Abstract
Background:
The COVID-19 pandemic accelerated telemedicine use nationally, but differences across health systems are understudied. We examine telemedicine use for adults with diabetes and/or hypertension across ten health systems and analyze practice and patient characteristics associated with greater use.
Methods:
Encounter-level data from the AMGA Optum™ Data Warehouse for March 13, 2020 to December 31, 2020 were analyzed, which included 3,016,761 clinical encounters from 764,521 adults with diabetes and/or hypertension attributed to one of 1,207 practice sites with ≥50 system-attributed patients. Linear spline regression estimated whether practice size and ownership were associated with telemedicine during the adoption (Weeks 0–4), de-adoption (Weeks 5–12), and maintenance (Week 13–42) periods, controlling for patient socioeconomic and clinical characteristics.
Results:
Telemedicine use peaked at 11% to 42% of weekly encounters after 4 weeks. In adjusted analyses, small practices had lower use for adults with diabetes during the maintenance period compared to larger practices. Practice ownership was not associated with telemedicine use. Practices with higher shares of Black patients continued to expand telemedicine use during the de-adoption and maintenance periods.
Conclusion:
Practice ownership was not associated with telemedicine use during first months of the pandemic. Small practices de-adopted telemedicine to a greater degree than medium and large sized practices. Technical support for small practices, irrespective of their ownership, could enable telemedicine use for adults with diabetes and/or hypertension.
Keywords: telemedicine, diabetes, hypertension, health systems, practice ownership
Precis:
Small practices had lower telemedicine use than medium and large sized practices after the twelfth week of shelter-in-place ordinances, highlighting that telemedicine is operationally challenging for small practices to maintain. Technical support for small system-affiliated practices, irrespective of their ownership, could help expand and maintain telemedicine use for adults with chronic conditions.
Objectives/Introduction
Prior to the COVID-19 pandemic, only about 50 health systems in the United States had an existing infrastructure for delivering telemedicine.1 Health care systems and their affiliated medical practices faced challenges of implementing telemedicine, especially video-based clinical encounters, due to billing challenges, required technology and workflow changes, and unstable, low quality internet connections for some patients.2–4 Patient preferences for in-person communication, viewed as more trustworthy, also contributed to low telemedicine use before the pandemic.5
Evidence indicates that the pandemic rapidly accelerated telemedicine implementation nationally,6–11 supported by a temporary federal waiver that permitted multiple flexibilities, including permitting audio-only encounters for Medicare telemedicine services, requiring managed care plans to reimburse clinicians at the same rate for telemedicine and in-person encounters, and permitting use of widely available platforms, such as FaceTime and Skype, without enforcement of Health Insurance Portability and Accountability Act penalties.12 Large-scale national studies during the pandemic indicate that telemedicine use peaked early in the pandemic, by April or May 2020, and quickly tapered off through the end of the year.4,7–9,13,14 To our knowledge, however, there is no evidence comparing health system maintenance of telemedicine after the first surge of the pandemic.
As a result of shelter-in-place ordinances, adults with diabetes and/or hypertension were vulnerable because their routine care involves close monitoring and medication management. These patients are not only likely to be at higher risk of COVID-19-related complications,15 but are at risk for exacerbations due to reduced access to care and utilization.16 Little research has compared telemedicine adoption and maintenance for adults with diabetes15,17 and/or hypertension across multiple health systems.
Leveraging electronic health record (EHR) and administrative data from ten members of AMGA (American Medical Group Association), we examine telemedicine adoption in health systems and analyze the physician practice and patient characteristics associated with rapid implementation through April 2020 and maintenance of telemedicine services through December 2020. Medical specialists tended to use telemedicine more than primary care physicians and surgical specialists during the pandemic,18 highlighting that practice ownership and specialty mix may contribute to telemedicine use. We hypothesized that independent practices would lag in telemedicine adoption compared to practices owned by systems because past evidence indicates that health system and medical group ownership of practices is associated with broader use of health information technology (IT) compared to independent physician practices, including disease registries, reminder systems, clinical decision support, and patient portals.19,20 Past research also indicates that larger physician practices, as measured by total physicians, adopt more chronic care management processes and health IT functions compared to small practices,19,21,22 although the capabilities of small practices are improving over time.23 Given previously documented technical and cultural barriers associated with implementing telemedicine,24 we hypothesized that small practices would be less likely to adopt and maintain telemedicine for adults with diabetes and/or hypertension compared to medium and large-sized practices.
Methods
Data
Data are sourced from Optum data available to AMGA, a nonprofit trade association representing more than 400 multispecialty medical groups and health systems with a total of more than 175,000 physicians. Some AMGA members contributed data to a common data repository managed by Optum and through a partnership with AMGA provided access to their data. Because the data elements are derived from EHRs, practice management systems, disease registries, and population health software, data are mapped and normalized to allow valid and reliable comparisons across organizations. The 10 systems represent a diverse population of health care systems across urban, suburban, and rural locations in 9 U.S. states and range in size from 14 to 638 practice locations and from 70 to 2,100 physician full-time equivalents (Appendix, Table 1). Encounter-level data for the early pandemic period, March 13, 2020 to December 31, 2020, were analyzed for patients with an established diagnosis of diabetes and/or hypertension. These encounter-level data documented telemedicine (remote video, audio only, or e-visit) use6 and patient characteristics.
We assigned clinicians to practice locations using National Provider Identifiers (NPIs) available in 2019 IQVIA OneKey data crosswalked with the AMGA Optum data. OneKey is a commercially available database of physician practice characteristics that integrates data from the American Medical Association, public sources, and proprietary data to describe medical practices, including information about practices such as practice ownership, size, addresses, and NPIs. Encounters without a practice site identifier were excluded (n=361,745, 8.7%). Because we were interested in examining weekly practice-level trends, which required multiple patients per week for reliable estimates, we excluded encounters from practice sites with <50 patients (184,003 encounters, 4.4%) during the study period. Analytic sample exclusions are detailed in Appendix, Table A2.
The analytic sample includes 3,016,761 encounters from 764,521 adults with diabetes and/or hypertension. Because we were interested in telemedicine use among established patients of health care systems, we limited the analytic sample to patients with at least one visit and at least one diagnosis of diabetes and/or hypertension between January 1, 2019 and March 12, 2020. We transformed the data into a practice-week dataset and analyzed weekly practice-level volume of telemedicine versus in-person encounters. Weeks were defined in increments of seven days starting March 13, 2020, totaling 42 weeks through December 31, 2020. Weekly visits were adjusted for weeks with holidays by dividing the total number of visits by the fraction of non-holiday days over seven days. For example, if one day of the week is a holiday and there were 10 total visits during that week for a practice, the 10 visits would be normalized to 11.67 weekly visits.
For regression analyses, we segmented the pandemic period into sub-periods using splines and analyzed weekly practice-level telemedicine use as a proportion of total encounters for three periods separately for the two patient subgroups: 1) adults diagnosed with diabetes (with or without hypertension), and 2) adults diagnosed with hypertension (without diabetes). We examined the two subgroups separately because compared to hypertension (without diabetes), managing diabetes entails addressing more standards of care25 and primary care practices were more likely to have established diabetes care management processes in place before the pandemic.26,27 Appendix Table A3 summarizes encounter and patient counts for these two subgroups by practice ownership.
We identified two time cut points with marked changes in telemedicine volumes: 1) week 5 as the onset of a telemedicine de-adoption period, and 2) week 13 when de-adoption slows down as the telemedicine maintenance period. We confirmed these cut points by piecewise linear regression and spline analyses, given the nonlinearity of data as assessed by the Shapiro-Wilk test (p < 0.0001). Based on these analyses, we defined week 1 to week 4 as the telemedicine adoption period, week 5 to week 12 as the telemedicine de-adoption period, and week 13 to week 42 as the telemedicine maintenance period. Appendix, Figure A1 summarizes temporal patterns in telemedicine use across the health care systems. The University of California, Berkeley Office for the Protection of Human Subjects approved reliance on Dartmouth College’s Committee for the Protection of Human Subjects institutional review board for study approval (#28763).
Outcome Measure
The study outcome measure is weekly practice-level telemedicine encounters as a proportion of all clinical encounters. Telemedicine encounters include encounters that occurred through remote video, audio, or an e-visit.
Main Independent Variables
The main independent variables are practice ownership and practice size. Practice ownership is a categorical variable of 1) independent practices, 2) medical group owned practices, and 3) hospital and/or health care system owned practices. Practices were categorized by size based on quartiles of the distribution of total physicians: 1) 0 to 1 physician, which includes advanced practice clinician-only practices (0 physicians) and solo physician practices (1 physician), 2) 2–3 physicians, 3) 4–6 physicians, and 4) 7 physicians or more.
Control Variables
Regression analyses control for practice and patient characteristics potentially associated with practice ownership, size, and telemedicine encounters. Practice characteristics included the number of advanced practice clinicians and specialty physician mix, as measured by the specialist-to-primary care physician ratio. Practices without specialists were categorized into one group and practice locations with specialists were categorized based on terciles of the distribution, resulting in a four-part categorical variable consisting of specialty mix: no specialists (72.5%), low specialty (9.2%), moderate specialty (9.1%), and high specialty (9.2%) mix.
Socio-demographic and clinical characteristics of patients were measured at the practice level and included the proportion of each practice’s eligible patients who are from each sex, race/ethnicity, marital status, urbanicity category, health insurance category, and proportions of patients with diagnoses of mental health conditions, atherosclerotic cardiovascular disease, chronic kidney disease, heart failure, obesity, and opioid use disorder. The median household income and Charlson comorbidity score28 of a practice’s patients were also included as covariates. We controlled for the proportion of patients with prescriptions for diabetes and hypertension medications in each practice. For the regression models for adults with diabetes (with or without hypertension), we controlled for the proportion of each practice’s patients with diabetes who were prescribed: 1) no glucose-lowering medications, 2) non-insulin glucose-lowering medications only, 3) insulin (with or without other glucose-lowering medications). For the hypertension (without diabetes) regression models, instead of diabetes medications, we account for the proportion of patients prescribed anti-hypertensive medications. Table 1 notes in detail the medications included.
Table 1.
Descriptive Summary of Patient Characteristics
| Overall | Hypertension (without diabetes) | Diabetes (with or without hypertension) | |
|---|---|---|---|
| Number of Patients | 764,521 | 484,845 | 279,676 |
| (100%) | (63.4%) | (36.6%) | |
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Patient Characteristics | |||
| Age | 64.1 (14.0) | 63.8 (14.5) | 64.6 (13.2) |
| Female (%) | 52.6 | 54.2 | 49.6 |
| Race/Ethnicity (%) | |||
| White | 79.3 | 81.2 | 75.9 |
| Hispanic | 3.7 | 2.8 | 5.4 |
| Black | 5.0 | 4.4 | 6.0 |
| Asian | 1.1 | 0.9 | 1.5 |
| Other race | 10.9 | 10.7 | 11.1 |
| Marital Status (%) | |||
| Married or Domestic Partnership | 60.9 | 61.4 | 60.1 |
| Divorced | 8.6 | 8.4 | 8.9 |
| Never married | 13.2 | 12.9 | 13.9 |
| Widowed | 10.3 | 10.2 | 10.4 |
| Other marital status | 7.0 | 7.1 | 6.7 |
| Median household income (US$; mean, SD) | 62,189.5 (20,464.7) | 63,123.9 (20,851.7) | 60,569.5 (19,671.2) |
| Encounter types | |||
| Total encounters | 3.9 (3.4) | 3.6 (3.1) | 4.4 (3.7) |
| Total in-person encounters | 3.1 (3.0) | 2.9 (2.7) | 3.5 (3.3) |
| Total telemedicine audio encounters | 0.2 (0.5) | 0.1 (0.5) | 0.2 (0.6) |
| Total telemedicine video encounters | 0.5 (1.1) | 0.5 (1.0) | 0.6 (1.2) |
| Total e-visit encounters | 0.0 (0.2) | 0.0 (0.2) | 0.0 (0.3) |
| Telemedicine exposed (%) | 39.4 | 37.4 | 42.6 |
| Urbanicity (%) | |||
| Metropolitan | 77.0 | 77.6 | 75.9 |
| Isolated | 4.5 | 4.4 | 4.8 |
| Rural (large) | 10.4 | 10.0 | 11.0 |
| Rural (small) | 7.0 | 6.9 | 7.3 |
| Insurance Class (%) | |||
| Commercial | 36.0 | 38.3 | 32.0 |
| Dual Medicare/Medicaid | 1.3 | 1.2 | 1.3 |
| Medicaid | 3.2 | 2.7 | 3.9 |
| Medicare | 55.2 | 53.3 | 58.5 |
| Others | 4.4 | 4.4 | 4.3 |
| Comorbidities (%) | |||
| Charlson score (mean, SD) | 1.9 (2.2) | 1.5 (1.9) | 2.6 (2.4) |
| Atherosclerotic Cardiovascular Disease | 24.0 | 21.3 | 28.7 |
| Chronic Kidney Disease | 16.2 | 11.2 | 24.7 |
| Heart Failure | 8.1 | 6.2 | 11.4 |
| Mental health diagnosis | 34.0 | 34.0 | 33.9 |
| Obesity | 26.6 | 22.0 | 34.7 |
| Opioid Use Disorder | 1.3 | 1.2 | 1.3 |
| Diagnoses (%) | |||
| Diabetes only | 6.6 | - | 18.0 |
| Hypertension only | 63.4 | 100.0 | - |
| Diabetes and Hypertension | 30.0 | - | 82.0 |
| Prescriptions (%) | |||
| Diabetes Medication | |||
| Diabetes with no drugs | - | - | 20.9 |
| Diabetes with non-insulin drugs only | - | - | 44.9 |
| Diabetes with insulin | - | - | 34.2 |
| Anti-hypertensive Medication | 84.2 | 86.4 | 80.4 |
Note: Diagnoses are obtained from the US National Library of Medicine Value Set Authority Center (NLM-VSAC) and we included all code classified as mental health conditions by NLM-VSAC. Insulin included prescriptions classified as insulin (basal), insulin (bolus), or insulin combination (basal and bolus). Non-insulin glucose-lowering medications included: biguanides, sulfonylureas, TZD, A-G inhibitors (<1%), meglitinides (<1%), DPP-4, SGLT2, amylin (<1%), and GLP-1. Anti-hypertensive medications include one or more of the following prescriptions: diuretics, beta-blockers, angiotensin converting enzyme inhibitors, angiotensin-receptor blockers, calcium channel blockers, alpha blockers, alpha-2 receptor agonists, combined alpha and beta-blockers, central agonists, peripheral adrenergic inhibitors, and vasodilators.
Statistical Analyses
Weekly patient encounters were analyzed from March 13 to December 31, 2020. Linear spline regression models were estimated to assess whether practice size and ownership were associated with telemedicine adoption and total encounter volume, controlling for patient sociodemographic and clinical characteristics, in each of the three periods (adoption, de-adoption, and maintenance). System fixed effects accounted for idiosyncratic effects of the ten health systems, and standard errors were clustered at the practice level. Models were estimated separately for: 1) adults with diabetes (with or without hypertension) and 2) adults with hypertension (without diabetes). We examined variance inflation factors (VIFs) and considered VIF of > 2.0 as an indication of potential collinearity among model covariates.29
Results
Of the 1,207 practice locations included in the analytic sample, most (76.9%) were owned by the health system that contributed data, while 5.2% were owned by a medical group affiliated with the health system, and 17.9% were independent practices with a system affiliation (Appendix, Table A4). The average patient age was 64.1 years (SD=14.0), and most patients were insured by Medicare (55.2%) or a commercial health plan (36.0%). Table 1 summarizes patient characteristics.
The average number of encounters per patient during the study period was 3.9 with a standard deviation (SD) of 3.4 encounters. Adults with diabetes (with or without hypertension) had an average of 4.4 total encounters (SD=3.7), while adults with hypertension (without diabetes) had an average of 3.6 total encounters (SD=3.1). Overall, in-person visits averaged 3.1 encounters (SD=3.0), telemedicine video visits averaged 0.5 encounters (SD=1.1), and telemedicine audio-only visits averaged 0.2 (SD=0.5) encounters during the study period.
Analyses of weekly trends revealed that telemedicine accounted for a high of 25% of weekly encounters in weeks 3 through week 5 of shelter-in-place ordinances, declined starting in week 6 through week 12, and stabilized from week 13 through the end of the calendar year or the maintenance period, when telemedicine accounted for 14% of weekly encounters (Figure 1). There was high variation in telemedicine use across the 10 health systems over time (Figure 2), with peak telemedicine use ranging from 11% to 42% of weekly encounters across the health systems, leveling off during the maintenance period at 6% to 32% of weekly encounters. Total encounter volume stabilized by week 12 (Appendix, Figure A2).
Figure 1.
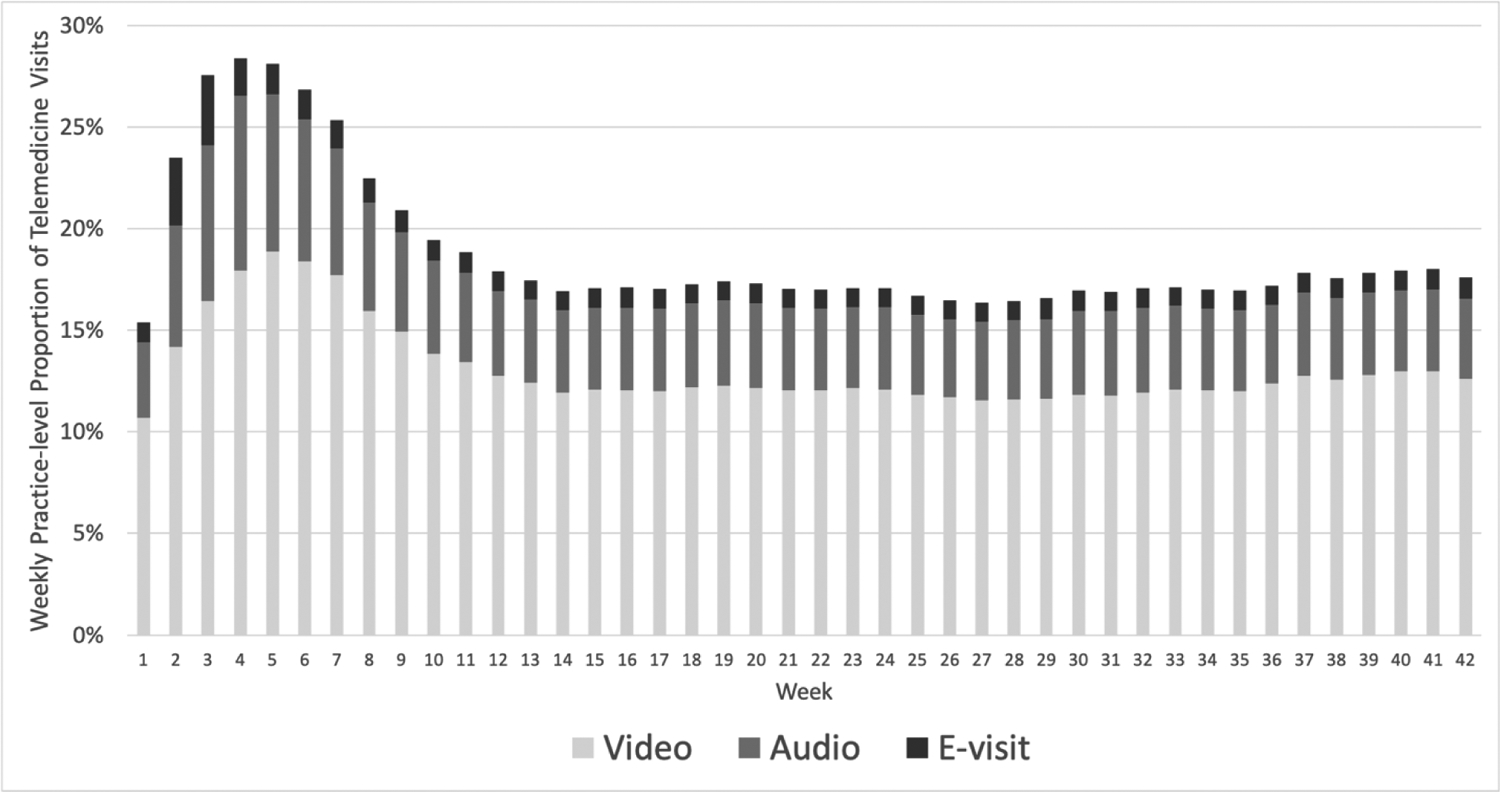
COVID-19 Era Weekly Composition of Telemedicine Visits among Adults with Diabetes and/or Hypertension Across 10 Health Care Systems
Analyses of weekly practice-level telemedicine visits as a proportion of overall visits among adults with diabetes and/or hypertension. Overall visits include in-person visits and telemedicine visits (video, audio, and e-visits).
Figure 2.
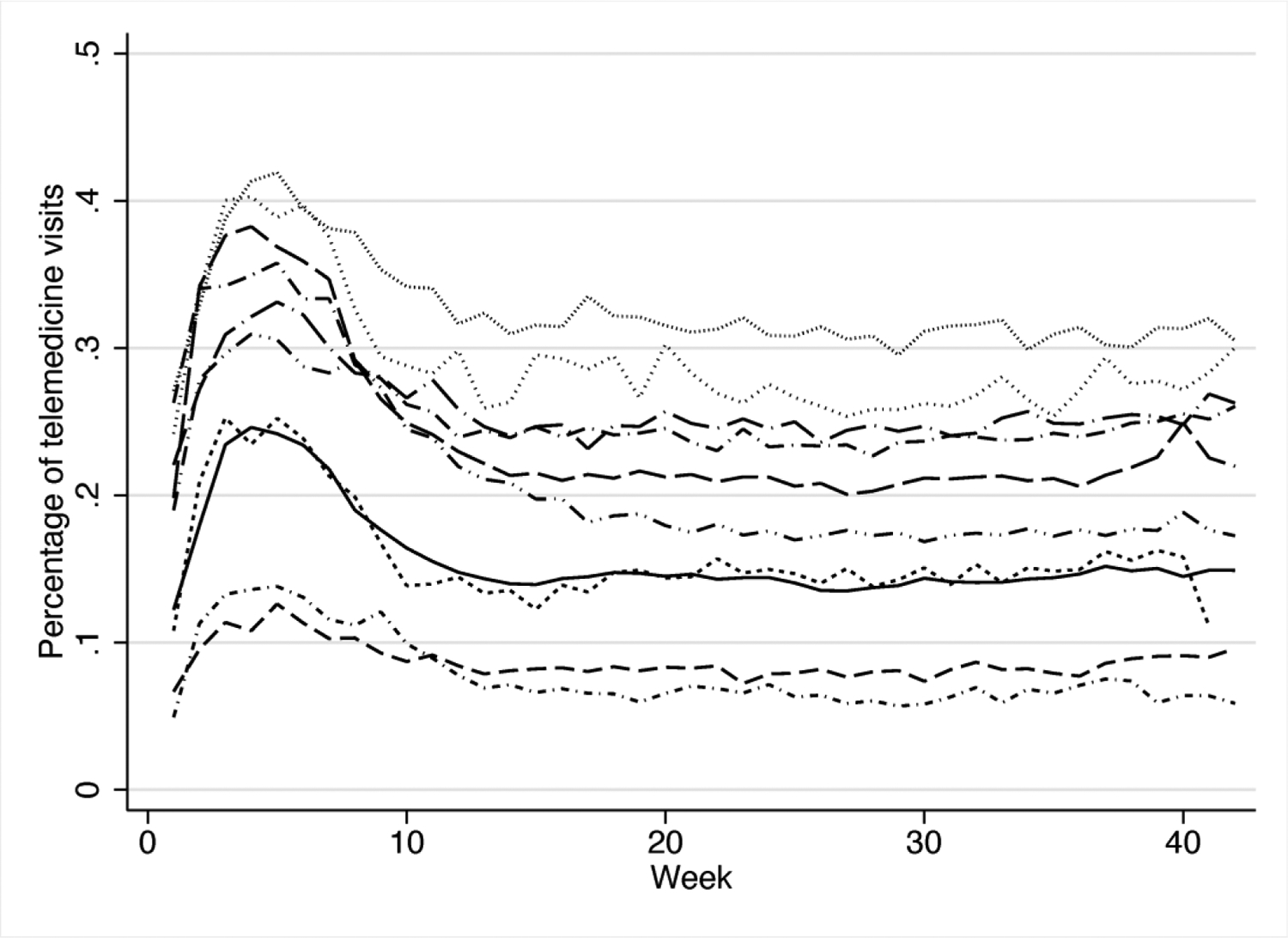
Weekly Telemedicine Use Trends for Adults with Diabetes and/or Hypertension, by Health System, March 15-December 31, 2020
Analyses of weekly health care system-level telemedicine visits as a proportion of overall visits among adults with diabetes and/or hypertension. Overall visits include in-person visits and telemedicine visits (video, audio, and e-visits). The ten trend lines depict the weekly telemedicine use pattern for each of the ten health care systems.
Results from regression analyses of adults with diabetes indicate that small practice size, practices with only advanced practice clinicians (0 physicians) and solo practices (1 physician) had 2% lower telemedicine use compared to larger practices during the maintenance period (Table 2). Practice ownership was not associated with telemedicine use in any period for adults with diabetes.
Table 2.
Practice and Patient Characteristics Associated with Telemedicine Use for Adults with Diabetes
| Patient n=279,676 | |||
|---|---|---|---|
| Adoption Period | De-Adoption Period | Maintenance Period | |
| Week | 0.05*** | −0.02*** | −0.00* |
| Practice Characteristics | |||
| Total advanced practice clinicians (standardized) | 0.00 | −0.00 | 0.00 |
| Size | |||
| Small, 0 to 1 physician (reference) | - | - | - |
| Medium, 2 to 3 physicians | 0.01 | 0.02 | 0.02** |
| Medium, 4 to 6 physicians | 0.01 | 0.01 | 0.02** |
| Large, 7 or more physicians | 0.01 | 0.01 | 0.02* |
| Specialty Mix | |||
| No specialists (reference) | - | - | - |
| Low specialty | 0.02 | 0.02 | 0.01 |
| Moderate specialty | 0.01 | 0.02 | 0.02* |
| High specialty | 0.01 | 0.02 | 0.00 |
| Ownership | |||
| System (reference) | - | - | - |
| Medical group | −0.00 | −0.01 | −0.01 |
| Independent | −0.00 | −0.01 | −0.01 |
| Patient Characteristics | |||
| Age (standardized) | −0.00 | −0.01* | −0.02*** |
| Female | 0.04** | 0.03** | 0.03*** |
| Race/Ethnicity | |||
| White (reference) | - | - | - |
| Hispanic | −0.02 | 0.01 | 0.04 |
| Black | 0.03 | 0.09*** | 0.06*** |
| Asian | −0.04 | −0.02 | 0.02 |
| Other race | −0.02 | 0.00 | −0.00 |
| Marital Status | |||
| Married or domestic partnership (reference) | - | - | - |
| Divorced | −0.02 | 0.01 | −0.01 |
| Never married | 0.02 | 0.01 | 0.01 |
| Widowed | −0.02 | 0.01 | −0.00 |
| Other marital status | 0.05* | 0.04 | 0.04** |
| Median household income (standardized) | 0.03*** | 0.04*** | 0.02*** |
| Urbanicity | |||
| Metropolitan (reference) | - | - | - |
| Isolated | −0.03 | −0.04* | −0.03*** |
| Rural (large) | −0.03 | −0.06*** | −0.04*** |
| Rural (small) | −0.06*** | −0.06*** | −0.04*** |
| Insurance Class | |||
| Medicare (reference) | - | - | - |
| Commercial | 0.02 | −0.00 | 0.00 |
| Dual Medicare/Medicaid | 0.06 | 0.04 | 0.04 |
| Medicaid | 0.00 | −0.06** | −0.03* |
| Other insurance | 0.02 | 0.01 | −0.02 |
| Charlson score (standardized) | −0.01 | −0.02*** | −0.00 |
| Comorbidities | |||
| Atherosclerotic Cardiovascular Disease | −0.02 | −0.03* | 0.01 |
| Chronic Kidney Disease | 0.01 | 0.05*** | 0.04*** |
| Heart Failure | 0.00 | 0.01 | −0.00 |
| Mental Health Diagnosis | 0.02 | −0.00 | 0.03*** |
| Obesity | −0.02 | −0.05*** | 0.01 |
| Hypertension | 0.02 | 0.02 | 0.02 |
| Diabetes Medication | |||
| No prescriptions (reference) | - | - | - |
| Non-insulin only | 0.01 | −0.00 | 0.02* |
| Insulin w/ or w/out non-insulin medications | 0.02 | 0.02 | 0.02* |
| Constant | −0.08 | 0.24*** | 0.10*** |
| Observations | 4,297 | 9,018 | 33,963 |
Notes: Practices with ≥ 50 attributed patients included.
*, **, and *** represents p < 0.05, p < 0.01, and p < 0.001, respectively. The regression models are linear spline models from weeks 1 to 4, weeks 5 to 12, and weeks 13 to 42. The models include system fixed effects, but these effects are omitted in the regression outputs above for brevity. The models also include standard errors clustered at the practice level.
Several practice characteristics were associated with telemedicine use among the diabetes patient sample (Table 2). Practices with greater shares of patients from rural and isolated areas had lower telemedicine use compared to practices with relatively more patients from metropolitan areas across periods. For a 1% increase in the proportion of female patients, practices had 3–4% higher telemedicine use. For a 1% increase in the proportion of Black patients, practices had 9% and 6% greater telemedicine use during the de-adoption and maintenance periods, respectively. To illustrate the effect size, the mean telemedicine use rate was 19% and an average of 9% of patients are Black; an absolute increase of 1% in Black patients (to 10% of patients) increases the practice telemedicine use rates to 21% and 20% during the de-adoption and maintenance periods, respectively.
Practice size and ownership were not associated with telemedicine use for hypertension (without diabetes) samples in any of the 3 periods (Table 3). High specialty mix compared to practices with no specialists at the practice level was associated with 4% greater telemedicine use as a percentage of total encounters for hypertension patients during the telemedicine adoption period.
Table 3.
Practice/Patient Characteristics Associated with Telemedicine Use for Adults with Hypertension
| Patient n=484,845 | |||
|---|---|---|---|
| Adoption Period | De-Adoption Period | Maintenance Period | |
| Week | 0.05*** | −0.02 | 0.00 |
| Practice Characteristics | |||
| Total advanced practice clinicians (standardized) | 0.01*** | −0.00 | 0.00 |
| Size | |||
| Small, 0 to 1 physician (reference) | - | - | - |
| Medium, 2 to 3 physicians | 0.00 | 0.01 | 0.01 |
| Medium, 4 to 6 physicians | 0.01 | 0.01 | 0.01 |
| Large, 7 or more physicians | −0.01 | −0.01 | 0.00 |
| Specialty Mix | |||
| No specialty(reference) | - | - | - |
| Low specialty | 0.02 | 0.01 | 0.01 |
| Moderate specialty | 0.02 | 0.01 | 0.01 |
| High specialty | 0.04* | 0.02 | 0.01 |
| Ownership | |||
| System (reference) | - | - | - |
| Medical group | 0.02 | 0.01 | −0.01 |
| Independent | −0.01 | 0.00 | −0.00 |
| Patient Characteristics | |||
| Age (standardized) | 0.00 | −0.02** | −0.02** |
| Female | 0.03* | 0.02 | 0.01 |
| Race/Ethnicity | |||
| White (reference) | - | - | - |
| Hispanic | −0.01 | 0.05 | 0.05* |
| Black | 0.02 | 0.11*** | 0.06*** |
| Asian | 0.16* | −0.02 | −0.02 |
| Other race | −0.00 | 0.02 | 0.00 |
| Marital Status | |||
| Married or domestic partnership (reference) | - | - | - |
| Divorced | −0.00 | −0.02 | −0.01 |
| Never married | 0.00 | −0.01 | 0.00 |
| Widowed | −0.01 | 0.02 | 0.00 |
| Other marital status | 0.05* | 0.05* | 0.04** |
| Median household income (standardized) | 0.03*** | 0.04*** | 0.02*** |
| Urbanicity | |||
| Metropolitan (reference) | - | - | - |
| Isolated | −0.04 | −0.06** | −0.03** |
| Rural (large) | −0.04** | −0.07*** | −0.05*** |
| Rural (small) | −0.03 | −0.06*** | −0.03*** |
| Insurance Class | |||
| Medicare (reference) | - | - | - |
| Commercial | 0.04* | −0.02 | 0.01 |
| Dual Medicare/Medicaid | 0.01 | 0.02 | 0.02 |
| Medicaid | −0.01 | −0.06* | −0.05*** |
| Other insurance | 0.09* | −0.02 | 0.01 |
| Charlson score (standardized) | −0.02*** | −0.02*** | 0.00 |
| Comorbidities | |||
| Atherosclerotic Cardiovascular Disease | −0.05** | −0.00 | −0.01* |
| Chronic Kidney Disease | 0.05 | 0.01 | 0.04* |
| Heart Failure | 0.02 | 0.03 | −0.01 |
| Mental Health Illness | 0.05** | 0.02 | 0.06*** |
| Obesity | −0.05** | −0.03* | −0.00 |
| Anti-hypertensive Medication | −0.02 | −0.02 | 0.01 |
| Constant | −0.03 | 0.34*** | 0.13*** |
| Observations | 4,445 | 9,260 | 35,034 |
Notes: Practices with ≥50 attributed patients included.
*, **, and *** represents p < 0.05, p < 0.01, and p < 0.001, respectively. The regression models are linear spline models from weeks 1 to 4, weeks 5 to 12, and weeks 13 to 42. The models include system fixed effects, but these effects are omitted in the regression outputs above for brevity. The models also include standard errors clustered at the practice level.
Patient characteristics associated with telemedicine use were similar for hypertension patients compared to diabetes patients, with the notable exception of insurance type. Among hypertension patients, Medicare and Medicaid insurance were significantly associated with less telemedicine use compared to commercially-insured patients.
The low VIFs among all the variables (VIF < 2.0) across all models indicate that collinearity among covariates is not a significant concern.
Discussion
Weekly practice-level telemedicine use for adults with diabetes and hypertension varied widely across ten health systems during the early COVID-19 pandemic. The wide range of 11% to 42% of telemedicine visits as a share of total weekly encounter volume during the adoption period (Weeks 1–4), the peak of telemedicine utilization, demonstrates that health systems had a strong influence on remote diabetes and hypertension care management during the early pandemic. We found that many systems institutionalized telemedicine, with use at levels upwards of one-third of total encounter volume during the maintenance period, while other systems did not scale up telemedicine beyond 15% of weekly encounters at any point in 2020.
Our results highlight that small practices face difficulty maintaining telemedicine for adults with diabetes or intentionally choose to de-adopt telemedicine over time. This finding is consistent with past research highlighting the challenges small practices face when attempting to implement care delivery and payment reforms.23,30 Importantly, this relationship did not extend to adults with hypertension (without diabetes), potentially because managing diabetes entails addressing more standards of care25 compared to hypertension (without diabetes) and primary care practices were more likely to have established care management processes in place for diabetes compared to hypertension before the pandemic.26,27
Small practices may need technical assistance and resources from health systems, payers, and governments to help them maintain telemedicine for their patients with diabetes and other chronic conditions. HI-TECH Act infrastructural investments in small practices to expand health IT functionality31 might be leveraged to support telemedicine as a patient-centered option that could reduce treatment burden for adults with chronic conditions.32
We anticipated that health system-owned practices would have higher telemedicine use compared to independent practices with health system affiliations, but found no such relationship in our main analyses. The study results suggest that health systems can influence telemedicine adoption and implementation equally for their owned and affiliated practices. Comparable telemedicine use for system owned and independent practices within the ten health care systems we examined stands in stark contrast to past evidence about independent practices that document their deficiencies in chronic care management capabilities.19,20 Our results highlight the potential chronic care management benefits of health care system affiliation for independent practices.
We also found that practices with relatively higher proportions of Black patients continued to expand telemedicine use through the end of 2020, at a time when practices with lower shares of Black patients were de-adopting or maintaining telemedicine use levels. Practices with high shares of Black patients may have more extensively redesigned care to accommodate patients during the pandemic. This finding is in contrast to evidence outside of health systems and in single health systems which found that Black patients were less likely to use telemedicine compared to White patients.33,34 Increased telemedicine use among practices with relatively high shares of Black patients may also reflect Black patients’ perceptions of the pandemic as a greater health threat, perhaps due to the consequences of systemic racism, than White patients.35
The study results should be considered in light of some limitations. First, we focused on practice size and ownership because extensive research highlights their association with practice capabilities,19,21,22 including health IT. We did not assess practice-level health IT or organizational culture because data are not available to assess these factors. These factors may, however, help to explain differences in telemedicine use and should be assessed in future research. Second, although practices with relatively high shares of Black patients increased telemedicine use relative to practices with lower shares of Black patients, unmeasured social and economic factors could account for this relationship. Moreover, Black patients may not have been the higher telemedicine users within these practices; evidence is needed to clarify why and how practices with high concentrations of Black patients accelerated telemedicine implementation. Finally, the analyses are cross-sectional, so temporal ordering and causal relationships cannot be assessed. Future research could examine the impact of practice ownership changes36 and telemedicine use to further elucidate the causal effect of practice ownership changes on telemedicine use.
Conclusion
Telemedicine use for adults with diabetes and hypertension varied widely across ten health systems during the early pandemic period. Solo physician and advanced practice clinician only practices had significantly lower telemedicine use among adults with diabetes with or without hypertension, highlighting that technical support for small practices, irrespective of their ownership, could support more extensive telemedicine use for adults with diabetes and/or hypertension.
Supplementary Material
Takeaway Points:
This study of ten health systems examines whether practice size and ownership are associated with more extensive adoption and maintenance of telemedicine for adults with diabetes and/or hypertension during the early pandemic.
Health systems varied widely in their use of telemedicine; use peaked at 11% to 42% of weekly clinical encounters after 4 weeks of shelter-in-place ordinances, leveling off to 6% to 32% of weekly encounters after 13 weeks.
Small practices (solo physicians and advanced practice clinician only practices) had 1–2% lower telemedicine use compared to larger practices after Week 13.
Practices with higher shares of Black patients continued to expand telemedicine use through the end of 2020, when practices with lower shares of Black patients were de-adopting or maintaining telemedicine use levels.
Funding:
This study was supported by the Agency for Healthcare Research and Quality’s (AHRQ’s) Comparative Health System Performance Initiative under Grant # 1U19HS024075, which examines how health care delivery systems promote evidence-based practices and patient-centered outcomes research in delivering care.
References
- 1.Hollander JE, Carr BG. Virtually Perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–1681. doi: 10.1056/NEJMp2003539 [DOI] [PubMed] [Google Scholar]
- 2.Graetz I, Gordon N, Fung V, Hamity C, Reed ME. The Digital Divide and Patient Portals: Internet Access Explained Differences in Patient Portal Use for Secure Messaging by Age, Race, and Income. Med Care. 2016;54(8):772–779. doi: 10.1097/MLR.0000000000000560 [DOI] [PubMed] [Google Scholar]
- 3.Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc. 2011;18(3):318–321. doi: 10.1136/jamia.2010.006015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khoong EC, Butler BA, Mesina O, et al. Patient interest in and barriers to telemedicine video visits in a multilingual urban safety-net system. Journal of the American Medical Informatics Association. 2021;28(2):349–353. doi: 10.1093/jamia/ocaa234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.So CF, Chung JW. Telehealth for diabetes self-management in primary healthcare: A systematic review and meta-analysis. J Telemed Telecare. 2018;24(5):356–364. doi: 10.1177/1357633X17700552 [DOI] [PubMed] [Google Scholar]
- 6.Mann DM, Chen J, Chunara R, Testa PA, Nov O. COVID-19 transforms health care through telemedicine: Evidence from the field. J Am Med Inform Assoc. Published online May 29, 2020. doi: 10.1093/jamia/ocaa072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Alexander GC, Tajanlangit M, Heyward J, Mansour O, Qato DM, Stafford RS. Use and Content of Primary Care Office-Based vs Telemedicine Care Visits During the COVID-19 Pandemic in the US. JAMA Netw Open. 2020;3(10):e2021476. doi: 10.1001/jamanetworkopen.2020.21476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eberly LA, Kallan MJ, Julien HM, et al. Patient Characteristics Associated With Telemedicine Access for Primary and Specialty Ambulatory Care During the COVID-19 Pandemic. JAMA Netw Open. 2020;3(12):e2031640. doi: 10.1001/jamanetworkopen.2020.31640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel SY, Mehrotra A, Huskamp HA, Uscher-Pines L, Ganguli I, Barnett ML. Variation In Telemedicine Use And Outpatient Care During The COVID-19 Pandemic In The United States: Study examines variation in total US outpatient visits and telemedicine use across patient demographics, specialties, and conditions during the COVID-19 pandemic. Health Affairs. 2021;40(2):349–358. doi: 10.1377/hlthaff.2020.01786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cantor JH, McBain RK, Pera MF, Bravata DM, Whaley CM. Who Is (and Is Not) Receiving Telemedicine Care During the COVID-19 Pandemic. American Journal of Preventive Medicine. 2021;61(3):434–438. doi: 10.1016/j.amepre.2021.01.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Friedman AB, Gervasi S, Song H, et al. Telemedicine catches on: changes in the utilization of telemedicine services during the COVID-19 pandemic. Am J Manag Care. 2022;28(1):e1–e6. doi: 10.37765/ajmc.2022.88771 [DOI] [PubMed] [Google Scholar]
- 12.Koonin LM, Hoots B, Tsang CA, et al. Trends in the Use of Telehealth During the Emergence of the COVID-19 Pandemic — United States, January–March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(43):1595–1599. doi: 10.15585/mmwr.mm6943a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peden CJ, Mohan S, Pagán V. Telemedicine and COVID-19: an Observational Study of Rapid Scale Up in a US Academic Medical System. J GEN INTERN MED. 2020;35(9):2823–2825. doi: 10.1007/s11606-020-05917-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rodriguez Jorge A., Betancourt Joseph R., Sequist Thomas D., Ganguli Ishani. Differences in the use of telephone and video telemedicine visits during the COVID-19 pandemic. Am J Manag Care. 2021;27(1):21–26. doi: 10.37765/ajmc.2021.88573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patel SY, McCoy RG, Barnett ML, Shah ND, Mehrotra A. Diabetes Care and Glycemic Control During the COVID-19 Pandemic in the United States. JAMA Intern Med. 2021;181(10):1412–1414. doi: 10.1001/jamainternmed.2021.3047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ansari Z, Laditka JN, Laditka SB. Access to Health Care and Hospitalization for Ambulatory Care Sensitive Conditions. Med Care Res Rev. 2006;63(6):719–741. doi: 10.1177/1077558706293637 [DOI] [PubMed] [Google Scholar]
- 17.Quinton JK, Ong MK, Sarkisian C, et al. The Impact of Telemedicine on Quality of Care for Patients with Diabetes After March 2020. J Gen Intern Med. 2022;37(5):1198–1203. doi: 10.1007/s11606-021-07367-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sharma AE, Khoong EC, Sierra M, et al. System-Level Factors Associated With Telephone and Video Visit Use: Survey of Safety-Net Clinicians During the Early Phase of the COVID-19 Pandemic. JMIR Form Res. 2022;6(3):e34088. doi: 10.2196/34088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodriguez HP, McClellan SR, Bibi S, Casalino LP, Ramsay PP, Shortell SM. Increased Use of Care Management Processes and Expanded Health Information Technology Functions by Practice Ownership and Medicaid Revenue. Med Care Res Rev. 2016;73(3):308–328. doi: 10.1177/1077558715613233 [DOI] [PubMed] [Google Scholar]
- 20.Bishop TF, Shortell SM, Ramsay PP, Copeland KR, Casalino LP. Trends in hospital-ownership of physician practices and the effect on processes to improve quality. Am J Manag Care. 2016;22(3):172–176. [PMC free article] [PubMed] [Google Scholar]
- 21.Bishop TF, Ramsay PP, Casalino LP, Bao Y, Pincus HA, Shortell SM. Care Management Processes Used Less Often For Depression Than For Other Chronic Conditions In US Primary Care Practices. Health Affairs. 2016;35(3):394–400. doi: 10.1377/hlthaff.2015.1068 [DOI] [PubMed] [Google Scholar]
- 22.Wiley JA, Rittenhouse DR, Shortell SM, et al. Managing Chronic Illness: Physician Practices Increased The Use Of Care Management And Medical Home Processes. Health Affairs. 2015;34(1):78–86. doi: 10.1377/hlthaff.2014.0404 [DOI] [PubMed] [Google Scholar]
- 23.Rittenhouse DR, Ramsay PP, Casalino LP, McClellan S, Kandel ZK, Shortell SM. Increased Health Information Technology Adoption and Use Among Small Primary Care Physician Practices Over Time: A National Cohort Study. Ann Fam Med. 2017;15(1):56–62. doi: 10.1370/afm.1992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang T, Mosier J, Subbian V. Identifying Barriers to and Opportunities for Telehealth Implementation Amidst the COVID-19 Pandemic by Using a Human Factors Approach: A Leap Into the Future of Health Care Delivery? JMIR Hum Factors. 2021;8(2):e24860. doi: 10.2196/24860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American Diabetes Association. Standards of Medical Care in Diabetes-2017 Abridged for Primary Care Providers. Clin Diabetes. 2017;35(1):5–26. doi: 10.2337/cd16-0067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Miake-Lye IM, Chuang E, Rodriguez HP, Kominski GF, Yano EM, Shortell SM. Random or predictable?: Adoption patterns of chronic care management practices in physician organizations. Implement Sci. 2017;12(106). doi: 10.1186/s13012-017-0639-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hammersley V, Parker R, Paterson M, et al. Telemonitoring at scale for hypertension in primary care: An implementation study. Rahimi K, ed. PLoS Med. 2020;17(6):e1003124. doi: 10.1371/journal.pmed.1003124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schneeweiss S, Maclure M. Use of comorbidity scores for control of confounding in studies using administrative databases. International Journal of Epidemiology. 2000;29(5):891–898. doi: 10.1093/ije/29.5.891 [DOI] [PubMed] [Google Scholar]
- 29.O’brien RM. A Caution Regarding Rules of Thumb for Variance Inflation Factors. Qual Quant. 2007;41(5):673–690. doi: 10.1007/s11135-006-9018-6 [DOI] [Google Scholar]
- 30.Casalino LP, Wu FM, Ryan AM, et al. Independent Practice Associations And Physician-Hospital Organizations Can Improve Care Management For Smaller Practices. Health Affairs. 2013;32(8):1376–1382. doi: 10.1377/hlthaff.2013.0205 [DOI] [PubMed] [Google Scholar]
- 31.Adler-Milstein J, Jha AK. HITECH Act Drove Large Gains In Hospital Electronic Health Record Adoption. Health Affairs. 2017;36(8):1416–1422. doi: 10.1377/hlthaff.2016.1651 [DOI] [PubMed] [Google Scholar]
- 32.Spencer-Bonilla G, Serrano V, Gao C, et al. Patient Work and Treatment Burden in Type 2 Diabetes: A Mixed-Methods Study. Mayo Clinic Proceedings: Innovations, Quality & Outcomes. 2021;5(2):359–367. doi: 10.1016/j.mayocpiqo.2021.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khatana SAM, Yang L, Eberly LA, Julien HM, Adusumalli S, Groeneveld PW. Predictors of telemedicine use during the COVID-19 pandemic in the United States–an analysis of a national electronic medical record database. Wilson FA, ed. PLoS ONE. 2022;17(6):e0269535. doi: 10.1371/journal.pone.0269535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chunara R, Zhao Y, Chen J, et al. Telemedicine and healthcare disparities: a cohort study in a large healthcare system in New York City during COVID-19. Journal of the American Medical Informatics Association. 2021;28(1):33–41. doi: 10.1093/jamia/ocaa217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Campos-Castillo C, Anthony D. Racial and ethnic differences in self-reported telehealth use during the COVID-19 pandemic: a secondary analysis of a US survey of internet users from late March. Journal of the American Medical Informatics Association. 2021;28(1):119–125. doi: 10.1093/jamia/ocaa221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Poon BY, Shortell S, Rodriguez HP. Physician Practice Transitions to System Ownership Do Not Result in Diminished Practice Responsiveness to Patients. Health Serv Res. 2018;53(4):2268–2284. doi: 10.1111/1475-6773.12804 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


