Highlights
-
•
Women who use opioids (WWUO) suboptimally access and use effective contraception.
-
•
We mapped 28 studies identifying contraceptive barriers and facilitators for WWUO.
-
•
Contraceptive barriers and facilitators for WWUO exist at many levels of influence.
-
•
We identified no studies that included participants from marginalized groups.
-
•
Future research should target more diverse populations in community settings.
Keywords: Hormonal contraception, Long-acting reversible contraception, Contraceptive access, Opioids, Opioid use, Opioid use disorder, Scoping review
Abstract
Existing research has found that women who use opioids (WWUO) experience challenges to hormonal and long-acting reversible contraception (HC-LARC) access and use. Facilitators of such use are unclear. We conducted a scoping review to comprehensively map the literature on barriers to and facilitators of HC-LARC access and use in the United States among reproductive-aged WWUO. In accordance with the JBI Manual of Evidence Synthesis, we conducted literature searches for empirical articles published from 1990 to 2021. Independent reviewers screened references, first by titles and abstracts, then by full-text, and charted data of eligible articles. We coded and organized HC-LARC barriers and facilitators according to a four-level social-ecological model (SEM) and categorized findings within each SEM level into domains. We screened 4,617 records, of which 28 articles focusing on HC-LARC (n = 18), LARC only (n = 6), or testing an intervention to increase HC-LARC uptake (n = 4) met inclusion criteria. We identified 13 domains of barriers and 11 domains of facilitators across four SEM levels (individual, relationship, community, societal). The most frequently cited barriers and facilitators were methods characteristics, partner and provider relations, transportation, healthcare availability and accessibility, cost, insurance, and stigma. Future studies would benefit from recruiting participants and collecting data in community settings, targeting more diverse populations, and identifying neighborhood, social, and policy barriers and facilitators. Reducing barriers and improving equity in HC-LARC access and use among WWUO is a complex, multifaceted issue that will require targeting factors simultaneously at multiple levels of the social-ecological hierarchy to effect change.
1. Introduction
In the United States (US), opioid use and opioid-related morbidity and mortality among reproductive-aged women continues to worsen with the evolving opioid epidemic. Between 1999 and 2014, rates of diagnosed opioid use disorder (OUD) at delivery increased fourfold (Haight et al., 2018). Prescription opioid overdose deaths rose 596 % among women from 1999 to 2016 (NIDA, 2020). Moreover, polysubstance use has become exceedingly common among women who use opioids (WWUO).1 Between 2005 and 2014, among US women aged 18–44 reporting non-medical opioid use, only 10.8 % used opioids without concurrent use of additional substances, such as cannabis or stimulants (Jarlenski et al., 2017).
In 2015, Terplan and colleagues published a seminal systematic review comprised of 24 studies in which they reported that only 55 % of women with opioid and other substance use disorders (SUD) used any form of contraception; barrier methods were the most common (62 %), while long-acting reversible contraception (LARC) or sterilization accounted for 8 % of use (Terplan et al., 2015). Since that time, additional studies have documented that reproductive-aged WWUO and are at risk of unintended pregnancy do not use hormonal contraception and LARC (HC-LARC)2 because of barriers related to accessing and using those methods. Two such studies were narrative reviews: one published in 2016 and the other in 2020 (Black and Day, 2016, Stone et al., 2020). The 2016 review by Black and Day focused on barriers to contraceptive access and uptake among women with any SUD. The more recent review by Stone and colleagues specifically documented barriers to contraceptive access and uptake among women with OUD. In that study, barriers included but were not limited to “patient misconception or lack of reproductive health knowledge, cost, poor access to care, partner violence, fear of criminalization, comorbid conditions, and healthcare provider misconceptions or practice limitations” (Stone et al., 2020). Although both reviews were comprehensive in nature, neither used a systematic methodological approach to map and synthesize the literature, nor did they identify facilitators to HC-LARC access and use.
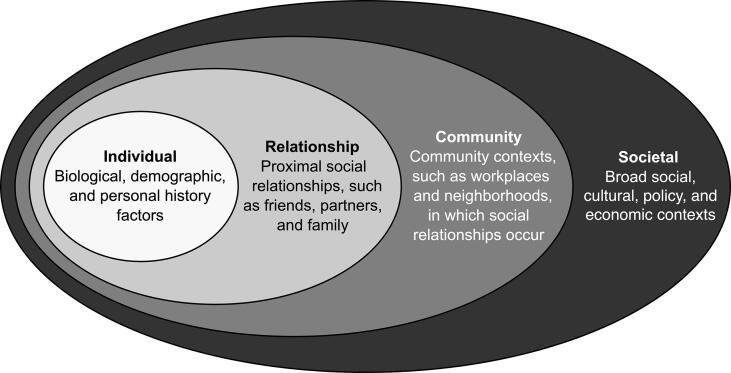
Using a theory-driven approach, we conducted a scoping review to comprehensively identify literature on barriers to and facilitators of HC-LARC access and use in the US among WWUO. Specifically, we used the social-ecological model (SEM), which is a theoretical framework developed by Urie Bronfenbrenner in 1979 for understanding various determinants of health behavior (Glanz et al., 2008), as an organizing framework to guide this research. The specific objectives of the scoping review were to: 1) assess the breadth and types of evidence available on barriers and facilitators to HC-LARC access and use among reproductive-aged WWUO; 2) summarize and map barriers and facilitators according to a four-level SEM framework; and 3) identify gaps in knowledge about barriers and facilitators to inform where future research is needed. The results of this review will help to identify knowledge gaps and provide guidance on developing multilevel interventions and other solutions aimed at reducing disproportionate barriers to HC-LARC access and use for WWUO.
2. Methods
2.1. Design
We conducted this scoping review using guidance from the latest version of the JBI Manual for Evidence Synthesis (Peters et al., 2020, Peters et al., 2015). We drew upon the five stages of Arksey and O’Malley’s scoping review framework: 1) identifying the research question; 2) identifying relevant studies; 3) study selection; 4) charting the data; and 5) collating, summarizing, and reporting the results (Arksey and O'Malley, 2005). The optional sixth stage of consultation with stakeholders was not used. For transparency and reproducibility, we adhere to reporting guidelines outlined in the Preferred Reporting Items for Systematic Reviews and meta-Analyses Extension for protocols (PRISMA-P), abstracts (PRISMA-A), searches (PRISMA-S), and scoping reviews (PRISMA-ScR) (Appendix A) (Beller et al., 2013, Moher et al., 2015, Rethlefsen et al., 2021, Tricco et al., 2018). This review has been registered with Open Science Framework (OSF) (https://osf.io/wx7vb). Per the University of Utah Institutional Review Board (IRB), reviews do not meet the definition of human subjects research and therefore do not require IRB approval.
2.2. Eligibility criteria
Studies were eligible for inclusion if: 1) participants were women aged 18–56 years reporting use of prescribed or non-prescribed opioids (e.g. hydrocodone, morphine, heroin), or medication for OUD (MOUD) (i.e. buprenorphine, methadone, or naltrexone); 2) they reported HC-LARC barriers or facilitators, defined as factors deterring or contributing to the access and use of HC-LARC methods, respectively; 3) they were conducted in US settings; 4) they used quantitative (e.g. randomized controlled trials, surveys), qualitative (e.g. focus groups, interviews), or systematic review study designs; 5) they were published in the year 1990 or later, which coincides with the onset of increased opioid prescribing in the US (Jenkins, 2021). To ensure that findings were reflective of the true population of interest, we did not include studies in which the proportion of women participants using opioids was not reported or <25 %. We recognize the diversity of gender identities of people seeking contraceptive care, and will use the term “woman” throughout as used in the primary sources. Contrary to the protocol, we did not include studies that reported on barrier methods only as we determined that factors affecting access to these widely available, over-the-counter methods are different. Moreover, we excluded studies without methods, such as case reports, commentary articles, and narrative reviews; we acknowledge our protocol registered to OSF incorrectly indicated we would include these evidence sources.
2.3. Search strategy
We developed and conducted the literature searches for electronic sources using a combination of appropriate database subject headings and keywords harvested from sentinel articles, database indexing, and team feedback. The strategy was developed by an information specialist (MMM) for the primary database, Medline, and then translated to other selected databases. Peer review of search strategies was performed by library colleagues using the Peer Review of Electronic Search Strategies (PRESS) guidelines (McGowan et al., 2016). No methods filters were applied. Date limits were applied to capture studies published during or after 1990. All search strategies can be found in Appendix B.
We searched the following electronic sources: Medline (Ovid) 1990–2021, Embase (Elsevier) 1990–2021, CINAHL Complete (Ebscohost) 1990–2021, Cochrane Library (Wiley) 1990–2021 including CENTRAL (wiley.com) 1990–2021, Academic Search Ultimate (Ebscohsot) 1990–2021, PsycINFO (Ebscohost) 1990–2021, Scopus (scopus.com) 1990–2021, Sociological Abstracts (ProQuest) 1990–2021, and Web of Science Core Collection (Clarivate) 1990–2021. No grey literature, as identified in our protocol, was searched due to time constraints. Also, due to technical difficulties, Sociological Abstracts (ProQuest) was not included in search results. Search results were imported into Covidence (Covidence Systematic Review Software) for study-screening and selection.
2.4. Study screening and selection
Five independent reviewers (JK-M, TG, ET, KB, GMS) working in blinded duos screened titles and abstracts for eligibility, then reviewed full texts for inclusion. Voting conflicts were resolved through discussion with the research team. To ensure reliability and consistency in the study selection process, we examined pairwise inter-rater reliability prior to starting the title and abstract screening (n = 100) and full-text review (n = 10) to ensure at least 80 % agreement between reviewers. We checked references of our included studies and identified nine records to review in Covidence; two met eligibility criteria and were included in the final sample. See Appendix C for bibliographies of included studies and excluded studies with reasons for exclusion.
2.5. Data extraction
Four team members (JK-M, TG, ET, EC) working in blinded duos extracted the following data from the selected studies: citation details; study aims/objectives; study design; location; setting; participants and sample size; opioid use; contraceptive focus of study; and, HC-LARC barriers and facilitators (Appendix D). To be as inclusive as possible, we extracted barriers and facilitators that had any endorsement by participants.
We used an iterative process of independent extraction (five studies at a time), followed by comparison of extracted elements between team members and refinement of the extraction tool. EC supervised data extraction and extraction conflicts were resolved through discussion with the research team during (bi)weekly team meetings. Prior to extraction, we pilot tested the extraction form using a sample of five studies to ensure at least 80 % agreement across extracted elements. Data were charted using Microsoft Excel 365 (Microsoft Corp., Redmond, WA, USA).
2.6. Framework analysis
We reported data using basic descriptive statistics and framework analysis, which is an analytic method that allows pre-selected themes to be assigned to the data (Gale et al., 2013). We coded and organized the extracted HC-LARC barriers and facilitators according to four levels of the SEM framework (Fig. 1) (Krug et al., 2002); within each level, we categorized findings into domains. If barriers or facilitators were categorized by the study authors, we followed their a priori categorization. For all others, we looked for context to assign barriers and facilitators to a specific level of influence and domain. Data were compiled and synthesized by EC and verified by JK-M; final categorization findings was determined by consensus from both team members.
Fig. 1.
Social-ecological model framework and definitions.
3. Results
3.1. Characteristics of studies
We identified 11,437 records in database searching, and after removing 6,829 duplicates, we screened titles and abstracts of 4,608 records, resulting in a total of 84 articles that were assessed in full-text review, of which 28 met the inclusion criteria, including two of nine studies from reference checks. See Appendix E for the PRISMA flow diagram of source results. Articles focused on any HC-LARC method (n = 18), focused specifically on LARC (n = 6), or tested an intervention to increase HC-LARC uptake (n = 4) (Table 1).
Table 1.
Characteristics of studies included in the scoping review.
| First author, year | Location | Study design | Contraceptive focus of study | Setting | Study population | Na | Opioid use in study population, % |
|---|---|---|---|---|---|---|---|
| Hormonal or long-acting reversible contraception (HC-LARC) | |||||||
| Armstrong et al., 1991 | Pennsylvania | Mixed methods (interviews, focus groups, and clinic records) | Opinions and attitudes related to use of contraceptive and family planning services | Methadone, drug-free outpatient, and residential SUD treatment facilities | Drug treatment patients; aged 16–56 years | 599b | 100 % in drug treatment; 25 % injected heroin in the past 4 weeks |
| Bornstein et al., 2019 | California | Qualitative (interviews) |
Perceptions and experiences with pregnancy, contraception, and reproductive decision making | Methadone clinics | Sexually-active, non-pregnant methadone patients; aged 21–39 years | 22 | 100 % taking Rx methadone |
| Collier et al., 2019 | Vermont | Retrospective chart review (medical records) | MOUD treatment location, pregnancy planning, and postpartum contraceptive uptake | University-affiliated academic medical center | Patients with 2 consecutive pregnancies taking MOUD during ≥ 1 of the pregnancies; mean age: 25.8 years | 98 | 95.9 % and 97.0 % taking MOUD during 1st and 2nd pregnancies, respectively |
| Fischbein et al., 2018 | Ohio | Mixed methods (survey and interviews) | Decisions, preferences, and perceptions related to contraceptive use | Residential and non-residential SUD treatment facilities | Pregnant or recently pregnant drug treatment patients; mean age: 27.6 years | 42 | 100 % Rx opioid abuse/dependence in the past 12 months |
| Florsheim et al., 2020 | California | Qualitative (interviews) | Factors affecting access to contraception | Public, non-clinical locations during outreach and naloxone distribution | Non-pregnant syringe exchange program clients; aged 23–39 years | 14 | 100 % injecting drugs; 57.1 % heroin use |
| Gipson et al., 2021 | California | Quantitative (survey) | Pregnancy preferences and contraceptive use | Methadone clinics | Non-pregnant methadone patients; aged 18–44 years | 50 | 100 % taking Rx methadone |
| Handy et al., 2018 | Ohio | Retrospective chart review (medical records) | Rx contraceptive initiation | OUD outpatient clinic offering non–/pharmacologic services | Non-pregnant adolescents and young adults initiating OUD treatment; aged 14–25 years | 123 | 100 % taking naloxone/ buprenorphine; 74 % combined Rx opioid/heroin |
| Hathazi et al., 2009 | California | Qualitative (interviews) | Pregnancy experiences and contraceptive use | Public, non-clinical locations | Homeless adolescents and young adults (women and men) with ≥ 1 pregnancy events; aged 16–28 years | 20 | 100 % injecting drugs; 55 % injected heroin in the past 4 weeks |
| Hurley et al., 2020 | Missouri | Qualitative (interviews) | Contraceptive services integration into non-traditional OUD care settings | SEPs, recovery support programs, SUD treatment facilities and clinics, EDs, and FQHCs | Sexually-active, reproductive-aged women with OUD and professional stakeholders working with people with OUD | 15 | 33.3 % in active opioid use; 66.7 % in recovery from active opioid use |
| Krans et al., 2018 | Pennsylvania | Retrospective cohort study (medical records) | Receipt of postpartum contraceptive method | University-affiliated academic medical center | Pregnant patients with OUD; mean age: 29 years | 248 | 81.4 % and 44.4 % of cohort participants initiated MOUD during pregnancy |
| Leinaar et al., 2020 | Tennessee | Quantitative (survey) | Contraceptive barriers and associations with contraceptive use | Outpatient MOUD clinics | Non-pregnant patients receiving treatment for OUD; aged 18–55 years | 91 | 100 % taking MOUD |
| Leinaar et al., 2019 | Tennessee | Quantitative (survey) | Contraceptive use and reproductive healthcare access | Outpatient MOUD clinics | Non-pregnant patients receiving treatment for OUD; aged 18–55 years | 91 | 100 % taking MOUD |
| MacAfee et al., 2020a | Michigan | Quantitative (survey) | Sexual and reproductive health services access and barriers to access | Methadone, outpatient, and residential SUD treatment facilities | Non-pregnant patients receiving treatment for OUD; aged 18–50 years | 260 | 100 % in treatment for OUD; 100 % history of non-medical opioid use |
| MacAfee et al., 2020b | Michigan | Qualitative (interviews) | Barriers and facilitators to accessing sexual and reproductive health services | Outpatient and residential SUD treatment programs | SUD treatment patients and direct patient care providers at SUD treatment facilities | 17 | 100 % in SUD treatment; 53.3 % opioid use |
| Meschke et al., 2018 | Tennessee | Quantitative (survey) | Contraceptive knowledge, attitudes, and behavior and associations with contraceptive use | Outpatient MOUD clinics | Non-pregnant and pregnant patients receiving treatment for OUD; aged 18–45 years | 287 | 100 % taking MOUD |
| Parlier et al., 2014 | North Carolina | Retrospective chart review (medical records) | Prevalence and predictors of postpartum contraceptive use | High-risk maternity care clinic | Recently pregnant patients using Rx or illicit opioids or MOUD; aged 19–41 years | 94 | 61.5 % taking methadone; 12.5 % taking buprenorphine; 26 % not taking MOUD |
| Perry et al., 2020 | California | Quantitative (survey) | Contraceptive need and predictors of receiving contraceptive services | SEP | Patients receiving services at SEP; aged 18–44 years | 96 | 74 % used heroin in the past 6 months |
| Sobel et al., 2021 | Massachusetts | Qualitative (interviews) | Experiences with contraceptive decision-making | University-affiliated academic medical center | Recently pregnant patients with OUD; aged 21–40 years | 20 | 55 % taking methadone; 30 % taking buprenorphine; 15 % not taking MOUD |
| Long-active reversible contraception (LARC) | |||||||
| Kotha et al., 2019 | Pennsylvania | Retrospective cohort study (medical records) | Factors contributing to receipt of postpartum LARC | University-affiliated academic medical center | Pregnant patients with OUD receiving MOUD; mean age: 27 years | 791 | 80 % taking methadone; 20 % taking buprenorphine |
| Mastey et al., 2020 | Massachusetts | Retrospective cohort study (medical records) | Patterns and predictors of postabortion LARC uptake | Planned Parenthood health centers | Patients with a completed induced abortion procedure using and not using MOUD; aged < 18-≥35 years | 768 | 100 % using MOUD on day of abortionc |
| Matusiewicz et al., 2017 | Vermont | Quantitative (survey) | Interest in, concerns about, and knowledge of LARC | Outpatient MOUD clinics | Patients receiving treatment for OUD at risk of unintended pregnancy; aged 18–49 years | 83 | 61.4 % taking methadone; 38.6 % taking buprenorphine |
| McNeely et al., 2019 | Tennessee | Mixed methods (interviews, observation, and clinic records) | Family planning education and LARC provision | County jails | Incarcerated women; aged 18–50 years | 921 | 75.1 % history of opioid use; 23.8 % history of opioid use during pregnancy |
| Rey et al., 2020 | Vermont | Quantitative (survey) | Knowledge, attitudes, experiences, and barriers related to LARC use | Outpatient MOUD clinic | Patients receiving treatment for OUD; aged 18–44 years | 200 | 100 % taking MOUD |
| Smith et al., 2019 | Tennessee | Mixed methods (survey and interviews) | Knowledge and use of LARC | OUD outpatient clinic offering non–/pharmacologic services | Non-pregnant patients receiving treatment for OUD; aged 18–49 years | 50 | 100 % in treatment for OUD |
| Intervention | |||||||
| Heil et al., 2016 | Vermont | Pilot randomized controlled trial | Rx contraceptive initiation and continuation | Outpatient MOUD clinics | Patients receiving MOUD at risk of unintended pregnancy; aged 18–44 years | 31 | 100 % taking MOUD; 90 % taking Rx methadone |
| Heil et al., 2021 | Vermont | Randomized clinical trial | Rx contraceptive and LARC use | OUD outpatient clinic offering non–/pharmacologic services | Patients receiving MOUD at risk of unintended pregnancy; aged 20–44 years | 138 | 100 % taking MOUD |
| Jones et al., 2021 | North Carolina | Pilot randomized controlled trial | Any contraceptive and LARC method receipt | OUD outpatient clinic offering non–/pharmacologic services | Non-pregnant, reproductive-aged patients receiving MOUD; aged 18–40 years | 90 | 100 % taking MOUD |
| Rinehart et al., 2021 | Colorado | Pilot randomized controlled trial | Receipt of family planning services and Rx contraceptive use | OUD outpatient clinic offering non–/pharmacologic services | Patients receiving MOUD at risk of unintended pregnancy; aged 18–44 years | 119 | 75.6 % taking methadone; 24.4 % taking buprenorphine |
Abbreviations: HC-LARC = hormonal or long-acting reversible contraception; N = sample size; SUD = substance use disorder; Rx = prescription; MOUD = medication for opioid use disorder (i.e. methadone and buprenorphine [or buprenorphine-containing products, such as buprenorphine/naloxone]); OUD = opioid use disorder; SEPs = syringe exchange programs; EDs = emergency departments; FQHCs = federally qualified health centers; LARC = long-acting reversible contraception.
For studies that included men, professional stakeholders, providers, or women participants not taking opioids, we reported N only for women participants taking opioids.
A subset of women (N = 35) participated in the focus groups.
Among the cohort using MOUD.
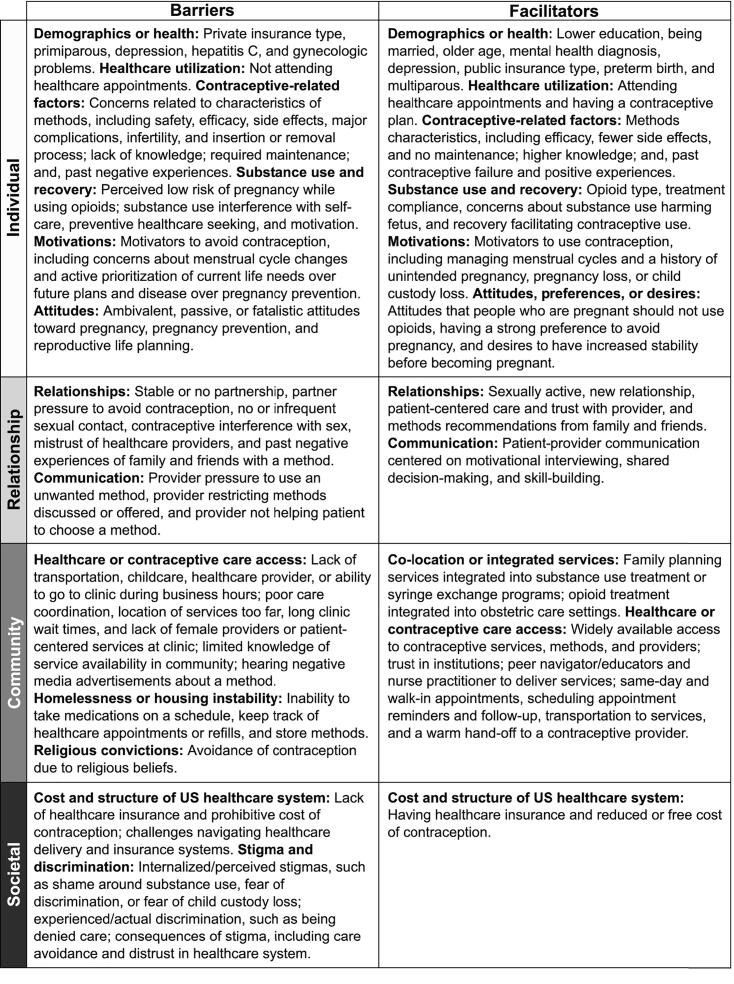
3.2. Barriers and facilitators
We identified six domains of barriers and six domains of facilitators at the individual level; two domains of barriers and two domains of facilitators at the relationship level; three domains of barriers and two domains of facilitators at the community level; and two domains of barriers and one domain of facilitators at the societal level (Fig. 2). Table 2 presents domains and their associated SEM level reported within the included studies. We describe HC-LARC barriers and facilitators below according to SEM levels.
Fig. 2.
Author-identified domains of barriers to and facilitators of hormonal and long-acting reversible contraception access and use among women who use opioids, by social-ecological model levels.
Table 2.
Studies examining barriers to and facilitators of hormonal and long-acting reversible contraception access and use among women who use opioids, by social-ecological model levels and author-identified domains.
 |
Abbreviations: B = Barriers; F = Facilitators; HC-LARC = Hormonal or long-acting reversible contraception; LARC = long-active reversible contraception.
a Symbol (/) indicates that religion was examined as a barrier but not endorsed by any study participants.
3.2.1. Individual-level barriers
3.2.1.1. Demographics or health
Having public compared to private insurance was a barrier (Kotha et al., 2019), as was giving birth for the first time (i.e. primiparous) compared to having multiple births (Kotha et al., 2019), depressed mood (Meschke et al., 2018), and having Hepatitis C (Kotha et al., 2019). One study reported not being eligible for contraception because of gynecologic problems as a barrier (Rey et al., 2020).
3.2.1.2. Healthcare utilization
Missed healthcare appointments due to difficulty keeping them (Leinaar et al., 2020) or forgetting them (Meschke et al., 2018) were barriers, as was avoiding use of family planning services over concerns about receiving bad health news (Armstrong et al., 1991). Postpartum visit non-attendance was a reported barrier to postpartum contraceptive use (Parlier et al., 2014). One study reported discomfort with the examination as a reason for missing or not scheduling a family planning appointment (Meschke et al., 2018).
3.2.1.3. Contraceptive-related factors
Concerns about characteristics of methods were common barriers, including: safety (Armstrong et al., 1991, McNeely et al., 2019, Meschke et al., 2018), efficacy/effectiveness (Armstrong et al., 1991, Hurley et al., 2020), and side effects (Armstrong et al., 1991, Bornstein et al., 2019, Fischbein et al., 2018, Hurley et al., 2020, Leinaar et al., 2020, MacAfee et al., 2020a, Matusiewicz et al., 2017, McNeely et al., 2019, Meschke et al., 2018, Rey et al., 2020, Smith et al., 2019, Sobel et al., 2021). Fear of major complications (Rey et al., 2020, Smith et al., 2019), infection (Leinaar et al., 2020, Matusiewicz et al., 2017, Sobel et al., 2021), and bleeding/spotting (Rey et al., 2020) were LARC-related barriers. Four studies identified concerns related to LARC placement or removal, including: concerns about the insertion or removal process (Matusiewicz et al., 2017), fear of pain during insertion (Rey et al., 2020), concerns about forgetting when to remove a method and potential fertility effects (Sobel et al., 2021), and not wanting foreign objects in the body (Rey et al., 2020) or in a particular location in the body (Rey et al., 2020, Smith et al., 2019). Method maintenance, including having to remember appropriate use (Florsheim et al., 2020) or to take a daily pill (Sobel et al., 2021), were barriers for HC methods, whereas not having control over starting and stopping the method was a LARC barrier (Rey et al., 2020). Lack of knowledge (Matusiewicz et al., 2017, Meschke et al., 2018, Rey et al., 2020, Smith et al., 2019) or having enough knowledge (Heil et al., 2016) about contraception were consistent barriers, as were having past negative experiences with contraception related to method failure (Bornstein et al., 2019, Florsheim et al., 2020), side effects (Bornstein et al., 2019), appropriate storage and use (Florsheim et al., 2020), and complications (Smith et al., 2019). Concerns that contraception would cause infertility (Bornstein et al., 2019, Rey et al., 2020, Smith et al., 2019); delay a desired future pregnancy (Bornstein et al., 2019, Smith et al., 2019); and physically or psychologically interfere with sex (Rey et al., 2020, Smith et al., 2019), the body’s natural processes (MacAfee et al., 2020a), and mood stabilizing medications (Sobel et al., 2021) were barriers. Having an alternate method preference and perceived contraindications were also barriers (Smith et al., 2019).
3.2.1.4. Substance use and recovery
Perceived low risk of pregnancy while using opioids and other substances was a consistently reported barrier (Bornstein et al., 2019, Florsheim et al., 2020, MacAfee et al., 2020a, Smith et al., 2019). Contributing factors for this perception included reduced or no sexual activity (Bornstein et al., 2019, Smith et al., 2019), irregular or no menses (Bornstein et al., 2019, Florsheim et al., 2020), older age leading to lower fertility levels (Smith et al., 2019), not having a past pregnancy while using substances or methadone despite having unprotected sex (Bornstein et al., 2019), and belief that substance use has caused infertility or actual infertility (Bornstein et al., 2019, MacAfee et al., 2020a, Rey et al., 2020). Competing priorities over pregnancy prevention, reproductive health, and self-care during periods of active substance use (Florsheim et al., 2020, Hurley et al., 2020, MacAfee et al., 2020b, Sobel et al., 2021) and over preventive care and health needs during early recovery (Hurley et al., 2020, MacAfee et al., 2020b) were commonly reported barriers. One study reported that substance use interfered with motivation to use contraception and make proactive decisions around using contraception (Bornstein et al., 2019). Preoccupation with substance use (MacAfee et al., 2020b), substance use during sex (Hathazi et al., 2009), and longer duration of time since first opioid use (Meschke et al., 2018) were identified barriers. One study reported that contraceptive methods could be reminders of substance use and that side effects could prompt relapse, which influenced the acceptability of methods (Sobel et al., 2021).
3.2.1.5. Motivations
A commonly reported motivator to avoid HC-LARC was concerns about menstrual cycle changes (Matusiewicz et al., 2017, Smith et al., 2019, Sobel et al., 2021). Active prioritization of current life needs over future plans (Bornstein et al., 2019) and disease prevention over pregnancy prevention (Armstrong et al., 1991, Sobel et al., 2021) were additional barriers as were other non-specific motivations (Matusiewicz et al., 2017).
3.2.1.6. Attitudes
Ambivalent attitudes toward pregnancy or pregnancy prevention were present among individuals not using contraception (Bornstein et al., 2019, MacAfee et al., 2020a, Meschke et al., 2018, Smith et al., 2019). Passive attitudes around planning, decision-making, and taking action related to reproductive health or life matters (Armstrong et al., 1991, Bornstein et al., 2019, Florsheim et al., 2020, Heil et al., 2016) and fatalistic attitudes toward the ability to prevent pregnancy (Armstrong et al., 1991, Bornstein et al., 2019) were commonly reported barriers. Having the attitude that contraception was inconvenient was reported as a barrier in one study (MacAfee et al., 2020a).
3.2.2. Individual-level facilitators
3.2.2.1. Demographics or health
Receiving less than a high school education (Handy et al., 2018), being married (Kotha et al., 2019), older age (Mastey et al., 2020), and having a prior mental health diagnosis (Handy et al., 2018) were facilitators, as were two factors also identified as barriers: having public insurance compared to self-pay (Mastey et al., 2020) and screening positive for depression (Perry et al., 2020). Preterm as compared to full-term delivery was a facilitator for postpartum contraceptive use (Parlier et al., 2014), as was having previous pregnancies (i.e. multigravida) (Handy et al., 2018, Mastey et al., 2020, Meschke et al., 2018).
3.2.2.2. Healthcare utilization
Returning for a follow-up healthcare visit (Handy et al., 2018) and not missing healthcare appointments (Meschke et al., 2018) were facilitators. One study reported that medical record documentation of a LARC contraceptive plan prior to delivery was a facilitator for postpartum LARC use (Kotha et al., 2019).
3.2.2.3. Contraceptive-related factors
Characteristics of methods, including higher efficacy/effectiveness (Fischbein et al., 2018, Smith et al., 2019), perceptions of fewer side effects (Fischbein et al., 2018), and not having to remember ongoing maintenance (Florsheim et al., 2020), were facilitators for HC-LARC methods. One study documented higher contraceptive-related knowledge among persons using contraception than those not using contraception (Meschke et al., 2018). Past positive experiences with LARC (Smith et al., 2019) and past experiences of getting pregnant while using contraception (Meschke et al., 2018) were LARC use facilitators.
3.2.2.4. Substance use and recovery
Use of prescription opioids as opposed to heroin and MOUD compliance were associated with contraceptive initiation among adolescents with OUD (Handy et al., 2018). Concerns that substance use would harm the fetus was a facilitator in one study (Florsheim et al., 2020). Three studies identified aspects related to recovery as facilitators, including: recovery as an optimal time to prioritize health needs (Armstrong et al., 1991, Hurley et al., 2020), and the belief that the daily routine of recovery facilitates remembering to take a daily oral contraceptive pill (Sobel et al., 2021).
3.2.2.5. Motivations
Menstruation-related factors, including maintaining regular cycles (Smith et al., 2019) and suppressing cycles (Florsheim et al., 2020, Sobel et al., 2021), were motivators to use HC-LARC. A history of: unintended pregnancy (Perry et al., 2020), pregnancy loss (McNeely et al., 2019), and child custody loss (McNeely et al., 2019) were also facilitators.
3.2.2.6. Attitudes, preferences, or desires
Attitudes that people who are pregnant should not use opioids (Meschke et al., 2018) or methadone (Bornstein et al., 2019) facilitated HC-LARC use. Having a strong preference to avoid pregnancy was a facilitator (Gipson et al., 2021, Meschke et al., 2018). Desires to have increased stability with regards to substance use, housing, or socioeconomic circumstances before having (more) children affected contraceptive decision-making (Bornstein et al., 2019, Florsheim et al., 2020, Sobel et al., 2021), as did the desire to be proactive against losing custody of (a) child(ren) (McNeely et al., 2019).
3.2.3. Relationship-level barriers
3.2.3.1. Relationships
Being in a monogamous (Fischbein et al., 2018) or stable (Bornstein et al., 2019) partner relationship was identified as a barrier, as was not being in a relationship (MacAfee et al., 2020a, Rey et al., 2020). Intimate partner or sexual violence (Armstrong et al., 1991, Handy et al., 2018), partner pressure to become pregnant (Leinaar et al., 2020), partner pressure to avoid contraception (Leinaar et al., 2020, Meschke et al., 2018), and concerns about partner disapproval (Armstrong et al., 1991) were barriers. Not having sexual relations (MacAfee et al., 2020a, Meschke et al., 2018, Rey et al., 2020), having infrequent sex (MacAfee et al., 2020a, Meschke et al., 2018), and experiencing contraceptive interference with sex (Armstrong et al., 1991) were additional barriers. Three studies identified mistrust of healthcare providers as barriers (Armstrong et al., 1991, Heil et al., 2016, MacAfee et al., 2020a). Negative experiences of friends or family influenced decisions not to use LARC methods (Matusiewicz et al., 2017, Rey et al., 2020, Smith et al., 2019).
3.2.3.2. Communication
Concerns about provider pressure to use an unwanted contraceptive method was identified as a barrier (MacAfee et al., 2020a). Aspects of provider communication, including restricting methods discussed (Florsheim et al., 2020) or provided (MacAfee et al., 2020a), recommending that the patient not use a particular method (Rey et al., 2020), and not helping the patient decide on a method (Heil et al., 2016), were additional barriers.
3.2.4. Relationship-level facilitators
3.2.4.1. Relationships
Being sexually active with the opposite sex compared to not sexually active was associated with contraceptive use (Leinaar et al., 2019), as was being in a relationship with a new partner (Fischbein et al., 2018). Patient-centered care, defined as non-judgmental, compassionate, respectful, or comfortable care, within a patient-provider relationship was consistently reported as a facilitator (Armstrong et al., 1991, Hurley et al., 2020, Jones et al., 2021, McNeely et al., 2019), as was not being treated differently by a provider because of substance use (MacAfee et al., 2020b). One study reported that receiving LARC recommendations from a provider and information from friends and family facilitated LARC use (Smith et al., 2019).
3.2.4.2. Communication
Patient-provider communication strategies were facilitators, including: motivational interviewing (Jones et al., 2021, Rinehart et al., 2021); discussions around managing side effects (Heil et al., 2016, Heil et al., 2021); shared decision-making (Heil et al., 2016, Heil et al., 2021, Jones et al., 2021); use of real-life examples or visual tools to educate on contraceptive methods (Heil et al., 2016, Heil et al., 2021, Jones et al., 2021, Rinehart et al., 2021); and communication skill-building, including active listening, communication with providers, negotiation for safer sex with partners, and goal-setting techniques (Jones et al., 2021).
3.2.5. Community-level barriers
3.2.5.1. Healthcare or contraceptive care access
Lack of transportation was consistently identified as a barrier (Florsheim et al., 2020, Hurley et al., 2020, Leinaar et al., 2020, MacAfee et al., 2020a, MacAfee et al., 2020b). One study identified location of services being too far away and not being able to get time off work, find childcare, and go to clinic during business hours as barriers (MacAfee et al., 2020a). LARC barriers included having to go to a provider or clinic for placement and removal (Rey et al., 2020, Smith et al., 2019). Two studies identified gaps in care coordination in jail or upon reentry into the community as barriers (Florsheim et al., 2020, McNeely et al., 2019). Not having a healthcare provider (Meschke et al., 2018) or access to a healthcare facility to obtain a method (Rey et al., 2020) were identified barriers, as was the inability to obtain a method covered under Medicaid (Fischbein et al., 2018). Clinic-related factors, including long appointment wait times (Hurley et al., 2020), lack of female providers (MacAfee et al., 2020a), and lack of patient-centered services (Hurley et al., 2020), were reported as barriers. Limited knowledge of service options/availability in the community (Armstrong et al., 1991, Hurley et al., 2020, MacAfee et al., 2020a, MacAfee et al., 2020b), and hearing negative information about a method on the television or internet (Rey et al., 2020), were also barriers.
3.2.5.2. Homelessness or housing instability
Three studies reported homelessness/housing instability as a barrier due to the inability to: maintain a regular dosing schedule (Hathazi et al., 2009), keep track of healthcare appointments and prescription refills (Florsheim et al., 2020, Sobel et al., 2021), properly store contraceptive methods (Florsheim et al., 2020, Sobel et al., 2021), and have regular access to a restroom (Sobel et al., 2021).
3.2.5.3. Religious convictions
Religion was identified as a LARC use barrier by a small number of participants in one study (Rey et al., 2020). Another study surveyed participants about religious convictions as a barrier, but no participants endorsed this item (Leinaar et al., 2020).
3.2.6. Community-level facilitators
3.2.6.1. Co-location or integrated services
A commonly identified facilitator at the community level was co-location or integrated services, including: family planning services integrated into substance use treatment settings (Armstrong et al., 1991, Heil et al., 2021, Hurley et al., 2020, MacAfee et al., 2020b), family planning services integrated into syringe exchange programs (Florsheim et al., 2020), and opioid treatment integrated into obstetric care settings (Collier et al., 2019, Krans et al., 2018). Two studies reported trust with substance use providers and convenience as the primary benefits of co-location or service integration (Florsheim et al., 2020, MacAfee et al., 2020b).
3.2.6.2. Healthcare or contraceptive care access
Widely available access to contraceptive services, methods, and prescribers, including in multiple, diverse, and convenient locations, was consistently reported as a facilitator (Fischbein et al., 2018, Florsheim et al., 2020, Hurley et al., 2020, Krans et al., 2018, Leinaar et al., 2020, Sobel et al., 2021). One study reported institutional trust as a facilitator (Hurley et al., 2020). The same study identified community outreach and information dissemination through opinion leaders as facilitators to improve HC-LARC access in hard-to-reach communities (Hurley et al., 2020). Peer navigators, nurse practitioners, and peer educators were used to facilitate contraceptive education and service provision (Heil et al., 2016, Heil et al., 2021, Hurley et al., 2020, Rinehart et al., 2021). Healthcare appointment-related factors, including same-day appointments (Heil et al., 2016, Heil et al., 2021, Jones et al., 2021), short wait times (Hurley et al., 2020), walk-in appointments (Hurley et al., 2020), and scheduling reminders (Rinehart et al., 2021, Sobel et al., 2021), were commonly identified facilitators, as were providing transportation to appointments (Jones et al., 2021, MacAfee et al., 2020b, Rinehart et al., 2021) and a warm hand-off or referral to a contraceptive provider (Rinehart et al., 2021). Two intervention studies identified financial incentives for attending follow-up appointments as facilitators to contraceptive adherence (Heil et al., 2016, Heil et al., 2021).
3.2.7. Societal-level barriers
3.2.7.1. Cost and structure of US healthcare system
Two of the most consistently reported barriers were lack of insurance (Florsheim et al., 2020, Hurley et al., 2020, MacAfee et al., 2020b, Meschke et al., 2018, Rey et al., 2020) and prohibitive cost (Fischbein et al., 2018, Hurley et al., 2020, Leinaar et al., 2020, MacAfee et al., 2020a, MacAfee et al., 2020b, Meschke et al., 2018, Rey et al., 2020, Smith et al., 2019). One study identified challenges of navigating healthcare delivery and insurance systems, including not knowing which reproductive services were covered under insurance, as barriers (MacAfee et al., 2020b).
3.2.7.2. Stigma and discrimination
Internalized and perceived stigmas were commonly identified barriers, including: shame/embarrassment around substance use or disclosing substance use (Armstrong et al., 1991, Florsheim et al., 2020, MacAfee et al., 2020b); and fear of: provider discrimination (Hurley et al., 2020, Leinaar et al., 2020, MacAfee et al., 2020a, MacAfee et al., 2020b), child custody loss or protective services involvement (Florsheim et al., 2020, Hurley et al., 2020, Leinaar et al., 2020, MacAfee et al., 2020b), and forced sterilization (Leinaar et al., 2020). Experienced discrimination, including overt provider judgement or discrimination, such as being denied care, was also a barrier (Armstrong et al., 1991, MacAfee et al., 2020b). Five studies identified the consequences of stigma and discrimination as barriers, including: care avoidance (Hurley et al., 2020, Leinaar et al., 2020, MacAfee et al., 2020b), and feelings of general distrust toward the healthcare system (Armstrong et al., 1991, MacAfee et al., 2020a).
3.2.8. Societal-level facilitators
3.2.8.1. Cost and structure of US healthcare system
Having insurance (MacAfee et al., 2020b) and receiving contraception at reduced or free cost (Fischbein et al., 2018, Heil et al., 2016, Heil et al., 2021, Hurley et al., 2020) were commonly reported facilitators.
4. Discussion
This scoping review identified barriers to and facilitators of HC-LARC access and use in the US among WWUO. Barriers and facilitators were commonly reported at each level of the four-level SEM framework, with a majority of studies reporting both. The most frequently cited barriers and facilitators were methods characteristics, partner and provider relationships, transportation, healthcare availability and accessibility, cost, insurance, and stigma (Fig. 2 and Table 2). Most barriers and facilitators were similar concepts but differed on whether that factor was present or absent.
Barriers and facilitators were largely consistent across studies, with two exceptions. Having Medicaid insurance was an identified barrier (Kotha et al., 2019) and a facilitator (Mastey et al., 2020) to HC-LARC use. These findings are understandable given that Mastey et al used self-pay as a reference group, rather than private insurance like Kotha et al, and insurance facilitates healthcare access. Likewise, screening positive for depression was both a barrier (Meschke et al., 2018) and a facilitator (Perry et al., 2020). We hypothesize that some women may find depression as a reason to seek out healthcare while others may not. For several other factors, we noted individual differences in whether those factors were perceived as barriers or facilitators. For example, menstrual cycle changes that occur with HC-LARC use, such as reduced bleeding, were welcomed by some participants but undesired by others. This speaks to the need for individualized contraceptive care and the importance of providers building rapport with patients to elicit contraceptive preferences prior to making method recommendations.
HC-LARC barriers and facilitators related to substance use and recovery, such as misconceptions about fertility and competing priorities, were important but in the minority. Most barriers and facilitators that we identified are universal to all women. Side effects—the most frequently cited barrier in this review—are the primary reason for dissatisfaction-related discontinuation of oral pills and LARC among US women (Moreau et al., 2007). Other commonly identified HC-LARC barriers and facilitators in the general population were also present here and included: safety; effectiveness; menstrual concerns; effects on fertility; patient-provider interactions; contraceptive experiences of family and friends; appointment accessibility; insurance; and cost (Asker et al., 2006, Berndt and Bell, 2021, Brown et al., 2019, Coates et al., 2018, Culwell and Feinglass, 2007, Kavanaugh et al., 2013, Lessard et al., 2012, Obstetricians and Gynecologists, 2015).
Our goal for this review was not to ascribe a value judgement to barriers or facilitators. Some of the factors that deter or enable HC-LARC access and use are not inherently positive or negative. For instance, we listed passive attitudes about pregnancy or pregnancy prevention as a barrier because this factor was present among women not using contraception. However, not all individuals have strong and consistent desires to avoid pregnancy nor is pregnancy planning important or attainable for all individuals, especially those whose socioeconomic circumstances do not meet the social standard of what is considered suitable for childbearing (Aiken et al., 2016). Even when a pregnancy is unplanned, it does not mean that it will be unwelcome or unwanted, as pregnancy intentions and emotional responses to pregnancy are dynamic and change over time as personal circumstances change (Aiken et al., 2016, Geist et al., 2021).
4.1. Evidence gaps and recommendations for practice
Consistent with the outlined objectives, we identified several knowledge gaps. Most studies recruited women receiving OUD treatment from clinical settings; few recruited WWUO from community-based settings. This may reflect the fact that contacting potential participants within clinical treatment settings is easier than establishing contact with people actively using in the community. Nonetheless, the drawback of this approach is that information is lacking on HC-LARC barriers and facilitators experienced by women not engaged with the healthcare system. Further research into this area would identify some of the impediments and facilitators these individuals experience in accessing care and offer insights into potential solutions. We did not find any studies focused on other marginalized groups, including black, indigenous, veteran, or rural populations. Given that individuals in these communities already experience multiple forms of social-structural marginalization, understanding the full range of their contraceptive experiences is an important step in advancing reproductive health equity.
There is an opportunity for research to further examine HC-LARC barriers and facilitators at broader levels of the SEM. Factors such as neighborhood environment, community resources, social networks, technology/media influences, cultural values, and policies were infrequently addressed in the included studies. Individual behavior is embedded within a system of overlapping interpersonal, social, and structural influences (Glanz et al., 2008). An effective approach to improve HC-LARC access and use among WWUO would simultaneously intervene at multiple levels of the social-ecological hierarchy, combining behavioral modifications with interventions at the community and societal levels (Alvidrez et al., 2019). Indeed, the four intervention studies that we reviewed were multicomponent and intervened minimally at three SEM levels, and all of them showed improvements in contraceptive outcomes at post-intervention assessment compared to baseline (Heil et al., 2016, Heil et al., 2021, Jones et al., 2021, Rinehart et al., 2021).
4.2. Strengths and limitations
Strengths of this review include the use of a rigorous methodological approach, application of a theoretical framework, and inclusion of various study designs; the main limitation is generalizability. Findings are not generalizable to non-US settings because we restricted the studies geographically to avoid having heterogenous societal contexts present. Moreover, results are not generalizable to women using non-opioid substances or barrier methods. Condoms are inexpensive, widely accessible, provide dual protection, and are the most commonly used contraceptive method among WWUO (Terplan et al., 2015). Several studies included in this review identified prevention of sexually transmitted infections as a motivator for condom use (Armstrong et al., 1991, Fischbein et al., 2018, Sobel et al., 2021). Therefore, a systematic review of barriers, facilitators, and interventions focused on condom access and use is an important topic for future work. Another limitation is that we may have missed relevant barriers and facilitators due to excluding studies in which the proportion of sample participants using opioids was not reported, though this decision improved the generalizability of results to the population of interest. Included articles may also have missed barriers and facilitators due to the challenges of identifying and distilling factors responsible for affecting contraceptive access and use, particularly among women facing multiple forms of instability, psychiatric comorbidities, or pregnancy ambivalence. Finally, we categorized barriers and facilitators according to a priori codes and assigned subjective labels; other researchers may have coded and organized barriers and facilitators in an alternate manner.
5. Conclusion
This scoping review assessed the breadth of existing literature from 1990 to 2021 on barriers of and facilitators to HC-LARC access and use in the US among reproductive-aged WWUO. We identified numerous barriers and facilitators across four levels of the SEM framework. Future studies would benefit from recruiting participants and collecting data in community settings, targeting more diverse populations, and identifying neighborhood, social, and policy barriers and facilitators. Reducing barriers and improving equity in HC-LARC access and use among WWUO is a complex, multifaceted issue. Multilevel, multicomponent interventions targeting modifiable factors simultaneously across social-ecological hierarchy may provide the best path forward to effect change.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
WWUO = women who use opioids.
HC-LARC = hormonal and long-acting reversible contraception.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2023.102111.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
Data availability
No data was used for the research described in the article.
References
- Aiken A.R., Borrero S., Callegari L.S., Dehlendorf C. Rethinking the pregnancy planning paradigm: unintended conceptions or unrepresentative concepts? Perspect. Sex Reprod. Health. 2016;48:147–151. doi: 10.1363/48e10316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alvidrez J., Castille D., Laude-Sharp M., Rosario A., Tabor D. The national institute on minority health and health disparities research framework. Am. J. Public Health. 2019;109:S16–S20. doi: 10.2105/AJPH.2018.304883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arksey H., O'Malley L. Taylor and Francis Group Ltd; 2005. Scoping studies: Towards a Methodological Framework, International Journal of Social Research Methodology: Theory and Practice; pp. 19–32. [Google Scholar]
- Armstrong K.A., Kenen R., Samost L. Barriers to family planning services among patients in drug treatment programs. Fam. Plann. Perspect. 1991;23(264–6):70. [PubMed] [Google Scholar]
- Asker C., Stokes-Lampard H., Beavan J., Wilson S. What is it about intrauterine devices that women find unacceptable? Factors that make women non-users: a qualitative study. J. Fam. Plann. Reprod. Health Care. 2006;32:89–94. doi: 10.1783/147118906776276170. [DOI] [PubMed] [Google Scholar]
- Beller E.M., Glasziou P.P., Altman D.G., Hopewell S., Bastian H., Chalmers I., Gøtzsche P.C., Lasserson T., Tovey D., et al. PRISMA for abstracts: reporting systematic reviews in journal and conference abstracts. PLoS Med. 2013;10:e1001419. doi: 10.1371/journal.pmed.1001419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berndt V.K., Bell A.V. “This is what the truth is”: provider-patient interactions serving as barriers to contraception. Health (London) 2021;25:613–629. doi: 10.1177/1363459320969775. [DOI] [PubMed] [Google Scholar]
- Black, K.I., Day, C.A., 2016. Improving access to long-acting contraceptive methods and reducing unplanned pregnancy among women with substance use disorders. Substance abuse: research and treatment 10:SART. S34555. [DOI] [PMC free article] [PubMed]
- Bornstein M., Gipson J.D., Bleck R., Sridhar A., Berger A. Perceptions of pregnancy and contraceptive use: an in-depth study of women in Los Angeles methadone clinics. Womens Health Issues. 2019;29:176–181. doi: 10.1016/j.whi.2018.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown B.P., Chor J., Hebert L.E., Webb M.E., Whitaker A.K. Shared negative experiences of long-acting reversible contraception and their influence on contraceptive decision-making: a multi-methods study. Contraception. 2019;99:228–232. doi: 10.1016/j.contraception.2019.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coates C., Gordon C.M., Simpson T. A qualitative study exploring contraceptive practices and barriers to long-acting reversible contraceptive use in a sample of adolescents living in the southern United States. J. Pediatr. Adolesc. Gynecol. 2018;31:605–669. doi: 10.1016/j.jpag.2018.07.006. [DOI] [PubMed] [Google Scholar]
- Collier K.W., MacAfee L.K., Kenny B.M., Meyer M.C. Does co-location of medication assisted treatment and prenatal care for women with opioid use disorder increase pregnancy planning, length of interpregnancy interval, and postpartum contraceptive uptake? J. Subst. Abuse Treat. 2019;98:73–77. doi: 10.1016/j.jsat.2018.12.001. [DOI] [PubMed] [Google Scholar]
- Covidence systematic review software, V.H.I., Melbourne, Australia. Available at www.covidence.org.
- Culwell K.R., Feinglass J. The association of health insurance with use of prescription contraceptives. Perspect. Sex Reprod. Health. 2007;39:226–230. doi: 10.1363/3922607. [DOI] [PubMed] [Google Scholar]
- Fischbein R.L., Lanese B.G., Falletta L., Hamilton K., King J.A., Kenne D.R. Pregnant or recently pregnant opioid users: contraception decisions, perceptions and preferences. Contracept. Reprod. Med. 2018;3:4. doi: 10.1186/s40834-018-0056-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Florsheim O.K., Augustine D., Van Ligten M.M., Thiel de Bocanegra H., Perry R. Understanding contraceptive needs of women who inject drugs in orange county: a qualitative study. J. Addict. Med. 2020;14:14. doi: 10.1097/ADM.0000000000000795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale N.K., Heath G., Cameron E., Rashid S., Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. BioMed Central. 2013:117. doi: 10.1186/1471-2288-13-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geist C., Everett B.G., Simmons R.G., Sanders J.N., Gawron L.M., Myers K., Turok D.K. Changing lives, dynamic plans: prospective assessment of 12-month changes in pregnancy timing intentions and personal circumstances using data from HER Salt Lake. PLoS One. 2021;16:e0257411. doi: 10.1371/journal.pone.0257411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gipson J.D., Bornstein M., Berger A., Rocca C.H. Desire to avoid pregnancy and contraceptive use among female methadone patients in Los Angeles. Contraception. 2021;103:322–337. doi: 10.1016/j.contraception.2021.01.019. [DOI] [PubMed] [Google Scholar]
- Glanz K., Rimer B.K., Viswanath K. John Wiley & Sons; 2008. Health Behavior and Health Education: Theory, Research, and Practice. [Google Scholar]
- Haight S.C., Ko J.Y., Tong V.T., Bohm M.K., Callaghan W.M. Opioid use disorder documented at delivery hospitalization - United States, 1999–2014. MMWR Morb. Mortal Wkly. Rep. 2018;67:845–889. doi: 10.15585/mmwr.mm6731a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handy C.J., Lange H.L.H., Manos B.E., Berlan E.D., Bonny A.E. A retrospective chart review of contraceptive use among adolescents with opioid use disorder. J. Pediatr. Adolesc. Gynecol. 2018;31:122–217. doi: 10.1016/j.jpag.2017.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hathazi D., Lankenau S.E., Sanders B., Jackson Bloom J. Pregnancy and sexual health among homeless young injection drug users. J. Adolesc. 2009;32:339–355. doi: 10.1016/j.adolescence.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heil S.H., Hand D.J., Sigmon S.C., Badger G.J., Meyer M.C., Higgins S.T. Using behavioral economic theory to increase use of effective contraceptives among opioid-maintained women at risk of unintended pregnancy. Prev. Med. 2016;92:62–67. doi: 10.1016/j.ypmed.2016.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heil S.H., Melbostad H.S., Matusiewicz A.K., Rey C.N., Badger G.J., Shepard D.S., Sigmon S.C., MacAfee L.K., Higgins S.T. Efficacy and cost-benefit of onsite contraceptive services with and without incentives among women with opioid use disorder at high risk for unintended pregnancy: a randomized clinical trial. J. Am. Med. Assoc. Psychiat. 2021;14:14. doi: 10.1001/jamapsychiatry.2021.1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurley E.A., Duello A., Finocchario-Kessler S., Goggin K., Stancil S., Winograd R.P., Miller M.K. Expanding contraception access for women with opioid-use disorder: a qualitative study of opportunities and challenges. Am. J. Health Promot. 2020;34:909–918. doi: 10.1177/0890117120927327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jarlenski M., Barry C.L., Gollust S., Graves A.J., Kennedy-Hendricks A., Kozhimannil K. Polysubstance use among US women of reproductive age who use opioids for nonmedical reasons. Am. J. Public Health. 2017;107:1308–1310. doi: 10.2105/AJPH.2017.303825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jenkins R.A. The fourth wave of the US opioid epidemic and its implications for the rural US: a federal perspective. Prev. Med. 2021;152 doi: 10.1016/j.ypmed.2021.106541. [DOI] [PubMed] [Google Scholar]
- Jones H.E., Martin C.E., Andringa K.R., Ellerson R.M., Johnson E., Hairston E., Ke O.G. Sex and female empowerment (SAFE): a randomized trial comparing sexual health interventions for women in treatment for opioid use disorder. Drug Alcohol Depend. 2021;221 doi: 10.1016/j.drugalcdep.2021.108634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kavanaugh M.L., Jerman J., Ethier K., Moskosky S. Meeting the contraceptive needs of teens and young adults: youth-friendly and long-acting reversible contraceptive services in U.S. family planning facilities. J. Adolesc. Health. 2013;52:284–292. doi: 10.1016/j.jadohealth.2012.10.276. [DOI] [PubMed] [Google Scholar]
- Kotha A., Chen B.A., Lewis L., Dunn S., Himes K.P., Krans E.E. Prenatal intent and postpartum receipt of long-acting reversible contraception among women receiving medication-assisted treatment for opioid use disorder. Contraception. 2019;99:36–41. doi: 10.1016/j.contraception.2018.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krans E.E., Bobby S., England M., Gedekoh R.H., Chang J.C., Maguire B., Genday P., English D.H. The Pregnancy Recovery Center: a women-centered treatment program for pregnant and postpartum women with opioid use disorder. Addict. Behav. 2018;86:124–219. doi: 10.1016/j.addbeh.2018.05.016. [DOI] [PubMed] [Google Scholar]
- Krug, E.G., Dahlberg, L.L., Mercy, J.A., Zwi, A.B., Lozano, R., 2002. Violence: a global public health problem. World report on violence and health: 3-21.
- Leinaar E., Johnson L., Yadav R., Rahman A., Alamian A. Healthcare access, pregnancy intention, and contraceptive practices among reproductive-aged women receiving opioid agonist therapy in northeast Tennessee. South. Med. J. 2019;112:382–436. doi: 10.14423/SMJ.0000000000000990. [DOI] [PubMed] [Google Scholar]
- Leinaar E., Brooks B., Johnson L., Alamian A. Perceived barriers to contraceptive access and acceptance among reproductive-age women receiving opioid agonist therapy in northeast Tennessee. South. Med. J. 2020;113:213–228. doi: 10.14423/SMJ.0000000000001095. [DOI] [PubMed] [Google Scholar]
- Lessard L.N., Karasek D., Ma S., Darney P., Deardorff J., Lahiff M., Grossman D., Foster D.G. Contraceptive features preferred by women at high risk of unintended pregnancy. Perspect. Sex. Reprod. Health. 2012;44:194–200. doi: 10.1363/4419412. [DOI] [PubMed] [Google Scholar]
- MacAfee L.K., Harfmann R.F., Cannon L.M., Kolenic G., Kusunoki Y., Terplan M., Dalton V.K. Sexual and reproductive health characteristics of women in substance use treatment in Michigan. Obstet. Gynecol. 2020;135:361–439. doi: 10.1097/AOG.0000000000003666. [DOI] [PubMed] [Google Scholar]
- MacAfee L.K., Harfmann R.F., Cannon L.M., Minadeo L., Kolenic G., Kusunoki Y., Dalton V.K. Substance use treatment patient and provider perspectives on accessing sexual and reproductive health services: barriers, facilitators, and the need for integration of care. Subst. Use Misuse. 2020;55:95–107. doi: 10.1080/10826084.2019.1656255. [DOI] [PubMed] [Google Scholar]
- Mastey N., Roe A.H., Maurer R., Janiak E., Goldberg A.B. Contraception after surgical abortion in patients with opioid use disorder. Womens Health Issues. 2020;27:27. doi: 10.1016/j.whi.2020.11.012. [DOI] [PubMed] [Google Scholar]
- Matusiewicz A.K., Melbostad H.S., Heil S.H. Knowledge of and concerns about long-acting reversible contraception among women in medication-assisted treatment for opioid use disorder. Contraception. 2017;96:365–439. doi: 10.1016/j.contraception.2017.07.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGowan J., Sampson M., Salzwedel D.M., Cogo E., Foerster V., Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J. Clin. Epidemiol. Elsevier USA. 2016:40–46. doi: 10.1016/j.jclinepi.2016.01.021. [DOI] [PubMed] [Google Scholar]
- McNeely C.A., Hutson S., Sturdivant T.L., Jabson J.M., Isabell B.S. Expanding contraceptive access for women with substance use disorders: partnerships between public health departments and county jails. J. Public Health Manag. Pract. 2019;25:229–237. doi: 10.1097/PHH.0000000000000850. [DOI] [PubMed] [Google Scholar]
- Meschke L.L., McNeely C., Brown K.C., Prather J.M. Reproductive health knowledge, attitudes, and behaviors among women enrolled in medication-assisted treatment for opioid use disorder. J. Womens Health. 2018;27:1215–1224. doi: 10.1089/jwh.2017.6564. [DOI] [PubMed] [Google Scholar]
- Moher D., Shamseer L., Clarke M., Ghersi D., Liberati A., Petticrew M., Shekelle P., Stewart L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015;4:1–9. doi: 10.1186/2046-4053-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreau C., Cleland K., Trussell J. Contraceptive discontinuation attributed to method dissatisfaction in the United States. Contraception. 2007;76:267–272. doi: 10.1016/j.contraception.2007.06.008. [DOI] [PubMed] [Google Scholar]
- NIDA, 2020. Sex and Gender Differences in Substance Use, Drug Facts.
- Obstetricians, A.C.o., Gynecologists, 2015. Committee opinion no. 615: access to contraception. Obstetrics & Gynecology 125:250-255. [DOI] [PubMed]
- Parlier A.B., Fagan B., Ramage M., Galvin S. Prenatal care, pregnancy outcomes, and postpartum birth control plans among pregnant women with opiate addictions. South. Med. J. 2014;107:676–683. doi: 10.14423/SMJ.0000000000000189. [DOI] [PubMed] [Google Scholar]
- Perry R., Landrian A., McQuade M., Thiel de Bocanegra H. Contraceptive need, intimate partner violence, and reproductive coercion among women attending a syringe exchange program. J. Addict. Med. 2020;14:e70–e75. doi: 10.1097/ADM.0000000000000579. [DOI] [PubMed] [Google Scholar]
- Peters, M., Godfrey, C., McInerney, P., Munn, Z., Trico, A., Khalil, H., 2020. Chapter 11: Scoping Reviews, JBI Manual for Evidence Synthesis. JBI.
- Peters M.D.J., Godfrey C.M., Khalil H., McInerney P., Parker D., Soares C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid.-Based Healthcare. Lippincott Williams and Wilkins. 2015:141–216. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- Rethlefsen M.L., Kirtley S., Waffenschmidt S., Ayala A.P., Moher D., Page M.J., Koffel J.B. PRISMA-S: an extension to the PRISMA statement for reporting literature searches in systematic reviews. Syst. Rev. 2021;10:1–19. doi: 10.1186/s13643-020-01542-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rey C.N., Badger G.J., Melbostad H.S., Wachtel D., Sigmon S.C., MacAfee L.K., Dougherty A.K., Heil S.H. Perceptions of long-acting reversible contraception among women receiving medication for opioid use disorder in Vermont. Contraception. 2020;101:333–337. doi: 10.1016/j.contraception.2020.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rinehart D.J., Stowell M., Collings A., Durfee M.J., Thomas-Gale T., Jones H.E., Binswanger I. Increasing access to family planning services among women receiving medications for opioid use disorder: a pilot randomized trial examining a peer-led navigation intervention. J. Subst. Abuse Treat. 2021;126 doi: 10.1016/j.jsat.2021.108318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith C., Morse E., Busby S. Barriers to reproductive healthcare for women with opioid use disorder. J. Perinat. Neonatal Nurs. 2019;33:E3–E11. doi: 10.1097/JPN.0000000000000401. [DOI] [PubMed] [Google Scholar]
- Sobel L., Lee Y.W., White K.O., Woodhams E., Patton E. Contraceptive decision making among pregnancy-capable individuals with opioid use disorder at a tertiary care center in Massachusetts. Contraception. 2021;10:10. doi: 10.1016/j.contraception.2021.06.002. [DOI] [PubMed] [Google Scholar]
- Stone R.H., Griffin B., Fusco R.A., Vest K., Tran T., Gross S. Factors affecting contraception access and use in patients with opioid use disorder. J. Clin. Pharmacol. 2020:S63–S73. doi: 10.1002/jcph.1772. [DOI] [PubMed] [Google Scholar]
- Terplan M., Hand D.J., Hutchinson M., Salisbury-Afshar E., Heil S.H. Contraceptive use and method choice among women with opioid and other substance use disorders: a systematic review. Prev. Med. 2015;80:23–31. doi: 10.1016/j.ypmed.2015.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tricco A.C., Lillie E., Zarin W., O'Brien K.K., Colquhoun H., Levac D., Moher D., Peters M.D.J., Horsley T., et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Internal Med. American College of Physicians. 2018:467. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No data was used for the research described in the article.