Context:
Childhood lead poisoning prevention in the United States was marked by a largely failed medical approach from 1971 to 1990; an emergent (but small) healthy housing primary prevention strategy from 1991 to 2015; and implementation of large-scale proven interventions since then.
Program:
Childhood Lead Poisoning Prevention & Healthy Housing.
Methods:
Historic and recent health and housing data from the National Health and Nutrition Examination Survey (NHANES) and the American Healthy Homes Survey (AHHS) were retrieved to analyze trends and associated policy gaps.
Evaluation:
Approximately 590 000 US children aged 1 through 5 years had elevated blood lead levels of 3.5 μg/dL and greater in 2016, and 4.3 million children resided in homes with lead paint in 2019. Despite large improvements, racial and other disparities remain stubbornly and statistically significant. The NHANES and the AHHS require larger sample sizes. The Centers for Disease Control and Prevention has not published children's blood lead surveillance and NHANES data in several years; the Department of Housing and Urban Development (HUD) has no analogous housing surveillance system; and the Environmental Protection Agency (EPA) and the Occupational Safety and Health Administration (OSHA) have not updated training, Superfund, and occupational standards in decades.
Discussion:
The nation has been without a plan and an associated budget for more than 2 decades. Congress has not reformed the nation's main lead poisoning prevention laws in more than 30 years. Such reforms include stopping US companies from producing new residential lead paint in other countries; enabling the disclosure law to identify all residential lead hazards; closing loopholes in federally assisted housing regulations and mortgage insurance standards; harnessing tax policy to help homeowners mitigate lead hazards; streamlining training requirements; increasing the size of health and housing surveys and surveillance systems; and updating housing codes, medical guidance, dust lead standards, training, Superfund, and worker exposure limits. Congress and the president should reauthorize a cabinet-level task force (dormant since 2010) to develop a new strategic plan with an interagency budget to implement it. These reforms will scale and optimize markets, subsidies, enforcement, and other proven interventions to end ineffective, costly, harmful, and irrational cost shifting that threatens children, workers, and affordable housing.
Keywords: disparities, housing, lead poisoning
Introduction
Three eras
This article identifies historic trends to inform how antiquated federal laws can be modernized to implement proven interventions at the needed scale. The past 50 years were marked by 3 distinct phases in US childhood lead poisoning prevention: a medical approach from 1971 to 1991; an emergent integrated housing and health primary prevention approach from 1992 to 2015; and since then, attempts to bring proven interventions to scale and address other housing-related health problems. Each approach had limitations, explaining why childhood lead poisoning and other hazards in homes continue to threaten millions of children annually.
1970-1991
Congress enacted the Lead Based Paint Poisoning Prevention Act in 1971,1 following decades when lead and other industries put lead into food canning,2 gasoline,3 paint,4 water pipes,5 and many other consumer and commercial products. Because it was regarded initially as a health problem, widespread blood lead screening programs began in this era but were limited to identifying children following exposure, not to prevent it. Response to poisoned children was often delayed or nonexistent and, in most cases, did not identify and safely remediate lead hazards in the children's homes.6
Population-wide representative blood lead surveys from the National Health and Nutrition Examination Survey (NHANES) first appeared in the middle to late 1970s.7 Corrective measures were largely limited to bans on new residential lead paint (1978) and lead drinking water pipes (1987); retooling food-canning factories and refineries to eliminate lead solder and lead gasoline, respectively (1985); industrial emission controls (1973); and regulation of occupational lead exposure for industrial (1978) and construction (1996) workers. Public health guidance from the Surgeon General in 1971 relied on observation of clinical symptoms, recommending intervention at blood lead levels of 60 to 80 μg/dL8 (a fatal dose is generally on the order of 100-150 μg/dL in young children).
These early efforts reduced deaths but exposures remained widespread. Virtually no action was taken in the housing profession and no federal funds were appropriated for residential remediation. As a result, both public and private housing with lead paint hazards were seldom repaired, poisoning millions of children. Court decisions, such as Ashton v Pierce in 1983, relied on the presence of lead paint, not exposure science, and early remediation typically used dangerous paint removal methods that are banned today; these methods often backfired and increased exposures instead of reducing them.9
By the mid-1980s, new pathway exposure studies emerged10 and a bombshell report to Congress in 1988 renewed public attention to the problem,11 despite attempts to bury it within the federal bureaucracy.12 As a result of the successful phaseouts of lead in gasoline, food canning, and banning production of new residential lead paint and new lead water pipes, some believed that the problem had been solved.
However, NHANES data during this time (see the “Results” section) demonstrated that high blood lead levels remained widespread. By 1990-1991, the Centers for Disease Control and Prevention (CDC), the Department of Housing and Urban Development (HUD), and the Environmental Protection Agency (EPA) each developed their own separate strategic and uncoordinated plans. Litigation escalated but was focused on landlords and their insurance companies and not the industries that had released their lead products into millions of homes. Although a few children won large awards, most received nothing and were never diagnosed or had their day in court. Confusion about how to safely remediate lead or measure it reliably was widespread. By 1991, the sole reliance on the clinical medical approach had clearly failed.
1992-2014
In 1992, Congress passed Title X of the Housing and Community Development Act,13 marking the first time the housing profession finally became involved following Congressional hearings that included parent's voices. It assigned clear duties to HUD, EPA, and CDC, and authorized the first federal funding to remediate privately owned housing where risks were greatest. Most importantly, Title X redefined the meaning of a lead paint “hazard,” based on the exposure science that had appeared in the late 1980s. Science and informed citizens drove policy. Throughout the mid- to late-1990s, capacity to implement corrective measures and funding expanded but remained far too small to fully address the problem.
In 2000, the president's cabinet released a 10-year plan to eliminate lead poisoning as a major public health problem by 2010 with an associated budget,14 marking the first (and only) high-level federal plan. But it was never funded adequately by Congress. Although there was another plan released mainly by EPA in 2018, it explicitly stated that it was “not a budget document.”15
Significant political interference occurred at both HUD and CDC in 2004 and 2012, respectively.16 Funding for HUD's lead program declined in this time period and CDC lead funding was virtually eliminated in 2012 and 2013 (Figure 1). It would take a tragedy to refocus the nation's attention.
FIGURE 1.
Federal Funding for Lead Paint (2000-2022)a,b Abbreviations: CDC, Centers for Disease Control and Prevention; EPA, Environmental Protection Agency; HUD, Department of Housing and Urban Development. aThe CDC funding was virtually eliminated in 2012 and 2013. The HUD funding declined from 2004 to 2016. Both HUD and CDC funding increased since 2016. The EPA funding has remained relatively unchanged for its lead paint program appropriations; the EPA funding does not include Superfund, water, or research. bFrom National Safe and Healthy Housing Coalition. This figure is available in color online (www.JPHMP.com)
2014-2022
In 2014, the Flint lead water crisis first gained national attention, reawakening the nation to the continuing lead problem. The CDC surveillance programs had been defunded in 2012-2013, so the problem was noticed only after a local physician found a troubling trend in increased children's blood lead,17 and the public protested a decline in water quality.
The renewed interest in the lead problem resulted in large federal funding increases, beginning in 2017 (Figure 1). But challenges remained. For example, in a bipartisan infrastructure act passed in 2021, Congress provided billions for drinking water lead pipe replacement but ignored lead paint and other health hazards in housing.18
Methods
We acquired the NHANES data from the 1970s to 2016 and the American Healthy Homes Survey data (and its predecessors) from 1990 to 2021, focusing on child blood lead and housing trends and disparities by race and ethnicity and income. We also analyzed the main national laws on childhood lead poisoning.
Results
Racial and ethnic disparities and population trends in children's blood lead
There are approximately 590 000 young children with elevated blood lead levels today, using the CDC's definition of the blood lead reference value (the 97.5th percentile of the child population blood lead distribution) and the recent estimate of the number of children between 1 and 6 years of age (23.6 million19).
Figures 2A to 2D show trends in childhood blood lead levels over the past half century from NHANES. Figure 2A demonstrates that the difference in geometric mean blood lead levels between White and non-Hispanic Black children remained statistically significant in 2016 (the most recent published data), although the difference in the upper confidence intervals was small (about 0.2 μg/dL). In earlier years, NHANES showed that this difference was far greater (Figures 2B to 2D). Overall, groups showed continued improvements in reduced blood lead levels (the 2016 NHANES suggests that there may be some increases in blood lead levels ≥3.5 μg/dL).
FIGURE 2.
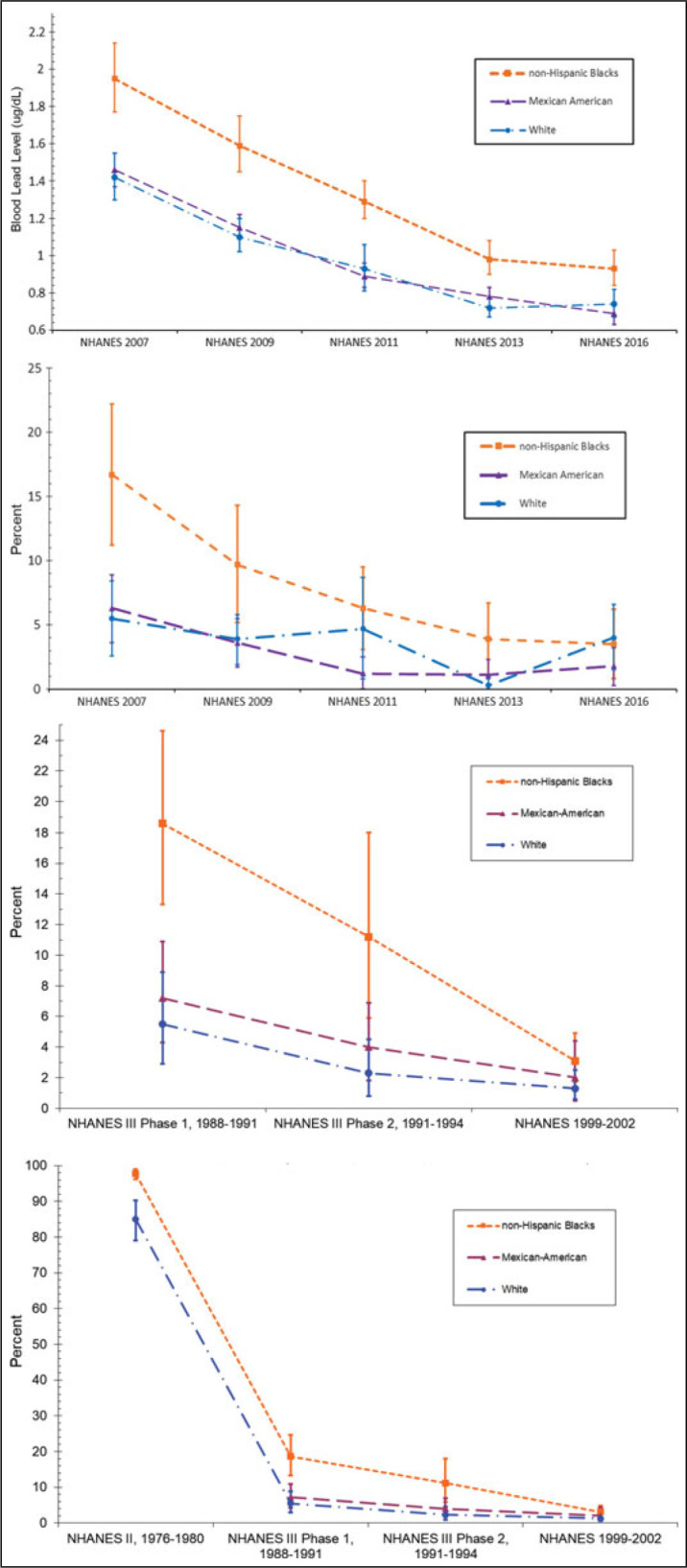
(A) Geometric Mean Blood Lead Levels in Children Aged 1 Through 5 Years, With 95% Confidence Intervals, US NHANES 2007-2016; (B) Percentage of Children Aged 1 Through 5 Years With Blood Lead Levels of 3.5 μg/dL and Greater, With 95% Confidence Intervals, US NHANES 2007-2016; (C) Percentage of US Children Aged 1 Through 5 Years With Blood Lead Levels of 10 μg/dL and Greater, With 95% Confidence Intervals, US NHANES 1988-2002; and (D) Percentage of US Children Aged 1 Through 5 Years With Blood Lead Levels of 10 μg/dL and Greater, With 95% Confidence Intervals, US NHANES 1976-2002a Abbreviation: NHANES, National Health and Nutrition Examination Survey. aFrom NHANES data and David Jacobs. This figure is available in color online (www.JPHMP.com)
Figures 2B to 2D show blood lead level trends using the CDC's different trigger levels at different time periods: the most recent reference value of 3.5 μg/dL and greater (adopted in 2021),20 5 μg/dL and greater (adopted in 2012),21 and the “level of concern” of 10 μg/dL and greater (adopted in 1991).22 In the 1970s, virtually all non-Hispanic Black children and more than 80% of White children had blood lead levels of 10 μg/dL and greater. In more recent years, the data show instability in estimates of 3.5 μg/dL and greater, particularly for White and Hispanic children, possibly because the survey size is too small and laboratory blood lead reporting limits may not be reliable.
From 1976-1980 to 2015-2016, the geometric mean blood lead level of the US population aged 1 to 74 years declined 93.6% from 12.8 to 0.82 μg/dL. In 2015-2016, 0.2% of children aged 1 to 5 years had blood lead levels of 10 μg/dL and greater, and 1.3% had 5 μg/dL and greater (these were the 2 blood lead trigger levels used in the 1990s and 2010s, respectively).23
These data demonstrate that blood lead levels improved greatly over the past 50 years, but significant racial and ethnic disparities and widespread exposures are still occurring.
Racial and ethnic disparities and population trends in housing lead paint hazards
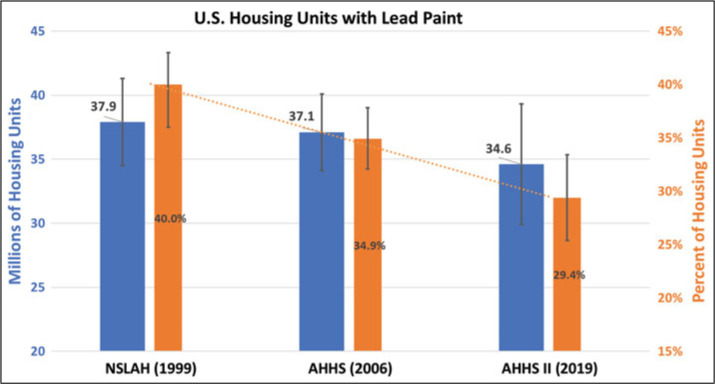
Four nationally representative housing lead paint surveys were completed by HUD in 1990,24 1999,25 2006,26 and 201927 (Figure 3). The 1990 survey showed 64 million homes with lead paint (not shown in the figures). A second survey a decade later estimated 38 million homes. From 1999 to 2019, the percentage of homes with lead paint declined from 40% to 29% (38-35 million housing units).
FIGURE 3.
Housing With Lead Paint With 95% Confidence Intervals, 1999-2019a Abbreviations: AHHS, American Healthy Homes Survey; NSLAH, National Survey of Lead and Allergens in Housing. aFrom US Department of Housing and Urban Development. Findings on lead-based paint/hazards from the American Healthy Homes Survey II, CDC Lead Exposure and Prevention Advisory Committee Meeting, May 14, 2021. This figure is available in color online (www.JPHMP.com)
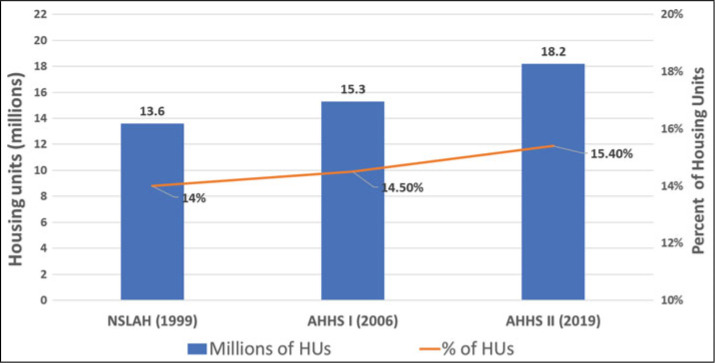
Yet, the number of homes with deteriorated lead paint increased by 4.6 million homes from 1999 to 2019 as the housing stock continued to age (Figure 4). The percentage of homes in poverty (annual income <$30 000 to $35 000) with lead paint declined from 40% to 33% between 2012 and 2019, but lower-income households still were significantly more likely to have lead paint. In short, lead paint deterioration is worsening, and disparities remain pronounced.
FIGURE 4.
Housing With Significantly Deteriorated Lead Paint, 1999-2019a Abbreviations: AHHS, American Healthy Homes Survey; HUs, housing units; NSLAH, National Survey of Lead and Allergens in Housing. aFrom US Department of Housing and Urban Development. Findings on lead-based paint/hazards from the American Healthy Homes Survey II, CDC Lead Exposure and Prevention Advisory Committee Meeting, May 14, 2021. This figure is available in color online (www.JPHMP.com)
Trends in lead paint disparities by race are more unclear. In the 1999 housing survey, 41% (±11%) of homes occupied by African American families had lead paint, compared with 40% (±4%) of homes occupied by White families (the 1990 survey did not report its findings by race). The 2006 survey found a larger disparity in homes with lead paint (45% ± 4% of African American homes and 32% ± 3% of homes with Whites), but the 2019 survey found that 25% (±7%) and 45% (±10%) of homes had lead paint for African American and White households, respectively. These inconsistent results are likely due to the small scale of the housing surveys (the 1999 survey; 2006; and 2019 surveys had only 831, 1131, and 703 housing units in them, respectively). Although these surveys were weighted to represent the 117-million-unit US housing stock, these small numbers likely account for the unstable estimates, as is the case for blood lead in the NHANES survey. Larger NHANES and AHHS surveys would likely identify disparities more clearly, but neither CDC nor HUD has articulated plans to do so.
The housing surveys used differing definitions of lead paint hazards in the form of deteriorated lead paint, lead-contaminated dust, and lead-contaminated bare soil, and are not reported here. However, blood lead is highly correlated with household-settled dust lead and bare soil lead,28 with both showing marked improvement. In 2019, the housing surveys showed that the arithmetic mean dust lead loading on floors nationwide improved by 73% (3.68 μg/ft2 compared with 13.6 μg/ft2 in 1999). On windowsills, mean dust lead levels improved by 72% (54 μg/ft2 compared with 195 μg/ft2 in 1999). The 2021 EPA and HUD lead dust standards for floors and windowsills were 10 and 100 μg/ft2, respectively.29 The housing surveys also showed that the number and percentage of homes with soil lead hazards decreased substantially from 2012 to 2019. The national mean residential bare soil lead level declined from 184 ppm in 2006 to 99 ppm in 2019, well below the current EPA/HUD limits of 1200 ppm for bare soil in nonplay areas, and 400 ppm in play areas.
Other sources
Lead remains a multimedia pollutant and can be a problem in drinking water, hobbies, food, small aircraft fuel emission, demolition, home remedies, consumer products, and other sources and pathways; they are reviewed elsewhere,30 and water lead exposures are described in Supplemental Digital Content 1, available at http://links.lww.com/JPHMP/B94. A new federal strategy (see the “Discussion” section) can also consider these other sources and how best to identify new and emerging sources regulated by the Food and Drug Administration (FDA), the Consumer Product Safety Commission (CPSC), the Occupational Safety and Health Administration (OSHA), and others.
Discussion and Conclusions
Both disparities and lead exposures remain widespread, despite long-term improvements. The data show that the problem is not confined to a few isolated “hot spots” such as Flint or a few inner city neighborhoods; indeed, 1 analysis showed that tens of thousands of jurisdictions have lead exposures worse than Flint.31 Another 2018 study showed that housing remains a core problem with deteriorating lead-based paint and lead dust as the main contributing environmental factor in about 90% of all childhood lead poisoning.32 New models using complex algorithms and mapping are useful for focusing attention on disparities in risk for exposure.33 However, given substantial evidence of widespread exposure, targeting interventions solely to identified “hot spots” will leave many children at risk.
The trends in blood lead and housing demonstrate that resources over decades have been well targeted, shown by improvements in disparities in both blood lead and housing conditions. But because those disparities remain and because elevated exposures still afflict nearly 600 000 children each year, federal laws require reform.
Our analysis suggests that Congress should focus on the following specific issues and laws, summarized in the bullets below and detailed in the later sections of this article:
There has been no cabinet-level federal interagency strategy with an interagency budget to eliminate childhood lead poisoning as a major public health problem since 2000 (new Title X section 1064).
Disclosure has been limited to “known” paint and/or hazards and most houses remain uninspected, meaning there is typically nothing to disclose (Title X Section 1018).
Tenant-based Section 8 housing choice vouchers (HUD's largest housing program) do not require lead paint risk assessments (Title X Section 1012).
Single family housing mortgage insurance is the only federally assisted housing program that was never reformed to properly evaluate and remediate lead paint hazards (Title X Section 1012).
Eligibility requirements for HUD lead paint grants for privately owned housing are needlessly complex and narrow, with many low- and moderate-income families unable to obtain assistance (Title X Section 1011).
Although many have a successful track record in conducting lead hazard control work, nonprofit organizations are ineligible for HUD's lead hazard control grants (Title X Section 1011).
Training requirements require simplification because there is needless duplication among professionals and trades (Title X Section 1021).
US corporations are still permitted to produce new lead paint in other countries (Title X Section 1021, new Subsection 409).
Homeowners remain ineligible for lead abatement tax credits or other tax incentives, unlike landlords, a striking disparity (Title X new Section 1062).
The National Safe and Healthy Housing Standard has not been adopted for federally assisted housing (new Title X Section 1063).
EPA lead exposure standards do not have clear evaluation criteria (Title X Section 403).
CDC blood lead surveillance data and NHANES data have been collected but have not been released for several years (National Nutrition Monitoring and Related Research Act, Public Law 101-445).
CDC lead poisoning medical management guidelines and guidance to state and local lead poisoning prevention programs have not been updated for many years (Public Health Service Act, as amended through Public Law 117–159).
OSHA's Permissible Exposure Limit and its occupational health standard for lead have not been updated since 1978 (Title X Section 1031 and the Occupational Safety and Health Act).
EPA Superfund regarding lead needs updating (Comprehensive Environmental Response, Compensation, and Liability Act).
Local and state governments are already acting to bring such reforms to scale. But the reforms summarized previously will all require Congressional action. Without such action, the nation will continue to needlessly absorb approximately $80 billion annually in costs from childhood lead exposure that could be saved,34 as well as avoiding needless harm and suffering. The detailed analysis of the reforms that Congress should consider follows.
New federal lead poisoning strategy (new Title X Section 1064)
The nation has been without a long-term high-level federal strategy since the president's cabinet produced one in 2000. That 2000 strategy included an interagency budget and a forecast on what resources would be needed to conquer the problem. Congress or the president can require the HUD and HHS secretaries to convene cabinet-level officials and others to develop and implement a new strategy that addresses current understanding of children's lead exposure. This cabinet can also address current fragmented strategies at different agencies at different staff levels. This new strategy can examine drinking water and other sources and pathways of lead exposure. An executive order has been drafted and awaits the president's signature and Congress can authorize a new cabinet task force.35
Disclosure (Title X Section 1018)
Most homes remain uninspected for lead. The current law is limited to disclosure of “known lead paint and/or lead-based paint hazards,” which allows most sellers or landlords to simply check a “don't know” box on a form, denying buyers and renters the knowledge of whether lead paint hazards are present. This loophole means that parents usually do not have the information they need to protect their children because they do not know exactly where the lead is located in their homes, and landlords, property managers, and owners do not know where their maintenance and capital improvements should be focused. Requiring inspections/risk assessments at the time of lease or sale for older housing will enable corrective actions before children are exposed by identifying exactly where lead hazards are located. This would also permit the housing market to help finance lead remediation like any other home improvement, because the market cannot work correctly if hazards remain unknown.
Tenant-based Section 8 vouchers (Title X Section 1012)
Visual assessment of paint condition in HUD's Housing Choice Section 8 Voucher Program is currently required, but because lead paint is not visible to the naked eye, lead paint hazards are not identified. Lead inspections/risk assessments should be required in the Section 8 program, as is currently the case in public housing, project-based Section 8 housing, and most other housing programs. Title X in 1992 did not explicitly include provisions for tenant-based Section 8, which is HUD's largest private housing rental assistance program. This new policy requires HUD to implement lead paint risk assessments under the authority of the 1937 Housing Act, which provides for “decent, safe and sanitary housing.”36
Single family mortgage insurance (Title X Section 1012)
The only HUD program not to be updated in 1999,37 the federal Single Family Mortgage Insurance program retains antiquated and hazardous requirements (limited repainting and rudimentary sweeping), unlike the multifamily federal mortgage insurance program. The new policy requires Fannie Mae, Freddie Mac, and the Federal Housing Administration to all include lead paint risk assessment and remediation in their underwriting standards for single-family mortgage insurance and become consistent with other federally assisted housing lead paint requirements. Because it is backed by the federal government, mortgage insurance is a subsidy that uses taxpayer dollars. It makes little sense to require protection for children in multifamily-insured homes but to ignore single-family insured ones.
Eligibility requirements for grants (Title X Section 1011a)
Currently, Title X requires needlessly complicated requirements for HUD lead paint grants, with certain percentages of housing to be at certain low-income limits, and other restrictions on the percentage of units occupied by children depending on building size. Together, these make implementation of the grants needlessly difficult. Congress can define a family as low-income if it is eligible for similar low-income programs, such as CDBG, HOME, DOE weatherization assistance, LIHEAP, Medicaid, CHIP, SNAP, or similar program. The reform also increases the allowable income limit to 120% of the area median income, because moderate-income families also often cannot afford lead remediation without assistance.
Grantee definition (Title X Section 1011b)
Title X limits eligibility for HUD's main lead paint hazard grants to a state or unit of local government. This means that nonprofit organizations are not eligible to apply. In the years since Title X was passed, many nonprofit organizations have built capacity to conduct lead hazard control assessment and remediation in Cleveland, Rhode Island, Maryland, and other localities38 with local government, philanthropic, or other funding. This reform will enable nonprofits as well as state or other units of local government to be eligible, which will enable remediation to proceed more quickly.
Training requirements (Title X Section 1021)
Title X currently requires 2 needlessly complicated sets of training requirements: one for a very small highly trained inspection and remediation workforce and another for a much larger but less-trained workforce engaged in typical painting or renovation work. There are now potentially 7 different disciplines with differing and needlessly bewildering training requirements: lead inspectors, lead risk assessors, sampling technicians, project designers, abatement supervisors, abatement workers and renovation, and repair and painting contractors. A reformed Title X can consolidate training requirements to shorten them for abatement (now typically 5 days) and lengthen them for typical painting or renovation work (now typically 1 day), such that all trades that disturb lead paint in the course of their duties undergo a streamlined 2-day training course. The reform also requires clearance testing for renovation, repair and painting work regulated by EPA, which does not currently require such testing, unlike federally assisted housing undergoing rehabilitation, repair, or painting. Clearance testing ensures that homes are safe for children to occupy following repairs that disturb paint and create lead-contaminated dust.
New lead paint production (Title X Section 1021, Subsection 409 “Prohibited Acts”)
Evidence gathered by the World Health Organization, the United Nations Environment Program, community groups, and researchers shows that a small number of US corporations still produce lead paint that is used for residential purposes in other countries.39 In the United States, production of new lead paint for residential use has been banned since 1978. A reformed Title X can require that companies producing or selling any paint in the United States are prohibited from producing new lead paint in other countries. Substitutes for lead in paint have been available for decades and are available at comparable prices.40
Tax credit (new Title X Section 1062)
A lead hazard remediation tax credit for homeowners enables low- and moderate-income families to be treated the same as landlords. Current Internal Revenue Service regulations permit landlords to deduct lead assessment and remediation costs as a business expense but homeowners cannot. The lead paint tax credit will stimulate private sector investment in lead assessment and remediation and will incentivize compliance with the new lead disclosure inspection requirements.
Standards for healthy housing (new Title X Section 1063)
The National Safe and Healthy Housing Standard, a model code released by the National Center for Healthy Housing and the American Public Health Association in 2014,41 is the first to support specific healthy housing requirements. Currently, housing codes rely on scattered federal, state, and local housing codes or model codes that in general fail to consider lead or other healthy home issues.
EPA lead standards (Title X Section 403)
Title X required EPA to establish standards for lead in dust, soil, and other media to guide lead hazard assessment and remediation efforts. But it did not adequately define criteria to use in developing such standards and how frequently the agency should reevaluate the standards. This has created needless litigation and confusion. The new reform requires EPA to update its lead dust exposure standards every 5 years, the same as for outdoor air priority pollutants (one of which includes airborne outdoor lead). The reform also requires EPA to balance health protection (to ensure that the vast majority of children are protected) with measurement reliability, feasibility, and sustainability. The reform will also end current confusion over hazard standards and clearance standards by requiring them to be numerically identical.
Blood surveillance reporting (Lead Contamination Control Act of 1988 and National Nutrition Monitoring and Related Research Act, Public Law 101-445)
The CDC has not updated its blood lead surveillance reporting since 2018.42 The new policy requires the CDC to update its surveillance data annually and also requires states to report their data to the CDC. Surveillance helps ensure that resources are directed to areas of greatest need, that case management services are provided to exposed children, and that emerging threats are detected early. This amendment also requires HUD to establish an analogous housing surveillance system to ensure that the same house does not poison multiple children. The amendment requires that the CDC collect lead dust samples from homes of children who participate in NHANES, which lapsed in 2004. The NHANES data on childhood blood lead levels by race and ethnicity and by the current blood lead reference value must be released within 18 months of the survey (such detailed NHANES data have not been released since the 2015-2016 survey, with only a general summary table released with 2018 data).43
Occupational lead exposure (Title X Section 1031 and the OSHA Act)
OSHA established a lead permissible exposure limit (PEL) for industrial workers in 1978, but it did not establish such a limit for construction workers until Title X in 1992 required it. The current PEL of 50 μg/m3 (first established in 1978 and extended to construction workers in 1996) is clearly outdated. The OSHA recently announced a notice of proposed rulemaking to update its lead standard, a process likely to take many years. Congress can require OSHA to update its PEL to no more than 10 μg/m3 as an 8-hour time-weighted average and reform other parts of the occupational lead standard within 1 year.
Superfund (Comprehensive Environmental Response, Compensation, and Liability Act)
In 1980, Congress passed the Comprehensive Environmental Response, Compensation, and Liability Act (CERCLA), better known as Superfund. The Superfund program addresses short- and long-term risks of chemical spills and releases and supports the permanent cleanup and rehabilitation of hazardous waste sites. But the regulations at 40CFR 300.430 (f)(4)) attempt to implement the permanent solution, which may not be appropriate at many sites because this term implies that there is a final solution that can be clearly defined in advance of remediation.44 In addition, the existing superfund legislation does not allow the flexibility or resources to maintain the remediation strategies. Sites are often subject to the conflicting goals and rules of local, state, and federal jurisdictions, and the Superfund regulations ignore lead paint problems. Reform of Title X could support and inform a careful review of the Superfund Act pertaining to lead.
Conclusion
Lead exposures are widespread and still marked by disparities in both blood lead and housing. Although progress has been made, the nation's primary lead laws are now decades old. Congress can reform these laws to eliminate childhood lead poisoning as a major public health problem. These reforms will prevent lead poisoning and scale and optimize markets, subsidies, enforcement, and other interventions to end ineffective, costly, harmful, and irrational cost shifting that threatens children, workers, and affordable housing.
Implications for Policy & Practice
Racial, ethnic, and other disparities remain significant despite progress.
Childhood exposures to lead are widespread.
The nation's lead poisoning prevention laws have not been updated in decades and require reform.
Larger population surveys are needed to both target resources and evaluate population-wide exposure trends.
CDC has not released surveillance and NHANES blood lead data for race, ethnicity, and socioeconomic status at the current reference value in several years.
The overarching goal for the 21st century should be to bring every baby home to a lead safe environment.
Supplementary Material
Footnotes
Sherry Dixon helped tabulate NHANES data; Sarah Keeley helped create graphics; and Jonathan Wilson, Amanda Reddy, Sarah Goodwin, and Larry Brooks provided helpful comments on earlier drafts.
The views in this article are those of the authors and do not necessarily reflect those of the US government or the authors' employers.
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal's Web site (http://www.JPHMP.com).
Contributor Information
David E. Jacobs, Email: djacobs@nchh.org, dejacobsdc@gmail.com.
Mary Jean Brown, Email: mjb686@outlook.com.
References
- 1.Lead-Based Paint Poisoning Prevention Act. Pub L No. 91–695, §1, 84 Stat 2078 (January 13, 1971). https://www.govinfo.gov/content/pkg/STATUTE-84/pdf/STATUTE-84-Pg2078.pdf. Accessed October 18, 2022.
- 2.Farfel M. Reducing lead exposure in children. Ann Rev Public Health. 1985;6:333–360. [DOI] [PubMed] [Google Scholar]
- 3.Bridbord K, Hanson D. A personal perspective on the initial federal health-based regulation to remove lead from gasoline. Environ Health Perspect. 2009;117:1195–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Markowitz G, Rosner D. Deceit and Denial. 1st ed. Berkeley, CA: University of California Press; 2013. [Google Scholar]
- 5.Rabin R. The lead industry and lead water pipes: “a modest campaign.” Am J Public Health. 2008;98(9):1584–1592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chisolm JJ, Harrison HE. The exposure of children to lead. Pediatrics. 1956;18(6):943–958. [PubMed] [Google Scholar]
- 7.Mahaffey KR, Annest JR, Roberts J, Murphy RS. National estimates of blood lead levels, US 1976-1980. New Eng J Med. 1982;307(10):573–579. [DOI] [PubMed] [Google Scholar]
- 8.Steinfield JL. Medical aspects of childhood lead poisoning. HSMHA Health Rep. 1971;86(2):140–143. [PMC free article] [PubMed] [Google Scholar]
- 9.Farfel M, Chisolm J. Health and environmental outcomes of traditional and modified practices for abatement of residential lead-based paint. Am J Public Health. 1990;80(10):1240–1245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bornschein RL, Succop P, Kraft KM, Clark CS, Peace B, Hammond PB. Exterior surface dust lead, interior house dust lead and childhood lead exposure in an urban environment. In: Hemphill DD, ed. Trace Substances in Environmental Health, 20. Proceedings of University of Missouri's 20th Annual Conference, June 1986. Columbia, MO: EPA and University of Missouri; 1987:322–332. [Google Scholar]
- 11.Mushak P, Crocetti A. The Nature and Extent of Childhood Lead Poisoning: A Report to Congress. Atlanta, GA: Agency for Toxic Substances and Disease Registry. US Public Health Service; 1988. [Google Scholar]
- 12.Weisskopf M. Authors protest report on lead poisoning: researchers resign, call changes misleading. Washington Post. June 13, 1987. [Google Scholar]
- 13.Housing and Community Development Act of 1992. Title X. Pub L No. 102-550.
- 14.Jacobs DE, Matte TD, Moos L, Nilles B, Rodman J. President's task force on children's environmental health risks and safety risks. Eliminating Childhood Lead Poisoning: A Federal Strategy. Washington, DC; 2000. http://www.cdc.gov/nceh/lead/about/fedstrategy2000.pdf. Accessed October 18, 2022. [Google Scholar]
- 15.President's Task Force on Environmental Health Risks and Safety Risks to Children. Key federal programs to reduce childhood lead exposures and eliminate associated health Impacts. https://ptfcehs.niehs.nih.gov/sites/niehs-ptfceh/files/features/assets/files/key_federal_programs_to_reduce_childhood_lead_exposures_and_eliminate_associated_health_impactspresidents_508.pdf. Published 2016. Accessed October 18, 2022.
- 16.Jacobs DE. Fifty Years of Peeling Away the Lead Paint Problem: Protecting Our Children's Future with Healthy Housing. San Diego, CA: Elsevier; 2022. [Google Scholar]
- 17.Hanna-Attisha M, LaChance J, Sadler RC, Champney Schnepp A. Elevated blood lead levels in children associated with the Flint drinking water crisis: a spatial analysis of risk and public health response. Am J Public Health. 2016;106(2):283–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.H.R.3684—Infrastructure Investment and Jobs Act, signed into law by President Biden on Nov 15, 2021. https://www.congress.gov/bill/117th-congress/house-bill/3684/text. Accessed October 18, 2022.
- 19.The estimate of 590,000 children with elevated blood lead levels is calculated by 2.5% x 23.6 million = 590,000. The number of children in the United States in 2020, by age group is reported by Statistica. https://www.statista.com/statistics/457786/number-of-children-in-the-us-by-age/. Published 2022. Accessed October 18, 2022.
- 20.Ruckart PZ, Jones RL, Courtney JG, et al. Update of the blood lead reference value—United States, 2021. MMWR Morb Mortal Wkly Rep. 2021;70(43):1509–1512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Advisory Committee on Childhood Lead Poisoning Prevention, CDC. Low Level Lead Exposure Harms Children: A Renewed Call for Primary Prevention. Atlanta, GA: US Department of Health & Human Services, CDC; 2012. https://www.cdc.gov/nceh/lead/acclpp/final_document_030712.pdf. Accessed August 29, 2022. [Google Scholar]
- 22.Centers for Disease Control and Prevention. Preventing Lead Poisoning in Children. Washington, DC: Department of Health & Human Services; 1991. https://wonder.cdc.gov/wonder/prevguid/p0000029/p0000029.asp#head001000000000000. Accessed August 29, 2022. [Google Scholar]
- 23.Dignam T, Kaufmann RB, LeStourgeon L, Brown MJ. Control of lead sources in the United States, 1970-2017: public health progress and current challenges to eliminating lead exposure. J Public Health Manag Pract. 2019;25(1 suppl):S13–S22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Department of Housing and Urban Development. Comprehensive and workable plan for the abatement of lead-based paint privately owned housing. https://www.huduser.gov/portal/publications/affhsg/comp_work_plan_1990.html. Published 1990. Accessed October 18, 2022.
- 25.Jacobs DE, Clickner RL, Zhou JL, et al. The prevalence of lead-based paint hazards in U.S. housing. Environ Health Perspect. 2002;110:A599–A606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.US Department of Housing and Urban Development. American Healthy Housing Survey. Lead and arsenic findings. https://www.hud.gov/sites/documents/AHHS_REPORT.PDF. Published 2012. Accessed October 18, 2022.
- 27.US Department of Housing and Urban Development. American Healthy Housing Survey II. https://www.hud.gov/program_offices/healthy_homes/ahhs_ii. Published 2021. Accessed October 18, 2022.
- 28.Wilson J, Dixon S, Wisinski C, et al. Pathways and sources of lead exposure: Michigan Children's Lead Determination (the Mi Child Study). Env Res. 2022;215(pt 2):114204. [DOI] [PubMed] [Google Scholar]
- 29.US Environmental Protection Agency. Hazard standards and clearance levels for lead in paint, dust and soil. Effective date: March 8, 2021. 40 CFR part 745.
- 30.Agency for Toxic Substances and Disease Registry. Toxicological profile for lead. https://www.atsdr.cdc.gov/toxprofiles/tp13.pdf. Published August 2020. Accessed October 18, 2022. [PubMed]
- 31.Pell MB, Schneyer J. Off the charts: the thousands of U.S. locales where lead poisoning is worse than in Flint. Reuters. 2016. https://www.reuters.com/investigates/special-report/usa-lead-testing/#:∼:text=In%20all%2C%20Reuters%20found%20nearly,at%20least%20four%20times%20higher. Accessed October 18, 2022. [Google Scholar]
- 32.Kent County. Lead task force ending child lead exposure in Kent County. https://www.accesskent.com/Health/Lead/pdf/2018_Report.pdf. Published January 2018. Accessed October 18, 2022.
- 33.Xue J, Zartarian V, Tornero-Velez R, et al. A generalizable evaluated approach, applying advanced geospatial statistical methods, to identify high lead exposure locations at census tract scale: Michigan case study. Environ Health Perspect. 2022;130(7):77004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pew Charitable Trusts and Robert Wood Johnson Foundation. 10 policies to prevent and respond to childhood lead exposure. https://nchh.org/resource-library/hip_10-policies-to-prevent-and-respond-to-childhood_lead_exposure_english.pdf. Published August 2017. Accessed October 18, 2022.
- 35.National Center for Healthy Housing and Day One Project. Draft executive order. Ensuring healthy homes: eliminating lead and other housing hazards. https://uploads.dayoneproject.org/2022/03/03155514/Executive-Order-Lead-and-Healthy-Homes-1.18.22-update.pdf. Published 2021. Accessed August 29, 2022.
- 36.US Housing Act Of 1937, As Amended. 42 USC §1437.
- 37.Requirements for Notification, Evaluation and Reduction of Lead-Based Paint Hazards in Federally Owned Residential Property and Housing Receiving Federal Assistance (“Lead Safe Housing Rule”) 24 Code of Federal Regulations, Part 35, Subpart E (reserved), 1999. [PubMed]
- 38.National Center for Healthy Housing. Lead poisoning prevention stories case studies. https://nchh.org/who-we-are/nchh-publications/case-studies/lpp-stories-case-studies/. Published 2017. Accessed October 18, 2022.
- 39.United Nations Environment Program and World Health Organization. Global alliance to end lead paint. https://www.unep.org/explore-topics/chemicals-waste/what-we-do/emerging-issues/global-alliance-eliminate-lead-paint. Published March 2022.
- 40.United Nations Environment Programme. Lead Paint Reformulation Technical Guidelines. Geneva, Switzerland: United Nations Environment Programme; 2022. https://www.unep.org/resources/toolkits-manuals-and-guides/lead-paint-reformulation-technical-guidelines. Accessed October 18, 2022. [Google Scholar]
- 41.National Center for Healthy Housing. National healthy housing standard. https://nchh.org/tools-and-data/housing-code-tools/national-healthy-housing-standard/. Published 2014. Updated 2018. Accessed October 18, 2022.
- 42.Centers for Disease Control and Prevention. Blood lead levels (μg/dL) among U.S. children < 72 months of age, by state, year, and blood lead level (BLL) group. https://www.cdc.gov/nceh/lead/docs/cbls-national-data-table-508.pdf. Published 2018. Accessed October 18, 2022.
- 43.National Report on Human Exposure to Environmental Chemicals. Centers for Disease Control and Prevention. Biomonitoring Data Tables for Environmental Chemicals. https://www.cdc.gov/exposurereport/data_tables.html#print. Published September 26, 2022. Accessed October 18, 2022.
- 44.Moore JN, Luoma SN. Hazardous wastes from large-scale metal extraction. A case study. Environ Sci Technol. 1990;24(9):1278–1285. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.