Abstract
Background
Evidence revealed that there is a statistically significant gender difference in Health-related quality of life (HRQoL) among HIV-positive people on Antiretroviral therapy (ART). Consequently, HIV-positive women have low scores in all HRQoL domains than men. Despite this fact, previous studies in Ethiopia focused on general HIV-positive people and paid less attention to HIV-positive women. Therefore, this study was intended to measure HRQoL and associated factors among HIV-positive women on ART follow-up in north Shewa zone public hospitals, central Ethiopia.
Methods
An institution-based cross-sectional study was conducted from February 01-April 30, 2022. Four hundred twenty-six women on ART were included using a systematic random sampling technique. Face-to-face interviews and medical record reviews were used to collect data. Both bivariable and multiple linear regressions were computed to identify the factors associated with HRQoL. A p-value <0.05 was used to assert statistically significant variables in multiple linear regression analysis.
Results
The overall mean (SD) score of the HRQoL was 11.84 (2.44). And, 44.7% [95% CI: 40.3, 49.5] of the women have poor HRQoL. In multiple linear regression analysis, factors like depression (β = −0.35), Post-Traumatic Stress Disorder (PTSD) (β = −0.16), age (β = −0.07), rural residence (β = −0.52), and bedridden functional status (β = −1.02) were inversely associated with HRQoL. Oppositely, good treatment adherence (β = 0.46) was positively associated with overall HRQoL, keeping other factors constant.
Conclusion
This study reveals a high magnitude of poor HRQoL among HIV-positive women. Therefore, as HRQoL domains are comprehensive indicators of living status, healthcare service providers should be dedicated to screening and supporting HIV-positive women with poor HRQoL. Additionally, healthcare providers should also pay special attention to routine PTSD screening and management for HIV-positive women due to its detrimental effect on HRQoL.
Keywords: HIV/AIDS, Antiretroviral therapy, Quality of life, Women, Ethiopia
1. Introduction
Human Immuno-deficiency Virus/Acquired Immuno-deficiency Syndrome (HIV/AIDS) remains a major global public health concern, infecting 84.2 million [64.0 million-113.0 million] people and killing 40.1 million [33.6–48.6 million] people to date [1]. By the end of 2021, there were an estimated 38.4 million [33.9–43.8 million] people living with HIV [1] of which 54% were women and girls [2]. In the same year, 1.5 million [1.1 million-2.0 million] people became newly infected with HIV, with women and girls accounting for 49% [2]. Concerning the regional burden, African women and girls are disproportionately affected by HIV/AIDS, accounting for 63% of HIV patients and 60% of new infections in Africa [3]. Also in Ethiopia, women account for 59% of HIV patients and 51% of new infections [4].
Quality of Life (QoL) is an individual's perception of their position in life in the context of the culture and value systems in which they live and about their goals, expectations, standards, and concerns. QoL is also used as one of the widely accepted theoretical frameworks for assessing the living conditions of patients and it also is recognized as a key component of public health [5]. HRQoL is a multidimensional and complex concept and reflects subjective perceptions of individuals, their physical health, psychological state, level of independence, social relationships, personal beliefs, and relationship to salient features of their environment [6,7]. HRQoL is referring to the impact of disease and treatment on QoL. It is a core concept that comprises mostly self-reported measures of physical and mental health dimensions, and it has become an increasingly popular subjective health evaluation method in chronic diseases [8].
HIV/AIDS is often excluded from the list of chronic diseases though it is widely recognized as a chronic illness within HIV care [9]. Subsequently, HIV-positive people have significantly lower HRQoL than the general population, even among virologically and immunologically stable patients [10]. Because, AIDS impairs HRQoL, which is an important measurable outcome of HIV treatment in the era of Highly Active Antiretroviral Treatment (HAART), complementing more objective outcomes such as death [11].
Evidence revealed that there is a statistically significant gender difference in HRQoL among HIV-positive people on HAART; women have low scores in all HRQoL domains as compared to men [[12], [13], [14]]. On top of the gender difference, studies also indicated that HIV-positive women have significantly poorer functioning and well-being than HIV-negative women [15]. As a result, there is now mounting evidence that constitutes HRQoL as an important area of research and there is a need for further investigation along with the factors that influence it among HIV-positive women [16].
As evinced so far, factors like frequent HIV symptoms [17], anxiety [18], depression [13,[17], [18], [19], [20]], perceived stigma [12,17,21], food insecurity [19], TB/HIV co-infection [13], rural residence [13], and being anemic [13] were negatively associated with HRQoL in HIV-positive women. Oppositely, factors like problem-focused coping [17], perceived situational control [17], healthy lifestyles [17], social support [13,18,21,22], higher wealth status [22], higher CD4 count [21], and resilience [19] were positively associated with HRQoL in the similar population. Despite this documentation, the stipulation for more studies to measure variation in HRQoL over time is suggested [23].
Even though there is a gender difference in HRQoL, previous studies in Ethiopia focused on general HIV-positive people and paid less attention to HIV-positive women [[24], [25], [26]]. Aside from the scarcity of studies on HRQoL among HIV-positive women in Ethiopia, there was no similar study in the specific study area. Therefore, this study was intended to measure HRQoL and associated factors among HIV-positive women on ART follow-up in north Shewa zone public hospitals, central Ethiopia.
2. Methods
2.1. Study area, design, and period
This study was conducted in the North Shewa zone, Oromia regional state, central Ethiopia. Four public hospitals that are currently providing HIV/AIDS care and treatment (namely: Salale university comprehensive specialized hospital, Kuyu General Hospital, Sheno health center, and Gundo-meskel primary hospital) were included in the study. A cross-sectional study was conducted from February 01-April 30, 2022 among HIV-positive women (aged 18 and above years) attending ART clinics in public hospitals of the zone.
2.2. Sampling procedures
A single population mean formula was used to calculate the sample size. Accordingly, from a previous study [22] standard deviation (σ) = 2.19448 and n = 344 were considered. Likewise, a 95% confidence level, and 15% contingency were applied. Thus, from the above parameters
| nf = ((Zα/2)2 *σ2) / d2 |
| nf = ((1.96)2 * (2.19448)2) / (0.23128)2 |
Nf = 370. Thus, after a 15% contingency was added, 426 women were sampled. Then, the sample size was distributed using proportional allocation to size (PAS) to each ART clinic of the included public hospitals. Finally, a systematic random sampling technique was used to recruit the study participants.
2.3. Measurements
HRQoL was measured using the WHO QoL-HIV BREF scale among HIV/AIDS patients. The questionnaire contains 31 items distributed into 6 domains: physical, social relationships, level of independence, and spirituality domains each with 4 items, and psychological and environmental domains with 5 and 8 items, respectively. The individual items are rated on a 5-point Likert scale where 1 indicates low/negative perceptions and 5 indicates high/positive perceptions. The remaining two items measure the overall perceived quality of life and general health perception of women living with HIV [27]. The tool was validated in Ethiopian HIV-positive women (Cronbach's α > 0.80). As well, the scale's six domains exhibited good concurrent validity, with a coefficient of r = 0.63–0.82 [28]. Furthermore, the WHO QoL-HIV BREF scale tool demonstrated excellent reliability among HIV-positive women in Ethiopia (Cronbach-alpha = 0.89) [22]. The tool was also reliable in this study (Cronbach α = 0.92).
Anxiety and Depression were measured by Hospital Anxiety and Depression Scale (HADS). The tool is validated in Ethiopian HIV-positive patients. The internal consistency of the HADS was 0.78, 0.76, and 0.87 for the anxiety and depression subscales and the full scale, respectively. The intra-class correlation coefficient (ICC) was 80%, 86%, and 84% for the anxiety and depression subscales, and total scores respectively [29]. The tool was also reliable in this study (Cronbach α = 0.72).
The wealth index was measured using 15 simplified household assets questions available from www.equitytool.org. Accordingly, the wealth index of the household was classified into five quintiles. Then, the wealth index of the 1st and 2nd quintiles were classified as poorest, those in the 3rd quintile were middle, and those in the 4th and 5th quintiles were richest. The tool has 84.2% agreement and 0.76 kappa statistics with the 2016 Ethiopian Demographic Health Survey (EDHS) wealth index questionnaire [30].
Social support was measured by Oslo‐3 Social Support Scale (OSS‐3). The tool comprises valid values ranging from 3 to 14. A score ranging from 3 to 8 is classified as “poor support”, 9–11 is classified as “intermediate support”, and 12–14 is classified as “strong support”. The tool has a Cronbach-alpha of 0.88 [31]. The tool was also reliable in this study (Cronbach α = 0.73).
Perceived stigma was assessed by a 10-item perceived HIV stigma scale. The level of perceived stigma was measured by Likert scale questions (strongly disagree - strongly agree) with a value of 1–5, respectively. The study participants who scored mean and above from 10 stigma assessment questions were classified as having perceived stigma [32]. The tool was also reliable in this study (Cronbach α = 0.73).
Post-Traumatic Stress Disorder (PTSD) was measured by the Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) tool. The tool has five items with binary options (yes/no) and a score ≥3 indicates the presence of PTSD symptoms [33]. The tool was also reliable in this study (Cronbach α = 0.76).
Adherence to ART was measured based on patients’ recall of their compliance with the prescribed doses in the last 30 days. Patients who reported an intake of ≥95% of the prescribed medication were considered good adherent, and those with a reported intake of <95% were classified as poor adherent [34].
2.4. Data collection procedures
Data were collected through a face-to-face interview and a review of medical records based on the proportion of HIV-positive women allocated to each hospital. Specifically, data on the women's socio-demographic, clinical, and psycho-social characteristics were collected using pretested semi-structured interview-administered questionnaires. In addition, data on the women's HIV-related characteristics were extracted from medical records. Four trained nurses collected data under the supervision of two public health professionals.
2.5. Statistical analysis
The collected data were entered into Epi data version 3.1 and then exported to SPSS version 25 for analysis. Participant characteristics were described using descriptive statistics like frequency and percentage, mean and standard deviation (SD), and median and inter-quantile range (IQR). Only variables significant at p-value <0.25 in simple linear regression were included in subsequent multiple linear regression analysis. In multiple linear regression, variables with a p-value <0.05 were taken as statistically significant. Results were presented as β-coefficient with a 95% confidence interval (CI), and p-value. The assumptions of least squares regression (linearity, normal distribution, equal variances, and independent observations) were checked. Thus, assumptions of linearity and equal variances were checked by visual inspection of scatter plots, and there was no clear pattern on the scatter plot. The normal probability plot showed that the error term was normally distributed. The low variance inflation factor (<2.8) indicated that the associated independent variable has lower collinearity with the other variables in the model. A good fit model for multiple linear regression was determined (Adjusted R2 = 0.737).
2.6. Data quality assurance
WHO QoL-HIV BREF scale is a validated and well-adapted tool for Ethiopian HIV-positive women [28]. Besides, all questionnaires were translated into the local languages (Afan Oromo and Amharic) by two independent bilingual translators and back-translated to English to guarantee consistency. A one-day training was given to the data collectors and supervisors. Ten percent (10%) of the questionnaire was pre-tested at Chancho general hospital and mandatory clarifications and modifications on ambiguous points were made. Likewise, a reliability test was done and tools with Cronbach-alpha >0.7 were used during the actual data collection.
Ethical approval
An ethical approval letter was obtained from the Institution review board of Salale University. A permission letter was secured from each health facility's administration. The purpose of the study was informed to the patients and written informed consent was obtained from each participant before the interview. Additionally, all the information obtained from each study participant was kept confidential throughout the process of this study.
3. Results
3.1. Sociodemographic characteristics
The response rate of the study was 97%. The women's mean (SD) age was 36 [9] years old. And, the age range was 47 (minimum 18 and maximum 65) years old. About 277 (67.2%) of the women were urban residents and more than half, 217 (52.7%) were married followed by widowed, 100 (24.3%). Moreover, about 19 (28.9%) of the women lack formal education and about 160 (38.8%) were in the poorest wealth index category (Table 1).
Table 1.
Socio-demographic characteristics of the HIV-positive women attending ART clinics in north Shewa zone public hospitals (n = 412).
| Variable name | Category | Freq. (%) |
|---|---|---|
| Age | 18–28 | 97 (23.5) |
| 29–39 | 177 (43.0) | |
| 40+ | 138 (33.5) | |
| Residence | Rural | 135 (32.8) |
| Urban | 277 (67.2) | |
| Marital status | Divorced | 41 (10.0) |
| Married | 217 (52.7) | |
| Single | 54 (13.1) | |
| Widowed | 100 (24.3) | |
| Educational status | No formal education | 119 (28.9) |
| primary (1–8 grade) | 96 (23.3) | |
| Secondary (9–12) | 78 (18.9) | |
| College and above | 119 (28.9) | |
| Wealth index category | Poorest (1st and 2nd quintiles) | 160 (38.8) |
| Middle (3rd quintile) | 88 (21.4) | |
| Richest (4th and 5th quintiles) | 164 (39.8) | |
| Occupation status | Housewife | 159 (38.6) |
| Government employee | 92 (22.3) | |
| Private employee | 44 (10.7) | |
| Student | 35 (8.5) | |
| Unemployed | 78 (18.9) | |
| Othersa | 4 (1.0) |
Daily laborer, driver.
3.2. Clinical characteristics
Of the total women, 364 (88.3%) have been above 60 months since diagnosed with HIV/AIDS. The mean (SD) baseline CD4 was 200 (52), while the mean (SD) current CD4 was 500 (100). Additionally, 305 (74.0%) were in baseline stage 3 WHO clinical stage, while 300 (72.8%) were currently in WHO clinical stage 1. Moreover, 230 (55.8%) of the participants had one form of opportunistic infection. Tuberculosis, 79 (19.2%) was the top opportunistic infection. Besides, 68 (16.5%) of the participants were non-adherent to the treatment (Table 2).
Table 2.
Clinical characteristics of the HIV-positive women attending ART clinics in north Shewa zone public hospitals (n = 412).
| Variable | Category | Freq. (Percentage) |
|---|---|---|
| Duration since diagnosed | less than 60 months | 48 (11.7) |
| above 60 months | 364 (88.3) | |
| Treatment adherence | Adherent | 344 (83.5) |
| Non-adherent | 68 (16.5) | |
| Baseline WHO clinical stage | Stage 1 | 14 (3.4) |
| Stage 2 | 57 (13.8) | |
| Stage 3 | 305 (74.0) | |
| Stage 4 | 36 (8.7) | |
| Current WHO clinical stage | Stage 1 | 300 (72.8) |
| Stage 2 | 86 (20.9) | |
| Stage 3 | 8 (1.9) | |
| Stage 4 | 18 (4.4) | |
| Opportunistic infections | Yes | 230 (55.8) |
| No | 182 (44.2) | |
| Current ART regimen | 1st line | 286 (69.4) |
| 2nd regimen | 118 (28.6) | |
| 3rd regimen | 8 (1.9) | |
| ARV side effects | Yes | 113 (27.4) |
| No | 299 (72.6) | |
| Current functional status | Working | 312 (75.7) |
| Bedridden | 12 (2.9) | |
| Ambulatory | 88 (21.4) |
3.3. Psychosocial and behavioral characteristics
Of the total women, 21.1% and 35.2% have anxiety and depression respectively. Additionally, 75.7% of women have poor social support. Furthermore, 49.8% of the women reported suffering from perceived stigma, while 27.7% were screened positive for Post-Traumatic Stress Disorder (PTSD). About 19% of the women stated that they are currently using substances (either alcohol, cigarette, or shisha) (Table 3).
Table 3.
Psychosocial and behavioral characteristics of HIV-positive women attending ART clinics in north Shewa zone public hospitals (n = 412).
| Variable name | Category | Freq. (Percentage) |
|---|---|---|
| Anxiety | Present | 87 (21.1) |
| Absent | 325 (78.9) | |
| Depression | Depressed | 145 (35.2) |
| Non-depressed | 267 (64.8) | |
| Social support | Poor | 312 (75.7) |
| Intermediate | 96 (23.3) | |
| Strong | 4 (1.0) | |
| Perceived stigma | Stigmatized | 205 (49.8) |
| Not-stigmatized | 207 (50.2) | |
| Post-Traumatic Stress Disorder | Screened positive | 114 (27.7) |
| Screened negative | 298 (72.3) | |
| Current substance use | Yes | 78 (18.9) |
| No | 334 (81.1) |
3.4. Health-related quality of life
The overall mean (SD) of the HRQoL was 11.84 (2.44) (Table 4). And, 44.7% [95% CI: 40.3, 49.5] of the women have poor HRQoL. Furthermore, on perceived measures of general QoL and health status, 53.4% of participants reported good general QoL, while 11.6% reported poor/very poor. In terms of perceived satisfaction with their health, 25.5% of participants were dissatisfied/very dissatisfied, while 60.9% were satisfied/very satisfied.
Table 4.
Overall and domains’ HRQoL mean score of HIV-positive women attending ART clinics in north Shewa zone public hospitals (n = 412).
| HRQoL domains | Items | Mean | Standard deviation | Minimum | Maximum |
|---|---|---|---|---|---|
| Physical domain | 4 | 10.66 | 2.77 | 4 | 18 |
| Psychological domain | 5 | 12.44 | 3.04 | 4 | 17.6 |
| Level of independence | 4 | 11.74 | 2.43 | 6 | 19 |
| Social relationship | 4 | 13.20 | 3.24 | 4 | 20 |
| Environmental | 8 | 12.67 | 2.82 | 5.50 | 17.50 |
| Spirituality | 4 | 10.31 | 2.81 | 5 | 20 |
| Overall HRQoL | 29 | 11.84 | 2.44 | 5.58 | 16.27 |
3.4.1. Domain of HRQoL
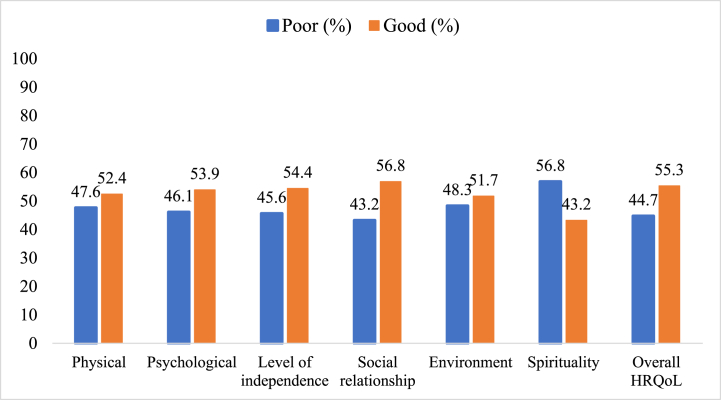
Among the HRQoL domains, the spirituality domain had the highest rate of poor HRQoL (56.8%) followed by the environment domain (48.3%). In contrast, the social relationship was found to have the minimum poor HRQoL (43.2%) (Fig. 1).
Fig. 1.
Total and each domain HRQoL status of HIV-positive women attending ART clinics in north Shewa zone public hospitals (n = 412).
3.4.2. Factors associated with HRQoL
In simple linear regression analysis factors like depression, Post-Traumatic Stress Disorder, age of the women, being rural residents, current WHO clinical stage-2, duration since HIV diagnosis, bedridden functional status, comorbidity of chronic disease(s), and current substance use were inversely associated with a higher score of HRQoL. However, good treatment adherence, strong social support, and a higher current CD4 count were factors directly associated with a higher score of HRQoL (Table 5).
Table 5.
Simple and multiple linear regression for factors associated with HRQoL among HIV-positive women attending ART clinics in north Shewa zone public hospitals (n = 412).
| Variable | Simple linear regression |
Multiple linear regression |
||
|---|---|---|---|---|
| Unstandardized coefficients (β) | 95% CI for β | Unstandardized coefficients (β) | 95% CI for β | |
| Age | −0.18 | (-0.19, -0.16) | −0.07 | (-0.09, -0.05)a |
| Rural residence | −1.73 | (-2.21, -1.26) | −0.52 | (-0.79, -0.24)a |
| Good treatment adherence | 0.85 | (0.22, 1.48) | 0.46 | (0.12, 0.79)a |
| Depression | −0.52 | (-0.55, -0.48) | −0.35 | (-0.40, -0.31)a |
| Strong social support | 1.45 | (-0.96, 3.86) | −0.28 | (-1.59, 1.02) |
| Current CD4 count | 0.10 | (0.008, 0.12) | 0.001 | (-0.0003, 0.003) |
| Current WHO clinical stage-2 | −2.81 | (-3.32, −2.29) | −0.33 | (0.68, 0.03) |
| Duration since HIV diagnosis | −0.018 | (-0.022, −0.015) | −0.001 | (0.004, 0.002) |
| Bedridden functional status | −5.77 | (-7.07, -4.48) | −1.02 | (-1.84, -0.21)b |
| Comorbidity of chronic disease(s) | −0.75 | (-1.47, −0.03) | 0.09 | (-0.29, 0.48) |
| Post-Traumatic Stress Disorder | −0.49 | (-0.70, -0.29) | −0.16 | (-0.28, -0.04)b |
| Current substance use | −1.97 | (-2.55, −1.40) | 0.29 | (-0.07, 0.65) |
Significant at p-value <0.001.
Significant at p-value <0.05.
In multiple linear regression analysis, factors like depression, Post-Traumatic Stress Disorder, age of the women, rural residents, and bedridden functional status were inversely associated with a higher score of HRQoL. On the other hand, good treatment adherence was positively associated with an overall higher score of HRQoL, keeping other factors constant (Table 5).
Accordingly, as women's age increase by one year, their HRQoL score is expected to fall by 0.07 unit averagely (β = −0.07). Rural women were supposed to have a 0.52 lower HRQoL score than urban women (β = −0.52). Besides, as the depression scale increases by a unit, the women's HRQoL score is reduced by 0.35 units (β = −0.35). The rate of the average change in HRQoL among women who are bedridden functional status is 1.02 lower compared to women who are ambulatory/working functional status (β = −1.02). Moreover, as the PTSD scale increase by one unit, the HRQoL is anticipated to decrease by 0.16 units (β = −0.16). In contrast to the above, women who have good treatment adherence are expected to have a 0.46 higher HRQoL score as compared to women who have poor treatment adherence status (β = 0.46) (Table 5).
4. Discussion
This study measures the HRQoL and associated factors among HIV-positive women. The overall mean (SD) of the HRQoL was 11.84 (2.44) and 44.7% of the women have poor HRQoL. This finding was lower than the study conducted among HIV-positive women in Jimma, Ethiopia (53.5%) [22]. HRQoL might increase as a result of time changes, service expansion, and improvements. In contrast, the level of poor HRQoL in this study was higher than the study from south India (7.9%) [35]. This could be attributed to differences in the status of the enrolled women, the sample size, and socio-demographic factors.
However, the level of poor HRQoL in this study was found to be consistent with the pooled prevalence of HRQoL among general HIV-positive people in Ethiopia (45.27%) [36]. Over time monitoring of HRQoL will support HIV care and treatment practices to settle auspicious outcomes [23]. Additionally, the study from Indonesia reported a comparable finding (45%) [37]. The similarity in the use of the WHO QoL-HIV BREF tool to collect data might result in equivalent findings.
In this study, age was inversely associated with HRQoL. Studies from India [38] and Canada [19] have reported comparable findings. This might be due to the complex interactions of health-related socio-ecological factors affecting aging among HIV-positive women [19]. Conversely, the studies from Northeast Ethiopia [39] and the southeastern United States [40] reported opposing findings. Having a stable home environment and fewer home responsibilities, and perceiving fewer wasted chances in furthering career goals among older women may lead to better HRQoL [40]. A place of residence was another socio-demographic factor associated with HRQoL. Consequently, rural HIV-positive women had lower HRQoL scores. The previous studies conducted in western [13] and northern [12] Ethiopia confirmed this. In rural residents, the presence of relatively poor infrastructure, greater financial inadequacy, high stigmatization, and marginalization may result in poor HRQoL.
Being well adhered to ART was found to increase HRQoL score. The previous literature review and a study from China found that ART adherence improves HRQoL [41,42]. As well, a study from Colombia found that non-adherence to combined ART was associated with lower QoL [43]. Improving patients’ devotion and compliance toward their treatment, health, and understanding of the significance of ART adherence is crucial. In contrast, a study of HIV-positive transgender women in Sao Paulo, Brazil, found no association between these two variables [44].
In the assessment of the mental health domain, depression was found to have a negative association with HRQoL. A study from Thailand also confirms this finding [20]. Additionally, a considerable body of studies shows that depression has a significant negative effect on QoL among HIV-positive people [17,19,[44], [45], [46]]. This suggests the necessity to reconsider mental health care strategies for HIV-positive women. Moreover, the presence of PTSD symptoms was also inversely associated with HRQoL. Comparably, previously reported that the occurrence of PTSD symptoms is threatening HIV-positive people QoL [47]. This is because HIV is one of the trauma-inducing chronic illnesses with negative effects on HRQoL. Another study also implied that poor adherence to antiretroviral therapy is a pathway through which PTSD symptoms exert a negative influence on the HRQoL of HIV-positive people [48]. Consequently, early detection of PTSD among HIV-positive people is crucial to address the issue [49].
4.1. Strengths of the study
In this study, a locally validated HRQoL measuring tool was used, and the tool's reliability was also comprehensively analyzed in this study. Also, the current findings have implications for medical/public health decision-making in terms of designing evidence-based interventions considering the chronic nature of HIV infection and patient-disclosed outcomes on HRQoL. Moreover, the identification of psychological risk factors like PTSD as being associated with poor HRQoL provides a window of opportunity to improve HRQoL; thus, intervention strategies to prevent and control PTSD should be viewed as critical to HIV-positive women.
4.2. Limitations of the study
The cross-sectional nature of the study does not allow temporality ascertainment. Furthermore, recall bias and social desirability biases may exist because participants were asked to respond based on their life experiences. Additionally, HIV-positive women who were unaware of their sero-status, were not receiving care, or were hospitalized did not participate in this study — the findings cannot be generalized to these populations.
5. Conclusion
This study found that nearly half of the HIV-positive women have poor HRQoL. Moreover, the age of the women, rural residents, depression, bedridden functional status, and PTSD were inversely associated with a higher score of HRQoL. Conversely, good treatment adherence was positively associated with an overall higher score of HRQoL. Subsequently, because HRQoL domains are comprehensive indicators of living status, HIV-positive women with poor HRQoL should be identified and supported. Furthermore, interventions aimed at improving HRQoL in HIV-positive women should incorporate/reinforce approaches for routine PTSD and depressive symptoms screening and management due to their negative impact on HRQoL. Moreover, routine assessment of treatment adherence and apt interventions at every clinic visit should be encouraged to increase the HRQoL of HIV-positive women. Also, HIV-positive women who are elderly, bedridden, and live in rural areas should be given special consideration due to their potential poor HRQoL. More research on similar populations using other HRQoL measuring tools than the WHO-QOL-HIV BREF is also suggested to address the issue of tool invariance and thus facilitate comparability. Besides, future research should attempt to identify novel variables that influence the level of HRQoL in diverse contexts.
Declarations
Author contribution statement
Derara Girma, Hiwot Dejene, and Leta Adugna Geleta: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Mengistu Tesema, Elsabeth Legesse, Tadesse Nigussie, Berhanu Senbeta Deriba, Tinsae Abeya Geleta, Degemu Sahlu, Addisu Waleligne, Sisay Abebe Debela, and Mukemil Awol: Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research work was funded by Salale University, Ethiopia [Ref. No.: SlU-IRB-023-2022]
Data availability statement
Data will be made available on request.
Declaration of interest's statement
The authors declare no competing interests.
Acknowledgments
We would like to thank the ART clinic staff and administration of north Shewa zone public hospitals. Our deep gratitude also goes to the study participants, data collectors, and supervisors.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e13318.
Appendix A. Supplementary data
The following are the Supplementary data to this article.
References
- 1.World Health Organization . 2022. HIV [Internet]https://www.who.int/news-room/fact-sheets/detail/hiv-aids [cited 2022 Aug 27]. Available from: [Google Scholar]
- 2.UNAIDS . 2022. Global HIV & AIDS Statistics - Fact Sheet [Internet]https://www.unaids.org/en/resources/fact-sheet [cited 2022 Aug 27]. Available from: [Google Scholar]
- 3.African Union and UN Women. Gender Equality . 2021. Women's Empowerment (GEWE) and HIV in Africa: the Impact of Intersecting Issues and Key Continental Priorities [Internet]https://au.int/sites/default/files/documents/41625-doc-AU_GEWE_Advocacy_Brief_ENGLISH_Final [cited 2022 Aug 27]. Available from: [Google Scholar]
- 4.UNAIDS . 2021. HIV and AIDS Estimates: Country Fact Sheets (Ethiopia) [Internet]https://www.unaids.org/en/regionscountries/countries/ethiopia [cited 2022 Aug 27]. Available from: [Google Scholar]
- 5.WHO . 2012. WHOQOL-measuring Quality of Life [Internet]https://www.who.int/tools/whoqol [cited 2021 Aug 26]. Available from: [Google Scholar]
- 6.Karimi M., Brazier J. Health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics. 2016;34(7):645–649. doi: 10.1007/s40273-016-0389-9. [DOI] [PubMed] [Google Scholar]
- 7.Foundation Health Measure Report Health-related quality of life and well-being. Heal people. 2020;2010(November):1–6. [Google Scholar]
- 8.Kaplan R.M., Ries A.L. Quality of life: concept and definition. COPD. 2007;4(3):263–271. doi: 10.1080/15412550701480356. [DOI] [PubMed] [Google Scholar]
- 9.Swendeman D., Ingram B.L., Rotheram-Borus M.J. Common elements in self-management of HIV and other chronic illnesses: an integrative framework. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2009;21(10):1321–1334. doi: 10.1080/09540120902803158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miners A., Phillips A., Kreif N., Rodger A., Speakman A., Fisher M., et al. Health-related quality-of-life of people with HIV in the era of combination antiretroviral treatment: a cross-sectional comparison with the general population. Lancet HIV. 2014;1(1):e32–e40. doi: 10.1016/S2352-3018(14)70018-9. [DOI] [PubMed] [Google Scholar]
- 11.Hays R.D., Cunningham W.E., Sherbourne C.D., Wilson I.B., Wu A.W., Cleary P.D., et al. Health-related quality of life in patients with human immunodeficiency virus infection in the United States: results from the HIV cost and services utilization study. Am. J. Med. 2000;108(9):714–722. doi: 10.1016/s0002-9343(00)00387-9. [DOI] [PubMed] [Google Scholar]
- 12.Tesfay A., Gebremariam A., Gerbaba M., Abrha H. Gender differences in health related quality of life among people living with HIV on highly active antiretroviral therapy in mekelle town, northern Ethiopia. BioMed Res. Int. 2015:1–9. doi: 10.1155/2015/516369. http://www.hindawi.com/journals/bmri/2015/516369/ [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gebremichael D.Y., Hadush K.T., Kebede E.M., Zegeye R.T. Gender difference in health related quality of life and associated factors among people living with HIV/AIDS attending anti-retroviral therapy at public health facilities, western Ethiopia: comparative cross sectional study. BMC Publ. Health. 2018;18(1):1–11. doi: 10.1186/s12889-018-5474-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ahmed A., Saqlain M., Bashir N., Dujaili J., Hashmi F., Mazhar F., et al. Health-related quality of life and its predictors among adults living with HIV/AIDS and receiving antiretroviral therapy in Pakistan. Qual. Life Res. 2021;30(6):1653–1664. doi: 10.1007/s11136-021-02771-y. [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mast T.C., Kigozi G., Wabwire-Mangen F., Black R., Sewankambo N., Serwadda D., et al. Measuring quality of life among HIV-infected women using a culturally adapted questionnaire in Rakai district, Uganda. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2004;16(1):81–94. doi: 10.1080/09540120310001633994. [DOI] [PubMed] [Google Scholar]
- 16.McDonnell K.A., Gielen A.C., Wu A.W., O'Campo P., Faden R. Measuring health related quality of life among women living with HIV. Qual. Life Res. 2000;9(8):931–940. doi: 10.1023/a:1008909919456. [DOI] [PubMed] [Google Scholar]
- 17.Vyavaharkar M., Moneyham L., Murdaugh C., Tavakoli A. Factors associated with quality of life among rural women with HIV disease. AIDS Behav. 2012;16(2):295–303. doi: 10.1007/s10461-011-9917-y. [DOI] [PubMed] [Google Scholar]
- 18.Xiaowen W., Guangping G., Ling Z., Jiarui Z., Xiumin L., Zhaoqin L., et al. Depression and anxiety mediate perceived social support to predict health-related quality of life in pregnant women living with HIV. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2018;30(9):1147–1155. doi: 10.1080/09540121.2018.1456640. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 19.Kteily-Hawa R., Andany N., Wang Y., Logie C.H., Tharao W., Conway T., et al. Quality of life of older women living with HIV: comparative assessment of physical and mental health-related markers using a large Canadian Sexual and Reproductive Health Cohort Study. HIV Res Clin Pract. 2019;20(2):35–47. doi: 10.1080/15284336.2018.1554373. [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 20.Aurpibul L., Tongprasert F., Wichasilp U., Tangmunkongvorakul A. Depressive symptoms associated with low quality of life among pregnant and postpartum women living with HIV in chiang mai, Thailand. Int J Matern Child Heal AIDS. 2020;9(3):421–429. doi: 10.21106/ijma.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nyamathi A.M., Ekstrand M., Yadav K., Ramakrishna P., Heylen E., Carpenter C., et al. Quality of life among women living with HIV in rural India. J. Assoc. Nurses AIDS Care. 2017;28(4):575–586. doi: 10.1016/j.jana.2017.03.004. https://journals.lww.com/00001782-201707000-00013 [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abebe Weldsilase Y., Likka M.H., Wakayo T., Gerbaba M. Health-related quality of life and associated factors among women on antiretroviral therapy in health facilities of Jimma town, southwest Ethiopia. Adv Public Heal. 2018:1–12. [Google Scholar]
- 23.Vo Q.T., Hoffman S., Nash D., El-Sadr W.M., Tymejczyk O.A., Gadisa T., et al. Gender differences and psychosocial factors associated with quality of life among ART initiators in Oromia, Ethiopia. AIDS Behav. 2016;20(8):1682–1691. doi: 10.1007/s10461-016-1396-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ghiasvand H., Waye K.M., Noroozi M., Harouni G.G., Armoon B., Bayani A. Clinical determinants associated with quality of life for people who live with HIV/AIDS: a Meta-analysis. BMC Health Serv. Res. 2019;19(1):1–11. doi: 10.1186/s12913-019-4659-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dinsa Ayeno H., Megersa Atomsa K., Melesie Taye G. Assessment of health-related quality of life and associated factors among HIV/AIDS patients on highly active antiretroviral therapy (HAART) at ambo general hospital, west Shewa, Ethiopia. HIV AIDS Res. Palliat. Care. 2020;12:467–478. doi: 10.2147/HIV.S259510. https://www.dovepress.com/assessment-of-health-related-quality-of-life-and-associated-factors-am-peer-reviewed-article-HIV [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Surur A.S., Teni F.S., Wale W., Ayalew Y., Tesfaye B. Health related quality of life of HIV/AIDS patients on highly active anti-retroviral therapy at a university referral hospital in Ethiopia. BMC Health Serv. Res. 2017;17(1):1–8. doi: 10.1186/s12913-017-2714-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.World Health Organization WHOQOL-HIV instrument scoring and coding. Users Manual. 2002:1–13. [Google Scholar]
- 28.Agala C.B., Fried B.J., Thomas J.C., Reynolds H.W., Lich K.H., Whetten K., et al. Reliability, validity and measurement invariance of the WHO's quality of life scale among women of reproductive age living with HIV in Ethiopia - a quasi-experimental study. Appl Res Qual Life. 2021;16(4):1785–1812. [Google Scholar]
- 29.Reda A.A. Reliability and validity of the Ethiopian version of the hospital anxiety and depression scale (HADS) in HIV infected patients. PLoS One. 2011;6(1):1–6. doi: 10.1371/journal.pone.0016049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chakraborty N.M., Fry K., Behl R., Longfield K. Simplified asset indices to measure wealth and equity in health programs: a reliability and validity analysis using survey data from 16 countries. Glob Heal Sci Pract. 2016;4(1):141–154. doi: 10.9745/GHSP-D-15-00384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Duko B., Geja E., Zewude M., Mekonen S. Prevalence and associated factors of depression among patients with HIV/AIDS in Hawassa, Ethiopia, cross-sectional study. Ann. Gen. Psychiatr. 2018;17(1):4–9. doi: 10.1186/s12991-018-0215-1. [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Melis T., Fikadu Y., Lemma L. Perceived stigma and associated factors among HIV positive adult patients attending antiretroviral therapy clinics at public facilities of butajira town, southern Ethiopia. HIV AIDS Res. Palliat. Care. 2020;12:717–724. doi: 10.2147/HIV.S280501. https://www.dovepress.com/perceived-stigma-and-associated-factors-among-hiv-positive-adult-patie-peer-reviewed-article-HIV [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.National Center for PTSD . vol. 5. 2015. https://www.ptsd.va.gov (Primary Care PTSD Screen for DSM-5 (PC-PTSD-5)). Available from: [Google Scholar]
- 34.Tesfay Gebreagziabher T., Woldemariam G.T. Antiretroviral treatment adherence and determinant factors among adult people infected with human immunodeficiency virus in eastern tigray general hospitals, northern Ethiopia, 2019. HIV AIDS Res. Palliat. Care. 2020;12:497–505. doi: 10.2147/HIV.S273917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Alexander G., Thomas R.A. Health-related quality of life in HIV-positive women on long-term antiretroviral therapy—a study from Bangalore, south India. World J. AIDS. 2022;12(2):97–110. [Google Scholar]
- 36.Mengistu N., Hareru H.E., Shumye S., Yimer S., Sisay D., Kaso A.W., et al. Health related quality of life and its association with social support among people living with HIV/AIDS receiving antiretroviral therapy in Ethiopia: a systematic review and meta-analysis. Health Qual. Life Outcome. 2022;20(1):1–8. doi: 10.1186/s12955-022-01985-z. [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Martina Evi S., Thongpat S., Nitirat P. Quality of life of HIV-infected women in medan, north sumatera, Indonesia. Int. J. Sci. Basic Appl. Res. 2017;36(5):319–324. [Google Scholar]
- 38.Arjun B.Y., Unnikrishnan B., Ramapuram J.T., Thapar R., Mithra P., Kumar N., et al. Factors influencing quality of life among people living with HIV in coastal south India. J. Int. Assoc. Phys. AIDS Care. 2017;16(3):247–253. doi: 10.1177/2325957415599213. [DOI] [PubMed] [Google Scholar]
- 39.Mohammed S.A., Yitafr M.G., Workneh B.D., Hailu A.D. Health-related quality of life and associated factors among people living with human immunodeficiency virus on highly active antiretroviral therapy in North East Ethiopia: cross-sectional study. PLoS One. 2021;16(3 March 2021):1–14. doi: 10.1371/journal.pone.0247777. [Internet] Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Murdaugh C., Moneyham L., Jackson K., Phillips K., Tavakoli A. Predictors of quality of life in HIV-infected rural women: psychometric test of the chronic illness quality of life ladder. Qual. Life Res. 2006;15(5):777–789. doi: 10.1007/s11136-005-5002-1. [DOI] [PubMed] [Google Scholar]
- 41.Gakhar H., Kamali A., Holodniy M. Health-related quality of life assessment after antiretroviral therapy: a review of the literature. Drugs. 2013;73(7):651–672. doi: 10.1007/s40265-013-0040-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang H., Zhou J., He G., Luo Y., Li X., Yang A., et al. Consistent ART adherence is associated with improved quality of life, CD4 counts, and reduced hospital costs in central China. AIDS Res. Hum. Retrovir. 2009;25(8):757–763. doi: 10.1089/aid.2008.0173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Narváez M., Lins-Kusterer L., Valdelamar-Jiménez J., Brites C. Quality of life and antiretroviral therapy adherence: a cross-sectional study in Colombia. AIDS Res. Hum. Retrovir. 2022;38(8):660–669. doi: 10.1089/AID.2021.0233. https://www.liebertpub.com/doi/10.1089/aid.2021.0233 [Internet] Available from: [DOI] [PubMed] [Google Scholar]
- 44.Sabino T.E., Avelino-Silva V.I., Cavalcantte C., Goulart S.P., Luiz O.C., Fonseca L.A.M., et al. Adherence to antiretroviral treatment and quality of life among transgender women living with HIV/AIDS in São Paulo, Brazil. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2020:1–8. doi: 10.1080/09540121.2019.1710449. 0(0) [DOI] [PubMed] [Google Scholar]
- 45.Tostes M.A., Chalub M., Botega N.J. The quality of life of HIV-infected women is associated with psychiatric morbidity. AIDS Care - Psychol Socio-Medical Asp AIDS/HIV. 2004;16(2):177–186. doi: 10.1080/09540120410001641020. [DOI] [PubMed] [Google Scholar]
- 46.Siregar M.L., Abdullah V., Mamfaluti T. Correlation of depression and quality of life in HIV/AIDS patients. IOP Conf. Ser. Earth Environ. Sci. 2018;125(1) [Google Scholar]
- 47.Luo S., Lin C., Ji G., Li L. Post-traumatic stress disorder symptoms among people living with HIV/AIDS in rural China. AIDS Behav. 2017;21(11):3202–3208. doi: 10.1007/s10461-016-1641-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Onu D.U. Adherence to antiretroviral therapy mediates the link between posttraumatic stress disorder symptoms and health-related quality of life. S. Afr. J. Psychol. 2021;52(2):238–248. doi: 10.1177/00812463211048122. [Internet] Available from: [DOI] [Google Scholar]
- 49.Arebo B., Ewach G.F., Omara J., Oyella P., Aciro Lucky R., Kabunga A. Post-Traumatic stress disorder and coping strategies among people with HIV in lira district, Uganda: a cross-sectional study. HIV AIDS Res. Palliat. Care. 2022;14(May):255–264. doi: 10.2147/HIV.S358575. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.