Abstract
Objectives
The treatments for high-grade non-muscle invasive bladder cancer (NMIBC) vary between bladder preserving intravesical approaches and radical cystectomy. The impact of these treatments on health-related quality of life may vary widely. The purpose of this study was to elicit the general public’s perspective on quality of life, measured as utility scores associated with treatment for Bacillus Calmette-Guerin (BCG)-unresponsive NMIBC and disease progression, for supporting economic evaluation of newly developed treatments for NMIBC.
Materials and Methods
Part I involved the development and testing of health states describing NMIBC, which was informed by a rapid review, expert input and a patient advisor. Part II involved elicitation of societal utility values for the different health states. Time trade-off (TTO) interviews were conducted with members of the UK general public. Five health states described different NMIBC scenarios including disease recurrence and progression. Participants ranked each health state, followed by the TTO valuation exercise. Descriptors included NMIBC symptom severity, impact and treatment characteristics.
Results
In total, 202 members of the general public participated. The mean age was 46 (standard deviation [SD] 14.6) years. Sample mean (SD) EQ-5D-5L visual analogue scale (VAS) and index scores were 83.2 (12.3) and 0.89 (0.18), respectively. Mean utilities were 0.781 for No High-Grade Recurrence, 0.586 for High-Grade Recurrence, 0.572 for > 1-Year Post-cystectomy and 0.283 for metastatic disease. The First Year Post-cystectomy path health state had a mean utility of 0.288. Pairwise comparisons found statistically significant differences between utilities (p < 0.001), except between High-Grade Recurrence and > 1-Year Post-cystectomy (p = 0.524). There were significant differences in utility scores by age and employment status.
Conclusion
This study provides utility scores for health states describing living with NMIBC, which is associated with a significant health-related quality-of-life burden. These values address an existing gap in available data and have the potential to be used in models evaluating the cost-effectiveness of both current and newly developed treatments for bladder cancer.
Supplementary Information
The online version contains supplementary material available at 10.1007/s41669-023-00392-4.
Key Points for Decision Makers
| This study provides utility scores for non-muscle invasive bladder cancer (NMIBC) health states, associated with a significant health-related quality-of-life burden. |
| We found significant differences between utilities, except between High-Grade Recurrence and > 1-Year Post-cystectomy, there were also significant differences in utility scores by age and employment status. |
| These values address an existing gap in available data and can be used in cost-effectiveness models of current and newly developed treatments for bladder cancer. |
Introduction
Bladder cancer is the most common cancer of the urothelial carcinomas, accounting for 3% of all cancer diagnoses and 3% of all cancer deaths in the United Kingdom (UK) [1, 2]. It is the sixth most common cancer in the United States (US), where it is estimated that approximately 84,000 people were diagnosed in 2021 [3]. About two-thirds of patients are diagnosed with non-muscle invasive bladder cancer (NMIBC), and another third with muscle invasive bladder cancer (MIBC). Whilst MIBC has a poor prognosis, NMIBC is burdensome due to frequent recurrences, frequent interventions and a lasting threat of progressing to MIBC [4]. Typically, NMIBC is treated by trans-urethral resection of bladder tumour (TURBT) with subsequent adjuvant chemotherapy and/or a guideline recommendation for adjuvant intravesical Bacillus Calmette-Guerin (BCG) therapy for up to 3 years in high-risk NMIBC [5, 6]. Patients who present with a high-risk NMIBC often receive BCG instillation as the initial therapy (see European Association of Urology [EAU] guidelines, NMIBC 2022 [6]). Primary cystectomy is advocated for patients with very high features [7]. However, up to half of patients either do not respond to BCG instillation therapy, or their response declines after the initial instillation—thus requiring more advanced interventions [8]. According to European treatment guidelines, the best evidence-based treatment recommendation for patients unresponsive to BCG is radical cystectomy [9]. There is a recognised urgent need for novel agents of treatment for NMIBC that can help slow progression of the illness while sparing the bladder [8].
Approval decisions for new therapies in many markets are based on the relationship between the additional cost and health-related quality-of-life (HRQoL) benefit that the new therapy confers (cost-effectiveness). In order to have a uniform assessment of HRQoL benefit irrespective of the condition and/or treatment, quality-adjusted life-years (QALYs) are most often used. A QALY describes the expected number of life-years generated adjusted for (multiplied) with a QALY weight. This QALY weight is referred to as a “utility” value, where a value of 1 represents perfect health, a value of 0 represents a state equivalent to dead and values less than 0 indicate the state is valued as being worse than dead [10, 11]. The utility score reflects the general population’s preferences for different disease health state descriptions based upon their perceived quality-of-life implications. In that way, the resulting utility scores describe the societal, not necessarily the individual’s, valuation of a health condition and lays the ground for decision-making on allocation of publicly (via taxation) or privately funded healthcare. At present there are limited utility scores describing the treatment pathway of BCG-unresponsive NMIBC patients in a methodologically consistent way. A study assessing utility scores of disease states among NMIBC patients is therefore necessary for assessing the cost-effectiveness of new treatments that have the potential to delay or avoid radical cystectomy. A variety of different approaches can be taken to derive or elicit utility values, and a number of factors can influence their methodological quality or contextual applicability [12]. Vignette-based utility studies are generally employed in situations where no standardised approach is feasible or appropriate to provide suitable data. Vignettes (sometimes referred to as “scenarios” or “health state descriptions”) allow for a depiction of specific health states that can be valued to inform economic decision-making [13].
Data from the BOXIT trial (a pivotal phase III trial) show that there is a decrement to HRQoL associated with NMIBC progression leading to greater healthcare costs [14]. HRQoL is defined by National Institute for Health and Care Excellence (NICE) as “a combination of a person’s physical, mental and social well-being; not merely the absence of disease” [15]. According to a recent cross-sectional survey study, HRQoL was significantly worse in bladder cancer patients in comparison to those with colorectal or prostate cancer, as well as members of the general population [16]. The results from these studies suggest a persistent impact of bladder cancer for patients that extends beyond successful treatment and subsequent recovery. Although the studies previously cited provide insight into HRQoL in patients with NMIBC, the assessment approaches employed do not meet the specific requirements to generate data suitable for inclusion in cost-effectiveness analyses (i.e. utility scores cannot be reliably derived for specific populations using a recognised utility measure or approach).
The purpose of this study was to elicit the general public’s perspective on quality of life, measured as utility scores, associated with treatment for BCG-unresponsive NMIBC and disease progression.
Materials and Methods
Study Design
The study consisted of two primary parts: health state vignette description development (part I) and utility score elicitation (part II). Part II used the time trade-off (TTO) approach [17], which is a methodology appropriate for health technology assessment (HTA) of novel treatments for evidence submission to regulatory agencies, including the NICE [18]. In the health state description development phase (part I), interviews were conducted with urologists to develop bladder cancer health states suitable for the utility elicitation exercise. In addition, a bladder cancer patient advisor reviewed and provided additional feedback on the states. In the second phase of the study (part II), the health states were piloted in face-to-face interviews with members of the general public from the UK, per NICE guidelines [18]. After revisions were made based on the pilot interview feedback, the health states were used in the utility elicitation phase; these health states are detailed in full in “Supplementary File 1” (see the electronic supplementary material). The utility scores were elicited in a TTO task [19] with a 10-year time horizon for chronic health states and a 1-year path state for a transient health state. The TTO task was performed in-person in August 2021 with members of the general public. All procedures and materials were approved by an independent institutional review board (Ethical & Independent Review Services; study number 21084).
Health State Development
A rapid review was conducted to develop a clinician interview guide and ensure the health states were consistent with published research on the impact of the condition and its treatment. The review focused on bladder cancer treatments and associated side effects, and disease progression. It was based on papers delivered by Ferring and Google scholar search. Two rounds of telephone interviews were conducted with three urologists who all had significant clinical experience treating patients with bladder cancer. The first round of interviews identified common treatments and monitoring procedures, symptoms, and side effects routinely observed in clinical practice. Draft health states were then developed using lay-person terminology to be easily comprehended by the general public. This approach involved researchers experienced in the process of creating patient-facing materials carefully assessing the language used to ensure that the required reading age (Flesch-Kincaid Grade) was minimised. In the second round of interviews, the clinicians reviewed the draft health states to assess their accuracy and suggest changes, as appropriate. After the second round, the health state content was edited to represent a typical patient experience. Subsequently, a patient advisor reviewed the draft health states for content validity and acceptability from a patient perspective, and changes were made based on their feedback. The health states developed included:
- Chronic (valued in the TTO task with a 10-year time horizon)
-
oT: No High-Grade Recurrence
-
oL: High-Grade Recurrence
-
oW: > 1-Year Post-cystectomy
-
oH: MIBC with Metastatic Disease
-
o
- Path (valued in the TTO task with a 1-year time horizon)
-
oD: First Year Post-cystectomy (male)
-
oG: First Year Post-cystectomy (female)
-
o
Each health state was represented by a random letter to avoid any complications resulting from the perceived ordering of states. The NMIBC No High-Grade Recurrence health state reflects patients who are on, or have received, a treatment that controls the tumour and the disease (health state T). The NMIBC High-Grade Recurrence state (health state L) represented a situation where the tumour has stopped responding to the previous treatment and therefore the next line of treatment should be considered. Although the recommended further treatment is typically radical cystectomy, it is theoretically possible that patients receive another bladder-sparing therapy, e.g. further cytotoxic instillation therapy or repeated TURBT.
Those patients who undergo radical cystectomy, either as recurrent NMIBC or MIBC patients, will face perioperative implications on their functioning and quality of life. This perioperative period is set to 1 year (a path health state) to incorporate immediate surgery-related complications and adaptations in daily life. Two different state vignettes were developed to reflect outcomes specific to either men (health state D) or women (health state G).
In a longer time perspective, it is expected that patients having undergone radical cystectomy have fully adapted to their new chronic health state W: > 1-Year Post-cystectomy.
Muscle invasive disease is represented by health state H since patients not undergoing radical cystectomy most likely will develop metastatic disease. Although other bladder-sparing treatments for these patients exist (e.g. radiotherapy and systemic chemotherapy), the prognosis is worse than for NMIBC.
Participants
Participants included in the study were individuals drawn from the UK general public, aged 18 years or older and that were willing to provide written informed consent. Participants responded to regional advertisements and attended one of the study locations where screening took place. Participants were required to demonstrate a minimally acceptable level of cognitive ability to perform the utility elicitation interview, which was judged by the interviewer. Individuals who had previously been diagnosed with any form of bladder cancer, or who currently had any other form of cancer, were excluded from taking part. This step was taken to minimise the impact of personal experience of cancer influencing valuations. Eligible individuals undertook the interview activities face-to-face with an experienced researcher using specially prepared TTO props.
Pilot Study
A background information section on previous treatment experiences prior to developing BCG-unresponsive tumour was developed for participants to read before reviewing the health states. Vignette-based health state utility valuation studies are typically conducted with “chronic” health states, which change over a longer time period. Health states that change over a short time period are called “path states” or “path health states”. In the current study, all health states, apart from First Year Post-cystectomy (D/G), were chronic health states, to be used in a TTO task with a 10-year time horizon. The health state that incorporated the radical cystectomy surgery and recovery time was developed as a path state, to be used in a TTO task with a 12-month time horizon.
To assess the comprehension of the health states and utility exercise feasibility, a pilot study was conducted with members of the general public. Health state descriptions were piloted in two rounds of interviews with 30 participants. At the start of the interview, participants were asked to review the background section and health state descriptions. Participants ranked the health states in their preferred order and completed the TTO exercise with the interviewer. Participants were asked for feedback on health state wording and to discuss any differences between the health states. Round 1 participant feedback (n = 14 participants) was incorporated into health state descriptions presented to round 2 participants (n = 16). After the second round of the interviews, the health states were finalised for use in the main study. The pilot study confirmed that the ranking and TTO tasks were feasible for all respondents, with participants indicating that the health states were clear and comprehensible.
Interview Procedures
Each participant attended one interview session. Interviewers were trained by senior researchers with extensive experience in conducting TTO interviews. The interviewers conducted the interviews using a standardised script and started by confirming participant eligibility prior to obtaining consent. Participants were then asked to read the background information sheet detailing NMIBC. To familiarise participants with the health states and their descriptions, participants were asked to read and then rank them based on their preferences, from best to worst. These rankings were recorded by the interviewer for each health state. The health states were presented to the participants in random order before their initial ranking exercise.
Next, participants completed the TTO exercise [19]. The participants were offered a choice between spending 10 years (or 12 months for health states D and G) in the described impaired health state or spending varying amounts of time in full health. If the participant indicated they preferred to die than live in the health state, they were given the choice between dead and a 10-year period (or a 12-month period for health states D and G) that started with varying amounts of time in the specific health state, followed by full health for the remainder of the 10 years. The utility score for each health state was elicited when the participant was indifferent between the two choices as it was the point where the participant was willing to trade off a certain number of life-years in the health state to attain full health (albeit for fewer life-years). Interviews typically lasted approximately 45–60 min. Finally, sociodemographic and clinical forms and the EQ-5D-5L questionnaire were completed. [20] The EQ-5D-5L is a generic measure of HRQoL that can be administered to adults to assess overall health status.
Statistical Analysis Procedures
Statistical analyses were completed using SAS® (version 9.4). Continuous variables, including utilities and differences between health state utilities, were summarised by mean, standard deviation (SD), minimum and maximum values. Categorical variables, such as gender and race, are presented by frequencies and percentages. Pairwise comparisons were performed using t tests to compare utility scores between all health states. Utilities and difference scores were calculated separately for subgroups of participants. These analyses examined whether preferences for various health states differed between the subgroups of participants’ employment (employed vs. not employed), sex (male vs. female), level of education attainment (more educated; university level and higher, the median education level of the sample vs. less educated; vocational level and below) and age (younger [≤ 55 years old] vs. older [> 55 years old]).
To characterise the sample in terms of quality-of-life impact, descriptive analyses were conducted to summarise EQ-5D-5L scores. Utility scored were generated via the 5D-3L crosswalk algorithm by van Hout and colleagues [21] in line with NICE recommendations [22].
Results
Demographic Characteristics and EQ-5D-5L Scores
Details of the demographic characteristics and EQ-5D-5L scores are shown in Table 1.
Table 1.
Demographic and clinical characteristics
| Demographic characteristics | Total sample (N = 202) |
|---|---|
| Mean age (SD) | 46.0 (14.6) |
| Min. age | 19 |
| Max. age | 81 |
| Sex at birth: female, N (%) | 92 (45.5%) |
| Racial background, N (%) | |
| White | 107 (53.0%) |
| Mixed/multiple ethnic groupsa | 20 (9.9%) |
| Asian | 28 (13.9%) |
| African, Caribbean or Black | 43 (21.3%) |
| Otherb | 4 (2.0%) |
| Marital statusc, N (%) | |
| Not married | 109 (54.0%) |
| Married/cohabitating/living with partner | 93 (46.0%) |
| Employment status, N (%) | |
| Full-time work | 100 (49.5%) |
| Part-time work | 43 (21.3%) |
| Self-employed | 20 (9.9%) |
| Homemaker | 1 (0.5%) |
| Unemployed | 7 (3.5%) |
| Retired | 21 (10.4%) |
| Disabled | 1 (0.5%) |
| Student | 9 (4.5%) |
| Education level, N (%) | |
| No formal qualifications | 1 (0.5%) |
| GCSE/O' levels or equivalent | 18 (8.9%) |
| A' levels or equivalent | 33 (16.3%) |
| Vocational/work-based qualifications | 25 (12.4%) |
| University degree (BA, BSc) | 82 (40.6%) |
| Postgraduate degree (MA, PhD, PGCE) | 43 (21.3%) |
| EQ-5D-5L VAS score, mean (SD) | 83.17 (12.28) |
| EQ-5D-5L index score, mean (SD) | 0.89 (0.18) |
Max maximum, min minimum, SD standard deviation, VAS visual analogue scale
aMixed ethnic/racial background includes White and Black Caribbean (7), White and Black African (1), White and Asian (5), preferred not to say (2) and other mixed/multiple ethnic groups as reported by respondents (5)
bOther ethnic/racial background in the general public sample includes African/Indian (1), Arab (1), Indian (1) and Hispanic (1)
cNot married includes single, divorced, separated and widowed
Health State Utilities
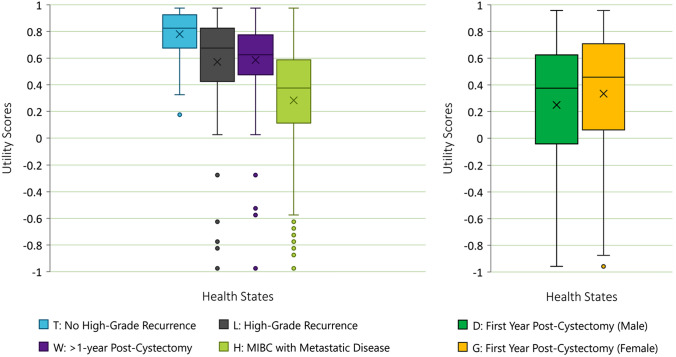
In the introductory ranking task, participants ranked the health states from least to most preferable to live in for a period of 10 years. Of these, the majority of the participants ranked health state T: No High-Grade Recurrence as the most preferable (n = 199, 98.5%). Conversely, health state H: MIBC with Metastatic Disease was ranked as least preferable by the majority of participants (n = 179, 88.6%). In review of the utility scores obtained, health state T: No High-Grade Recurrence had the highest mean (SD) utility value at 0.781 (0.166), followed by L: High-Grade Recurrence at 0.586 (0.289), W: > 1-Year Post-cystectomy at 0.572 (0.358), combined path health state D/G: First Year Post-cystectomy at 0.288 (0.509), and H: MIBC with Metastatic Disease at 0.283 (0.454), see Table 2. Box plots illustrating the variance in utility values between each of the health states are shown in Fig. 1. Utility scores for NMIBC health states are shown in further detail in Supplementary Table 1 (see the electronic supplementary material).
Table 2.
Differences between health state utility scoresa (Student’s t tests)
| Health states | Mean (SD) of health state | Mean (SD) difference score | Mean (SD) difference score younger (mean age 38) vs. older (mean age 64) |
|---|---|---|---|
| Chronic health states (N = 202) | |||
| T: no high-grade recurrence | 0.78 (0.17) | 0.19*(0.25) |
Younger = 0.16 (0.19) Older = 0.27 (0.36)* |
| L: high-grade recurrence | 0.59 (0.29) | ||
| T: no high-grade recurrence | 0.78 (0.17) | 0.21* (0.32) |
Younger = 0.19 (0.29) Older = 0.25 (0.39) |
| W: > 1-year post-cystectomy | 0.57 (0.36) | ||
| T: no high-grade recurrence | 0.78 (0.17) | 0.50* (0.43) |
Younger = 0.45 (0.40) Older = 0.61 (0.49)* |
| H: MIBC with metastatic disease | 0.28 (0.45) | ||
| L: high-grade recurrence | 0.59 (0.29) | 0.01 (0.31) |
Younger = 0.03 (0.28) Older = −0.02 (0.39) |
| W: > 1-year post-cystectomy | 0.57 (0.36) | ||
| L: high-grade recurrence | 0.59 (0.29) | 0.30* (0.36) |
Younger = 0.29 (0.36) Older = 0.34 (0.36) |
| H: MIBC with metastatic disease | 0.28 (0.45) | ||
| W: > 1-year post-cystectomy | 0.57 (0.36) | 0.29 * (0.39) |
Younger = 0.26 (0.39) Older = 0.36 (0.40)* |
| H: MIBC with metastatic disease | 0.28 (0.45) | ||
| Path health statesb | |||
| D: (male) first year post-cystectomy (N = 110) | 0.25 (0.50) | − 0.08 (0.51) | – |
| G: (female) first year post-cystectomy (N = 92) | 0.33 (0.52) | ||
MIBC muscle invasive bladder cancer, SD standard deviation, TTO time trade-off
*p < 0.05
aTTO scores are on a scale anchored with 0 representing dead and 1 representing full health
bPath health states D and G comparison is an independent t test between males and females. All other comparisons are paired t tests
Fig. 1.
Box plots of NMIBC health state utility scores. The box plot shows minimum, lower quartile, median, mean, upper quartile and maximum utility scores for each of the health states including outliers (defined as 1.5 times the interquartile range larger than the third quartile or 1.5 times the interquartile range smaller than the first quartile). MIBC muscle invasive bladder cancer, NMIBC non-muscle invasive bladder cancer
Pairwise comparisons were performed with chronic health states using t tests (Table 2). All health state comparisons were significantly different (p < 0.001), except for L: High-Grade Recurrence and W: > 1-Year Post-cystectomy (p = 0.524). Findings from an independent t test comparing path health states D (male) and G (female) were not significant (p = 0.241).
Furthermore, pairwise comparisons of differences between each health state utility score were compared within subgroups. There were significant differences in utility score differences by age group between health states T and L, T and H, as well as for health states W and H. There were no statistically significant differences in utility difference scores by sex, employment or education level.
Subgroup analyses for each health state exclusively were carried out. For the subgroups of younger and older participants, there were statistically significant differences (p < 0.05) in utility scores for chronic health states W: > 1-Year Post-cystectomy (younger = 0.621, older = 0.498,) and H: MIBC with Metastatic Disease (younger = 0.334, older = 0.157). For the path health state D/G: First Year Post-cystectomy, there was a significant difference by age (younger = 0.346, older = 0.143) and among females (younger = 0.437, older = 0.072) but not in males. Additionally, utility scores for T: No High-Grade Recurrence were significantly different by employment status (employed = 0.770, not employed = 0.824). There were no other significant differences in utility score comparisons when reviewing sex or education level differences.
The majority of participants were willing to trade time for all health states, indicating the health states are associated with substantial burden to quality of life. Participants were least willing to trade time for T: No High-Grade Recurrence (n = 31, 15.3%), which was ranked as the most preferable. More than a quarter of participants rated D/G: First Year Post-cystectomy as equal to (n = 55, 27.2%) or worse than dead. A sizable minority of participants rated H: MIBC with Metastatic Disease as equal to (n = 1, 0.5%) or worse than dead (n = 34, 16.8%). These results demonstrate the magnitude of HRQoL burden the general public perceives these health states to be associated with. Compared to younger participants, a larger proportion of older participants rated H: MIBC with Metastatic Disease (younger: n = 20, 13.9%; older: n = 14, 24.1%) and D/G: First Year Post-cystectomy (younger: n = 34, 23.6%; older: n = 19, 32.8%) as worse than dead.
Discussion
A vignette-based utility elicitation study was conducted with health states mimicking the treatment pathway of a cohort of BCG-unresponsive patients. This began with a health state where the tumour is responding to the treatment, then non-responding, potentially undergoing radical cystectomy and/or progress to MIBC with metastatic disease.
Preferences for the health states varied, but utilities generally followed expected patterns—the more severe bladder cancer health states resulted in lower utility scores. Health state H: MIBC with Metastatic Disease had a substantially lower mean utility than the utilities of the other chronic health states, highlighting the extreme impact of metastatic bladder cancer on HRQoL. Mean utility scores ranged from 0.781 for T: No High-Grade Recurrence to 0.283 for H: MIBC with Metastatic Disease. Similar values for metastatic disease in other primary tumours have been previously reported, with one study showing a colorectal cancer metastatic (progressive) utility score of 0.21. [23] The path health state D/G: First Year Post-cystectomy had a utility score similar to the MIBC with Metastatic Disease health state at 0.288. These results demonstrate the added value of delaying the need for radical cystectomy to treat high-risk NMIBC—keeping the patient in a more highly valued health state for a longer time compared to the other health states. In fact, almost one-sixth of the respondents did not want to trade any amount of time in the T: No High-Grade Recurrence health state.
This study was conducted with members of the general public and not NMIBC patients. This is an accepted approach by HTA agencies, including NICE [18]. The debate of experiential versus hypothetical societal utility scores is ongoing, but it is generally agreed that the preferences of the public who fund the healthcare system need to incorporated. The systematic review and meta-analysis from Peeters and Stiggelbout [24] presented a comparison of health state scores derived from patient and general public samples. Higher utility scores are occasionally seen in patients compared to the general public. More recently, Ludwig and colleagues [25] demonstrated patient preferences that differed from general public preferences, where patients reported more concern about functional aspects than about pain and anxiety when compared to the general public. Another recent study [26] showed minimal differences in utility scores between general public and patient samples when utility scores were collected using the same health states for both groups. It could furthermore be argued that due to the vignette-based methodology used in the study, it places a limit on its ecological validity. Until a more definitive answer to the question of experiential versus general public utilities is found, we suggest collecting and presenting utilities in the most robust manner possible and in line with guidance issued on best practice [27].
Another possible study limitation is generalisability. While efforts were made to ensure that no demographic group was overrepresented, generalisability to the broader UK population was difficult to achieve as data collection occurred during the coronavirus disease 2019 (COVID-19) pandemic. As such, data collection was limited largely to London, which has a higher proportion of ethnic minority individuals compared to the UK as a whole. The study sample had a much higher proportion of African, Caribbean or Black and Asian individuals than both the general UK population and the general London population [28, 29]. The possibility exists that cultural differences attached to race may have affected the resulting utility scores. In review of other characteristics, the study sample mimics the UK general public for marital status [28] and employment [29], but their education level skewed higher than that found in the UK census data [28]. However, the most recent UK census data (2011) may lag recent efforts to increase accessibility to a university education: the Department for Education reported that for 2017–2018, over half of young people in the UK were continuing on to university [30]. The study sample’s EQ-5D health scores were comparable to general public samples [31], although it should be noted the current study used the EQ-5D-5L, and public norms present results using the EQ-5D-3L. While the study sample’s race was arguably not generalisable to the UK public, the study sample’s age, gender, employment status, overall health and marital status were, minimising the effect of the race differential. Use of statistical techniques such as multiple regression could be employed to further examine the extent to which these factors could have influenced the values obtained.
The path health state (represented in health states D [men] and G [women] covering radical cystectomy surgery and the 12 months post-surgery) has a shorter, 1-year time horizon, making it difficult to compare against the chronic health states with their 10-year time horizon. A longer time horizon would not be appropriate due to the short-term or changing nature of the health state. One-year post-cystectomy, patients have recovered significantly from the procedure, adjusted to their new condition, and have a much-improved quality of life. Due to the differences in time horizons, it is not recommended to compare utility scores between path and chronic health states.
Despite these limitations, the use of vignettes is a widely accepted approach for estimating utilities associated with a range of health conditions [26]. Other generic preference-based measures, such as the 12-item Short Form Health Survey (SF-12) [32] or EQ-5D-5L, are not sensitive enough to capture the treatment and monitoring impacts of NMIBC, such as quarterly TURBTs. This is seen recently in a cross-sectional study with bladder cancer patients, which utilised the EORTC QLQC30 [33] to estimate utility scores [34]. The utility scores in this survey were much higher than seen in our study, most likely due to the generic nature of the questionnaire, which does not measure some of the impacts specific to bladder cancer.
Further research is required to better understand the HR QoL impact of bladder cancer in general. The present study only partly addresses one specific technical aspect of this shortcoming. The literature review undertaken highlighted a paucity of both good quality quantitative and qualitative research into the impact of the condition and its treatment. Given the significant burden this can present for individuals, efforts should be made to explore this further, in line with the increasing commitment to patient centricity and shared treatment decision-making. At a minimum, routine inclusion of a robust HRQoL assessment approach in future clinical studies should provide a more sound basis for comparison of newly developed treatments.
This original study has provided utility scores for different health states in NMIBC. This addresses an existing gap in the literature and provides potential data suitable for use in models assessing the cost-effectiveness of bladder cancer treatments [27].
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The study team would like to thank and acknowledge Anne Rentz for working as co-principal investigator, Louis Matza for working as senior reviewer and Ella Brookes for her role as project manager. Additionally, the study team would like to thank the interview team consisting of Elizabeth Gibbons, Lucy Hetherington, Dorsa Khazaei, Ashley Duenas, Natasha Ramachandran and Hayley Karn. A special thanks goes to Melanie Costin for her assistance as patient advisor.
Declarations
Funding
This research study and manuscript was conducted and written by Evidera by PPD, being funded in full by Ferring Pharmaceuticals.
Conflict of interest
Owen Alan Edwards Cooper, Natalia Piglowska, Charlie Smith and Paul Swinburn are employees of Evidera PPD, a CRO paid by Ferring Pharmaceuticals A/S to conduct this study. Ola Ghatnekar and Jørn Skibsted Jakobsen are employees of Ferring Pharmaceuticals A/S. James Catto received honoraria for membership of advisory boards for Ferring Pharmaceuticals A/S. Günter Niegisch received consulting fees from Ferring Pharmaceuticals A/S.
Ethics approval
All procedures and materials were approved by an independent institutional review board (Ethical & Independent Review Services; study number 21084). This study was conducted according to the Declaration of Helsinki.
Consent to participate
All participants provided written informed consent before entering the study.
Consent for publication
All authors of this manuscript consented for publication.
Availability of data and material
Health states descriptions are provided in a supplementary file. All other documents will be available on request.
Code availability
Not applicable.
Authors' contributions
All authors meet the requirements for authorship as specified by the International Committee of Medical Journal Editors (ICMJE) guidelines. All authors have read and approved the final version of the manuscript, and agree to be accountable for the work. OC, NP, CS and PS drafted and finalized the manuscript. OG, JC, GN and JSJ reviewed the manuscripts and provided comments.
Contributor Information
Owen Alan Edwards Cooper, Email: Owen.Cooper@evidera.com.
Ola Ghatnekar, Email: Ola.Ghatnekar@ferring.com.
Natalia Piglowska, Email: Natalia.Piglowska@evidera.com.
Charlie A. Smith, Email: Charlie.Smith@evidera.com
Paul Swinburn, Email: Paul.Swinburn@evidera.com.
James W. F. Catto, Email: J.Catto@sheffield.ac.uk
Günter Niegisch, Email: Guenter.Niegisch@med.uni-duesseldorf.de.
Jørn Skibsted Jakobsen, Email: Joern.Jakobsen@ferring.com.
References
- 1.Cancer Research UK. Bladder cancer statistics. [cited 2021 April 1]; https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bladder-cancer#heading-Zero. Accessed 26 Aug 2021.
- 2.Cumberbatch MGK, Jubber I, Black PC, Esperto F, Figueroa JD, Kamat AM, et al. Epidemiology of bladder cancer: a systematic review and contemporary update of risk factors in 2018. Eur Urol. 2018;74(6):784–795. doi: 10.1016/j.eururo.2018.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Urology Care Foundation. Non-muscle Invasive Bladder Cancer. [cited 2021 August 26]; https://www.urologyhealth.org/urology-a-z/n/non-muscle-invasive-bladder-cancer. Accessed 26 Aug 2021.
- 4.Noon AP, Albertsen PC, Thomas F, Rosario DJ, Catto JW. Competing mortality in patients diagnosed with bladder cancer: evidence of undertreatment in the elderly and female patients. Br J Cancer. 2013;108(7):1534–1540. doi: 10.1038/bjc.2013.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Babaian KN, Adams PG, McClure C, Tompkins B, McMurray M. Bacillus Calmette-Guérin immunotherapy for bladder cancer overview of BCG immunotherapy. 2020 [updated 2020; cited 2021 September 20]; https://emedicine.medscape.com/article/1950803-overview. Accessed 26 Aug 2021.
- 6.EAU Pocket Guidelines. Edn. presented at the EAU Annual Congress Amsterdam. 2022.
- 7.Catto JWF, Gordon K, Collinson M, Poad H, Twiddy M, Johnson M, et al. Radical cystectomy against intravesical BCG for high-risk high-grade nonmuscle invasive bladder cancer: results from the randomized controlled BRAVO-feasibility study. J Clin Oncol. 2021;39(3):202–214. doi: 10.1200/JCO.20.01665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rayn KN, Hale GR, Grave GP, Agarwal PK. New therapies in nonmuscle invasive bladder cancer treatment. Indian J Urol. 2018;34(1):11–19. doi: 10.4103/iju.IJU_296_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.European Association of Urology. Non-muscle-invasive Bladder Cancer. 2021 [updated 2021; cited 2021 October 13]; https://uroweb.org/guideline/non-muscle-invasive-bladder-cancer/#7_4. Accessed 26 Aug 2021.
- 10.Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull. 2010;96:5–21. doi: 10.1093/bmb/ldq033. [DOI] [PubMed] [Google Scholar]
- 11.Torrance GW. Utility approach to measuring health-related quality of life. J Chronic Dis. 1987;40(6):593–603. doi: 10.1016/0021-9681(87)90019-1. [DOI] [PubMed] [Google Scholar]
- 12.Zoratti, et al. Evaluating the conduct and application of health utility studies: a review of critical appraisal tools and reporting checklists. Eur J Health Econ. 2021;22:723–733. doi: 10.1007/s10198-021-01286-0. [DOI] [PubMed] [Google Scholar]
- 13.Matza, et al. Vignette-based utilities: usefulness, limitations, and methodological recommendations. Value Health. 2021;24(6):812–821. doi: 10.1016/j.jval.2020.12.017. [DOI] [PubMed] [Google Scholar]
- 14.Cox E, Saramago P, Kelly J, Porta N, Hall E, Tan WS, et al. Effects of bladder cancer on UK Healthcare costs and patient health-related quality of life: evidence from the BOXIT trial. Clin Genitourin Cancer. 2020;18(4):e418–e442. doi: 10.1016/j.clgc.2019.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Institute for Health and Care Excellence. Glossary. [cited 2022 April 28]; https://www.nice.org.uk/glossary?letter=h. Accessed 26 Aug 2021.
- 16.Catto JWF, Downing A, Mason S, Wright P, Absolom K, Bottomley S, et al. Quality of life after bladder cancer: a cross-sectional survey of patient-reported outcomes. Eur Urol. 2021;79(5):621–632. doi: 10.1016/j.eururo.2021.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Torrance GW, Thomas WH, Sackett DL. A utility maximization model for evaluation of health care programs. Health Serv Res. 1972;7(2):118–133. [PMC free article] [PubMed] [Google Scholar]
- 18.National Institute for Health and Care Excellence. Guide to the methods of technology appraisal 2013. April 2013 [updated April 2013; cited March 2022]; https://www.nice.org.uk/process/pmg9/chapter/foreword. Accessed 26 Aug 2021. [PubMed]
- 19.Lugner AK, Krabbe PFM. An overview of the time trade-off method: concept, foundation, and the evaluation of distorting factors in putting a value on health. Expert Rev Pharmacoecon Outcomes Res. 2020;20(4):331–342. doi: 10.1080/14737167.2020.1779062. [DOI] [PubMed] [Google Scholar]
- 20.Rabin R, Gudex C, Selai C, Herdman M. From translation to version management: a history and review of methods for the cultural adaptation of the EuroQol five-dimensional questionnaire. Value Health. 2014;17(1):70–76. doi: 10.1016/j.jval.2013.10.006. [DOI] [PubMed] [Google Scholar]
- 21.van Hout B, Janssen MF, Feng YS, Kohlmann T, Busschbach J, Golicki D, et al. Interim scoring for the EQ-5D-5L: mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health. 2012;15(5):708–715. doi: 10.1016/j.jval.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 22.Position statement on use of the EQ-5D-5L value set for England (updated October 2019)|Technology appraisal guidance|NICE guidance|Our programmes|What we do|About|NICE
- 23.Best JH, Garrison LP, Hollingworth W, Ramsey SD, Veenstra DL. Preference values associated with stage III colon cancer and adjuvant chemotherapy. Qual Life Res. 2010;19(3):391–400. doi: 10.1007/s11136-010-9589-5. [DOI] [PubMed] [Google Scholar]
- 24.Peeters Y, Stiggelbout AM. Health state valuations of patients and the general public analytically compared: a meta-analytical comparison of patient and population health state utilities. Value Health. 2010;13(2):306–309. doi: 10.1111/j.1524-4733.2009.00610.x. [DOI] [PubMed] [Google Scholar]
- 25.Ludwig K, Ramos-Goni JM, Oppe M, Kreimeier S, Greiner W. To what extent do patient preferences differ from general population preferences? Value Health. 2021;24(9):1343–1349. doi: 10.1016/j.jval.2021.02.012. [DOI] [PubMed] [Google Scholar]
- 26.Matza LS, Deger KA, Vo P, Maniyar F, Goadsby PJ. Health state utilities associated with attributes of migraine preventive treatments based on patient and general population preferences. Qual Life Res. 2019;28(9):2359–2372. doi: 10.1007/s11136-019-02163-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Brazier J, Ara R, Azzabi I, Busschbach J, Chevrou-Séverac H, Crawford B, et al. Identification, review, and use of health state utilities in cost-effectiveness models: an ISPOR good practices for outcomes research task force report. Value Health. 2019;22(3):267–275. doi: 10.1016/j.jval.2019.01.004. [DOI] [PubMed] [Google Scholar]
- 28.Office for National Statistics. Nomis. [cited 2021 October 25]; https://www.nomisweb.co.uk/. Accessed 26 Aug 2021.
- 29.Office for National Statistics. Coronavirus (COVID-19). [cited 2021 October 25]; https://www.ons.gov.uk/. Accessed 26 Aug 2021.
- 30.BBC News. The symbolic target of 50% at university reached. 2019 [updated 2019; cited 2021 October 25]; Available from: https://www.bbc.com/news/education-49841620. Accessed 26 Aug 2021.
- 31.Janssen B, Cabases J, Szende A. Self-reported population health: An international perspective based on EQ-5D. Dordrecht: Springer; 2014. [PubMed] [Google Scholar]
- 32.Jenkinson C, Layte R. Development and testing of the UK SF-12 (short form health survey) J Health Serv Res Policy. 1997;2(1):14–18. doi: 10.1177/135581969700200105. [DOI] [PubMed] [Google Scholar]
- 33.Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993;85(5):365–376. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- 34.Smith AB, McCabe S, Deal AM, Guo A, Gessner KH, Lipman R, et al. Quality of life and health state utilities in bladder cancer. Bladder Cancer. Preprint:1–6. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.