Abstract
Acute traumatic aortic injuries are of the most lethal sequelae of penetrating thoracic injuries and require rapid detection and management. The American College of Radiology currently recommends the use of noncontrast CT, followed by computed tomography angiography (CTA) as the first-line imaging modalities when traumatic aortic injury is suspected. Direct signs of aortic injury on CTA include pseudoaneurysm, focal contour abnormality, intimal flap, intramural hematoma, an abrupt change in aortic caliber, and contrast extravasation. Aortic pseudoaneurysms are most often caused by blunt or penetrating trauma that results in damage to the vessel wall, turbulent blood flow, and formation of a surrounding hematoma contained by a wall of products from the clotting cascade. This wall is weaker than those of a true aneurysm and will ultimately rupture over time if not repaired. Traumatic aortic pseudoaneurysms are preferably treated by thoracic endovascular aortic repair using a prosthetic stent graft. Here, we present a 44-yearold female with a history of homelessness, polysubstance use disorder, and HIV who presented to the emergency department after being found down. She reported being shot by a pellet gun, and physical examination revealed a penetrating left-sided chest wound that appeared to be several days old. A STAT CTA was obtained and revealed a hemopneumothorax and possible thoracic aortic pseudoaneurysm. A left-sided chest tube was placed and the patient underwent thoracic endovascular aortic repair through right femoral arterial access and tolerated the procedure well. The patient was placed on daily aspirin postoperatively and discharged on post-op day 5.
Keywords: Traumatic aortic injury, Emergency radiology, Pseudoaneurysm, Pellet gun, Hemopneumothorax, Hemomediastinum
Introduction
Acute aortic injury represents an important component of emergent pathology that can present in most level 1 and level 2 trauma centers. While common, acute aortic injuries are almost exclusively fatal—80%-90% of acute traumatic aortic injuries are immediately fatal, with a large percentage of mortality occurring prior to hospital presentation [1]. The most common cause of acute thoracic aortic injury is a motor vehicle collision [1], non-accidental trauma such as gunshot and stab wounds still represent a significant cause of morbidity and mortality.
Noncontrast computed tomography and computed tomography angiography (CTA) are the gold standard in diagnosing acute aortic injury due to their speed, sensitivity, and specificity [6]. As technologies for fast, safe, and effective endovascular repair have become more widely utilized, patients who survive until admission to the hospital have higher rates of survival and lower rates of complications when compared to open surgical repair or conservative management [1].
History of present illness
A 44-year-old female with a history of homelessness, polysubstance use disorder, and HIV presents to the hospital after she was found down by police under a bridge in town. On arrival, the patient is somnolent, but when awoken she states that she was “shot by a pellet gun.” On examination, the patient is maintaining oxygen saturation of 100% on room air with reduced breath sounds throughout the left chest, has 2+ femoral pulses, and has a penetrating wound in the left upper chest that looks to be several days old.
Hospital course
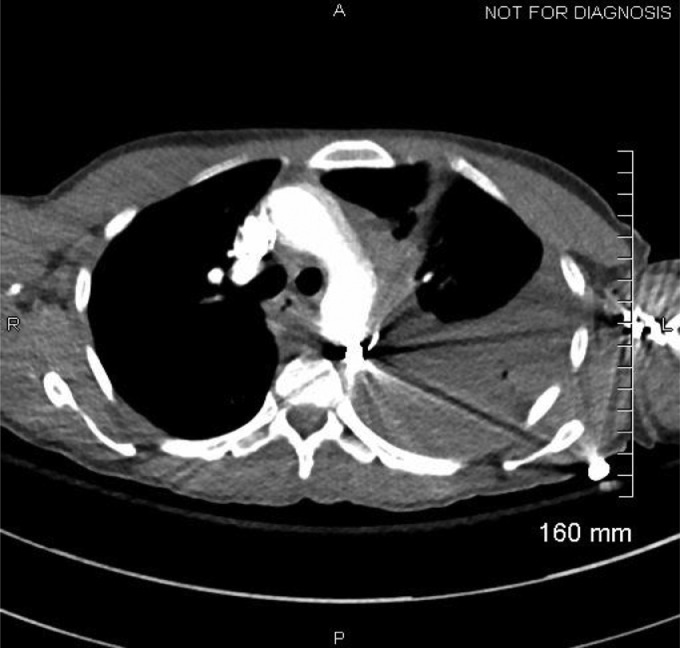
On arrival, the patient undergoes a portable chest x-ray Figure 1. Initial labs show the patient to be anemic (Hgb 9.1) and tachycardic but otherwise normal considering her history. A STAT CTA was performed Figures 2 and 3.
Fig. 1.
Portable Chest X-Ray On Arrival: Large hemopneumothorax demonstrated on the left. A pellet overlies the superior aspect of the mediastinum/aortic arch. This pellet is favored to be intrathoracic and the possibility of vascular injury cannot be excluded.
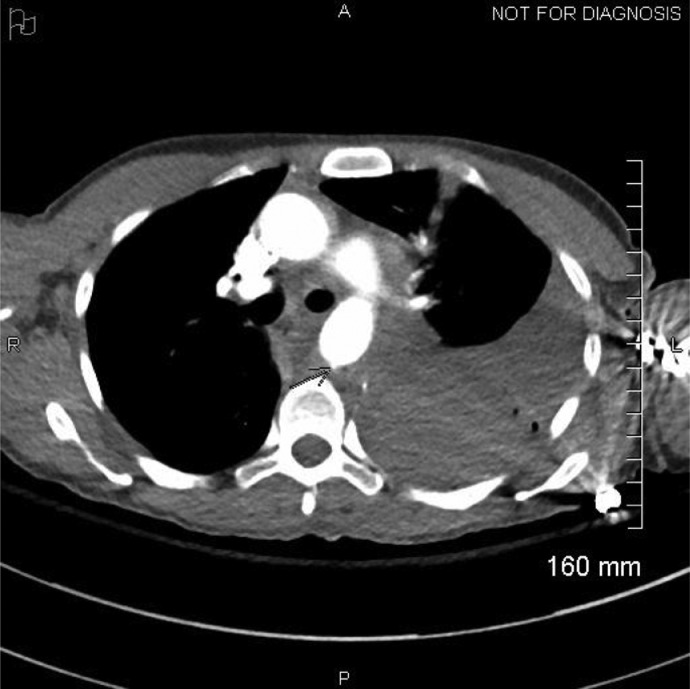
Fig. 2.
Penetrating injury to the left anterior chest wall between the first and second ribs at the costochondral junctions. A small contrast outpouching from the posterior aspect of the proximal descending thoracic aorta (4 cm distal to the left subclavian artery origin) at the level of the embedded pellet appears to represent a vessel infundibulum. However, given extensive periaortic hematoma, a small transmural aortic injury cannot be excluded.
Fig. 3.
Penetrating injury to the left anterior chest wall between the first and second ribs at the costochondral junctions. A small contrast outpouching from the posterior aspect of the proximal descending thoracic aorta (4 cm distal to the left subclavian artery origin) at the level of the embedded pellet appears to represent a vessel infundibulum. However, given extensive periaortic hematoma, a small transmural aortic injury cannot be excluded.
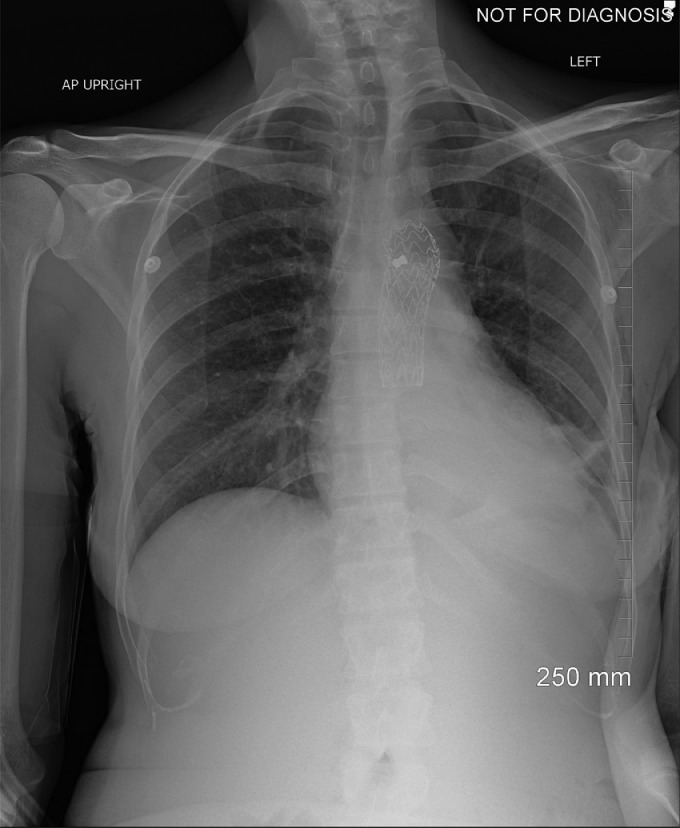
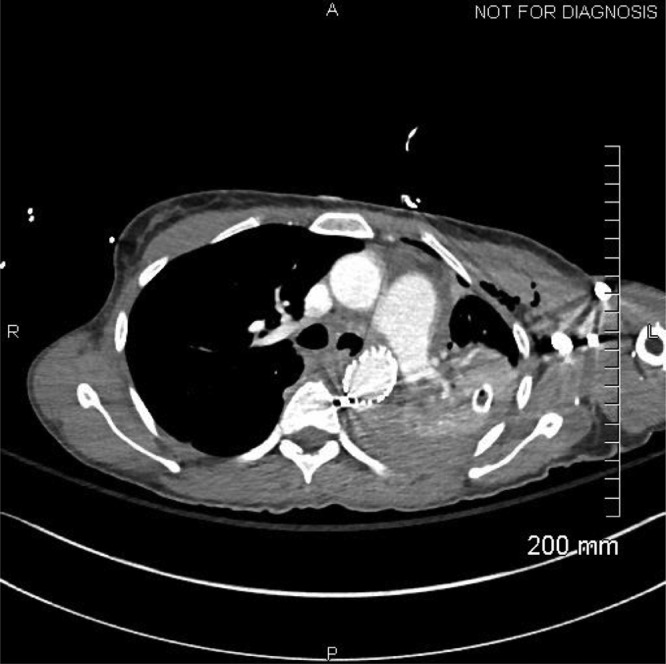
A left chest tube was urgently placed, and the patient was taken to the operating room with vascular surgery, where a thoracic endovascular aortic repair was completed through right femoral arterial access. A 0.26 cm x 10 cm thoracic stent graft was placed. The patient tolerated the procedure well and blood loss was minimal. The patient was placed on daily aspirin therapy postoperatively. Imaging obtained on post-operative day 1 demonstrates interval placement of a stent graft into the descending thoracic aorta and persistent hemopneumothorax Fig. 4, Fig. 5.
Fig. 4.
Portable Chest X-Ray 1: post-operation day 1. Interval placement of descending thoracic aortic stent. Interval placement of a left chest tube. Left-sided hemopneumothorax persists.
Fig. 5.
CT Chest W: post-operation day 1. Interval placement of left-sided thoracostomy tube. Left hemopneumothorax slightly decreased in size compared to prior examination. Interval placement of a stent graft into the descending thoracic aorta traversing a site of previous acute thoracic aortic injury revealed on prior CTA. There is no evidence of active extravasation from this site. Interval development of mucus in the trachea and left main bronchus.
On post-operation day 5, the patient was experiencing minimal thoracostomy tube output, no tube leakage, and chest x-ray evidence of a greatly improved hemopneumothorax, and the thoracostomy tube was withdrawn. Chest x-rays taken after removal showed no recurrence of pneumothorax. During the patient's stay, infectious disease was consulted for management of her uncontrolled HIV. They did not recommend any management at this time due to a history of poor compliance and planned to follow up as an outpatient. The chapter of the Christian Mission at the University of Louisville Hospital was consulted due to the patient's history of homelessness and they arranged for travel after discharge and housing with her uncle who was currently staying with the Christian Mission in Louisville. After the removal of the thoracostomy tube, the patient was amenable to discharge. Her lab values were normal, she did not need a transfusion of blood during her stay.
Discussion
A pellet gun is a type of air gun that uses mechanically compressed air to fire small (<0.5 g) metal projectiles at velocities up to 940 feet/s [1]. They are capable of causing significant penetrating injuries and even death. More than 80% of reported pellet gun injuries occur in patients less than 20 years old, with only 5.4% of injuries occurring in patients 35 or older. The majority of incidents involve young males [2]. Although uncommon, pellet guns have been documented to cause penetrating traumatic injury to the abdominal viscera, heart, lungs, and great vessels [3]. The patient discussed in this case suffered an acute traumatic aortic injury (ATAI) secondary to a pellet gun—a rare mechanism of aortic injury for which there is a paucity of documented cases.
Acute traumatic aortic injuries occur in 1%-2% of all trauma patients at level 1 or level 2 trauma centers. Although the majority of ATAI in the thoracic aorta are caused by motor vehicle collisions, 5% are caused by penetrating gunshot wounds. An associated hemothorax and/or pneumothorax are present in 53.5% of cases involving the thoracic aorta [4]. ATAI are highly lethal, and most cases result in death prior to reaching the hospital. Of those that reach the hospital, 38.2% are hypotensive on admission [5]. After stabilization, rapid detection of ATAI is critical for diagnosis and management. Chest radiographs are often the first opportunity to detect significant mediastinal structure abnormalities and evaluate for any retained penetrating foreign body. The American College of Radiology currently recommends the use of noncontrast computed tomography followed by CTA as the first-line imaging modality when traumatic aortic injury is suspected [6], and recent studies have shown CTA to have excellent sensitivity (96.0%-100%) and specificity (95.0%-99.8%) [4]. Direct signs of ATAI on CTA include pseudoaneurysm, focal contour abnormality, intimal flap, intramural hematoma, an abrupt change in aortic caliber, and contrast extravasation. Careful tracing of the aortic contour in the axial plane can help with identification of subtle abnormalities like pseudoaneurysms [7].
Aortic pseudoaneurysms are most often caused by blunt or penetrating trauma that results in damage to the vessel wall, turbulent blood flow, and formation of a surrounding hematoma contained by a wall of products from the clotting cascade. This wall is weaker than those of a true aneurysm and will ultimately rupture over time if not repaired [8]. Pseudoaneurysms are classified as a grade III aortic injury. Traumatic aortic pseudoaneurysms are preferably treated by thoracic endovascular aortic repair using a prosthetic stent graft [8,9]. Endovascular treatment has very favorable morbidity and mortality rates when compared with open repair, and reported complications are primarily related to prosthetic endovascular grafts in general [9].
Acknowledgment
None.
Patient consent
Written informed consent was obtained for the publication of the current case. No patient identifiers are disclosed.
Footnotes
Competing Interests: none.
Reference
- 1.Stefanopoulos P.K., Pinialidis D.E., Hadjigeorgiou G.F., Filippakis K.N. Wound ballistics 101: the mechanisms of soft tissue wounding by bullets. Eur J Trauma Emerg Surg. 2017;43:579–586. doi: 10.1007/s00068-015-0581-1. [DOI] [PubMed] [Google Scholar]
- 2.McNeill AM, Annest JL. The ongoing hazard of BB and pellet gun-related injuries in the United States. Ann Emerg Med. 1995;26(2):187–194. doi: 10.1016/s0196-0644(95)70150-8. PMID: 7618782. [DOI] [PubMed] [Google Scholar]
- 3.Guenther T, Chen S, Wozniak C, Leshikar D. Fatal cardiac injury sustained from an air gun: case report with review of the literature. Int J Surg Case Rep. 2020;70:133–136. doi: 10.1016/j.ijscr.2020.04.039. Epub 2020 May 11. PMID: 32417728; PMCID: PMC7229402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown SR, Still SA, Eudailey KW, Beck AW, Gunn AJ. Acute traumatic injury of the aorta: presentation, diagnosis, and treatment. Ann Transl Med. 2021;9(14):1193. doi: 10.21037/atm-20-3172. PMID: 34430634; PMCID: PMC8350653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Branco BC, Musonza T, Long MA, Chung J, Todd SR, Wall MJ, et al. Survival trends after inferior vena cava and aortic injuries in the United States. J Vasc Surg. 2018;68(6):1880–1888. doi: 10.1016/j.jvs.2018.04.033. Epub 2018 Jun 28. PMID: 30473029. [DOI] [PubMed] [Google Scholar]
- 6.Demehri S, Rybicki FJ, Desjardins B, Fan CM, Flamm SD, Francois CJ, et al. ACR Appropriateness Criteria(®) blunt chest trauma–suspected aortic injury. Emerg Radiol. 2012;19:287–292. doi: 10.1007/s10140-011-1012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fishman JE, Nuñez D, Kane A, Rivas LA, Jacobs WE. Direct versus indirect signs of traumatic aortic injury revealed by helical CT: performance characteristics and interobserver agreement. AJR Am J Roentgenol. 1999;172(4):1027–1031. doi: 10.2214/ajr.172.4.10587141. PMID: 10587141. [DOI] [PubMed] [Google Scholar]
- 8.Rivera PA, Dattilo JB. StatPearls. StatPearls Publishing; Treasure Island (FL): 2021. Pseudoaneurysm. PMID: 31194401. [Google Scholar]
- 9.Manetta Frank, Newman Joshua, Mattia Allan. Indications for thoracic endovascular aortic repair (TEVAR): a brief review. Int J Angiol. 2018;27(04):177–184. doi: 10.1055/s-0038-1666972. [DOI] [PMC free article] [PubMed] [Google Scholar]