Abstract
Background
Anxiety and depression are the most common mental disorders worldwide. Owing to the lack of psychiatrists around the world, the incorporation of artificial intelligence (AI) into wearable devices (wearable AI) has been exploited to provide mental health services.
Objective
This review aimed to explore the features of wearable AI used for anxiety and depression to identify application areas and open research issues.
Methods
We searched 8 electronic databases (MEDLINE, PsycINFO, Embase, CINAHL, IEEE Xplore, ACM Digital Library, Scopus, and Google Scholar) and included studies that met the inclusion criteria. Then, we checked the studies that cited the included studies and screened studies that were cited by the included studies. The study selection and data extraction were carried out by 2 reviewers independently. The extracted data were aggregated and summarized using narrative synthesis.
Results
Of the 1203 studies identified, 69 (5.74%) were included in this review. Approximately, two-thirds of the studies used wearable AI for depression, whereas the remaining studies used it for anxiety. The most frequent application of wearable AI was in diagnosing anxiety and depression; however, none of the studies used it for treatment purposes. Most studies targeted individuals aged between 18 and 65 years. The most common wearable device used in the studies was Actiwatch AW4 (Cambridge Neurotechnology Ltd). Wrist-worn devices were the most common type of wearable device in the studies. The most commonly used category of data for model development was physical activity data, followed by sleep data and heart rate data. The most frequently used data set from open sources was Depresjon. The most commonly used algorithm was random forest, followed by support vector machine.
Conclusions
Wearable AI can offer great promise in providing mental health services related to anxiety and depression. Wearable AI can be used by individuals for the prescreening assessment of anxiety and depression. Further reviews are needed to statistically synthesize the studies’ results related to the performance and effectiveness of wearable AI. Given its potential, technology companies should invest more in wearable AI for the treatment of anxiety and depression.
Keywords: wearable artificial intelligence, artificial intelligence, wearable devices, anxiety, depression, scoping review, mobile phone
Introduction
Background
Anxiety and depression are among the common mental illnesses with a high global prevalence. It was reported that as of 2020, a total of 19% of people worldwide were living with depression or anxiety, which prevented them from doing their daily activities as they normally would have for ≥2 weeks [1]. In addition to having a significant economic impact on society [2], anxiety and depression affect people in terms of years lost because of illness. The statistics are astounding; depression is the world’s leading cause of disability within the youth population [3-5]. As per a study among US adults, at 18 years of age, adults with depression had 28 more years of quality-adjusted life expectancy than adults without depression, resulting in a 28.9-year quality-adjusted life expectancy loss owing to depression [6]. Depression is also a significant risk factor when it comes to suicide [7]. Given the abovementioned statistics and the fact that there are only approximately 9 psychiatrists per 100,000 people in high-income countries [8] and 0.1 per 1 million people in low-income countries [9], the situation is challenging to say the least. Current approaches for the assessment of anxiety and depression disorders are primarily based on the clinical observation of patients’ mental states, clinical history, and self-report questionnaires, such as the Generalized Anxiety Disorder-7 for anxiety and Patient Health Questionnaire-9 for depression. However, these methods are subjective, time consuming, and challenging to repeat. As a result, contemporary psychiatric assessments can be inaccurate and ineffective at assessing anxiety and depression symptoms in a reliable and personalized manner. Therefore, there is a significant need to develop automatic techniques to address the limitations of the current psychiatric approaches for assessing anxiety and depression disorders and overcome the shortages and uneven distribution of mental health professionals.
Recently, there have been rapid ongoing developments in artificial intelligence (AI) technology and wearable technology for health care and clinical use, offering numerous advantages for individualizing diagnoses and the treatment management of psychiatric disorders, including anxiety and depression [10-12]. Wearable technology includes electronic devices that users can wear near the body (eg, smartwatches, smart glasses, and smart bracelets), on the body (eg, electrocardiogram electrodes), and in the body (eg, implantable smart patches) and electronic textiles (eg, smart clothes). Wearable devices are designed to provide a constant stream of health care data for disease diagnosis and treatment. This is achieved by continuously recording physiological parameters such as temperature; blood pressure; blood oxygen; respiratory rate; physical movement; and the electrical activity of the heart, brain, and skin. Symptoms of anxiety and depression can be assessed by many parameters collected in real time by wearable devices for the diagnosis and monitoring of patients with anxiety and depression.
However, the dramatically accelerating pace of the development and adoption of wearables coupled with a shortage of skilled caregivers has led to an evolving need for automatic, efficient, and real-time approaches to analyze the large volumes of data collected by wearable sensors. This has motivated the integration of AI methods into wearable devices, introducing the “Wearable AI” technology. Wearable AI refers to intelligent electronic devices that are designed to be worn on the user’s body and possess intelligent operations. Wearable devices typically deal with monitoring and analyzing patients’ health data. However, when paired with AI, wearable devices introduce fundamental developments in the diagnosis and treatment of anxiety and depression. It has the potential to provide an early and accurate diagnosis of anxiety and depression, facilitate more individualized treatment for patients with anxiety and depression, and assist in developing preventive measures for groups at the risk of anxiety and depression.
Research Problem and Aim
Several studies were published on wearable devices combined with AI for the treatment of anxiety and depression. Several reviews were conducted to summarize previous studies; however, they had the following limitations. First, they focused on wearable devices rather than wearable devices paired with AI [10-15]. Second, they did not describe in detail the features of the used wearable devices and AI models [10-15]. Third, they targeted only certain age groups, such as children and adolescents [10,12]. Fourth, they focused on wearable devices for either anxiety [11,14] or depression [12,13,15] rather than both anxiety and depression. Fifth, they did not search relevant databases, such as MEDLINE [14], PsycINFO [10,13,15], IEEE Xplore [10-14], and ACM Digital Library [10-15]. Finally, they focused on wearable devices used for only diagnostic purposes using only electrocardiogram data [11] or electroencephalogram data [15]. Therefore, the need for a review that focuses on AI-paired wearable devices for anxiety and depression has never been higher. The quality of this review should as high as that of a previous review conducted on AI-paired wearable devices for diabetes [16]. The current review aims to explore the features of wearable AI used for anxiety and depression to both help customers make educated selections and help the research community advance in this field by identifying gaps and examining future prospects.
Methods
Overview
To achieve the objective of the study, we conducted a scoping review consistent with PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews) [17]. PRISMA-ScR checklist for this review is presented in Multimedia Appendix 1 [17]. The methods used in this review are detailed in the following subsections.
Search Strategy
To identify relevant studies, we searched 8 electronic databases on May 30, 2022: MEDLINE (via Ovid), PsycINFO (via Ovid), Embase (via Ovid), CINAHL (via EBSCO), IEEE Xplore, ACM Digital Library, Scopus, and Google Scholar. We set up an automatic biweekly search for 24 weeks (ending on September 30, 2022). Given that Google Scholar retrieved a massive number of hits and ordered them based on their relevance, only the first 100 hits (ie,10 pages) were checked in this review. To identify additional studies, we checked the reference lists of the included studies (ie, backward reference list checking) and screened studies that cited the included studies (ie, forward reference list checking).
To develop the search query, 3 experts in digital mental health were consulted, and relevant previous reviews were checked. The search query was composed of 3 groups of terms: terms related to AI (eg, artificial intelligence, machine learning, and deep learning), terms related to wearable devices (eg, wearable OR smart watch OR smartwatch), and terms related to anxiety and depression (eg, anxiety OR anxious OR depression). Multimedia Appendix 2 presents the detailed search query used for searching each database.
Study Eligibility Criteria
This review included studies that focused on developing AI algorithms for anxiety and depression using data collected by wearable devices. Specifically, we focused on all AI algorithms used for any purpose related to anxiety and depression (eg, diagnosis, monitoring, screening, therapy, prediction, and prevention). The wearable devices that were used for collecting data had to be noninvasive on-body wearables, such as smartwatches, smart glasses, smart clothing, smart bracelets, and smart tattoos. By contrast, we excluded studies that used data collected by the following devices: nonwearable devices, handheld devices (eg, mobile phones), near-body wearable devices, in-body wearable devices (eg, implants), wearable devices connected to nonwearable devices using wires, and wearable devices that can be placed on users only by an expert (eg, wearable devices composed of many electrodes that need to be placed in very specific points of the body). Studies that used data collected via any method (eg, nonwearable devices, questionnaires, and interviews) in addition to via wearable devices were considered in this review. We excluded studies that showed only a theoretical framework of AI-based wearable devices for anxiety and depression. We included journal articles, conference papers, and dissertations that were published in the English language since 2015. We excluded reviews, preprints, conference abstracts, posters, protocols, editorials, and commentaries. No restrictions were enforced regarding the measured outcomes, setting, or country of publication.
Study Selection
We followed 3 steps in the study selection process. In the first step, we used EndNote X9 (Clarivate Plc) to remove duplicates from all the retrieved studies. In the second step, we checked the titles and abstracts of the remaining publications. Finally, we screened the entire texts of the studies selected in the previous step. Two reviewers independently performed the study selection process. Disagreements between them in the second and third steps were resolved through discussion. Cohen κ was calculated to measure the interrater agreement [18], and it was 0.85 for “title and abstract” screening and 0.92 for full-text reading.
Data Extraction
Two reviewers used Excel (Microsoft Corp) to independently extract data on study metadata, wearable devices, and AI techniques. Any disagreements between the reviewers were resolved through discussion. The data extraction form used in this review was piloted using 5 studies and is shown in Multimedia Appendix 3.
Data Synthesis
Data extracted from the included studies were synthesized using the narrative approach, wherein data were summarized and described using texts, tables, and figures. More specifically, we began by describing the metadata of the included studies (eg, year of publication and country of publication). Then, we presented the features of the wearable devices used in the included studies (eg, their status, type, placement, and operating system). Finally, we summarized the characteristics of the AI techniques used (eg, AI algorithms used, their aim, data set size, and data input type). We used Microsoft Excel to manage data synthesis.
Results
Search Results
As shown in Figure 1, searching all preidentified databases retrieved 1203 records. Of these 1203 records, 340 (28.26%) duplicates were detected and removed using a reference management software (EndNote X9). Screening the titles and abstracts of the remaining 71.74% (863/1203) of records resulted in the exclusion of 58.6% (506/1203) of records. Of the remaining 41.4% (357/1203) of records, we could not find the full text of 0.8% (3/1203) of records. Reading the full text of the remaining 99.2% (354/357) of records led to the exclusion of 84.2% (298/357) of records for several reasons, which are shown in Figure 1. We identified 13 additional records relevant to this review by backward and forward reference list checking. In total, 69 records were included in this review [19-87].
Figure 1.
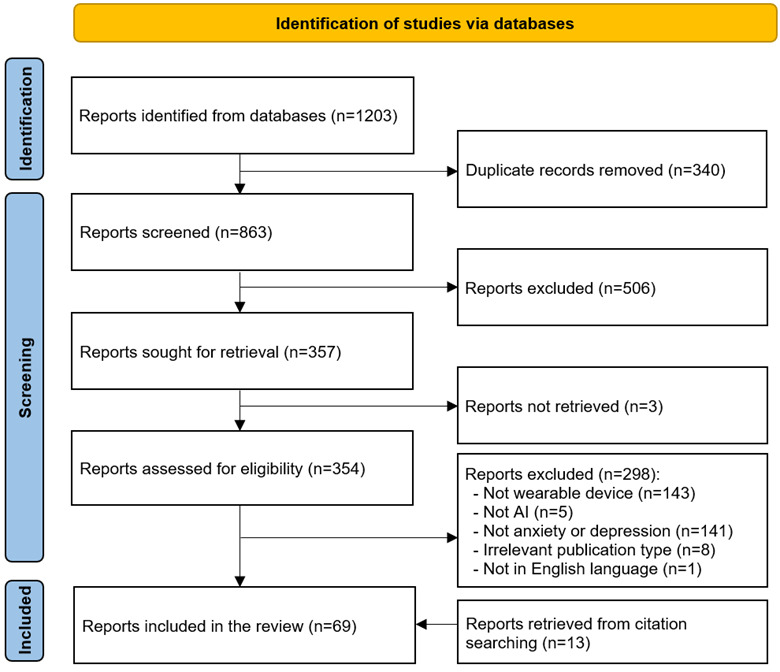
Flowchart of the study selection process. AI: artificial intelligence.
Characteristics of the Included Studies
The included studies were published between 2015 and 2022 (Table 1). The year in which the largest number of included studies was published was 2021 (17/69, 25%), followed by 2019 (16/69, 23%) and then 2020 (15/69, 22%). The studies were conducted in 21 countries (Table 1). More than a quarter (21/69, 30%) of the studies were published in the United States. The included studies were peer-reviewed journal articles (49/69, 71%), conference proceedings (18/69, 26%), and theses (2/69, 3%).
Table 1.
Characteristics of the included studies (N=69).
| Features | Values | References | |
| Year of publication, n (%) | |||
|
|
2022 | 10 (13) | [27,30,38,48,52,59,63,64,69,81] |
|
|
2021 | 17 (25) | [19-21,23,25,28,41,45,49,54,61,62,68,73,74,77,78] |
|
|
2020 | 15 (22) | [22,29,31,33,40,43,44,53,57,60,66,70,71,76,79] |
|
|
2019 | 16 (23) | [26,32,34,42,46,47,51,56,65,67,72,75,80,84-86] |
|
|
2018 | 5 (7) | [35,36,50,55,83] |
|
|
2017 | 4 (6) | [24,37,39,58] |
|
|
2016 | 1 (1) | [87] |
|
|
2015 | 1 (1) | [82] |
| Type of publication, n (%) | |||
|
|
Journal article | 49 (71) | [19,21,23,25-30,34,38-46,48-54,56-61,64-66,69-71,73-75,77-79,81,82,84,86,87] |
|
|
Conference paper | 18 (26) | [20,22,24,31-33,35-37,55,62,63,67,68,72,80,83,85] |
|
|
Thesis | 2 (3) | [47,76] |
| Country of publication, n (%) | |||
|
|
United States | 21 (30) | [24,25,30,31,37,41,42,50,54-56,59,61,66,74,76,77,80,83-85] |
|
|
Mexico | 7 (10) | [34,58,65,69-71,86] |
|
|
Norway | 6 (9) | [20,32,35,36,43,47] |
|
|
United Kingdom | 5 (7) | [29,38,48,72,78] |
|
|
South Korea | 5 (7) | [26-28,46,60] |
|
|
Japan | 4 (6) | [33,63,67,79] |
|
|
Pakistan | 3 (4) | [21,22,45] |
|
|
China | 3 (4) | [23,39,44] |
|
|
India | 2 (3) | [51,53] |
|
|
Taiwan | 2 (3) | [62,81] |
|
|
Others | 11 (16) | [19,40,49,52,57,64,68,73,75,82,87] |
| Number of participants | |||
|
|
Mean (SD; range) | 186.9 (522.2; 8-4036) | [19-87] |
|
|
1-100, n (%) | 53 (77) | [19-22,24,26,27,30-40,42-49,53,55,56,58-68,70,71,75-79,81-83,85-87] |
|
|
101-500, n (%) | 11 (16) | [23,25,41,50,51,54,57,69,73,80,84] |
|
|
>500, n (%) | 5 (7) | [28,29,52,72,74] |
| Age of the participants (years) | |||
|
|
Mean (SD; range) | 36.4 (15.44; 5.2-78) | [19-21,26-30,32,34-38,41-43,46-48,51,52,54-59,61-71,73-80,83,85,86] |
|
|
<18, n (%) | 5 (7) | [54-56,59,76] |
|
|
18-40, n (%) | 17 (25) | [21,26,29,37,51,52,58,66,67,73-75,77,78,80,83,85] |
|
|
41-65, n (%) | 25 (36) | [19,20,27,30,32,34-36,38,41-43,47,48,57,62-65,68-71,79,86] |
|
|
>65, n (%) | 3 (4) | [27,46,61] |
| Sex (female; %), mean (SD; range) | 59.4 (15.64; 2.4-100) | [19-22,26-32,34-38,41-48,50,52,53,55-59,61-71,73,75-81,83,85,86] | |
| Participant health conditionsa, n (%) | |||
|
|
Depression | 32 (46) | [19,20,23,24,26,30,32,34-38,42,43,46-48,50,57,59,60,62,65-71,77,79,86] |
|
|
Healthy | 27 (39) | [19,20,32,34-36,42,43,47,48,50,54-57,60,62,65,67-71,75,76,79,86] |
|
|
Any health condition | 26 (38) | [21,22,25,27-29,31,33,39,41,44,45,52,53,58,61,63,64,72-74,80,83-85,87] |
|
|
Internalizing disorders | 4 (6) | [54-56,76] |
|
|
Bipolar | 3 (4) | [26,49,82] |
|
|
Others | 6 (9) | [40,51,69,75,78,81] |
aNumbers do not add up, as participants in many studies had >1 health condition.
The number of participants in the included studies ranged from 8 to 4036, with an average of 186.7 (SD 522.2; Table 1). The mean age of the participants was reported in 72% (50/69) of studies and ranged between 5.2 and 78 years, with an average of 36.4 (SD 15.4) years. Only 9% (6/69) of the included studies targeted children (aged <18 years), and 4% (3/69) of studies focused on only older adults (aged ≥65 years). The percentage of female participants was reported in 54 studies and varied between 2.4% and 100%, with an average of 59.8% (SD 15.3%). More than one-third (26/69, 38%) of the studies recruited individuals with any health condition, and approximately 30% (21/69) of the studies included both patients with depression and healthy individuals. Multimedia Appendix 4 [19-87] shows the characteristics of each included study.
Features of Wearable Devices
The included studies focused on wearable devices for depression (44/69, 64%), anxiety (17/69, 25%), or both (8/69, 12%). Approximately, 90% (62/69) of the included studies used commercial wearable devices (Table 2). The included studies used 41 different wearable devices. All studies, except for 7, used only 1 wearable device. The most common wearable device used in the included studies was Actiwatch AW4 (Cambridge Neurotechnology Ltd; 17/69, 25%), followed by Fitbit (Fitbit Inc) series (eg, Fitbit Charge, Fitbit Flex, and Fitbit Altra; 13/69, 19%) and Empatica (Empatica Inc) series (eg, E3 and E4; 7/69, 10%). The commercial wearable devices were manufactured by 25 different companies, the most common companies of which was Cambridge Neurotechnology (17/69, 25%), followed by Fitbit Inc (13/69, 19%) and Empatica Inc (7/69, 10%). Multimedia Appendix 5 [19-87] shows the features of the wearable devices in each included study.
Table 2.
Features of the wearable devices (WDs) the included studies focused on (N=69).
| Features | Values, n (%) | References | |
| Target condition | |||
| Depression | 44 (64) | [19,20,23-28,30,32,34-38,42,43,46-53,57,59,60,62,64-71,73,77,79,82-84,86] | |
| Anxiety | 17 (25) | [21,22,31,39-41,45,58,61,72,74,75,78,80,81,85,87] | |
| Anxiety and depression | 8 (12) | [29,33,44,54-56,63,76] | |
| Status of WDa | |||
| Commercial | 63 (91) | [19-38,40-43,46-60,62-71,73-81,83-87] | |
| Noncommercial | 7 (10) | [39,44,45,61,72,82,87] | |
| Name of WDb | |||
| Actiwatch AW4 (Cambridge Neurotechnology) | 17 (25) | [19,20,32,34-36,42,43,47,48,62,65,68-71,86] | |
| Fitbit series (Fitbit Inc) | 13 (19) | [25,26,30,31,33,38,50,52,59,63,73,80,84] | |
| Empatica series (Empatica Inc) | 7 (10) | [27,37,58,66,75,78,85] | |
| 3-Space Sensor (Yost Labs) | 4 (6) | [54-56,76] | |
| Muse | 3 (4) | [21,22,58] | |
| Others | 29 (42) | [23,24,28,29,39-41,44-46,49,51,53,57,58,60,61,64,67,72,74,77,79-83,85,87] | |
| Not reported | 5 (7) | [39,44,45,61,72] | |
| Company of WDb | |||
| Cambridge Neurotechnology | 17 (25) | [19,20,32,34-36,42,43,47,48,62,65,68-71,86] | |
| Fitbit Inc | 11 (16) | [25,26,30,31,33,38,50,52,59,63,73,80,84] | |
| Empatica Inc | 7 (10) | [27,37,58,66,75,78,85] | |
| YEI Technology | 4 (6) | [54-56,76] | |
| InteraXon | 3 (4) | [21,22,58] | |
| Philips | 3 (4) | [41,46,57] | |
| Others | 27 (39) | [23,24,28,29,39,40,44,45,49,51,53,57,58,60,61,64,67,72,74,77,79-83,85,87] | |
| Not applicable | 5 (7) | [39,44,45,61,72,82] | |
| Type of WDb | |||
| Smart band | 50 (72) | [21-26,28-31,33-40,42,44,45,47,50-59,61,63,66,69-76,78,79,81,84,85] | |
| Smartwatch | 16 (23) | [19,20,32,41,43,46,48,49,60,62,65,67,68,77,83,86] | |
| Others (smart shirt, smart adhesive electrodes, smart headset, smart glasses, smart ring, and smart shirt) | 5 (7) | [64,80,82,85,87] | |
| Placementb | |||
| Wrist | 57 (83) | [19,20,23-39,41-52,57-63,65-71,73-75,77-81,83-86] | |
| Head | 7 (10) | [21,22,53,54,58,76,87] | |
| Waist | 6 (9) | [28,54-56,72,76] | |
| Chest | 4 (6) | [58,80,82,85] | |
| Others (ankle, arm, eyes, finger, hand, neck, and thigh) | 1 (each) (1) | [27,39,40,64,87] | |
| Compatibility with OSc,d | |||
| Windows (Corp) | 52 (75) | [19-22,25-27,30-38,40-43,46-50,52,53,57-59,61-63,65-75,78,80,81,83-87] | |
| iOS (Apple Inc) | 36 (52) | [21-31,33,37,38,50-53,58-60,63,64,66,73-75,77-81,83-85,87] | |
| Android | 35 (51) | [21-23,25-28,30,31,33,37,38,40,50-53,58-60,63,64,66,73-75,77-81,83-85,87] | |
| Mac OS (Apple Inc) | 27 (39) | [21,22,25-27,30,31,33,37,38,50,52,53,58,59,63,66,67,73-75,78,80,81,84,85,87] | |
| Linux | 3 (4) | [21,22,58] | |
| Not reported | 8 (12) | [39,44,45,54-56,76,82] | |
| Gatewaye | |||
| Smartphone | 21 (30) | [23,25,26,29-31,33,38,40,50,52,59-61,63,64,73,79,80,83,84] | |
| PC | 13 (19) | [25,26,30,31,33,38,50,52,59,63,73,80,84] | |
| Tablet | 13 (19) | [25,26,30,31,33,38,50,52,59,63,73,80,84] | |
| Silmee L20 gateway | 1 (1) | [79] | |
| Not reported | 48 (70) | [19-22,24,27,28,32,34-37,39,41-49,51,53-58,62,65-72,74-78,81,82,85-87] | |
| Hostf | |||
| PC | 46 (67) | [19-22,27,28,32,34-37,39-49,53-58,62,65-72,74-78,81,85-87] | |
| Server | 30 (43) | [23,25-27,29-31,33,37,38,50,52,58-61,63,64,66,73-75,78-85] | |
| Smartphone | 16 (23) | [21,22,24,27,37,51,53,58,66,74,75,77,78,81,85,87] | |
| Tablet | 8 (12) | [21,22,53,58,74,77,81,87] | |
| Mode of data transferg | |||
| Bluetooth | 41 (59) | [21-27,29-31,33,37,38,40,50-56,58-61,63,64,66,73-81,83-85,87] | |
| Docking station | 27 (39) | [19,20,27,32,34-37,41-43,47-49,57,62,65-71,75,78,85,86] | |
| Internet | 24 (35) | [23,25,26,29-31,33,38,40,50,52,54-56,59,61,63,64,73,76,79,80,83,84] | |
| Removable media | 8 (12) | [39,44,45,54-56,76,82] | |
| Wired | 8 (12) | [28,46,54-56,58,72,76] | |
| ANT+ (ANT Wireless) | 1 (1) | [81] | |
aThe number of studies does not add up, as 1 (1%) study has both commercial and noncommercial wearable devices.
bThe number of studies does not add up, as several studies have used >1 wearable device.
cThe number of studies does not add up, as several studies have used >1 wearable device, and many wearable devices are compatible with >1 operating system.
dOS: operating system.
eThe number of studies does not add up, as several studies used >1 wearable device, and many wearable devices used >1 gateway.
fThe number of studies does not add up, as several studies used >1 wearable device, and many wearable devices used >1 host.
gThe number of studies does not add up, as several studies used >1 wearable device, and many wearable devices used >1 mode of data transfer.
The wearable devices in the included studies were available in 7 forms, but the most common form was smart bands (50/69, 72%), followed by smartwatches (16/69, 23%; Table 2). The wearable devices in the included studies were worn on 11 different parts of the body, but wrist-worn devices were the most common (57/69, 83%) in the included studies. The compatibility of the wearable devices with the operating systems of other devices was identified in 61 studies. The wearable devices were compatible with only 1 operating system in 41% (25/61) of the studies and >1 operating system in 59% (36/61) of the studies. The most common operating systems compatible with the wearable devices in the included studies was Windows (Microsoft Corp; 52/61, 85.2%), followed by iOS (Apple Inc; 36/61, 59%) and Android (35/61, 57%).
Only 21 studies (30%) used a gateway between the wearable device and the main host device (Table 2). In 62% (13/21) of studies, the gateways were PCs, smartphones, and tablets. The included studies used 4 types of host devices (ie, end gate devices that store data collected by wearable devices). More than one host device was used in 20% (14/69) of studies. The most common host device in the included studies was computer (46/69, 67%), followed by database server (30/69, 43%). Data were transferred from the wearable device to the host device through 6 different modes. In approximately 46% (32/69) of the studies, >1 mode of data transfer was used. The most common mode was Bluetooth (41/69, 59%), followed by docking stations (27/69, 39%) and the internet (24/69, 35%).
Wearable devices measured >1 biosignal in 88% (61/69) of the studies (Table 3). The most commonly measured biosignals were physical activity measures (eg, step counts, calories, distance, and metabolic rate; 62/69, 90%), followed by sleep measures (eg, duration and patterns; 53/69, 77%) and heart rate measures (eg, heart rate, heart rate variability, and interbeat interval; 32/69, 46%). The wearable devices in the included studies contained 18 different sensors, and those in approximately 64% (44/69) of the included studies contained >1 sensor. The most common sensor in the wearable devices were accelerometers (63/69, 91%), followed photoplethysmography sensors (31/69, 45%). Although the wearable devices in 67% (46/69) of the studies used an opportunistic approach to collect data (ie, an automatic approach without the user’s input), those in the rest of the studies (23/69, 33%) used both opportunistic and participatory approaches (ie, manual input by the user). The wearable devices in 55% (38/69) of the studies used a passive sensing method to collect data (ie, the sensor captures only signals that come from an object without the transmission of signals to it), whereas those in the remaining (31/69, 45%) studies used both a passive sensing approach and an active sensing approach (ie, the sensor emits signals or light to an object and then captures the reflected signals or light via a detector to measure the biosignal). Multimedia Appendix 6 [19-87] shows the features of the sensors of the wearable devices in each included study.
Table 3.
Features of the sensors of the wearable devices in the included studies (N=69).
| Feature | Studies, n (%) | References | |||
| Measured biosignalsa | |||||
| Physical activity measures | 62 (90) | [19,20,23-28,30-39,41-52,54-60,62-86] | |||
| Sleep measures | 53 (77) | [19,20,23-27,30-38,41-43,46-52,57-60,62-71,73-75,77-86] | |||
| Heart rate measures | 32 (46) | [23,26,27,29-31,33,37,38,40,50,51,58-61,63,64,66,72-75,77-83,85,87] | |||
| Skin temperature | 12 (17) | [27,37,39,44,58,64,66,75,78,79,83,85] | |||
| Electrodermal activity | 11 (16) | [27,37,40,58,61,66,72,75,78,83,85] | |||
| Light exposure | 7 (10) | [28,41,46,49,57,77,83] | |||
| Electroencephalograph | 5 (7) | [21,22,53,58,87] | |||
| Respiration measures | 5 (7) | [40,64,72,80,82] | |||
| Audio | 4 (6) | [39,44,54,83] | |||
| Electrocardiograph sensor | 3 (4) | [40,80,85] | |||
| UV level | 3 (4) | [64,79,83] | |||
| Skin humidity | 2 (3) | [39,44] | |||
| Air pressure | 2 (3) | [60,83] | |||
| Others (blood oxygen saturation and location) | 1 (each) (1) | [40,81] | |||
| Sensors in the wearablesb | |||||
| Accelerometer | 63 (91) | [19,20,23-39,41-52,54-60,62-86] | |||
| PPGc sensors | 31 (45) | [23,26,27,29-31,33,37,38,40,50,51,58-61,63,64,66,72-75,77-81,83,85,87] | |||
| Thermometer | 12 (17) | [27,37,39,44,58,64,66,75,78,79,83,85] | |||
| Gyroscope | 12 (17) | [39,44,45,54-56,60,64,72,76,77,83] | |||
| Electroencephalograph sensor | 11 (16) | [27,37,40,58,61,66,72,75,78,83,85] | |||
| Altimeter | 10 (14) | [26,31,33,38,50,63,73,74,80,81] | |||
| Light sensors | 7 (10) | [28,41,46,49,57,77,83] | |||
| Electrocardiograph sensor | 5 (7) | [40,58,80,82,85] | |||
| Compass | 5 (7) | [54-56,76,77] | |||
| Microphone | 4 (6) | [39,44,54,83] | |||
| UV sensor | 3 (4) | [64,79,83] | |||
| Barometer | 2 (3) | [60,83] | |||
| Others (GPS, oximeter, and piezoelectric sensor) | 1 (each) (1) | [40,81,83] | |||
| Sensing approachd | |||||
| Opportunistic | 69 (100) | [19-87] | |||
| Participatory | 23 (33) | [19,20,27,32,34-37,42,43,46-48,57,58,62,65,66,68-71,86] | |||
| Sensing typee | |||||
| Passive | 38 (55) | [19-22,25,26,28,33,35-37,40,42-50,53-58,63,65,67-71,76,82,84,86] | |||
| Passive and Active | 31 (45) | [23,24,26,27,29-32,34,38,39,41,51,52,59-62,64,66,72-75,77-81,83,85,87] | |||
aThe number of studies does not add up, as several studies used >1 wearable device, and most wearable devices assess >1 biosignal.
bThe number of studies does not add up, as several studies used >1 wearable device, and most wearable devices have >1 sensor.
cPPG: photoplethysmography.
dThe number of studies does not add up, as several studies used >1 wearable device, and many wearable devices used >1 sensing approach.
eThe number of studies does not add up, as several studies used >1 wearable device, and many wearable devices used >1 sensing type.
Features of AI Algorithms
The included studies used AI for three clinical purposes: (1) diagnosing or screening for anxiety and depression (41/69, 59%), (2) monitoring symptoms or levels of anxiety and depression (15/69, 22%), and (3) predicting the occurrence or level of anxiety and depression in the future based on previous and current biosignals (13/69, 19%; Table 4). The included studies used only machine learning algorithms (46/69, 67%), only deep learning algorithms (7/69, 10%), or both machine learning and deep learning algorithms (16/69, 23%). The studies used these algorithms to solve classification problems (63/69, 91%), regression problems (11/69, 16%), and clustering problems (3/69, 4%). More than 50 different algorithms were used in the included studies; however, the most commonly used algorithm was random forest (36/69, 52%), followed by support vector machine (26/69, 38%), logistic regression (16/69, 23%), decision tree (16/69, 23%), extreme gradient boosting (11/69, 16%), and k-nearest neighbors (11/69, 16%). Multimedia Appendix 7 [19-87] shows the features of the AI algorithms used in each included study.
Table 4.
Features of the artificial intelligence (AI) algorithms used in the included studies (N=69).
| Feature | Studies, n (%) | References | ||
| AI category | ||||
| MLa | 46 (67) | [19,20,23,25,26,31,33,34,37,39,40,42,46,49-61,63-67,69-71,73,75-81,83,84,86,87] | ||
| DLb | 7 (10) | [24,29,32,44,47,62,82] | ||
| ML and DL | 16 (23) | [21,22,27,28,30,35,36,38,41,43,45,48,68,72,74,85] | ||
| Problem-solving approachesc | ||||
| Classification | 63 (91) | [19-36,38-58,60-65,67-73,75,76,78-82,84-87] | ||
| Regression | 11 (16) | [37,42,50,59,66,73,74,77,79,83,85] | ||
| Clustering | 3 (4) | [31,74,85] | ||
| AI algorithmd | ||||
| Random forest | 36 (52) | [19-23,26,27,30,33-38,41,43,45,46,49,51,53,59-61,64-66,68-71,77-79,81,86] | ||
| Support vector machine | 26 (38) | [19,20,23,27,30,31,35,38,40,41,49,53,55,56,58,60,61,64,67,72,75,77-80,87] | ||
| Logistic regression | 16 (23) | [19,21-23,25,28,30,38,46,49,51,55-57,61,64] | ||
| Decision tree | 16 (23) | [20,23,27,35,38,40,46,49,54-56,72,76,78,81] | ||
| Extreme gradient boosting | 11 (16) | [20,27,28,41,42,59,64,73,74,79,81] | ||
| k-nearest neighbors | 11 (16) | [23,27,35,38,40,41,55,56,64,78,87] | ||
| AdaBoost | 9 (13) | [25,30,35,37,59,68,77,81,84] | ||
| Multilayer perceptron | 8 (12) | [21,22,24,27,28,72,74,82] | ||
| Convolutional neural network | 7 (10) | [32,43-45,47,48,62] | ||
| Gradient boosting | 5 (7) | [25,27,45,59,77] | ||
| Naive Bayes | 5 (7) | [23,35,38,40,53] | ||
| Others | 28 (41) | [19,28-31,35-37,40,41,43-45,47,48,50-53,59,63,66,68,74,77,81,83,85] | ||
| Aim of AI algorithm | ||||
| Diagnosis or screening | 41 (59) | [19,21,22,28,32,35,36,38-40,43,46-49,51,53-57,61-63,65,67-71,73-76,78-80,82,83,85,87] | ||
| Monitoring | 15 (22) | [20,23,27,34,37,42,44,45,50,58,60,64,66,72,86] | ||
| Prediction | 13 (19) | [24-26,29-31,33,41,52,59,77,81,84] | ||
| Ground truth assessmente | ||||
| MADRSf | 17 (25) | [19,20,32,34-36,42,43,47,48,62,65,68-71,86] | ||
| PHQg-4, -8, and -9 | 13 (19) | [23,24,27,28,30,38,52,53,59,60,73,77,83] | ||
| STAIh | 8 (12) | [21,22,29,31,39,44,61,74] | ||
| DSMi-IV and -5 | 6 (9) | [26,50,55,56,60,82] | ||
| BDI-IIj | 4 (6) | [25,44,60,84] | ||
| Others | 26 (38) | [27,29,33,37,40,41,45,46,49-51,54,57,58,63,64,66,69,75,76,78,79,81,82,85,87] | ||
| Not reported | 3 (4) | [67,72,80] | ||
| Validation approachk | ||||
| k-fold cross-validation | 33 (48) | [21-24,27,30,32,34,35,37,38,40,41,45,47,51,52,60,62,63,66,68,69,73-75,78-83,87] | ||
| Hold-out cross-validation | 25 (36) | [26,28,29,31,32,34,37,44-46,48,49,51,60-62,66,67,70,71,74,81,82,84,86] | ||
| Leave-one-out cross-validation | 20 (29) | [20,25,32,33,36,37,42,43,45,50,53-56,58,59,75,76,84,85] | ||
| Nested cross-validation | 3 (4) | [19,64,77] | ||
| External validation | 1 (1) | [57] | ||
| Time-series cross-validation | 1 (1) | [64] | ||
| Repeated random subsampling | 1 (1) | [87] | ||
| Not reported | 3 (4) | [39,65,72] | ||
| Performance measuresl | ||||
| Accuracy | 50 (72) | [20-29,31-33,35,36,38-40,42,43,46-49,51,53-56,60-64,67-71,73,75,76,78,79,81,82,84,86-88] | ||
| Sensitivity | 41 (59) | [19,21-23,26-28,32-36,38,41-43,46,47,51-54,56-58,60,62,64,65,67-73,79-81,84,86] | ||
| F1-score | 30 (43) | [19-22,25,27,28,32,33,35,36,38,44,46,47,50-52,60-64,67-69,72,80,81,84] | ||
| Specificity | 28 (41) | [19,21,26,32,34-36,41-43,46,47,51-54,56,58,62,65,67,70,71,73,79-81,86] | ||
| Precision | 24 (35) | [19,22,28,32,33,35,36,38,46,47,51,53,58,60,62,64,67,68,70-73,84,86] | ||
| Area under the curve | 22 (32) | [19,26,28,30,34,40,41,46,51,54-57,62,64,65,67,69,70,73,81,86] | ||
| Mean absolute error | 9 (13) | [21,22,48,59,66,73,77,79,83] | ||
| Matthews correlation coefficient | 9 (13) | [35,36,43,47,62,68,69] | ||
| Cohen κ | 7 (10) | [21,22,40,42,52,68,73] | ||
| Root mean square error | 6 (9) | [21,22,37,59,66,73] | ||
| Balanced accuracy | 6 (9) | [19,41,52,67,80,86] | ||
| Receiver operating characteristic | 6 (9) | [19,27,55,65,81,86] | ||
| Correlation coefficient (r) | 5 (7) | [42,66,74,79,83] | ||
| Others | 13 (19) | [22,40,50,52,53,57,59,71,73,74,77,85,86] | ||
aML: machine learning.
bDL: deep learning.
cThe number of studies does not add up, as many studies have used >1 problem-solving approach.
dThe number of studies does not add up, as many studies have used >1 AI algorithm.
eThe number of studies does not add up, as many studies have used >1 tool to assess the ground truth.
fMADRS: Montgomery-Asberg Depression Rating Scale.
gPHQ: Patient Health Questionnaire.
hSTAI: State-Trait Anxiety Inventory.
iDSM: Diagnostic and Statistical Manual of Mental Disorders.
jBDI-II: Beck Depression Inventory-Second Edition.
kThe number of studies does not add up, as many studies have used >1 validation approach.
lThe number of studies does not add up, as most studies used >1 performance measure.
The included studies identified the ground truth based on 27 different tools, but the most common tool was Montgomery-Asberg Depression Rating Scale (MADRS; 17/69, 25%), followed by Patient Health Questionnaire-9 (12/69, 17%) and State-Trait Anxiety Inventory (8/69, 12%). The included studies used 7 different validation methods for the models. Approximately, 22% (15/69) of the included studies used >1 validation method (Table 4). The most commonly used validation method was k-fold cross-validation (33/69, 48%), followed hold-out cross-validation (25/69, 36%) and leave-one-out cross-validation (20/69, 29%). The included studies evaluated the performance of the models using 33 metrics. The most common metric used in the included studies was accuracy (50/69, 72%), followed by sensitivity (41/69, 59%), F1-score (30/69, 43%), specificity (28/69, 41%), precision (24/69, 35%), and area under the curve (22/69, 32%).
Approximately, 20% (14/69) of the included studies reported the data set size used for developing (ie, training and testing) the models (Table 5). The data set size ranged between 168 and 1,570,144 inputs, with an average of 168,023 (SD 428,843) inputs. The included studies used data sets from either closed sources (ie, collected by the authors of the study or obtained from previous studies; 50/69, 72%) or open sources (ie, public databases; 19/69, 28%). Depression was the most common data set obtained from open sources and used in the included studies (16/19, 84%). In 59% (41/69) of the studies, AI algorithms were developed using only data collected by wearable devices. Of the included studies, approximately 17% (12/69) developed AI algorithms using data collected by a combination of wearable devices and self-administered questionnaires (ie, self-reported data), approximately 13% (9/69) developed AI algorithms using data collected by a combination of wearable devices and nonwearable devices (eg, smartphones), and approximately 10% (7/69) developed AI algorithms using data collected by a combination of wearable devices, nonwearable devices, and self-administered questionnaires. The included studies used >50 categories of data to develop their models. Although 43% (30/69) of the studies used only 1 category of data to develop their models, the rest (39/69, 57%) of the studies used >1 category of data. The most common category of data used to develop the models was physical activity data (eg, step counts, calories, and metabolic rate; 53/69, 77%), followed by sleep data (eg, duration and patterns; 27/69, 39%), heart rate data (eg, heart rate, heart rate variability, and interbeat interval; 26/69, 38%), mental health measures (eg, depression level, anxiety level, stress level, and mood status; 14/69, 20%), location data (eg, latitude, longitude, percentage of time spent at home, and stationary time; 10/69, 14%), smartphone use data (eg, display on or off, charging activity, and the number of apps used; 10/69, 14%), and social interactions (eg, call and message logs; 10/69, 14%). The number of features used in the model development ranged from 2 to 5173. In approximately half (33/69, 48%) of the studies, the number of features was ≤10. Multimedia Appendix 8 [19-87] shows the features of the data used for AI development in each included study.
Table 5.
Features of the data used for artificial intelligence (AI) development in the included studies (N=69).
| Feature | Values | References | |
| Data set size, mean (SD; range) | 168,022.5 (428,843.2; 168-1,570,144) | [22,23,28,37,41,44,45,51,58,60-62,70,73] | |
| Data set source, n (%) | |||
| Open | 19 (28) | [19,20,28,31,32,34,36,42,43,47,48,62,65,68-71,74,86] | |
| Closed | 50 (72) | [21-27,29,30,33,35,37-41,44-46,49-61,63,64,66,67,72,73,75-85,87] | |
| Data types, n (%) | |||
| WDa based | 41 (59) | [20-22,27,29,31-36,38,39,41-48,53-56,58,61,62,65,67,69-71,73,75,76,78-80,82,87] | |
| WD based and self-reported | 12 (17) | [19,26,28,30,49,51,52,57,68,81,85,86] | |
| WD based and non-WD based | 9 (13) | [23,25,40,50,59,66,72,74,84] | |
| WD based, non-WD based, and self-reported | 7 (10) | [24,37,60,63,64,77,83] | |
| Data input to AI algorithmb, n (%) | |||
| Physical activity data | 53 (77) | [19,20,23-27,30-32,34-38,41-51,54-57,59,60,62-74,76,77,79,81,83-86] | |
| Sleep data | 27 (39) | [23-26,30,33,37,38,41,46,49-52,57,59,60,63,64,66,73,74,77,79,81,83,84] | |
| Heart rate data | 26 (38) | [23,26,27,29-31,40,50,51,58-61,63,64,66,72,75,77-81,83,85,87] | |
| Mental health measures | 14 (20) | [24,26,30,37,46,49,50,52,57,60,64,77,81,85] | |
| Social interaction data | 10 (14) | [23-25,37,59,60,66,72,83,84] | |
| Location data | 10 (14) | [23,25,37,50,59,64,66,74,83,84] | |
| Smartphone use data | 10 (14) | [23,25,37,59,60,64,66,74,83,84] | |
| Electrodermal activity data | 10 (14) | [27,37,40,58,61,66,72,75,78,85] | |
| Skin temperature data | 5 (7) | [27,75,78,79,85] | |
| Demographic data | 5 (7) | [30,52,57,68,85] | |
| Electroencephalograph data | 4 (6) | [21,22,53,87] | |
| Light exposure | 4 (6) | [26,46,60,79] | |
| Audio data | 4 (6) | [39,44,54,85] | |
| Others | 17 (25) | [24,28,30,37,49,52,57,60,63,66,72-74,77,81,82,85] | |
| Number of featuresc, n (%) | |||
| 1-10 | 33 (48) | [19,21-25,27,34-40,43,46,47,50,54-58,67,69-72,75,78,82,83,87] | |
| 11-20 | 16 (23) | [23,26,28,30,33,45,48,51-53,57,61,68,72,76,86] | |
| 21-30 | 6 (9) | [44,52,60,63,73,85] | |
| 31-40 | 6 (9) | [23,34,38,50,66,73] | |
| 41-50 | 6 (9) | [23,41,64,73,77,80] | |
| >50 | 8 (12) | [23,27,59,73,74,79,81,84] | |
| Not reported | 8 (12) | [20,29,31,32,42,49,62,65] | |
aWD: wearable device.
bThe number of studies does not add up, as many studies used >1 data input.
cThe number of studies does not add up, as several studies used various numbers of features.
Discussion
Principal Findings
This scoping review aimed at exploring the features of AI and wearable devices used for anxiety and depression. In this review, approximately two-thirds of the studies used wearable AI for depression, whereas the remaining studies used it for anxiety. This may be attributed to the ability of wearables to collect biosignals related to the symptoms of depression and anxiety. More specifically, it is well known that depression is associated with a decrease in activity and changes in sleep behaviors [13,89,90], which can be objectively measured using wearable devices. Furthermore, the analysis of depression symptoms does not rely on highly accurate data; that is, general trends are sufficient to provide indications. By contrast, anxiety is usually associated with heart rate variability [91]. Although wearable devices can have an acceptable heart rate accuracy [92], the quality of one device is different from that of another [93]. Moreover, monitoring the heart rate without contextual information might be misleading because multiple factors impact the heart rate; thus, detecting anxiety based on only objective biosignals is questionable. Combining the data from wearable devices with additional data sources is crucial. So far, only a few studies included in this review were based on a combination of data from different sources (ie, wearable devices, nonwearable devices, and self-administered questionnaires).
In this review, the most frequent application of wearable AI was in the diagnosis of or screening for anxiety and depression. A similar result was reported in 2 previous reviews, which showed that most studies focused on using wearables for diagnostic purposes [10,13]. Although wearable AI can be used for interventional and treatment purposes (eg, personalized mindfulness, meditation, and biofeedback therapy [14]), none of the systems in the included studies were used for such purposes. This may be attributed to the lack of evidence on the effectiveness of wearable AI in improving anxiety and depression.
Smart bands worn on the wrist were the most common type of wearable device used in the studies. This has been indicated in previous reviews as well [10,13,14]. This can be attributed to the fact that wrist-worn wearable devices are less distractive and less obtrusive, easy to use, and more stylish and familiar to most people. According to Hunkin et al [94], such features are crucial for users’ acceptance and use of wearable devices.
The most commonly used category of data for model development was physical activity data, followed by sleep data and heart rate data. This is expected given that depression and anxiety are associated with physical activity [13,89,90], sleep patterns [13,95,96], and heart rate [91]. In addition, as this review demonstrated, these are the most common biosignals measured by commercial wearable devices.
Surprisingly, more than half of the studies considered only data from wearables in their AI algorithms. However, wearables cannot detect all the symptoms relevant to anxiety and depression for 2 reasons. First, wearable devices cannot detect several physiological data, such as weight loss or gain and changes in appetite [13]. Second, wearable devices cannot evaluate subjective symptoms such as social interaction, medical history, and lifestyle changes [13]. It might be questioned whether research has started to overrely on the diagnostic and predictive power of data from only wearable devices.
Approximately, one-fourth of the studies relied on a data set called Depresjon [35] to develop their models. Depresjon is a freely available data set that contains data related to motor activity measured using an actigraph watch worn on the wrist (Actiwatch AW4) [35]. The data set also contains data related to depression levels assessed using MADRS [35]. This explains why the most common wearable device used in the included studies was Actiwatch AW4 and why MADRS was the most frequently used tool to assess the ground truth.
Regarding the target population, we must recognize that most studies addressed individuals aged between 18 and 65 years. Global statistics show that the that the incidence of depression and anxiety is slightly higher in age groups between 15-64 years than adult aged ≥65 years [1]. This might explain why the studies mainly targeted the age group of 18 to 65 years. Another explanation might be that wearables are more popular among adults in that age group.
This review showed that k-fold cross-validation was the most frequently used validation method. This can be attributed to several factors. First, in comparison with hold-out cross-validation, k-fold cross-validation is prone to less variation, as each observation is used for both training and testing. Second, the training set in k-fold cross-validation is larger than that in hold-out cross-validation; therefore, k-fold cross-validation has reduced bias and reduced overestimation of test error. Finally, k-fold cross-validation is computationally less expensive than leave-one-out cross-validation, as the algorithm needs to rerun only k times (usually ≤10).
Research and Practical Implications
The performance of wearable AI in diagnosing, monitoring, and predicting anxiety and depression was not assessed in this review. Systematic reviews and meta-analyses are needed to examine the performance of wearable AI devices. Future studies should also compare the performance of different wearable devices (eg, Fitbit vs Empatica), worn at different locations (eg, wrist, chest, and waist), and using different data types (eg, wearable-based data vs wearable-based data and self-reported data). Conducting systematic reviews of such studies can help researchers, developers, and wearable device companies identify the most significant features and powerful AI algorithms for diagnosing, monitoring, and predicting anxiety and depression.
AI research highly depends on the available data sets. However, when only 1 data set is exploited by researchers, no conclusions regarding the generalizability of study results can be drawn. Therefore, we recommend that researchers (1) publish their data sets in open databases after ensuring participants’ privacy and confidentiality and (2) exploit different data sets available in open databases.
This review found a lack of AI-based wearable devices used for treatment purposes, although wearable AI can be used to provide many interventions for anxiety and depression, such as personalized mindfulness, meditation, and biofeedback therapy. Technology companies should invest more in wearable AI devices for the treatment of anxiety and depression. Researchers should also assess the effectiveness of such technologies in improving anxiety and depression.
The ground truth of mental states (anxiety or depression) in the included studies was identified using 27 different tools. Although most of these tools have been validated extensively, they do not usually include physiological biomarkers (eg, physical activity, heart rate, electrodermal activity, respiratory rate, and electroencephalogram). This brings into question the validity and reliability of drawing conclusions about mental states (anxiety or depression) based on physiological biomarkers when the ground truth of mental states is assessed using subjective questionnaires. Accordingly, the performance of AI-based wearable devices will be underestimated.
Although the current studies have shown that wearable AI can be used for monitoring symptoms or levels of anxiety and depression, continuous tracking of physiological biomarkers could trigger emotional instability and ruminative thinking [97]. Although wearable AI can approximate mental states (eg, feeling nervous, anxious, or on edge) through heart rate and other variables, it could provide many false positives, thereby exacerbating or increasing the anxiety or depression of an individual. The abovementioned downsides of wearable AI should be considered and mitigated before developing AI-based wearables in the future. More research is needed on the use of wearable devices and individuals’ emotional and behavioral responses to the automated feedback from wearable devices.
Wearable AI can help individuals conduct prescreening assessments of mental health and well-being without an initial hospital or clinical encounter. The individual could be notified through the wearable device, smartphone, or desktop application about their mental health status, which would encourage them to visit a mental health and well-being professional. Such prescreening feedback from wearables may help reduce mental health stigma and allow a higher number of individuals to seek help from a mental health professional.
The quality of the data, whether obtained from open sources or generated by wearable devices, should be emphasized. To do so, there is a need for more practical standards for wearable device development that ensure accurate measurement of different signals generated by wearable devices to improve algorithmic performance.
Limitations
This review excluded many studies that focused on nonwearable devices, handheld devices (eg, mobile phones), near-body wearable devices, in-body wearable devices (eg, implants), wearable devices connected to nonwearable devices using wires, and wearable devices that can be placed on users only by experts. Therefore, our findings may not be generalizable to contexts in which such excluded devices are applied. Owing to practical constraints, we included only studies published in the English language. We also restricted our search to studies published from 2015 onward, given that this is a fast-growing field and, thereby, studies published before 2015 can be deemed outdated. Consequently, it is likely that we missed some studies published in other languages or before 2015. Another limitation of this review is that we cannot comment on the performance of wearable AI in diagnosing, monitoring, and predicting anxiety and depression and the importance of features and variables, as this is beyond the scope of this review and requires systematic reviews, wherein the quality of the evidence and risk of bias are assessed.
Conclusions
Wearable AI can offer great promise in providing mental health services related to anxiety and depression. Wearable AI can be used by individuals for the prescreening assessment of anxiety and depression. Further reviews are needed to statistically synthesize the results of studies on the performance and effectiveness of wearable AI. More studies are needed on the use of wearable devices and individuals’ emotional and behavioral responses to the automated feedback from wearable devices. Given its potential, technology companies should invest more in wearable AI for the treatment of anxiety and depression. The downsides of wearable AI devices (eg, false positive alerts and triggering emotional instability and ruminative thinking) should be considered and mitigated before developing them in the future.
Abbreviations
- AI
artificial intelligence
- MADRS
Montgomery-Asberg Depression Rating Scale
- PRISMA-ScR
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews
PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews) checklist.
Search strategy.
Data extraction form.
Characteristics of each included study.
Features of wearable devices.
Features of the sensors of wearable devices.
Features of artificial intelligence algorithms.
Features of the data used in artificial intelligence algorithms.
Data Availability
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Footnotes
Authors' Contributions: A Abd-alrazaq, A Ahmed, and SA developed the protocol with guidance from and under the supervision of JS. A Abd-alrazaq searched the electronic databases and conducted backward and forward reference list checks. The study selection process was conducted by A Abd-alrazaq and RA. The data extraction process was conducted by RA and SA. A Abd-alrazaq and SA conducted the data synthesis. A Abd-alrazaq wrote the Results and Methods sections. A Ahmed and A Abd-alrazaq wrote the Introduction section. KD, A Abd-alrazaq, MH, and FF wrote the Discussion section. The manuscript was critically revised for important intellectual content by all the authors. All the authors approved the manuscript for publication and agree to be accountable for all aspects of the work.
Conflicts of Interest: None declared.
References
- 1.The role of science in mental health: Insights from the Wellcome Global Monitor. Wellcome Trust. 2020. https://cms.wellcome.org/sites/default/files/2021-10/wellcome-global-monitor-mental-health.pdf .
- 2.Konnopka A, König H. Economic burden of anxiety disorders: a systematic review and meta-analysis. Pharmacoeconomics. 2020 Jan 24;38(1):25–37. doi: 10.1007/s40273-019-00849-7.10.1007/s40273-019-00849-7 [DOI] [PubMed] [Google Scholar]
- 3.Hammen C, Brennan PA, Keenan-Miller D. Patterns of adolescent depression to age 20: the role of maternal depression and youth interpersonal dysfunction. J Abnorm Child Psychol. 2008 Nov 13;36(8):1189–98. doi: 10.1007/s10802-008-9241-9. [DOI] [PubMed] [Google Scholar]
- 4.Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Charlson FJ, Norman RE, Flaxman AD, Johns N, Burstein R, Murray CJ, Vos T. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013 Nov 09;382(9904):1575–86. doi: 10.1016/S0140-6736(13)61611-6.S0140-6736(13)61611-6 [DOI] [PubMed] [Google Scholar]
- 5.Wilson S, Hicks BM, Foster KT, McGue M, Iacono WG. Age of onset and course of major depressive disorder: associations with psychosocial functioning outcomes in adulthood. Psychol Med. 2014 Jul 10;45(3):505–14. doi: 10.1017/s0033291714001640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jia H, Zack MM, Thompson WW, Crosby AE, Gottesman II. Impact of depression on quality-adjusted life expectancy (QALE) directly as well as indirectly through suicide. Soc Psychiatry Psychiatr Epidemiol. 2015 Jun 7;50(6):939–49. doi: 10.1007/s00127-015-1019-0. https://europepmc.org/abstract/MED/25660550 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hawton K, Casañas I Comabella C, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013 May;147(1-3):17–28. doi: 10.1016/j.jad.2013.01.004.S0165-0327(13)00036-0 [DOI] [PubMed] [Google Scholar]
- 8.Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, AlMazroa MA, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basáñez M, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabé E, Bhalla K, Bhandari B, Bikbov B, Abdulhak AB, Birbeck G, Black JA, Blencowe H, Blore JD, Blyth F, Bolliger I, Bonaventure A, Boufous S, Bourne R, Boussinesq M, Braithwaite T, Brayne C, Bridgett L, Brooker S, Brooks P, Brugha TS, Bryan-Hancock C, Bucello C, Buchbinder R, Buckle G, Budke CM, Burch M, Burney P, Burstein R, Calabria B, Campbell B, Canter CE, Carabin H, Carapetis J, Carmona L, Cella C, Charlson F, Chen H, Cheng AT, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahiya M, Dahodwala N, Damsere-Derry J, Danaei G, Davis A, Leo DD, Degenhardt L, Dellavalle R, Delossantos A, Denenberg J, Derrett S, Des Jarlais DC, Dharmaratne SD, Dherani M, Diaz-Torne C, Dolk H, Dorsey ER, Driscoll T, Duber H, Ebel B, Edmond K, Elbaz A, Ali SE, Erskine H, Erwin PJ, Espindola P, Ewoigbokhan SE, Farzadfar F, Feigin V, Felson DT, Ferrari A, Ferri CP, Fèvre EM, Finucane MM, Flaxman S, Flood L, Foreman K, Forouzanfar MH, Fowkes FG, Fransen M, Freeman MK, Gabbe BJ, Gabriel SE, Gakidou E, Ganatra HA, Garcia B, Gaspari F, Gillum RF, Gmel G, Gonzalez-Medina D, Gosselin R, Grainger R, Grant B, Groeger J, Guillemin F, Gunnell D, Gupta R, Haagsma J, Hagan H, Halasa YA, Hall W, Haring D, Haro JM, Harrison JE, Havmoeller R, Hay RJ, Higashi H, Hill C, Hoen B, Hoffman H, Hotez PJ, Hoy D, Huang JJ, Ibeanusi SE, Jacobsen KH, James SL, Jarvis D, Jasrasaria R, Jayaraman S, Johns N, Jonas JB, Karthikeyan G, Kassebaum N, Kawakami N, Keren A, Khoo J, King CH, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Laden F, Lalloo R, Laslett LL, Lathlean T, Leasher JL, Lee YY, Leigh J, Levinson D, Lim SS, Limb E, Lin JK, Lipnick M, Lipshultz SE, Liu W, Loane M, Ohno SL, Lyons R, Mabweijano J, MacIntyre MF, Malekzadeh R, Mallinger L, Manivannan S, Marcenes W, March L, Margolis DJ, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGill N, McGrath J, Medina-Mora ME, Meltzer M, Memish ZA, Mensah GA, Merriman TR, Meyer A, Miglioli V, Miller M, Miller TR, Mitchell PB, Mock C, Mocumbi AO, Moffitt TE, Mokdad AA, Monasta L, Montico M, Moradi-Lakeh M, Moran A, Morawska L, Mori R, Murdoch ME, Mwaniki MK, Naidoo K, Nair MN, Naldi L, Narayan KM, Nelson PK, Nelson RG, Nevitt MC, Newton CR, Nolte S, Norman P, Norman R, O'Donnell M, O'Hanlon S, Olives C, Omer SB, Ortblad K, Osborne R, Ozgediz D, Page A, Pahari B, Pandian JD, Rivero AP, Patten SB, Pearce N, Padilla RP, Perez-Ruiz F, Perico N, Pesudovs K, Phillips D, Phillips MR, Pierce K, Pion S, Polanczyk GV, Polinder S, Pope CA, Popova S, Porrini E, Pourmalek F, Prince M, Pullan RL, Ramaiah KD, Ranganathan D, Razavi H, Regan M, Rehm JT, Rein DB, Remuzzi G, Richardson K, Rivara FP, Roberts T, Robinson C, De Leòn FR, Ronfani L, Room R, Rosenfeld LC, Rushton L, Sacco RL, Saha S, Sampson U, Sanchez-Riera L, Sanman E, Schwebel DC, Scott JG, Segui-Gomez M, Shahraz S, Shepard DS, Shin H, Shivakoti R, Silberberg D, Singh D, Singh GM, Singh JA, Singleton J, Sleet DA, Sliwa K, Smith E, Smith JL, Stapelberg NJ, Steer A, Steiner T, Stolk WA, Stovner LJ, Sudfeld C, Syed S, Tamburlini G, Tavakkoli M, Taylor HR, Taylor JA, Taylor WJ, Thomas B, Thomson WM, Thurston GD, Tleyjeh IM, Tonelli M, Towbin JA, Truelsen T, Tsilimbaris MK, Ubeda C, Undurraga EA, van der Werf MJ, van Os J, Vavilala MS, Venketasubramanian N, Wang M, Wang W, Watt K, Weatherall DJ, Weinstock MA, Weintraub R, Weisskopf MG, Weissman MM, White RA, Whiteford H, Wiebe N, Wiersma ST, Wilkinson JD, Williams HC, Williams SR, Witt E, Wolfe F, Woolf AD, Wulf S, Yeh P, Zaidi AK, Zheng Z, Zonies D, Lopez AD. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012 Dec;380(9859):2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 9.Oladeji BD, Gureje O. Brain drain: a challenge to global mental health. BJPsych Int. 2016 Aug 02;13(3):61–3. doi: 10.1192/s2056474000001240. https://europepmc.org/abstract/MED/29093905 .S2056474000001240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Welch V, Wy TJ, Ligezka A, Hassett LC, Croarkin PE, Athreya AP, Romanowicz M. Use of mobile and wearable artificial intelligence in child and adolescent psychiatry: scoping review. J Med Internet Res. 2022 Mar 14;24(3):e33560. doi: 10.2196/33560. https://www.jmir.org/2022/3/e33560/ v24i3e33560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elgendi M, Menon C. Assessing anxiety disorders using wearable devices: challenges and future directions. Brain Sci. 2019 Mar 01;9(3):50. doi: 10.3390/brainsci9030050. https://www.mdpi.com/resolver?pii=brainsci9030050 .brainsci9030050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sequeira L, Perrotta S, LaGrassa J, Merikangas K, Kreindler D, Kundur D, Courtney D, Szatmari P, Battaglia M, Strauss J. Mobile and wearable technology for monitoring depressive symptoms in children and adolescents: a scoping review. J Affect Disord. 2020 Mar 15;265:314–24. doi: 10.1016/j.jad.2019.11.156.S0165-0327(19)31030-4 [DOI] [PubMed] [Google Scholar]
- 13.Lee S, Kim H, Park MJ, Jeon HJ. Current advances in wearable devices and their sensors in patients with depression. Front Psychiatry. 2021 Jun 17;12:672347. doi: 10.3389/fpsyt.2021.672347. https://europepmc.org/abstract/MED/34220580 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Juchems, PC. The use of wearable devices in the treatment and detection of anxiety: a systematic scoping review. University of Twente. 2022. [2022-12-30]. http://essay.utwente.nl/89469/1/Juchems_MA_BMS.pdf .
- 15.Yasin S, Hussain SA, Aslan S, Raza I, Muzammel M, Othmani A. EEG based major depressive disorder and bipolar disorder detection using neural networks:a review. Comput Methods Programs Biomed. 2021 Apr;202:106007. doi: 10.1016/j.cmpb.2021.106007. doi: 10.1016/j.cmpb.2021.106007.S0169-2607(21)00082-1 [DOI] [PubMed] [Google Scholar]
- 16.Ahmed A, Aziz S, Abd-Alrazaq A, Farooq F, Sheikh J. Overview of artificial intelligence-driven wearable devices for diabetes: scoping review. J Med Internet Res. 2022 Aug 09;24(8):e36010. doi: 10.2196/36010. https://www.jmir.org/2022/8/e36010/ v24i8e36010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018 Oct 02;169(7):467–73. doi: 10.7326/M18-0850. https://www.acpjournals.org/doi/abs/10.7326/M18-0850?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .2700389 [DOI] [PubMed] [Google Scholar]
- 18.Cochrane Handbook for Systematic Reviews of Interventions: Cochrane Book Series. New York, New York, United States: Wiley; 2008. [Google Scholar]
- 19.Adamczyk J, Malawski F. Comparison of manual and automated feature engineering for daily activity classification in mental disorder diagnosis. Comput Inform. 2021;40(4):850–79. doi: 10.31577/cai_2021_4_850. [DOI] [Google Scholar]
- 20.Aminifar A, Rabbi F, Pun VK, Lamo Y. Monitoring motor activity data for detecting patients’ depression using data augmentation and privacy-preserving distributed learning. Proceedings of the 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC); 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC); Nov 01-05, 2021; Mexico. 2021. [DOI] [PubMed] [Google Scholar]
- 21.Arsalan A, Majid M. A study on multi-class anxiety detection using wearable EEG headband. J Ambient Intell Human Comput. 2021 Apr 11;13(12):5739–49. doi: 10.1007/s12652-021-03249-y. [DOI] [Google Scholar]
- 22.Arsalan A, Majid M, Anwar SM. Electroencephalography Based Machine Learning Framework for Anxiety Classification. Intelligent Technologies and Applications. 2020;1198:187–197. doi: 10.1007/978-981-15-5232-8_17. [DOI] [Google Scholar]
- 23.Bai R, Xiao L, Guo Y, Zhu X, Li N, Wang Y, Chen Q, Feng L, Wang Y, Yu X, Xie H, Wang G. Tracking and monitoring mood stability of patients with major depressive disorder by machine learning models using passive digital data: prospective naturalistic multicenter study. JMIR Mhealth Uhealth. 2021 Mar 08;9(3):e24365. doi: 10.2196/24365. https://mhealth.jmir.org/2021/3/e24365/ v9i3e24365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bennett CC, Sabanovic S, Piatt JA, Nagata S, Eldridge L, Randall N. A robot a day keeps the blues away. Proceedings of the 2017 IEEE International Conference on Healthcare Informatics (ICHI); IEEE International Conference on Healthcare Informatics (ICHI); Aug 23-26, 2017; Park City, UT, USA. 2017. https://ieeexplore.ieee.org/document/8031208 . [Google Scholar]
- 25.Chikersal P, Doryab A, Tumminia M, Villalba DK, Dutcher JM, Liu X, Cohen S, Creswell KG, Mankoff J, Creswell JD, Goel M, Dey AK. Detecting depression and predicting its onset using longitudinal symptoms captured by passive sensing: a machine learning approach with robust feature selection. ACM Trans Comput Human Interact. 2021 Feb 28;28(1):1–41. doi: 10.1145/3422821. [DOI] [Google Scholar]
- 26.Cho C, Lee T, Kim M, In HP, Kim L, Lee H. Mood prediction of patients with mood disorders by machine learning using passive digital phenotypes based on the circadian rhythm: prospective observational cohort study. J Med Internet Res. 2019 Apr 17;21(4):e11029. doi: 10.2196/11029. https://www.jmir.org/2019/4/e11029/ v21i4e11029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Choi J, Lee S, Kim S, Kim D, Kim H. Depressed mood prediction of elderly people with a wearable band. Sensors (Basel) 2022 May 31;22(11):4174. doi: 10.3390/s22114174. https://www.mdpi.com/resolver?pii=s22114174 .s22114174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Choi J, Ko I, Han S. Depression level classification using machine learning classifiers based on actigraphy data. IEEE Access. 2021;9:116622–46. doi: 10.1109/access.2021.3105393. [DOI] [Google Scholar]
- 29.Coutts LV, Plans D, Brown AW, Collomosse J. Deep learning with wearable based heart rate variability for prediction of mental and general health. J Biomed Inform. 2020 Dec;112:103610. doi: 10.1016/j.jbi.2020.103610. https://linkinghub.elsevier.com/retrieve/pii/S1532-0464(20)30238-0 .S1532-0464(20)30238-0 [DOI] [PubMed] [Google Scholar]
- 30.Dai R, Kannampallil T, Zhang J, Lv N, Ma J, Lu C. Multi-task learning for randomized controlled trials: a case study on predicting depression with wearable data. Proc ACM Interact Mob Wearable Ubiquitous Technol. 2022 Jul 04;6(2):1–23. doi: 10.1145/3534591. [DOI] [Google Scholar]
- 31.Feng T, Narayanan SS. Modeling behavioral consistency in large-scale wearable recordings of human bio-behavioral signals. Proceedings of the ICASSP 2020 - 2020 IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP); IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP); May 04-08, 2020; Barcelona, Spain. 2020. pp. 1011–1015. https://ieeexplore.ieee.org/document/9054493 . [Google Scholar]
- 32.Frogner JI, Noori FM, Halvorsen P, Hicks SA, Garcia-Ceja E, Torresen J, Riegler MA. One-dimensional convolutional neural networks on motor activity measurements in detection of depression. Proceedings of the 4th International Workshop on Multimedia for Personal Health & Health Care; MM '19: The 27th ACM International Conference on Multimedia; Oct 21, 2019; Nice, France. 2019. pp. 9–15. https://dl.acm.org/doi/10.1145/3347444.3356238 . [Google Scholar]
- 33.Fukuda S., Matsuda Y., Tani Y., Arakawa Y., Yasumoto K. Predicting depression and anxiety mood by wrist-worn sleep sensor. Proceedings of the 2020 IEEE International Conference on Pervasive Computing and Communications Workshops (PerCom Workshops); IEEE International Conference on Pervasive Computing and Communications Workshops (PerCom Workshops); Mar 23-27, 2020; Austin, TX, USA. 2020. pp. 1–6. https://ieeexplore.ieee.org/document/9156176 . [DOI] [Google Scholar]
- 34.Galván-Tejada CE, Zanella-Calzada LA, Gamboa-Rosales H, Galván-Tejada JI, Chávez-Lamas NM, Gracia-Cortés MD, Magallanes-Quintanar R, Celaya-Padilla JM. Depression episodes detection in unipolar and bipolar patients: a methodology with feature extraction and feature selection with genetic algorithms using activity motion signal as information source. Mobile Inform Syst. 2019 Apr 23;2019:1–12. doi: 10.1155/2019/8269695. [DOI] [Google Scholar]
- 35.Garcia-Ceja E, Riegler M, Jakobsen J, Tørresen J, Nordgreen T, Oedegaard KJ, Fasmer OB. Depresjon: a motor activity database of depression episodes in unipolar and bipolar patients. Proceedings of the 9th ACM Multimedia Systems Conference; MMSys '18: 9th ACM Multimedia Systems Conference; Jun 12 - 15, 2018; Amsterdam Netherlands. 2018. pp. 472–477. https://dl.acm.org/doi/10.1145/3204949.3208125 . [Google Scholar]
- 36.Garcia-Ceja E, Riegler M, Jakobsen P, Torresen J, Nordgreen T, Oedegaard KJ, Fasmer OB. Motor activity based classification of depression in unipolar and bipolar patients. Proceedings of the 2018 IEEE 31st International Symposium on Computer-Based Medical Systems (CBMS); IEEE 31st International Symposium on Computer-Based Medical Systems (CBMS); Jun 18-21, 2018; Karlstad, Sweden. 2018. pp. 316–321. https://ieeexplore.ieee.org/document/8417257 . [DOI] [Google Scholar]
- 37.Ghandeharioun A, Fedor S, Sangermano L, Ionescu D, Alpert J, Dale C, Sontag D, Picard R. Objective assessment of depressive symptoms with machine learning and wearable sensors data. Proceedings of the 2017 Seventh International Conference on Affective Computing and Intelligent Interaction (ACII); The Seventh International Conference on Affective Computing and Intelligent Interaction (ACII); Oct 23-26, 2017; San Antonio, TX, USA. 2017. pp. 325–332. https://ieeexplore.ieee.org/document/8273620 . [DOI] [Google Scholar]
- 38.Griffiths C, da Silva KM, Leathlean C, Jiang H, Ang CS, Searle R. Investigation of physical activity, sleep, and mental health recovery in treatment resistant depression (TRD) patients receiving repetitive transcranial magnetic stimulation (rTMS) treatment. J Affect Disord Rep. 2022 Apr;8:100337. doi: 10.1016/j.jadr.2022.100337. https://linkinghub.elsevier.com/retrieve/pii/S2666-9153(22)00030-0 .S2666-9153(22)00030-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gu J, Gao B, Chen Y, Jiang L, Gao Z, Ma X, Ma Y, Woo WL, Jin J. Wearable social sensing: content-based processing methodology and implementation. IEEE Sensors J. 2017 Nov 1;17(21):7167–76. doi: 10.1109/jsen.2017.2754289. [DOI] [Google Scholar]
- 40.Ihmig FR, Neurohr-Parakenings F, Schäfer SK, Lass-Hennemann J, Michael T. On-line anxiety level detection from biosignals: machine learning based on a randomized controlled trial with spider-fearful individuals. PLoS One. 2020;15(6):e0231517. doi: 10.1371/journal.pone.0231517. https://dx.plos.org/10.1371/journal.pone.0231517 .PONE-D-19-29665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jacobson NC, Lekkas D, Huang R, Thomas N. Deep learning paired with wearable passive sensing data predicts deterioration in anxiety disorder symptoms across 17-18 years. J Affect Disord. 2021 Mar 01;282:104–11. doi: 10.1016/j.jad.2020.12.086. https://europepmc.org/abstract/MED/33401123 .S0165-0327(20)33176-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jacobson NC, Weingarden H, Wilhelm S. Digital biomarkers of mood disorders and symptom change. NPJ Digit Med. 2019 Feb 1;2(1):3. doi: 10.1038/s41746-019-0078-0. doi: 10.1038/s41746-019-0078-0.78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jakobsen P, Garcia-Ceja E, Riegler M, Stabell LA, Nordgreen T, Torresen J, Fasmer OB, Oedegaard KJ. Applying machine learning in motor activity time series of depressed bipolar and unipolar patients compared to healthy controls. PLoS One. 2020 Aug 24;15(8):e0231995. doi: 10.1371/journal.pone.0231995. https://dx.plos.org/10.1371/journal.pone.0231995 .PONE-D-20-09443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jin J, Gao B, Yang S, Zhao B, Luo L, Woo WL. Attention-block deep learning based features fusion in wearable social sensor for mental wellbeing evaluations. IEEE Access. 2020;8:89258–68. doi: 10.1109/access.2020.2994124. [DOI] [Google Scholar]
- 45.Khan NS, Ghani MS, Anjum G. ADAM-sense: anxiety-displaying activities recognition by motion sensors. Pervasive Mobile Comput. 2021 Dec;78:101485. doi: 10.1016/j.cmpb.2021.106007. doi: 10.1016/j.cmpb.2021.106007. [DOI] [Google Scholar]
- 46.Kim H, Lee S, Lee S, Hong S, Kang H, Kim N. Depression prediction by using ecological momentary assessment, Actiwatch data, and machine learning: observational study on older adults living alone. JMIR Mhealth Uhealth. 2019 Oct 16;7(10):e14149. doi: 10.2196/14149. https://mhealth.jmir.org/2019/10/e14149/ v7i10e14149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kulam S. Time-series classification with uni-dimensional convolutional neural networks: an experimental comparison with long short-term memory networks. Scinapse. 2019. Jan 1, [2022-10-11]. https://www.scinapse.io/papers/3018311128 .
- 48.Kumar A, Sangwan SR, Arora A, Menon VG. Depress-DCNF: a deep convolutional neuro-fuzzy model for detection of depression episodes using IoMT. Applied Soft Comput. 2022 Jun;122:108863. doi: 10.1016/j.asoc.2022.108863. doi: 10.1016/j.asoc.2022.108863. [DOI] [Google Scholar]
- 49.Llamocca P, López V, Santos M, Čukić M. Personalized characterization of emotional states in patients with bipolar disorder. Mathematics. 2021 May 22;9(11):1174. doi: 10.3390/math9111174. [DOI] [Google Scholar]
- 50.Lu J, Shang C, Yue C, Morillo R, Ware S, Kamath J, Bamis A, Russell A, Wang B, Bi J. Joint modeling of heterogeneous sensing data for depression assessment via multi-task learning. Proc ACM Interact Mob Wearable Ubiquitous Technol. 2018 Mar 26;2(1):1–21. [Google Scholar]
- 51.Mahendran N, Vincent DR, Srinivasan K, Chang C, Garg A, Gao L, Reina DG. Sensor-assisted weighted average ensemble model for detecting major depressive disorder. Sensors (Basel) 2019 Nov 06;19(22):4822. doi: 10.3390/s19224822. https://www.mdpi.com/resolver?pii=s19224822 .s19224822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Makhmutova M, Kainkaryam R, Ferreira M, Min J, Jaggi M, Clay I. Predicting changes in depression severity using the PSYCHE-D (prediction of severity change-depression) model involving person-generated health data: longitudinal case-control observational study. JMIR Mhealth Uhealth. 2022 Mar 25;10(3):e34148. doi: 10.2196/34148. https://mhealth.jmir.org/2022/3/e34148/ v10i3e34148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mallikarjun H, Manimegalai P. Manoglanistara - emotional wellness phases prediction of adolescent female students by using brain waves. Current Signal Transduction Ther. 2021 Jan 15;15(3):315–23. doi: 10.2174/1574362414666190703151853. [DOI] [Google Scholar]
- 54.McGinnis EW, Scism J, Hruschak J, Muzik M, Rosenblum KL, Fitzgerald K, Copeland W, McGinnis RS. Digital phenotype for childhood internalizing disorders: less positive play and promise for a brief assessment battery. IEEE J Biomed Health Inform. 2021 Aug;25(8):3176–84. doi: 10.1109/jbhi.2021.3053846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McGinnis RS, McGinnis EW, Hruschak J, Lopez-Duran NL, Fitzgerald K, Rosenblum KL, Muzik M. Rapid anxiety and depression diagnosis in young children enabled by wearable sensors and machine learning. Proceedings of the 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC); 40th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC); Jul 18-21, 2018; Honolulu, HI, USA. 2004. [DOI] [PubMed] [Google Scholar]
- 56.McGinnis RS, McGinnis EW, Hruschak J, Lopez-Duran NL, Fitzgerald K, Rosenblum KL, Muzik M. Rapid detection of internalizing diagnosis in young children enabled by wearable sensors and machine learning. PLoS One. 2019 Jan 16;14(1):e0210267. doi: 10.1371/journal.pone.0210267. https://dx.plos.org/10.1371/journal.pone.0210267 .PONE-D-18-15797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Minaeva O, Riese H, Lamers F, Antypa N, Wichers M, Booij SH. Screening for depression in daily life: development and external validation of a prediction model based on actigraphy and experience sampling method. J Med Internet Res. 2020 Dec 01;22(12):e22634. doi: 10.2196/22634. https://www.jmir.org/2020/12/e22634/ v22i12e22634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Miranda D, Favela J, Arnrich B. Detecting anxiety states when caring for people with dementia. Methods Inf Med. 2018 Jan 22;56(01):55–62. doi: 10.3414/me15-02-0012. [DOI] [PubMed] [Google Scholar]
- 59.Mullick T, Radovic A, Shaaban S, Doryab A. Predicting depression in adolescents using mobile and wearable sensors: multimodal machine learning-based exploratory study. JMIR Form Res. 2022 Jun 24;6(6):e35807. doi: 10.2196/35807. https://formative.jmir.org/2022/6/e35807/ v6i6e35807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Narziev N, Goh H, Toshnazarov K, Lee SA, Chung K, Noh Y. STDD: short-term depression detection with passive sensing. Sensors (Basel) 2020 Mar 04;20(5):1396. doi: 10.3390/s20051396. https://www.mdpi.com/resolver?pii=s20051396 .s20051396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nath RK, Thapliyal H. Machine learning-based anxiety detection in older adults using wristband sensors and context feature. SN Comput Sci. 2021 Jun 26;2(5) doi: 10.1007/s42979-021-00744-z. [DOI] [Google Scholar]
- 62.Nguyen DK, Chan CL, Li AH, Phan DV. Deep Stacked Generalization Ensemble Learning models in early diagnosis of depression illness from wearable devices data. Proceedings of the 5th International Conference on Medical and Health Informatics; ICMHI 2021: 2021 5th International Conference on Medical and Health Informatics; May 14 - 16, 2021; Kyoto Japan. 2021. pp. 7–12. https://dl.acm.org/doi/fullHtml/10.1145/3472813.3472815 . [DOI] [Google Scholar]
- 63.Sensor- and Video-Based Activity and Behavior Computing: Proceedings of 3rd International Conference on Activity and Behavior Computing (ABC 2021) Singapore: Springer; 2022. [Google Scholar]
- 64.Opoku Asare K, Moshe I, Terhorst Y, Vega J, Hosio S, Baumeister H, Pulkki-Råback L, Ferreira D. Mood ratings and digital biomarkers from smartphone and wearable data differentiates and predicts depression status: a longitudinal data analysis. Pervasive Mobile Comput. 2022 Jul;83:101621. doi: 10.1016/j.asoc.2022.108863. doi: 10.1016/j.asoc.2022.108863. [DOI] [Google Scholar]
- 65.Pacheco-González SL, Zanella-Calzada LA, Galván-Tejada CE, Chávez-Lamas NM, Rivera-Gómez JF, Galván-Tejada JI. Evaluation of five classifiers for depression episodes detection. Res Comput Sci. 2019 Dec 31;148(10):129–38. [Google Scholar]
- 66.Pedrelli P, Fedor S, Ghandeharioun A, Howe E, Ionescu DF, Bhathena D, Fisher LB, Cusin C, Nyer M, Yeung A, Sangermano L, Mischoulon D, Alpert JE, Picard RW. Monitoring changes in depression severity using wearable and mobile sensors. Front Psychiatry. 2020 Dec 18;11:584711. doi: 10.3389/fpsyt.2020.584711. https://europepmc.org/abstract/MED/33391050 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Qian K, Kuromiya H, Ren Z, Schmitt M, Zhang Z, Nakamura T, Yoshiuchi K, Schuller BW, Yamamoto Y. Automatic Detection of Major Depressive Disorder via a Bag-of-Behaviour-Words Approach. Proceedings of the Third International Symposium on Image Computing and Digital Medicine. 2019:71–75. doi: 10.1145/3364836.3364851. [DOI] [Google Scholar]
- 68.Raihan M, Bairagi AK, Rahman S. A machine learning based study to predict depression with monitoring Actigraph watch data. Proceedings of the 2021 12th International Conference on Computing Communication and Networking Technologies (ICCCNT); 2021 12th International Conference on Computing Communication and Networking Technologies (ICCCNT); Jul 06-08, 2021; Kharagpur, India. 2021. pp. 1–5. https://ieeexplore.ieee.org/document/9579614 . [DOI] [Google Scholar]
- 69.Rodríguez-Ruiz JG, Galván-Tejada CE, Luna-García H, Gamboa-Rosales H, Celaya-Padilla JM, Arceo-Olague JG, Galván Tejada JI. Classification of depressive and schizophrenic episodes using night-time motor activity signal. Healthcare (Basel) 2022 Jul 05;10(7):1256. doi: 10.3390/healthcare10071256. https://www.mdpi.com/resolver?pii=healthcare10071256 .healthcare10071256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rodríguez-Ruiz JG, Galván-Tejada CE, Vázquez-Reyes S, Galván-Tejada JI, Gamboa-Rosales H. Classification of depressive episodes using nighttime data; a multivariate and univariate analysis. Program Comput Soft. 2020 Dec 22;46(8):689–98. doi: 10.1134/s0361768820080198. [DOI] [Google Scholar]
- 71.Rodríguez-Ruiz JG, Galván-Tejada CE, Zanella-Calzada LA, Celaya-Padilla JM, Galván-Tejada JI, Gamboa-Rosales H, Luna-García H, Magallanes-Quintanar R, Soto-Murillo MA. Comparison of night, day and 24 h motor activity data for the classification of depressive episodes. Diagnostics (Basel) 2020 Mar 17;10(3):162. doi: 10.3390/diagnostics10030162. https://www.mdpi.com/resolver?pii=diagnostics10030162 .diagnostics10030162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rother R, Sun Y, Lo B. Living in the Internet of Things (IoT 2019) London: The Institution of Engineering and Technology; 2019. Internet of things based pervasive sensing of psychological anxiety via wearable devices under naturalistic settings. [Google Scholar]
- 73.Rykov Y, Thach T, Bojic I, Christopoulos G, Car J. Digital biomarkers for depression screening with wearable devices: cross-sectional study with machine learning modeling. JMIR Mhealth Uhealth. 2021 Oct 25;9(10):e24872. doi: 10.2196/24872. https://mhealth.jmir.org/2021/10/e24872/ v9i10e24872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Saha K, Grover T, Mattingly SM, swain VD, Gupta P, Martinez GJ, Robles-Granda P, Mark G, Striegel A, De Choudhury M. Person-centered predictions of psychological constructs with social media contextualized by multimodal sensing. Proc ACM Interact Mob Wearable Ubiquitous Technol. 2021 Mar 19;5(1):1–32. [Google Scholar]
- 75.Šalkevicius J, Damaševičius R, Maskeliunas R, Laukienė I. Anxiety level recognition for virtual reality therapy system using physiological signals. Electronics. 2019 Sep 16;8(9):1039. doi: 10.3390/electronics8091039. [DOI] [Google Scholar]
- 76.Scism J. Applications of wearable sensors in delivering biologically relevant signals. University of Vermont. 2020. [2022-10-11]. https://scholarworks.uvm.edu/cgi/viewcontent.cgi?article=2314&context=graddis .
- 77.Shah RV, Grennan G, Zafar-Khan M, Alim F, Dey S, Ramanathan D, Mishra J. Personalized machine learning of depressed mood using wearables. Transl Psychiatry. 2021 Jun 09;11(1):338. doi: 10.1038/s41398-021-01445-0. doi: 10.1038/s41398-021-01445-0.10.1038/s41398-021-01445-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Shaukat-Jali R, van Zalk N, Boyle DE. Detecting subclinical social anxiety using physiological data from a wrist-worn wearable: small-scale feasibility study. JMIR Form Res. 2021 Oct 07;5(10):e32656. doi: 10.2196/32656. https://formative.jmir.org/2021/10/e32656/ v5i10e32656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tazawa Y, Liang K, Yoshimura M, Kitazawa M, Kaise Y, Takamiya A, Kishi A, Horigome T, Mitsukura Y, Mimura M, Kishimoto T. Evaluating depression with multimodal wristband-type wearable device: screening and assessing patient severity utilizing machine-learning. Heliyon. 2020 Feb;6(2):e03274. doi: 10.1016/j.heliyon.2020.e03274. https://linkinghub.elsevier.com/retrieve/pii/S2405-8440(20)30119-5 .S2405-8440(20)30119-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tiwari A, Cassani R, Narayanan SS, Falk TH. A comparative study of stress and anxiety estimation in ecological settings using a smart-shirt and a smart-bracelet. Proceedings of the Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Conference; Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. Conference; Jul 23-27, 2019; Berlin, Germany. 2019. [DOI] [PubMed] [Google Scholar]
- 81.Tsai C, Chen P, Liu D, Kuo Y, Hsieh T, Chiang D, Lai F, Wu C. Panic attack prediction using wearable devices and machine learning: development and cohort study. JMIR Med Inform. 2022 Feb 15;10(2):e33063. doi: 10.2196/33063. https://medinform.jmir.org/2022/2/e33063/ v10i2e33063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Valenza G, Citi L, Gentili C, Lanata A, Scilingo EP, Barbieri R. Characterization of depressive states in bipolar patients using wearable textile technology and instantaneous heart rate variability assessment. IEEE J Biomed Health Inform. 2015 Jan;19(1):263–74. doi: 10.1109/jbhi.2014.2307584. [DOI] [PubMed] [Google Scholar]
- 83.Wang R, Wang W, daSilva A, Huckins JF, Kelley WM, Heatherton TF, Campbell AT. Tracking depression dynamics in college students using mobile phone and wearable sensing. Proc ACM Interact Mob Wearable Ubiquitous Technol. 2018 Mar 26;2(1):1–26. [Google Scholar]
- 84.Xu X, Chikersal P, Doryab A, Villalba DK, Dutcher JM, Tumminia MJ, Althoff T, Cohen S, Creswell KG, Creswell JD, Mankoff J, Dey AK. Leveraging routine behavior and contextually-filtered features for depression detection among college students. Proc ACM Interact Mob Wearable Ubiquitous Technol. 2019 Sep 09;3(3):1–33. [Google Scholar]
- 85.Yadav M, Sakib MN, Feng K, Chaspari T, Behzadan A. Virtual reality interfaces and population-specific models to mitigate public speaking anxiety. Proceedings of the 8th International Conference on Affective Computing and Intelligent Interaction (ACII); The 8th International Conference on Affective Computing and Intelligent Interaction (ACII); Sep 03-06, 2019; Cambridge, UK. 2022. pp. 1–7. https://ieeexplore.ieee.org/document/8925509 . [DOI] [Google Scholar]
- 86.Zanella-Calzada L, Galván-Tejada CE, Chávez-Lamas NM, Gracia-Cortés MD, Magallanes-Quintanar R, Celaya-Padilla J, Galván-Tejada JI, Gamboa-Rosales H. Feature extraction in motor activity signal: towards a depression episodes detection in unipolar and bipolar patients. Diagnostics (Basel) 2019 Jan 10;9(1):8. doi: 10.3390/diagnostics9010008. https://www.mdpi.com/resolver?pii=diagnostics9010008 .diagnostics9010008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zheng Y, Wong TC, Leung BH, Poon CC. Unobtrusive and multimodal wearable sensing to quantify anxiety. IEEE Sensors J. 2016 May;16(10):3689–96. doi: 10.1109/jsen.2016.2539383. [DOI] [Google Scholar]
- 88.Kang M, Chai K. Wearable sensing systems for monitoring mental health. Sensors (Basel) 2022 Jan 27;22(3):994. doi: 10.3390/s22030994. https://www.mdpi.com/resolver?pii=s22030994 .s22030994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Byeon H. Relationship between physical activity level and depression of elderly people living alone. Int J Environ Res Public Health. 2019 Oct 22;16(20):4051. doi: 10.3390/ijerph16204051. https://www.mdpi.com/resolver?pii=ijerph16204051 .ijerph16204051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Puccinelli PJ, da Costa TS, Seffrin A, de Lira CA, Vancini RL, Nikolaidis PT, Knechtle B, Rosemann T, Hill L, Andrade MS. Correction to: reduced level of physical activity during COVID-19 pandemic is associated with depression and anxiety levels: an internet-based survey. BMC Public Health. 2021 Mar 29;21(1):613. doi: 10.1186/s12889-021-10684-1. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-021-10684-1 .10.1186/s12889-021-10684-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chalmers JA, Quintana DS, Abbott MJ, Kemp AH. Anxiety disorders are associated with reduced heart rate variability: a meta-analysis. Front Psychiatry. 2014 Jul 11;5:80. doi: 10.3389/fpsyt.2014.00080. https://europepmc.org/abstract/MED/25071612 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Nelson BW, Allen NB. Accuracy of consumer wearable heart rate measurement during an ecologically valid 24-hour period: intraindividual validation study. JMIR Mhealth Uhealth. 2019 Mar 11;7(3):e10828. doi: 10.2196/10828. https://mhealth.jmir.org/2019/3/e10828/ v7i3e10828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bent B, Goldstein BA, Kibbe WA, Dunn JP. Investigating sources of inaccuracy in wearable optical heart rate sensors. NPJ Digit Med. 2020;3:18. doi: 10.1038/s41746-020-0226-6. doi: 10.1038/s41746-020-0226-6.226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hunkin H, King DL, Zajac IT. Perceived acceptability of wearable devices for the treatment of mental health problems. J Clin Psychol. 2020 Jun;76(6):987–1003. doi: 10.1002/jclp.22934. [DOI] [PubMed] [Google Scholar]
- 95.Lovato N, Gradisar M. A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med Rev. 2014 Dec;18(6):521–9. doi: 10.1016/j.smrv.2014.03.006.S1087-0792(14)00039-2 [DOI] [PubMed] [Google Scholar]
- 96.Ramsawh HJ, Stein MB, Belik SL, Jacobi F, Sareen J. Relationship of anxiety disorders, sleep quality, and functional impairment in a community sample. J Psychiatr Res. 2009 Jul;43(10):926–33. doi: 10.1016/j.jpsychires.2009.01.009.S0022-3956(09)00021-1 [DOI] [PubMed] [Google Scholar]
- 97.Murnane EL, Cosley D, Chang P, Guha S, Frank E, Gay G, Matthews M. Self-monitoring practices, attitudes, and needs of individuals with bipolar disorder: implications for the design of technologies to manage mental health. J Am Med Inform Assoc. 2016 May;23(3):477–84. doi: 10.1093/jamia/ocv165.ocv165 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews) checklist.
Search strategy.
Data extraction form.
Characteristics of each included study.
Features of wearable devices.
Features of the sensors of wearable devices.
Features of artificial intelligence algorithms.
Features of the data used in artificial intelligence algorithms.
Data Availability Statement
The data supporting the findings of this study are available from the corresponding author upon reasonable request.


