Abstract
Background
Brazilian butt lift (BBL) surgery has been the fastest growing aesthetic surgical procedure over the past decade. By 2017, the risk of death from pulmonary fat (PFE) was identified, earning the BBL the highest mortality rate of any aesthetic surgical procedure. South Florida carries the highest BBL mortality by far in the nation.
Objectives
The purpose of this study was to explore the factors involved in making South Florida an outlier in terms of BBL mortality.
Methods
The anatomic findings of the gluteal dissections from 11 post-BBL surgery autopsies (22 hemibuttocks) were assessed for commonalities. The public records of patients who died from BBL-related fat emboli were examined to determine commonalities.
Results
All BBL PFE cases had fat grafts injected into the gluteal musculature in multiple different levels. Another commonality involved the location where the surgery took place, with the great majority of patients (92%) undergoing surgery at high-volume, budget clinics located in South Florida. Short surgical times of approximately 90 minutes appeared to be the norm for these cases.
Conclusions
South Florida has experienced 25 BBL-related fat emboli deaths between 2010 and 2022; however, 14 of these occurred after publication of the Aesthetic Surgery Education and Research Foundation's 2018 guidelines and the 2019 Florida Board of Medicine's BBL “subcutaneous-only” rule. The working environment at the clinics, and the short surgical times for these cases, may be the most important contributors to the BBL mortality in South Florida.
Özet
Arka Plan
Brezilya popo kaldırma (BBL) ameliyatı, son on yılda en hızlı büyüyen estetik cerrahi operasyon olmuştur. Pulmoner yağ embolisi nedeniyle (PFE) ölüm riski 2017 yılı itibariyle belirlendi ve BBL, estetik cerrahi operasyonlar arasında en yüksek ölüm oranına sahip oldu. Güney Florida, ülkedeki açık ara en yüksek BBL ölüm oranını taşımaktadır.
Amaçlar
Bu çalışmanın amacı, Güney Florida'yı BBL mortalitesi açısından aykırı değer yapan faktörleri araştırmaktı.
Yöntemler
BBL ameliyatı sonrası ölen 11 kişinin yapılan otopsiden (22 kalça) alınan gluteal diseksiyonların anatomik bulguları ortaklıklar açısından değerlendirildi. Ortak noktaları belirlemek için BBL ile ilişkili yağ embolisinden ölen hastaların kamuya açık kayıtları incelenmiştir.
Sonuçlar
Tüm BBL PFE vakalarında, birden fazla farklı seviyede gluteal kas sistemine enjekte edilen yağ greftleri vardı. Diğer bir ortak nokta, ameliyatın yapıldığı yerdi ve hastaların büyük çoğunluğu (%92) Güney Florida'da bulunan yüksek hacimli, bütçeye uygun kliniklerde ameliyat oluyordu. Yaklaşık 90 dakikalık kısa cerrahi süreleri bu vakalar için normal gibi görünüyordu.
Sonuçlar
Güney Florida'da, 2010 - 2022 yılları arasında BBL ile ilişkili 25 yağ emboli ölüm vakası yaşandı; ancak bunların 14'ü, Estetik Cerrahi Eğitim ve Araştırma Vakfı'nın 2018 yönergelerinin ve 2019 Florida Tıp Kurulu'nun BBL "yalnızca deri altı" kuralının yayınlanmasından sonra meydana geldi. Kliniklerdeki çalışma ortamı ve bu vakalar için kısa cerrahi süreleri, Güney Florida'daki BBL mortalitesine en önemli katkıda bulunan faktörler olabilir.
Level of Evidence: 4

See the Commentary on this article here.
Gluteal enhancement by means of fat grafting is not a recently developed surgical procedure. Plastic surgeons worldwide have been performing this surgery for almost 40 years, following the description of the modern version of the procedure by Toledo.1 Early accounts point towards this being a strictly subcutaneous operation with a relatively low associated morbidity and mortality. The typical fat volumes transferred also appear to have been relatively modest in relation to today’s average transfer volumes. By the turn of the century, the procedure had come to be known as the “Brazilian butt lift” (BBL),2 and soon thereafter became one of the most sought-after aesthetic body contouring procedures in the United States.
This surge was driven by the evolving aesthetic ideals of US women from the thin, athletic, “hard bodies” of the 1990s, to the fuller, more voluptuous figures exemplified by several well-known celebrities. In addition, many women now choose to emphasize aesthetically attractive ethnic traits such as wider hips and fuller buttocks.3 Social media has also played a major role in popularizing these silhouettes.
As fat transfer volumes increased to a level that surgeons once thought would overwhelm the subcutaneous recipient site, surgeons began grafting deeper into the well-vascularized gluteal musculature. These techniques of “intramuscular fat grafting” allowed for large-volume fat transfers to be injected into a well-perfused recipient site, theoretically resulting in a higher percentage survival of the grafted fat. Surgeons with expertise in gluteal contouring surgery developed techniques for intramuscular fat grafting4–6 and delineated what were at the time thought to be “safe areas” for fat grafting within the gluteal musculature.7 However, since then, detailed MRI venography studies of the gluteal venous system and subsequent postmortem exams suggest that there really is no “safe zone” for fat grafting in the intramuscular or submuscular plane.8 During the decade between 2010 and 2021, BBL surgery was one of the fastest growing procedures in aesthetic surgery.9 Unfortunately, with the increase in cases came an unprecedented surge in the mortality associated with this procedure.
Understanding the Mortality Associated With BBL Surgery
In 2015, Cárdenas-Camarena et al reviewed the experience of plastic surgeons in Mexico and Colombia over the past 10 and 15 years, respectively, and identified 13 pulmonary fat emboli (PFE) deaths in Mexico and 9 PFE deaths in Colombia after gluteal fat grafting.10 They analyzed the autopsy findings and found that all the deaths were associated with intramuscular fat grafting. For the first time, the danger of grafting fat into the gluteal muscles was recognized and these authors recommended surgeons avoid fat graft injections into the deep gluteal muscle.
In July 2016, the Aesthetic Surgery Education and Research Foundation (ASERF) sent a gluteal fat grafting survey (Supplemental Appendix) to all active members of The Aesthetic Society and the International Society for Aesthetic Plastic Surgery (4843 questionnaires). A total of 692 surgeons responded (14.3%) on 198,857 cases. The survey asked members if they were aware of any BBL deaths, and from the answers estimated the mortality to be between 1/2351 and 1/6241, earning BBL notoriety as the deadliest procedure in plastic surgery.11 This survey raised the alarm about BBL deaths, with many voices in plastic surgery asking if this procedure was too risky to perform.12 Media reports documented that, in 2017, 5 deaths following BBL had occurred in South Florida alone.
The focus thus shifted to South Florida as the site with the highest number of BBL deaths in the United States. The Miami-Dade Medical Examiner determined the cause of death for these patients to be PFE. The postmortem results confirmed a 2-factor hypothesis for this fatal complication: fat must be injected into the gluteal muscles and a gluteal vein injury must be present. These events can occur when fat is injected under the deep gluteal fascia into the gluteus maximus and when the fat grafting cannula inadvertently injures an intramuscular or submuscular gluteal vein, creating a route for the fat graft to enter the venous system and travel to the heart and lungs with fatal results.
To study the factors associated with this unusually high mortality rate, ASERF created an international intersociety work group called the Gluteal Fat Grafting Task Force. Both authors served as consultants to this task force. Under the direction of Peter Rubin, MD, the task force convened in Miami in 2017 (Figure 1). Its goal was to create an appropriate anatomic model to study the pathophysiology behind these deaths, identify contributing anatomic factors, and determine safer fat graft injection techniques.
Figure 1.
Model validation team: Drs Onelio Garcia Jr., Joseph Finocchiaro, Richard D’Amico, Justin Fraioli, J. Peter Rubin, Pat Pazmiño, and David Turer.
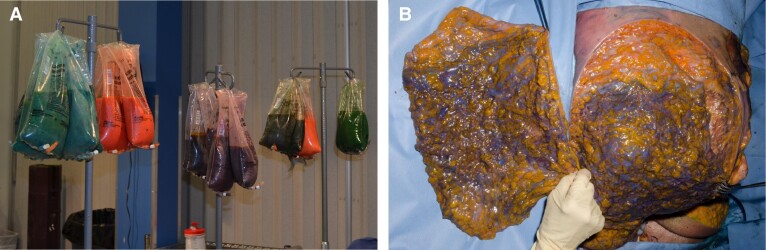
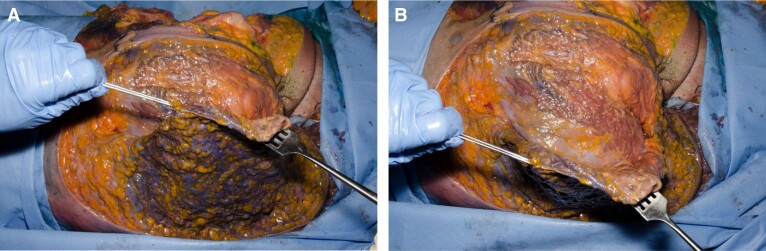
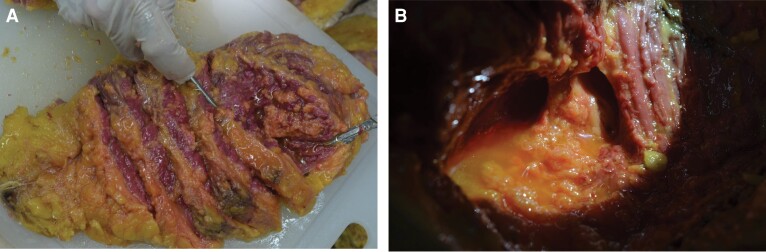
The central hypothesis for this study was that “safe approaches for gluteal fat grafting could be delineated by modeling the operation in commercial cadavers.” Once the commercial cadaver model was validated, 2 separate sessions were scheduled with invited surgeons, who performed their usual BBL techniques under video fluoroscopic monitoring and used color-coded human supernatant fat to track fat graft dispersion (Figure 2A). Upon completion of the fat grafting sessions, the buttocks were systematically dissected, and the colored fat dispersion documented by high-resolution photography (Figure 2B). All invited surgeons, who intended to fat graft only within the subcutaneous space, were able to do so, even when injecting large volumes (>1000 mL) into each buttock (Figure 3A,B). The 3 most important safety recommendations derived from these cadaver studies were: (1) fat graft should only be injected into the subcutaneous space; (2) surgeons should avoid injecting at a downward angle; and (3) surgeons should use a stiff cannula (≥4 mm) to avoid the cannula bending seen with thinner cannulas that can lead to an inadvertent deep misplacement of the cannula tip.
Figure 2.
(A) Dyed human supernatant fat from liposuction and (B) color-coded fat graft within the subcutaneous space following gluteal injections.
Figure 3.
(A) Invited injectors stayed in the subcutaneous plane, even when injecting large volumes (>1000 mL/buttock). (B) Note that all color-coded fat is superficial to the deep gluteal fascia/muscle fascia.
In 2018, ASERF compiled the information acquired from these cadaver studies to publish a set of 10 guidelines that emphasized the subcutaneous-only injection technique with recommendations that focused on cannula awareness during fat grafting: using a stiff cannula (>4 mm), avoiding a Luer-Lock interface to prevent inadvertent cannula misguidance, preferring intergluteal (sacral) incisions, and continuous tactile awareness of the cannula tip. These practice guidelines were widely distributed throughout 2018 to all members of The Aesthetic Society, the American Society of Plastic Surgeons (ASPS), the International Society of Aesthetic Plastic Surgery (ISAPS), and other international plastic surgery societies.13
In early May 2019, ASERF repeated the gluteal fat grafting online survey by sending 5048 invitations; 572 responses (11.3%) were received from plastic surgeons reporting on 29,843 cases. This second survey demonstrated that the societies’ education campaigns had been remarkably successful in that 94% of respondents noted that they were aware of the new safety recommendations and 86% of respondents were now only fat grafting in the subcutaneous plane. This survey asked respondents if they were aware of any new BBL deaths, and estimated that by 2019, the BBL mortality rate had dropped to 1/14,921, which if accurate, would have surpassed the safety profile of abdominoplasty (1/13,193 at the time of the survey).14
In April 2019, the Florida Board of Medicine (FL BoM) held a special session to discuss the high mortality rate of BBL surgery in the state. One author (O.G.) appeared before the FL BoM on behalf of the Florida Society of Plastic Surgeons. During this meeting, the FL BoM affirmed that the standard of care for gluteal fat grafting in 2019 was a “subcutaneous-only injection” technique and then drafted the June 2019 emergency rule which mandated gluteal fat grafting to the subcutaneous space (above the deep gluteal fascia). The BoM noted that physicians who injected fat graft under the deep gluteal fascia or into the gluteal muscles would be subject to disciplinary action, including the loss of their medical licenses.15
By 2019, Florida surgeons were well aware that the standard of care for safe gluteal fat grafting was a “subcutaneous-only injection” technique. The major plastic surgery societies, armed with information gathered from cadaver laboratories and postmortem examinations, disseminated appropriate BBL guidelines to their membership. By June 2019, the FL BoM had introduced its “subcutaneous-only injection” mandate and forwarded alerts to every licensed physician in the state. One would assume that because of all these advances, BBL-related deaths would have decreased since 2019. However, unfortunately, in South Florida, the opposite happened.
METHODS
By 2017, the Chief Medical Examiner at the Miami-Dade Medical Examiner’s Office, Dr Emma Lew, and her staff of medical examiners, had become the foremost authority on BBL-associated PFE deaths. She was invited to the Gluteal Task Force commercial cadaver injection sessions so that she could witness the mechanism of injury resulting in PFE during BBL procedures. She, in turn, invited the authors to advise on the surgical aspects of the gluteal dissections at the Miami-Dade Medical Examiner’s Office.
After the Medical Examiner completed the routine autopsy, a detailed gluteal dissection was performed to determine if fat grafts were present within the gluteal muscles and to look for evidence of any vascular injuries to explain the cause and mechanism of death. The authors observed 11 postmortem gluteal dissections (22 hemibuttocks).
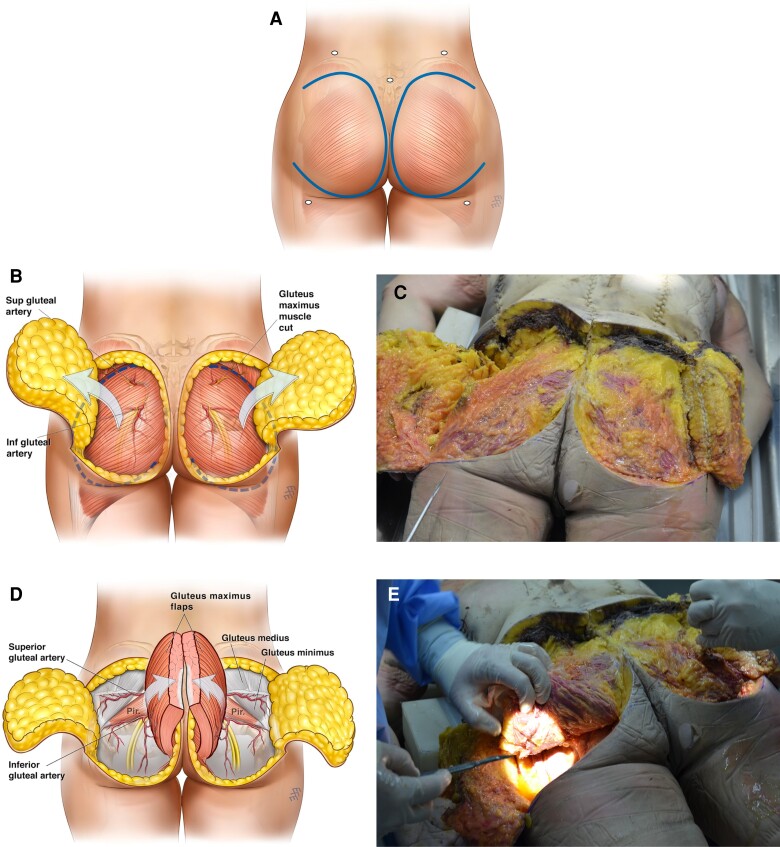
A standardized “gluteal butterfly” dissection technique, described by the authors, was used in these dissections. Circumlinear incisions are first made to create skin and subcutaneous flaps that are based laterally on the outer thigh. Care is taken not to incorporate the patient’s surgical access incisions in this skin flap (Figure 4A). The dissection is continued through the epidermis, dermis, superficial subcutaneous fat, superficial gluteal fascia, and deep subcutaneous fat, until the deep gluteal fascia that is adherent to the external surface of the gluteus maximus is reached. At this level, the skin-subcutaneous flap is elevated off the deep gluteal fascia, and displaced laterally, exposing the surface of the deep gluteal fascia and the muscle belly of the gluteus maximus underneath (Figure 4B). The gluteus maximus is then detached from its lateral insertions and reflected medially, exposing the submuscular vasculature (Figure 4C). At this time, care is taken to examine the superior and inferior gluteal vessels and their tributaries within the muscle for the presence of fat graft and vessel injuries. After this exam, the skin-subcutaneous flap and the muscle belly of the gluteus maximus receive “bread loaf” incisions to identify fat graft within these structures (Figure 4D,E). The authors also reviewed the publicly available autopsy records and corresponding media reports of these deaths to identify commonalities.
Figure 4.
Gluteal butterfly autopsy technique. (A) Step 1: initial skin incision of laterally based cutaneous flaps. (B) Step 2: the skin-subcutaneous flap is dissected from medial to lateral, exposing the deep gluteal fascia and the muscle belly of the gluteus maximus underneath the fascia. (C) The exposed deep gluteal fascia is seen at autopsy. (D) Step 3: the gluteus maximus is detached from lateral attachments and trochanter and reflected medially, exposing the gluteal arteries and veins. (E) Underbelly of gluteus maximus and exposed gluteal vessels noted at autopsy. (F) Step 4: the gluteus maximus muscle belly is cut horizontally in a bread-loaf fashion to document the fat graft position within the muscle belly. (G) Horizontal breadloaf incisions through the gluteus maximus muscle belly are shown at autopsy. (H, I) Close-up views of incised muscle belly with intramuscular fat grafts oriented in tracts within the multiple cannula tunnels. Artwork created by and published with permission from Dr Levent Efe, CMI.
RESULTS
A total of 25 PFE BBL deaths were recorded between January 2010 and April 2022 in South Florida alone (other BBL deaths from sepsis, intestinal perforation, thromboembolic pulmonary emboli, severe anemia, and cardiac events were noted but remain outside the scope of this study). Details of these deaths are given in Table 1.
Table 1.
Demographics of South Florida BBL PFE Fatalities
| Surgery date | Age (decade) | BMI (kg/m2) | ABPS surgeon | Budget clinic | Cause of death |
|---|---|---|---|---|---|
| 2010.12 | 30-40 | 24.4 | No | Yes | PFE |
| 2011.06 | 30-40 | 29.3 | No | Yes | PFE |
| 2012.03 | 30-40 | 23.4 | Yes | Yes | PFE |
| 2013.07 | 50-60 | 31.1 | No | Yes | PFE |
| 2015.07 | 50-60 | 32.2 | Yes | Yes | PFE |
| 2016.05 | 20-30 | 27.8 | No | Yes | PFE |
| 2017.03 | 30-40 | 29.8 | Yes | Yes | PFE |
| 2017.03 | 20-30 | 25.5 | BE | Yes | PFE |
| 2017.04 | 30-40 | 22.8 | BE | Yes | PFE |
| 2017.06 | 30-40 | 30 | No | Yes | PFE |
| 2017.12 | 40-50 | 30.4 | No | Yes | PFE |
| 2018.06 | 30-40 | 29.1 | Yes | Yes | PFE |
| 2018.09 | 50-60 | 34.3 | Yes | No | PFE |
| 2019.05 | 20-30 | 30.2 | Yes | Yes | PFE |
| 2019.08 | 20-30 | 27.33 | Yes | No | PFE |
| 2020.09 | 40-50 | 28.2 | Yes | Yes | PFE |
| 2021.01 | 30-40 | 27.42 | Yes | Yes | PFE |
| 2021.01 | 20-30 | 30 | Yes | Yes | PFE |
| 2021.03 | 40-50 | 42 | No | Yes | PFE |
| 2021.05 | 30-40 | 36.9 | Yes | Yes | PFE |
| 2021.06 | 30-40 | 36 | Yes | Yes | PFE |
| 2021.06 | 40-50 | 37.8 | Yes | Yes | PFE |
| 2022.02 | NA | NA | Yes | Yes | PFE |
| 2022.04 | 40-50 | 42 | Yes | Yes | PFE |
| 37 | 31.0 |
Total PFE deaths, 25; ABPS deaths, 17 (17/25 = 68%); deaths in budget clinics, 23 (23/25 = 92%). ABPS, American Board of Plastic Surgery; BBL, Brazilian butt lift; BE, board eligible, PFE, pulmonary fat emboli; NA, not available.
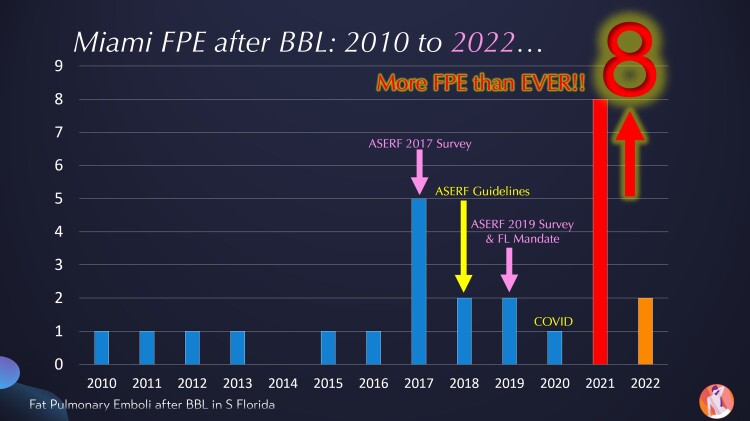
From 2010 to 2016, an average of 1 BBL PFE-associated death per year was recorded. The 7 deaths between 2017 and 2018 raised alarms in the state and prompted the FL BoM to pass the 2019 emergency rule restricting gluteal fat grafting to the subcutaneous space. Unfortunately, neither the ASERF recommendations nor the 2019 Florida emergency rule improved BBL PFE-associated mortality. In fact, the years following these safety recommendations and the subcutaneous-only rule have been the deadliest ever. There have been 14 deaths recorded in Florida since the ASERF guidelines and 12 deaths since the 2019 “subcutaneous-only injection” emergency rule was enacted. The worst year by far was 2021, with a total of 6 BBL PFE deaths and 2 nonfatal cases of BBL PFE(Figure 5).
Figure 5.
There have been 25 PFE BBL-related deaths in South Florida between 2010 and 2022. Fourteen of the deaths have occurred since the ASERF guidelines were published. Twelve of the deaths have occurred since the ASERF 2019 survey that depicted a better mortality rate than abdominoplasty and the Florida Board of Medicine BBL mandate. 2021 was the deadliest year so far, with at least 6 BBL PFE deaths and 2 nonfatal BBL PFE cases confirmed. ASERF, Aesthetic Surgery Education and Research Foundation; BBL, Brazilian butt lift; PFE, pulmonary fat emboli.
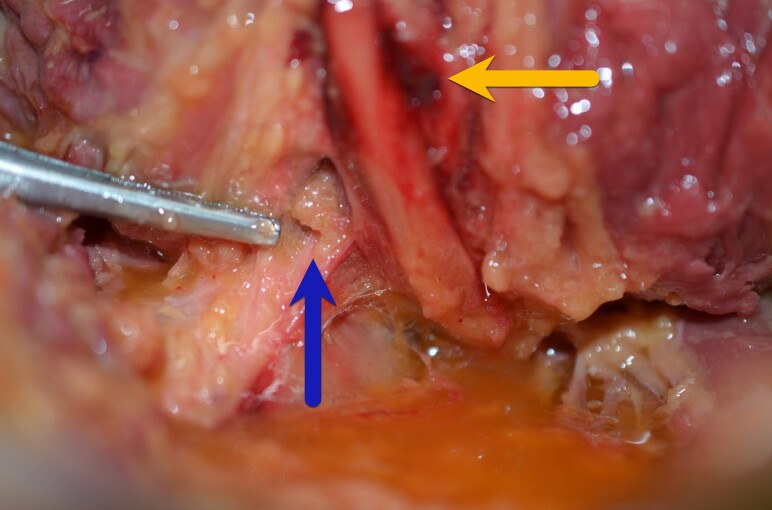
Typical findings in the postmortem gluteal dissections included a zone of vascular injury adjacent to the gluteal vessels (Figure 6) and numerous fat grafts, injected at multiple levels within the muscle and in the submuscular space. Like all human muscles, gluteal muscles do not have intramuscular fat. A patient where fat graft is noted throughout the subcutaneous flap but not within the gluteal muscle belly received “subcutaneous-only” fat graft injections. A patient with fat graft within the gluteal muscle belly received an intramuscular fat graft injection. In some dissections, the application of pressure to the infragluteal fold resulted in the flow of free fat graft from the inferior muscle belly into the submuscular space (Figure 7). This may explain why in several of the BBL deaths, the operating surgeons noted that the patient arrested at the end of the surgery, shortly after turning the patient from the prone to the supine position. This usually benign maneuver could place significant pressure on the lower buttocks, allowing the free fat grafts to migrate from a submuscular position to where the concomitant vessel injury is located.
Figure 6.
Close-up view of the gluteal vessels with the gluteus maximus muscle reflected medially. Note the zone of injury near the vessels (yellow arrow) and free fat grafts adjacent to the vessels (blue arrow), in the submuscular space.
Figure 7.
Pressure on the lower buttocks of post–Brazilian butt lift patients results in rapid flow of free fat grafts into the submuscular space.
BBL surgery is a “blind” procedure performed by tactile feel. All indications from recent studies point to subcutaneous fat grafting as the only safe technique to avoid PFE complications.16–20 As previously mentioned, the autopsy findings in these BBL-associated deaths are not consistent with a “few inadvertent passes” of the grafting cannula into the muscle. Assuming the surgeons involved in these deaths were genuinely trying to inject only into the subcutaneous space, then the only logical explanation for the postmortem findings is that they completely lost tactile perception as to the location of the tip of their injection cannula or were so inexperienced with the procedure that they could not recognize the proper anatomic space.
DISCUSSION
Although this paper has focused on the 25 BBL PFE deaths in South Florida, our community has seen even more BBL deaths from other causes such as sepsis, anemia (hemoglobin <3 g/dL), bowel and organ perforation, ischemic strokes, thromboembolic pulmonary emboli, and cardiac events. We identified 1 non-BBL PFE death during this period. This is consistent with the exceedingly rare risk of a microfat embolism from liposuction alone, calculated to be 1 in 18,868 or 0.0053% by Hughes in an ASAPS survey of 94,000 liposuction cases.21
We have also confirmed 2 nonfatal PFE cases, where the patients survived after extracorporeal membrane oxygenation, craniotomy (a BBL patient with a patent foramen ovale where fat embolized to the brain), and intensive care but remained with serious debilitating sequelae.
In our community, these BBL PFE deaths are only the tip of the BBL morbidity iceberg. South Florida emergency departments have seen sharp rises in serious BBL complications including acute anemia, hypovolemia, bowel perforations, liver lacerations, bladder injuries, pneumothoraces, major vascular injuries, and sciatic nerve injury with infection (after a cannula that had perforated the small intestine was used to graft fat submuscularly into the sciatic nerve). This paper, however, focused only on PFE mortality because it is unique to this procedure, the cause of death can be established by autopsy, because of the high attention it has garnered within our community and our specialty, and most importantly, because the authors strongly believe that it can be prevented.
The Florida plastic surgeons responsible for these deaths were aware of the subcutaneous-only gluteal fat graft recommendations. They documented their “subcutaneous-only” approach and the multiple precautions they took to stay subcutaneous.22 And yet, despite these efforts, the autopsies noted that each of these surgeons injected fat graft intramuscularly and deaths from PFE are now occurring at a higher rate than when the pathophysiology was not as well understood.
Postmortem Findings Reveal Injection Technique
During the 2019 ASPS Breast Surgery and Body Contouring Symposium, Dr Alan Matarasso, the president of the ASPS, noted that the “BBL is the only aesthetic procedure that has its own autopsy technique.” The gluteal butterfly autopsy technique illustrated above allowed for consistent dissections in the cadaver laboratory and morgue. The autopsies confirmed the 2-factor hypothesis for PFE after gluteal fat grafting—fat must be injected into the muscle and a vessel injury must be present. As the location and arborization of the vascular tree is variable between patients, surgeons cannot reliably prevent an PFE by relying on surface anatomy to avoid the putative positions of the inferior and superior gluteal vein trunks.8 The factor that a surgeon can control is to avoid injecting into the gluteal muscle at all times. This can be accomplished by consistently visualizing the subcutaneous position of the cannula tip before fat injection.
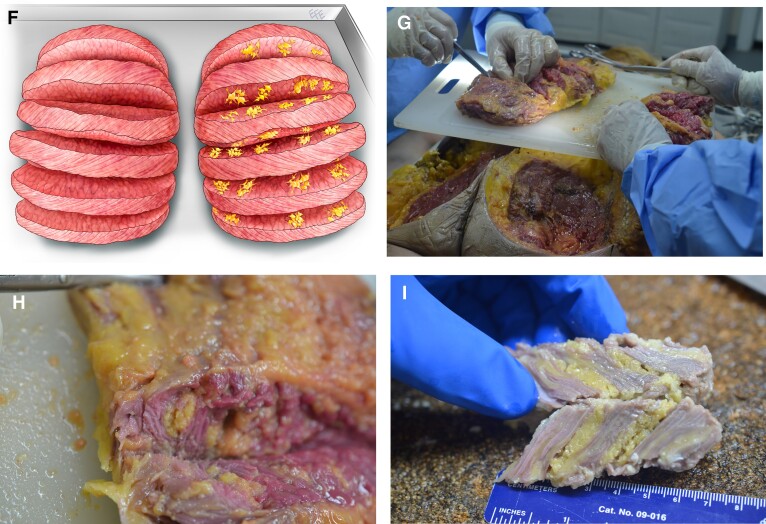
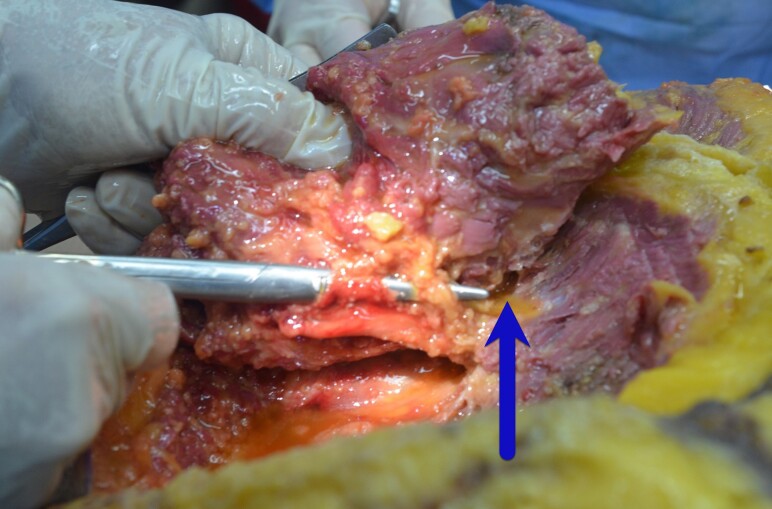
Common findings in the postmortem gluteal dissections included a typical zone of injury adjacent to the gluteal vessels, submuscular fat graft, and tracts of fat graft at multiple sites and levels coursing horizontally (parallel to the muscle belly) through the gluteal muscles (Figure 8). These multiple horizontal tracts of fat graft at different sites and levels reveal the path of the intramuscular cannula as it was depositing fat graft within the gluteal muscle (Figure 9A,B). What was never noted in the postmortem exams was a collection of fat graft directly under the deep gluteal fascia or fat graft that began just under the deep gluteal fascia and radiated vertically deep into the muscle belly. Those findings would have been expected if subcutaneous fat graft had leaked through defects within the deep gluteal fascia and entered the gluteal muscle belly. The actual postmortem findings are not consistent with intramuscular fat graft as the result of 1 or 2 inadvertent cannula passes or subcutaneous fat graft that leaked into the muscle belly through a small perforation of the deep gluteal fascia. The postmortem findings document that the surgeon had performed an intramuscular fat graft technique, whether intentionally or the result of not being aware of the intramuscular position of the cannula at the time of injection.
Figure 8.
Cannula tracts are identified deep in the muscle adjacent to the gluteal vessels. Note the free fat grafts (blue arrow), in proximity to the vessels.
Figure 9.
(A) Bread-loafed gluteus maximus muscle displays multiple injection tunnels within the muscle with widely disseminated fat grafts within the muscle. (B) Close-up photograph of the typical cannula tunnels within the gluteus maximus muscle.
These postmortem findings are consistent with the dynamic cadaver studies completed by Del Vecchio et al, who proved that subcutaneous fat graft could not migrate through a perforation in the deep gluteal fascia caused by a cannula and that subcutaneous fat graft could only pass through the deep gluteal fascia if there was a large defect (>1 cm), such as when they created defects in the deep gluteal fascia with a biopsy instrument.23,24 Surgeons should take comfort that the postmortem findings and cadaver studies concur that subcutaneous fat graft will not migrate into gluteal muscle belly, even if there are small cannula perforations in the deep gluteal fascia.
BBL Surgeon and Facility as Mortality Risk Factors
South Florida is home to a diverse medical community, and we are often asked about the distribution of BBL deaths among American Board of Plastic Surgery (ABPS) board-certified plastic surgeons and other physicians. We noted that between 2010 and 2022, 9 physicians who were not ABPS board-certified had a documented BBL PFE death, but more importantly, 17 ABPS board-certified plastic surgeons had a BBL PFE death. Board-certified plastic surgeons were responsible for more than two-thirds (68%) of the BBL PFE deaths in South Florida. This is directly and adversely affecting our specialty.
More importantly, of the 25 BBL PFE-associated deaths, 23 of the surgeries (92%) were performed at high-volume, budget clinics. Two of the deaths were attributed to an outlier ABPS surgeon who has had 3 deaths from body contouring procedures (2 BBL-associated) along with numerous other serious body contouring complications (Table 2).
Table 2.
Location of Surgery for the 25 South Florida BBL PFE-Associated Deaths 2010 to 2022
| Location | No. (%) of deaths |
|---|---|
| Low-budget, high-volume clinics | 23 (92%) |
| Single ABPS plastic surgeon (3 confirmed body contouring deaths, 2 BBLs) | 2 (8%) |
ABPS, American Board of Plastic Surgery; BBL, Brazilian butt lift.
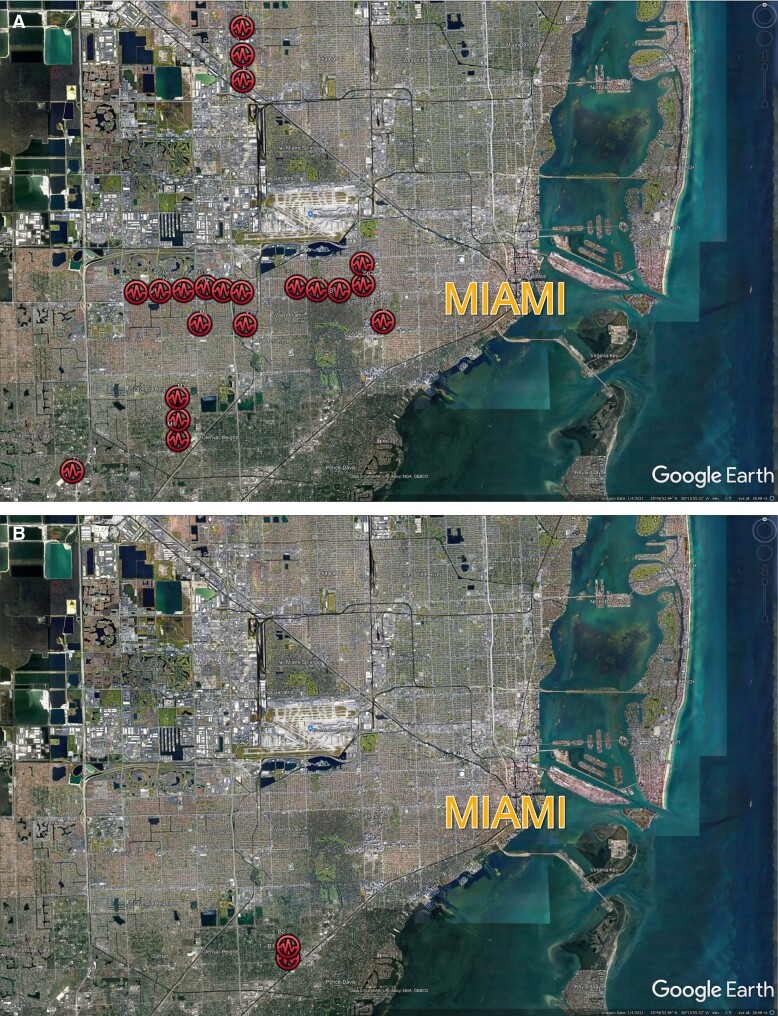
These findings highlight the fact that proper surgeon credentials, such as ABPS board certification, are not on their own protective. In South Florida, a more important correlation is where the surgery was performed, as ABPS surgeons and non-ABPS physicians working at high-volume, budget clinics accounted for 92% of these BBL PFE deaths. Mapping the location of these deaths highlights this striking risk factor (Figure 10A,B).
Figure 10.
(A) Brazilian butt lift pulmonary fat emboli deaths in high-volume budget clinics. (B) Brazilian butt lift pulmonary fat emboli deaths not in high-volume budget clinics. Imagery used in accordance with copyright permission, 2022 TerraMetrics, Map Data 2022 Google.
South Florida BBL PFE Mortality
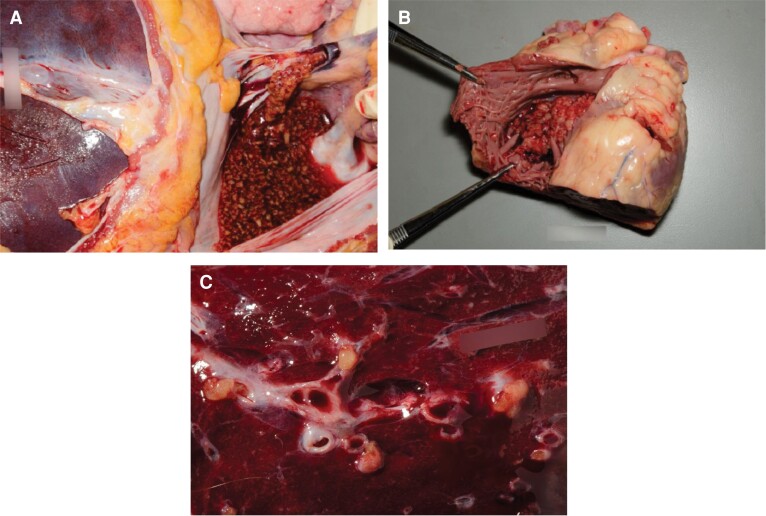
By 2017, it had become increasingly clear that the most common cause of death from BBL was an PFE. The physiologic and clinical differences between macrofat emboli and microfat emboli syndrome were well described in the literature.25,26 Microfat emboli syndrome carries a reported mortality in the 10% to 30% range.27,28 A delay in treatment of the syndrome is associated with a 35% mortality,29 which may be a frequent occurrence in the plastic surgery population undergoing outpatient surgery. Macrofat pulmonary emboli following BBL surgery, however, is almost always a fatal event. A 2018 publication reviewing 16 BBL deaths found that 50% of the patients died on the operating table, and the other 50% were dead within 3 hours after surgery.30 Since that report, there have been 3 reported cases of survival (2 of these cases occurred in South Florida) following macrofat emboli associated with BBL surgery (2 patients with macrofat pulmonary emboli; 1 patient with patent foramen ovale and a cerebral fat embolism).31,32 The most important commonality among these survival cases was extremely rapid access to intensive care at a tertiary care facility, with in-house specialists and the availability of extracorporeal membrane oxygenation devices. Despite these heroic, life-saving measures, all 3 surviving patients suffered serious debilitating sequelae from their fat emboli episode. Because the majority of BBL surgeries take place in office-based operating rooms and outpatient surgery centers, it is highly unlikely that these conditions, necessary for the slimmest chance of survival, will present themselves. It is more accurate to say that that the large amounts of fat graft seen in the heart, major vessels, and lungs of BBL PFE patients are incompatible with life (Figure 11A-C).
Figure 11.
(A) Fat graft pouring out of vena cava. Fat graft entered the venous system and coalesced into a thrombus in the vena cava and the pulmonary arteries, giving it a more solid appearance than the loose fat graft that was injected in the subcutaneous space and intramuscular layers. (B) Fat graft within the right atrium. (C) Fat emboli within lung parenchyma.
The mortality rate for BBLs has been difficult to estimate. In May 2019, ASERF repeated its online survey and noted that 94% of respondents were aware of the 2018 ASERF recommendations and understood the dangers of intramuscular gluteal fat grafting, and that 86% of surgeons reported utilizing a subcutaneous-only injection technique at the time. The survey also noted that in the United States and internationally, “Two fatal PFEs were reported in the last 24 months (time between the 2017-2019 surveys).”14 Unfortunately, this did not correlate with the South Florida experience where at least 8 autopsy reports documented BBL PFE deaths in that same period!
Although the autopsy-documented BBL PFE deaths in South Florida are a startling numerator, it is difficult for us describe the denominator in our mortality rate because many of these cases are performed in high-volume, budget clinics that do not report their numbers or the person who actually performed the procedure. The 2019 ASERF survey calculated the BBL mortality rate by asking respondents if they were aware of a BBL death and then dividing it by the estimated number of BBLs performed. From these data, this survey described the mortality rate of a BBL surgery as 1/14,921, lower than that of an abdominoplasty at 1/13,193 in 2019. A more recent, 2020 article described the mortality rate of abdominoplasty at 1/13,000 and that of BBL at 1/20,000.33
Nevertheless, the comparison to abdominoplasty is not favorable. Although recent literature34 depicts a favorable comparison in mortality rates of BBL surgery vs abdominoplasty, that does not appear to be the case in South Florida. According to the statistics from The Aesthetic Society, plastic surgeons perform abdominoplasty surgery at least 4 times more frequently than BBL surgery. Approximately 243,000 abdominoplasties were reported in the 2020 to 2021 statistics, whereas approximately 61,000 buttock augmentations were reported during the same period (the buttock data included both fat grafting and implants).9 However, in South Florida, abdominoplasty-related deaths are rare in comparison to BBL-related deaths. For example, there were 31 BBL-related (PFE + non-PFE) deaths in Florida between 2010 and 2022. Applying the 4:1 ratio of abdominoplasties to BBLs reported in The Aesthetic Society statistics, one would expect approximately 124 abdominoplasty-related deaths in South Florida during that same period for the mortality rates to be comparable. There have been 13 BBL-related (PFE + non-PFE) deaths in South Florida in the past 3 years (2019-2022). In a procedure with a higher reported mortality rate, which is performed at least 4 times more commonly than BBL surgery, one should expect approximately 52 deaths during that same 3-year period. However, the numbers are not even close: abdominoplasty-related deaths in the area are in single-digit numbers over the same period, including the fact that some of the deaths were the result of diagnosed pulmonary emboli and were not pursued by the Medical Examiner’s Office.
The Unique South Florida Experience
Why is South Florida different from the rest of the country regarding BBL mortality? It is striking that 92% of these deaths in South Florida occurred in the high-volume, budget clinics, mostly owned, and operated, by businessmen, often with criminal records.35 These clinics are in fierce competition to offer the lowest prices through internet and social media marketing, mostly to out-of-town patients. The attraction for out-of-town patients is easy to understand. At the time of this writing, a Google search for “bbl price Miami” reveals high-volume, budget clinics offering the procedure for only US$2900. The only way to remain profitable at this price point is for a clinic to perform as many procedures as possible, as quickly as possible, and minimize patient interaction.
This high-volume, minimal-patient-interaction practice model is best described by the surgeons who work there. In a single meeting this year, the FL BoM disciplined 3 surgeons who each had a BBL PFE death: Surgeon A (ABPS board-certified), Surgeon B (ABPS board-certified) and Surgeon C (no board certification). In the meeting’s public documents, Surgeon A stated in a deposition that he only had a “slight” independent recollection of his patient who died from a BBL PFE, that he did not participate in the preoperative history and physical, did not review the surgical procedure, and was not involved in preoperative or postoperative teaching, consent, or overview. He also testified that the first time he met the patient was the day of surgery, shortly before the procedure began.22
For Surgeon B, the FL BoM public documents note that: “This case has confirmed for him that it is simply too difficult to ensure during this blind procedure that he is in the appropriate place, and thus it is not a procedure he wants to perform again.” Surgeon B also addressed the fact that this BBL was his seventh surgery that day and that surgery had started at 8:31 pm,36 but he “has changed his practice to try and ensure this never happens again. Most importantly, he will no longer plan to start procedures after 6 pm.”22,37 The FL BoM placed a restriction on Surgeon A prohibiting him from doing BBLs for 1 year, Surgeon B received a permanent restriction on his medical license that restricts him from ever doing a BBL for the rest of his career, and Surgeon C had his medical license revoked.37,38
Surgeon B’s BBL PFE death as the seventh surgery that day highlights that the budget clinic pricing structure is predicated on surgery volume. It is not unusual for surgeons in these clinics to schedule 8 or 10 BBL procedures in 1 day. A recent exposé on these clinics by National Geographic revealed that the surgeon of record runs several operating rooms simultaneously with the surgical assistants performing significant, critical portions of the surgeries.39 It is not protective to the patient if the surgeon is ABPS board-certified if the clinic’s business model does not permit the surgeon to perform all critical parts of the surgery or to interact and care for the patient preoperatively and postoperatively.
And yet despite the high number of patient deaths and disciplinary actions on individual surgeons, very little has changed in the South Florida budget clinics. After a clinic is associated in the media with reports of multiple deaths, the clinic changes its name, but little else. Some clinics have gone through three or four name changes, attracting unknowing patients who would otherwise have avoided the previous clinic names associated with publicized BBL deaths.40 As most of these clinics are owned by businessmen, they cannot be disciplined by the FL BoM, leaving patients at risk and the independent contractor surgeons assuming the exposure.35
A Way Forward
The patience of the Florida community, its legislators, and the FL BoM is wearing thin. Tolerating the high number of BBL-related deaths and maintaining the status quo is not an option. And yet there is debate about how to move forward. Who should be performing these procedures and under what circumstances? Are plastic surgeons even capable of consistently staying in the subcutaneous tissue when fat grafting the buttocks? Will the FL BoM consider the procedure too risky and issue new mandates that restrict or ban BBL surgery altogether?
Having a state board of medicine dictate how surgeons must perform a particular surgery does not set a good precedent for our specialty. The FL BoM felt compelled to act by passing the recent 2022 emergency ruling. It is a fact that BBL-related deaths have significantly increased in South Florida since the 2019 Florida BBL rule went into effect. The number of autopsy reports during that period provide tangible evidence of how serious the situation has become. Many of these deaths have been highly publicized by the local media, prompting community leaders and state legislators to call for a solution to this problem.
The significant anatomic variability of the gluteal venous systems between patients and even between the left and right sides of the same patient has been documented by MRI venography.8 This unpredictable arborization of the venous tree prevents even an expert surgeon from depending on their experience and knowledge of anatomy to consistently avoid all of the gluteal veins in an inadvertent muscle injection when performing a subcutaneous-only fat graft injection. Instructing surgeons on surface anatomy to avoid unpredictable venous structures will not prevent more PFE or patient deaths.
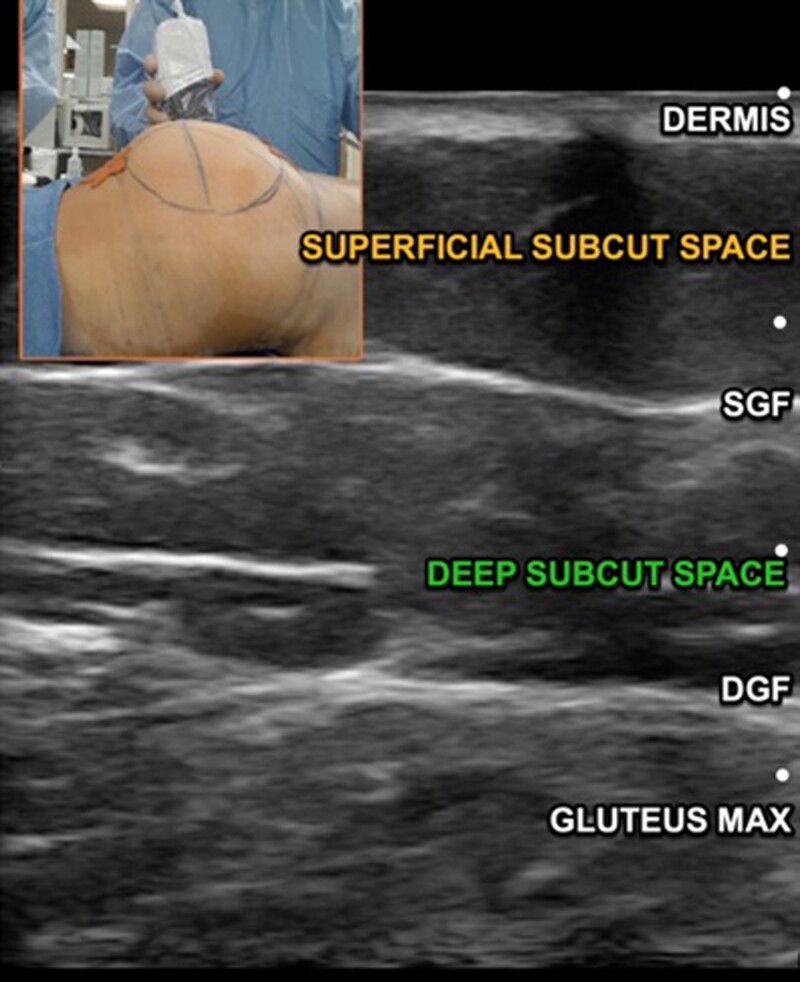
The authors believe that when this procedure is properly performed, with the surgeon adhering to a “subcutaneous-only injection” technique, it is associated with high patient satisfaction while maintaining an acceptable safety profile, equivalent to other common body contouring procedures. Subcutaneous fat grafting can be consistently performed by utilizing technology that confirms the subcutaneous placement of fat graft in every patient. Impedance cannulas that differentiate a subcutaneous from an intramuscular cannula position have been shown to be quite accurate and can be used as a valuable teaching tool.41 A cannula injecting fat graft can also be easily visualized with inexpensive (less than US$3000) hand-held intraoperative ultrasound devices that confirm the precise location of the injection cannula in “real time” during the fat grafting procedure.42 Ultrasound can be used to confirm the subcutaneous position of the cannula tip before any fat graft is injected, ensuring a consistent subcutaneous-only fat injection technique.43 Ultrasound-assisted BBL surgery is gaining popularity among some plastic surgeons. The procedure is extremely precise, safe, and easily taught to a trained plastic surgeon. Intraoperative ultrasound has high resolution and is anatomically accurate (Figure 12). Video of the intraoperative ultrasound can serve as documentation that all fat graft was injected subcutaneously. One of the authors (P.P.) has been a proponent of this method for 9 years and has shared his ultrasound technique with numerous plastic surgeons.43,44
Figure 12.
High-resolution ultrasound image displaying the dermis, superficial subcutaneous space, SGF, deep subcutaneous space, DGF, and gluteus maximus muscle. Florida Board of Medicine 2022 regulations require that all surgeons performing Brazilian butt lift surgery utilize ultrasound guidance to ensure that all fat grafting is performed only above the DGF. DGF, deep gluteal fascia; SGF, superficial gluteal fascia.
Organized plastic surgery can take an active role in hands-on training for ultrasound assisted gluteal fat grafting. The successful implementation of the Ultrasonic-Assisted Liposuction Task Force over 25 years ago serves as a good historical precedent in that respect.45
Recently, some have suggested that the large number of daily cases undertaken by surgeons at the high-volume, budget clinics may be a significant risk factor in the high mortality associated with BBL surgery in South Florida.46 Although the authors are in complete agreement that the extremely high volume of cases that the clinic surgeons are attempting every day are related to the high mortality, simply restricting the daily number of BBL surgeries will not, by itself, solve the problem. The short operative times for many of these cases is truly alarming because they are indicative of a surgical technique at a speed that is at best imprecise, and at worst unsafe. Unfortunately, simply restricting the number of BBL surgeries per day will not translate into an increase in surgical times for these procedures. The high-volume, budget clinics are run under a business model that is predicated on volume surgery. Their current fee structure does not allow for a BBL surgery to take any longer because the profit margin is so narrow that the clinic would lose money on longer cases. A restriction in the number of daily BBL cases would just mean that the rest of the clinic’s surgical schedule would be filled by other surgeries. However, the BBL procedures would still be performed at dangerously fast technical speeds because it is the only way they can financially “make ends meet” under their current pricing structure.
The FL BoM reviewed the impact of its 2019 BBL subcutaneous-only injection rule and the fact that there have been more BBL PFE deaths after the 2019 rule than before the rule went into effect. It is important to note that all surgeons who had a BBL PFE death documented that they thought they only injected fat graft into the subcutaneous space. This confirms that these surgeons were all aware of the FL BoM 2019 mandate and documented that they thought they performed the subcutaneous-only technique appropriately, and yet the blind nature of fat grafting prevented each surgeon from avoiding a PFE fatality. Clearly, documenting the surgeon’s intentions but continuing to operate blindly does not protect the patient. During their June 2022 meeting, the FL BoM deemed the high number of recent BBL deaths to be an emergency and passed an emergency rule that went into effect for 90 days on June 14, 202247 (Standards of Care for Gluteal Fat Grafting Procedures, 64B8-9.009, FAC, Standard of Care for Office Surgery). The rule restricts surgeons to 3 BBL surgeries per day and requires that all BBLs be performed with ultrasound guidance. A time-stamped and dated ultrasound video of the procedure must be kept as part of the patient’s medical records. Ultrasound video would allow the surgeon to document the subcutaneous placement of fat graft in every patient, rather than rely on a surgeon writing that they thought they performed a blind procedure correctly. The 2022 emergency rule went into effect almost 3 years to the date of the original 2019 subcutaneous-only injection rule.37 At the time of this writing, the clinic owners and their surgeons are suing the Florida Department of Health, stating that there is no emergency and that this rule constitutes a restriction of trade.
Lessons From South Florida That Affect the Nation
Common findings among the postmortem examinations of BBL-related deaths included the presence of intramuscular fat graft as horizontal tracts coursing through the muscle. Fat grafts were never noted directly under the deep gluteal fascia or radiating from the deep gluteal fascia into the muscle belly. Intramuscular fat graft was the result of fat graft placed with multiple intramuscular passes of an injection cannula. These findings confirm previous dynamic cadaver studies and can reassure surgeons that fat graft that is only placed within the subcutaneous space will remain there even if the cannula perforated the deep gluteal fascia several times.
The high number of BBL PFE deaths among our patients is a cultural issue among our specialty. Although 92% of these PFE BBL deaths occurred at these high-volume, budget clinics, they would not have occurred without the participation of board-certified plastic surgeons. Aside from the 2 deaths from a single outlier ABPS surgeon, all the other BBL PFE deaths in our community took place at high-volume, budget clinics. South Florida is the epicenter for BBL-related mortality, yet during the 12-year period covered in this paper, not a single BBL PFE death in the area has been attributed to a ABPS board-certified surgeon working in a traditional private practice or an academic setting. It is apparent that factors such as proper training and board certification alone cannot overcome the dangerous working environment associated with the high-volume, budget clinics. Two-thirds of the deaths are attributed to board-certified plastic surgeons working in these budget clinics!
Although BBL-related morbidity is generally associated with South Florida, it affects the entire nation. Plastic surgeons and primary care providers from around the United States routinely call about their patients who traveled to South Florida for a budget BBL, then returned home with serious complications and without reasonable means of contacting the physician who performed the surgery. These issues will only worsen as the high-volume, budget clinics of South Florida are now spreading across the United States, opening offices and bringing their practice model to new American cities.
CONCLUSIONS
After years of postmortem exams, multiple cadaver studies, and case analyses, we now understand the pathophysiology of BBL-related PFE deaths and the risk factors associated with BBL mortality. It is unconscionable to continue with the unacceptably high mortality rate of a purely elective, aesthetic procedure—particularly when we have sound evidence that it can be performed safely by employing recommended techniques. By incorporating inexpensive noninvasive technology, plastic surgeons can document that they are performing this procedure safely, protecting patients and their own medical licenses.
Supplemental Material
This article contains supplemental material located online at www.aestheticsurgeryjournal.com.
Supplementary Material
Acknowledgments
The authors thank Emma Lew, MD, Chief Medical Examiner Miami-Dade County, for her assistance and support with the postmortem gluteal dissections; and J Peter Rubin, MD, for his exceptional leadership as principal investigator for the Gluteal Fat Grafting Task Force Cadaver Studies.
Contributor Information
Pat Pazmiño, Division of Plastic and Reconstructive Surgery, University of Miami Miller School of Medicine, Miami, FL, USA.
Onelio Garcia, Jr., Division of Plastic and Reconstructive Surgery, University of Miami Miller School of Medicine, Miami, FL, USA.
Disclosures
Dr Pazmiño is a consultant to Clarius (Burnaby, Vancouver, Canada). Dr Garcia is a consultant to Mentor Corp. (Irvine, CA), Solta Medical (Hayward, CA), Bard, BD (Murray Hill, NJ), and MTF (Edison, NJ). Drs Pazmiño and Garcia both serve as consultants to the Aesthetic Surgery Education and Research Foundation (ASERF) Gluteal Fat Grafting Task Force.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
- 1. Toledo LS. Gluteal augmentation with fat grafting. The Brazilian buttock technique: 30 years’ experience. Clin Plast Surg. 2015;42(2):253–261. doi: 10.1016/j.cps.2014.12.004 [DOI] [PubMed] [Google Scholar]
- 2. Rhone N. Society's singing a new tune: The derriere is where it's at. Chicago Tribune. Published July 5, 2006. Accessed September 13, 2022. https://www.chicagotribune.com/news/ct-xpm-2006-07-05-0607040287-story.html
- 3. Roberts TL, Weinfeld AB, Bruner TW, Nguyen K. “Universal” and ethnic ideals of beautiful buttocks are best obtained by autologous micro fat grafting and liposuction. Clin Plast Surg. 2006;33(3):371–394. doi: 10.1016/j.cps.2006.05.001 [DOI] [PubMed] [Google Scholar]
- 4. Ali A. Contouring of the gluteal region in women: enhancement and augmentation. Ann Plast Surg. 2011;67(3):209–214. doi: 10.1097/SAP.0B013E318206595B [DOI] [PubMed] [Google Scholar]
- 5. Murillo WL. Buttock augmentation: case studies of fat injection monitored by magnetic resonance imaging. Plast Reconstr Surg. 2004;114(6):1606–1614. doi: 10.1097/01.PRS.0000138760.29273.5D [DOI] [PubMed] [Google Scholar]
- 6. Mendieta CG. Gluteal reshaping . Aesthet Surg J. 2007;27(6):641–655. doi: 10.1016/J.ASJ.2007.09.001 [DOI] [PubMed] [Google Scholar]
- 7. Mendieta C, Stuzin JM. Gluteal augmentation and enhancement of the female silhouette: analysis and technique. Plast Reconstr Surg. 2018;141(2):306–311. doi: 10.1097/PRS.0000000000004094 [DOI] [PubMed] [Google Scholar]
- 8. Turin SY, Fracol M, Keller E, et al. . Gluteal vein anatomy: location, caliber, impact of patient positioning, and implications for fat grafting. Aesthet Surg J. 2020;40(6):642–649. doi: 10.1093/ASJ/SJZ260 [DOI] [PubMed] [Google Scholar]
- 9. The Aesthetic Society’s Cosmetic Surgery National Data Bank: Statistics 2021. Aesthet Surg J. 2022;42(Supplement_1):1–16. doi: 10.1093/asj/sjac116 [DOI] [PubMed] [Google Scholar]
- 10. Cárdenas-Camarena L, Bayter JE, Aguirre-Serrano H, Cuenca-Pardo J. Deaths caused by gluteal lipoinjection: what are we doing wrong? Plast Reconstr Surg. 2015;136(1):58–66. doi: 10.1097/PRS.0000000000001364 [DOI] [PubMed] [Google Scholar]
- 11. Mofid MM, Teitelbaum S, Suissa D, et al. . Report on mortality from gluteal fat grafting: recommendations from the ASERF Task Force. Aesthet Surg J. 2017;37(7):796–806. doi: 10.1093/asj/sjx004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nahai F. Acceptable risk: who decides? Aesthet Surg J. 2017;37(7):852–853. doi: 10.1093/ASJ/SJX087 [DOI] [PubMed] [Google Scholar]
- 13. Mills D, Rubin JP, Saltz R. Fat Grafting to the Buttocks | Urgent Warning to Surgeons Performing Fat Grafting to the Buttocks. American Society of Plastic Surgeons. Published 2018. Accessed September 13, 2022.https://www.plasticsurgery.org/for-medical-professionals/advocacy/key-issues/fat-grafting-to-the-buttocks
- 14. Rios L, Gupta V. Improvement in Brazilian butt lift (BBL) safety with the current recommendations from ASERF, ASAPS, and ISAPS. Aesthet Surg J. 2020;40(8):864–870. doi: 10.1093/asj/sjaa098 [DOI] [PubMed] [Google Scholar]
- 15. Florida Board of Medicine . Accessed July 9, 2022. https://www.flrules.org/Gateway/View_notice.asp? id=22065771
- 16. O’Neill RC, Hanson SE, Reece E, Winocour S. Safety considerations of fat grafting in buttock augmentation. Aesthet Surg J. 2021;41(Supplement_1):S25–S30. doi: 10.1093/asj/sjab092 [DOI] [PubMed] [Google Scholar]
- 17. Turer DM, Rubin JP. Commentary on: safe gluteal fat graft avoiding a vascular or nervous injury: an anatomical study in cadavers. Aesthet Surg J. 2019;39(2):185–186. doi: 10.1093/ASJ/SJY302 [DOI] [PubMed] [Google Scholar]
- 18. Garcia O, Pazmiño P, Turer D, Rubin J. Buttock fat grafting insights from the Multi-Society Task Force (cadaver demo). Presented at: Plastic Surgery, The Meeting 2018; October 1, 2018, Chicago, IL. ASPS; 2018.
- 19. Pane TA. Experience with high-volume buttock fat transfer: a report of 137 cases. Aesthet Surg J. 2019;39(5):526–532. doi: 10.1093/asj/sjy191 [DOI] [PubMed] [Google Scholar]
- 20. Kalaaji A, Dreyer S, Vadseth L, Maric I, Jönsson V, Haukebøe TH. Gluteal augmentation with fat: retrospective safety study and literature review. Aesthet Surg J. 2019;39(3):292–305. doi: 10.1093/ASJ/SJY153 [DOI] [PubMed] [Google Scholar]
- 21. Hughes CE. Reduction of lipoplasty risks and mortality: an ASAPS survey. Aesthet Surg J. 2001;21(2):120–127. doi: 10.1067/MAJ.2001.115166 [DOI] [PubMed] [Google Scholar]
- 22.Florida Board of Medicine Board Meeting, June 3, 2022. Accessed July 9, 2022. https://drive.google.com/file/d/1Kow1fv323GdI2ApEoVlQnKcnipGKTh6w/view
- 23. del Vecchio DA, Villanueva NL, Mohan R, et al. . Clinical implications of gluteal fat graft migration: a dynamic anatomical study. Plast Reconstr Surg. 2018;142(5):1180–1192. doi: 10.1097/PRS.0000000000005020 [DOI] [PubMed] [Google Scholar]
- 24. Wall S, Delvecchio D, Teitelbaum S, et al. . Subcutaneous migration: a dynamic anatomical study of gluteal fat grafting. Plast Reconstr Surg. 2019;143(5):1343–1351. doi: 10.1097/PRS.0000000000005521 [DOI] [PubMed] [Google Scholar]
- 25. Cárdenas-Camarena L, Durán H, Robles-Cervantes JA, Bayter-Marin JE. Critical differences between microscopic (MIFE) and macroscopic (MAFE) fat embolism during liposuction and gluteal lipoinjection. Plast Reconstr Surg. 2018;141(4):880–890. doi: 10.1097/PRS.0000000000004219 [DOI] [PubMed] [Google Scholar]
- 26. Garcia O. Commentary on: the potential role of corticosteroid prophylaxis for the prevention of microscopic fat embolism syndrome in gluteal augmentations. Aesthet Surg J. 2020;40(1):90–92. doi: 10.1093/asj/sjz196 [DOI] [PubMed] [Google Scholar]
- 27. Wang HD, Zheng JH, Deng CL, Liu QY, Yang SL. Fat embolism syndromes following liposuction. Aesthetic Plast Surg. 2008;32(5):731–736. doi: 10.1007/S00266-008-9183-1 [DOI] [PubMed] [Google Scholar]
- 28. Levy D. The fat embolism syndrome. A review. Clin Orthop Relat Res. 1990;261(261):281–286. doi: 10.1097/00003086-199012000-00034 [DOI] [PubMed] [Google Scholar]
- 29. Habashi NM, Andrews PL, Scalea TM. Therapeutic aspects of fat embolism syndrome. Injury. 2006;37(4): S68–S73. doi: 10.1016/j.injury.2006.08.042 [DOI] [PubMed] [Google Scholar]
- 30. Bayter-Marin JE, Cárdenas-Camarena L, Aguirre-Serrano H, Durán H, Ramos-Gallardo G, Robles-Cervantes JA. Understanding fatal fat embolism in gluteal lipoinjection: a review of the medical records and autopsy reports of 16 patients. Plast Reconstr Surg. 2018;142(5):1198–1208. doi: 10.1097/PRS.0000000000004904 [DOI] [PubMed] [Google Scholar]
- 31. Peña W, Cárdenas-Camarena L, Bayter-Marin JE, et al. . Macro fat embolism after gluteal augmentation with fat: first survival case report. Aesthet Surg J. 2019;39(9):NP380–NP383. doi: 10.1093/asj/sjz151 [DOI] [PubMed] [Google Scholar]
- 32. Wolfe EM, Weber LE, Wo LM, et al. . Two cases surviving macro fat emboli complications following gluteal fat grafting. Aesthet Surg J. 2022;42(8):902–906. doi: 10.1093/ASJ/SJAC063 [DOI] [PubMed] [Google Scholar]
- 33. Rohrich RJ, Savetsky IL, Avashia YJ. Assessing cosmetic surgery safety: the evolving data. Plast Reconstr Surg Glob Open. 2020;8(5):2643. doi: 10.1097/GOX.0000000000002643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Vecchio DAD, Wall SJ, Mendieta CG, et al. . Safety comparison of abdominoplasty and Brazilian butt lift: what the literature tells us. Plast Reconstr Surg. 2021;148(6):1270–1277. doi: 10.1097/PRS.0000000000008599 [DOI] [PubMed] [Google Scholar]
- 35. Sallah M, Perez M, Reilly S. Felons opened plastic surgery businesses where women died. USA Today. Published April 28, 2020. Accessed July 8, 2022. https://www.usatoday.com/in-depth/news/investigations/2019/04/22/felons-opened-plastic-surgery-businesses-where-women-died/3501970002/
- 36. Neal DJ. State: fatal Brazilian butt lift was day’s 7th illegal surgery by Coral Gables doctor. Miami Herald. Published November 22, 2021. Accessed July 8, 2022.https://www.miamiherald.com/news/health-care/article256016237.html#storylink=cpy
- 37. Masihy M. Florida Board of Medicine takes action following Brazilian butt lift deaths. NBC 6 South Florida. Published June 3, 2022. Accessed July 8, 2022. https://www.nbcmiami.com/investigations/board-takes-action-following-brazilian-butt-lift-deaths/2776749/
- 38. Castillo E. Florida Board of Medicine enforces a daily limit on Brazilian butt lift surgeries. Yahoo News. Published June 22, 2022. Accessed July 9, 2022. https://www.yahoo.com/video/florida-board-medicine-enforces-daily-224257734.html
- 39. van Zeller M. Trafficked with Mariana van Zeller: Black Market Surgery. National Geographic. Published December 1, 2021. Accessed July 9, 2022. https://www.nationalgeographic.com/tv/shows/trafficked-with-mariana-van-zeller/episode-guide/season-02/episode-01-black-market-surgery/vdka25475912
- 40. Chang D. Another patient dies at a Miami cosmetic surgery clinic. Miami Herald. December 15, 2017.
- 41. Turer DM, Qaium EB, Lawrence AM, Clark WW, Rubin JP. A smart sensing cannula for fat grafting. Plast Reconstr Surg. 2019;144(2):385–388. doi: 10.1097/PRS.0000000000005866 [DOI] [PubMed] [Google Scholar]
- 42. Cansancao AL, Condé-Green A, Vidigal RA, Rodriguez RL, D’Amico RA. Real-time ultrasound-assisted gluteal fat grafting. Plast Reconstr Surg. 2018;142(2):372–376. doi: 10.1097/PRS.0000000000004602 [DOI] [PubMed] [Google Scholar]
- 43. Pazmiño P. ultraBBL: Brazilian butt lift using real-time intraoperative ultrasound guidance. In: Ultrasound-Assisted Liposuction. Springer, 2020:147–172. doi: 10.1007/978-3-030-26875-6_10 [DOI] [Google Scholar]
- 44. Thaller S, Panthaki Z. Tips and Tricks in Plastic Surgery. Springer, 2021. doi: 10.1007/978-3-030-78028-9 [DOI] [Google Scholar]
- 45. Fredricks S. Analysis and introduction of a technology: ultrasound-assisted lipoplasty task force. Clin Plast Surg. 1999;26(2):187–204. doi: 10.1016/S0094-1298(20)32604-3 [DOI] [PubMed] [Google Scholar]
- 46. del Vecchio D, Kenkel JM. Practice advisory on gluteal fat grafting. Aesthet Surg J. 2022;42(9):1019-1029. doi: 10.1093/asj/sjac082. [DOI] [PubMed] [Google Scholar]
- 47. [Florida Board of Medicine. 64B8-9.009: Standard of care for office surgery - Florida administrative rules, law, code, register - FAC, FAR, eRulemaking. Florida Administrative Code & Florida Administrative Registrar. Published July 12, 2022. Accessed October 8, 2022.]; https://www.flrules.org/gateway/ruleno.asp?id=64B8-9.009 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.