Abstract
Background:
Preoperative anemia is common and associated with adverse postoperative outcomes. Assessment of hemoglobin concentrations may facilitate optimization prior to surgery. However, phlebotomy-based hemoglobin measurement may contribute to patient discomfort and iatrogenic blood loss, which makes non-invasive hemoglobin estimation attractive in this setting.
Study Design and Methods:
This is a prospective study of adult patients presenting for preoperative evaluation before elective surgery at a tertiary care medical center. The Masimo Pronto Pulse CO-Oximeter was utilized to estimate blood hemoglobin concentrations (SpHb), which were then compared with hemoglobin concentrations obtained via complete blood count. Receiver operating curves were used to identify SpHb values maximizing specificity for anemia detection while meeting a minimum sensitivity of 80%.
Results:
A total of 122 patients were recruited with median (interquartile range) age of 66 (58, 72) years. SpHb measurements were obtained in 112 patients (92%). SpHb generally overestimated hemoglobin with a mean (± 1.96 × standard deviation) difference of 0.8 (−2.2, 3.9) g/dL. Preoperative anemia, defined by hemoglobin <12.0 g/dL in accordance with institutional protocol, was present in 22 patients (20%). The optimal SpHb cut-point to identify anemia was 13.5 g/dL: sensitivity 86%, specificity 81%, negative predictive value 96%, positive predictive value 53%. Utilizing this cut-point, 60% (73/122) of patients could have avoided phlebotomy-based hemoglobin assessment, while an anemia diagnosis would have been missed in <3% (3/122).
Conclusion:
The use of SpHb devices for anemia screening in surgical patients is feasible with the potential to reliably rule-out anemia despite limited accuracy.
Keywords: anemia, hemoglobin, preoperative, surgery, non-invasive
Introduction:
Anemia is frequently encountered prior to surgical intervention, though its prevalence varies greatly depending on the study population.1–3 Preoperative anemia is an established risk factor for adverse perioperative outcomes, including allogeneic transfusion, renal dysfunction, pulmonary complications, prolonged hospitalization, and mortality.1,3–7 Thus, anemia identification and management prior to surgery may result in improved patient outcomes, including enhanced hemoglobin recovery, reduced transfusion requirements, and fewer hospital readmissions.8–10 Appropriate and timely diagnosis of anemia involves assessment of hemoglobin concentrations, which is typically performed through invasive laboratory testing. However, phlebotomy may be uncomfortable for patients and contributes to blood loss, even though the volume required for sampling is low. Further, venipuncture for hemoglobin assessment may potentially be of limited clinical utility in patients subsequently discovered to be non-anemic.
Non-invasive hemoglobin measurement (e.g., SpHb, Masimo, Irvine, California) represents a potential alternative for anemia screening prior to surgery that is free of any direct patient harm, easy to perform, and provides near-instantaneous results, making it particularly convenient in the setting of patient evaluation with narrow timeframes preceding intervention. While SpHb hemoglobin assessment has been shown to have similar accuracy compared to other invasive alternatives to venipuncture,11 imperfect correlation with gold-standard hemoglobin concentrations obtained via complete blood counts (CBC) on hematology analyzers has thus far limited clinical implementation despite convenience and ease of use.12,13 However, non-invasive hemoglobin assessment may still hold utility as an anemia screening tool in elective surgical patients. Specifically, non-invasive hemoglobin sensors such as SpHb could potentially be employed to exclude the presence of preoperative anemia with a high degree of certainty, thereby saving patients from additional, albeit more thorough, laboratory testing; though studies are needed to determine SpHb values that optimize performance. A recent study that evaluated the use of SpHb for anemia screening in patients undergoing surgical intervention has shown promising results.14
The goal of this investigation is to assess the utility of SpHb as a screening tool to reliably rule out the presence of anemia. Secondarily, we assess the relationships between SpHb-derived hemoglobin concentrations and hemoglobin concentrations obtained by CBC.
Methods:
This prospective observational cohort study was initiated as a quality improvement project in the Mayo Clinic Preoperative Evaluation (POE) Clinic in Rochester, Minnesota with waived requirement for written informed consent by the local Institutional Review Board (IRB). All consecutive adult patients (age ≥18 years) presenting for preoperative evaluation prior to elective surgery in the POE Clinic from June 1, 2021 to August 31, 2021 for whom a CBC order was to be placed as part of routine preoperative care were considered eligible. Patients could only be included once. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines were used in study conduct and reporting of results.15
Blood samples for CBC assessment were obtained via venous sampling by trained phlebotomy professionals and immediately sent to a clinical laboratory for analysis on a Sysmex XN-9000 automated hematology analyzer. Immediately following phlebotomy sampling (i.e., within 10 minutes and prior to laboratory analysis of CBC samples), SpHb measurements were obtained using the Masimo Pronto Pulse CO-Oximeter with an Adult Reusable Sensor. The sensor was placed on the patient’s ring finger ipsilateral to the site of phlebotomy. After the device completed self-calibration as indicated by a visual loading graph and an audible sound, the estimated hemoglobin concentration was recorded by trained personnel. This entire process from turning on the monitor, moving through self-calibration, and displaying results occurred over approximately 1 minute. If the device failed to provide a reading, a second attempt was made using the middle finger on the same hand. If this still proved unsuccessful, a third and final attempt was performed using the ring finger on the opposite hand. Using the same device, perfusion index (PI) values were collected as a quality control indicator of pulse strength, although these values were not routinely recorded during the first month of the project. PI values range from 0.02% (very weak) to 20% (very strong) and represent the ratio of pulsatile to non-pulsatile blood flow at the anatomic site of the SpHb sensor. When an SpHb measurement could not be obtained, this was documented as not available. Standard laboratory CBC results were extracted from the electronic medical record within 24 hours of measurement and recorded in the same electronic database. Hemoglobin concentrations from CBC assessments were used as the gold-standard reference for true hemoglobin concentrations.
Statistical analysis:
Baseline demographic, clinical, and laboratory features are summarized as counts (%) and median (interquartile range) for categorical and continuous data elements, respectively. Anemia was defined as a hemoglobin concentration <12.0 g/dL irrespective of patient gender given that this was the hemoglobin threshold employed in our preoperative anemia protocol at the time of the study. Secondarily, anemia was defined using a gender-neutral anemia definition of <13.0 g/dL, as has been recommended in previous preoperative anemia research,7 and using World Health Organization (WHO) definitions of hemoglobin concentrations <12.0 g/dL in women and <13.0 g/dL in men.16
The primary objectives of the study were: 1) to determine the feasibility of SpHb assessment in the preoperative setting, defined by SpHb attainment in >90% of patients, and 2) to assess the utility of SpHb as an anemia screening tool by identifying SpHb values that maximize specificity while meeting a minimum sensitivity threshold of 80%. Restated, we wanted to ensure a high negative predictive value (NPV) such that SpHb values indicating non-anemic status for any given patient would indeed have a high probability of representing the absence of anemia on gold-standard CBC testing (i.e., minimizing false negatives). As the current gold-standard for patients scheduled for surgery with moderate-to-high blood loss risk in our POE clinic is to obtain CBC assessment, a tool that provides hemoglobin predictions that are highly sensitive with high NPV could be employed to reliably exclude the presence of anemia and potentially prevent unnecessary phlebotomy for hemoglobin assessment. Positive predictive value (PPV) and specificity are less of a concern in this setting, as CBC testing is currently the standard practice for all patients and would still be performed for those with SpHb values indicating the potential presence of anemia. Receiver operating characteristic (ROC) curves were created with available SpHb concentrations using the aforementioned anemia definitions. SpHb values that optimized test specificity subject to a minimum sensitivity of 80% were reported as optimal SpHb anemia screening cut-offs.
Beyond identifying optimal SpHb values, we also aimed to determine the relationships between SpHb values and gold-standard CBC hemoglobin concentrations. A Bland-Altman plot was used to evaluate overall agreement between SpHb and CBC hemoglobin concentrations, by plotting differences in SpHb values and CBC hemoglobin concentrations (y-axis) versus the mean of SpHb and CBC hemoglobin concentrations (x-axis). Limits of agreement (LOA) were calculated based on the mean and standard deviation (SD) of the observed differences (mean ± 1.96 × SD) between SpHb and CBC hemoglobin measurements and represents an interval which can be expected to contain 95% of all differences. As additional exploratory analyses, we describe differences in patient demographic and clinical features and PI values based upon the presence or absence of a successful SpHb reading. Wilcoxon rank sum tests and Fisher’s exact tests were employed for continuous and categorical data elements, respectively. The correlation between PI values and the SpHb-CBC hemoglobin difference was assessed with Spearman’s correlation coefficients, and ROC curves were evaluated for SpHb readings above and below a threshold PI value of 2. As this study was conducted as a pre-defined 3-month quality improvement project, a formal power analysis was not performed. For all comparisons, a p-value <0.05 was used to define statistical significance.
Results
A total of 122 patients were approached for SpHb measurement during the study period. An SpHb measurement was unable to be obtained in 10 (8%) patients, leaving 112 unique patients with paired SpHb and CBC hemoglobin concentrations (Figure 1). Patients without successful SpHb assessment (n=10) had lower CBC hemoglobin concentrations (12.2 [9.9, 12.7] g/dL vs. 13.8 [12.5, 14.7] g/dL), lower PI values (0.8% [0.3, 1.0] vs. 2.8% [1.6, 4.8]), and differences in self-identified race (80% White vs. 96% White) compared to those with successful SpHb assessment (Supplemental Table). Among those with available SpHb assessments (n=112), the median age was 66 (58, 72) years with equal female and male representation (Table 1). Hypertension (60%), solid tumors (40%), diabetes mellitus (13%) and chronic kidney disease (11%) were the most common medical comorbidities. The most frequent surgery types, in descending order, were orthopedics (32%), neurological and spine surgery (26%), urology (11%), and cardiovascular surgery (9%).
Figure 1.

Study flow diagram
Table 1:
Baseline demographic and clinical features (n=112)
| Age, years | 66 (58, 72) |
| Body Mass Index, kg/m2 | 29 (26, 35) |
| Gender, Female | 56 (50) |
| Race/Ethnicity | |
| White | 108 (96) |
| American Indian | 1 (1) |
| Black | 0 (0) |
| Other | 2 (2) |
| Hispanic Ethnicity | 2 (2) |
| Comorbidities | |
| Myocardial Infarction | 5 (4) |
| Congestive Heart Failure | 6 (5) |
| Hypertension | 67 (60) |
| Chronic Kidney Disease | 12 (11) |
| Peripheral Vascular Disease | 5 (4) |
| CVA/TIA | 7 (6) |
| Dementia | 1 (1) |
| COPD | 4 (4) |
| Connective Tissue Disease | 5 (4) |
| Peptic Ulcer Disease | 2 (2) |
| Liver Disease | 3 (3) |
| Diabetes Mellitus | 14 (13) |
| Hemiplegia | 1 (<1) |
| Cancer (solid tumor) | 45 (40) |
| Raynaud’s | 2 (2) |
| Surgical Service | |
| Orthopedic | 36 (32) |
| Neurological, Spine | 29 (26) |
| Urology | 12 (11) |
| Cardiovascular | 10 (9) |
| Head and Neck | 7 (6) |
| Hepatobiliary and Pancreas | 6 (5) |
| Colon and Rectal | 4 (4) |
| Interventional Radiology | 3 (3) |
| Oral and Maxillofacial | 2 (2) |
| Endocrine and Metabolic | 1 (<1) |
| GYN | 1 (<1) |
| General Surgery | 1 (<1) |
CVA/TIA: Cerebrovascular Accident/Transient Ischemic Attack; COPD: Chronic Obstructive Pulmonary Disease; GYN: Gynecology. Values represent median (IQR) or count (%) for continuous and categorical data, respectively.
Median hemoglobin concentrations by SpHb and CBC were 14.5 g/dL (13.2, 15.4) and 13.8 g/dL (12.5, 14.7), respectively. Twenty-two (20%) patients had CBC hemoglobin concentrations <12.0 g/dL, and 25 (22%) met WHO anemia criteria. The mean (LOA) difference between SpHb values and CBC-derived hemoglobin concentrations was 0.8 (−2.2, 3.9) g/dL with higher hemoglobin concentrations generally observed for SpHb (Figure 2). The mean (LOA) differences for women and men were 1.0 (−2.3, 4.4) g/dL and 0.7 (−1.9, 3.2) g/dL, respectively.
Figure 2.
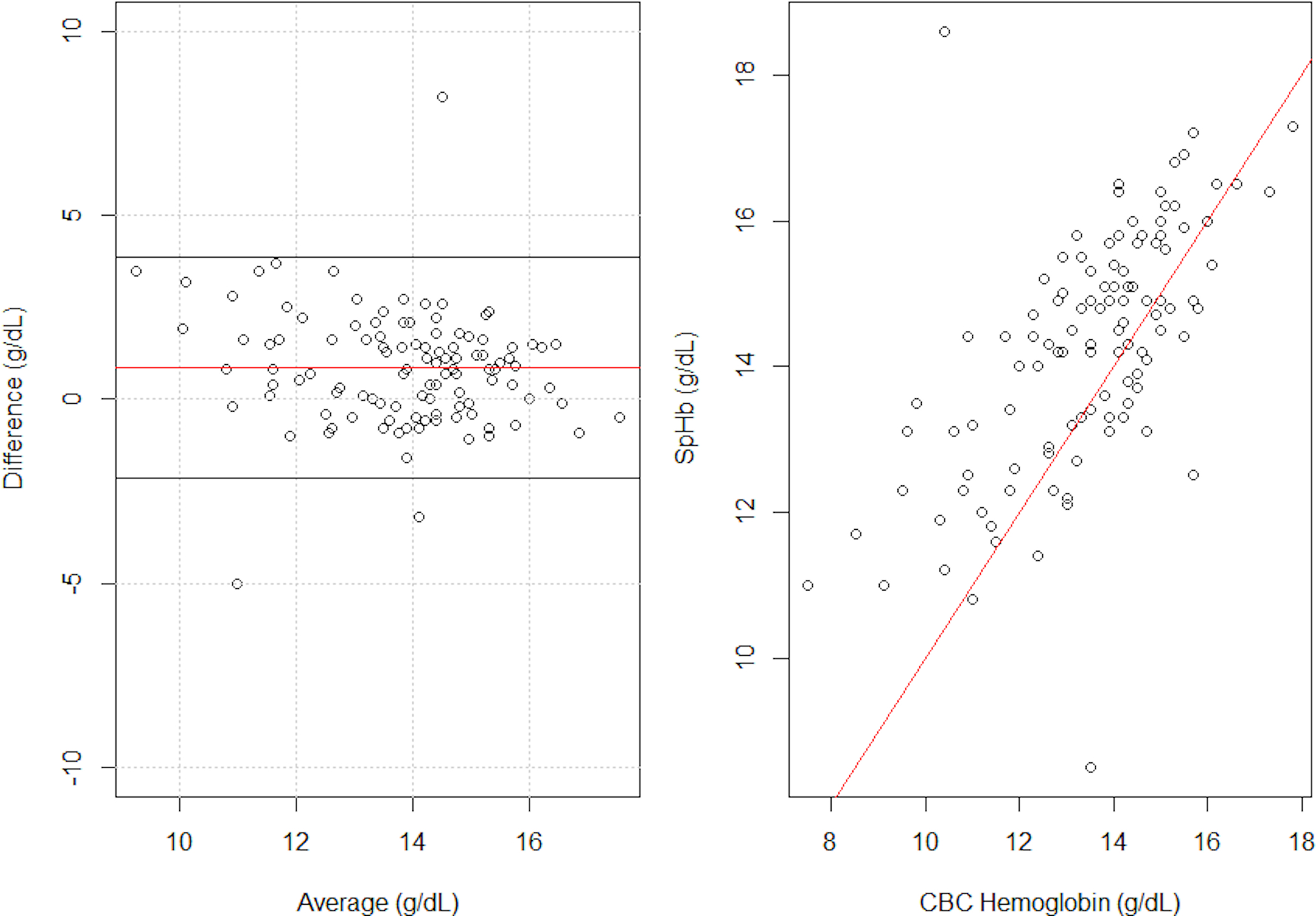
Bland Altman and scatter plot between SpHb and CBC hemoglobin measurements
Left panel represents Bland Altman plot showing the difference between SpHb and CBC hemoglobin measurements (y-axis) by the average (x-axis), with the horizontal lines representing the mean difference and 95% limits of agreement. Right panel represents a scatter plot of SpHb by CBC hemoglobin measurements, with the line representing SpHb = CBC hemoglobin.
Employing a gender-neutral CBC hemoglobin threshold of 12.0 g/dL to define anemia, the optimal hemoglobin concentration SpHb cut-point was 13.5 g/dL with an Area Under Curve (AUC) of 0.87, sensitivity of 86%, specificity 81%, NPV 96%, and PPV 53% (Figure 3). At this SpHb threshold, there were 73 true negative readings and 3 false negatives, such that 60% of all patients (73/122) could have successfully avoided CBC-based hemoglobin assessment prior to surgery and <3% (3/122) would have had their anemia diagnosis missed without CBC assessment. Paired SpHb-CBC hemoglobin concentrations for these 3 patients were: 14.4 g/dL – 11.7 g/dL, 14.4 g/dL – 10.9 g/dL, and 18.6 g/dL – 10.4 g/dL. ROC characteristics using WHO anemia definitions and a gender-neutral definition of <13.0 g/dL are provided in Table 2, with AUCs ranging from 0.80 – 0.88 and NPV values ranging from 88 – 97%.
Figure 3.

Receiver operating characteristic curves for SpHb detection of anemia using gender-neutral definitions of hemoglobin <12.0 g/dL (black) and <13.0 g/dL (gray)
Table 2:
Receiver operating characteristic curve features
| CBC Hb (g/dL) | SpHb (g/dL) | Sensitivity | Specificity | NPV | PPV | AUC |
|---|---|---|---|---|---|---|
|
| ||||||
| Hb < 12.0 | 13.5 | 86.4% | 81.1% | 96.1% | 52.8% | 0.87 |
| Hb < 13.0 | 14.4 | 82.1% | 67.1% | 87.5% | 57.1% | 0.80 |
| WHO definitions | ||||||
| Female Hb < 12.0 | 13.5 | 92.3% | 76.7% | 97.1% | 54.5% | 0.84 |
| Male Hb < 13.0 | 14.4 | 83.3% | 72.7% | 94.1% | 45.5% | 0.88 |
CBC Hb: hemoglobin concentration as measured by complete blood count; SpHb: non-invasive hemoglobin concentration cut point; Hb: hemoglobin concentration; CBC: complete blood count; NPV: Negative Predictive Value; PPV: Positive Predictive Value; AUC: Area Under Curve; WHO definitions: World Health Organization criteria for anemia (Hb <12.0 g/dL in females and Hb <13.0 g/dL in males).
Among the 112 patients with successful SpHb readings, PI values were recorded by the study team for 89 (79%). PI values were not correlated with the SpHb-CBC hemoglobin difference (Spearman p −0.065, p=0.55). ROC characteristics for those with PI values ≥2 (n=58) employing an anemia definition of hemoglobin <12.0 g/dL revealed an optimal SpHb cut-point of 13.6 g/dL (AUC 0.92, sensitivity 88%, specificity 86%, NPV 98%, and PPV 50%). For those with PI <2 (n=31), the optimal SpHb cut-point was 13.2 g/dL (AUC 0.93, sensitivity 100%, specificity 85%, NPV 100%, PPV 78%).
Discussion
SpHb measurements using Masimo Pronto Pulse CO-Oximeter were able to be obtained in more than 90% of patients presenting for preoperative evaluation prior to elective surgery. Further, SpHb values greater than or equal to 13.5 g/dL had NPV greater than 95% for anemia, suggesting that the device can be reliably employed in this patient population to rule out, as opposed to confirm, the presence of preoperative anemia. SpHb generally overestimated the true hemoglobin concentration by approximately 1.0 g/dL, though with wide limits of agreement. Although PI values were lower in patients unable to attain a SpHb reading, these values were not correlated with SpHb accuracy.
Non-invasive hemoglobin estimation devices have been compared to invasive point of care (POC) devices in various clinical settings with disparate findings. For example, a study comparing the Masimo Pronto-7 SpHb and the invasive HemoCue 201+ found both devices had comparable performance among adult and pediatric patients in the outpatient setting,11 while others have noted inferior performance of non-invasive devices for anemia screening in refugees, blood donors, and surgical patients.12,17,18 With regards to performance against traditional hematology analyzers, non-invasive hemoglobin estimates generally fall within 1–2 g/dL of gold-standard laboratory-based hemoglobin measurements.13,19 Therefore, non-invasive estimations of hemoglobin concentrations using SpHb and similar technologies, in isolation, are generally not suitable at present for clinical decisions dependent on highly accurate assessments of hemoglobin concentrations.12–14,19
Nonetheless, the potential applications of non-invasive hemoglobin devices as perioperative anemia screening tools should not be overlooked. Several groups have evaluated various non-invasive hemoglobin sensors in the preoperative setting. In a recent study from a preoperative clinic in Singapore, SpHb values were obtained via the Masimo Rad-67 Rainbow sensor in more than 99% of approached subjects.20 Sensitivity and specificity were 62% and 88%, respectively, for the detection of hemoglobin concentrations <13.0 g/dL, leading the authors to conclude further technological advancement is necessary before routine preoperative use. In a similar study from Australia, patients were screened for anemia preoperatively with the Masimo Pronto-7.21 SpHb measurements were unable to be obtained in 20% of patients, which the authors attributed largely to technical failures including the use of an inappropriately sized finger probe. Sensitivity and specificity to detect anemia using WHO definitions were 57% and 82%, respectively, in women and 92% and 74% in men, with the authors concluding that SpHb may be reasonably considered for preoperative anemia identification in men rather than women. Finally, in a study from Germany, SpHb measurements using the Masimo Pronto Rad-67 were obtained in 99% of participants, with a bias of 0.2 g/dL and LOA from −2.5 g/dL to 2.8 g/dL compared to hematology analyzers.14 Although this performance was deemed not clinically acceptable to replace laboratory hemoglobin assessment, pre-defined SpHb cut-off values of 14.6 g/dL and 15.2 g/dL in women and men, respectively, resulted in sensitivities of 98.8% and 96.4% for the detection of anemia using WHO definitions. At these SpHb cut-off values, invasive hemoglobin testing could have been avoided in 28% of men and 9% of women.
The findings of the current investigation using the Masimo Pronto Pulse CO-Oximeter have several notable consistencies with previous investigations, including a high rate of feasibility (i.e., successful measurement in >90% of patients), general overestimation of laboratory-based hemoglobin concentrations with wide limits of agreement, and limited utility in ruling in the presence of anemia (i.e., moderate-to-low specificity and positive predictive value). However, recognizing that a major goal of preoperative evaluation is to exclude the presence of clinically actionable anemia, this investigation suggests that SpHb may be beneficial for this purpose. Using a predefined minimum sensitivity of 80%, SpHb had a 96% negative predictive value, such that 60% of patients could have avoided invasive hemoglobin assessment prior to surgery with less than 3% proceeding to the operating room with a missed anemia diagnosis. These results were generally consistent for men and women. Importantly, previous work has shown that thrombocytopenia, the other major finding on a CBC of potential significance for elective surgical patients, is extraordinarily rare in those without concurrent anemia or a known history of thrombocytopenia (<1% of patients);22 hence a low likelihood of anemia also implies a low likelihood of clinically actionable thrombocytopenia, lending further support to the safety of excluding preoperative CBC assessment in those with SpHb concentrations above threshold. Hence, non-invasive spot checking of hemoglobin concentrations as part of routine preoperative screening through the Masimo Pronto Pulse CO-Oximeter has the potential to 1) reduce preoperative blood loss related to diagnostic testing, albeit small in volume (i.e. approximately 5 ml per CBC), 2) prevent discomfort associated with venipuncture among patients with SpHb levels above threshold (i.e., unlikely to be anemic) and improve overall patient experience, 3) minimize healthcare worker risks associated with needle use, 4) streamline preoperative workflows by stratifying patients likely to benefit from further diagnostic testing, 5) provide near-instantaneous feedback to patients and care teams regarding general hematological status, and 6) reduce workloads in hematology laboratories. Additionally, cost savings may accompany SpHb implementation. Estimated costs include an upfront purchase price of approximately $1000 for a Masimo Pronto device and approximately $1.50 per SpHb reading (i.e., $600 for a reusable sensor permitting 400 unique SpHb readings). Comparatively, the direct costs of CBC testing, not inclusive of venipuncture costs, are estimated at $7.77 using 2021 Centers for Medicare and Medicaid Services reimbursement data, which would equate to over $3100 for 400 patients.
There are several limitations to this study. First, many of the suggested benefits resulting from the implementation of SpHb (i.e., reducing patient discomfort and needlestick injuries, improving preclinical workflows) are contingent on patients not requiring a more specific and comprehensive laboratory workup prior to their surgical intervention. However, imagining a future in which non-invasive or minimally invasive techniques are applicable for a broader range of laboratory tests, the use of SpHb to reduce preoperative CBC testing represents a step forward. Second, these results are only applicable to the Masimo Pronto Pulse CO-Oximeter as employed in our preoperative anemia clinic. Dedicated studies are needed to evaluate the accuracy of this device and related devices prior to implementation in each clinical setting. Third, this study was defined by a relatively limited sample size with limited racial heterogeneity, which may affect generalizability of results. Indeed, patients unable to attain a SpHb reading were less likely to be White and had lower PI values, reflecting impaired strength of measurements at the sensor. Given that other non-invasive sensors such as pulse oximeters, which also rely on cutaneous light transmission, have differential performance across self-identified racial groups,23,24 formal evaluations of SpHb devices with greater diversity of participant inclusion are essential prior to broader utilization in more diverse clinical practices. Fourth, we did not assess the reproducibility of SpHb results with repeated measurements. Fifth, given limited sample size we were unable to adjust for patient demographic and clinical features that may influence device performance. Finally, this technique does not facilitate evaluation of iron stores, and hence it cannot exclude the presence of iron deficiency without anemia.
In conclusion, the utilization of SpHb as assessed by the Masimo Pronto Pulse CO-Oximeter is feasible in a preoperative clinic with the potential to reliably exclude the presence of anemia using data-driven threshold values. While SpHb generally overestimates invasive hemoglobin measurements with relatively wide variation and should not replace laboratory-based testing in high-risk patients, they may nonetheless be employed to reduce the overall burden of preoperative laboratory testing by identifying those with low likelihood of anemia.
Supplementary Material
Acknowledgements
The authors would like to acknowledge the fantastic contributions of the Mayo Clinic POE team. The authors would also like to express their gratitude to Judd Schlotthauer for his assistance in securing devices for this pilot quality improvement project.
Financial Disclosures:
Dr. Warner is supported by grant K23HL153310 from the National Heart Lung and Blood Institute (NHLBI) of the National Institutes of Health (NIH). Study design and conduct are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Glossary
- AUC
Area Under Curve
- CBC
Complete Blood Count
- CI
Confidence Interval
- IRB
Institutional Review Board
- Hb
Hemoglobin concentration
- LOA
Limit of Agreement
- NPV
Negative Predictive Value
- PI
Perfusion Index
- POC
Point of Care
- POE
Preoperative Evaluation
- PPV
Positive Predictive Value
- ROC
Receiver Operating Characteristic
- SpHb
Non-invasive hemoglobin measurement
- WHO
World Health Organization
Footnotes
Conflicts of Interest: The authors declare no conflicts of interest. The manufacturer of SpHb sensors (Masimo) was not involved in any aspect of study design or conduct nor in the reporting of results.
References
- 1.Lin Y Preoperative anemia-screening clinics. Hematology Am Soc Hematol Educ Program. 2019;2019(1):570–576. doi: 10.1182/hematology.2019000061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gómez-Ramírez S, Bisbe E, Shander A, Spahn DR, Muñoz M. Management of Perioperative Iron Deficiency Anemia. Acta Haematol. 2019;142(1):21–29. doi: 10.1159/000496965 [DOI] [PubMed] [Google Scholar]
- 3.Desai N, Schofield N, Richards T. Perioperative Patient Blood Management to Improve Outcomes. Anesth Analg. 2018;127(5):1211–1220. doi: 10.1213/ANE.0000000000002549 [DOI] [PubMed] [Google Scholar]
- 4.Fowler AJ, Ahmad T, Phull MK, Allard S, Gillies MA, Pearse RM. Meta-analysis of the association between preoperative anaemia and mortality after surgery. Br J Surg. 2015;102(11):1314–1324. doi: 10.1002/bjs.9861 [DOI] [PubMed] [Google Scholar]
- 5.Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113(6):1338–1350. doi: 10.1097/ALN.0b013e3181fc6e0a [DOI] [PubMed] [Google Scholar]
- 6.Miceli A, Romeo F, Glauber M, de Siena PM, Caputo M, Angelini GD. Preoperative anemia increases mortality and postoperative morbidity after cardiac surgery. J Cardiothorac Surg. 2014;9:137. Published 2014 Aug 5. doi: 10.1186/1749-8090-9-137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Warner MA, Shore-Lesserson L, Shander A, Patel SY, Perelman SI, Guinn NR. Perioperative Anemia: Prevention, Diagnosis, and Management Throughout the Spectrum of Perioperative Care. Anesth Analg. 2020;130(5):1364–1380. doi: 10.1213/ANE.0000000000004727 [DOI] [PubMed] [Google Scholar]
- 8.Spahn DR, Schoenrath F, Spahn GH, et al. Effect of ultra-short-term treatment of patients with iron deficiency or anaemia undergoing cardiac surgery: a prospective randomised trial. Lancet. 2019;393(10187):2201–2212. doi: 10.1016/S0140-6736(18)32555-8 [DOI] [PubMed] [Google Scholar]
- 9.Richards T, Baikady RR, Clevenger B, et al. Preoperative intravenous iron to treat anaemia before major abdominal surgery (PREVENTT): a randomised, double-blind, controlled trial. Lancet. 2020;396(10259):1353–1361. doi: 10.1016/S0140-6736(20)31539-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lasocki S, Krauspe R, von Heymann C, Mezzacasa A, Chainey S, Spahn DR. PREPARE: the prevalence of perioperative anaemia and need for patient blood management in elective orthopaedic surgery: a multicentre, observational study. Eur J Anaesthesiol. 2015;32(3):160–167. doi: 10.1097/EJA.0000000000000202 [DOI] [PubMed] [Google Scholar]
- 11.Shah N, Osea EA, Martinez GJ. Accuracy of noninvasive hemoglobin and invasive point-of-care hemoglobin testing compared with a laboratory analyzer. Int J Lab Hematol. 2014;36(1):56–61. doi: 10.1111/ijlh.12118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Young MF, Raines K, Jameel F, et al. Non-invasive hemoglobin measurement devices require refinement to match diagnostic performance with their high level of usability and acceptability. PloS One. 2021;16(7):e0254629. Published 2021 Jul 16. doi: 10.1371/journal.pone.0254629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gayat E, Aulagnier J, Matthieu E, Boisson M, Fischler M. Non-invasive measurement of hemoglobin: assessment of two different point-of-care technologies. PloS One. 2012;7(1):e30065. doi: 10.1371/journal.pone.0030065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wittenmeier E, Paumen Y, Mildenberger P, et al. Non-invasive haemoglobin measurement as an index test to detect pre-operative anaemia in elective surgery patients – a prospective study. Anaesthesia. 2021;76(5):647–654. doi: 10.1111/anae.15312 [DOI] [PubMed] [Google Scholar]
- 15.von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61(4):344–349. doi: 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. Haemoglobin concentrations for the diagnosis of anemia and assessment of severity. World Health Organization. 2011; https://apps.who.int/iris/handle/10665/85839 [Google Scholar]
- 17.Avcioglu G, Nural C, Yilmaz FM, Baran P, Erel Ö, Yilmaz G. Comparison of noninvasive and invasive point-of-care testing methods with reference method for hemoglobin measurement. J Clin Lab Anal. 2018;32(3):e22309. doi: 10.1002/jcla.22309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lamhaut L, Apriotesei R, Combes X, Lejay M, Carli P, Vivien B. Comparison of the accuracy of noninvasive hemoglobin monitoring by spectrophotometry (SpHb) and HemoCue® with automated laboratory hemoglobin measurement. Anesthesiology. 2011;115(3):548–554. doi: 10.1097/ALN.0b013e3182270c22 [DOI] [PubMed] [Google Scholar]
- 19.Dewhirst E, Naguib A, Winch P, et al. Accuracy of noninvasive and continuous hemoglobin measurement by pulse co-oximetry during preoperative phlebotomy. J Intensive Care Med. 2014;29(4):238–242. doi: 10.1177/0885066613485355 [DOI] [PubMed] [Google Scholar]
- 20.Ke YH, Hwang KY, Thin TN, Sim YE, Abdullah HR. The usefulness of non-invasive co-oximetry haemoglobin measurement for screening pre-operative anaemia. Anaesthesia. 2021;76(1):54–60. doi: 10.1111/anae.15171 [DOI] [PubMed] [Google Scholar]
- 21.Khalafallah AA, Chilvers CR, Thomas M, et al. Usefulness of non-invasive spectrophotometric haemoglobin estimation for detecting low haemoglobin levels when compared with a standard laboratory assay for preoperative assessment. Br J Anaesth. 2015;114(4):669–676. doi: 10.1093/bja/aeu403 [DOI] [PubMed] [Google Scholar]
- 22.Matzek LJ, Hanson AC, Schulte PJ, Evans KD, Kor DJ, Warner MA. The Prevalence and Clinical Significance of Preoperative Thrombocytopenia in Adults Undergoing Elective Surgery: An Observational Cohort Study. Anesth Analg. 2021;132(3):836–845. doi: 10.1213/ANE.0000000000005347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Henry NR, Hanson AC, Schulte PJ, et al. Disparities in Hypoxemia Detection by Pulse Oximetry Across Self-Identified Racial Groups and Associations With Clinical Outcomes. Crit Care Med. 2022;50(2):204–211. doi: 10.1097/CCM.0000000000005394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sjoding MW, Dickson RP, Iwashyna TJ, Gay SE, Valley TS. Racial Bias in Pulse Oximetry Measurement [published correction appears in N Engl J Med. 2021 Dec 23;385(26):2496]. N Engl J Med. 2020;383(25):2477–2478. doi: 10.1056/NEJMc2029240 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


