Abstract
Background
Studies from Western countries indicated that older adults were more resilient than younger ones to deteriorating mental health during the COVID-19 pandemic. As high late-life suicide rates have been reported in East Asia, it is possible that the pandemic impact might differ between East and West. We investigated the pandemic impact on age-specific suicide patterns in Taiwan.
Methods
Interrupted time-series analysis was used to model the overall, and age-stratified, monthly suicide rates before (January 1st, 2017 to December 31st, 2019) and after (January 1st 2020 to December 31st 2021) the COVID-19 outbreak. Associations between confirmed COVID-19 deaths and suicide rates were also assessed.
Results
There was a significant decrease in overall suicide rates after the COVID-19 outbreak (p < 0.01) (annual average rates per 100,000 population of 16.4 prior, 15.2 after). The overall decrease was driven by fewer suicide deaths in the young- and older-middle-aged groups (25–44 and 45–64 years). However suicide rates in younger-age group (<25 years) were already increasing pre-pandemic, a trend which continued after the outbreak. Suicide rates for older people (≥65 years) also increased along with the increasing number of COVID-19 deaths during the pandemic period.
Limitations
Under-reporting and/or misclassification of suicides were possible.
Conclusions
The overall suicide rates in Taiwan did not change after the COVID-19 outbreak; however, suicide in older adults increased. Public health measures to reduce COVID-19 infections may have unintended and adverse consequences on the psychological wellbeing of older citizens.
Keywords: Suicide, Older adults, Pandemic, COVID-19, Taiwan
1. Introduction
Since the SARS-Cov-2 (Coronavirus disease 2019, COVID-19) pandemic was announced in early 2020, suicide prevention researchers have been concerned about the possibility of a rise in suicides (Gunnell et al., 2020; Pompili, 2021; Yip and Chau, 2020). Such concerns arise from the potential increase of a plethora of suicide risk factors after the pandemic onset. For example, the fear of contracting COVID-19 and death might aggravate anxiety, depression and other mental disorders (Sher, 2020). Public health measures (e.g. lockdown, school closure) to curb the spread of the virus were reported to increase loneliness, social disconnectedness, domestic violence and alcohol abuse (Sher, 2020; Yip and Chau, 2020). The pandemic also resulted in job losses and financial crises, which are well-recognized contributing factors of suicide (Chen et al., 2010; Rehkopf and Buka, 2006). In addition, some evidence suggests that COVID-19-related inflammation and associated immune responses might directly increase the risk of mood disorders and suicide (Banerjee et al., 2021).
However, historical data on pandemic impact of suicide are inconclusive (Rogers et al., 2021). A recent Swedish study spanning from 1910 to 1978 did not find a significant association between influenza deaths and suicide rate changes (Ruck et al., 2021). There was a significant increase in suicide rate, predominantly in older people, during the SARS-CoV-1 epidemic (which largely affected East Asian countries) in 2003 (Chang et al., 2022; Yip et al., 2010). Moreover, an analysis of suicide rate in 21 high-middle income countries six months after the SARS-CoV-2 pandemic suggested no overall rate increase (Pirkis et al., 2021). A follow-up study of 33 countries some 9–15 months later confirmed this; however, age-group-specific findings were inconsistent across countries (Pirkis et al., 2022a).
In 2020, with strict border controls, COVID-19 was relatively well-contained in Taiwan, with only 799 confirmed cases and no COVID-19-related death in that year. Our initial study of suicides in Taiwan was conducted on 2020 cause-of-death data, showing a slight decrease in the overall suicide rate (Chen et al., 2022). This finding appeared to be mainly driven by the decrease in suicides in the young- and older-middle-aged group (25–64 years); although we noted that suicide rates in people aged 65 years and older showed a slight (not statistically significant) increase after the pandemic onset.
Our findings were at odds with reports from many Western countries, where older adults, compared to their younger counterparts, were largely thought to have better mental health resilience since the announcement of the pandemic (Cray and Vahia, 2022; Vahia et al., 2020; Barber and Kim, 2021; Losada-Baltar et al., 2021; Palgi et al., 2020). Researchers hypothesized that this may have been associated with better financial stability (Hadjistavropoulos and Asmundson, 2022; Vahia et al., 2020) and/or better abilities to regulate emotions (Charles, 2010), compared with younger people.
Taiwan had a different COVID-19 experience in 2021, compared with 2020. There was an upsurge of COVID-19 cases in May–July 2021, resulting in 16,250 confirmed cases and 850 deaths. Stricter public health measures were implemented to reduce the virus spread during the period, such as restrictions on visiting people in hospitals and long-term care institutions, bans on religious and social gatherings, and closure of dining-in establishments. This potentially exerted a much greater impact on the mental health of Taiwanese people than had been experienced in 2020. This paper extends our 2020 analysis (Chen et al., 2022) with the aim of examining changes over time. We compared suicide rates by age group in the three years pre-pandemic (Jan. 2017–Dec. 2019) with the two-year period after the pandemic was declared (Jan. 2020–Dec. 2021). We also tested whether age-specific suicide rates were related to the number of COVID-19 related deaths after the pandemic onset.
2. Methods
2.1. Data
Monthly overall and age-stratified suicide mortality data were retrieved from Taiwan's national cause-of-death file for the years 2017–2021. The ICD-10 codes which identified suicide deaths were X60-X84, whilst COVID-19 cases and deaths were obtained from Taiwan Center for Disease Control (Taiwan Center for Disease Control, 2022).
2.2. Statistical analysis
Interrupted time series analysis was conducted to evaluate the longitudinal effects of the COVID-19 pandemic on monthly suicide rates in Taiwan. As the first COVID-19 case in Taiwan was reported in January 2020, this was defined as the onset of the pandemic for our analysis. The influence of COVID-19 was modeled as a dummy variable that had the value of 0 prior to the pandemic (Jan 2017–Dec 2019) and the value 1 for years 2020 and 2021. The impact of time (Time), the number of COVID-19 confirmed cases (Covid-19 Case), the number of COVID-19 deaths (Covid-19 Death) and their corresponding logarithm transformation over time, were modeled to explore their association with the overall and age-stratified suicide rates. Age groups were young (<25 years), middle-aged (25–44 years, 45–64 years) and older (≥65 years). The residual diagnostics of the chosen model, together with Durbin-Watson statistics, were examined to assess the appropriateness of model fitting. The dataset and analytic codes are provided in the appendix.
3. Results
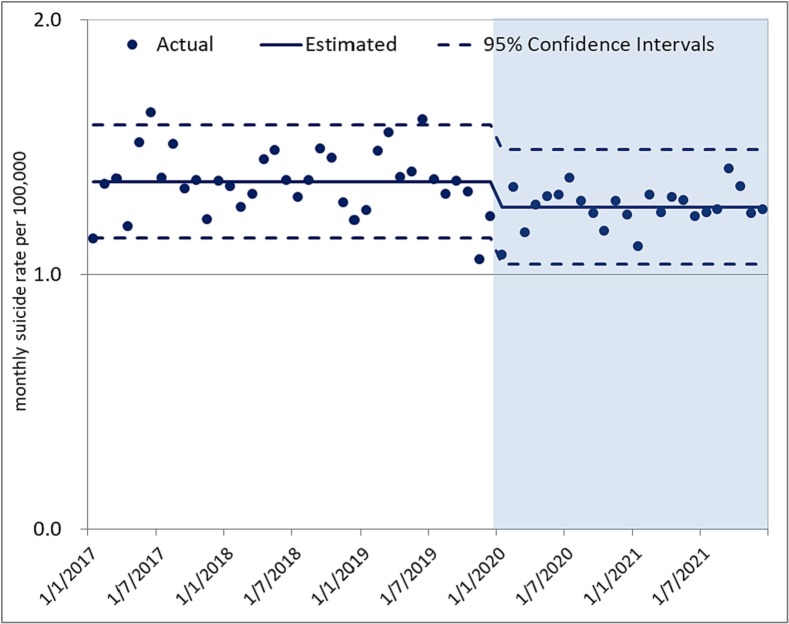
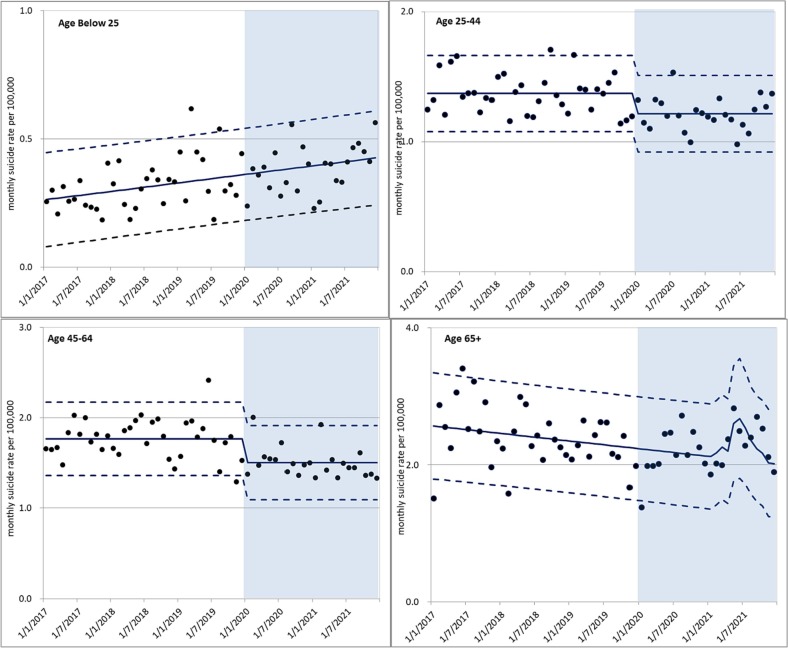
Overall suicide rates decreased significantly by 7.3 % (p < 0.01) after the pandemic (Fig. 1 ). In the previous (pre-pandemic) three years, the average annual suicide rate was 16.4 cases per 100,000, whilst in 2020 and 2021, the estimated average rate was 15.2 cases per 100,000 population. Age-stratified analysis indicated that the decrease in overall suicide rate after the pandemic was driven by the middle-aged group (Fig. 2 ). Suicide by people younger than 25 years was already increasing before the pandemic, and continued to do so after its onset. Whilst there was decreasing average suicide rate in older people before the pandemic, this did not persist; and in fact we observed a suicide peak after the pandemic was announced.
Fig. 1.
The actual and estimated overall suicide rate trends before (Jan. 2017-Dec. 2019) and after (Jan. 2020–Dec. 2021) the COVID-19 outbreak in Taiwan.
Fig. 2.
The actual and estimated suicide rate trends before (Jan. 2017-Dec. 2019) and after (Jan. 2020–Dec. 2021) the COVID-19 outbreak by age groups in Taiwan.
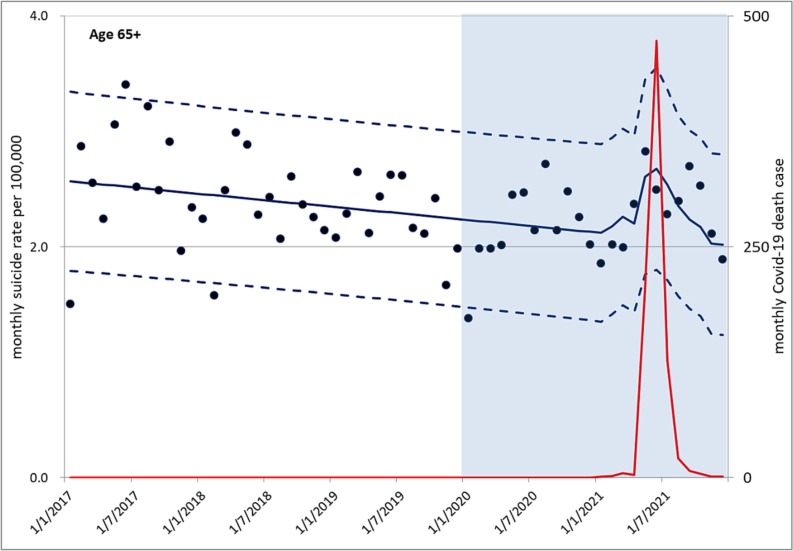
Table 1 details the findings of the interrupted time series analyses regarding the impact of the pandemic on overall and age-stratified suicide rates. Statistically-significant decreases in suicide rates after the pandemic were found in overall (β (s.e.) [β estimate and standard error] = −0.10 (0.03), p value < 0.01), and in the young- and older-middle-aged groups [β (s.e.) = −0.16 (0.04), p value < 0.01 in 25–44 year old group and − 0.26 (0.05), p value < 0.01 in 45–64 year old group, respectively]. The number of COVID-19 deaths was positively associated with increased suicide rates in older people but not in people younger than 65 years. We estimated that each unit of COVID-19 death by natural logarithm was associated with 0.10 suicides per 100,000 population increment in older people (p = 0.03). Fig. 3 illustrates the co-variation between COVID-19 deaths and the increase in suicide deaths in the older age group.
Table 1.
Interrupted time-series models assessing the association between COVID-19 outbreak and monthly suicide rates by age groups in Taiwan.
| Parameter estimate | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Age groups |
Overall |
Below 25 |
25–44 |
45–64 |
65 and above |
|||||
| Variable | Estimate (s.e) |
p-Value | Estimate (s.e) |
p-Value | Estimate (s.e) |
p-Value | Estimate (s.e) |
p-Value | Estimate (s.e) |
p-Value |
| Intercept | 1.37 | <0.01 | −1.62 | <0.01 | 1.37 | <0.01 | 1.77 | <0.01 | 8.94 | <0.01 |
| (0.02) | (0.47) | (0.02) | (0.03) | (2.25) | ||||||
| Time | 0.00 | <0.01 | −0.00 | <0.01 | ||||||
| (0.00) | (0.00) | |||||||||
| No. of Covid-19a | −0.10 | <0.01 | −0.16 | <0.01 | −0.26 | <0.01 | ||||
| (0.03) | (0.04) | (0.05) | ||||||||
| Log(Covid-19Death)b | 0.10 | 0.03 | ||||||||
| (0.04) | ||||||||||
s.e.: standard error.
Covid-19 is an indicator variable with the value 1 between Jan2020 and Dec2021 and 0 for the rest.
Log(Covid-19Death) is the logarithm transformation of Covid-19 death case.
Fig. 3.
The number of COVID-19 deaths (red line) and suicide rate trends in older age groups (≥65 years) during the study period, 2017–2022. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
4. Discussion
4.1. Main findings
This paper presents new information on suicide rates before, and during the COVID-19 pandemic in Taiwan, and thus provides important information on how people of different ages in one East Asian context responded to the mental challenges of living through the pandemic. Whilst overall suicide rates in Taiwan decreased in the two years after the onset of the COVID-19 pandemic, this decrease was largely driven by lower suicide rates reported for people aged between 25 and 64 years. Public health concerns should be raised by the different patterns in suicide rates in people younger than 25 years, and people aged 65 years and older. Suicide rates in younger people were already increasing pre-pandemic, a trend which continued in the first two years of the pandemic. On the other hand, suicide rates in older people were decreasing prior to the onset of the pandemic, but increased significantly after it, with this increase being significantly associated with the number of COVID-19 deaths. Similar associations between suicides and Covid-19 deaths were not observed in younger people.
4.2. Explanations and comparisons with previous studies
Concurring with historical data on influenza pandemic (Chang et al., 2020; Ruck et al., 2021) and international comparisons on the impact of COVID-19 on suicide rates (Pirkis et al., 2022b; Pirkis et al., 2021), no increase in overall suicide rates in Taiwan was observed two years after the onset of the pandemic. According to Durkheim (1897), abrupt social transitions and crisis may cause social disruptions and dysregulations; a consequence of which might be a rise in suicide rates. However, this is not inevitable, as social calamities might alternatively enhance social integrations, where people stand together to fight for a shared goal. This can increase the sense of belongingness and cohesiveness, in such a way where suicide rates may reduce (Claassen et al., 2010; Lester, 1994). However, it is important to continue to pay attention to vulnerable subgroups, those who were affected the most during the pandemic. Their story might be masked if only population-wide statistics are considered. Since the outbreak of the COVID-19 pandemic, older adults are likely to have experienced specific adversities. For instance, if they get sick, they are most likely to have severe physical complications and mortality risks (e.g. De Pue et al., 2021; Modig et al., 2021; United Nations, 2020). Also, public health measures designed to mitigate the spread of COVID-19 have had unique impacts on older adults around the world. For instance, the suspension of many social support services and disruptions of routine medical care services have disproportionally affected older adults worldwide. Furthermore, social interactions with family and friends (for instance, restricted visiting in hospitals and long-term care settings, or restricted opportunities to dine out, or worship) were highly restricted; and confining older people to their houses, or even to their own rooms was likely to have large impact on their mental wellbeing and life quality. Moreover, whilst younger people may have gradually adapted to a new digital way of life post-COVID (such as using online platforms to socialize, work, or access tele-healthcare), older people may have had less incentive and capability to do so, because of lack of knowledge, facilities and/or opportunities to seek support, or to learn from others. This may have left many older adults feeling isolated, disconnected from family and friends, and disadvantaged because they had few alternative ways of conducting their pandemic lives (Litchfield et al., 2021; Song et al., 2021). The likely cumulative disadvantages (physically, psychologically and socially) may have left many older adults particularly vulnerable to pandemic-related psychological distress symptoms such as anxiety and depression (Hadjistavropoulos and Asmundson, 2022). We postulated that the increased suicide rates found in older Taiwanese adults during the COVID-19 pandemic reflected the impact of public health directives which were actually intended to protect them from illness. Indeed, as shown in our analysis, the older adults' suicide rate surged during May and July 2021, it was a time when Taiwan Central Epidemic Control Center issued Level-3 COVID-19 alert (Taipei City Government, 2021). Regulations enacted during the period including mandatory face mask wearing when going out, restricted social gatherings, closure of entertainment venues, and advice for citizens to stay at home during the period. This finding has historical precedence in how older people in Taiwan and/or East Asia responded to the SARS-CoV-1 epidemic in 2003. At that time, there was a significant increase in suicide rate, predominantly in older people (Chang et al., 2022; Yip et al., 2010). The impact on mental health of the two SARS outbreaks some 20 years apart, is perhaps the best indicator of how pandemics affect older people in East Asia.
It is possible that rapid modernization and Westernization combined with population-aging has posed unforeseen challenges in elder care in East Asian countries (Lee and Mjelde-Mossey, 2004). Emphasizing filial piety, elder care in East Asian countries has been highly dependent on the younger generations, as Government investment in elder care has been limited (Lee and Mjelde-Mossey, 2004). However, younger people in current and future generations might not embrace the same Confucian value of filial piety, thus the mismatch of caring expectations by older people and caring capacities of younger people could be related to the high rate of elder suicides in East Asia (Chen et al., 2012; Liu, 2009). The recent pandemic may further have imposed unprecedented suicide crisis in this already vulnerable group in the region. Because of restrictions on social gatherings, even the most willing of families would have found it difficult to provide ongoing support to isolated older relatives or friends.
The decrease in suicide rates by middle-aged people in Taiwan could be related to the sense of relatively-favorable control of COVID-19 in Taiwan, compared to other countries in the world. Even though the surge of COVID-19 cases in May 2021 had an economic impact; unemployment rates increased only marginally from 3.64 % in April to 4.11 % in May 2021 (National Statistics R. O. C. (Taiwan), 2022). The COVID-19 outbreak was controlled within three months and the economy recovered quickly. Moreover, the unemployment rate decreased from a high of 4.80 % in June 2021 to 3.64 % in December 2021. This might explain the reduced suicide rate found in the working population during this period.
The increasing youth suicide rate over the past 10 years in Taiwan has been reported previously (Chen et al., 2021). The pandemic did not seem to affect this trend, and further investigations are required urgently to understand the reasons underlying this trend, and to put actions in place to avert the crisis of the potentially-avoidable loss of young lives.
5. Limitations
Our study has two main limitations. First, under-reporting and misclassification of suicide is possible. For example, an earlier study indicated that many suicides were categorized to death by ‘undetermined intent’ (Chang et al., 2010). Suicide is still a highly stigmatized condition (Chang et al., 2010; Kapusta et al., 2011); hence the direction of the misclassification, if any, would be towards the null. Second, sex-stratified data were unavailable when we prepared this manuscript, thus we were unable to examine gender differences.
6. Conclusions
The mental health impact of the COVID-19 pandemic, and resultant suicides, varied by age-groups in Taiwan. The increasing suicide trend for older people during the pandemic suggested the severity of the impact of living through the pandemic-related public health restrictions, on their mental health. Whilst these public health measures were essential to control the spread of the virus, they disrupted many critical social support resources; particularly for older adults in East Asian contexts. Thus in protecting the health of nations, Governments may have inadvertently undermined the mental health of already vulnerable older people. As the world is coming to grips with the impact of the pandemic, considerations would seem essential in post-pandemic planning, into how better to implement social distancing measures for future health challenges, that do not expose vulnerable people of any age to further mental health stressors.
CRediT authorship contribution statement
YYC: acquired the data and drafted the manuscript.
CTY: conducted the statistical analysis, revised the method section, composed the figure.
PSFY: conceived the study and critically revised the manuscript.
All the authors have read and approved of the contents of the submitted manuscript. They all agree to be listed as coauthors and have accepted the order of authorship. This manuscript has not been published previously and is not under consideration for publication elsewhere.
Funding statement
YYC was supported by the Ministry of Science and Technology of Taiwan under Grant (MOST111-2314-B-532-003-MY3); the National Health Research Institutes under Grant (NHRI-EX111-10818PI) and the Department of Health, Taipei City Government under Grant (11101-62-001).
Conflict of interest
None declared.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jad.2023.02.006.
Appendix A. Supplementary data
Supplementary material
References
- Banerjee D., Kosagisharaf J.R., Sathyanarayana Rao T.S. 'The dual pandemic' of suicide and COVID-19: a biopsychosocial narrative of risks and prevention. Psychiatry Res. 2021;295 doi: 10.1016/j.psychres.2020.113577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barber S.J., Kim H. COVID-19 worries and behavior changes in older and younger men and women. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021;76:e17–e23. doi: 10.1093/geronb/gbaa068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang S.S., Sterne J.A., Lu T.H., Gunnell D. 'Hidden' suicides amongst deaths certified as undetermined intent, accident by pesticide poisoning and accident by suffocation in Taiwan. Soc. Psychiatry Psychiatr. Epidemiol. 2010;45:143–152. doi: 10.1007/s00127-009-0049-x. [DOI] [PubMed] [Google Scholar]
- Chang Y.H., Chang S.S., Hsu C.Y., Gunnell D. Impact of pandemic on suicide: excess suicides in Taiwan during the 1918–1920 influenza pandemic. J. Clin. Psychiatry. 2020;81 doi: 10.4088/JCP.20l13454. [DOI] [PubMed] [Google Scholar]
- Chang S.S., Lin C.Y., Liang Y.L., Chang Y.H., Hsu C.Y., Yip P.S.F. The impact of 2003 SARS epidemic on suicide in Taiwan and Hong Kong. Psychiatry Clin. Neurosci. 2022;76:202–203. doi: 10.1111/pcn.13336. [DOI] [PubMed] [Google Scholar]
- Charles S.T. Strength and vulnerability integration: a model of emotional well-being across adulthood. Psychol. Bull. 2010;136:1068–1091. doi: 10.1037/a0021232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Y.Y., Yip P.S.F., Lee C., Fan H.F., Fu K.W. Economic fluctuations and suicide: a comparison of Taiwan and Hong Kong. Soc. Sci. Med. 2010;71:2083–2090. doi: 10.1016/j.socscimed.2010.09.043. [DOI] [PubMed] [Google Scholar]
- Chen Y.Y., Wu K.C.C., Yousuf S., Yip P.S.F. Suicide in Asia: opportunities and challenges. Epidemiol. Rev. 2012;34:129–144. doi: 10.1093/epirev/mxr025. [DOI] [PubMed] [Google Scholar]
- Chen Y.Y., Yang C.T., Pinkney E., Yip P.S.F. The age-period-cohort trends of suicide in Hong Kong and Taiwan, 1979–2018. J. Affect. Disord. 2021;295:587–593. doi: 10.1016/j.jad.2021.08.084. [DOI] [PubMed] [Google Scholar]
- Chen Y.Y., Yang C.T., Pinkney E., Yip P.S.F. Suicide trends varied by age-subgroups during the COVID-19 pandemic in 2020 in Taiwan. J. Formos. Med. Assoc. 2022;121:1174–1177. doi: 10.1016/j.jfma.2021.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claassen C.A., Carmody T., Stewart S.M., Bossarte R.M., Larkin G.L., Woodward W.A., Trivedi M.H. Effect of 11 september 2001 terrorist attacks in the USA on suicide in areas surrounding the crash sites. Br. J. Psychiatry. 2010;196:359–364. doi: 10.1192/bjp.bp.109.071928. [DOI] [PubMed] [Google Scholar]
- Cray H.V., Vahia I.V. Two years of COVID-19: understanding impact and implications for the mental health of older adults. Am. J. Geriatr. Psychiatry. 2022;30:444–447. doi: 10.1016/j.jagp.2022.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Pue S., Gillebert C., Dierckx E., Vanderhasselt M.A., De Raedt R., Van den Bussche E. The impact of the COVID-19 pandemic on wellbeing and cognitive functioning of older adults. Sci. Rep. 2021;11:4636. doi: 10.1038/s41598-021-84127-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkheim E. Free Press; New York: 1897/1951. Suicide: A Study in Sociology. [Google Scholar]
- Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., Khan M., O'Connor R.C., Pirkis J., Covid- Suicide Prevention Research Collaboration Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7:468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadjistavropoulos T., Asmundson G.J.G. COVID stress in older adults: considerations during the omicron wave and beyond. J. Anxiety Disord. 2022;86 doi: 10.1016/j.janxdis.2022.102535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapusta N.D., Tran U.S., Rockett I.R., De Leo D., Naylor C.P., Niederkrotenthaler T., Voracek M., Etzersdorfer E., Sonneck G. Declining autopsy rates and suicide misclassification: a cross-national analysis of 35 countries. Arch. Gen. Psychiatry. 2011;68:1050–1057. doi: 10.1001/archgenpsychiatry.2011.66. [DOI] [PubMed] [Google Scholar]
- Lee M.Y., Mjelde-Mossey L. Cultural dissonance among generations: a solution-focused approach with east asian elders and their families. J. Marital. Fam. Ther. 2004;30:497–513. doi: 10.1111/j.1752-0606.2004.tb01258.x. [DOI] [PubMed] [Google Scholar]
- Lester D. Gender equality and the sex differential in suicide rates. Psychol. Rep. 1994;75:1162. doi: 10.2466/pr0.1994.75.3.1162. [DOI] [PubMed] [Google Scholar]
- Litchfield I., Shukla D., Greenfield S. Impact of COVID-19 on the digital divide: a rapid review. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-053440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H.L. Epidemiologic characteristics and trends of fatal suicides among the elderly in Taiwan. Suicide Life Threat. Behav. 2009;39:103–113. doi: 10.1521/suli.2009.39.1.103. [DOI] [PubMed] [Google Scholar]
- Losada-Baltar A., Jimenez-Gonzalo L., Gallego-Alberto L., Pedroso-Chaparro M.D.S., Fernandes-Pires J., Marquez-Gonzalez M. "We are staying at home." association of self-perceptions of aging, personal and family resources, and loneliness with psychological distress during the lock-down period of COVID-19. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021;76:e10–e16. doi: 10.1093/geronb/gbaa048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modig K., Ahlbom A., Ebeling M. Excess mortality from COVID-19: weekly excess death rates by age and sex for Sweden and its most affected region. Eur. J. Pub. Health. 2021;31:17–22. doi: 10.1093/eurpub/ckaa218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Statistics R. O. C. (Taiwan) National statistics R. O. C; Taiwan: 2022. Statistical Analysis.https://www.stat.gov.tw/ct.asp?xItem=47781&CtNode=4944&mp=4 [Google Scholar]
- Palgi Y., Shrira A., Ring L., Bodner E., Avidor S., Bergman Y., Cohen-Fridel S., Keisari S., Hoffman Y. The loneliness pandemic: loneliness and other concomitants of depression, anxiety and their comorbidity during the COVID-19 outbreak. J. Affect. Disord. 2020;275:109–111. doi: 10.1016/j.jad.2020.06.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkis J., John A., Shin S., DelPozo-Banos M., Arya V., Analuisa-Aguilar P., Appleby L., Arensman E., Bantjes J., Baran A., Bertolote J.M., Borges G., Brecic P., Caine E., Castelpietra G., Chang S.S., Colchester D., Crompton D., Curkovic M., Deisenhammer E.A., Du C., Dwyer J., Erlangsen A., Faust J.S., Fortune S., Garrett A., George D., Gerstner R., Gilissen R., Gould M., Hawton K., Kanter J., Kapur N., Khan M., Kirtley O.J., Knipe D., Kolves K., Leske S., Marahatta K., Mittendorfer-Rutz E., Neznanov N., Niederkrotenthaler T., Nielsen E., Nordentoft M., Oberlerchner H., O'Connor R.C., Pearson M., Phillips M.R., Platt S., Plener P.L., Psota G., Qin P., Radeloff D., Rados C., Reif A., Reif-Leonhard C., Rozanov V., Schlang C., Schneider B., Semenova N., Sinyor M., Townsend E., Ueda M., Vijayakumar L., Webb R.T., Weerasinghe M., Zalsman G., Gunnell D., Spittal M.J. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021;8:579–588. doi: 10.1016/S2215-0366(21)00091-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkis J., Gunnell D., Shin S., Baños M.D.P. Did suicide numbers diverge from pre-existing trends during the first 9–15 months of the COVID-19 pandemic? Interrupted time series analyses of total and sex- and age-specific suicide counts in 33 countries. SSRN Electron. J. 2022 doi: 10.2139/ssrn.4066503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkis J., Gunnell D., Shin S., Del Pozo-Banos M., Arya V., Aguilar P.A., Appleby L., Arafat S.M.Y., Arensman E., Ayuso-Mateos J.L., Balhara Y.P.S., Bantjes J., Baran A., Behera C., Bertolote J., Borges G., Bray M., Brecic P., Caine E., Calati R., Carli V., Castelpietra G., Chan L.F., Chang S.S., Colchester D., Coss-Guzman M., Crompton D., Curkovic M., Dandona R., De Jaegere E., De Leo D., Deisenhammer E.A., Dwyer J., Erlangsen A., Faust J.S., Fornaro M., Fortune S., Garrett A., Gentile G., Gerstner R., Gilissen R., Gould M., Gupta S.K., Hawton K., Holz F., Kamenshchikov I., Kapur N., Kasal A., Khan M., Kirtley O.J., Knipe D., Kolves K., Kolzer S.C., Krivda H., Leske S., Madeddu F., Marshall A., Memon A., Mittendorfer-Rutz E., Nestadt P., Neznanov N., Niederkrotenthaler T., Nielsen E., Nordentoft M., Oberlerchner H., O'Connor R.C., Papsdorf R., Partonen T., Phillips M.R., Platt S., Portzky G., Psota G., Qin P., Radeloff D., Reif A., Reif-Leonhard C., Rezaeian M., Roman-Vazquez N., Roskar S., Rozanov V., Sara G., Scavacini K., Schneider B., Semenova N., Sinyor M., Tambuzzi S., Townsend E., Ueda M., Wasserman D., Webb R.T., Winkler P., Yip P.S.F., Zalsman G., Zoja R., John A., Spittal M.J. Suicide numbers during the first 9–15 months of the COVID-19 pandemic compared with pre-existing trends: an interrupted time series analysis in 33 countries. EClinicalMedicine. 2022;51 doi: 10.1016/j.eclinm.2022.101573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pompili M. Can we expect a rise in suicide rates after the Covid-19 pandemic outbreak? Eur. Neuropsychopharmacol. 2021;52:1–2. doi: 10.1016/j.euroneuro.2021.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehkopf D.H., Buka S.L. The association between suicide and the socio-economic characteristics of geographical areas: a systematic review. Psychol. Med. 2006;36:145–157. doi: 10.1017/S003329170500588X. [DOI] [PubMed] [Google Scholar]
- Rogers J.P., Chesney E., Oliver D., Begum N., Saini A., Wang S., McGuire P., Fusar-Poli P., Lewis G., David A.S. Suicide, self-harm and thoughts of suicide or self-harm in infectious disease epidemics: a systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 2021;30 doi: 10.1017/S2045796021000214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruck C., Mataix-Cols D., Malki K., Adler M., Flygare O., Runeson B., Sidorchuk A. Swedish nationwide time series analysis of influenza and suicide deaths from 1910 to 1978. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2021-049302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher L. The impact of the COVID-19 pandemic on suicide rates. QJM. 2020;113:707–712. doi: 10.1093/qjmed/hcaa202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Y., Qian C., Pickard S. Age-related digital divide during the COVID-19 pandemic in China. Int. J. Environ. Res. Public Health. 2021;18:11285. doi: 10.3390/ijerph182111285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taipei City Government . Taipei City Government; 2021. Level 3 COVID-19 Alert in Place for Taipei City Effective May 15.https://english.gov.taipei/News_Content.aspx?n=A11F01CFC9F58C83&s=ED6AC6D701EA9817 [Google Scholar]
- Taiwan Center for Disease Control . Taiwan Center for Disease Control; 2022. COVID-19.https://www.cdc.gov.tw/ [Google Scholar]
- United Nations . United Nations; 2020. Policy Brief: The Impact of COVID-19 on Older Persons.https://unsdg.un.org/sites/default/files/2020-05/Policy-Brief-The-Impact-of-COVID-19-on-Older-Persons.pdf [Google Scholar]
- Vahia I.V., Jeste D.V., Reynolds C.F., 3rd Older adults and the mental health effects of COVID-19. JAMA. 2020;324:2253–2254. doi: 10.1001/jama.2020.21753. [DOI] [PubMed] [Google Scholar]
- Yip P.S.F., Chau P.H. Physical distancing and emotional closeness amidst COVID-19. Crisis. 2020;41:153–155. doi: 10.1027/0227-5910/a000710. [DOI] [PubMed] [Google Scholar]
- Yip P.S.F., Cheung K.S.L., Law S.C.K., Chi I., Robine J.M. The demographic window and economic dependency ratio in the Hong Kong SAR. Asian Popul. Stud. 2010;6:241–260. doi: 10.1080/17441730.2010.494452. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material