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 2 | 2 | 2 | 20 |
| 2 | BAE | 2 | 0 | 0 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 0 | 0 | 14 |
| 3 | GHADEROSHI | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 0 | 0 | 14 |
| 4 | GLIKSON | 2 | 2 | 0 | 2 | 0 | 2 | 0 | 0 | 2 | 2 | 2 | 0 | 14 |
| 5 | HUNTER | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 1 | 0 | 15 |
| 6 | KAHEKATA | 2 | 2 | 2 | 2 | 0 | 1 | 0 | 0 | 1 | 2 | 1 | 1 | 14 |
| 7 | KILEEN | 2 | 0 | 0 | 2 | 0 | 2 | 0 | 0 | 2 | 1 | 2 | 1 | 12 |
| 8 | MAGLIULO | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 2 | 1 | 19 |
| 9 | MARCHIONI | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 0 | 0 | 14 |
| 10 | PRESUTTI | 2 | 2 | 0 | 2 | 0 | 2 | 2 | 0 | 2 | 2 | 0 | 1 | 15 |
Q1- Clearly stated aim; Q2- Inclusion of consequetive patients; Q3- prospective data; Q4- End point data mentioned; Q5- Unbiased (blinding); Q6- Follow-up period adequate; Q7- Lost to follow-up < 5%; Q8- Prospective study size calculation; Q9- Control group appropriate; Q10- Same period of evaluation for both groups; Q11- Similar groups; Q12- Appropriate statistical analysis
Table 3.
Cochrane Risk Of Bias Tool Assessment For The Included Study
| Selection Bias | |
| Random sequence generation | Low risk of bias |
| Allocation concealment | Low risk of bias |
| Reporting Bias | Low risk of bias |
| Other Bias | Unclear |
Author: Das et al. [8] (Randomized Control Study)
Sample size calculation, ODDS ratio, relative risk and 95% confidence interval were not mentioned in any of the studies. Blinding and allocation methods were reported only in one study which was a randomized controlled trial. Only 4 out of 11 studies were prospectively designed.
Outcomes
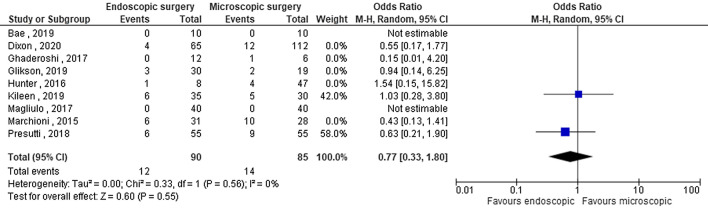
Residual Disease
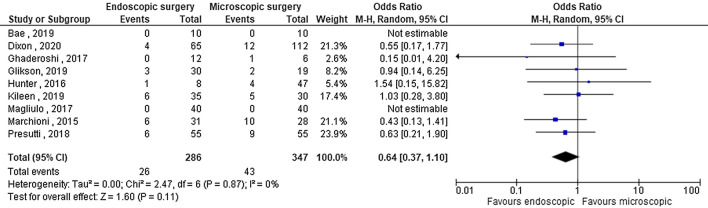
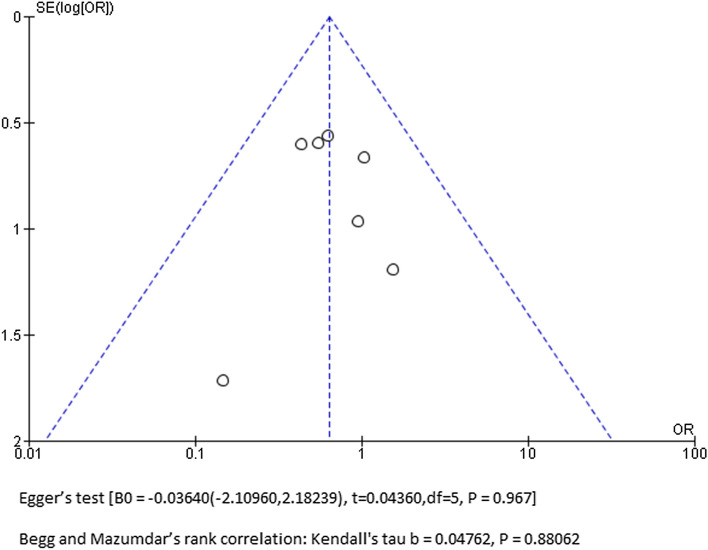
Seven out of 11 included studies provided residual disease data. Total of 633 ears were included in the quantitative analysis of which 286 were endoscopic and 347 were microscopic techniques. No heterogeneity of the OR noted among the included studies (OR:0.64, 95% CI:0.37–1.10, I2:0%, P:0.87) [Fig. 2]. The overall effect showed residual disease rate was comparable between the groups (Z:1.60, P:0.11). There was no possible publication bias [Fig. 3].
Fig. 2.
Forest plot for residual disease
Fig. 3.
Funnel plot for residual disease
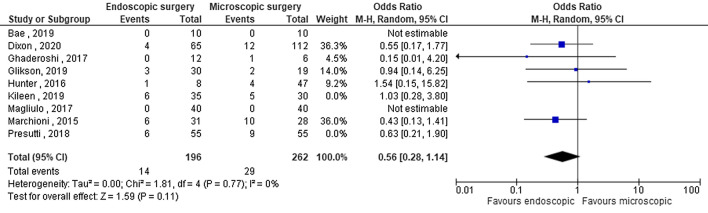
Subgroup analysis among the pediatric and adult age group revealed no heterogeneity and the pooled analysis showed endoscopic technique rendered equivalent residual disease rate compared to microscopic technique [Figs. 4, 5].
Fig. 4.
Sub-group analysis of pediatric population for residual disease
Fig. 5.
Sub-group analysis of adult population for residual disease
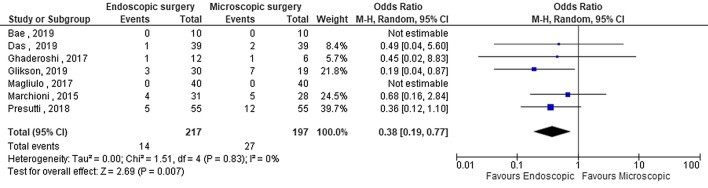
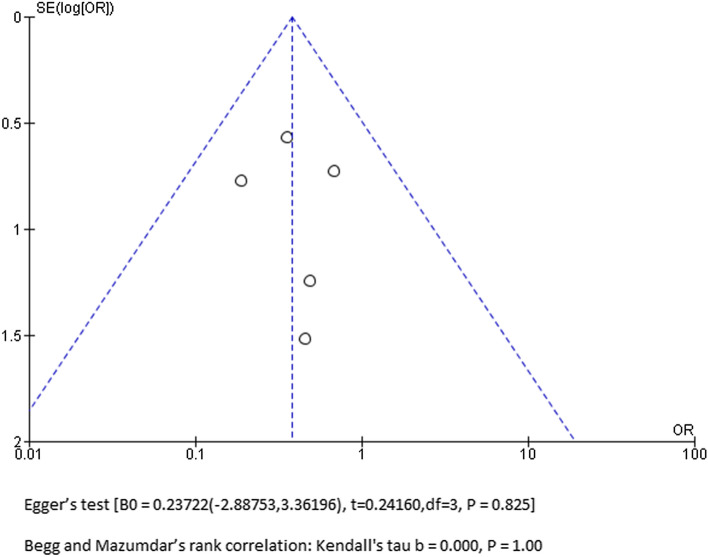
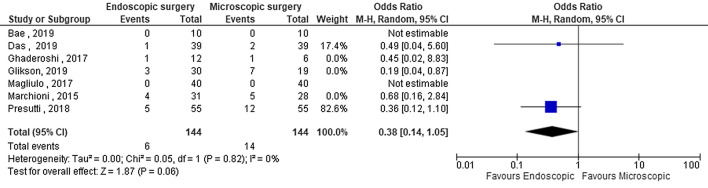
Recurrence
The recurrence rate was given only in 7 studies for quantitative analysis. Total number of ears included in the analysis was 414 out of which 217 underwent endoscopic technique and 197 ears underwent microscopic technique. All the 7 studies had more than 12 months follow up period. The quantitative analysis revealed no heterogeneity among the variables in the included studies (OR:0.38, 95% CI:0.19–0.77, I2:0%, P:0.83) [Fig. 6]. The pooled analysis for overall effect showed that recurrence rate was lower among the endoscopic technique as compared to the microscopic technique (Z:2.69, P:0.007). Funnel plot revealed no publication bias [Fig. 7].
Fig. 6.
Forest plot for recurrance rate
Fig. 7.
Funnel plot for recurrance rate
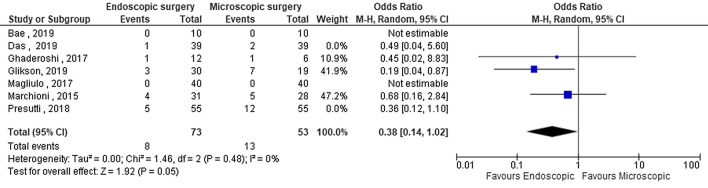
Subgroup analysis was done for recurrence among adult and pediatric population. 126 pediatric population (MES-53, EES-73) and 288 adult population (MES-144, EES-144) were included. There was no heterogeneity among the studies and pooled analysis revealed lower recurrence rate in the endoscopic technique for pediatric subgroup compared to microscopic technique [Fig. 8, 9].
Fig. 8.
Sub-group analysis of pediatric population for recurrance rate
Fig. 9.
Sub-group analysis of adult population for recurrance rate
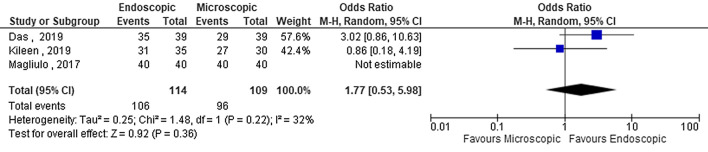
Graft Success Rate
Only 3 studies provided the data for graft success rate. 223 ears were included in the quantitative analysis (MES-109, EES-114). There was moderate heterogeneity for the variable among the studies (OR:1.77, 95% CI:0.53–5.98, I2:32%, P:0.22) and the overall effect showed graft success rate was equivalent between the two groups (Z:0.92, P:0.36) [Fig. 10].
Fig. 10.
Forest plot for graft success rate
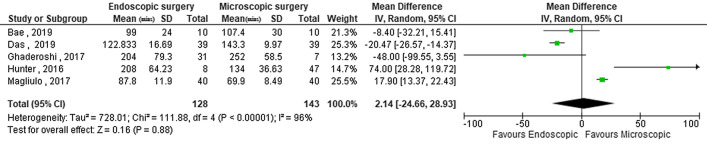
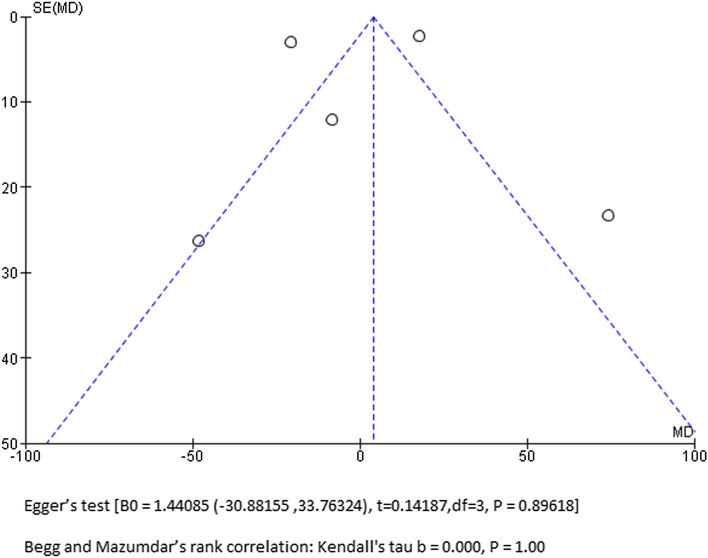
Surgery Duration
The surgery duration was given as mean with standard deviation in 5 studies (Total: 271, EES:128, MES:143). The continuous variables were represented as weighted mean difference (WMD). There was high degree of heterogeneity among the studies with I2 value of 96% (WMD: 2.14, 95% CI:-24.66–28.93, I2:96%, P: < 0.00001) [Fig. 11]. The pooled analysis for overall effect showed no statistically significant difference in the surgical duration among both the groups (Z:0.16, P:0.88). The funnel plot showed no possible publication bias [Fig. 12].
Fig. 11.
Forest plot for surgery duration
Fig. 12.
Funnel plot for surgery duration
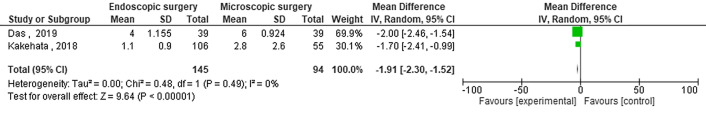
Post-operative Pain:
Two out of 11 studies provided data regarding post-operative pain (Total: 239, EES:145, MES:94). There was no heterogeneity (WMD: 1.91, 95% CI:-2.3 to -1.52, I2:0%, P:0.49) and the overall effect revealed lesser post-operative pain among the endoscopic technique (Z:9.64, P: < 0.00001) [Fig. 13].
Fig. 13.
Forest plot for post-operative pain
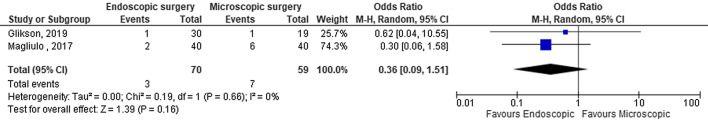
Post-operative Vertigo
Post-operative vertigo was given in 2 studies (Total:129, EES:70, MES:59). The pooled analysis for the overall effect revealed that the incidence of post-operative vertigo was equivalent among both the groups and without any heterogeneity among the included studies [Fig. 14].
Fig. 14.
Forest plot for post-operative vertigo
Discussion
The principle of cholesteatoma treatment is extensive disease removal along with reconstruction of hearing. Preservation of normal mucociliary function, clearance of ventilation pathway of middle ear and mastoid and improved hearing outcome are the essential factors that aid in improved surgical as well as patient related outcomes. In this context, the main drawback with the traditional microscopic approach is the visualization of the hidden areas such as epitympanic recess, retrotympanum and hypotympanum which comprise the ‘blind spots’ of the tympanic cleft [1, 18–20]. Endoscopes were initially used as an adjunct to overcome this difficulty and the present day otologists are performing totally endoscopic ear surgery (TEES) with comparable results to the microscopic ear surgery with respect to middle ear cholesteatoma.
This systematic review and meta-analysis was performed to assess and compare the structural, functional and quality of life outcomes between the microscopic and endoscopic ear surgery in middle ear cholesteatoma. The structural outcomes were evaluated by means of recurrence rate, residual disease and graft uptake rate, functional outcome in terms of post-operative A-B gap closure while the QOL outcomes were assessed in terms of surgery duration, complications, post-operative pain and vertigo.
Success of cholesteatoma treatment depends mainly on the structural and functional outcomes. Recidivism (recurrence and residual) and middle ear structural integrity in terms of graft uptake indicates the structural outcome. Incomplete disease removal, failure to clear the middle ear ventilation pathway and excessive mucosal damage can affect the structural outcomes [17, 21, 22].
Residual disease is equivalent to the disease left behind during the surgery due to improper visualization or limited access to the hidden areas. In this context endoscopes have become the excellent tool along with the microscope as hybrid procedure in order to decrease the residual disease. The use of endoscope as an adjunct has reduced the recidivism from 47 to 6% [17, 23].
In our analysis, the rate of residual disease among the included studies ranged from 6–33% in endoscopic technique and 10–40% among microscopic technique. Although individual studies showed lower residual rates among the endoscopic group, the pooled analysis for overall effect revealed residual rates were similar between the groups. The most common area of residual disease is tympanic cavity and not the mastoid [17, 21, 22, 25, 26]. So the visualization and removal of disease from the tympanic cavity is more important than excessive removal of mastoid cells. This concept has led to the basis for decreased residual disease among the endoscopic technique.
There is a debate in the type of surgery performed in children regarding whether extensive debridement is necessary or adequate removal with preservation of normal mucosa is warranted. The reasons for aggressive removal in pediatric patients include pneumatized mastoid and their predisposition to complications [24]. Extensive mastoid dissection leads to large mastoid cavity that results in hearing impairment and cavity related problems. Endoscopic approach to cholesteatoma has been favored by many otologists in order to reduce the cavity related complications, improve the hearing without any compromise on the disease clearance. We performed a sub-group analysis of outcomes for pediatric and adult population among both the techniques in order to reduce the heterogeneity. The overall effect revealed that endoscopic ear surgery conferred similar residual disease as compared to microscopic surgery among the pediatric population.
Recurrence of the disease occurs after adequate removal of the disease during the initial surgery but when the factors causing the disease process still exists [21, 22]. Endoscopic technique is minimally invasive and improves the ventilatory pathway as well as retains normal mucociliary function which is the cornerstone of treating cholesteatoma and for preventing recurrence. In our analysis, recurrence rates among the included studies ranged from 2.5–18% among endoscopic technique and 5–37% among the microscopic technique. The pooled analysis revealed that recurrence rates are lower among the endoscopic ear surgery. The overall effect of recurrence rate for sub-group analysis showed lower recurrence rates among endoscopic technique for pediatric population.
In addition to the recidivism, the status of the middle ear and the neotympanum also has an impact on the structural and functional outcomes of the surgery. Structural integrity or graft uptake has been evaluated in terms of perforation, retraction pocket formation and cartilage displacement [7–17]. The extent of mucosal damage is less among the endoscopic technique which results in better graft success rate. In our analysis the overall effect showed that graft uptake rate was equivalent among both the approaches.
Functional outcome in terms of hearing improvement is essential in determining the efficacy of a surgical technique. The ossicular preservation is high among the endoscopic technique with 42% when compared to 10% among the microscopic technique [9, 10, 12]. Improved visualization of ossicular chain along with preservation of normal mastoid air cells helps in improved hearing outcome in the endoscopic technique. We considered post-operative A-B gap closure as the measure of hearing improvement. The mean A-B gap improvement ranges from 14-21 dB and 13-17 dB in endoscopic and microscopic approaches respectively in the literature. However in our analysis, only one study (Bae et al.) showed mean post-operative A-B closure of 6.7 dB and 1.7 dB among endoscopic and microscopic techniques respectively. Due to lack of proper audiological data among the included studies, analysis could not be performed.
Improved quality of life is an important factor to assess the efficacy of any surgical technique and the technique with equitable results and better quality of life outcomes is preferred. Endoscopic technique is a minimally invasive approach that fits the objective of decreased post-operative pain, less hospital stay, faster recovery and early return to daily routine. In addition, there is no need for mastoid bandage, head shave or visible post-aural scar resulting in improved cosmesis [27–30]. Post-operative pain is the only QOL outcome that was assessed among the included studies and our analysis showed that endoscopic ear surgery has advantage of rendering minimal post-operative pain compared to microscopic technique due to minimal tissue dissection and transcanal approach.
Complications after cholesteatoma surgery are few and rare which includes temporary (2–5%) and permanent facial palsy (< 1%), dizziness (3–15%), worsening of hearing (5–10%) and abnormal taste sensation (25–40%) [31]. However, only few studies have reported regarding the incidence of these complications. The incidence of post-operative vertigo was similar among the groups in our analysis.
There is a lack of uniformity in the reporting of staging and outcomes among various studies in the literature. Most of the studies in literature are non-comparative and are retrospectively designed. Despite multiple classifications for cholesteatoma being available in the literature there is no universally accepted single staging system [32, 33]. Furthermore the type of surgery performed should be defined based on the extent of the disease removal and type of hearing reconstruction performed. Pooled analysis for extent of cholesteatoma and type of surgery performed could not be performed due to this lack of uniformity in literature. Functional outcome in terms of hearing improvement had been evaluated by post-operative improvement in air and bone conduction and mean A-B gap closure. There is no uniformity in reporting the hearing improvement and only one out of 11 included studies provided the data regarding mean A-B gap closure. There is lack of data regarding conversion rate, complications and quality of life (QOL) in the literature. Most of the authors are endoscopic surgeons who have performed TEES and compared the results to microscopic approach which could lead to possible inherent reporting bias.
Traditionally microscopic technique has been used as the treatment modality for middle ear cholesteatoma. Though endoscopic technique has various advantages, the knowledge of inside-out anatomy and performing one-handed surgery requires a learning curve. Performing limited cholesteatoma involving the middle ear, attic and antrum is amenable to endoscopic technique and when the cholesteatoma extends to the mastoid beyond antrum the need for microscope arises.
Conclusion
Endoscope has been an invaluable tool in the cholesteatoma surgery over the past 20 years due to its excellent optics and minimally invasive technique. This systematic review and meta-analysis was conducted to evaluate and compare the efficacy of totally endoscopic ear surgery (TEES) with microscopic technique for middle ear cholesteatoma. There are anecdotal and single institution studies demonstrating the advantages of endoscopic technique over microscopic technique in middle ear cholesteatoma. However on evaluation of the present data available in the literature, both the techniques have similar outcomes except for a definite advantage of endoscopic technique in reducing the recurrence and post-operative discomfort. High quality comparative studies with uniform staging and outcome reporting system are required to evaluate the other aspects of endoscopic technique in cholesteatoma surgery.
Author Contribution
S. N: Substantial contributions to the conception or design of the work, revising it critically for important intellectual content, final approval of the version to be published. J G Aishwarya: Substantial contributions to the acquisition of data for the work, revising it critically for important intellectual content. Pooja K Vasu, Aditya Karthikeyan: Substantial contributions to the acquisition of data for the work and revising it. Martina Shalini: Substantial contribution for the statistical evaluation and revising it.
Funding
The authors have no relevant financial or non-financial interests to disclose. No funds, grants or other supports received for this study. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Declarations
Conflicts of Interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical Approval
Institutional Ethical Committee has confirmed that no ethical approval is required for this study since it is a systematic review and meta-analysis.
Informed Consent
Informed consent is not applicable since this is a systematic review and meta-analysis.
Standard of Reporting
This systematic review and meta-analysis has been performed and reported in compliance with PRISMA guidelines.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Thomassin JM, Korchia D, Doris JMD. Endoscopic-guided otosurgery in the prevention of residual cholesteatomas. Laryngoscope. 1993;103:939–943. doi: 10.1288/00005537-199308000-00021. [DOI] [PubMed] [Google Scholar]
- 2.El-Meselaty K. Endoscope affects decision making in cholesteatoma surgery. Otolaryngol Head Neck Surg. 2003;129:490–496. doi: 10.1016/S0194-59980301577-8. [DOI] [PubMed] [Google Scholar]
- 3.Liberati A, Altman D, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. [DOI] [PMC free article] [PubMed]
- 4.Cohen MS, Basonbul RA, Barber SR, Kozin ED, Rivas AC, Lee DJ. Development and validation of an endoscopic ear surgery classification system. Laryngoscope. 2018;128(4):967–970. doi: 10.1002/lary.26802. [DOI] [PubMed] [Google Scholar]
- 5.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 6.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions, Version 5.0.2 updated September 2009. The Cochrane Collaboration. http://cochrane.org/resources/hand book/.
- 7.Dixon PR, James AL. Evaluation of Residual Disease Following Transcanal Totally Endoscopic vs Postauricular Surgery Among Children With Middle Ear and Attic Cholesteatoma. JAMA Otolaryngol Head Neck Surg. 2020;146(5):408–413. doi: 10.1001/jamaoto.2020.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Das A, Mitra S, Ghosh D, Sengupta A. Endoscopic Versus Microscopic Management of Attic Cholesteatoma: A Randomized Controlled Trial. Laryngoscope. 2020;130(10):2461–2466. doi: 10.1002/lary.28446. [DOI] [PubMed] [Google Scholar]
- 9.Bae MR, Kang WS, Chung JW. Comparison of the clinical results of attic cholesteatoma treatment: endoscopic versus microscopic ear surgery. Clin Exp Otorhinolaryngol. 2019;12:156–162. doi: 10.21053/ceo.2018.00507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ghadersohi S, Carter JM, Hoff SR. Endoscopic transcanal approach to the middle ear for management of pediatric cholesteatoma. Laryngoscope. 2017;127:2653–2658. doi: 10.1002/lary.26654. [DOI] [PubMed] [Google Scholar]
- 11.Glikson E, Feinmesser G, Sagiv D, Wolf M, Migirov L, Shapira Y. Trans-canal endoscopic ear surgery and canal wall-up tympano-mastoidectomy for pediatric middle ear cholesteatoma. Eur Arch Otorhinolaryngol. 2019. [DOI] [PubMed]
- 12.Hunter JB, Zuniga MG, Sweeney AD, et al. Pediatric endoscopic cholesteatoma surgery. Otolaryngol Head Neck Surg. 2016;154:1121–1127. doi: 10.1177/0194599816631941. [DOI] [PubMed] [Google Scholar]
- 13.Kakehata S, Furukawa T, Ito T, Kubota T, Futai K, Watanabe T. Comparison of Postoperative Pain in Patients Following Transcanal Endoscopic Versus Microscopic Ear Surgery. Otol Neurotol. 2018;39(7):847–853. doi: 10.1097/MAO.0000000000001864. [DOI] [PubMed] [Google Scholar]
- 14.Killeen DE, Tolisano AM, Kou YF, Kutz JW, Jr, Isaacson B. Recidivism After Endoscopic Treatment of Cholesteatoma. Otol Neurotol. 2019;40(10):1313–1321. doi: 10.1097/MAO.0000000000002395. [DOI] [PubMed] [Google Scholar]
- 15.Magliulo G, Iannella G. Endoscopic versus microscopic approach in attic cholesteatoma surgery. Am J Otolaryngol. 2018;39:25–30. doi: 10.1016/j.amjoto.2017.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Marchioni D, Soloperto D, Rubini A, et al. Endoscopic exclusive transcanal approach to the tympanic cavity cholesteatoma in pediatric patients: Our experience. Int J Pediatr Otorhinolaryngol. 2015;79:316–322. doi: 10.1016/j.ijporl.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 17.Presutti L, Anschuetz L, Rubini A, et al. The impact of the transcanal endoscopic approach and mastoid preservation on recurrence of primary acquired attic cholesteatoma. Otol Neurotol. 2018;39:445–450. doi: 10.1097/MAO.0000000000001712. [DOI] [PubMed] [Google Scholar]
- 18.Tarabichi M. Endoscopic middle ear surgery. Ann Otol Rhinol Laryngol. 1999;108:39–46. doi: 10.1177/000348949910800106. [DOI] [PubMed] [Google Scholar]
- 19.Ayache S. Otoendoscopy in cholesteatoma surgery of the middle ear: what benefits can be expected? Otol Neurotol. 2008;29:1085–1090. doi: 10.1097/MAO.0b013e318188e8d7. [DOI] [PubMed] [Google Scholar]
- 20.Badr-el-Dine M. Value of ear endoscopy in cholesteatoma surgery. Otol Neurotol. 2002;23:631–635. doi: 10.1097/00129492-200209000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Marchioni D, Villari D, Mattioli F, Alicandri-Ciufelli M, Piccinini A, Presutti L. Endoscopic management of attic cholesteatoma a single- institution experience. Otolaryngol Clin North Am. 2013;46:201–209. doi: 10.1016/j.otc.2012.10.004. [DOI] [PubMed] [Google Scholar]
- 22.Marchioni D, Piccinini A, Alicandri-Ciufelli M, Presutti L. Endoscopic anatomy and ventilation of the epitympanum. Otolaryngol Clin North Am. 2013;46:165–178. doi: 10.1016/j.otc.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 23.Li Bo, Zhou Lingyun, Wang Miaowei, Wang Yanwen, Zou Jian. Endoscopic versus microscopic surgery for treatment of middle ear cholesteatoma: A systematic review and meta-analysis. Am J Otolaryngol. March 2020;102451. 10.1016/j.amjoto.2020.102451. [DOI] [PubMed]
- 24.Sarcu D, Isaacson G. Long-term results of endoscopically assisted pediatric cholesteatoma surgery. Otolaryngol Head Neck Surg. 2016;154:535–539. doi: 10.1177/0194599815622441. [DOI] [PubMed] [Google Scholar]
- 25.Presutti L, Marchioni D, Mattioli F, Villari D, Alicandri-Ciufelli M. Endoscopic management of acquired cholesteatoma: our experience. J Otolaryngol Head Neck Surg. 2008;37:481–487. [PubMed] [Google Scholar]
- 26.Presutti L, Gioacchini FM, Alicandri-Ciufelli M, Villari D, Marchioni D. Results of endoscopic middle ear surgery for cholesteatoma treatment: a systematic review. Acta Otorhinolaryngol Ital. 2014;34:153–157. [PMC free article] [PubMed] [Google Scholar]
- 27.Baumann I, Kurpiers B, Plinkert PK, Praetorius M (2009) Development and validation of the Chronic Otitis Media Outcome Test 15 (COMOT-15). Measurement of health-related quality of life in patients with chronic otitis media. HNO 57(9):889–895 [DOI] [PubMed]
- 28.Quaranta N, Iannuzzi L, Petrone P, D’Elia A, Quaranta A. Quality of life after cholesteatoma surgery: intact-canal wall tympanoplasty versus canal wall-down tympanoplasty with mastoid obliteration. Ann Otol Rhinol Laryngol. 2014;123(2):89–93. doi: 10.1177/0003489414523562. [DOI] [PubMed] [Google Scholar]
- 29.Bennett ML, Zhang D, Labadie RF, Noble JH. Comparison of middle ear visualization with endoscopy and microscopy. Otol Neurotol. 2016;37:362–366. doi: 10.1097/MAO.0000000000000988. [DOI] [PubMed] [Google Scholar]
- 30.Kiringoda R, Kozin ED, Lee DJ. Outcomes in Endoscopic Ear Surgery. Otolaryngol Clin North Am. 2016;49(5):1271–1290. doi: 10.1016/j.otc.2016.05.008. [DOI] [PubMed] [Google Scholar]
- 31.Kumar R, Karthikeyan CV, Singh CA, Preetam C, Sikka K. Iatrogenic facial nerve palsy “Prevention is better than cure”: Analysis of four cases. Indian J Otol. 2011;17:170–172. doi: 10.4103/0971-7749.94498. [DOI] [Google Scholar]
- 32.Linder Thomas E, Shah Shankar, Martha Aline Silveira, Roosli Christof, Emmett Susan D. Introducing the “ChOLE” Classification and Its Comparison to the EAONO/JOS Consensus Classification for Cholesteatoma Staging, Otol & Neurotol. 2019;40(1):63–72. [DOI] [PubMed]
- 33.Yung M, James A, Merkus P, Philips J, Black B, Tono T, Linder T, Dornhoffer J, İncesulu A. International Otology Outcome Group and the International Consensus on the Categorization of Tympanomastoid Surgery. J Int Adv Otol. 2018;14(2):216–226. doi: 10.5152/iao.2018.5553. [DOI] [PMC free article] [PubMed] [Google Scholar]