Abstract
The incidence of knee injuries in sport, particularly involving the ACL, appears to be increasing yearly, especially in younger age athletes. Even more concerning is the frequency of ACL reinjury also appears to be increasing year after year. Improving the objective criteria and testing methods used to determine return to play (RTP) readiness following ACL surgery is one aspect of the rehabilitation process that can significantly help in reducing reinjury rates. Currently, the majority of clinicians are still using post operative time frames as their number one criterion for clearance to RTP. This flawed method demonstrates an inadequate reflection of the true unpredictable, dynamic environment athletes are returning to participate in. In our clinical experience, objective testing to allow for clearance to sport participation following an ACL injury should incorporate neurocognitive and reactive testing due to the nature of the injury typically occurs because of failed control of unanticipated reactive movements. The purpose of this manuscript is to share a neurocognitive testing sequence we currently employ consisting of 8 tests in 3 categories: Blazepod tests, reactive shuttle run tests, and reactive hop tests. The use of a more dynamic reactive testing battery may decrease the reinjury rates when an athlete is cleared for participation by measuring readiness in chaotic circumstances that are more truly reflective of the sporting environment the athlete is working to return to and in the process give them a greater sense of confidence.
Keywords: ACL injury, neurocognitive training, reactive testing, return to play
Introduction
It is estimated there are between 200,000 to 250,000 anterior cruciate ligament (ACL) knee injuries sustained annually in the United States, resulting in approximately 150,000 to 165,000 ACL surgeries each year.1,2 The incidence of these serious knee injuries appears to be increasing yearly, especially in high school aged athletes. More troublesome than the frequency of ACL injuries, is the rate of reinjury also appears to be increasing year after year. Investigators have reported reinjury rates following ACL surgery to range as high as 30-39%.3,4 This rate of reinjury results in as many as 4 in every 10 surgeries being attributed to reinjury. This level of reinjury following ACL surgery is unacceptable. In these instances, the athlete has already suffered one significant knee injury, undergone surgery, and worked through the rehabilitation process afterwards only to suffer another ACL injury to either the opposite or the previously reconstructed knee. As health care providers we need to critically examine every available way to reduce ACL reinjury rates. One area that can significantly help in reducing these reinjury rates is improving the methodology used in return to play (RTP) testing following ACL surgery.
The cause of these unacceptably high reinjury rates has been attributed to a number of factors. First, there is a surprising overall lack of RTP testing generally utilized in making RTP decisions. Barber-Westin and Noyes3 reported in a large meta-analysis and systematic review of 716 articles that only 13% utilized objective criteria in determining readiness to return an athlete back to participation following ACL surgery. This lack of testing is extremely disappointing when you consider that a reduction in reinjury rates has been demonstrated by utilizing objective RTP testing in the decision-making process.5–7 Second, athletes are returning to participate in sport without completing the entire rehabilitation process, often due to insurance plan limitations, an inability to afford rehabilitation following the exhaustion of benefits, or self-discharge. Each of these factors results in incomplete rehabilitation, placing the athlete at risk of reinjury. Third, is the frequent lack of high-level activities and functional sport-specific challenges during the rehabilitation process. When an athlete is not challenged in a similar environment, with replicating demands matching those of the sport, they are often returning to the result inadequately prepared and therefore a higher risk of reinjury. Next, is the fact that most of the RTP tests currently in use are single task drills with anticipated movements. Sports are seldom single task activities and often involve unanticipated movements. Brophy et al8,9 and others10,11 have reported the majority of soccer injuries sustained to the female player occurred during defending and/or with unanticipated reactive movements. For example, a soccer player may be performing soccer drills with other players to create an environment of distraction, controlled chaos, and dual tasking. This combination of variables and the hierarchy of tasks inherent to sport makes single task drills insufficient to assess RTP readiness. Lastly, the athlete often goes back to their sport or activities unprepared and at risk of reinjury for a combination of the reasons listed above.
The present RTP testing methodology is underutilized and when employed not satisfactorily effective to appropriately determine RTP readiness of the athlete following ACL surgery. Most decisions are made in the Physician’s office, based solely on physical examination and subjective reporting. Typically, when RTP testing is performed, it is not done in the same environment or with sport specificity. Testing needs to be conducted with an emphasis on the performance of multiple tasks, neurocognitive challenges, and motor control. RTP decisions should be made by a team of health care providers looking at the athlete’s readiness from a variety of viewpoints to make an informed decision based on subjective, objective and functional data. RTP criteria should not be a single event to determine readiness to return athletes to all levels of sport.
RTP testing for the lower extremity following ACL surgery has been discussed extensively in the literature since the mid 1980’s. There are over 500 articles that present various testing procedures and protocols. These testing procedures include single leg hop testing, shuttle running, balance testing and functional movement screening, isokinetic testing, and limb symmetry index assessment to list just a few.12–19 While these tests are all good measures of what they are designed to assess, they all test a single task, and none involve reactive assessment. Even the tests used that replicate drills employed in sport training, are simply drills and not truly specific sport related activities. These tests are good, serve a vital purpose and we recommend them as tests to assist in determining rehabilitation progression.
Historically all these tests have been referred to as RTP tests. They are more appropriately tests suited to determine athlete readiness to begin progression through rehabilitation, running, jumping, agility drills, or other transitional programs. They are not true measures to assess readiness to return to competitive play. These tests are predictable, in that the athlete is asked to perform a specific movement or task and is evaluated based on their resultant performance of this movement. In sports, there are numerous unpredictable movements that the athlete must perform, most of these are reactive in nature and have multiple stimuli occurring simultaneously. Therefore, to effectively assess return to play readiness during the recovery after ACL surgery, the RTP tests must measure those types of sport activities, movements, and reactions. The problem is these tests do not assess reaction time, dynamic stabilization, dynamic reaction movements and do not tell us if the athlete is ready to initiate competitive practice or return to competitive play.
Although there are limitations in the previous metrics for clinical decision making for RTP, it is important to recognize some of the research of the tests which provide the criteria to progress to the neurocognitive testing. Refer to the list below for an example checklist or functional testing algorithm for a criterion-based approach for progression through rehabilitation and in preparation for using the advanced testing methods.20
VAS/NPRS
PROs
Kinesiophobia
Anthropometric measurement for effusion
Static balance/Dynamic balance
AROM/PROM – Knee/PF
Strength Testing – TLS: LSI, Unilateral ratios, Allometric scaling to BW
Special Tests for ligament stability: Lachman’s, Pivot Shift, KT1000/2000
Walking/running gait analysis
Functional movement patterns
Jump Test
Hop Tests
T-drill hop test
Change of Direction Test
LEFT (adds acceleration/deceleration [anterior/retro] and acute fatigue factor
Even though the “missing link” is the neurocognitive reactive testing, there must be preparatory testing that leads to criterion-based metrics that prepares the patients to perform the neurocognitive reactive testing. Therefore, criteria that can be used to determine the patient’s readiness for performing these advanced neuro-cognitive reactive tests are described in Table 1.
Table 1.
| Measurements | Methods of Assessments | Objective Criteria |
|---|---|---|
| Pain21 | VAS/NPRS | <3 during & after therapeutic exercises |
| PROs22 | ||
| Kinesiophobia23,24 | ACL-RSI | > 55 points |
| Posture | Posture Grid | LSI/WNL |
|
Gait/Running/Movement
Analysis |
Qualitative Analysis | WNL |
| Knee effusion | Anthropometric measurements /Sweep Test |
<1 cm. LSI |
| Palpation | No c/o pain | |
| Balance/Proprioception25 | Static Dynamic |
WNL-LSI WNL/LSI |
| AROM26,27 | Goniometry Digital gonios |
<10% LSI |
| PROM26,27 | Goniometry, Qualitative end feels |
< 10 % LSI |
| Special Tests | Lachman’s/ Pivot Shift |
Negative Negative |
|
Muscle Strength28
(Total Leg Strength-TAS) Core, Hip, Knee, Ankle |
HHD, Isokinetics | <10% LSI, %BW, Norms |
|
Muscle Power
(Total Leg Strength-TAS) Core, Hip, Knee, Ankle |
HHD, Isokinetics Force Plates |
<10% LSI, %BW, Norms; RFD |
|
Muscle Endurance
(Total Leg Strength-TAS) Core, Hip, Knee, Ankle |
Isokinetics Force Plates |
<10% LSI, %BW, Norms |
| Functional Tests29–35 | Jump Tests Hop Tests T-Drill Hop Test Change of Lateral Direction Test LEFT |
% - Height <10% -LSI; % Height; Norms <10 % - LSI <10% - LSI Norms |
The purpose of this manuscript is to present a proposed testing and RTP model we currently use clinically. This RTP testing includes neurocognitive testing, reactive motor control testing, dual tasking, and psychological readiness with the main focus on reactive unanticipated test movements.
Neurocognitive Testing
Appropriate testing of RTP readiness following ACL surgery, should not only assess if the athlete appears ready to resume play but also be directed toward minimizing the risk of reinjury. To accomplish this, testing must be more dynamic, sport oriented, and even unpredictable in nature. A neurocognitive testing battery must include measures of reactive response and incorporate sport-type reactions and movements. Testing must also be safe, easy to perform and measure, and require minimal equipment to complete. Neurocognitive testing is a way to measure various aspects of cognitive function non-invasively. These cognitive functions include things like reaction time, multi-tasking, attention, memory, and perception. Short tests designed to assess these functions produce objective measures that can be compared to standard scores or to an individual’s baseline scores when available. Readiness to return to sport involves more than just the readiness of the musculoskeletal system. The neurocognitive system is a vital aspect of sport due to the constant use of cognitive functions such as reaction time and multi-tasking. Reaction time testing has been shown to be highly reliable and can be used to assess an athlete’s cognitive and athletic ability.36 Musculoskeletal injuries affect the neurocognitive system as well, so assessing and training this system can lead to better outcomes when determining readiness to return to play. Simon et al37 demonstrated that the addition of a neurocognitive and anticipatory component to the traditional hop test series resulted in a statistical difference in performance and may improve functional return to sport testing. When comparing reactive versus preplanned agility testing, Serpell et al38 demonstrated a difference in mean reaction time between elite and subelite groups in the way in which they contributed to perceptual skills and/or reaction ability. All of these factors combine to make the incorporation of neurocognitive training and testing elements crucial to advancing the effectiveness of RTP testing following ACL surgery and help to minimize the risk of reinjury as the athlete returns to competition.
Proposed Testing Sequence
The neurocognitive testing sequence we currently employ consists of a total of 8 tests in 3 categories: Blazepod tests, reactive shuttle run tests, and reactive hop tests. Testing is performed sequentially using 3 Blazepod tests, 2 reactive shuttle runs and finally 3 reactive hop tests. Adequate rest and recovery are allowed between tests. Based on the duration of the tests, the patients are permitted a 1-3 minute rest between tests. The testing measures are:
Blazepod Tests
Blazepod Lateral Slide Test
The lateral slide test begins with four Blazepods positioned in a straight line five feet apart (60 inches). (Figure 1) The pods are configured in a randomized pattern using a single target color (blue) and five distracting colors (purple, green, orange, red, and yellow). One pod will light up the target color (blue) and the remaining three will be lit in distracting colors. Lights are set to transition on a hit and with zero-time delay between each transition. The athlete is instructed to begin in the center of the pods and will shuffle laterally targeting the blue light. Athletes are required to maintain a mini squat in an athletic position throughout the test and must avoid hopping or running between lights. Another individual will be tossing a soccer ball towards the target light. The athlete is instructed to catch the ball, tap the target light then toss the ball back while locating the next light and shuffling to it in a good athletic ready position. Once the test begins the goal is to tap as many lights as possible in 30 seconds. The total number of taps as well as average reaction time is calculated and scored following completion of the test.
Figure 1. Lateral slide test with light targets (Blazepods Inc.).
Each target light is 60 inches apart.
Blazepod 4 Corners Test
The 4 corners reactive test begins with four Blazepods positioned in a square 21 feet (252 inches) apart. (Figure 2) As in the first test the pods are configured in a randomized pattern where one pod will light up the target color (blue) and the remaining three will be a distracting color (purple, green, orange, red, and yellow). Lights are set to transition on a hit and with zero-time delay between each transition. The athlete is instructed to begin in the center of the pods and locate the blue light. Another individual will be tossing a soccer ball towards the target light. The athlete is instructed to catch the ball, tap the light then toss the ball back while locating the next light. Once the test begins the goal is to tap as many lights as possible in 30 seconds. Total number of taps as well as average reaction time is calculated following completion of the test.
Figure 2. Four corner target light test (Blazepods Inc.).

Each light target is 21 feet apart.
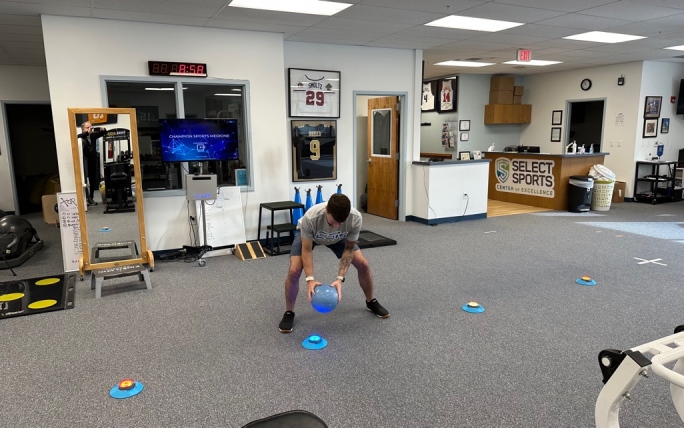
Blazepod Standing Right Versus. Left Reactive Test
The standing right versus left reactive test begins with four Blazepods positioned in a rectangle 36 inches in length and 12 inches wide. (Figure 3) The pods are configured in a randomized pattern so that any of the four can illuminate with only one at a single point in time. Lights are set to transition on a hit, with zero-time delay between each. In this test both blue and red are set as the target colors which represents the color in which the single pod will illuminate. The athlete begins in double limb stance with their feet shoulder width apart between the four pods performing fast feet. If the pod illuminates blue they are instructed to hit it with their left foot and if red, then hit it with their right foot. After each hit the pods will change color and the athlete must react to contact the next target color. Once the test begins the goal is to tap as many target lights as possible in 15 seconds. Total number of taps, number of errors, as well as average reaction time is calculated following completion of the test.
Figure 3. Standing Right versus Left Reactive target light test.

Targets are placed 3 feet apart and the participant is instructed to tap the right foot to the red target & the left foot to the blue target.
Reactive Shuttle Run Testing
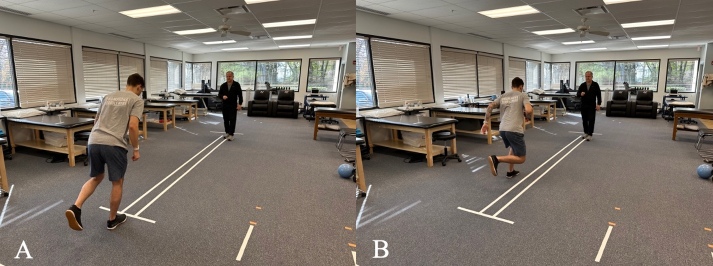
Reactive 10-yard T Shuttle Run Test
The reactive 10-yard T shuttle run test begins with 4 cones positioned in a “T”. (Figure 4) The individual cone is positioned 10 yards from the other three which are each 5 yards apart forming a “T”. The athlete begins at the individual cone and is instructed to sprint towards the cone directly in front of them. Once two thirds to the first cone, the tester will call out right or left, signifying the direction the athlete will begin to shuffle laterally towards. They are instructed to slide laterally 5 yards to the furthest cone, tap it, then reverse and slide laterally 10 yards to the furthest cone in the opposite direction and tap it. Once they tap the second cone, they reverse slide 5 yards back to the middle cone. Finally, after taping the middle cone the athlete will pivot and run 10 yards back to the starting position. The goal is to complete the test as quickly as possible. The time begins when they start their run and stops when they pass the final cone.
Figure 4. Reactive 10-yard T Shuttle Run Test.
This test involves a 10-yard run then a side shuffle to one direction for 5 yards & then in opposite direction for 5 yards and then turn and run back to start line.
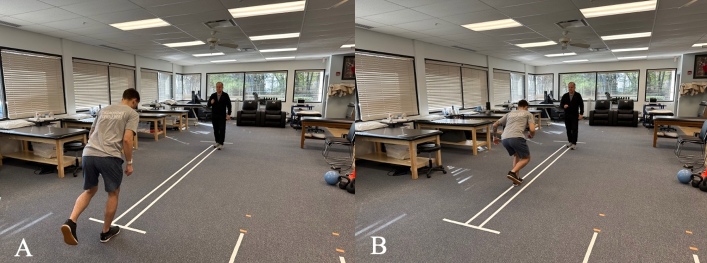
Reactive 10-Yard L Run Test
The reactive 10-yard L run test begins with 4 cones positioned in a “T”. (Figure 5) The individual cone is positioned 10 yards from the other three which are each 5 yards apart. The athlete is instructed to begin at the individual cone and sprint towards the cone directly in front of them. Once two thirds to the first cone, the tester will call out which direction the athlete will go. Once the direction is called, the athlete will turn in the direction named and sprint around the far cone. To finish the test the athlete will sprint back to the middle cone, pivot and then sprint back to the starting position, completing the “L”. The goal is to complete the test as quickly as possible. The time begins when they start their run and stops when they pass the finally cone.
Figure 5. Reactive 10 Yard L Run Test.
This test is performed with a 10 yard straight run then a turn to instructed direction for 5 yards and then a turn back to start position.
Reactive Hop Testing
Reactive Single Limb Hop for Distance
The reactive single limb hop for distance test begins with the athlete standing on one limb. The athlete is instructed to hop forward from the starting position as far as possible. (Figure 6) While in the air the tester will call out right or left designating the foot in which the athlete is required to land on. The goal of the test is to hop as far as possible and land solidly on the designated leg. Athletes must stick the landing for 2-3 seconds for the test to count. Three consecutive repetitions are performed, and the distance is averaged. The distance is measure from the starting line to the back of the landing leg heel.
Figure 6. Reactive Single Leg Hop for Distance Test.
The participant stands on one foot and hops outward – as the participant hops, they are instructed which foot to land on.
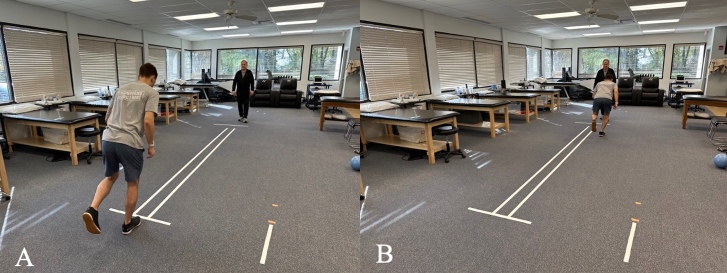
Reactive Single Limb Cross Over Hop for Distance
The reactive single limb cross over hop for distance test begins with the athlete standing on one limb. The test begins with the athlete hopping as far as possible off the single limb. While in the air the tester will call out the foot in which the athlete is required to land on, either left or right, crossing the center line of the testing field. (Figure 7) They will then complete the sequence by completing two more cross over hops on the same limb. The athlete is instructed to hop as far as possible with each hop and stick the final landing for 2-3 seconds. They will complete three consecutive repetitions and take the average distance between each test as the final score. The distance is measure from the starting line to the back of the athlete’s heel at the final hop.
Figure 7. Reactive Single Limb Cross Over Hop for Distance Test.
The participant stands on one foot and hops outward – as the participant hops, they are instructed which foot to land on and they must cross over the center tape. They will then complete the sequence by completing two more cross over hops on the same limb.
Reactive Single Limb Alternating Cross Over Hop for Distance
The reactive single limb alternating cross over hop for distance test begins with the athlete standing on one limb (Figure 8). The athlete is instructed to hop forward as far as possible. While in the air the tester will call out a foot on which the athlete is required to land, either left or right. The athlete will then complete the sequence by performing two more cross over hops successively on alternating limbs. The athlete is instructed to hop as far as possible with each hop and stick the final landing holding for 2-3 seconds. They will complete three consecutive repetitions and take the average distance between each test. As with the other tests the distance is measure from the starting line to the back of the athlete’s heel.
Figure 8. Reactive Single Limb Alternate Cross Over Hop for Distance Test.
The participant stands on one foot and hops outward – as the participant hops, they are instructed which foot to land on and they must cross over the center tape. The athlete will then complete the sequence by performing two more cross over hops successively on alternating limbs.
Videos of the drills and tests in this manuscript can be found here: VIDEO FOLDER.
Limitations
Although these are examples of some of the tests that are currently being used clinically because of ecological validity, nevertheless, we have to acknowledge the limitations of these tests. The tests have not been tested for reliability, validity or predicative validity regarding follow-up effectiveness for athletes to return to play, return to performance or prevention of reinjury.
Conclusion
The current state of RTP testing following ACL surgery is inadequate and does not reflect the true unpredictable, dynamic environment athletes are returning to. Not only is there a need for better utilization of RTP testing for predicting readiness, the significant incidence of reinjury must also be drastically reduced. These needs require both an improvement in the type of tests utilized and the overall use of subjective, objective and functional RTP testing in determining readiness to resume unrestricted activity. It is our hope that presenting this theoretical model for the use of neurocognitive testing in assessing athletic readiness that more critical thought will be placed on the type of testing needed to help determine when an athlete is capable of returning to sport. Also, the use of a more dynamic testing battery may decrease the reinjury rates when an athlete is cleared for participation.
References
- Current trends in anterior cruciate ligament reconstruction. Part 1: Biology and biomechanics of reconstruction. Fu Freddie H., Bennett Craig H., Lattermann Christian, Ma C. Benjamin. Nov;1999 The American Journal of Sports Medicine. 27(6):821–830. doi: 10.1177/03635465990270062501. doi: 10.1177/03635465990270062501. [DOI] [PubMed] [Google Scholar]
- Anterior Cruciate Ligament Injury Prevention and Rehabilitation: Let's Get it Right. Wilk Kevin E. Oct;2015 Journal of Orthopaedic & Sports Physical Therapy. 45(10):729–730. doi: 10.2519/jospt.2015.0109. doi: 10.2519/jospt.2015.0109. [DOI] [PubMed] [Google Scholar]
- Factors used to determine return to unrestricted sports activities after anterior cruciate ligament reconstruction. Barber-Westin Sue D., Noyes Frank R. Dec;2011 Arthroscopy: The Journal of Arthroscopic & Related Surgery. 27(12):1697–1705. doi: 10.1016/j.arthro.2011.09.009. doi: 10.1016/j.arthro.2011.09.009. [DOI] [PubMed] [Google Scholar]
- Paterno Mark V., Rauh Mitchell J., Schmitt Laura C., Ford Kevin R., Hewett Timothy E. The American Journal of Sports Medicine. 7. Vol. 42. SAGE Publications; Incidence of Second ACL Injuries 2 Years After Primary ACL Reconstruction and Return to Sport; pp. 1567–1573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grindem Hege, Snyder-Mackler Lynn, Moksnes Håvard, Engebretsen Lars, Risberg May Arna. British Journal of Sports Medicine. 13. Vol. 50. BMJ; Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study; pp. 804–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyritsis Polyvios, Bahr Roald, Landreau Philippe, Miladi Riadh, Witvrouw Erik. British Journal of Sports Medicine. 15. Vol. 50. BMJ; Likelihood of ACL graft rupture: not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture; pp. 946–951. [DOI] [PubMed] [Google Scholar]
- Return to play testing following anterior cruciate reconstruction – a systematic review & meta-analysis. Hurley Eoghan T., Mojica Edward S., Haskel Jonathan D., Mannino Brian J., Alaia Michael, Strauss Eric J., Jazrawi Laith M., Gonzlaez-Lomas Guillem. Jan;2022 The Knee. 34:134–140. doi: 10.1016/j.knee.2021.11.010. doi: 10.1016/j.knee.2021.11.010. [DOI] [PubMed] [Google Scholar]
- Defending Puts the Anterior Cruciate Ligament at Risk During Soccer: A Gender-Based Analysis. Brophy R.H., Stepan J.G., Silvers H.J., Mandelbaum B.R. 2015Sports Health. 7(3):244–249. doi: 10.1177/1941738114535184. doi: 10.1177/1941738114535184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gender influences: the role of leg dominance in ACL injury among soccer players. Brophy R., Silvers H. J., Gonzales T., Mandelbaum B. R. Jun 11;2010 British Journal of Sports Medicine. 44(10):694–697. doi: 10.1136/bjsm.2008.051243. doi: 10.1136/bjsm.2008.051243. [DOI] [PubMed] [Google Scholar]
- Three distinct mechanisms predominate in non-contact anterior cruciate ligament injuries in male professional football players: a systematic video analysis of 39 cases. Walden M, Krosshaug T, Bjorneboe J, Andersen T E, Faul O, Hagglund M. 2015Br J Sports Med. 49(22):1452–1460. doi: 10.1136/bjsports-2014-094573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechanisms of anterior cruciate ligament injuries in elite women’s netball: a systematic video analysis. Stuelcken Max C., Mellifont Daniel B., Gorman Adam D., Sayers Mark G.L. 2016Journal of Sports Sciences. 34(16):1516–1522. doi: 10.1080/02640414.2015.1121285. doi: 10.1080/02640414.2015.1121285. [DOI] [PubMed] [Google Scholar]
- Rehabilitation and return to sport testing after Anterior Cruciate Ligament Reconstruction: Where are we in 2022? Gokeler A., Dingenen B., Hewett T.E. 2022Rehabilitation and Return to Sport in Athletics. 4(1):E77–E82. doi: 10.1016/j.asmr.2021.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logerstedt David, Grindem Hege, Lynch Andrew, Eitzen Ingrid, Engebretsen Lars, Risberg May Arna, Axe Michael J., Snyder-Mackler Lynn. The American Journal of Sports Medicine. 10. Vol. 40. SAGE Publications; Single-legged Hop Tests as Predictors of Self-reported Knee Function After Anterior Cruciate Ligament Reconstruction: The Delaware-Oslo ACL Cohort Study; pp. 2348–2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quantitative assessment of functional limitations in normal and anterior cruciate ligament-deficient knees. Barber SUE D., Noyes FRANK R., Mangine ROBERT E., McCloskey JOHN W., Hartman WILLJAM. Jun;1990 Clinical Orthopaedics and Related Research. 255:204–214. doi: 10.1097/00003086-199006000-00028. doi: 10.1097/00003086-199006000-00028. [DOI] [PubMed] [Google Scholar]
- Noyes Frank R., Barber Sue D., Mangine Robert E. The American Journal of Sports Medicine. 5. Vol. 19. SAGE Publications; Abnormal Lower Limb Symmetry Determined by Function Hop Tests after Anterior Cruciate Ligament Rupture; pp. 513–518. [DOI] [PubMed] [Google Scholar]
- Bolgla Lori A., Keskula Douglas R. Journal of Orthopaedic & Sports Physical Therapy. 3. Vol. 26. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Reliability of lower extremity functional performance tests; pp. 138–142. [DOI] [PubMed] [Google Scholar]
- Myer Gregory D., Schmitt Laura C., Brent Jensen L., Ford Kevin R., Barber Foss Kim D., Scherer Bradley J., Heidt Robert S. Jr., Divine Jon G., Hewett Timothy E. Journal of Orthopaedic & Sports Physical Therapy. 6. Vol. 41. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); Utilization of modified NFL combine testing to identify functional deficits in athletes following ACL reconstruction; pp. 377–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The relationships among isometric, isotonic, and isokinetic concentric and eccentric quadriceps and hamstrings force and three components of athletic performance. Anderson Mark A., Gieck Joe H., Perrin David, Weltman Art, Rutt Richard, Denegar Craig. Sep;1991 Journal of Orthopaedic & Sports Physical Therapy. 14(3):114–120. doi: 10.2519/jospt.1991.14.3.114. doi: 10.2519/jospt.1991.14.3.114. [DOI] [PubMed] [Google Scholar]
- Wilk Kevin E., Romaniello William T., Soscia Susan M., Arrigo Christopher A., Andrews James R. Journal of Orthopaedic & Sports Physical Therapy. 2. Vol. 20. Journal of Orthopaedic & Sports Physical Therapy (JOSPT); The relationship between subjective knee scores, isokinetic testing, and functional testing in the ACL-reconstructed knee; pp. 60–73. [DOI] [PubMed] [Google Scholar]
- Functional Progression of a Patient Through a Rehabilitation Program. Davies G.J., Zillmer D.A. 2000Orthopaedic Physical Therapy Clinics of North America. 9:103–118. [Google Scholar]
- Douleurs après ligamentoplastie du ligament croise antérieur: démembrement et prise en charge. Savalli L, Hernandez-Sendin M.I, Puig P.L, Trouvé P. Aug;2004 Annales de Réadaptation et de Médecine Physique. 47(6):299–308. doi: 10.1016/j.annrmp.2004.05.005. doi: 10.1016/j.annrmp.2004.05.005. [DOI] [PubMed] [Google Scholar]
- Anterior cruciate ligament reconstruction: the short-term recovery using the Knee Injury and Osteoarthritis Outcome Score (KOOS) Hill Gareth N., O’Leary Sean T. Sep 30;2013 Knee Surgery, Sports Traumatology, Arthroscopy. 21(8):1889–1894. doi: 10.1007/s00167-012-2225-x. doi: 10.1007/s00167-012-2225-x. [DOI] [PubMed] [Google Scholar]
- Critical Criteria Recommendations: Return to Sport After ACL reconstruction requires evaluation of time after surgery of 8 months, >2 functional tests, psychological readiness, and quadriceps/hamstring strength. Turk Robby, Shah Sarav, Chilton Matthew, Thomas Terence L., Anene Chibuzo, Mousad Albert, Le Breton Stephen, Li Lambert, Pettit Rob, Ives Katharine, Ramappa Arun. Oct 7;2022 Arthroscopy: The Journal of Arthroscopic & Related Surgery. doi: 10.1016/j.arthro.2022.08.038. doi: 10.1016/j.arthro.2022.08.038. [DOI] [PubMed]
- Huang Hui, Nagao Masashi, Arita Hitoshi, Shiozawa Jun, Nishio Hirofumi, Kobayashi Yohei, Kaneko Haruka, Nagayama Masataka, Saita Yoshitomo, Ishijima Muneaki, Takazawa Yuji, Ikeda Hiroshi, Kaneko Kazuo. Health and Quality of Life Outcomes. 1. Vol. 17. Springer Science and Business Media LLC; Reproducibility, responsiveness and validation of the Tampa Scale for Kinesiophobia in patients with ACL injuries. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knee joint position sense ability in elite athletes who have returned to international level play following ACL reconstruction: A cross-sectional study. Relph Nicola, Herrington Lee. Dec;2016 The Knee. 23(6):1029–1034. doi: 10.1016/j.knee.2016.09.005. doi: 10.1016/j.knee.2016.09.005. [DOI] [PubMed] [Google Scholar]
- Range of Motion, Strength, and Function After ACL Reconstruction Using a Contralateral Patellar Tendon Graft. Shelbourne K. Donald, Benner Rodney, Gray Tinker, Bauman Scot. Nov 1;2022 Orthopaedic Journal of Sports Medicine. 10(11):232596712211381. doi: 10.1177/23259671221138103. doi: 10.1177/23259671221138103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osteoarthritis after anterior cruciate ligament reconstruction: the importance of regaining and maintaining full range of motion. Shelbourne K. Donald, Freeman Heather, Gray Tinker. 2012Sports Health: A Multidisciplinary Approach. 4(1):79–85. doi: 10.1177/1941738111430201. doi: 10.1177/1941738111430201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- How limb dominance influences limb symmetry in ACL patients: effects on functional performance. Zumstein F., Centner C., Ritzmann R. Dec 7;2022 BMC Sports Science, Medicine and Rehabilitation. 14(1):206. doi: 10.1186/s13102-022-00579-y. doi: 10.1186/s13102-022-00579-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strength Asymmetry and Landing Mechanics at Return to Sport after Anterior Cruciate Ligament Reconstruction. Schmitt LAURA C., Paterno MARK V., Ford KEVIN R., Myer GREGORY D., Hewett TIMOTHY E. Jul;2015 Medicine & Science in Sports & Exercise. 47(7):1426–1434. doi: 10.1249/mss.0000000000000560. doi: 10.1249/mss.0000000000000560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Acceleration and Orientation Jumping Performance Differences Among Elite Professional Male Handball Players With or Without Previous ACL Reconstruction: An Inertial Sensor Unit-Based Study. Setuain Igor, González-Izal Miriam, Alfaro Jesús, Gorostiaga Esteban, Izquierdo Mikel. May 21;2015 PM&R. 7(12):1243–1253. doi: 10.1016/j.pmrj.2015.05.011. doi: 10.1016/j.pmrj.2015.05.011. [DOI] [PubMed] [Google Scholar]
- Knee extensor strength, hop performance, patient-reported outcome and inter-test correlation in patients 9–12 months after anterior cruciate ligament reconstruction. Ebert Jay R., Edwards Peter, Preez Luke Du, Furzer Bonnie, Joss Brendan. Jun;2021 The Knee. 30:176–184. doi: 10.1016/j.knee.2021.04.012. doi: 10.1016/j.knee.2021.04.012. [DOI] [PubMed] [Google Scholar]
- White Allison K., Klemetson Chelsea J., Farmer Brooke, Katsavelis Dimitrios, Bagwell Jennifer J., Grindstaff Terry L. International Journal of Sports Physical Therapy. 2. Vol. 13. International Journal of Sports Physical Therapy; COMPARISON OF CLINICAL FATIGUE PROTOCOLS TO DECREASE SINGLE-LEG FORWARD HOP PERFORMANCE IN HEALTHY INDIVIDUALS; pp. 143–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Test Re-Test Reliability of A Novel Single Leg Hop Test (T-Drill Hop Test) Negrete Rodney, Simms Samantha, Gross Jacob, Nunes Rabello Lucas, Hixon Matt, Zeini Ibrahim M., Jenkins Walter L., Davies George J. Jun 1;2021 International Journal of Sports Physical Therapy. 16(3):724–731,. doi: 10.26603/001c.23677. doi: 10.26603/001c.23677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- A Novel Test to Assess Change of Direction: Development, Reliability, and Rehabilitation Considerations. Worst H., Henderson N., DeCarreau R., Davies G.J. 2019IJSPT. 14(2):228–236. [PMC free article] [PubMed] [Google Scholar]
- A multi-center study of the test-retest reliability of the lower extremity functional test. Tabor Michael A., Davies George J., Kernozek Thomas W., Negrete Rodney J., Hudson Vincent. Aug;2002 Journal of Sport Rehabilitation. 11(3):190–201. doi: 10.1123/jsr.11.3.190. doi: 10.1123/jsr.11.3.190. [DOI] [Google Scholar]
- The evaluation of a new lower-body reaction time test. Spiteri Tania, Cochrane Jodie L., Nimphius Sophia, et al. Jan;2013 Journal of Strength and Conditioning Research. 27(1):174–180. doi: 10.1519/jsc.0b013e318250381f. doi: 10.1519/jsc.0b013e318250381f. [DOI] [PubMed] [Google Scholar]
- Neurocognitive challenged hops reduced functional performance relative to traditional hop testing. Simon Janet E., Millikan Nathan, Yom Jae, Grooms Dustin R. Jan;2020 Physical Therapy in Sport. 41:97–102. doi: 10.1016/j.ptsp.2019.12.002. doi: 10.1016/j.ptsp.2019.12.002. [DOI] [PubMed] [Google Scholar]
- The development of a new test of agility for rugby league. Serpell B.G., Ford M., Young W.B.., et al. 2010J Strength Cond Res. 24(12):3270–3277. doi: 10.1519/JSC.0b013e3181b60430. [DOI] [PubMed] [Google Scholar]