Context:
Electronic health record (EHR) data can potentially make chronic disease surveillance more timely, actionable, and sustainable. Although use of EHR data can address numerous limitations of traditional surveillance methods, timely surveillance data with broad population coverage require scalable systems. This report describes implementation, challenges, and lessons learned from the Multi-State EHR-Based Network for Disease Surveillance (MENDS) to help inform how others work with EHR data to develop distributed networks for surveillance.
Program:
Funded by the Centers for Disease Control and Prevention (CDC), MENDS is a data modernization demonstration project that aims to develop a timely national chronic disease sentinel surveillance system using EHR data. It facilitates partnerships between data contributors (health information exchanges, other data aggregators) and data users (state and local health departments). MENDS uses query and visualization software to track local emerging trends. The program also uses statistical and geospatial methods to generate prevalence estimates of chronic disease risk measures at the national and local levels. Resulting data products are designed to inform public health practice and improve the health of the population.
Implementation:
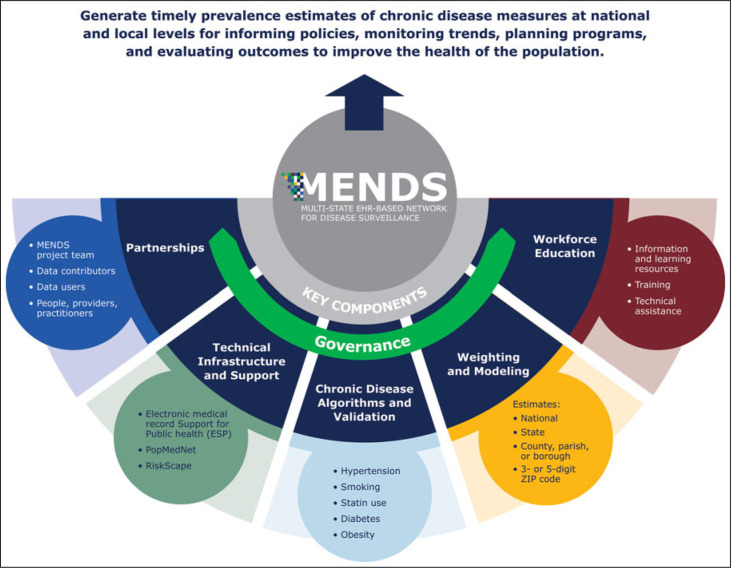
MENDS includes 5 partner sites that leverage EHR data from 91 health system and clinic partners and represents approximately 10 million patients across the United States. Key areas of implementation include governance, partnerships, technical infrastructure and support, chronic disease algorithms and validation, weighting and modeling, and workforce education for public health data users.
Discussion:
MENDS presents a scalable distributed network model for implementing national chronic disease surveillance that leverages EHR data. Priorities as MENDS matures include producing prevalence estimates at various geographic and subpopulation levels, developing enhanced data sharing and interoperability capacity using international data standards, scaling the network to improve coverage nationally and among underrepresented geographic areas and subpopulations, and expanding surveillance of additional chronic disease measures and social determinants of health.
Keywords: chronic disease, data network, electronic health record, health informatics, health information technology, hypertension, interoperability, population health, public health practice, surveillance
Context
Timely public health surveillance data are essential to guide policy development, allocate resources, and evaluate interventions to protect and improve health in all communities.1–3 Electronic health records (EHRs) have the potential to modernize surveillance by providing clinically detailed data on broadly distributed large populations in a timely, automated, and sustainable manner.4,5 Such surveillance can provide actionable insights into geographic patterns and temporal trends of disease.4
Traditional public health surveillance methods for nonreportable chronic conditions (eg, population-based surveys) can be largely manual and labor-intensive, include limited clinical detail, or are subject to extended delays between data acquisition and dissemination. While traditional surveillance is useful, EHR data can be complementary and provide an opportunity to overcome many of these limitations.4 State health departments are building familiarity and capacity for using EHR data for immunizations and state-regulated reportable conditions—primarily using electronic case reporting (eCR)—in accordance with federal program requirements.6 Additional mechanisms and scalable systems that leverage EHR data for robust chronic disease surveillance are needed.
Limited literature exists on the adoption of EHR-based population health surveillance of chronic diseases, suggesting its potential might not yet be fully realized. State, tribal, local, and territorial (STLT) health departments may not have tapped into EHR data to monitor chronic disease occurrence, medical care, and outcomes at the population level.4,7 The volume, detail, and timeliness of EHR data would allow public health agencies to track chronic diseases and risk factors, including hypertension, diabetes, obesity, smoking, and others. Furthermore, these data would provide meaningful insights into the effects of efforts to improve risk factor control and treatment intensification.4 A national EHR-based sentinel surveillance network could support public health monitoring of chronic disease patterns to inform more effective policies and programs at various geographic and subpopulation levels. For example, recommendations have called for a national system for cardiovascular health and disease surveillance that incorporates use of EHR data.8 This report presents the development of a novel model for implementing national chronic disease surveillance that leverages EHR data, including key challenges and lessons learned to help inform how others work with EHR data, especially distributed networks for surveillance.
Program: The Multi-State EHR-Based Network for Disease Surveillance
In 2018, the Centers for Disease Control and Prevention (CDC) awarded the National Association of Chronic Disease Directors (NACDD) 5 years of funding to demonstrate the feasibility and value of using EHR data for chronic disease surveillance. The Multi-State EHR-Based Network for Disease Surveillance (MENDS) demonstration project builds a chronic disease surveillance model that leverages clinically detailed EHR data of large, diverse populations to generate prevalence estimates of chronic disease and its risk factors. The pilot's focus is implementing surveillance for conditions related to cardiovascular health, enhancing public health capacity to use EHR data for chronic disease surveillance and evaluation, and identifying strategies to establish and scale a national chronic disease sentinel surveillance network. MENDS aims to be a timely (ie, monthly or quarterly data updates), automated chronic disease surveillance system for monitoring trends, informing policies, planning programs, and evaluating outcomes.9 The timely data generated from such a system would benefit competencies and practices of chronic disease units and specialty teams in STLT health departments that need those data to make effective public health decisions.9–11 In addition, MENDS supports healthcare organizations' efforts to advance population health.
Selection of a model and principles for national implementation of a distributed network for surveillance
The MDPHnet-distributed network for surveillance in Massachusetts was selected as a model to scale a national sentinel surveillance system. MDPHnet uses 3 open-source software platforms: Electronic medical record Support for Public health (ESP),12 PopMedNet,13 and RiskScape.14 ESP uses EHR data to identify notifiable and chronic diseases.12,15 PopMedNet enables distribution of queries and facilitates secure data sharing.13,15,16 RiskScape is a Web-based data visualization tool.14,17
The MENDS team, coordinated by the partner with expertise in building information partnerships, scanned existing surveillance system models, strengths, and limitations to scale and enhance national implementation, using the MDPHnet model. The team reviewed 19 examples of 5 EHR-based models (distributed network, partnership with healthcare entities, partnership with a data aggregator, national surveillance system, and disease-specific surveillance system). From the scan and other practice-based informed criteria of interest,18 5 key principles emerged that the team determined could optimize a national implementation of a distributed network for surveillance:
Take advantage of the breadth of clinical data available in EHR systems, including current and historical vital signs, laboratory tests, medications, and diagnoses;
Use disease and condition algorithms that are transparent and clinically meaningful;
Allow data owners to retain as much control and oversight of their data as needed to facilitate participation;
Use open-source resources; and
Be compatible with data from any EHR or EHR-based software system and emerging data exchange standards. One standard for developing enhanced data sharing and interoperability capacity that will be prioritized as MENDS progresses is Fast Healthcare Interoperability Resources (FHIR), published by Health Level 7 (HL7) International.19
Furthermore, an optimal system could be scalable across regions, provide surveillance data for public health organizations at multiple geographic levels, and advance data contributor access to tools that inform practice and support population health goals. Elements of these principles also align with CDC's Data Modernization Initiative (DMI) and the Federal Data Strategy.20,21
MENDS partners
MENDS is guided by project team partners with expertise in informatics, clinical medicine, public policy, and public health surveillance. Table 1 lists these organizations and their roles. Partnering data contributors (health information exchanges [HIEs], other data aggregators) have robust patient-level data from approximately 91 health system and clinic partners across the United States. Data contributors, in turn, collaborate with public health data users—often state and local departments of health (DOHs)—to form a partner site. CDC is a data user of the overall network. Table 1 lists MENDS partner site organizations.
TABLE 1. MENDS Project Team and Partner Sites.
| Organization | Project Team Role |
|---|---|
| National Association of Chronic Disease Directors (NACDD) | Direct CDC grantee that provides project oversight, establishes strategic direction, and serves as the Coordinating Center for MENDS |
| Centers for Disease Control and Prevention (CDC) | Both funder and subject matter expert in surveillance, small area estimation, electronic case definitions, and data modernization |
| Commonwealth Informatics (CI) | Information technology vendor to support the ESP, PopMedNet, and RiskScape software platforms for MENDS and the system's overall implementation and maintenance, including data quality assurance and algorithm development |
| Harvard Medical School, Department of Population Medicine (DPM) | Original developers of ESP platform and MDPHnet and leaders of the MDPHnet Coordinating Center that support algorithm development and validation efforts |
| Public Health Informatics Institute (PHII), a program of the Task Force for Global Health | An organization with expertise in building governance and information partnerships across MENDS |
| University of Massachusetts Lowell | Technical lead for developing weighting and modeling methods to generate prevalence estimates for varying geographic levels and subpopulations |
| Partner Site Data Contributor a | Data User |
| AllianceChicago | Chicago Department of Public Health Cook County Department of Public Health |
| Louisiana Public Health Institute/REACHnet | Louisiana Office of Public Health New Orleans Health Department Texas Department of State Health Services |
| OneHealthPort | Washington State Department of Health |
| Trustees of Indiana University and Regenstrief Institute | Indiana Department of Health Marion County Public Health Department |
| University of Colorado Anschutz Medical Campus and Health Data Compass | University of Colorado Anschutz Medical Campus |
aData contributors are stewards of data from their associated healthcare organization partners.
Methods: MENDS Implementation
MENDS implementation comprises 6 key areas: governance, partnerships, technical infrastructure and support, chronic disease algorithms and validation, weighting and modeling, and workforce education for public health data users, as shown in Figure 1.
FIGURE 1.
MENDS Key Components
Governance
MENDS governance is the foundation for building trust and consensus, sharing information, and making decisions. A Governance Committee, representative of data contributors and data users, establishes legal agreements to share data and creates documentation of policies and procedures (eg, MENDS Governance Principles, Policies, and Processes22) that codify how the network operates. The committee is the primary forum for partner sites to discuss MENDS data management, use, exchange, and release of information products at the national and local levels. An intentional early investment in governance has been critical to proactively identify policy and procedure gaps and address them in a consistent, thoughtful, and timely manner.
Data contributors executed legal agreements (eg, Business Associate Agreement, Data-Sharing and Use Agreement [DSUA]) with the information technology (IT) vendor to support software use and system activities. Similar agreements were executed with NACDD and a technical partner to permit access to limited data sets for validation and advanced analytic purposes. When providing DOHs access to MENDS data tools, some data contributors executed DSUAs to govern those relationships. To support partner site governance work, CDC provided a written determination that MENDS operates within the public health authority pursuant to the Health Insurance Portability and Accountability Act. Because it is public health surveillance, MENDS is exempt from institutional review board (IRB) review, although several data contributors sought institutional IRB approval for their participation.
Partnerships
Leveraging data exchange partnerships with healthcare organizations, data contributors install and maintain an ESP datamart connected to PopMedNet and RiskScape for MENDS. At least 89% and up to 100% of encounters in each data contributor's datamart are ambulatory visits. Combined datamart coverages are mostly adults 20 years and older (82%), are female (55%), and are white (66%), Black (15%), Hispanic (15%), Asian and Pacific Islander (3%), American Indian or Alaska Native (1.5%), and additional racial and ethnic subpopulations.
Effective information partnerships require time, staff resources, and organizational commitment. Each organization needs a value case at the site level for why and how MENDS will lead to enduring benefits for the organization and its partners.11 Data contributors may benefit from MENDS by gaining new insights and tools to advance population health and clinical quality improvement, strengthening data aggregators' role and efforts of their associated healthcare organization partners. Data contributors also may gain relationships with other MENDS sites and their data users. Data contributors work closely with data users authorized to use MENDS data for surveillance. Local, state, and national data users may benefit from an increased capability to access and act on timely EHR-based surveillance data and can monitor population health changes, allocate resources, and evaluate targeted health interventions.
Technical infrastructure and support
MENDS requires data contributors to meet extensive technical requirements for access to EHR data, support of IT and executive staff, dedicated hardware, and installation of ESP and PopMedNet software packages. Each data contributor had its own source data format (eg, OMOP,23 PCORnet,24 Consolidated Clinical Document Architecture [C-CDA]25) from which ESP extracted data. ESP can extract data from any EHR or EHR-based software system. Contributors provision EHR-based data per the MENDS ESP data model, including patients' demographics, encounters, laboratory tests, medications, and diagnosis records from January 1, 2017, forward, with at least quarterly updates of new information. Installation, configuration, and administration of ESP and PopMedNet require considerable application-specific knowledge. To save time and streamline personnel training, all sites work with an IT vendor experienced with ESP, PopMedNet, and RiskScape.
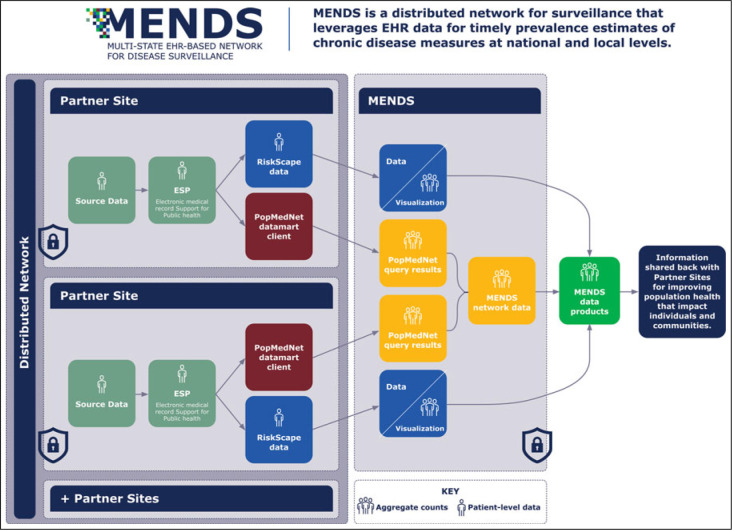
Figure 2 shows the technical structure and data relationships for MENDS, as a distributed network model, at partner site and network levels. Variances in staffing, server and software infrastructure, and other technical requirements among partner sites influenced implementation progress. The average time between ESP software installation and the initial baseline data load was 9 months (range of 7-11 months). For a subset of partner sites that advanced to the next stage, average time between initial baseline data load and data availability in RiskScape was 3 months, exclusive of the time needed for algorithm validation.
FIGURE 2.
MENDS Technical Structure, Software, and Data Flow
Abbreviation: EHR, electronic health record.
Chronic disease algorithms and validation
EHR data for public health surveillance rely on using algorithms to identify chronic disease conditions and risk factors of interest, related outcomes, and measures. Table 2 shows the implemented MENDS priority algorithms and associated clinical data components. The team's selection of algorithms was based on CDC priorities and leveraged algorithm development and validation work previously conducted and defined by MDPHnet,26,27 informed by electronic clinical quality measures (eCQMs) and clinical decision-making. A statin use algorithm, informed by the statin therapy eCQM,28 is currently under development by the MENDS team.
TABLE 2. Clinical Algorithms, Sociodemographic Strata, and Data Components.
| Clinical Data Components | |
|---|---|
| Priority clinical algorithms26–28 | |
| Hypertension | |
| Diagnosed hypertension | Diagnosis codes |
| Controlled hypertension | Blood pressure, diagnosis codes |
| Clinical hypertension | Blood pressure, diagnosis codes, medications |
| Smoking | Social history |
| Cholesterol management | |
| Statin use | Diagnosis codes, medications, laboratory results |
| Diabetes | |
| Type 1 | Diagnosis codes, medications, laboratory results |
| Type 2 | Diagnosis codes, medications, laboratory results |
| Gestational diabetes | Diagnosis codes, medications, laboratory results |
| Prediabetes | Diagnosis codes, laboratory results |
| Obesity | |
| BMI | Weight, height |
| BMI percentile | Weight, height, age, sex |
| Other clinical algorithms 26 | |
| Pregnancy status | Encounter pregnancy field (estimated date of delivery), diagnosis codes |
| Sociodemographic strata | |
| Race (American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or Other Pacific Islander, white, more than one race, unspecified) | Patient demographics |
| Ethnicity (Hispanic or Latino, not Hispanic or Latino, unspecified) | Patient demographics |
| Sex (female, male, other, unspecified) | Patient demographics |
| Age (continuous variable, classified into age groups) | Patient demographics calculated from date of birth |
| 5-digit ZIP code | Patient demographics |
| Primary insurance | Encounter |
Abbreviation: BMI, body mass index.
MENDS uses a multistage approach for data quality assessment and algorithm validation, including internal and external comparisons. Internal validation builds on partner sites' data quality systems already in place and capabilities from their membership in other data networks. The team first confirms that source data loaded as expected. Data are characterized, and the team determines whether any anomalies exist in source data or in loading and mapping of source data. The team then applies case-finding algorithms to the validated raw data (eg, blood pressures, medications) to identify conditions (eg, controlled hypertension). These results are validated internally against source data and will be validated externally (eg, comparison of prevalence calculated via MENDS with the expected prevalence from Behavioral Risk Factor Surveillance System [BRFSS] and other independent surveys or data sources).29,30 Completing internal validation stages has taken approximately a year on average, which includes investigating findings, applying corrections when warranted, and often reloading and reprocessing data.
Weighting and modeling
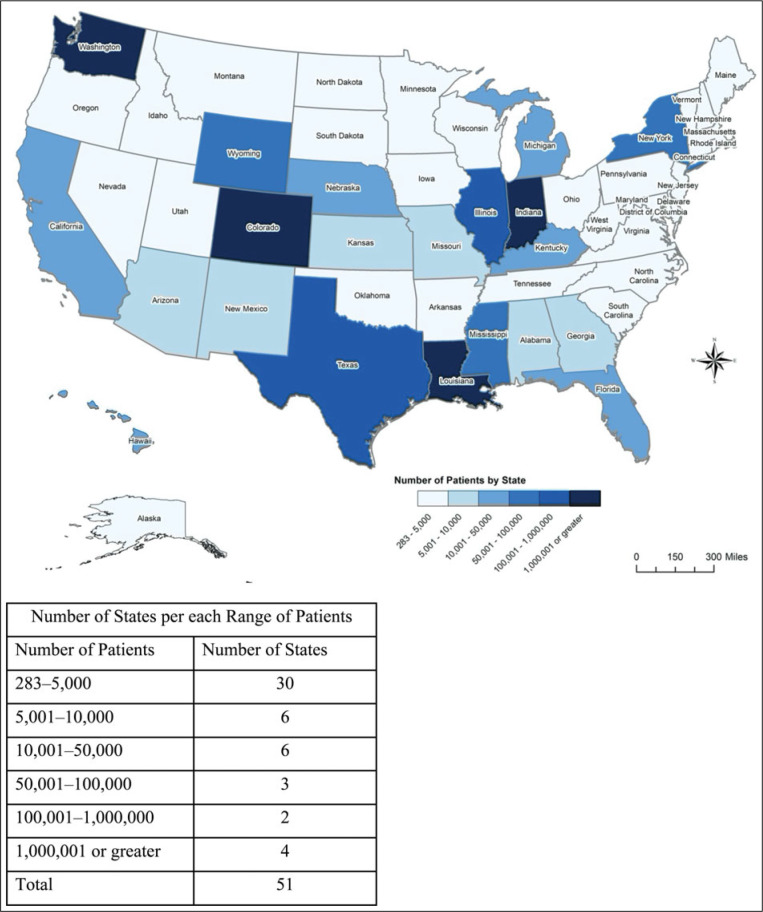
The large volume of rich, clinical data in MENDS makes in-depth analyses possible. Partner sites represent approximately 10 million patients across the United States (see Figure 3). Fifteen states have more than 10 000 patients, meeting a threshold where generated prevalence estimates are likely to achieve a precision of ±1% or better. Clinical partners' selection was nonrandom, and their data are not statistically representative of the total populations living in their catchment areas, nor of their respective locales, states, or the United States at large. Therefore, MENDS has developed weighting and modeling methods to produce more reliable local, state, and national prevalence estimates. Methods will be refined as MENDS data availability changes over time.
FIGURE 3.
MENDS Coverage Map Showing Distribution of MENDS Patients by State
MENDS applies statistical procedures to create reliable prevalence estimates from EHR data that reflect the underlying populations at target geographic levels. The team applies poststratified weighting according to sex, age, race/ethnicity, and rural-urban distributions from the US Census and American Community Surveys (ACS).31 Weighting reduces bias and improves precision of estimates by accounting for systemic differences in sociodemographic profiles between the MENDS patient population and the underlying general population. To address uneven geographic and sociodemographic coverage of the data, MENDS applies small area/domain estimation models to generate prevalence estimates, as well as geographic and sociodemographic disparities at the local, state, and national levels.
Workforce education for public health data users
Partner sites receive focused information, training, and technical assistance on MENDS and the use of EHR data for chronic disease surveillance, including query and visualization software guidance. The team developed project resources, one being a Learning Community to build public health data user confidence with EHR-based surveillance.9 Opportunities such as MENDS data user meetings and RiskScape application demonstrations have been offered.
EHR-based surveillance and a distributed data network architecture were novel to DOH data users participating in MENDS. The ability to supplement traditional public health surveillance tools, such as population-based surveys, with EHR-based surveillance was a major change to data users' existing surveillance process, methods, and interpretation. Educational resources orient new MENDS data users and more broadly increase public health understanding and use of clinical data for chronic disease surveillance. This work supports larger efforts to communicate data modernization needs to partners and prepare the public health workforce to adopt new tools to generate meaningful insights.5,20
Lessons Learned Shaping MENDS Implementation
MENDS has experienced both expected and unexpected challenges, including some that had compound impacts or contributed to lengthy implementation delays. Addressing key lessons learned has accelerated partner site selection and implementation; improved documentation of network functionality; and clarified roles, responsibilities, and technical requirements to meet goals.
Rethinking the partner site recruitment approach
MENDS first recruited state health departments as primary partners, largely through NACDD's outreach to an extensive network of state and territorial health department chronic disease leaders and members. At that time, few state health departments had direct access to the type and level of EHR-based data that the project required. In addition, most had limited ability to effectively partner with healthcare organizations that could contribute EHR data to MENDS. MENDS then shifted to recruiting data contributors, specifically large data aggregators for efficiency and scale, that are stewards of data from their multiple clinical partners and could approve the sharing of data needed for project participation. This change resulted in a wider population coverage than initially anticipated. Data contributors recruited as partner sites, contracting with NACDD for MENDS, then focused on bringing proximal DOHs into MENDS as public health data users to support surveillance activities. The MENDS team provided outreach support as needed to form a partner site. The 2 types of partner site organizations—data contributors and data users—have equal voting weight in the governance of the network.
Instituting a discovery process
Multiple partner sites progressed far into the recruitment and implementation process before discovering the technical or data requirements of MENDS could not be met. As a result, MENDS refined how it evaluates candidate sites. Preliminary discussions assess interest, readiness, and capacity to meet core requirements. Sites now confirm they meet 2 criteria: (1) minimally appropriate hardware requirements (storage size dependent on the size of the active patient population, number of years of data, and density of patient data); and (2) provision of specific, needed data elements as indicated through a precontract data confirmation investigation. These prerequisites ensure the efficiency of data processing and the sites' ability to contribute to the network's surveillance goals. This discovery process, along with better documentation of participation requirements, has resulted in an acceleration in new partner onboarding.
Strengthening a new type of information partnership to share data for public health
Several recruited data contributors had not participated in a public health surveillance project or worked with a DOH chronic disease partnership before MENDS. Through this pilot, data contributors learned about the public health surveillance landscape and data users learned about the data systems that collect EHR data and how they function with MENDS software tools. The approach to this information partnership and the dynamics of the data contributor–data user relationship have taken different forms, demonstrating there is no one-size-fits-all approach for building these partnerships.11
Fostering governance flexibility to meet partner site needs beyond the network
MENDS success required alignment with the many internal and external relationships maintained by the partner sites; these ranged from their internal health system collaborators to participation in other networks. Organizations at the site level had existing policy, governance structures, and compliance requirements that had to be reflected in MENDS governance. It was key to establish a governance approach flexible enough to operate across the differences. Furthermore, as precautionary data security controls were strengthened to protect against unauthorized use and release, MENDS allowed sites to develop customized data security plans for their site-specific environments.
Aligning a phased algorithm validation effort to capacity
As part of the multistage approach to validation used, internal algorithm validation was a major effort for partner sites because access to source data was required to verify the code correctly identified conditions. To help sites manage this effort, MENDS created additional documentation to better communicate the validation process during technical implementation, prioritized indicators, and supported sites in validating one indicator at a time, allowing them to staff the effort more easily.
Piloting gains to efficiency through HL7 FHIR standards
Variation associated with data contributors' different source data formats (eg, OMOP, PCORnet) required creating custom scripts to extract, transform, and load data from each partner, a resource-heavy and time-intensive effort. FHIR, specifically the Bulk Data Access Application Programming Interface (API), may simplify MENDS data provisioning, reducing the burden, and streamline the overall technical effort to bring partners onboard, potentially accelerating the expansion of the network and adding to cost-effectiveness and sustainability. One partner site will test this capability by piloting data provisioning from an OMOP database using FHIR.
Discussion
EHR-based surveillance has the potential to provide routine public health surveillance for nonreportable chronic conditions that is timely, actionable, and sustainable and to complement existing disease surveillance systems such as BRFSS and National Health and Nutrition Examination Survey (NHANES).4,29,30,32 EHR-based surveillance data could be valuable to both public health and healthcare partners, contributing to shared goals for improving population health that have an impact on individuals and communities.
As a demonstration project for building an EHR-based chronic disease surveillance model, MENDS has yielded promising implementation strategies and preliminary local prevalence estimates. Through partnerships between public health and healthcare organizations, EHR data have been transmitted using open-source software platforms and standardized across sites by applying algorithms and validation. Available as aggregate prevalence estimates and in more granular formats generated from specialized queries, the data can also be explored further using PopMedNet query and RiskScape visualization tools.13,14 MENDS has demonstrated the capability to meet principles and criteria distilled to optimize the project and can support CDC's DMI.
Moreover, MENDS could contribute opportunities for DOH uptake of EHR-based surveillance beyond federal program requirements. State health departments' receipt and use of EHR surveillance data rely on eCR data, systems, and policy for individually reportable services, events, and conditions, which have not generally enabled surveillance of nonreportable chronic conditions. However, opportunities may exist to build out the eCR infrastructure to gather information for additional use cases, such as for chronic disease surveillance (eg, using eCQMs for blood pressure control,33 including through eCR Now34). MENDS experience in leveraging EHR data for chronic disease surveillance can inform these future enhancements.
Most challenges have been overcome with additional outreach, communication, documentation, investigation, or training but not without impacts on the project timeline. For example, development of flexible policies and practices to allow partner sites to meet their own institutional and compliance requirements and inclusion of a data confirmation investigation have strengthened the process and could expedite onboarding of new sites. The relationships established, coupled with shared goals for the project, have helped keep sites engaged during implementation delays.
The team anticipates a continued, thoughtful reliance on governance to shape MENDS and contribute to the network's adaptability to future change and longevity. MENDS is examining data quality, including data concordance between HIE warehouses and source EHRs reported in other analyses,35 to improve reliability and strengthen use of data products and visualizations. Critical evaluation areas for MENDS include assessing signs of success and scalability as a pilot, achieving key attributes of public health surveillance system evaluation frameworks (eg, data quality, representativeness),36 and determining whether the program is beneficial to partner organizations, including how MENDS data are used. The team is evaluating the validity of prevalence estimates in comparison with estimates generated from other national chronic disease surveillance systems.
As MENDS matures, goals will broaden to strategically address the future of EHR-based surveillance. MENDS will include the following aims, as feasible:
Adapting to emerging standards (eg, HL7 FHIR) and leveraging the growing interoperability of EHRs, in alignment with public health data modernization efforts.3,5,18,20 The large data sets from current sites in the network require extensive transformation and processing to ensure they are accurate. Use of HL7 FHIR standards requires more technical effort and investment in the short term, responding to federal compliance pressures, but could minimize the data flow work to onboard new sites as policy levers influencing future data availability are still under development. MENDS could explore additional FHIR functionality (eg, FHIR-based queries).
Expanding geographic reach and breadth of conditions. Adding partner sites and healthcare organization partners will fill in geographic gaps and underrepresented regions, increasing representativeness and enhancing the value of estimates for small geographic locales and subpopulations. Early work in weighting and modeling, and strategic selection of future sites, can further support robust national and local estimates of a variety of chronic diseases.37 Adding data elements and algorithms related to cognitive/behavioral health, injuries, and other nonreportable conditions (eg, hypertensive disorders of pregnancy) may also enhance the network's value for myriad partners. MENDS can be incrementally scaled to serve as a tool to monitor and identify emerging policy and practice opportunities.
Remaining positioned to leverage the adoption of EHR data standards that identify social determinants of health. MENDS can potentially provide timely prevalence data on high-priority subpopulations for addressing inequities. Although MENDS includes some sociodemographic data that facilitate an understanding of health inequities, the advent of standards for social determinants of health data (eg, food insecurity, housing status) adds value and would bring a health equity focus to surveillance.
All these extensions of MENDS capabilities will enhance its ability to support timely, actionable, and sustainable routine chronic disease surveillance by the public health community.
Implications for Policy & Practice
Modernizing surveillance using EHR data has the potential to be timely, actionable, and sustainable, producing reliable estimates at different geographic levels that can complement existing chronic disease surveillance methods. These activities strengthen infrastructure that can be leveraged across priorities and conditions and have wide public health applicability.
MENDS is a demonstration project that aims to improve use of EHR-based chronic disease surveillance data. MENDS supports CDC's DMI by increasing public health workforce capacity to analyze, interpret, and act on EHR-based surveillance data in decision making about chronic disease prevention, treatment, and control. Partner site data reflect more than 10 million patients from approximately 91 health systems and clinics across the United States.
This report describes MENDS implementation and lessons learned to help inform development of a national chronic disease sentinel surveillance system and other EHR-based chronic disease surveillance models, especially distributed networks for surveillance. Furthermore, MENDS will test HL7 FHIR capability, supporting existing and future policy levers for increased interoperability to enable access to population-level data. These first years of MENDS have created a novel infrastructure to support STLT health departments with their chronic disease surveillance efforts and goals to improve the health of the population.
Footnotes
The creation of this information is associated with Multi-State EHR-Based Network for Disease Surveillance (MENDS). The authors acknowledge the contribution of MENDS partner sites and project team (https://chronicdisease.org/MENDSINFO). Furthermore, the authors acknowledge the following people for their contributions to the development of this publication: Laura Nasuti, PhD, MPH, who provided consultant services for NACDD early in the manuscript's development regarding the design, coordination of authors, and writing of the manuscript; and MENDS project team partners Bill Brand, MPH, and Bob Zambarano, PhD, who reviewed the paper for its alignment with governance- and technical-focused components, respectively. In addition, the authors acknowledge Thomas G. Land, PhD, formerly of the University of Massachusetts Medical School, who contributed to early MENDS implementation and project vision; Robert Merritt, MA, and Elin Begley, MPH, from the Division for Heart Disease and Stroke Prevention, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention, who provided oversight to this project; and the following NACDD consultants and staff: Miriam Patanian, MPH; Kathy Foell, MS; Kayla Craddock, MPH; Jeanne Alongi, DrPH, MPH; and Marti Macchi, MEd, MPH.
The “Improving Chronic Disease Surveillance and Management Through the Use of Electronic Health Records/Health Information Systems” project is supported by the Centers for Disease Control and Prevention (CDC) of the US Department of Health and Human Services (HHS) as part of a financial assistance award totaling $2 500 000 with 100% funded by CDC/HHS.
The contents are those of the authors and do not necessarily represent the official views of, nor an endorsement, by CDC/HHS or the US government.
Nine authors declare that they have no financial disclosures to report. Most authors (organizational affiliations) have had contracts with NACDD to conduct this work. Two authors are affiliated with an organization that has funding from Massachusetts Department of Public Health for support and development of Electronic medical record Support for Public health (ESP) and MDPHnet, which is the underlying technology of MENDS.
The authors declare that they have no conflicts of interest.
Written work prepared by employees of the Federal Government as part of their official duties is, under the U.S. Copyright Act, a “work of the United States Government” for which copyright protection under Title 17 of the United States Code is not available. As such, copyright does not extend to the contributions of employees of the Federal Government.
No copyrighted materials were used in this article.
Human Participant Compliance Statement: CDC provided a written determination that MENDS operates within the public health authority pursuant to the Health Insurance Portability and Accountability Act. As a public health surveillance project, MENDS does not require institutional review board approval.
Contributor Information
Katherine H. Hohman, Email: khohman@chronicdisease.org.
Amanda K. Martinez, Email: amartinez_ic@chronicdisease.org.
Michael Klompas, Email: mklompas@bwh.harvard.edu.
Emily M. Kraus, Email: emily@kraushold.com.
Wenjun Li, Email: Wenjun_Li@uml.edu.
Thomas W. Carton, Email: tcarton@lphi.org.
Noelle M. Cocoros, Email: Noelle_Cocoros@harvardpilgrim.org.
Sandra L. Jackson, Email: icl1@cdc.gov.
Bryant Thomas Karras, Email: bryant.karras@doh.wa.gov.
Jennifer L. Wiltz, Email: igc2@cdc.gov.
Hilary K. Wall, Email: ifx0@cdc.gov.
References
- 1.10 Essential Public Health Services Futures Initiative Task Force. 10 Essential Public Health Services. https://phnci.org/national-frameworks/10-ephs. Published 2020. Accessed November 4, 2022.
- 2.Centers for Disease Control and Prevention (CDC). Public health surveillance and data—public health surveillance at CDC. https://www.cdc.gov/surveillance/improving-surveillance/Public-health-surveillance.html. Accessed November 4, 2022.
- 3.Centers for Disease Control and Prevention. Surveillance systems: using surveillance systems to prevent and control chronic diseases. https://www.cdc.gov/chronicdisease/data/surveillance.htm. Accessed November 4, 2022.
- 4.Birkhead GS, Klompas M, Shah NR. Uses of electronic health records for public health surveillance to advance public health. Annu Rev Public Health. 2015;36:345–359. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Public health data modernization executive summary. https://www.cdc.gov/surveillance/pubs-resources/dmi-summary/index.html. Accessed November 4, 2022.
- 6.Centers for Medicare & Medicaid Services. Promoting interoperability programs. https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms. Accessed November 4, 2022.
- 7.Paul MM, Greene CM, Newton-Dame R, et al. The state of population health surveillance using electronic health records: a narrative review. Popul Health Manag. 2015;18(3):209–216. [DOI] [PubMed] [Google Scholar]
- 8.Roger VL, Sidney S, Fairchild AL, et al. , on behalf of the American Heart Association Advocacy Coordinating Committee. Recommendations for cardiovascular health and disease surveillance for 2030 and beyond: a policy statement from the American Heart Association. Circulation. 2020;141(9):e104–e119. [DOI] [PubMed] [Google Scholar]
- 9.National Association of Chronic Disease Directors. Multi-State EHR-Based Network for Disease Surveillance (MENDS). https://chronicdisease.org/page/MENDSinfo. Accessed November 4, 2022.
- 10.National Association of Chronic Disease Directors. Chronic disease competencies. https://chronicdisease.org/page/competencies. Accessed November 4, 2022.
- 11.Kraus EK, Brand B, Hohman KH, Baker EL. New directions in public health surveillance: using electronic health records to monitor chronic disease. J Public Health Manag Pract. 2022;28(2):203–206. [DOI] [PubMed] [Google Scholar]
- 12.Electronic medical record Support for Public health (ESP). Home page. https://www.esphealth.org. Accessed November 4, 2022.
- 13.PopMedNet™. Home page. https://www.popmednet.org. Accessed November 4, 2022.
- 14.Electronic medical record Support for Public health (ESP). RiskScape. https://www.esphealth.org/riskscape. Accessed November 4, 2022.
- 15.Vogel J, Brown JS, Land T, Platt R, Klompas M. MDPHnet: secure, distributed sharing of electronic health record data for public health surveillance, evaluation, and planning. Am J Public Health. 2014;104(12):2265–2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davies M, Erickson K, Wyner Z, Malenfant JM, Rosen R, Brown J. Software-enabled distributed network governance: the PopMedNet experience. EGEMS (Wash DC). 2016;4(2):1213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cocoros NM, Kirby C, Zambarano B, et al. RiskScape: a data visualization and aggregation platform for public health surveillance using routine electronic health record data. Am J Public Health. 2021;111(2):269–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Public Health Informatics Institute. Leveraging clinical data for public health and hypertension surveillance. https://phii.org/wp-content/uploads/2021/06/Leveraging-Clinical-Data-for-Public-Health-and-Hypertension-Surveillance-20180123.pdf. Published 2018. Accessed November 4, 2022.
- 19.HL7® FHIR®: Release 4. https://www.hl7.org/fhir/index.html. Accessed November 4, 2022.
- 20.Centers for Disease Control and Prevention. Data Modernization Initiative. https://www.cdc.gov/surveillance/surveillance-data-strategies/data-IT-transformation.html. Accessed November 4, 2022.
- 21.US Government. Federal data strategy: leveraging data as a strategic asset. https://strategy.data.gov. Accessed November 4, 2022.
- 22.Public Health Informatics Institute. Multi-State EHR-Based Network for Disease Surveillance (MENDS) governance principles, policies, and processes. https://chronicdisease.org/wp-content/uploads/2021/07/MENDS_Governance_Document_V2_approved.pdf. Published 2021. Accessed November 4, 2022.
- 23.Observational Medical Outcomes Partnership (OMOP) Common Data Model. https://ohdsi.github.io/CommonDataModel. Accessed November 4, 2022.
- 24.The National Patient-Centered Clinical Research Network (PCORnet®). Data. https://pcornet.org/data. Accessed November 4, 2022.
- 25.HL7 International. Consolidated Clinical Document Architecture (C-CDA®) (HL7 CDA® RT Implementation Guide: Consolidated CDA Templates for Clinical Notes—US Realm). http://www.hl7.org/implement/standards/product_brief.cfm?product_id=492. Accessed November 4, 2022.
- 26.Electronic medical record Support for Public health (ESP). ESP algorithms. https://espnet.atlassian.net/wiki/spaces/EP/pages/93585410/ESP+Algorithms. Accessed November 4, 2022.
- 27.National Association of Chronic Disease Directors. MENDS hypertension indicator documentation. https://public.3.basecamp.com/p/WNt21XSim7prLbG59estg6v3. Accessed November 4, 2022.
- 28.eCQI Resource Center. Statin therapy for the prevention and treatment of cardiovascular disease. https://ecqi.healthit.gov/ecqm/ec/2021/cms347v4. Accessed November 4, 2022.
- 29.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System. https://www.cdc.gov/brfss/index.html. Accessed November 4, 2022.
- 30.Klompas M, Cocoros NM, Menchaca JT, et al. State and local chronic disease surveillance using electronic health record systems. Am J Public Health. 2017;107(9):1406–1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.US Census Bureau. American Community Survey. https://www.census.gov/programs-surveys/acs. Published 2018. Accessed November 4, 2022.
- 32.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. https://www.cdc.gov/nchs/nhanes/index.htm. Accessed November 4, 2022.
- 33.Heisey-Grove D, Wall HK, Helwig A, Wright JS; Centers for Disease Control and Prevention. Using electronic clinical quality measure reporting for public health surveillance. MMWR Morb Mortal Wkly Rep. 2015;64(16):439–442. [PMC free article] [PubMed] [Google Scholar]
- 34.GitHub, Inc. eCR Now. https://github.com/drajer-health/eCRNow. Accessed November 4, 2022.
- 35.Horth RZ, Wagstaff S, Jeppson T, et al. Use of electronic health records from a statewide health information exchange to support public health surveillance of diabetes and hypertension. BMC Health. 2019;19(1):1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.German RR, Lee LM, Horan JM, et al. Updated guidelines for evaluating public health surveillance systems: recommendations from the Guidelines Working Group. MMWR Recomm Rep. 2001;50(RR-13):1–35. [PubMed] [Google Scholar]
- 37.Nasuti L, Andrews B, Li W, Wiltz J, Hohman KH, Patanian M. Using latent class analysis to inform the design of an EHR-based national chronic disease surveillance model [published online ahead of print May 3, 2022]. Chronic Illn. doi:10.1177/17423953221099043. [DOI] [PMC free article] [PubMed] [Google Scholar]