Abstract
Background
Dynamic balance is a vital aspect of everyday life. It is important to incorporate an exercise program that is useful for maintaining and improving balance in patients with chronic low back pain (CLBP). However, there is a lack of evidence supporting the effectiveness of spinal stabilization exercises (SSEs) on improving dynamic balance.
Purpose
To determine the effectiveness of SSEs on dynamic balance in adults with CLBP.
Study Design
A double-blind randomized clinical trial.
Methods
Forty participants with CLBP were assigned randomly into either an SSE group or a general exercise (GE) group, which consisted of flexibility and range-of-motion exercises. Participants attended a total of four to eight supervised physical therapy (PT) sessions and performed their assigned exercises at home in the first four weeks of the eight-week intervention. In the last four weeks, the participants performed their exercises at home with no supervised PT sessions. Participants’ dynamic balance was measured using the Y-Balance Test (YBT) and the normalized composite scores, Numeric Pain Rating Scale and Modified Oswestry Low Back Pain Disability Questionnaire scores were collected at baseline, two weeks, four weeks, and eight weeks.
Results
A significant difference between groups from two weeks to four weeks (p = 0.002) was found, with the SSE group demonstrating higher YBT composite scores than the GE group. However, there were no significant between-group differences from baseline to two weeks (p =0.098), and from four weeks to eight weeks (p = 0.413).
Conclusions
Supervised SSEs were superior to GEs in improving dynamic balance for the first four weeks after initiating intervention in adults with CLBP. However, GEs appeared to have an effect equivalent to that of SSEs after 8-week intervention.
Levels of Evidence
1b.
Keywords: Instability, Lumbar spine, Movement impairment, Postural stability, Supervised exercises
INTRODUCTION
Low back pain (LBP) is the leading cause of disability and a primary contributor to work absenteeism and loss of productivity globally.1–4 Over 50% of individuals with chronic LBP (CLBP) may not recover until one year later.2 Impairments from LBP include mobility deficits,5 physical disabilities,6 and balance disturbances.7–10 Several studies have identified alterations in muscle recruitment and movement patterns as potential pathomechanisms which further lead to spinal instability.6–9,11 Recently, evidence revealed that dynamic balance is reduced in individuals with CLBP and in individuals with a history of LBP as compared to asymptomatic controls.7,8 The reduced use of the lumbopelvic movement to maintain balance has been reported to be due to the reduced motion of the lumbar spine and hip.12 Furthermore, once individuals with LBP lose their balance, they have more difficulty regaining it, and balance deficits can persist even after their LBP has subsided.8 Although pain is a major factor in CLBP, pain is not the only impairment present in CLBP populations. Balance abnormalities and pain-avoiding compensations could further contribute to an individual’s increased re-injury risk and chronicity.2,8,9 Moreover, individuals with LBP can be fearful of performing dynamic tasks because of a fear of additional pain and injury in response to the movement.2,8,9
Uncertainty remains regarding the best treatment approach for LBP. Evidence suggests that exercise therapy is a moderately effective intervention for treating LBP.6,13 A systematic review found that therapeutic exercises were associated with small-to-moderate effects on pain and with an increased likelihood of return-to-work for patients with LBP.13 Spinal stabilization exercise (SSE) programs are widely used by physical therapists for rehabilitation of patients with LBP.14–17 Evidence has shown that recruitment of spinal stabilization muscles (e.g., transversus abdominis and lumbar multifidi) may be altered in patients with LBP as compared to healthy controls. It has been proposed that SSEs are used to retrain proper activation and coordination of the trunk musculature to increase spinal stability and reduce pain.14–18 SSEs also have been shown to be effective for improving pain, disability, and physical performance in patients with LBP.4,16–18 Systematic reviews have indicated that SSEs were more effective than general exercises for decreasing pain and improving disability in patients with LBP.4,16,18 Furthermore, recent research reports showed that some forms of SSEs have promising outcomes on postural control in patients with LBP.19,20
Although balance has been used as an outcome measure to examine the effects of SSEs on patients with LBP, the balance measures commonly used in the literature consist of only static postural control assessments and lack dynamic component assessments.21,22 For instance, force plates and the NeuroCom Balance Master® measure ground reaction forces and center of pressure (CoP) displacement, and both provide quantified measures of static or semi-dynamic postural control, but do not measure an individual’s ability to maintain balance while performing a purposeful maneuver.8,21,22 Moreover, these static balance tests usually are used in a laboratory setting, are expensive and time-consuming, and often are impractical for use in clinical settings.8,21
In recent years, several tests have been used to investigate dynamic balance in LBP populations, such as the Star Excursion Balance Test (SEBT),7,10,23,24 the Y-Balance Test (YBT),8,25 and the functional reach test.26,27 Of these dynamic tests, the reliability and validity of the YBT has been established specifically for the CLBP population. In addition, the YBT is a shorter version of the SEBT, and is more feasible for clinical practice. The YBT evaluates single-leg-balance, dynamic neuromuscular control, proprioception, and strength of an individual while simultaneously moving the non-stance limb in anterior (ANT), posteromedial (PM), and posterolateral (PL) directions.21,28,29 The YBT is portable and easy to administer, and it requires little training, making it practical to use in multiple settings.8,25,28,29 Recently, a relaiblity and validity study aimed to determine the inter-rater reliability of the YBT and to compare dynamic balance between young adults with CLBP and an asymptomatic group found that the YBT had an excellent inter-rater reliability, with intraclss correlation coefficients ranging from 0.99 to 1.0. In addition, the CLBP group had a significantly lower composite score (p < 0.001) and shorter reach distances in the ANT (p = 0.023), PM (p < 0.001), and PL (p = 0.001) directions than the asymptomatic group.25
Initial evidence regarding the effect of SSEs on postural control in patients with LBP has been encouraging; however, balance measures used in these studies primarily assessed static postural control and did not have dynamic components, which are imperative for performing daily functional activities. Additionally, these static balance tests are impractical for use in clinical settings. Given that dynamic balance is a vital aspect of everyday life and that diminished balance is a well-recognized impairment in individuals with LBP, including athletic patients with CLBP who are physically active, it is important to routinely include a relatively quick and cost-effective balance test in physical therapy (PT) practice, and to incorporate an exercise program that is useful for maintaining and improving balance in LBP populations. However, there is a lack of evidence supporting the effectiveness of SSEs on improving dynamic balance. To date, no randomized clinical trials have been conducted to assess the effectiveness of SSEs on dynamic balance in adults with CLBP using the YBT. Therefore, the primary purpose of this study was to determine the effectiveness of SSEs on dynamic balance in adults with CLBP. The secondary purpose of this study was to examine whether or not the participants who received an SSE program (treatment group) would have greater improvement in pain intensity and disability level than those who received a general exercise (GE) program (placebo group). The GE program consisted of general range-of-motion (ROM) and flexibility exercises.
METHODS
Study Design
This study was a double-blinded randomized clinical trial, to compare two exercise programs: SSE vs. GE on dynamic balance, pain intensity, and disability level in adults with CLBP. The two independent variables were group, which was a between-subject factor, and time, which was a within-subject factor. The independent variable of group had two levels: (1) the treatment group which received SSEs, and (2) the placebo group, which received general ROM and flexibility exercises. The independent variable of time had four levels: baseline, and 2 weeks, 4 weeks, and 8 weeks after intervention. The three dependent variables were: (1) dynamic balance measured by the YBT, (2) pain intensity measured by the Numeric Pain Rating Scale (NPRS), and (3) disability level measured by the Modified Oswestry Low Back Pain Disability Questionnaire (OSW).
Participants
The sample size for this study was determined based on a priori power analysis using G*Power version 3.1.9 using a small-to-medium effect size of 0.20 and an alpha level of 0.05.30 Based on the analysis, 40 participants were needed to ensure an adequate power level of 0.80 for a mixed-model analysis of variance (ANOVA) test. Participants were recruited regardless of ethnicity, sex, or race through flyers, word of mouth marketing, and emails. Approval from the Texas Woman’s University institutional review board was obtained for the study, and it was registered with ClinicalTrials.gov (NCT03597191). Once the participant agreed to participate in the study, the participant signed a written informed consent form. Consenting participants were screened for their eligibility, and those who qualified were assigned randomly to one of the two groups. Eligible participants were individuals who had CLBP (back pain for a duration of more than 12 weeks).2 Additional inclusion criteria included: (1) age of 18 to 65 years; (2) ability to understand, speak, and follow verbal instructions in English; and (3) a minimum pain intensity score of 2/10 using the NPRS in the past week.
Participants were excluded from the study if they have had or reported any of the following: (1) serious spinal conditions, such as fracture, infection, or tumor; (2) signs of nerve root compression; (3) a history of lower extremity or lumbar spine surgery; (4) a history of hip, knee, or ankle pain in the previous two years; (5) current pregnancy; (6) systemic disease (e.g., rheumatologic or neurological disorders); (7) vestibular or other balance disorders; (8) ongoing treatment for inner ear, sinus, or upper respiratory infection; (9) a concussion within the previous three months; (10) a history of falls or fear of falling; and (11) a need for any form of walking aids (cane, walker). Participants were screened with neurological tests, which included reflexes, sensation, strength, and the straight-leg-raise (SLR) test for the lower extremities to further assess their eligibility for the study. The SLR test was considered positive when pain referred below the knee was present during passive SLR testing and was used to rule out participants with lumbar radiculopathy. These neurological tests are parts of a standard PT examination used in clinics for assessing neurological signs and symptoms. In addition, a physical examination was performed based on the test procedures described by Hicks et al.14
Instrumentation and Outcome Measures
The Y-Balance Test Kit (Functional Movement Systems, Inc. Chatham, VA) was used to assess dynamic balance in this study. This kit contains a single central stance platform with three moveable reach indicators arranged in the ANT, PM, and PL directions. Dynamic balance of an individual is quantified by measuring how far the individual places the reach indicator relative to the stance platform while maintaining a unilateral stance. A farther reach distance is indicative of a greater dynamic balance.28 The YBT has been shown to be a reliable measure of dynamic balance, with intraclass correlation coefficients (ICCs) ranging from 0.85 to 0.91 for intra-tester reliability, and from 0.99 to 1.00 for inter-tester reliability.28 The reliability of composite reach scores has been reported to be good-to-excellent, with the ICCs being 0.91 for intra-tester and 0.99 for inter-tester reliability. The YBT has a minimal detectable change of 8.62 centimeters.28 The reach distances were measured in centimeters and were averaged and normalized to the participant’s leg length. Leg length was measured twice for each leg, and the two measurements were averaged. In particular, participants’ leg length was measured to the nearest millimeter using a tape measure from the inferior tip of the anterior superior iliac spine to the distal border of the ipsilateral medial malleolus with the participant lying supine on an examination table.25 The composite score was calculated by taking the average between the right and the left reach distances for all three directions and then summing the averages of the three reach directions. The score was then divided by three times the average leg length and multiplied by 100.31 The YBT composite scores were used for statistical analysis and collected at baseline, two weeks, four weeks, and eight weeks after intervention was initiated.
Examiners
Two investigators participated in this study. Investigator #1, the primary investigator (PI) was blinded to participants’ group assignment and intervention and performed the eligibility screening and standard PT examination for all participants. In addition, the PI collected the pre- and post-intervention measurements of dynamic balance using the YBT, pain scores using the NPRS, and disability level using the OSW. Investigator #2 was blinded to participants’ pre- and post-intervention measurements and was responsible for group allocation and administering the intervention, either an SSE program or a GE program, to participants in both groups.
Procedures
Eligible participants filled out an intake form, including questions about demographic data (age, sex, height, weight, occupation, limb dominance), duration of symptoms, painful side of the LBP, and physical activity level (minutes per week). The leg dominance was determined by asking the participants to report their preferred leg used when kicking a ball.32 In addition, participants completed the Fear-Avoidance Beliefs Questionnaire (FABQ) and Patient-Reported Outcomes Measurement Information System®-29 (PROMIS-29), which were used to describe the participants of this study. All participants were asked to rate their average pain intensity in the low back in the past week and to rate their current pain level using NPRS. Next, participants were asked to complete the OSW. The FABQ, PROMIS-29, NPRS, and OSW have been reliable and valid tools for assessing LBP-related fear-avoidance beliefs, participants’ traits, pain intensity, and perceived disability, respectively.33–38
Next, the YBT was used to assess participants’ dynamic balance. Each participant’s leg length was measured bilaterally in centimeters and was used to normalize reach distances because leg length has been shown to be a factor affecting YBT performance.39 Next, each participant was asked to slide a reach indicator along a pipe in the three testing directions: ANT, PM, and PL on both legs as described in details by Alshehre et al.25 The PI was responsible for giving verbal instructions and visual demonstrations of the YBT, as well as recording the YBT measures. The trial was discarded and retried when the participant (1) moved the foot of the stance leg from the platform or crossed the marked line, (2) kicked, pushed, or stepped on the reach indicator, (3) touched the floor with the reaching leg, or (4) lost balance before returning to the standing position. To reduce fatigue, participants were given a rest of a minimum 10 seconds between each reach and 30 seconds between each direction of testing.40 The reach distance was measured to the nearest centimeters by reading the line at the proximal edge of the reach indicator. Three successful test trials in each direction (ANT, PM, and PL) on each leg were recorded and normalized to the leg length and the composite score was used for data analysis.
Interventions
Participants in the treatment group were instructed in the SSEs, modeled after the SSE program designed by Hicks et al.14 Each participant was instructed to perform four exercises in total, one exercise from each of the following four categories: (a) abdominal bracing, (b) quadruped, (c) prone plank, and (d) side plank exercises. Each exercise was progressed and advanced in difficulty by increasing repetitions, hold times, and/or extremity movements. For the SSEs, the progression of exercises was based on the participants’ performance at each supervised PT session based on pre-established criteria by Hicks et al.14 The SSE program and criteria for progression are listed in Appendix A.
The placebo group performed a GE program, consisting of ROM and flexibility exercises for the low back and lower extremities. Each participant was instructed to perform four exercises in total, one exercise from each of the following four categories: (a) knee to chest, (b) lower trunk rotation, (c) prone press-ups, and (d) hamstring stretch exercises. These exercises were progressed by increasing repetitions and pain-free ROM. The exercise programs and criteria for progression are listed in Appendix B.
On the first visit, the participants in both groups were instructed in the exercises at a level that they could perform without pain. All participants were provided exercise handouts and also were asked to fill out an exercise log form to track the frequency of their home exercise sessions and to determine their compliance. In both groups, Investigator #2 instructed and corrected performance when necessary, and progressed the exercise program for each participant. As such, when participants performed the exercise with proper technique and without any rest breaks, they were instructed to progress to the next level of the exercise and were asked to discontinue the previous level of that exercise from their program. The proper technique was achieved by instructing the participants to tighten their abdominal muscles while breathing normally and maintaining a steady continuous muscle contraction with no recruitment of accessory muscles.41 Participants were instructed to perform the most updated exercises at home once a day at least five times a week.
The participants were asked to attend a total of four to eight supervised PT sessions and one follow-up session after the four-week intervention was completed for exercise progression and to ensure that they performed the exercises properly. Each session took about 30 to 45 minutes for exercise progression or an hour for collection of outcome measures and exercise progression. The intervention frequency and duration were chosen to reflect common PT practice. Each participant also was asked to perform their assigned exercise program at least five times per week, and the on-site visits were counted toward the required exercise frequency. After the 4-week intervention, each participant was asked to continue their exercise program at home five times a week for another four weeks. On their follow-up visit at week eight, the participants were instructed on how to progress their exercises.
All participants were instructed to bring the exercise log to each visit and to submit it to the investigators at the eight-week follow-up in order to determine compliance with the program. The average compliance was calculated using the completed exercise sessions divided by the prescribed exercise sessions. This equals to the number of exercise sessions completed out of the total possible exercise sessions. For this study, the average compliance for completing the prescribed home exercise program for the first four weeks (supervised PT sessions), the last four weeks (unsupervised PT sessions), and the total compliance for the duration of the study for both groups was calculated.
Data Analysis
All statistical analyses were performed using SPSS Statistics, Version 25 (IBM Corp., Armonk, NY, USA). Descriptive statistics, including frequencies, means, and standard deviations, were calculated for the demographic data of the participants and the outcome measures (YBT composite score, NPRS, and OSW). Independent t-tests were used for ratio data to determine if there was a difference between groups at baseline, including demographic data, such as age, weight, height, body mass index, and duration of symptoms, and baseline outcome measures. Chi-square analysis was used for non-ratio data to determine between-group differences for non-parametric baseline data, such as sex, onset of symptoms, pain distribution. Three separate 2 (group) x 4 (time) analyses of variance (ANOVAs) with repeated measures were used to determine any differences in the three outcome measures between groups. Follow-up analysis was performed if there was a significant interaction. The alpha level was set at 0.05 for all statistical analyses.
RESULTS
Fifty-three participants were recruited for the study and were also assessed for other outcomes. The CONSORT diagram in Figure 1 summarizes the screening, enrollment, randomization, and analysis of participants for this study. The 40 participants who completed this study were generally young with an average age of 39.9 ± 12.5 years and a range of 21 to 64 years. Both groups had lower physical activity levels (99.7 ± 145.1) than the recommended weekly minutes by the 2008 guidelines for adults, which is a minimum of 150 minutes per week.42 All participants had CLBP without signs of lumbar radiculopathy, with symptoms averaging for 95.2 ± 87.5 months. In addition, the participants had an average NPRS score of 3.5 ± 1.6 and an average OSW score of 18.1 ± 9.1, indicating that participants, in general, had relatively low pain intensity and a mild disability level. Table 1 describes the characteristics of the participants who completed the study.
Figure 1. Consort diagram of participants’ screening, enrollment, randomization, and analysis.
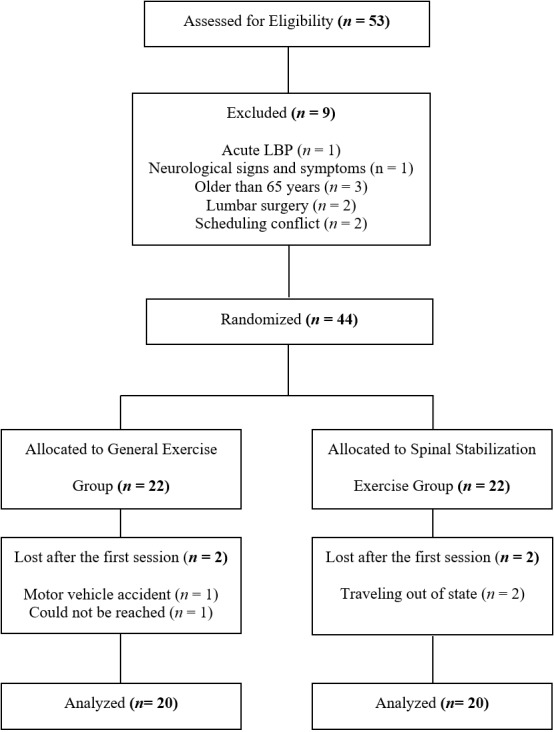
Table 1. Participants Characteristics at Baseline (Mean ± Standard Deviation).
| All Participants (n = 40) |
GE Group (n = 20) |
SSE Group (n = 20) |
p-value | |
|---|---|---|---|---|
| Age (years) | 39.9 ± 12.5 | 41.0 ± 13.3 | 38.8 ± 11.8 | 0.583 |
| Sex | 0.337 | |||
| Males | 23 (57.5%) | 10 (50%) | 13 (65%) | |
| Females | 17 (42.5%) | 10 (50%) | 7 (35%) | |
| Weight (kg) | 79.8 ± 15.7 | 81.1 ± 15.8 | 78.6 ± 16.0 | 0.625 |
| Height (cm) | 169.7 ± 10.1 | 172.3 ± 10.0 | 167.2 ± 9.8 | 0.112 |
| BMI (kg/m2) | 28.0 ± 6.6 | 27.5 ± 5.5 | 28.6 ± 7.7 | 0.612 |
| Leg dominance | 0.292 | |||
| Right | 36 (90%) | 19 (95%) | 17 (85%) | |
| Left | 4 (10%) | 1 (5%) | 3 (15%) | |
| Physical activity (min/wk.) | 99.7 ± 145.1 | 113.5 ± 127.8 | 86.0 ± 162.9 | 0.556 |
| Duration of LBP (months) | 95.2 ± 87.5 | 111.9 ± 86.3 | 78.6 ± 87.7 | 0.234 |
| Onset of LBP | 1.000 | |||
| Gradual | 36 (90%) | 18 (90%) | 18 (90%) | |
| Traumatic | 4 (10%) | 2 (10%) | 2 (10%) | |
| Painful side of LBP | 0.803 | |||
| Bilateral (Central) | 14 (35%) | 8 (40%) | 6 (30%) | |
| Unilateral | 26 (65%) | |||
| Right LBP | 13 (32.5%) | 6 (30%) | 7 (35%) | |
| Left LBP | 13 (32.5%) | 6 (30%) | 7 (35%) | |
| Pain distribution | 0.705 | |||
| LBP Only | 30 (75%) | 15 (75%) | 15 (75%) | |
| Above the knee | 1 (2.5%) | 1 (5%) | 0 | |
| Below the knee | 9 (22.5%) | 4 (20%) | 5 (25%) | |
| FABQ | ||||
| Physical activity scale | 10.1 ± 6.5 | 10.1 ± 5.6 | 10.1 ± 7.4 | 1.000 |
| Work scale | 8.4 ± 7.4 | 7.2 ± 8.1 | 9.5 ± 6.7 | 0.344 |
| PROMIS-29a | ||||
| Physical functionb | 43.4 ± 2.4 | 43.4 ± 2.4 | 43.4 ± 2.4 | 0.512 |
| Anxietyb | 51.2 ± 3.1 | 51.2 ± 3.1 | 53.7 ± 2.8 | 0.795 |
| Depressionb | 49.0 ± 3.2 | 49.0 ± 3.2 | 49.0 ± 3.2 | 0.815 |
| Fatigueb | 55.1 ± 2.4 | 53.1 ± 2.4 | 57.0 ± 2.3 | 0.229 |
| Sleep disturbanceb | 52.4 ± 3.4 | 52.4 ± 3.4 | 52.4 ± 3.4 | 0.695 |
| Social rolesb | 51.9 ± 2.2 | 53.7 ± 2.3 | 51.9 ± 2.2 | 0.487 |
| Pain interferenceb | 57.1 ± 1.9 | 57.1 ± 1.9 | 55.6 ± 1.9 | 0.558 |
| Pain intensity (0-10) | 4.3 ± 1.8 | 4.4 ± 2.3 | 4.1 ± 1.2 | 0.549 |
| Impact score (8-50)c | 20.1 ± 6.6 | 20.3 ± 6.5 | 19.9 ± 6.9 | 0.852 |
| NPRS (0-10) | ||||
| Current | 3.5 ± 1.6 | 3.5 ± 1.9 | 3.4 ± 1.3 | 0.846 |
| Average, past wk. | 4.7 ± 1.8 | 5.0 ± 2.2 | 4.5 ± 1.4 | 0.397 |
| OSW (%) | 18.1 ± 9.1 | 18.1 ± 9.4 | 18.2 ± 9.1 | 0.973 |
| YBT composite score (%LL) | 77.5 ± 12.1 | 72.9 ± 14.0 | 82.1 ± 7.7 | 0.014* |
GE = general exercise program, SSE = spinal stabilization exercise program, Kg = kilogram, cm = centimeter, m = meter, BMI = body mass index, min= minute, wk. = week, FABQ = Fear-Avoidance Beliefs Questionnaire, PROMIS-29 = Patient Reported Outcomes Measurement Information System, NPRS = Numeric Pain Rating Scale, OSW = Modified Oswestry Low Back Pain Disability Questionnaire, YBT = Y-Balance Test, %LL = Composite score normalized to leg length expressed as a percentage.
* indicates statistically significant, p < 0.05.a = p-values were computed using the raw scores, b = T-scores (population mean 50, standard deviation 10) available at the Assessment Center℠ website: http://assessmentcenter.net., c Impact score= Calculated as the sum of the reversed raw physical function score plus the raw pain interference score plus the pain intensity score.
Outcome Measurements
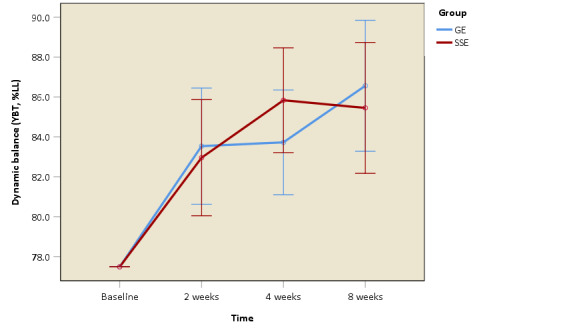
Table 2 displays the means and the standard deviations for the YBT, NPRS, and OSW at each time point. All three outcome measurements showed no significant differences between groups at baseline, except in the YBT composite scores. There was a significant difference in the dynamic balance between groups (t = -2.575, p = 0.014), with a lower YBT composite score in the GE group (72.9 ± 14.0) than in the SSE group (82.1 ± 7.7). Therefore, 2 x 4 ANCOVA with repeated measures was performed with the baseline YBT composite scores of all participants were used as covariates. The ANCOVA results revealed a statistically significant interaction of group by time for dynamic balance (F = 7.146, p < 0.001, partial η2 = 0.162), which indicates that there was a difference between the GE and SSE groups in dynamic balance over eight weeks as presented in Figure 2. Six separate 2 x 2 ANCOVAs with repeated measures were used to test for between-group differences in dynamic balance. A significant difference was found between groups from four weeks (p < 0.001) and eight weeks (p = 0.007) compared to baseline, and from two weeks to four weeks (p = 0.002), with the SSE group demonstrating higher YBT composite scores than the GE group. However, there were no statistically significant differences from baseline to two weeks (p = 0.098), two weeks to eight weeks (p = 0.107), and four weeks to eight weeks (p = 0.413) between groups. In addition, a significant main effect of time on the dynamic balance was found. Both groups demonstrated a significant improvement in dynamic balance from baseline to two weeks (p < 0.001), 2 weeks to 4 weeks (p = 0.023), and two weeks to eight weeks (p = 0.004), but there was no statistically significant difference from four weeks to eight weeks (p = 0.144) (Figure 2).
Table 2. Outcome Measurements (Mean ± Standard Deviation) at Baseline, 2 Weeks, 4 Weeks, and 8 Weeks after initiating intervention.
| All Participants (n = 40) |
GE Group (n = 20) |
SSE Group (n = 20) |
p-value | |
|---|---|---|---|---|
| Dynamic balance (YBT, %LL) | ||||
| Baseline | 77.5 ± 12.1 | 72.9 ± 14.0 | 82.1 ± 7.7 | 0.014* |
| 2 weeks | 83.2 ± 11.8 | 79.6 ± 13.3 | 86.8 ± 9.0 | |
| 4 weeks | 84.8 ± 9.9 | 80.7 ± 11.8 | 88.8 ± 5.5 | |
| 8 weeks | 86.0 ± 10.8 | 83.3 ± 12.0 | 88.7 ± 8.9 | |
| Pain intensity (NPRS, 1-10) | ||||
| Baseline | 3.5 ± 1.6 | 3.5 ± 1.9 | 3.4 ± 1.3 | 0.846 |
| 2 weeks | 2.9 ± 1.5 | 3.2 ± 1.8 | 2.5 ± 1.1 | |
| 4 weeks | 1.9 ± 1.7 | 2.2 ± 2.1 | 1.6 ± 1.1 | |
| 8 weeks | 2.0 ± 1.9 | 1.9 ± 1.9 | 2.0 ± 1.9 | |
| Disability level (OSW, 0-100%) | ||||
| Baseline | 18.1 ± 9.1 | 18.1 ± 9.4 | 18.2 ± 9.1 | 0.973 |
| 2 weeks | 15.7 ± 9.1 | 16.3 ± 9.1 | 15.1 ± 9.4 | |
| 4 weeks | 14.0 ± 9.8 | 15.4 ± 9.6 | 12.7 ± 9.9 | |
| 8 weeks | 12.3 ± 10.9 | 12.6 ± 9.1 | 12.0 ± 12.6 |
GE = general exercise program, SSE = spinal stabilization exercise program, p-values for between-group differences were determined by independent t-tests. YBT = Y-Balance Test, %LL = Composite score normalized to leg length expressed as a percentage, NPRS = Numeric Pain Rating Scale, OSW = Modified Oswestry Low Back Pain Disability Questionnaire.
* indicates statistically significant, p < 0.05.
Figure 2. Dynamic balance as measured by the Y-Balance Test (YBT) at baseline, and 2 weeks, 4 weeks, and 8 weeks after intervention was initiated, for both the general exercise (GE) group and the spinal-stabilization exercise (SSE) group.
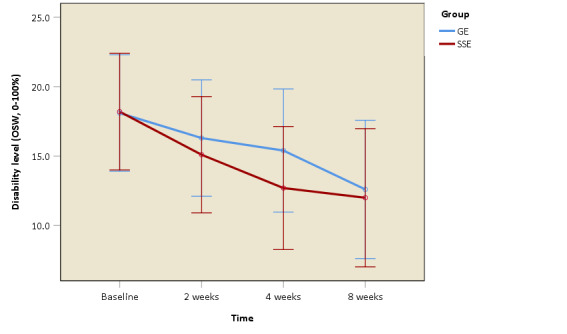
The ANOVA with repeated measures for the NPRS and OSW scores revealed no statistically significant interaction of group by time (F = 1.185, p = 0.319, partial η2 = 0.030), (F = 0.538, p = 0.605, partial η2 = 0.014), respectively. However, there was a significant main effect of time (p < 0.001) for both the NPRS and OSW scores. However, a significant main effect of time (p < 0.001) for both the NPRS and OSW scores was found. Post-hoc pair-wise comparisons showed significantly lower NPRS scores from baseline to two weeks (p = 0.007), from two weeks to four weeks (p < 0.001), but there was no statistically significant difference from four weeks to eight weeks (p = 0.818) (Figure 3). Similarly, post-hoc pair-wise reveled that both groups demonstrated a significant reduction in disability level from baseline to two weeks (p = 0.017), from two weeks to four weeks (p = 0.047), but there was no statistically significant difference from four weeks to eight weeks (p = 0.117) (Figure 4).
Figure 3. Pain intensity as measured by the Numeric Pain Rating Scale (NPRS) at baseline, and 2 weeks, 4 weeks, and 8 weeks after intervention was initiated, for both the general exercise (GE) group and the spinal-stabilization exercise (SSE) group.
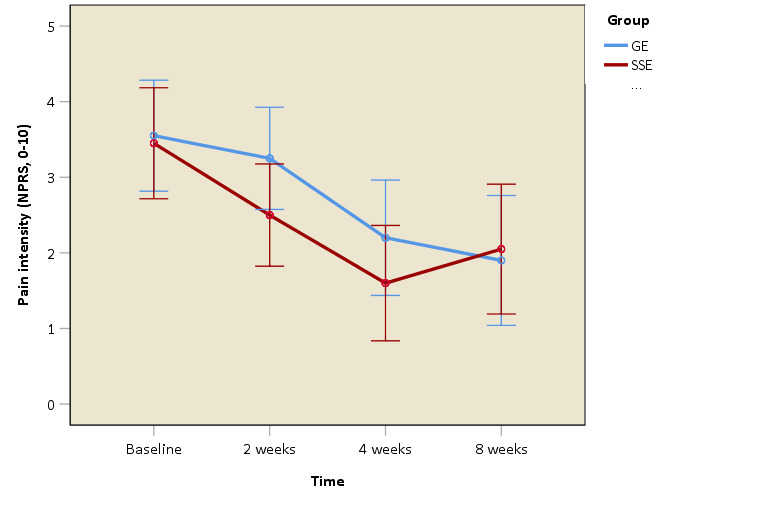
Figure 4. Disability level as measured by the Modified Oswestry Low Back Pain Disability Questionnaire (OSW) at baseline, and 2 weeks, 4 weeks, and 8 weeks after intervention was initiated, for both the general exercise (GE) group and the spinal-stabilization exercise (SSE) group.
Home Exercise Compliance
Table 3 lists the means, the standard deviations, and the compliance rates for home exercise compliance for both groups. No significant differences in compliance between the two groups for the duration of the study. However, paired t-tests for within-group differences revealed that the home exercise compliance was significantly higher during the first four weeks after initiating the intervention as compared to the last four weeks of intervention for both groups (t = 2.456, p = 0.024 for GE group, t = 2.163, p = 0.044 for SSE group). This indicates that all participants regardless of group performed their home exercises more often in the first four weeks, which included supervised PT sessions than they did in the last four weeks, which had no supervised PT sessions.
Table 3. Home Exercise Compliance (Mean ± Standard Deviation).
| All Participants (n = 40) |
GE Group (n = 20) |
SSE Group (n = 20) |
Between-group p-value |
|
| 0-4 weeks (%) | 85.9 ± 14.8 | 88.0 ± 15.6 | 83.7 ± 13.9 | 0.369 |
| 5-8 weeks (%) | 76.1 ± 22.7 | 77.5 ± 25.4 | 74.7 ± 20.4 | 0.707 |
| Total (%) | 81.0 ± 16.7 | 82.7 ± 18.8 | 79.2 ± 14.8 | 0.516 |
| Within-group p-value | 0.002* | 0.024* | 0.044* |
GE = general exercise program, SSE = spinal stabilization exercise program, p-values were determined by independent t-tests for between-group differences and paired t-tests for within-group differences. The within-group difference for both groups was determined by comparing the compliance of the first four weeks with the last four weeks.* indicates statistically significant, p < 0.05.
DISCUSSION
The results of this study show that four-week supervised SSEs were superior to GEs in improving dynamic balance in adults with CLBP after eight weeks of intervention. This implies that the SSE group was able to demonstrate better dynamic balance than the GE group for the first four weeks after initiating intervention, which included home exercises and supervised PT sessions. Then, the SSE group maintained the improvement of the first four weeks but showed no improvement in dynamic balance during the last four weeks, which included the participants performing exercises at home with no supervised PT sessions. However, there was no difference between the GE and the SSE groups in dynamic balance during the last four weeks of the intervention. These results support previous studies,19,20 which have shown that those with LBP who received SSEs for four weeks had significantly improved balance as compared to a control group. However, these two studies utilized different methods than the method used in the current study to assess balance, as Kim et al.19 and Rhee et al.20 used a pressure platform and force plates, respectively, to measure CoP excursions for balance ability. The authors of the prior studies hypothesized that SSEs might have improved neuromuscular responses to compensate for postural control deficits in patients with LBP.19,20
Given that balance is a motor control process which regulates movement quality and creates stability; improved neuromuscular control in this patient population can be achieved in part through strength from the lumbar spinal stabilizer muscles.43 Previous evidence has shown a delay in the firing of the deep abdominal muscles and decreased recruitment of the transversus abdominus and lumbar multifidus muscles in patients with CLBP as compared to asymptomatic individuals.14–17 Evidence also suggests that altered lumbar proprioception in those with LBP may cause reweighting of visual and vestibular sensory inputs to compensate for impaired proprioception in order to maintain an individual’s balance.44 An SSE program is a motor control intervention which has been used to retrain proper activation and coordination of the trunk musculature to increase spinal stability and reduce pain.14,18 In particular, spinal stabilization muscles, such as transversus abdominis and lumbar multifidi have been reported to play a major role in maintaining postural stability. Proper activation of these muscles in a feedforward mechanism reduces displacement of the body’s center of gravity.15 Based on these findings, it is speculated that SSEs may minimize faulty movement strategies and compensatory muscle contractions by properly coordinating abdominal and back musculature during functional tasks in the SSE group, which possibly led to better dynamic balance performance following the SSE program.
In contrast, a previous study reported that four weeks of SSEs combined with usual PT care (hot pack, ultrasound, and transcutaneous electric nerve stimulation) compared to usual PT care alone did not show greater improvement in postural control in patients with CLBP.45 However, balance was assessed differently between the studies. Salavati et al.45 assessed postural control using a Biodex Balance System®. In the current study, balance was measured using the YBT, which could be considered a more challenging balance task. It also could be argued that the two studies measured different constructs related to balance.
After the four-week supervised intervention, there was a trend that the GE group improved in dynamic balance during the last four weeks of the study. The GEs were designed to be similar to the SSEs in terms of frequency, duration, and number of one-on-one supervised PT sessions as well as contact time with the treating physical therapist. It is likely that the GEs, which consisted of ROM and flexibility exercises for the low back and lower extremities, could be learned more easily and performed independently at home by the participants, whereas SSEs may require supervised PT training. The SSEs could be considered a more complex exercise regimen and may require higher cognitive skills to be learned and performed as compared to the GEs. In addition, in terms of exercises intensity, it could be argued that level three of the GEs could be easier to perform, whereas level three of the SSEs could be considered more difficult, requiring more effort and PT supervision to perform correctly. Therefore, it is possible that the SSE group did not show continued improvements on dynamic balance because the effort needed to perform the SSEs was not to the same level of intensity it was for the first four weeks, which included PT supervision. However, it is also not certain whether the SSE group used proper exercise form during the unsupervised portion of the intervention. In addition, evidence has demonstrated that lower-extremity flexibility could affect YBT performance in healthy populations.46,47 Therefore, the GE group could have potentially increased lower-extremity flexibility after eight weeks of intervention and therefore could have been able to reach farther distances during the YBT. However, lower-extremity ROM was not assessed after implementing the intervention in this study, so it was not certain whether the improvement on the YBT performance is the result of increased lower-extremity flexibility.
The results of this study also indicate that all participants, regardless of intervention, made significant improvement in dynamic balance after eight weeks. A point of discussion here is that it is apparent that YBT performance may require both spinal stability and ROM/lower-extremity flexibility since both exercise programs seemed to help improve dynamic balance performance after eight weeks. It is also important to note that the small magnitude of change observed in dynamic balance in this study during the last four weeks may be due to the unsupervised nature of the exercises. In this study, home exercise compliance was significantly higher during the first four weeks after initiating the intervention as compared to the last four weeks for both groups. This indicates that all participants performed their home exercises more often in the first four weeks, which included supervised PT sessions, than they did in the last four weeks, which had no supervised PT sessions. Evidence has shown that PT supervised SSEs were shown to be more effective than the unsupervised PT SSEs in patients with LBP.41
All participants regardless of the intervention they received showed significant improvements in pain intensity and disability level over eight weeks. However, the decrease in pain intensity and disability level did not exceed the MCID or MDC, which is 2 points for the NPRS and 10 points for the OSW in patients with CLBP.36,48 This finding agrees with a pooled analysis that reported no significant benefits for pain or disability between SSEs versus other forms of active exercises. The authors indicated that improvements were minimal and not regarded as clinically significant.49 In addition, Salavati et al.45 reported that four weeks of SSEs combined with usual PT care as compared to usual PT care alone resulted in no significant improvement in pain and disability ratings in patients with CLBP. The trend toward better results in pain intensity and disability level suggests that significant changes may take longer than eight weeks to become detectable.
The current study is unique because it is the first to assess the effectiveness of SSEs on dynamic balance in adults with CLBP using the YBT. This study evaluated dynamic balance in a multi-planar manner while performing dynamic tasks that considerably challenged the stability of the spine. This study also demonstrates that the YBT is able to detect change in dynamic balance over time, suggesting that the YBT may be a useful tool for clinicians to assess dynamic balance deficits in patients with CLBP and monitor treatment progression. A better understanding of impairments associated with LBP would assist clinicians in developing personalized intervention programs and individualizing exercise prescription to address those identified at high risk for recurrent LBP.
Strengths and Limitations of the Study
Strengths of this study include the implementation of a double blinded, concealed allocation randomized clinical trial design in which the participants and the investigators were blinded. Specifically, one investigator was fully blinded to the participants’ group allocation and intervention while the other investigator was blinded to the participants’ pre- and post-intervention measurements. All participants were not informed whether they were assigned to the placebo or to the treatment group. Therefore, the design of the study provided control over potentially important sources of bias, so that the observed effects of the implemented interventions were less likely to be due to chance. However, there are limitations in this study. First, participants were recruited by means of advertisements; therefore, it is possible that individuals seeking medical care for their LBP are different from those responding to an advertisement, thus limiting the generalizability of the study results. In addition, only individuals with CLBP were enrolled in the study. Therefore, the findings are not applicable for individuals with acute or subacute LBP. Another possible limitation is that participants reported low pain intensity, mild disability level, and low physical activity level which limits the generalizability of findings to non-athlete individuals with mild pain and disability levels. Lastly, although efforts were made to control the potential influence of confounding factors that may affect YBT performance, factors such as knee and ankle strength and joint ROM were not investigated.
Recommendations for Future Research
Future studies are warranted with supervised SSEs and long-term follow-up to examine the effectiveness of these exercises on dynamic balance in individuals with LBP. In addition, future studies should consider measuring participants’ lower-extremity ROM across the study. Lastly, future research is needed to determine which directions of the YBT are the most sensitive to dynamic balance changes in LBP populations.
CONCLUSION
The results of this study show SSEs to be more effective than GEs in improving dynamic balance, but not pain intensity nor disability level in adults with CLBP. Specifically, four weeks of supervised SSEs along with a home exercise program is more effective in improving dynamic balance than GEs in participants with CLBP in four weeks. However, GEs appeared to have an effect equivalent to that of SSEs after four weeks of supervised intervention and another four weeks of unsupervised intervention. In addition, all participants had reduction in pain intensity and disability level over eight weeks after the intervention. However, no differences were found between groups, and the decrease in pain intensity and disability level did not exceed the MCID or MDC. The results of the study provide evidence for clinicians to include SSEs for improving dynamic balance in the management of patients with CLBP.
DISCLOSURE STATEMENT
No conflicts of interest were present in this study.
Supplementary Material
Acknowledgments
ACKNOWLEDGEMENTS
The authors would like to thank the Texas Physical Therapy Foundation for funding this study.
References
- What low back pain is and why we need to pay attention. Hartvigsen Jan, Hancock Mark J, Kongsted Alice, Louw Quinette, Ferreira Manuela L, Genevay Stéphane, Hoy Damian, Karppinen Jaro, Pransky Glenn, Sieper Joachim, Smeets Rob J, Underwood Martin, Buchbinder Rachelle, Hartvigsen Jan, Cherkin Dan, Foster Nadine E, Maher Chris G, Underwood Martin, van Tulder Maurits, Anema Johannes R, Chou Roger, Cohen Stephen P, Menezes Costa Lucíola, Croft Peter, Ferreira Manuela, Ferreira Paulo H, Fritz Julie M, Genevay Stéphane, Gross Douglas P, Hancock Mark J, Hoy Damian, Karppinen Jaro, Koes Bart W, Kongsted Alice, Louw Quinette, Öberg Birgitta, Peul Wilco C, Pransky Glenn, Schoene Mark, Sieper Joachim, Smeets Rob J, Turner Judith A, Woolf Anthony. Jun;2018 The Lancet. 391(10137):2356–2367. doi: 10.1016/s0140-6736(18)30480-x. doi: 10.1016/s0140-6736(18)30480-x. [DOI] [PubMed] [Google Scholar]
- Multidisciplinary biopsychosocial rehabilitation for subacute low back pain. Marin Teresa J, Van Eerd Dwayne, Irvin Emma, Couban Rachel, Koes Bart W, Malmivaara Antti, van Tulder Maurits W, Kamper Steven J. Jun 28;2017 Cochrane Database of Systematic Reviews. 2017(6) doi: 10.1002/14651858.cd002193.pub2. doi: 10.1002/14651858.cd002193.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the global burden of disease study 2016. Vos Theo, Abajobir Amanuel Alemu, Abate Kalkidan Hassen, Abbafati Cristiana, Abbas Kaja M, Abd-Allah Foad, Abdulkader Rizwan Suliankatchi, Abdulle Abdishakur M, Abebo Teshome Abuka, Abera Semaw Ferede, Aboyans Victor, Abu-Raddad Laith J, Ackerman Ilana N, Adamu Abdu Abdullahi, Adetokunboh Olatunji, Afarideh Mohsen, Afshin Ashkan, Agarwal Sanjay Kumar, Aggarwal Rakesh, Agrawal Anurag, Agrawal Sutapa, Ahmadieh Hamid, Ahmed Muktar Beshir, Aichour Miloud Taki Eddine, Aichour Amani Nidhal, Aichour Ibtihel, Aiyar Sneha, Akinyemi Rufus Olusola, Akseer Nadia, Al Lami Faris Hasan, Alahdab Fares, Al-Aly Ziyad, Alam Khurshid, Alam Noore, Alam Tahiya, Alasfoor Deena, Alene Kefyalew Addis, Ali Raghib, Alizadeh-Navaei Reza, Alkerwi Ala'a, Alla François, Allebeck Peter, Allen Christine, Al-Maskari Fatma, Al-Raddadi Rajaa, Alsharif Ubai, Alsowaidi Shirina, Altirkawi Khalid A, Amare Azmeraw T, Amini Erfan, Ammar Walid, Amoako Yaw Ampem, Andersen Hjalte H, Antonio Carl Abelardo T, Anwari Palwasha, Ärnlöv Johan, Artaman Al, Aryal Krishna Kumar, Asayesh Hamid, Asgedom Solomon W, Assadi Reza, Atey Tesfay Mehari, Atnafu Niguse Tadele, Atre Sachin R, Avila-Burgos Leticia, Avokphako Euripide Frinel G Arthur, Awasthi Ashish, Bacha Umar, Badawi Alaa, Balakrishnan Kalpana, Banerjee Amitava, Bannick Marlena S, Barac Aleksandra, Barber Ryan M, Barker-Collo Suzanne L, Bärnighausen Till, Barquera Simon, Barregard Lars, Barrero Lope H, Basu Sanjay, Battista Bob, Battle Katherine E, Baune Bernhard T, Bazargan-Hejazi Shahrzad, Beardsley Justin, Bedi Neeraj, Beghi Ettore, Béjot Yannick, Bekele Bayu Begashaw, Bell Michelle L, Bennett Derrick A, Bensenor Isabela M, Benson Jennifer, Berhane Adugnaw, Berhe Derbew Fikadu, Bernabé Eduardo, Betsu Balem Demtsu, Beuran Mircea, Beyene Addisu Shunu, Bhala Neeraj, Bhansali Anil, Bhatt Samir, Bhutta Zulfiqar A, Biadgilign Sibhatu, Bicer Burcu Kucuk, Bienhoff Kelly, Bikbov Boris, Birungi Charles, Biryukov Stan, Bisanzio Donal, Bizuayehu Habtamu Mellie, Boneya Dube Jara, Boufous Soufiane, Bourne Rupert R A, Brazinova Alexandra, Brugha Traolach S, Buchbinder Rachelle, Bulto Lemma Negesa Bulto, Bumgarner Blair R, Butt Zahid A, Cahuana-Hurtado Lucero, Cameron Ewan, Car Mate, Carabin Hélène, Carapetis Jonathan R, Cárdenas Rosario, Carpenter David O, Carrero Juan Jesus, Carter Austin, Carvalho Felix, Casey Daniel C, Caso Valeria, Castañeda-Orjuela Carlos A, Castle Chris D, Catalá-López Ferrán, Chang Hsing-Yi, Chang Jung-Chen, Charlson Fiona J, Chen Honglei, Chibalabala Mirriam, Chibueze Chioma Ezinne, Chisumpa Vesper Hichilombwe, Chitheer Abdulaal A, Christopher Devasahayam Jesudas, Ciobanu Liliana G, Cirillo Massimo, Colombara Danny, Cooper Cyrus, Cortesi Paolo Angelo, Criqui Michael H, Crump John A, Dadi Abel Fekadu, Dalal Koustuv, Dandona Lalit, Dandona Rakhi, das Neves José, Davitoiu Dragos V, de Courten Barbora, De Leo Diego De, Defo Barthelemy Kuate, Degenhardt Louisa, Deiparine Selina, Dellavalle Robert P, Deribe Kebede, Des Jarlais Don C, Dey Subhojit, Dharmaratne Samath D, Dhillon Preet Kaur, Dicker Daniel, Ding Eric L, Djalalinia Shirin, Do Huyen Phuc, Dorsey E Ray, dos Santos Kadine Priscila Bender, Douwes-Schultz Dirk, Doyle Kerrie E, Driscoll Tim R, Dubey Manisha, Duncan Bruce Bartholow, El-Khatib Ziad Ziad, Ellerstrand Jerisha, Enayati Ahmadali, Endries Aman Yesuf, Ermakov Sergey Petrovich, Erskine Holly E, Eshrati Babak, Eskandarieh Sharareh, Esteghamati Alireza, Estep Kara, Fanuel Fanuel Belayneh Bekele, Farinha Carla Sofia E Sa, Faro André, Farzadfar Farshad, Fazeli Mir Sohail, Feigin Valery L, Fereshtehnejad Seyed-Mohammad, Fernandes João C, Ferrari Alize J, Feyissa Tesfaye Regassa, Filip Irina, Fischer Florian, Fitzmaurice Christina, Flaxman Abraham D, Flor Luisa Sorio, Foigt Nataliya, Foreman Kyle J, Franklin Richard C, Fullman Nancy, Fürst Thomas, Furtado Joao M, Futran Neal D, Gakidou Emmanuela, Ganji Morsaleh, Garcia-Basteiro Alberto L, Gebre Teshome, Gebrehiwot Tsegaye Tewelde, Geleto Ayele, Gemechu Bikila Lencha, Gesesew Hailay Abrha, Gething Peter W, Ghajar Alireza, Gibney Katherine B, Gill Paramjit Singh, Gillum Richard F, Ginawi Ibrahim Abdelmageem Mohamed, Giref Ababi Zergaw, Gishu Melkamu Dedefo, Giussani Giorgia, Godwin William W, Gold Audra L, Goldberg Ellen M, Gona Philimon N, Goodridge Amador, Gopalani Sameer Vali, Goto Atsushi, Goulart Alessandra Carvalho, Griswold Max, Gugnani Harish Chander, Gupta Rahul, Gupta Rajeev, Gupta Tanush, Gupta Vipin, Hafezi-Nejad Nima, Hailu Gessessew Bugssa, Hailu Alemayehu Desalegne, Hamadeh Randah Ribhi, Hamidi Samer, Handal Alexis J, Hankey Graeme J, Hanson Sarah Wulf, Hao Yuantao, Harb Hilda L, Hareri Habtamu Abera, Haro Josep Maria, Harvey James, Hassanvand Mohammad Sadegh, Havmoeller Rasmus, Hawley Caitlin, Hay Simon I, Hay Roderick J, Henry Nathaniel J, Heredia-Pi Ileana Beatriz, Hernandez Julio Montañez, Heydarpour Pouria, Hoek Hans W, Hoffman Howard J, Horita Nobuyuki, Hosgood H Dean, Hostiuc Sorin, Hotez Peter J, Hoy Damian G, Htet Aung Soe, Hu Guoqing, Huang Hsiang, Huynh Chantal, Iburg Kim Moesgaard, Igumbor Ehimario Uche, Ikeda Chad, Irvine Caleb Mackay Salpeter, Jacobsen Kathryn H, Jahanmehr Nader, Jakovljevic Mihajlo B, Jassal Simerjot K, Javanbakht Mehdi, Jayaraman Sudha P, Jeemon Panniyammakal, Jensen Paul N, Jha Vivekanand, Jiang Guohong, John Denny, Johnson Sarah Charlotte, Johnson Catherine O, Jonas Jost B, Jürisson Mikk, Kabir Zubair, Kadel Rajendra, Kahsay Amaha, Kamal Ritul, Kan Haidong, Karam Nadim E, Karch André, Karema Corine Kakizi, Kasaeian Amir, Kassa Getachew Mullu, Kassaw Nigussie Assefa, Kassebaum Nicholas J, Kastor Anshul, Katikireddi Srinivasa Vittal, Kaul Anil, Kawakami Norito, Keiyoro Peter Njenga, Kengne Andre Pascal, Keren Andre, Khader Yousef Saleh, Khalil Ibrahim A, Khan Ejaz Ahmad, Khang Young-Ho, Khosravi Ardeshir, Khubchandani Jagdish, Kiadaliri Aliasghar Ahmad, Kieling Christian, Kim Yun Jin, Kim Daniel, Kim Pauline, Kimokoti Ruth W, Kinfu Yohannes, Kisa Adnan, Kissimova-Skarbek Katarzyna A, Kivimaki Mika, Knudsen Ann Kristin, Kokubo Yoshihiro, Kolte Dhaval, Kopec Jacek A, Kosen Soewarta, Koul Parvaiz A, Koyanagi Ai, Kravchenko Michael, Krishnaswami Sanjay, Krohn Kristopher J, Kumar G Anil, Kumar Pushpendra, Kumar Sanjiv, Kyu Hmwe H, Lal Dharmesh Kumar, Lalloo Ratilal, Lambert Nkurunziza, Lan Qing, Larsson Anders, Lavados Pablo M, Leasher Janet L, Lee Paul H, Lee Jong-Tae, Leigh James, Leshargie Cheru Tesema, Leung Janni, Leung Ricky, Levi Miriam, Li Yichong, Li Yongmei, Li Kappe Darya, Liang Xiaofeng, Liben Misgan Legesse, Lim Stephen S, Linn Shai, Liu Patrick Y, Liu Angela, Liu Shiwei, Liu Yang, Lodha Rakesh, Logroscino Giancarlo, London Stephanie J, Looker Katharine J, Lopez Alan D, Lorkowski Stefan, Lotufo Paulo A, Low Nicola, Lozano Rafael, Lucas Timothy C D, Macarayan Erlyn Rachelle King, Magdy Abd El Razek Hassan, Magdy Abd El Razek Mohammed, Mahdavi Mahdi, Majdan Marek, Majdzadeh Reza, Majeed Azeem, Malekzadeh Reza, Malhotra Rajesh, Malta Deborah Carvalho, Mamun Abdullah A, Manguerra Helena, Manhertz Treh, Mantilla Ana, Mantovani Lorenzo G, Mapoma Chabila C, Marczak Laurie B, Martinez-Raga Jose, Martins-Melo Francisco Rogerlândio, Martopullo Ira, März Winfried, Mathur Manu Raj, Mazidi Mohsen, McAlinden Colm, McGaughey Madeline, McGrath John J, McKee Martin, McNellan Claire, Mehata Suresh, Mehndiratta Man Mohan, Mekonnen Tefera Chane, Memiah Peter, Memish Ziad A, Mendoza Walter, Mengistie Mubarek Abera, Mengistu Desalegn Tadese, Mensah George A, Meretoja Tuomo J, Meretoja Atte, Mezgebe Haftay Berhane, Micha Renata, Millear Anoushka, Miller Ted R, Mills Edward J, Mirarefin Mojde, Mirrakhimov Erkin M, Misganaw Awoke, Mishra Shiva Raj, Mitchell Philip B, Mohammad Karzan Abdulmuhsin, Mohammadi Alireza, Mohammed Kedir Endris, Mohammed Shafiu, Mohanty Sanjay K, Mokdad Ali H, Mollenkopf Sarah K, Monasta Lorenzo, Montico Marcella, Moradi-Lakeh Maziar, Moraga Paula, Mori Rintaro, Morozoff Chloe, Morrison Shane D, Moses Mark, Mountjoy-Venning Cliff, Mruts Kalayu Birhane, Mueller Ulrich O, Muller Kate, Murdoch Michele E, Murthy Gudlavalleti Venkata Satyanarayana, Musa Kamarul Imran, Nachega Jean B, Nagel Gabriele, Naghavi Mohsen, Naheed Aliya, Naidoo Kovin S, Naldi Luigi, Nangia Vinay, Natarajan Gopalakrishnan, Negasa Dumessa Edessa, Negoi Ruxandra Irina, Negoi Ionut, Newton Charles R, Ngunjiri Josephine Wanjiku, Nguyen Trang Huyen, Nguyen Quyen Le, Nguyen Cuong Tat, Nguyen Grant, Nguyen Minh, Nichols Emma, Ningrum Dina Nur Anggraini, Nolte Sandra, Nong Vuong Minh, Norrving Bo, Noubiap Jean Jacques N, O'Donnell Martin J, Ogbo Felix Akpojene, Oh In-Hwan, Okoro Anselm, Oladimeji Olanrewaju, Olagunju Tinuke Oluwasefunmi, Olagunju Andrew Toyin, Olsen Helen E, Olusanya Bolajoko Olubukunola, Olusanya Jacob Olusegun, Ong Kanyin, Opio John Nelson, Oren Eyal, Ortiz Alberto, Osgood-Zimmerman Aaron, Osman Majdi, Owolabi Mayowa O, PA Mahesh, Pacella Rosana E, Pana Adrian, Panda Basant Kumar, Papachristou Christina, Park Eun-Kee, Parry Charles D, Parsaeian Mahboubeh, Patten Scott B, Patton George C, Paulson Katherine, Pearce Neil, Pereira David M, Perico Norberto, Pesudovs Konrad, Peterson Carrie Beth, Petzold Max, Phillips Michael Robert, Pigott David M, Pillay Julian David, Pinho Christine, Plass Dietrich, Pletcher Martin A, Popova Svetlana, Poulton Richie G, Pourmalek Farshad, Prabhakaran Dorairaj, Prasad Noela M, Prasad Narayan, Purcell Carrie, Qorbani Mostafa, Quansah Reginald, Quintanilla Beatriz Paulina Ayala, Rabiee Rynaz H S, Radfar Amir, Rafay Anwar, Rahimi Kazem, Rahimi-Movaghar Afarin, Rahimi-Movaghar Vafa, Rahman Mohammad Hifz Ur, Rahman Mahfuzar, Rai Rajesh Kumar, Rajsic Sasa, Ram Usha, Ranabhat Chhabi Lal, Rankin Zane, Rao Puja C, Rao Paturi Vishnupriya, Rawaf Salman, Ray Sarah E, Reiner Robert C, Reinig Nikolas, Reitsma Marissa B, Remuzzi Giuseppe, Renzaho Andre M N, Resnikoff Serge, Rezaei Satar, Ribeiro Antonio L, Ronfani Luca, Roshandel Gholamreza, Roth Gregory A, Roy Ambuj, Rubagotti Enrico, Ruhago George Mugambage, Saadat Soheil, Sadat Nafis, Safdarian Mahdi, Safi Sare, Safiri Saeid, Sagar Rajesh, Sahathevan Ramesh, Salama Joseph, Saleem Huda Omer Ba, Salomon Joshua A, Salvi Sundeep Santosh, Samy Abdallah M, Sanabria Juan R, Santomauro Damian, Santos Itamar S, Santos João Vasco, Santric Milicevic Milena M, Sartorius Benn, Satpathy Maheswar, Sawhney Monika, Saxena Sonia, Schmidt Maria Inês, Schneider Ione J C, Schöttker Ben, Schwebel David C, Schwendicke Falk, Seedat Soraya, Sepanlou Sadaf G, Servan-Mori Edson E, Setegn Tesfaye, Shackelford Katya Anne, Shaheen Amira, Shaikh Masood Ali, Shamsipour Mansour, Shariful Islam Sheikh Mohammed, Sharma Jayendra, Sharma Rajesh, She Jun, Shi Peilin, Shields Chloe, Shifa Girma Temam, Shigematsu Mika, Shinohara Yukito, Shiri Rahman, Shirkoohi Reza, Shirude Shreya, Shishani Kawkab, Shrime Mark G, Sibai Abla Mehio, Sigfusdottir Inga Dora, Silva Diego Augusto Santos, Silva João Pedro, Silveira Dayane Gabriele Alves, Singh Jasvinder A, Singh Narinder Pal, Sinha Dhirendra Narain, Skiadaresi Eirini, Skirbekk Vegard, Slepak Erica Leigh, Sligar Amber, Smith David L, Smith Mari, Sobaih Badr H A, Sobngwi Eugene, Sorensen Reed J D, Sousa Tatiane Cristina Moraes, Sposato Luciano A, Sreeramareddy Chandrashekhar T, Srinivasan Vinay, Stanaway Jeffrey D, Stathopoulou Vasiliki, Steel Nicholas, Stein Murray B, Stein Dan J, Steiner Timothy J, Steiner Caitlyn, Steinke Sabine, Stokes Mark Andrew, Stovner Lars Jacob, Strub Bryan, Subart Michelle, Sufiyan Muawiyyah Babale, Sunguya Bruno F, Sur Patrick J, Swaminathan Soumya, Sykes Bryan L, Sylte Dillon O, Tabarés-Seisdedos Rafael, Taffere Getachew Redae, Takala Jukka S, Tandon Nikhil, Tavakkoli Mohammad, Taveira Nuno, Taylor Hugh R, Tehrani-Banihashemi Arash, Tekelab Tesfalidet, Terkawi Abdullah Sulieman, Tesfaye Dawit Jember, Tesssema Belay, Thamsuwan Ornwipa, Thomas Katie E, Thrift Amanda G, Tiruye Tenaw Yimer, Tobe-Gai Ruoyan, Tollanes Mette C, Tonelli Marcello, Topor-Madry Roman, Tortajada Miguel, Touvier Mathilde, Tran Bach Xuan, Tripathi Suryakant, Troeger Christopher, Truelsen Thomas, Tsoi Derrick, Tuem Kald Beshir, Tuzcu Emin Murat, Tyrovolas Stefanos, Ukwaja Kingsley N, Undurraga Eduardo A, Uneke Chigozie Jesse, Updike Rachel, Uthman Olalekan A, Uzochukwu Benjamin S Chudi, van Boven Job F M, Varughese Santosh, Vasankari Tommi, Venkatesh S, Venketasubramanian Narayanaswamy, Vidavalur Ramesh, Violante Francesco S, Vladimirov Sergey K, Vlassov Vasiliy Victorovich, Vollset Stein Emil, Wadilo Fiseha, Wakayo Tolassa, Wang Yuan-Pang, Weaver Marcia, Weichenthal Scott, Weiderpass Elisabete, Weintraub Robert G, Werdecker Andrea, Westerman Ronny, Whiteford Harvey A, Wijeratne Tissa, Wiysonge Charles Shey, Wolfe Charles D A, Woodbrook Rachel, Woolf Anthony D, Workicho Abdulhalik, Xavier Denis, Xu Gelin, Yadgir Simon, Yaghoubi Mohsen, Yakob Bereket, Yan Lijing L, Yano Yuichiro, Ye Pengpeng, Yimam Hassen Hamid, Yip Paul, Yonemoto Naohiro, Yoon Seok-Jun, Yotebieng Marcel, Younis Mustafa Z, Zaidi Zoubida, Zaki Maysaa El Sayed, Zegeye Elias Asfaw, Zenebe Zerihun Menlkalew, Zhang Xueying, Zhou Maigeng, Zipkin Ben, Zodpey Sanjay, Zuhlke Liesl Joanna, Murray Christopher J L. Sep;2017 The Lancet. 390(10100):1211–1259. doi: 10.1016/s0140-6736(17)32154-2. doi: 10.1016/s0140-6736(17)32154-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the global burden of disease study 2015. Wang Haidong, Naghavi Mohsen, Allen Christine, Barber Ryan M, Bhutta Zulfiqar A, Carter Austin, Casey Daniel C, Charlson Fiona J, Chen Alan Zian, Coates Matthew M, Coggeshall Megan, Dandona Lalit, Dicker Daniel J, Erskine Holly E, Ferrari Alize J, Fitzmaurice Christina, Foreman Kyle, Forouzanfar Mohammad H, Fraser Maya S, Fullman Nancy, Gething Peter W, Goldberg Ellen M, Graetz Nicholas, Haagsma Juanita A, Hay Simon I, Huynh Chantal, Johnson Catherine O, Kassebaum Nicholas J, Kinfu Yohannes, Kulikoff Xie Rachel, Kutz Michael, Kyu Hmwe H, Larson Heidi J, Leung Janni, Liang Xiaofeng, Lim Stephen S, Lind Margaret, Lozano Rafael, Marquez Neal, Mensah George A, Mikesell Joe, Mokdad Ali H, Mooney Meghan D, Nguyen Grant, Nsoesie Elaine, Pigott David M, Pinho Christine, Roth Gregory A, Salomon Joshua A, Sandar Logan, Silpakit Naris, Sligar Amber, Sorensen Reed J D, Stanaway Jeffrey, Steiner Caitlyn, Teeple Stephanie, Thomas Bernadette A, Troeger Christopher, VanderZanden Amelia, Vollset Stein Emil, Wanga Valentine, Whiteford Harvey A, Wolock Timothy, Zoeckler Leo, Abate Kalkidan Hassen, Abbafati Cristiana, Abbas Kaja M, Abd-Allah Foad, Abera Semaw Ferede, Abreu Daisy M X, Abu-Raddad Laith J, Abyu Gebre Yitayih, Achoki Tom, Adelekan Ademola Lukman, Ademi Zanfina, Adou Arsène Kouablan, Adsuar José C, Afanvi Kossivi Agbelenko, Afshin Ashkan, Agardh Emilie Elisabet, Agarwal Arnav, Agrawal Anurag, Kiadaliri Aliasghar Ahmad, Ajala Oluremi N, Akanda Ali Shafqat, Akinyemi Rufus Olusola, Akinyemiju Tomi F, Akseer Nadia, Lami Faris Hasan Al, Alabed Samer, Al-Aly Ziyad, Alam Khurshid, Alam Noore K M, Alasfoor Deena, Aldhahri Saleh Fahed, Aldridge Robert William, Alegretti Miguel Angel, Aleman Alicia V, Alemu Zewdie Aderaw, Alexander Lily T, Alhabib Samia, Ali Raghib, Alkerwi Ala'a, Alla François, Allebeck Peter, Al-Raddadi Rajaa, Alsharif Ubai, Altirkawi Khalid A, Martin Elena Alvarez, Alvis-Guzman Nelson, Amare Azmeraw T, Amegah Adeladza Kofi, Ameh Emmanuel A, Amini Heresh, Ammar Walid, Amrock Stephen Marc, Andersen Hjalte H, Anderson Benjamin O, Anderson Gregory M, Antonio Carl Abelardo T, Aregay Atsede Fantahun, Ärnlöv Johan, Arsenijevic Valentina S Arsic, Artaman Al, Asayesh Hamid, Asghar Rana Jawad, Atique Suleman, Avokpaho Euripide Frinel G Arthur, Awasthi Ashish, Azzopardi Peter, Bacha Umar, Badawi Alaa, Bahit Maria C, Balakrishnan Kalpana, Banerjee Amitava, Barac Aleksandra, Barker-Collo Suzanne L, Bärnighausen Till, Barregard Lars, Barrero Lope H, Basu Arindam, Basu Sanjay, Bayou Yibeltal Tebekaw, Bazargan-Hejazi Shahrzad, Beardsley Justin, Bedi Neeraj, Beghi Ettore, Belay Haileeyesus Adamu, Bell Brent, Bell Michelle L, Bello Aminu K, Bennett Derrick A, Bensenor Isabela M, Berhane Adugnaw, Bernabé Eduardo, Betsu Balem Demtsu, Beyene Addisu Shunu, Bhala Neeraj, Bhalla Ashish, Biadgilign Sibhatu, Bikbov Boris, Abdulhak Aref A Bin, Biroscak Brian J, Biryukov Stan, Bjertness Espen, Blore Jed D, Blosser Christopher D, Bohensky Megan A, Borschmann Rohan, Bose Dipan, Bourne Rupert R A, Brainin Michael, Brayne Carol E G, Brazinova Alexandra, Breitborde Nicholas J K, Brenner Hermann, Brewer Jerry D, Brown Alexandria, Brown Jonathan, Brugha Traolach S, Buckle Geoffrey Colin, Butt Zahid A, Calabria Bianca, Campos-Nonato Ismael Ricardo, Campuzano Julio Cesar, Carapetis Jonathan R, Cárdenas Rosario, Carpenter David O, Carrero Juan Jesus, Castañeda-Orjuela Carlos A, Rivas Jacqueline Castillo, Catalá-López Ferrán, Cavalleri Fiorella, Cercy Kelly, Cerda Jorge, Chen Wanqing, Chew Adrienne, Chiang Peggy Pei-Chia, Chibalabala Mirriam, Chibueze Chioma Ezinne, Chimed-Ochir Odgerel, Chisumpa Vesper Hichilombwe, Choi Jee-Young Jasmine, Chowdhury Rajiv, Christensen Hanne, Christopher Devasahayam Jesudas, Ciobanu Liliana G, Cirillo Massimo, Cohen Aaron J, Colistro Valentina, Colomar Mercedes, Colquhoun Samantha M, Cooper Cyrus, Cooper Leslie Trumbull, Cortinovis Monica, Cowie Benjamin C, Crump John A, Damsere-Derry James, Danawi Hadi, Dandona Rakhi, Daoud Farah, Darby Sarah C, Dargan Paul I, das Neves José, Davey Gail, Davis Adrian C, Davitoiu Dragos V, de Castro E Filipa, de Jager Pieter, Leo Diego De, Degenhardt Louisa, Dellavalle Robert P, Deribe Kebede, Deribew Amare, Dharmaratne Samath D, Dhillon Preet K, Diaz-Torné Cesar, Ding Eric L, dos Santos Kadine Priscila Bender, Dossou Edem, Driscoll Tim R, Duan Leilei, Dubey Manisha, Duncan Bruce Bartholow, Ellenbogen Richard G, Ellingsen Christian Lycke, Elyazar Iqbal, Endries Aman Yesuf, Ermakov Sergey Petrovich, Eshrati Babak, Esteghamati Alireza, Estep Kara, Faghmous Imad D A, Fahimi Saman, Faraon Emerito Jose Aquino, Farid Talha A, Farinha Carla Sofia e Sa, Faro André, Farvid Maryam S, Farzadfar Farshad, Feigin Valery L, Fereshtehnejad Seyed-Mohammad, Fernandes Jefferson G, Fernandes Joao C, Fischer Florian, Fitchett Joseph R A, Flaxman Abraham, Foigt Nataliya, Fowkes F Gerry R, Franca Elisabeth Barboza, Franklin Richard C, Friedman Joseph, Frostad Joseph, Fürst Thomas, Futran Neal D, Gall Seana L, Gambashidze Ketevan, Gamkrelidze Amiran, Ganguly Parthasarathi, Gankpé Fortuné Gbètoho, Gebre Teshome, Gebrehiwot Tsegaye Tsewelde, Gebremedhin Amanuel Tesfay, Gebru Alemseged Aregay, Geleijnse Johanna M, Gessner Bradford D, Ghoshal Aloke Gopal, Gibney Katherine B, Gillum Richard F, Gilmour Stuart, Giref Ababi Zergaw, Giroud Maurice, Gishu Melkamu Dedefo, Giussani Giorgia, Glaser Elizabeth, Godwin William W, Gomez-Dantes Hector, Gona Philimon, Goodridge Amador, Gopalani Sameer Vali, Gosselin Richard A, Gotay Carolyn C, Goto Atsushi, Gouda Hebe N, Greaves Felix, Gugnani Harish Chander, Gupta Rahul, Gupta Rajeev, Gupta Vipin, Gutiérrez Reyna A, Hafezi-Nejad Nima, Haile Demewoz, Hailu Alemayehu Desalegne, Hailu Gessessew Bugssa, Halasa Yara A, Hamadeh Randah Ribhi, Hamidi Samer, Hancock Jamie, Handal Alexis J, Hankey Graeme J, Hao Yuantao, Harb Hilda L, Harikrishnan Sivadasanpillai, Haro Josep Maria, Havmoeller Rasmus, Heckbert Susan R, Heredia-Pi Ileana Beatriz, Heydarpour Pouria, Hilderink Henk B M, Hoek Hans W, Hogg Robert S, Horino Masako, Horita Nobuyuki, Hosgood H Dean, Hotez Peter J, Hoy Damian G, Hsairi Mohamed, Htet Aung Soe, Htike Maung Maung Than, Hu Guoqing, Huang Cheng, Huang Hsiang, Huiart Laetitia, Husseini Abdullatif, Huybrechts Inge, Huynh Grace, Iburg Kim Moesgaard, Innos Kaire, Inoue Manami, Iyer Veena J, Jacobs Troy A, Jacobsen Kathryn H, Jahanmehr Nader, Jakovljevic Mihajlo B, James Peter, Javanbakht Mehdi, Jayaraman Sudha P, Jayatilleke Achala Upendra, Jeemon Panniyammakal, Jensen Paul N, Jha Vivekanand, Jiang Guohong, Jiang Ying, Jibat Tariku, Jimenez-Corona Aida, Jonas Jost B, Joshi Tushar Kant, Kabir Zubair, Kamal Ritul, Kan Haidong, Kant Surya, Karch André, Karema Corine Kakizi, Karimkhani Chante, Karletsos Dimitris, Karthikeyan Ganesan, Kasaeian Amir, Katibeh Marzieh, Kaul Anil, Kawakami Norito, Kayibanda Jeanne Françoise, Keiyoro Peter Njenga, Kemmer Laura, Kemp Andrew Haddon, Kengne Andre Pascal, Keren Andre, Kereselidze Maia, Kesavachandran Chandrasekharan Nair, Khader Yousef Saleh, Khalil Ibrahim A, Khan Abdur Rahman, Khan Ejaz Ahmad, Khang Young-Ho, Khera Sahil, Khoja Tawfik Ahmed Muthafer, Kieling Christian, Kim Daniel, Kim Yun Jin, Kissela Brett M, Kissoon Niranjan, Knibbs Luke D, Knudsen Ann Kristin, Kokubo Yoshihiro, Kolte Dhaval, Kopec Jacek A, Kosen Soewarta, Koul Parvaiz A, Koyanagi Ai, Krog Norun Hjertager, Defo Barthelemy Kuate, Bicer Burcu Kucuk, Kudom Andreas A, Kuipers Ernst J, Kulkarni Veena S, Kumar G Anil, Kwan Gene F, Lal Aparna, Lal Dharmesh Kumar, Lalloo Ratilal, Lallukka Tea, Lam Hilton, Lam Jennifer O, Langan Sinead M, Lansingh Van C, Larsson Anders, Laryea Dennis Odai, Latif Asma Abdul, Lawrynowicz Alicia Elena Beatriz, Leigh James, Levi Miriam, Li Yongmei, Lindsay M Patrice, Lipshultz Steven E, Liu Patrick Y, Liu Shiwei, Liu Yang, Lo Loon-Tzian, Logroscino Giancarlo, Lotufo Paulo A, Lucas Robyn M, Lunevicius Raimundas, Lyons Ronan A, Ma Stefan, Machado Vasco Manuel Pedro, Mackay Mark T, MacLachlan Jennifer H, Razek Hassan Magdy Abd El, Magdy Mohammed, Razek Abd El, Majdan Marek, Majeed Azeem, Malekzadeh Reza, Manamo Wondimu Ayele Ayele, Mandisarisa John, Mangalam Srikanth, Mapoma Chabila C, Marcenes Wagner, Margolis David Joel, Martin Gerard Robert, Martinez-Raga Jose, Marzan Melvin Barrientos, Masiye Felix, Mason-Jones Amanda J, Massano João, Matzopoulos Richard, Mayosi Bongani M, McGarvey Stephen Theodore, McGrath John J, McKee Martin, McMahon Brian J, Meaney Peter A, Mehari Alem, Mehndiratta Man Mohan, Mejia-Rodriguez Fabiola, Mekonnen Alemayehu B, Melaku Yohannes Adama, Memiah Peter, Memish Ziad A, Mendoza Walter, Meretoja Atte, Meretoja Tuomo J, Mhimbira Francis Apolinary, Micha Renata, Millear Anoushka, Miller Ted R, Mirarefin Mojde, Misganaw Awoke, Mock Charles N, Mohammad Karzan Abdulmuhsin, Mohammadi Alireza, Mohammed Shafiu, Mohan Viswanathan, Mola Glen Liddell D, Monasta Lorenzo, Hernandez Julio Cesar Montañez, Montero Pablo, Montico Marcella, Montine Thomas J, Moradi-Lakeh Maziar, Morawska Lidia, Morgan Katherine, Mori Rintaro, Mozaffarian Dariush, Mueller Ulrich O, Murthy Gudlavalleti Venkata Satyanarayana, Murthy Srinivas, Musa Kamarul Imran, Nachega Jean B, Nagel Gabriele, Naidoo Kovin S, Naik Nitish, Naldi Luigi, Nangia Vinay, Nash Denis, Nejjari Chakib, Neupane Subas, Newton Charles R, Newton John N, Ng Marie, Ngalesoni Frida Namnyak, de Dieu Ngirabega Jean, Nguyen Quyen Le, Nisar Muhammad Imran, Pete Patrick Martial Nkamedjie, Nomura Marika, Norheim Ole F, Norman Paul E, Norrving Bo, Nyakarahuka Luke, Ogbo Felix Akpojene, Ohkubo Takayoshi, Ojelabi Foluke Adetola, Olivares Pedro R, Olusanya Bolajoko Olubukunola, Olusanya Jacob Olusegun, Opio John Nelson, Oren Eyal, Ortiz Alberto, Osman Majdi, Ota Erika, Ozdemir Raziye, PA Mahesh, Pain Amanda, Pandian Jeyaraj D, Pant Puspa Raj, Papachristou Christina, Park Eun-Kee, Park Jae-Hyun, Parry Charles D, Parsaeian Mahboubeh, Caicedo Angel J Paternina, Patten Scott B, Patton George C, Paul Vinod K, Pearce Neil, Pedro João Mário, Stokic Ljiljana Pejin, Pereira David M, Perico Norberto, Pesudovs Konrad, Petzold Max, Phillips Michael Robert, Piel Frédéric B, Pillay Julian David, Plass Dietrich, Platts-Mills James A, Polinder Suzanne, Pope C Arden, Popova Svetlana, Poulton Richie G, Pourmalek Farshad, Prabhakaran Dorairaj, Qorbani Mostafa, Quame-Amaglo Justice, Quistberg D Alex, Rafay Anwar, Rahimi Kazem, Rahimi-Movaghar Vafa, Rahman Mahfuzar, Rahman Mohammad Hifz Ur, Rahman Sajjad Ur, Rai Rajesh Kumar, Rajavi Zhale, Rajsic Sasa, Raju Murugesan, Rakovac Ivo, Rana Saleem M, Ranabhat Chhabi L, Rangaswamy Thara, Rao Puja, Rao Sowmya R, Refaat Amany H, Rehm Jürgen, Reitsma Marissa B, Remuzzi Giuseppe, Resnikoff Serge, Ribeiro Antonio L, Ricci Stefano, Blancas Maria Jesus Rios, Roberts Bayard, Roca Anna, Rojas-Rueda David, Ronfani Luca, Roshandel Gholamreza, Rothenbacher Dietrich, Roy Ambuj, Roy Nawal K, Ruhago George Mugambage, Sagar Rajesh, Saha Sukanta, Sahathevan Ramesh, Saleh Muhammad Muhammad, Sanabria Juan R, Sanchez-Niño Maria Dolores, Sanchez-Riera Lidia, Santos Itamar S, Sarmiento-Suarez Rodrigo, Sartorius Benn, Satpathy Maheswar, Savic Miloje, Sawhney Monika, Schaub Michael P, Schmidt Maria Inês, Schneider Ione J C, Schöttker Ben, Schutte Aletta E, Schwebel David C, Seedat Soraya, Sepanlou Sadaf G, Servan-Mori Edson E, Shackelford Katya A, Shaddick Gavin, Shaheen Amira, Shahraz Saeid, Shaikh Masood Ali, Shakh-Nazarova Marina, Sharma Rajesh, She Jun, Sheikhbahaei Sara, Shen Jiabin, Shen Ziyan, Shepard Donald S, Sheth Kevin N, Shetty Balakrishna P, Shi Peilin, Shibuya Kenji, Shin Min-Jeong, Shiri Rahman, Shiue Ivy, Shrime Mark G, Sigfusdottir Inga Dora, Silberberg Donald H, Silva Diego Augusto Santos, Silveira Dayane Gabriele Alves, Silverberg Jonathan I, Simard Edgar P, Singh Abhishek, Singh Gitanjali M, Singh Jasvinder A, Singh Om Prakash, Singh Prashant Kumar, Singh Virendra, Soneji Samir, Søreide Kjetil, Soriano Joan B, Sposato Luciano A, Sreeramareddy Chandrashekhar T, Stathopoulou Vasiliki, Stein Dan J, Stein Murray B, Stranges Saverio, Stroumpoulis Konstantinos, Sunguya Bruno F, Sur Patrick, Swaminathan Soumya, Sykes Bryan L, Szoeke Cassandra E I, Tabarés-Seisdedos Rafael, Tabb Karen M, Takahashi Ken, Takala Jukka S, Talongwa Roberto Tchio, Tandon Nikhil, Tavakkoli Mohammad, Taye Bineyam, Taylor Hugh R, Ao Braden J Te, Tedla Bemnet Amare, Tefera Worku Mekonnen, Have Margreet Ten, Terkawi Abdullah Sulieman, Tesfay Fisaha Haile, Tessema Gizachew Assefa, Thomson Alan J, Thorne-Lyman Andrew L, Thrift Amanda G, Thurston George D, Tillmann Taavi, Tirschwell David L, Tonelli Marcello, Topor-Madry Roman, Topouzis Fotis, Towbin Jeffrey Allen, Traebert Jefferson, Tran Bach Xuan, Truelsen Thomas, Trujillo Ulises, Tura Abera Kenay, Tuzcu Emin Murat, Uchendu Uche S, Ukwaja Kingsley N, Undurraga Eduardo A, Uthman Olalekan A, Dingenen Rita Van, van Donkelaar Aaron, Vasankari Tommi, Vasconcelos Ana Maria Nogales, Venketasubramanian Narayanaswamy, Vidavalur Ramesh, Vijayakumar Lakshmi, Villalpando Salvador, Violante Francesco S, Vlassov Vasiliy Victorovich, Wagner Joseph A, Wagner Gregory R, Wallin Mitchell T, Wang Linhong, Watkins David A, Weichenthal Scott, Weiderpass Elisabete, Weintraub Robert G, Werdecker Andrea, Westerman Ronny, White Richard A, Wijeratne Tissa, Wilkinson James D, Williams Hywel C, Wiysonge Charles Shey, Woldeyohannes Solomon Meseret, Wolfe Charles D A, Won Sungho, Wong John Q, Woolf Anthony D, Xavier Denis, Xiao Qingyang, Xu Gelin, Yakob Bereket, Yalew Ayalnesh Zemene, Yan Lijing L, Yano Yuichiro, Yaseri Mehdi, Ye Pengpeng, Yebyo Henock Gebremedhin, Yip Paul, Yirsaw Biruck Desalegn, Yonemoto Naohiro, Yonga Gerald, Younis Mustafa Z, Yu Shicheng, Zaidi Zoubida, Zaki Maysaa El Sayed, Zannad Faiez, Zavala Diego E, Zeeb Hajo, Zeleke Berihun M, Zhang Hao, Zodpey Sanjay, Zonies David, Zuhlke Liesl Joanna, Vos Theo, Lopez Alan D, Murray Christopher J L. Oct;2016 The Lancet. 388(10053):1459–1544. doi: 10.1016/s0140-6736(16)31012-1. doi: 10.1016/s0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comparing lumbo-pelvic kinematics in people with and without back pain: A systematic review and meta-analysis. Laird R.A., Gilbert J., Kent P., Keating J.L. 2014BMC Musculoskelet. Disord. 15(1):1–13. doi: 10.1186/1471-2474-15-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noninvasive treatments for acute, subacute, and chronic low back pain: A clinical practice guideline from the American College of Physicians. Qaseem Amir, Wilt Timothy J., McLean Robert M., Forciea Mary Ann, Clinical Guidelines Committee of the American College of Physicians Feb 14;2017 Annals of Internal Medicine. 166(7):514–530. doi: 10.7326/m16-2367. doi: 10.7326/m16-2367. [DOI] [PubMed] [Google Scholar]
- Efficacy of the star excursion balance test in detecting reach deficits in subjects with chronic low back pain. Ganesh G. Shankar, Chhabra Deepak, Mrityunjay K. 2015Physiotherapy Research International. 20(1):9–15. doi: 10.1002/pri.1589. doi: 10.1002/pri.1589. [DOI] [PubMed] [Google Scholar]
- Dynamic balance as measured by the Y-balance test is reduced in individuals with low back pain: a cross-sectional comparative study. Hooper Troy L., James C. Roger, Brismée Jean-Michel, Rogers Toby J., Gilbert Kerry K., Browne Kevin L., Sizer Phillip S. Nov;2016 Physical Therapy in Sport. 22:29–34. doi: 10.1016/j.ptsp.2016.04.006. doi: 10.1016/j.ptsp.2016.04.006. [DOI] [PubMed] [Google Scholar]
- Balance recovery reactions in individuals with recurrent nonspecific low back pain: Effect of attention. Etemadi Yasaman, Salavati Mahyar, Arab Amir M., Ghanavati Tabassom. Feb;2016 Gait & Posture. 44:123–127. doi: 10.1016/j.gaitpost.2015.11.017. doi: 10.1016/j.gaitpost.2015.11.017. [DOI] [PubMed] [Google Scholar]
- Static and dynamic balance deficiencies in chronic low back pain. Tsigkanos Christos, Gaskell Lynne, Smirniotou Athanasia, Tsigkanos Georgios. Nov 21;2016 Journal of Back and Musculoskeletal Rehabilitation. 29(4):887–893. doi: 10.3233/bmr-160721. doi: 10.3233/bmr-160721. [DOI] [PubMed] [Google Scholar]
- A hypothesis of chronic back pain: Ligament subfailure injuries lead to muscle control dysfunction. Panjabi Manohar M. 2006European Spine Journal. 15(5):668–676. doi: 10.1007/s00586-005-0925-3. doi: 10.1007/s00586-005-0925-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hip strategy for balance control in quiet standing is reduced in people with low back pain. Mok Nicola W., Brauer Sandra G., Hodges Paul W. Mar;2004 Spine. 29(6):E107–E112. doi: 10.1097/01.brs.0000115134.97854.c9. doi: 10.1097/01.brs.0000115134.97854.c9. [DOI] [PubMed] [Google Scholar]
- Nonpharmacologic therapies for low back pain: A systematic review for an american college of physicians clinical practice guideline. Chou R., Deyo R., Friedly J.., et al. 2017Ann. Intern. Med. 166(7):493–505. doi: 10.7326/M16-2459. [DOI] [PubMed] [Google Scholar]
- Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Hicks Gregory E., Fritz Julie M., Delitto Anthony, McGill Stuart M. Sep;2005 Archives of Physical Medicine and Rehabilitation. 86(9):1753–1762. doi: 10.1016/j.apmr.2005.03.033. doi: 10.1016/j.apmr.2005.03.033. [DOI] [PubMed] [Google Scholar]
- Core stability exercise principles. Akuthota Venu, Ferreiro Andrea, Moore Tamara, Fredericson Michael. Jan;2008 Current Sports Medicine Reports. 7(1):39–44. doi: 10.1097/01.csmr.0000308663.13278.69. doi: 10.1097/01.csmr.0000308663.13278.69. [DOI] [PubMed] [Google Scholar]
- Quality of systematic reviews on specific spinal stabilization exercise for chronic low back pain. Haladay Douglas E., Miller Sayers J., Challis John, Denegar Craig R. Apr;2013 Journal of Orthopaedic & Sports Physical Therapy. 43(4):242–250. doi: 10.2519/jospt.2013.4346. doi: 10.2519/jospt.2013.4346. [DOI] [PubMed] [Google Scholar]
- Core stabilization exercise prescription, part 2: A systematic review of motor control and general (global) exercise rehabilitation approaches for patients with low back pain. Brumitt Jason, Matheson J. W., Meira Erik P. Sep 4;2013 Sports Health: A Multidisciplinary Approach. 5(6):510–513. doi: 10.1177/1941738113502634. doi: 10.1177/1941738113502634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Motor control exercises reduces pain and disability in chronic and recurrent low back pain: A meta-analysis. Byström Martin Gustaf, Rasmussen-Barr Eva, Grooten Wilhelmus Johannes Andreas. Mar;2013 Spine. 38(6):E350–E358. doi: 10.1097/brs.0b013e31828435fb. doi: 10.1097/brs.0b013e31828435fb. [DOI] [PubMed] [Google Scholar]
- The effect of the neurac sling exercise on postural balance adjustment and muscular response patterns in chronic low back pain patients. Kim Ji Hae, Kim Young Eok, Bae Sea Hyun, Kim Kyung Yoon. 2013Journal of Physical Therapy Science. 25(8):1015–1019. doi: 10.1589/jpts.25.1015. doi: 10.1589/jpts.25.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- A randomized controlled trial to determine the effect of spinal stabilization exercise intervention based on pain level and standing balance differences in patients with low back pain. Rhee Hyun Sill, Kim Yoon Hyuk, Sung Paul S. 2012Medical Science Monitor. 18(3):CR174–CR181. doi: 10.12659/msm.882522. doi: 10.12659/msm.882522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinematic analysis of selected reach directions of the star excursion balance test compared with the Y-balance test. Fullam Karl, Caulfield Brian, Coughlan Garrett F., Delahunt Eamonn. Feb;2014 Journal of Sport Rehabilitation. 23(1):27–35. doi: 10.1123/jsr.2012-0114. doi: 10.1123/jsr.2012-0114. [DOI] [PubMed] [Google Scholar]
- An examination, correlation, and comparison of static and dynamic measures of postural stability in healthy, physically active adults. Sell Timothy C. May;2012 Physical Therapy in Sport. 13(2):80–86. doi: 10.1016/j.ptsp.2011.06.006. doi: 10.1016/j.ptsp.2011.06.006. [DOI] [PubMed] [Google Scholar]
- Effect of trunk muscles training using a star excursion balance test grid on strength, endurance and disability in persons with chronic low back pain. Ganesh G. Shankar, Chhabra Deepak, Pattnaik Monalisa, Mohanty Patitapaban, Patel Rishee, Mrityunjay Kumar. Jun 17;2015 Journal of Back and Musculoskeletal Rehabilitation. 28(3):521–530. doi: 10.3233/bmr-140551. doi: 10.3233/bmr-140551. [DOI] [PubMed] [Google Scholar]
- Evaluation of static and dynamic balance tests in single and dual task conditions in participants with nonspecific chronic low back pain. Hemmati Ladan, Rojhani-Shirazi Zahra, Malek-Hoseini Hamid, Mobaraki Ismail. Sep;2017 Journal of Chiropractic Medicine. 16(3):189–194. doi: 10.1016/j.jcm.2017.06.001. doi: 10.1016/j.jcm.2017.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reliability and validity of the Y-balance test in young adults with chronic low back pain. Alshehre Yousef, Alkhathami Khalid, Brizzolara Kelli, Weber Mark, Wang-Price Sharon. Jun 1;2021 International Journal of Sports Physical Therapy. 16(3):628. doi: 10.26603/001c.23430. doi: 10.26603/001c.23430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balance control in patients with subacute non-specific low back pain, with and without lumbar instability: A cross-sectional study. Hlaing Su Su, Puntumetakul Rungthip, Wanpen Sawitri, Boucaut Rose. Apr;2020 Journal of Pain Research. 13:795–803. doi: 10.2147/jpr.s232080. doi: 10.2147/jpr.s232080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Effect of proprioceptive neuromuscular facilitation integration pattern and swiss ball training on pain and balance in elderly patients with chronic back pain. Young Kim Jin, Je Choi Won, Hwa Seo Tae. 2015Journal of Physical Therapy Science. 27(10):3237–3240. doi: 10.1589/jpts.27.3237. doi: 10.1589/jpts.27.3237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The reliability of an instrumented device for measuring components of the star excursion balance test. Plisky P.J., Gorman P.P., Butler R.J.., et al. 2009N Am J Sports Phys Ther. 4(2):92–99. [PMC free article] [PubMed] [Google Scholar]
- Y- balance test: a reliability study involving multiple raters. Shaffer Scott W., Teyhen Deydre S., Lorenson Chelsea L., Warren Rick L., Koreerat Christina M., Straseske Crystal A., Childs John D. Nov;2013 Military Medicine. 178(11):1264–1270. doi: 10.7205/milmed-d-13-00222. doi: 10.7205/milmed-d-13-00222. [DOI] [PubMed] [Google Scholar]
- G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Faul Franz, Erdfelder Edgar, Lang Albert, Buchner Axel. May;2007 Behavior Research Methods. 39(2):175–191. doi: 10.3758/bf03193146. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- Sportsmetrics™ training improves power and landing in high school rowers. Chimera N.J., Kremer K. 2016Int J Sports Phys Ther. 11(1):44. [PMC free article] [PubMed] [Google Scholar]
- The influence of lower-limb dominance on postural balance. Alonso Angélica Castilho, Brech Guilherme Carlos, Bourquin Andréia Moraes, Greve Julia Maria D'Andréa. Dec;2011 Sao Paulo Medical Journal. 129(6):410–413. doi: 10.1590/s1516-31802011000600007. doi: 10.1590/s1516-31802011000600007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Identifying psychosocial variables in patients with acute work-related low back pain: the importance of fear-avoidance beliefs. Fritz Julie M, George Steven Z. Oct 1;2002 Physical Therapy. 82(10):973–983. doi: 10.1093/ptj/82.10.973. doi: 10.1093/ptj/82.10.973. [DOI] [PubMed] [Google Scholar]
- Psychometric properties of the Tampa scale for kinesiophobia and the fear-avoidance beliefs questionnaire in acute low back pain. Swinkels-Meewisse E.J., Swinkels R.A., Verbeek A.L., Vlaeyen J.W., Oostendorp R.A. Feb;2003 Manual Therapy. 8(1):29–36. doi: 10.1054/math.2002.0484. doi: 10.1054/math.2002.0484. [DOI] [PubMed] [Google Scholar]
- Performance of a patient reported outcomes measurement information system (PROMIS) short form in older adults with chronic musculoskeletal pain. Deyo Richard A., Ramsey Katrina, Buckley David I., Michaels LeAnn, Kobus Amy, Eckstrom Elizabeth, Forro Vanessa, Morris Cynthia. Dec 24;2015 Pain Medicine. 17(2):314–324. doi: 10.1093/pm/pnv046. doi: 10.1093/pm/pnv046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Responsiveness of the numeric pain rating scale in patients with low back pain. Childs John D., Piva Sara R., Fritz Julie M. Jun;2005 Spine. 30(11):1331–1334. doi: 10.1097/01.brs.0000164099.92112.29. doi: 10.1097/01.brs.0000164099.92112.29. [DOI] [PubMed] [Google Scholar]
- A comparison of five low back disability questionnaires: reliability and responsiveness. Davidson Megan, Keating Jennifer L. Jan 1;2002 Physical Therapy. 82(1):8–24. doi: 10.1093/ptj/82.1.8. doi: 10.1093/ptj/82.1.8. [DOI] [PubMed] [Google Scholar]
- A comparison of a modified Oswestry low back pain disability questionnaire and the Quebec back pain disability scale. Fritz Julie M, Irrgang James J. Feb 1;2001 Physical Therapy. 81(2):776–788. doi: 10.1093/ptj/81.2.776. doi: 10.1093/ptj/81.2.776. [DOI] [PubMed] [Google Scholar]
- Using the star excursion balance test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. Gribble Phillip, Hertel Jay, Plisky Phil. May 1;2012 Journal of Athletic Training. 47(3):339–357. doi: 10.4085/1062-6050-47.3.08. doi: 10.4085/1062-6050-47.3.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The effect of variable rest intervals and chronic ankle instability on triplanar ankle motion during performance of the star excursion balance test. Kwon Yong Ung, Blaise Williams D.S. Apr;2017 Human Movement Science. 52:143–150. doi: 10.1016/j.humov.2017.01.013. doi: 10.1016/j.humov.2017.01.013. [DOI] [PubMed] [Google Scholar]
- Spinal stabilization exercise effectiveness for low back pain in adolescent idiopathic scoliosis: A randomized trial. Zapata Karina Amani, Wang-Price Sharon S., Sucato Daniel J., Thompson Mary, Trudelle-Jackson Elaine, Lovelace-Chandler Venita. 2015Pediatric Physical Therapy. 27(4):396–402. doi: 10.1097/pep.0000000000000174. doi: 10.1097/pep.0000000000000174. [DOI] [PubMed] [Google Scholar]
- Awareness and knowledge of the 2008 physical activity guidelines for americans. Kay Melissa C., Carroll Dianna D., Carlson Susan A., Fulton Janet E. May;2014 Journal of Physical Activity and Health. 11(4):693–698. doi: 10.1123/jpah.2012-0171. doi: 10.1123/jpah.2012-0171. [DOI] [PubMed] [Google Scholar]
- Intratester and intertester reliability during the star excursion balance tests. Hertel Jay, Miller S. John, Denegar Craig R. May;2000 Journal of Sport Rehabilitation. 9(2):104–116. doi: 10.1123/jsr.9.2.104. doi: 10.1123/jsr.9.2.104. [DOI] [Google Scholar]
- Is standing balance altered in individuals with chronic low back pain? A systematic review. Berenshteyn Yevgeniy, Gibson Kelsey, Hackett Gavin C., Trem Andrew B., Wilhelm Mark. 2019Disability and Rehabilitation. 41(13):1514–1523. doi: 10.1080/09638288.2018.1433240. doi: 10.1080/09638288.2018.1433240. [DOI] [PubMed] [Google Scholar]
- Effect of spinal stabilization exercise on dynamic postural control and visual dependency in subjects with chronic non-specific low back pain. Salavati Mahyar, Akhbari Behnam, Takamjani Ismail Ebrahimi, Bagheri Hossein, Ezzati Kamran, Kahlaee Amir Hossein. Apr;2016 Journal of Bodywork and Movement Therapies. 20(2):441–448. doi: 10.1016/j.jbmt.2015.10.003. doi: 10.1016/j.jbmt.2015.10.003. [DOI] [PubMed] [Google Scholar]
- Using the star excursion balance test to assess dynamic postural-control deficits and outcomes in lower extremity injury: A literature and systematic review. Gribble Phillip A., Hertel Jay, Plisky Phil. May 1;2012 Journal of Athletic Training. 47(3):339–357. doi: 10.4085/1062-6050-47.3.08. doi: 10.4085/1062-6050-47.3.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Relationships between lower-extremity flexibility, asymmetries, and the Y balance test. Overmoyer Grant V., Reiser Raoul F. May;2015 Journal of Strength and Conditioning Research. 29(5):1240–1247. doi: 10.1519/jsc.0000000000000693. doi: 10.1519/jsc.0000000000000693. [DOI] [PubMed] [Google Scholar]
- The clinical importance of changes in outcome scores after treatment for chronic low back pain. Hägg O., Fritzell P., Nordwall A. Feb;2003 European Spine Journal. 12(1):12–20. doi: 10.1007/s00586-002-0464-0. doi: 10.1007/s00586-002-0464-0. [DOI] [PubMed] [Google Scholar]
- An update of stabilisation exercises for low back pain: A systematic review with meta-analysis. Smith Benjamin E, Littlewood Chris, May Stephen. Dec;2014 BMC Musculoskeletal Disorders. 15(1):1–21. doi: 10.1186/1471-2474-15-416. doi: 10.1186/1471-2474-15-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


