Highlights
-
•
Vulvar carcinoma and Herpes Simplex Virus (HSV) are found more frequently in women with Human Immunodeficiency Virus (HIV).
-
•
When examining a vulvar lesion, a high index of suspicion for vulvar carcinoma should be maintained.
-
•
Repeat biopsies should be performed whenever there is concern for failure of treatment course for an infectious lesion.
-
•
The mainstays of treatment for HSV lesions include surgical and oral antiviral/immunomodulating agents.
-
•
Five percent of patients with HIV and HSV will have HSV resistant to antiviral agents.
Keywords: Vulvar carcinoma, Herpes simplex virus, Human immunodeficiency virus
Abstract
Patients with human immunodeficiency virus (HIV) are at increased risk for developing other gynecologic conditions, including herpes simplex virus (HSV) and vulvar intraepithelial neoplasia (VIN)/carcinoma. We describe the case of a woman with a history of microinvasive vulvar squamous cell carcinoma who presented with hypertrophic ulcerated vulvar and peri-anal masses concerning for malignancy. This case highlights the need to maintain a high index of suspicion for malignancy and herpes simplex virus, even with negative polymerase chain reaction (PCR) test, as well as the difficulty of treating this often-resistant lesion.
1. Introduction
Vulvar carcinoma affects approximately 6,000 women each year in the United States. Risk factors for development include human papillomavirus infection, immunodeficiency, and vulvar or cervical intraepithelial neoplasia (VIN, CIN). The presentation of vulvar carcinoma can be mistaken for dermatologic conditions and sexually transmitted infections, and it can also be easily overlooked in the absence of a detailed physical exam or patient-reported symptoms. The presence of herpes simplex virus (HSV) in vulvar biopsies for VIN and vulvar carcinoma has been previously identified (Jasim et al., 2016). Likewise, HSV has been described to mimic and mask the diagnosis of VIN and vulvar carcinoma (Strehl et al., 2012, Frimer et al., 2011). In the workup of suspicious lesions, biopsy and infectious testing are crucial. We describe the case of a woman with a history of vulvar carcinoma and poorly controlled Human Immunodeficiency Virus (HIV) who presented with recurrent lesions suspicious for recurrence, requiring high degree of suspicion and repetitive thorough workup.
2. Case report
A 66 year-old woman with a history of HIV, microinvasive vulvar squamous cell carcinoma (SCC) and VIN 3 was treated with a partial radical vulvectomy-four years prior. Postoperatively, she had wound complications including ulcerations, drainage and inability to heal, requiring surgical debridement twice over an 11 month time period. As the pathology in the original vulvectomy was consistent with vulvar SCC and the patient was immune suppressed, there was concern for cancer recurrence, but biopsies repeatedly showed benign squamous epithelial hyperplasia. She was then lost to follow up for 2 years, after which time she had a normal office vulvar exam without lesions when she returned. Of note, she had been noncompliant with highly active anti-retroviral therapy (HAART).
Three years after her initial surgery, the patient presented to her Infectious Disease specialist with 2 weeks of vulvar itching and yellow discharge, her examination showed multiple ulcerated vulvar lesions and perianal lesions with purulent drainage (Fig. 1) and was immediately sent to the Emergency Department for further evaluation. Given the appearance of athe lesions, there was again concern for cancer recurrence, with possible superimposed infection. A genital HSV PCR culture was collected, broad spectrum antibiotics and valacyclovir were started, and the patient was taken to the operating room for examination under anesthesia and vulvar biopsies.
Fig. 1.
Intraoperative gross appearance of vulvar lesions. A. Entire vulvar and peri-anal view of multiple lesions. B. peri-anal ulcerated mass with hypopigmented and de-epithelialized tissue extending to the posterior fourchette. C. peri-clitoral 3 cm ulcerated mass, which was draining thick purulent material on presentation, with separate vesicular and ulcerated lesion inferior.
Serum HSV PCR, serum syphilis screen, and vulvar bacterial culture were negative, and biopsy results showed benign squamous epithelium with extensive acute and chronic inflammation and ulceration with granulation tissue and pseudoepitheliomatous hyperplasia and focal nuclear changes in squamous epithelium consistent with herpes simplex virus cytopathic effect. Antibiotics were then discontinued based on biopsy results and she was discharged on oral valacyclovir 1 g twice a day. On outpatient follow up, the valacyclovir was increased to 1 g three times per day, but without significant improvement over 2 months of treatment. Patient eventually underwent wide local excision of the peri-clitoral lesion and peri-anal lesions with the same pathology as the previous biopsies (Fig. 2) and no concern for recurrent malignancy. She continued high dose oral valacyclovir for the remaining peri-anal lesions. Upon post-operative follow-up, there was marked improvement of vulvar lesions but worsening of peri-anal lesions. The valacyclovir was changed to famicyclovir 500 mg twice a day for presumed failure to valacyclovir, HSV culture was sent but not resulted due to lab error. She has had continued improvement of the lesions since then. She continues on bictegravir-emtricitabine-tenofovir and raltegravir HAART, most recently with a viral load of 51. Compliance with treatment has correlated with her vulvar findings.
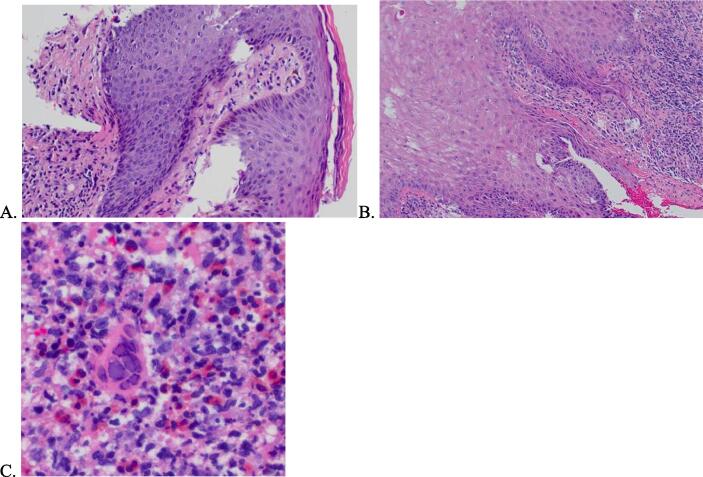
Fig. 2.
Histologic findings of biopsied mons vulvar lesion. A. Pseudoepitheliomatous hyperplasia, hematoxylin and eosin (100x) B. Acanthosis and parakeratosis, hematoxylin and eosin (200x) C. Herpes simplex virus cytopathic effect, hematoxylin and eosin (400x).
3. Discussion
Women with HIV have higher rates of VIN and vulvar carcinoma, as well as higher relapse rates after treatment (Dedes et al., 2008). This has been theorized to be due to the shared transmission mechanism of HIV and Human Papillomavirus (HPV), and poorly controlled HIV with its resultant immunosuppression further increases this risk (Jamieson et al., 2006). Recurrent HSV infections are common in patients with HIV, with 50–90 % of patients with HIV-1 reported to be co-infected with HSV (Strick et al., 2006). Increased pathogenesis of HIV has been described due to the increased mucosal shedding associated with HSV infection. While our patient’s serum HSV PCR test was negative, the histology was persistently consistent with HSV on multiple biopsies.
The lesion in our patient has been described by many terms, including vulvar pseudotumoral HSV, pseudoepitheliomatous hyperplasia, and hypertrophic herpes simplex genitalis (HHSG). Pseudoepitheliomatous hyperplasia is a reactive epithelial proliferation. It is a benign process that results from a chronic inflammatory response, such as this patient’s poor, prolonged healing from her initial vulvectomy, VIN, chronic HSV, or poorly controlled HIV. A related process has been described in the literature called HHSG. This is a rare type of nodular lesion of HSV, almost always found in the setting of positive HIV infection. On histology, it is plasma-rich and contains virocytes, and grossly appears as ulcerated, firm, nodular masses. In a case report and literature review by Strehl et al, this rare presentation was also found to be associated with intraepithelial neoplasia of the vulva, vaginal, and anus, although in less frequency than isolated HHSG lesions. The majority of the lesions described required a combination of surgery and oral therapy (antiviral and/or immunomodulatory) for improvement or resolution.
Resistance of HSV to antivirals occurs in about 5 % of patients with HIV (Reyes et al., 2003), but has been suggested to be even higher in hypertrophic HSV-associated lesions. The idea for surgery as part of treatment was first described in the 1970s, under the theory that epidermal denervation would prevent recurrence (Shelley, 1978). For most patients, this is not a definitive treatment, as recurrent lesions will appear in adjacent anogenital regions. However, for a small subset of patients with chronic anogenital HSV resistant to acyclovir, surgery with adjuvant antivirals is effective (Simonsen et al., 2008). In this case, surgical intervention also provided the dual role of tissue diagnosis. In the case of not just recurrent HSV but hypertrophic vulvar lesion with HSV, surgery often is required for large lesions as well as adjuvant antivirals or iammunomodulatory treatment, such as imiquimod and thalidomide which downregulate proinflammatory cytokines and stimulate natural immune cytotoxic effects and apoptosis, which down-regulate viral replication.
4. Conclusion
Hyperplastic HSV-associated vulvar lesions can present a diagnostic and therapeutic challenge, as they resemble pre-invasive and invasive carcinoma and are likely to be resistant to usual antiviral agents. A high suspicion for malignancy must be maintained with serial exams and repeat biopsies as necessary throughout the course of workup and treatment, which can take months to years. The treatment plan will likely include some combination of antiviral therapy, surgery, and immunomodulatory therapy, as well as continuing HAART for management of HIV.
CRediT authorship contribution statement
Rachel McKean: Writing – original draft, Conceptualization. Jennifer Wolf: Writing – original draft, Conceptualization. Ting Ting Wong: Validation, Writing – review & editing. Yong Mei Yin: Validation, Writing – review & editing. Margaux J. Kanis: Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgement
The authors want to thank the patient trusting in our proposed treatment strategy and granting approval for publishing her clinical case.
Informed consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Dedes K.J., Beneder C., Samartzis N., Muller M.D., Fink D., Fehr M.K. Outcome of treated anogenital intraepithelial neoplasia among human immunodeficiency virus-infected women. J Reprod Med Obstet Gynecol. 2008;53(12) [PubMed] [Google Scholar]
- Frimer M., Chudnoff S., Hebert T., Shahabi S. Pseudoepitheliomatous hyperplasia mimicking vulvar cancer in a patient with AIDS. J. Low. Genit. Tract Dis. 2011;15(1) doi: 10.1097/LGT.0b013e3181f0b8f5. [DOI] [PubMed] [Google Scholar]
- Jamieson D.J., Paramsothy P., Cu-Uvin S., Duerr A. Vulvar, vaginal, and perianal intraepithelial neoplasia in women with or at risk for human immunodeficiency virus. Obstet. Gynecol. 2006;107(5) doi: 10.1097/01.AOG.0000210237.80211.ff. [DOI] [PubMed] [Google Scholar]
- Jasim A., Proietto A., Scurry J. Herpes simplex virus infection of vulvar squamous cell carcinoma. Pathology. 2016;48 doi: 10.1016/j.pathol.2015.11.006. [DOI] [PubMed] [Google Scholar]
- Reyes M., Shaik N.S., Graber J.M., Nisenbaum R., Wetherall N.T., Fukuda K., et al. Acyclovir-resistant genital herpes among persons attending sexually transmitted disease and human immunodeficiency virus clinics. Arch. Intern. Med. 2003;163(1) doi: 10.1001/archinte.163.1.76. [DOI] [PubMed] [Google Scholar]
- Shelley W.B. Surgical treatment for recurrent herpes simplex. Lancet. 1978;312(8098) doi: 10.1016/s0140-6736(78)92340-1. [DOI] [PubMed] [Google Scholar]
- Simonsen M., Nahas S.C., Da Silva Filho E.V., Araújo S.E.A., Kiss D.R., Nahas C.S.R. Atypical perianal herpes simplex infection in HIV-positive patients. Clinics. 2008;Vol. 63 doi: 10.1590/s1807-59322008000100024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strehl J.D., Mehlhorn G., Koch M.C., Harrer E.G., Harrer T., Beckmann M.W., et al. HIV-associated hypertrophic herpes simplex genitalis with concomitant early invasive squamous cell carcinoma mimicking advanced genital cancer: Case report and literature review. Int. J. Gynecol. Pathol. 2012;Vol. 31 doi: 10.1097/PGP.0b013e318237d581. [DOI] [PubMed] [Google Scholar]
- Strick L.B., Wald A., Celum C. Management of herpes simplex virus type 2 infection in HIV type 1-infected persons. Clin. Infect. Dis. 2006;Vol. 43 doi: 10.1086/505496. [DOI] [PubMed] [Google Scholar]