A proactive employer-sponsored mental health program facilitated linkage to mental health services and prescription medications among participants who connected with a care concierge.
Keywords: emotional health, employee, employer, well-being, behavioral health, health program
Objective
The aim of this study is to determine if a proactive employer-sponsored mental health program closed gaps in detection and treatment of mental health conditions.
Methods
Of n = 56,442 eligible, n = 8170 (14.5%) participated in the optional screening. Participants with mental health risk were offered care concierge services including support, care planning, and connection to care. Difference in behavioral health care utilization, diagnoses, and prescriptions were evaluated postintervention through claims analysis.
Results
Compared with controls (n = 2433), those receiving concierge services (n = 369) were more likely to fill mental health prescriptions (adjusted hazards ratio [HR], 1.2; 1.0–1.5; P = 0.042), use professional mental health services (adjusted HR, 1.4; 1.1–1.8; P = 0.02), and use new mental health services (adjusted HR, 1.9; 1.2–2.8; P = 0.004) in the following 6 months.
Conclusions
This proactive mental health program with care concierge services identified risk, connected individuals to mental health care, and facilitated mental health treatment, among program participants.
Mental health conditions are prevalent, undetected,1 and undertreated,2 especially after stressful life events.1 The proportion of individuals with mental disorders who go untreated exceeds 50% for many conditions.2,3 Several barriers to mental health diagnosis and treatment exist.4,5 Underdetection and undertreatment often result from barriers in access to and utilization of mental health care.1,4 Almost half of those with mental health conditions report not obtaining behavioral health treatment because of access challenges, such as not knowing where to go for care.4 Access challenges may disproportionately impact low-income adults, who may work hourly wage jobs with inability to get time off from work for treatment.4 Access to mental health providers is also impacted by geography,5,6 in that the number of providers per capita in rural areas is half that in metropolitan areas throughout the United States.5 Denial of care, when mental health providers refuse new patients or to fail to accept their insurance, represents an addition barrier.6 Moreover, shortages in practicing psychiatrists in the United States are expected to reach between 14,280 and 31,091 by 2024, leading to further challenges in access.7
Untreated mental health conditions not only present a societal burden, but also present a major challenge for employers. Depression alone in employees accounts for up to 37% lost productivity, even when excluding short- and long-term disability.8,9 Most (81%) lost productivity is attributed to reduced performance while at work10; workers with depression report significantly more total health-related lost productivity time than those without depression (5.6 hours/wk vs 1.5 hours/wk, respectively).10 Without treatment, depression impedes on-the-job performance (absenteeism, decreased productivity, interpersonal problems).11
Depression, whether or not diagnosed, is associated with other physical health conditions4 and substantial health care costs.12 Yet, although individuals with “psychological distress” and those with diagnosed depression cost the health care system a similar amount on a per-capita basis,12 only 4% of the costs incurred by those with psychological distress are associated with mental health-related health services, compared with 14% among individuals with diagnosed depression.12 This suggests that individuals with psychological distress may not be identified or treated for their mental health conditions.12 In addition, individuals suffering from psychological distress may seek help for their unexplained physical symptoms, but their conditions may not be diagnosed or treated as mental health conditions.12 These findings support the need to proactively outreach to populations and encourage preventive mental health screenings that include risk of psychological distress due to stressful life events.
Workplace mental health has become an increasing priority for large employers. In 2018, an advisory council on mental health in the workplace published recommendations and a call to action to improve health and well-being of workers.13 Since that time, mental health of workers has escalated to a top priority by employers, especially for prevention and early intervention.14 Improving mental health care of workers has benefits for both clinical and workplace outcomes.15 Mental health treatments are effective in improving a person’s work performance11,16 and can lessen the burden of anxiety and/or depression in the workplace.17 For employers, identifying and connecting employees with mental health conditions to care can improve work performance,16 productivity,15 and retention of employees,15 and reduce duration of leaves.18 Early mental health treatment has been shown to be clinically beneficial and cost-effective in a health system setting.19 The costs of acute care for untreated behavioral health conditions often exceeds the costs of ongoing treatment.4 Thus, the identification and early treatment of mental health risk and conditions remain gaps in health care that also present a workplace problem.
Little evidence exists on the effectiveness of mental health interventions in the workplace on mental health treatment outcomes. Evaluation of mental health outcomes is necessary for identifying evidence-based approaches to mental health care that can be implemented by employers.20 Proactive mental health services that provide support may manage the negative consequences of the pandemic, with broader impact on improving mental health service.21
We previously reported22 early findings that implementation of a proactive, voluntary, population-level mental health screening program in an employer-sponsored setting identified individuals at risk for mental health conditions, including those with no history of treatment, and connected these individuals with care via a mental health care concierge.22 Whether mental health care concierge services facilitated the receipt of mental health treatments was unknown at the time. Here, we extended the analysis to a workforce population of more than 8000 employees and spouses/domestic partners, utilizing health care claims data to evaluate health care treatment and utilization after the intervention.
METHODS
Study Design
Mental health care utilization was evaluated through retrospective analysis of anonymized data after program participation in a workplace setting. This analysis was conducted according to the HIPAA Privacy Rule (Title 45 Code of Federal Regulations, Section 164.514e), which governs research conducted by Covered Healthcare Entities and allows retrospective analysis using a limited data set without requiring approval by an institutional review board.
Study Population
All active employees and spouses/domestic partners of a national health services company were invited to participate in a mental health and wellbeing program from September to December 2019. The program was communicated through employee communications channels including e-mail, print, word of mouth, and web-based access via the benefits portal. No prizes or incentives were used in the program. The program comprised a risk acuity survey and a follow up consultation that included a plan connecting the individual to care. Individuals categorized as having moderate, high, or severe risk were invited to participate in a follow-up 1:1 care concierge consultation. Individuals who completed the consultation and received a care plan (Mental Health Concierge Services Group) were compared with those who did not accept the invitation to the mental health care concierge services (Control Group). Administrative claims data, used to measure health care utilization results for each participant, were evaluated during the study period, which included the 12-month period immediately before the start date and the 2- to 6-month follow-up periods from the survey date (start date) to February 28, 2020 (end date). The follow-up period was deliberately set to end before the impact of the COVID-19 pandemic (March of 2020). Individuals with incomplete medical coverage during the study period were excluded from the analysis (n = 1413). Of those excluded from the analysis (n = 1413) based on incomplete medical claims, 25% (n = 359) were employees or spouses/domestic partners not enrolled in the employer-sponsored medical plan, and 75% had incomplete coverage in the 12 months prior (n = 659), in the study follow-up period (n = 272), or in both prior and follow-up periods (n = 123).
Mental Health and Wellbeing Program
The Balance mental health and wellbeing program was created by Johns Hopkins Medicine with the goal of raising mental health awareness and lowering the barriers to mental health care for those in need. Mental health screening was done with the Emvitals screening tool—a 48-item web-based questionnaire used to evaluate risk or emerging risk for depression, anxiety, traumatic stress, alcohol or other illicit substance use, sleep disturbance, financial stress, and low social support. Questions in the tool were based on validated instruments and published risk thresholds, including the Patient Health Questionnaire-8 (PHQ-8),23 General Anxiety Disorder-7 (GAD-7),24 abbreviated posttraumatic stress disorder (PTSD) Checklist–Civilian Version,25 and Alcohol Use Disorders Identification Test–Concise.26 Upon completing the assessment, participants immediately viewed a summary report of their results. Participant results emphasize an individual’s areas of most need. The detailed report gives the participant an overview of each aspect of their emotional health: mental health, well-being, and health and health behaviors are scored and summarized based on the participants responses.
Mental health care concierge services, provided by Guide+Thrive by BHS, were offered to participants with moderate or higher risk in one or more categories. Individuals who engaged with the care concierge were able to discuss areas revealed in the screening tool and/or priorities identified by the participant as most important. Care concierges (masters-level trained mental health clinicians) reviewed screening results on mental health risk and symptoms acuity, provided support, developed individualized mental health care plans, and made referrals to mental health care programs and services. Referrals were based on health plan coverage and included mental health care providers, employee assistance program services, emotional well-being services, financial support, and other employee health programs. Health plan benefits included Preferred Provider Organization and Exclusive Provider Organization plans, which had copayments, deductibles and coinsurance for behavioral services. Employee assistance program included six sessions per person per issue per year. Concierges remained involved until the participant successfully connected to needed care and, if applicable, confirmed satisfaction with the identified provider. Oversight of the Care concierge team was provided by members of the Johns Hopkins Medicine Department of Psychiatry. Extended mental health care programs, services, and resources were provided by the employer-sponsored health benefits.
Study Outcomes
The main outcome of interest was utilization of health care resources during a follow up period of 2 to 6 months after the invitation to participate in a follow-up 1:1 mental health care concierge consultation. Health care utilization, including pharmacy and professional services (outpatient and inpatient), was assessed through analysis of administrative claims classified into Major Practice Categories 04 (psychiatry) and 05 (chemical dependency), a high level categorization of Symmetry Episode Treatment Groups.27 Professional services represent the professional component of a given claim, whereas outpatient reflect the facility component of the claim. Supplementary Tables 1, http://links.lww.com/JOM/B203, and 2, http://links.lww.com/JOM/B204, provide a list of mental health professional services, and mental health medications, including Major Practice Category and Episode Treatment Group classifications.
The association between mental health risk and incident claims were evaluated in n = 2783 participants who answered anxiety-related and depression-related questions in the screening and had complete medical claims data over the study period. Risk level was calculated as the sum of scores in the GAD (range, 0–20) and PHQ items (range, 0–24) and analyzed as a continuous variable. Hazard ratios (HRs) were calculated to show likelihood of incurring a future professional or prescription claim for each one-unit change in score.
Statistical Analysis
Student t tests and chi-squared tests were used to assess difference in clinical characteristics between the groups. The relationship between the effect of intervention and mental health care claim was assessed using Cox proportional hazards regression. Time to first mental health care claim was the outcome of interest in these Cox models. New mental health prescriptions included claims in the follow-up period but no claims in the 1-year prior. The proportional hazards assumption was checked by including a time-dependent covariate representing the interaction between intervention and follow-up time. A nonsignificant P value for this covariate (P > 0.50) was taken as evidence that the proportional hazards assumption had been satisfied. To avoid overfitting, only variables significantly associated with mental health concierge service status in the univariate analysis were included (P < 0.05) in multivariable models. Follow-up time was entered as a continuous variable in the Cox models. Other control variables were entered according to the categories noted herein. Cox proportional hazard models that adjusted for mental health risk (moderate, high, severe), age, education, smoking, prior mental health claims, and follow-up time were used to estimate the effect of intervention based on the time to a first mental health care claim during follow-up.
Kaplan-Meier curve analysis was performed to estimate cumulative incidence of mental health claims during the follow-up. Significance between groups was evaluated using the log-rank test. Analyses were performed using SAS version 9.4.
RESULTS
All employees and spouses (n = 56,442) were invited to participate in the mental health assessment in 2019 (Fig. 1). Of those n = 8170 (14.5%) invitees who completed the assessment, n = 4215 (51.6%) scored at moderate, high or severe, risk in the assessment. Of those with risk (n = 4215), 541 completed a mental health care concierge visit in 2019 (representing 12.8% of those who screened with risk), of whom 369 (68.2%) were enrolled in an employer-sponsored health plan and had deidentified behavioral health utilization data available for the study period. Of the 369 who met with a care concierge and had claims data available, 94.6% (n = 349/369) were provided with a recommendation, and 43.6% (n = 152/349) had one or more mental health claims (outpatient, Rx, professional) during follow-up period. Of 3674 participants with moderate or higher risk who did not meet with the care concierge, 2433 had deidentified behavioral health utilization data available over the study period and were included in the analysis. Employees represented 95% of individuals in both the mental health care concierge group and control group (Table 1).
FIGURE 1.
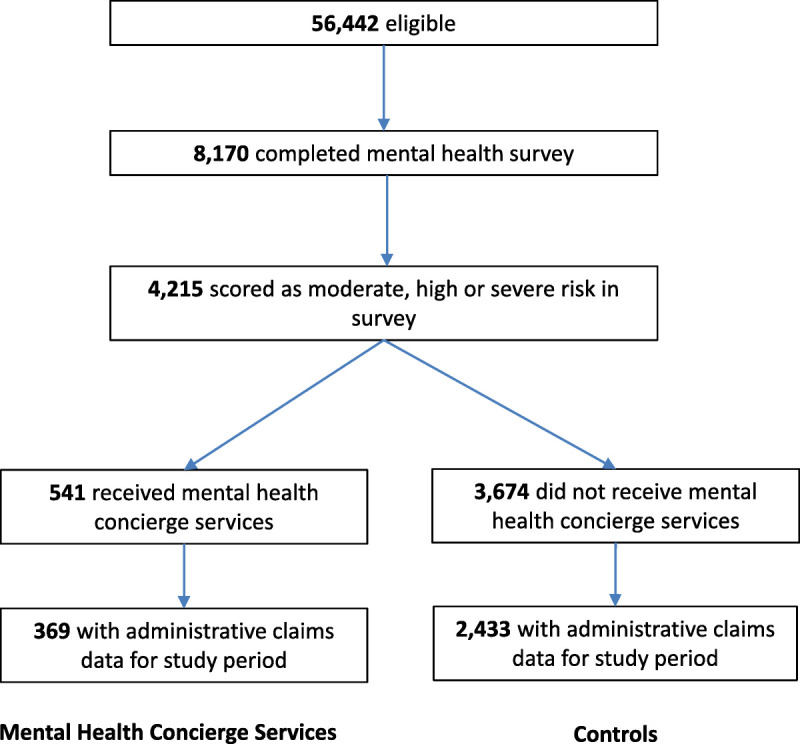
Participant flowchart.
TABLE 1.
Baseline Characteristics of Participants
| Characteristics | Metal Health Concierge Services (n = 369) | Control (n = 2433) | P |
|---|---|---|---|
| Number (SD) | |||
| Age | 45.5 (12.0) | 45.2 (11.0) | 0.63 |
| Follow-up days | 127 (32) | 143 (26) | <0.001 |
| Count (%) | |||
| Sex | |||
| Male | 76 (21) | 538 (22) | |
| Female | 293 (79) | 1895 (78) | 0.51 |
| Relationship | |||
| Spouse | 20 (5) | 131 (5) | |
| Employee | 349 (95) | 2302 (95) | 0.98 |
| Active Smoker | |||
| Yes | 47 (13) | 427 (19) | |
| No | 305 (87) | 1874 (81) | 0.02 |
| Race Ethnicity | |||
| Asian | 19 (5) | 158 (6) | |
| Black | 58 (16) | 478 (20) | |
| Other | 96 (26) | 671 (28) | |
| White | 196 (53) | 1126 (46) | 0.07 |
| Mental health risk | |||
| Moderate | 164 (44) | 1520 (62) | |
| High | 133 (36) | 561 (23) | |
| Severe | 72 (20) | 352 (15) | <0.001 |
| Prior mental health Rx | |||
| Yes | 149 (40) | 854 (35) | |
| No | 220 (60) | 1579 (65) | 0.049 |
| Education (college) | |||
| No | 20 (6) | 213 (10) | |
| Yes | 322 (94) | 2016 (90) | 0.03 |
| No. life events | |||
| 0 | 146 (39.6) | 1036 (42.6) | 0.24 |
| 1 | 127 (34.4) | 833 (34.2) | |
| 2 | 67 (18.2) | 394 (16.2) | |
| 3 | 26 (7.0) | 140 (5.8) | |
| 4+ | 3 (0.8) | 30 (1.2) |
Data presented as mean ± standard deviation for age and follow-up days and as a number (%) of participants for other variables.
At baseline, participants receiving mental health care services were less likely to currently use tobacco (13% vs 19%, P = 0.02), more likely to have had a prior mental health prescription (40% vs 35%, P = 0.049), more likely to have a college education (94% vs 90%, P = 0.03), and more likely to have severe mental health risk (20% vs 15%, P < 0.001)(Table 1).
The proportion of participants experiencing at least one stressful life event (eg, loss of a loved one, loss of a job, divorce or separation, birth of a child) in the past year was similar among care concierge participants (60.4%) and nonparticipants (57.4%; P = 0.24) (Table 1). Baseline rates of combined treatments (medication and professional or outpatient treatment) were similar between the groups (Table 1).
In the 6 months after program initiation (ie, invitation for concierge consultation), the cumulative incidence of mental health prescription medications was higher in participants, most notably in within the first 100 days of follow-up (P = 0.001) (Fig. 2). In both the unadjusted model (HR, 1.3; 1.1–1.6; P = 0.003) and models adjusted for mental health risk, prior mental health-related prescriptions, smoking, education, and follow-up days (HR, 1.2; 1.0–1.5; P = 0.042), individuals who completed a consultation with a care concierge were more likely to have an incident prescription for a mental health medication during the follow-up period); for the HR for new mental health prescriptions did not differ significantly between groups (HR, 1.4; 0.9–2.5; P = 0.17) (Table 2). Among mental health concierge participants, 36.6% (n = 135/369) had an event (relevant pharmacy claim) versus 30.5% (n = 742/2433) in the control group.
FIGURE 2.
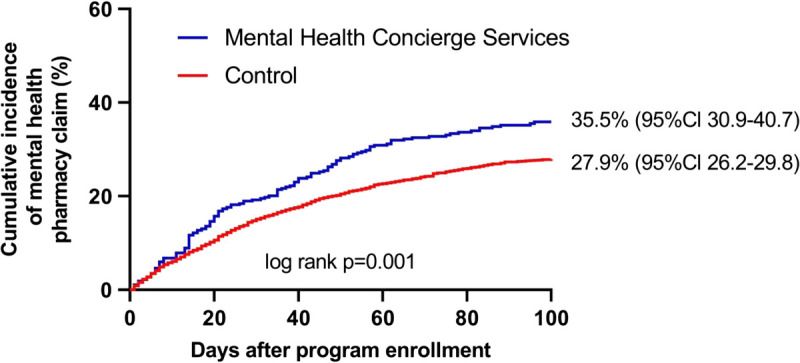
Cumulative incidence of mental health prescriptions.
TABLE 2.
Association of Mental Health Concierge Services With Medication, Professional Services, and Outpatient Services
| Model 1 | P | Model 2 | ||
|---|---|---|---|---|
| Endpoint | HR (95% CI) | HR (95% CI) | P | |
| Mental Health Medication | 1.3 (1.1–1.6) | 0.003 | 1.2 (1.0–1.5) | 0.042 |
| New Mental Health Medication(s) | 1.5 (0.9–2.5) | 0.12 | 1.4 (0.9–2.5) | 0.17 |
| Mental Health Professional Services | 1.4 (1.1–1.8) | 0.002 | 1.4 (1.1–1.8) | 0.02 |
| New Mental Health Professional Services | 1.9 (1.3–2.9) | 0.001 | 1.9 (1.2–2.9) | 0.004 |
| Mental Health Outpatient Services | 1.3 (0.8–2.2) | 0.35 | 1.1 (0.6–2.0) | 0.73 |
| New Mental Health Outpatient Services | 1.5 (0.8–3.0) | 0.19 | 1.7 (0.9–3.4) | 0.13 |
Model 1, unadjusted. Model 2, adjusted for, smoking, mental health risk, education, follow up days and prior mental health medication, or prior professional service claims, or prior outpatient service claims
CI, confidence interval; HR, hazard ratio.
In both the unadjusted model (HR, 1.4; 1.1–1.8; P = 0.002) and the adjusted models (HR, 1.4; 1.1–1.8; P = 0.02) (adjusted for mental health risk, prior mental health-related professional services, smoking, education, and follow-up days), individuals who competed a consultation with a care concierge were more likely to use mental health professional services during the follow-up period) (Fig. 3). Subgroup analysis revealed increased cumulative incidence of mental health professional service use within the follow-up period in the moderate (HR, 1.6; 1.0–2.4; P = 0.03) and severe risk groups (HR, 1.8; 1.1–3.1; P = 0.02). Among mental health concierge participants, 23.6% (n = 87/369) had an event (relevant professional services claim) versus 18.2% (n = 442/2433) in the control group. Rates of combined treatments (medication and professional or medication and outpatient) were similar between the mental health concierge services group and the control group. For medication and professional services, rates were similar in care concierge participants and nonparticipants (45.9% vs 46.5%, P = 0.90) and for medication and outpatient services (8.9% vs 8.1%, P = 0.75).
FIGURE 3.
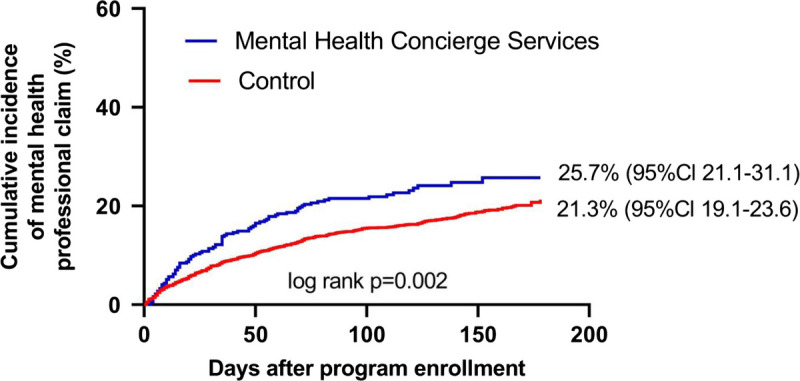
Cumulative incidence of mental health professional services.
The incidence of new professional service visits also increased in individuals receiving mental health concierge services relative to controls (Table 2). Among participants who had not used a professional service in the year preceding intervention, a higher incidence (first visit per person) of professional service visits was observed in the mental health concierge services group (HR, 1.9; 1.2–2.9; P = 0.004).
Scores on the GAD and PHQ instruments were associated with prescription use (as assessed by pharmacy claims) and professional visits. Higher levels of anxiety (as measured in the GAD instrument) were associated with a higher incidence of pharmacy claims (HR, 1.1; P < 0.0001). Higher levels of depression (as measured in the PHQ instrument) were associated with a higher incidence of pharmacy claims (HR, 1.1; P < 0.0001). Similarly, higher levels of anxiety and depression were associated with a higher incidence of professional claims (HR, 1.1; P < 0.0001; HR, 1.1; P < 0.0001, respectively).
DISCUSSION
The workplace mental health program consisting of proactive screening and care concierge services facilitated mental health treatment in a workforce population comprising employees and spouses/domestic partners, as evidenced by increased mental health prescription and professional health service use. This main finding extends on our prior work showing that implementation of a proactive and voluntary pilot mental health screening program in an employee population identified individuals at risk for mental health conditions, including those not currently in treatment, and connected those individuals with care.22 Demonstration of the outcomes of the workplace mental health intervention, including facilitating mental health treatment (eg, through professional visits and prescriptions), may help employers identify and implement interventions that have supporting evidence. Evidence-based interventions may better support employee mental health and reduce the burdens of underdetection and undertreatment of mental health conditions in workforce populations.
Proactive screening for mental health risk may contribute to better mental health care outcomes by identifying unrecognized risks or early symptoms, reducing underdetection, and reducing or delaying the onset of diagnosable disorders that require treatment.28,29 In our study, participants with moderate risk in screening showed the greatest increase in likelihood to receive mental health prescriptions and seek professional services. Thus, this program seems to aid in preventative mental health care by both identifying individuals who were exposed to risks or experiencing early symptoms and enabling intervention before onset of a diagnosable disorder. Early intervention and preventative programming for mental health care leads to better outcomes, especially for mood and anxiety disorders.28,30
Individuals who followed up with a care concierge had different characteristics than those who did not with respect to education, race/ethnicity (more White), and tobacco use. Because of these and other factors, participants who did not choose to meet with the care concierge may have had lower perceived need for help, existing mental health care providers, or the preference to handle problems without outside help. Low perceived need for mental health care is a common reason for not seeking mental health care, especially in those with mild to moderate disorders.31 Other barriers to mental health care include inconvenience and inability to obtain an appointment31 and low perceived cultural competence by the mental health care provider.32 For those with more severe conditions, stigma, low perceived efficacy of treatments, and desire to handle the problem on their own are more common barriers.31 As engagement with a care concierge can facilitate connections to mental health care, provide support and care management, improve mental health, and improve job performance,15,22,33 understanding characteristics of those who did and did not engage can inform strategies to engage more individuals in need with mental health services.
Participants who engaged with the care concierge were less likely to use tobacco (5.4% vs 18.6%) than those who did not meet with the care concierge. Several studies have reported on the association of tobacco use and mental health,34–37 where mental illness is 2–5 fold more common in smokers than nonsmokers.34,35,37 Individuals with mental illness often smoke to self-medicate.36 However, the relationship between tobacco use and mental illness appears bidirectional, where smoking has also been shown to cause depression, anxiety disorders, and schizophrenia and is a gateway to problematic substance use.34 Smoking may also impact the metabolism of some psychiatric medications, leading to lower therapeutic blood levels and the need for higher doses of medication to have the desired therapeutic impact.38 However, mental health treatment may also benefit tobacco cessation efforts, as prior research has shown that individuals with mental illness who received mental health treatment within the previous year were more likely to have quit smoking than those not receiving treatment.39 Thus, in an employee population, mental health interventions may compliment tobacco cessation programming.
Screening participants were highly educated, with more than 90% having some college education. Surprisingly, those who opted in to care concierge services had less education than those who did not. Inequity in mental health services use by education level has been previously reported, where individuals with higher education levels were more likely to receive services than individuals with lower education levels.40 For each additional level of education, individuals were 15% more likely to see a psychiatrist, 12% more likely to see a family doctor, 16% more likely to see a psychologist and 16% more likely to see a social worker.40 The lower education in those who opted into care in our report may be due to the previously established care in those who did not opt in to care concierge services. If so, the intervention may be facilitating care in those who may otherwise have not connected to care on their own without the intervention.
Participants who met with the care concierge had greater cumulative incidence of mental health prescriptions during the follow-up period, indicating the care concierge service may have played a role in facilitating the receipt of mental health treatment. Before the intervention, those who met with a care concierge had lower prescription drug use (35% vs 40%), potentially indicating a treatment gap that was narrowed with the intervention. Mental health prescription medication use was higher in participants than in published estimates where 15.8% of US adults had taken prescription medication for their mental health in 2019.41 Higher use of prescription medications observed in the present analysis, as compared with national estimates, may indicate that those who opted into the program may be more inclined to believe in the benefit of mental health intervention. Higher prior use of prior mental health prescriptions may also reflect the demographics including older age and majority female of the participating population. For example, National estimates have shown that the percentage of adults who had taken medication for their mental health in the past 12 months was higher among those aged 45 to 64 years (17.6%) and 65 years and over (17.7%), compared with those aged 18–44 (13.6%).41 In addition, women were more likely than men to have taken medication for their mental health (20.6% and 10.7%, respectively) and to have received counseling or therapy from a mental health professional (11.7% and 7.2%) in the past 12 months.41
Completion of a consultation with a care concierge where risks were discussed, care plans developed, and referrals to mental health supporting services and care were made was associated with greater likelihood of using mental health professional services during the follow-up period, including first time use. Timely access to mental health care is important to reducing unmet mental health care needs.42,43 Psychological treatments received during professional visits are an important component of mental health care because they yield similar efficacy to pharmacological treatments for depression and anxiety while reducing the risk of relapse even after its discontinuation.44,45 National data show that US adults are more likely to take prescription medication for their mental health (15.8%) than receive counseling or therapy from a mental health professional (9.5%).41 Yet, younger adults (aged 18–44 years) are more likely than older adults (aged 45+ years) to receive counseling or therapy from a mental health professional.41 Thus, therapy and counseling seems to be a more common treatment for younger adults. As previous reports have shown a preference for psychological treatment versus pharmacological treatments for mental health conditions45 and similar treatment efficacy,42,43 facilitating access and use of professional evidence-based psychological treatment may help to reduce treatment gaps in mental health care.45
Although the intervention and analysis period preceded the COVID-19 pandemic, large-scale disasters, such as a pandemic, are known to substantially impact mental health in ways that are influenced by sociodemographic factors, exposure, social support and personality factors.46 The societal impact of the COVID-19 pandemic had adverse mental health effects in both previously healthy people and in people with preexisting mental health disorders.20,21,47 Many (18.1%) individuals who experienced a COVID-19 diagnosis also experienced a psychiatric diagnosis within the following 3 months, including 5.8% with a first diagnosis.47 In addition, the COVID-19 pandemic disrupted mental health services, especially those related to prevention, psychotherapy, and counseling services.48 In light of the adverse impact on mental health, the COVID-19 pandemic also provided an opportunity to improve mental health services through more sustainable, efficient, and equitable delivery of mental health care.20 Thus, proactive, population-level mental health interventions as evaluated in the current investigation may become increasingly relevant in the aftermath of the pandemic.
The analysis presented here reflects outcomes of a program intervention intended to promote the uptake of evidence-based strategies into population health practice and to bridge the gap between the positive findings of an experimental study and outcomes in practice. Yet, this study had several potential limitations. Participation bias could have influenced outcomes. As only, 8170 (14.5%) of 56,442 eligible participated in screening and only 541 (12.8%) of 4215 with identified mental health risk engaged with a care concierge, those who opted into the screening and services likely had greater motivation to prioritize their mental health or need. Those with lower perceived need or greater barriers to engagement may have been underrepresented in this analysis. Thus, this intervention may have differentially nudged those with existing intent into treatment. In addition, given the nature of the available data, additional mental health outcomes could not be examined in the present study; these include outpatient visits, health care costs, symptom acuity, and use of mental health resources not reflected in medical claims data. As the study follow-up period was set to end before the impact of the COVID-19 pandemic, individuals who sought care after the study period were not included in the analysis. In addition, using the symmetry episode grouping methodology to identify individuals receiving behavioral health treatment through claims analysis may have overlooked inclusion of episodes of care for individuals requiring lower acuity care such as a single visit or referral to a non–health plan provider. Finally, Adjustment disorder (accompanied with descriptors of depression, anxiety, mixed affects) may be diagnosed in the medical setting for psychological care of the medically ill in liaison psychiatry49 when a person does not reach criteria for a major psychiatric nomenclature (depression and anxiety disorders).49 Adjustment disorder was not included in the present analysis due to a small sample size. Only 3.7% of participants (15 of 407 with both professional service and Rx across both groups) had a principal diagnosis of either adjustment or dysthymic disorder (persistent and chronic mild depressive disorder).
CONCLUSION
In summary, among program participants, the proactive mental health screening program with care concierge service demonstrated an impact on facilitating mental health treatment, including professional health services and prescriptions in a workforce population. Proactive models to screen for risk and emerging risk combined with concierge services to discuss risk, develop care plans, and make connections to care can be effective in closing the treatment gaps in mental health care. The workforce can be an important environment to deliver mental health services to both support the mental health needs of the employee population and benefit employee work performance. Successful mental health interventions should consider culture, race, and demographics to make programs accessible and desirable. Physical health interventions such as tobacco cessation and hypertension management should support mental health needs. Finally, considerations to increase participation in screening and engagement with mental health care services, including antistigma campaigns and broad communications, may further facilitate mental health care in the workplace.
Supplementary Material
Footnotes
Funding Sources: No funding was provided for this analysis. Work was performed as part of routine work responsibilities of the respective authors.
Conflict of Interest: M.S.F. and C.E.B. are employed by and has stock ownership in Quest Diagnostics. J.L.H. holds stock in and serves on the Board of Directors for Emvitals Inc. Emvitals was a paid vendor of Johns Hopkins Healthcare Solutions (JHHS) and provided the Emvitals technology platform, which was white labeled by JHHS, and sold to Quest Diagnostics in support of its employee well-being programs; we were not paid for any aspect of the research analysis and research paper preparation. N.A.J. is employed by and owns stock in Emvitals Inc. M.E.P. engaged in this research as part of his faculty position at Johns Hopkins, but was previously an advisor for, and has stock ownership in, Emvitals Inc. J.I.H. and P.M.K. report no conflicts of interest.
Ethical Considerations & Disclosures: Mental health care utilization was evaluated through retrospective analysis of anonymized data after program participation in a workplace setting. This analysis was conducted according to the HIPAA Privacy Rule (Title 45 Code of Federal Regulations, Section 164.514e), which governs research conducted by Covered Healthcare Entities and allows retrospective analysis using a limited data set without requiring approval by an institutional review board.
Supplemental digital contents are available for this article. Direct URL citation appears in the printed text and is provided in the HTML and PDF versions of this article on the journal’s Web site (www.joem.org).
Contributor Information
Carmen H. Tong, Email: Carmen.H.Tong@questdiagnostics.com.
Jennifer L. Hunter, Email: jhunter2124@gmail.com.
Nicole A. Jelovic, Email: njelovic@gmail.com.
Joanna I. Hayward, Email: jhayward@bhsonline.com.
Susan Carr, Email: scarr21@jhmi.edu.
Paul M. Kim, Email: pmkim@jhmi.edu.
Matthew E. Peters, Email: matthew.peters@jhmi.edu.
Charles E. Birse, Email: Charles.E.Birse@questdiagnostics.com.
REFERENCES
- 1.Williams SZ, Chung GS, Muennig PA. Undiagnosed depression: a community diagnosis. SSM Popul Health. 2017;3:633–638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kohn R, Saxena S, Levav I, Saraceno B. The treatment gap in mental health care. Bull World Health Organ. 2004;82:858–866. [PMC free article] [PubMed] [Google Scholar]
- 3.Kohn R Ali AA Puac-Polanco V, et al. Mental health in the Americas: an overview of the treatment gap. Rev Panam Salud Publica. 2018;42:e165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.US Government Accoutability Office . Behavioral health: research on health care costs of untreated conditions is limited. 2019. Available from: https://www.gao.gov/products/gao-19-274#. Accessed April 29, 2022.
- 5.Andrilla CHA, Patterson DG, Garberson LA, Coulthard C, Larson EH. Geographic variation in the supply of selected behavioral health providers. Am J Prev Med. 2018;54(6 Suppl 3):S199–S207. [DOI] [PubMed] [Google Scholar]
- 6.Bishop TF, Press MJ, Keyhani S, Pincus HA. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiat. 2014;71:176–181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Satiani A, Niedermier J, Satiani B, Svendsen DP. Projected workforce of psychiatrists in the United States: a population analysis. Psychiatr Serv. 2018;69:710–713. [DOI] [PubMed] [Google Scholar]
- 8.Greenberg PE, Fournier AA, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J Clin Psychiatry. 2015;76:155–162. [DOI] [PubMed] [Google Scholar]
- 9.McRee J. How perceptions of mental illness impact EAP utilization. Benefits Q. 2017;33:37–42. [PubMed] [Google Scholar]
- 10.Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D. Cost of lost productive work time among US workers with depression. JAMA. 2003;289:3135–3144. [DOI] [PubMed] [Google Scholar]
- 11.Mintz J, Mintz LI, Arruda MJ, Hwang SS. Treatments of depression and the functional capacity to work. Arch Gen Psychiatry. 1992;49:761–768. [DOI] [PubMed] [Google Scholar]
- 12.Chiu M, Lebenbaum M, Cheng J, de Oliveira C, Kurdyak P. The direct healthcare costs associated with psychological distress and major depression: a population-based cohort study in Ontario, Canada. PLoS One. 2017;12:e0184268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goetzel RZ Roemer EC Holingue C, et al. Mental health in the workplace: a call to action proceedings from the mental health in the workplace-public health summit. J Occup Environ Med. 2018;60:322–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Galea S, Merchant RM, Lurie N. The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern Med. 2020;180:817–818. [DOI] [PubMed] [Google Scholar]
- 15.Wang PS Simon GE Avorn J, et al. Telephone screening, outreach, and care management for depressed workers and impact on clinical and work productivity outcomes: a randomized controlled trial. JAMA. 2007;298:1401–1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berndt ER Finkelstein SN Greenberg PE, et al. Workplace performance effects From chronic depression and its treatment. J Health Econ. 1998;17:511–535. [DOI] [PubMed] [Google Scholar]
- 17.Joyce S Modini M Christensen H, et al. Workplace interventions for common mental disorders: a systematic meta-review. Psychol Med. 2016;46:683–697. [DOI] [PubMed] [Google Scholar]
- 18.Muramatsu K, Fujino Y, Kubo T, Otani M, Matsuda S. Relationship between treatment and period of absence among employees on sick leave due to mental disease. Ind Health. 2019;57:79–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Breitborde NJ Bell EK Dawley D, et al. The early psychosis intervention center (EPICENTER): development and six-month outcomes of an American first-episode psychosis clinical service. BMC Psychiatry. 2015;15:266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moreno C Wykes T Galderisi S, et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7:813–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Byrne A, Barber R, Hwai Lim C. Impact of the COVID-19 pandemic—a mental health service perspective. Progress Neurol Psychiatry. 2021;25:27–33b. [Google Scholar]
- 22.Fragala MS Hunter JL Satish A, et al. Workplace mental health: application of a population health approach of proactive screening to identify risk and engage in care. J Occup Environ Med. 2021;63:244–250. [DOI] [PubMed] [Google Scholar]
- 23.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009;114(1–3):163–173. [DOI] [PubMed] [Google Scholar]
- 24.Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders With the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016;39:24–31. [DOI] [PubMed] [Google Scholar]
- 25.Han B, Wong EC, Mao Z, Meredith LS, Cassells A, Tobin JN. Validation of a brief PTSD screener for underserved patients in federally qualified health centers. Gen Hosp Psychiatry. 2016;38:84–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bradley KA, DeBenedetti AF, Volk RJ, Williams EC, Frank D, Kivlahan DR. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcohol Clin Exp Res. 2007;31:1208–1217. [DOI] [PubMed] [Google Scholar]
- 27.Optum O. Symmetry® Episode Treatment Groups® Measuring health care with meaningful episodes of care. Eden Prairie (MN): Optum; 2012. Available from: https://www.optum.com/content/dam/optum/resources/whitePapers/symmetry_episode_treatment_groups_wp_06_2012.pdf. Accessed May 4, 2022. [Google Scholar]
- 28.National Research Council (US) and Institute of Medicine (US) Committee on the Prevention of Mental Disorders and Substance Abuse Among Children, Youth, and Young Adults: Research Advances and Promising Interventions . Preventing mental, emotional, and behavioral disorders among young people. Washington (DC): National Academies Press; 2009. Availabe at: https://www.ncbi.nlm.nih.gov/books/NBK32775/. Accessed April 29, 2022. [Google Scholar]
- 29.O'Connor EA, Whitlock EP, Gaynes B, Beil TL. Screening for depression in adults and older adults in primary care: An updated systematic review. Rockville (MD): Agency for Healthcare Research and Quality; 2009. Available from: https://www.ncbi.nlm.nih.gov/books/NBK36403/. Accessed April 29, 2022. [PubMed] [Google Scholar]
- 30.Anderson KK, John-Baptiste A, MacDougall AG, Li L, Kurdyak P, Osuch EA. Access and health system impact of an early intervention treatment program for emerging adults with mood and anxiety disorders. Can J Psychiatr. 2019;64:492–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mojtabai R Olfson M Sampson NA, et al. Barriers to mental health treatment: results from the National Comorbidity Survey Replication. Psychol Med. 2011;41:1751–1761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rice AN, Harris SC. Issues of cultural competence in mental health care. J Am Pharm Assoc (2003). 2021;61:e65–e68. [DOI] [PubMed] [Google Scholar]
- 33.Simon GE, Ludman EJ, Tutty S, Operskalski B, Von Korff M. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA. 2004;292:935–942. [DOI] [PubMed] [Google Scholar]
- 34.Prochaska JJ, Das S, Young-Wolff KC. Smoking, mental illness, and public health. Annu Rev Public Health. 2017;38:165–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Klungsoyr O, Nygard JF, Sorensen T, Sandanger I. Cigarette smoking and incidence of first depressive episode: an 11-year, population-based follow-up study. Am J Epidemiol. 2006;163:421–432. [DOI] [PubMed] [Google Scholar]
- 36.Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychol Rev. 2004;111:33–51. [DOI] [PubMed] [Google Scholar]
- 37.Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. JAMA. 2000;284:2606–2610. [DOI] [PubMed] [Google Scholar]
- 38.Zevin S, Benowitz NL. Drug interactions with tobacco smoking. An update. Clin Pharmacokinet. 1999;36:425–438. [DOI] [PubMed] [Google Scholar]
- 39.Cook BL, Wayne GF, Kafali EN, Liu Z, Shu C, Flores M. Trends in smoking among adults with mental illness and association between mental health treatment and smoking cessation. JAMA. 2014;311:172–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Steele LS, Dewa CS, Lin E, Lee KL. Education level, income level and mental health services use in Canada: associations and policy implications. Healthc Policy. 2007;3:96–106. [PMC free article] [PubMed] [Google Scholar]
- 41.Terlizzi EP, Zablotsky B. Mental health treatment among adults: United States, 2019. NCHS Data Brief. 2020;:1–8. [PubMed] [Google Scholar]
- 42.Wang PS, Berglund PA, Olfson M, Kessler RC. Delays in initial treatment contact after first onset of a mental disorder. Health Serv Res. 2004;39:393–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Brunner J, Schweizer CA, Canelo IA, Leung LB, Strauss JL, Yano EM. Timely access to mental health care among women veterans. Psychol Serv. 2019;16:498–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.DeRubeis RJ, Siegle GJ, Hollon SD. Cognitive therapy versus medication for depression: treatment outcomes and neural mechanisms. Nat Rev Neurosci. 2008;9:788–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McHugh RK, Whitton SW, Peckham AD, Welge JA, Otto MW. Patient preference for psychological vs pharmacologic treatment of psychiatric disorders: a meta-analytic review. J Clin Psychiatry. 2013;74:595–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. 2008;38:467–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Taquet M, Luciano S, Geddes JR, Harrison PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. 2021;8:130–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.World Health Organziation . The impact of COVID-19 on mental, neurological and substance use services. 2020. Available from: https://www.who.int/publications/i/item/978924012455. Accessed April 29, 2022.
- 49.Strain JJ. The adjustment disorder diagnosis, its importance to liaison psychiatry, and its psychobiology. Int J Environ Res Public Health. 2019;16:4645. [DOI] [PMC free article] [PubMed] [Google Scholar]


