Abstract
Background Context
Fluoroscopic devices can be used to visualize subcutaneous and osseous tissue, a useful feature during pedicle screw insertion in lumbar fusion surgery. It is important that both patient and surgeon are exposed as little as possible, since these devices use potential harmful ionizing radiation.
Purpose
This study aims to compare radiation exposure of different image-guided techniques in lumbar fusion surgery with pedicle screw insertion.
Study Design
Systematic review
Methods
Cochrane, Embase, PubMed and Web of Science databases were used to acquire relevant studies. Eligibility criteria were lumbar and/or sacral spine, pedicle screw, mGray and/or Sievert and/or mrem, radiation dose and/or radiation exposure. Image-guided techniques were divided in five groups: conventional C-arm, C-arm navigation, C-arm robotic, O-arm navigation and O-arm robotic. Comparisons were made based on effective dose for patients and surgeons, absorbed dose for patients and surgeons and exposure. Risk of bias was assessed using the 2017 Cochrane Risk of Bias tool on RCTs and the Cochrane ROBINS-I tool on NRCTs. Level of evidence was assessed using the guidelines of Oxford Centre for Evidence-based Medicine 2011.
Results
A total of 1423 studies were identified of which 38 were included in the analysis and assigned to one of the five groups. Results of radiation dose per procedure and per pedicle screw were described in dose ranges. Conventional C-arm appeared to result in higher effective dose for surgeons, higher absorbed dose for patients and higher exposure, compared to C-arm navigation/robotic and O-arm navigation/robotic. Level of evidence was 3 to 4 in 29 studies. Risk of bias of RCTs was intermediate, mostly due to inadequate blinding. Overall risk of bias score in NRCTs was determined as ‘serious’.
Conclusions
Ranges of radiation doses using different modalities during pedicle screw insertion in lumbar fusion surgery are wide. Based on the highest numbers in the ranges, conventional C-arm tends to lead to a higher effective dose for surgeons, higher absorbed dose for patients and higher exposure, compared to C-arm-, and O-arm navigation/robotic. The level of evidence is low and risk of bias is fairly high. In future studies, heterogeneity should be limited by standardizing measurement methods and thoroughly describing the image-guided technique settings.
Keywords: Systematic review, Lumbar fusion surgery, Image-guided techniques, Radiation dose, Effective dose, Absorbed dose, Exposure, Pedicle screws, Surgeon, Patient
Introduction
Several image-guided techniques have been developed and are used to assist adequate pedicle screw insertion during lumbar fusion surgery. Ionizing radiation in the form of X-rays creates an image of internal tissue by absorption of distinct amounts of radiation [1]. Based on differences in contrast among various organic and osseous tissues, safe pedicle screw insertion and adequate positioning of the pedicle screw is facilitated. The latter is of great importance, as malpositioned screws can cause neurological injuries, which can result in chronic complaints and decreased quality of life [2].
The downside of these image-guided techniques is exposure of patients and surgeons to ionizing radiation, therewith increasing the risk of developing DNA-damage related illnesses [3]. The guiding principle for most health and safety administrations is to keep this risk ‘as low as reasonably achievable’ (ALARA) [4]. This assures a balance between patients and surgeons’ safety on the one side and medical necessity on the other [4]. The two primary methods for reducing surgeons’ exposure to ionizing radiation are lead-based shielding and increased distance to the radiation source [4]. During surgery, lead-based shielding is worn by all subjects in the operating room (OR) except the patient. Increased distance can generally not be applied by those directly involved in surgery. Unavoidable radiation can therefore not be eliminated completely.
During pedicle screw insertion in lumbar fusion surgery, a number of image-guided techniques can be used. Conventional C-arms consist of a radiation-source, using X-ray radiation, and a detector, positioned above one another in a crescent shape [5]. This configuration allows for real time 2-dimensional imaging. By rotating the C-arm, images can be made in several planes and converted into 3-dimensional (3D) images, which are mostly performed preoperatively [6]. These images can be used for C-arm navigation, where a camera keeps track of markers positioned on top of surgical instruments in relation to the spinal markers positioned on the patient [6]. Related to navigation is robotic guidance, where an optimal screw trajectory is planned preoperatively and a robotic arm is guiding the pedicle screw insertion [7]. Another image-guided technique is the O-arm, which derives its name from its circular shape. It is positioned around the patient and encircles the region of interest completely [8]. The arm is manufactured to directly incorporate navigation-, and robotic-guidance [8]. These different X-ray sources can be used preoperatively for pedicle screw trajectory planning, intraoperatively during insertion of pedicle screws and after insertion of pedicle screws as final check of their position.
A recent systematic review and meta-analysis of Pennington et al. concluded that intraoperative CT-navigation resulted in a higher radiation dose for patients compared to other image-guided techniques [9]. Conventional fluoroscopy without navigation resulted in a higher radiation dose for surgeons. However, Pennington et al. included both thoracic and lumbar fusion surgeries, without distinguishing between these areas of the spine. It is important to determine the radiation dose of the short-segment surgeries of the lumbar spine, since there is an increasing trend in the number of lumbar fusion surgeries due to an aging population [10,11], which will expose surgeons to higher cumulative doses of radiation. Furthermore, they did not distinguish between types of radiation doses, being; effective dose (ED), absorbed dose (AD) and dose exposure [12]. In ED calculations, each tissue type has a tissue weighting factor, which is higher for more radiosensitive organs [12]. For example, ED will be higher when the thyroid, being more sensitive to ionizing radiation, is exposed in comparison to muscular tissue. For this reason, ED is the most preeminent outcome to measure radiation dose. ED is expressed in Sievert (Sv) or roentgen equivalent in man (rem) [12]. AD is a measure of the total energy absorbed by a unit mass. AD is expressed in Gray (Gy) or rad (radiation absorbed dose) [12]. Exposure is a measure of energy radiated onto an object expressed as dose area product (DAP) in mGycm2 and dose length product (DLP) in mGycm for C-, and O-arms, respectively [13]. This systematic review therefore aims at comparing radiation exposure of patients and surgeons between different image-guided techniques in lumbar fusion surgery with pedicle screw fixation, namely conventional C-arm, C-arm navigation, C-arm robotic, O-arm navigation and O-arm robotic. This comparison enables us to make recommendations for choosing the image-guided technique with the least radiation exposure, following the ALARA principle.
Methods
Search strategy and study selection
This systematic review was conducted according to the Prisma Statement [14]. The study protocol was approved by the co-authors and submitted to the PROSPERO-database (CRD42020202252). In collaboration with a medical information specialist (see Acknowledgements), searches were conducted using the following databases; PubMed, Cochrane, Embase and Web of Science. Detailed search strategies are available in Additional file 1. The last search was conducted on June 30th, 2021. First, duplicates were removed. Second, studies were screened on title and abstract. Third, full texts were screened on the following eligibility criteria; lumbar and/or sacral spine, pedicle screw, mGy and/or Sv and/or mrem and/or rad, radiation dose and/or radiation exposure. No language, dates of publication and number of patient inclusion restrictions were instated. Furthermore, cadaver and animal studies were included in the analyses. Studies including the thoracic spine were not included, regardless of the inclusion of the lumbosacral spine. Searches were independently performed by three authors (IC, RB, NP). If necessary, consensus was reached between authors through discussion. Gray literature and bibliographies of included studies were not checked for possible missing studies.
Data Extraction
Data were independently collected by three authors (IC, RB, NP), using a prospectively designed data collection sheet. The following data items were considered: year of publication, country of origin, data collection (retrospective or prospective), type of performed lumbar fusion surgery (all include pedicle screw insertion), number of levels of surgery, used image-guided technique, number of included patients, mean age of patient population, number of placed screws per patient, ED for patient and/or surgeon (mSv), AD for patient and/or surgeon (mGy) and exposure (mGycm2 or mGycm), mean radiation per screw. ED dose for surgeons was based on results of unprotected thyroid or chest dosimeters. To optimally compare radiation data, all ED were converted to mSv and AD to mGy. The conversion-factors from rem to mSv and from rad to Gy are both 100; 1 rad is equal to 0,01 Gy. Extracted data were confirmed by the radiation expert (RB).
Quality assessment
Quality of the included studies was assessed by three authors (IC, RD, NP). Level of evidence was determined using the scoring tool of Oxford Centre for Evidence-based Medicine 2011 [15]. Studies were scored between levels one and five, based on study design with a systematic review as level 1 and expert opinion as level 5. Risk of bias of randomized controlled trials (RCTs) was assessed using guidelines of the 2017 Cochrane Risk of Bias tool [16]. Risk of bias for seven distinct domains was determined and scored as a low, high or unclear. Non-randomized controlled trials (NRCTs) and case-series were assessed using the Cochrane ROBINS-I tool [17]. Bias for seven distinct domains was determined. Scores consisted of low, moderate, serious and critical risk of bias. A domain could be scored with ‘no information’ if appropriate information was not described in the study. Contrary to RCTs, the Cochrane handbook advises to determine an overall risk of bias score for NRCTs and case-series. This overall score is equal to the worst given score in any of the seven domains. In case of discrepancies between researchers, scores were discussed until consensus was achieved.
Statistical analysis
Results of studies reporting on two or more different image-guided techniques, were separated per technique. Data were organized in five groups: conventional C-arm, C-arm navigation, C-arm robotic, O-arm navigation and O-arm robotic. Due to heterogeneity and lack of reporting standard deviations, mean results were reported in ranges, as it was not possible to determine pooled means and standard deviations of each image-guided technique. For articles reporting on radiation exposure per patient, mean exposure per pedicle screw was calculated by dividing the mean dose by the mean number of screws placed. For calculated radiation per screw placed, we assumed that all intraoperative radiations were assignable to pedicle screw placement. Mean radiation doses were reported along with the associated standard deviation, where available.
Results
Search results
Results of the study selection process are summarized in of additional file 2. Database searches resulted in identification of 1423 studies. Ninety-seven studies were deemed eligible for full text screening. After full text analysis, 62 studies were excluded; 32 studies had insufficient/incomplete outcome measurements, 23 studies had an unsuitable patient cohort, five studies used the same patient cohorts and two studies did not describe the image-guided techniques that were used. Several studies were from the same research group, five of them were excluded after thorough review by three authors (IC, RD, NP), based on similar years of inclusion, settings of inclusion, number of included patients and baseline characteristics. If these variables differed between studies of the same research group, no reasons were found to assume that the same patients were included in the studies. Thirty-five studies were included for final analysis, including six RCTs [18], [19], [20], [21], [22], [23], 17 NRCTs [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40] and 12 case-series [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52]. Inclusions did not lead to disagreement between reviewers.
Quality assessment
Level of evidence was 2 in six studies [18], [19], [20], [21], [22], [23], 3 in 14 studies [[24], [25], [26],[29], [30], [31], [32], [33], [34], 36,37,39,41,42] and 4 in 15 studies [27,28,35,38,40,[43], [44], [45], [46], [47], [48], [49], [50], [51], [52]]. Risk of bias assessment was summarized in of additional file 3. Allocation concealment, blinding of participants and personnel, and incomplete outcome data were the primary domains of high or unclear risk of bias of RCTs. For NRCTs, overall score was ‘serious risk of bias’ in 27 out of 29 studies.
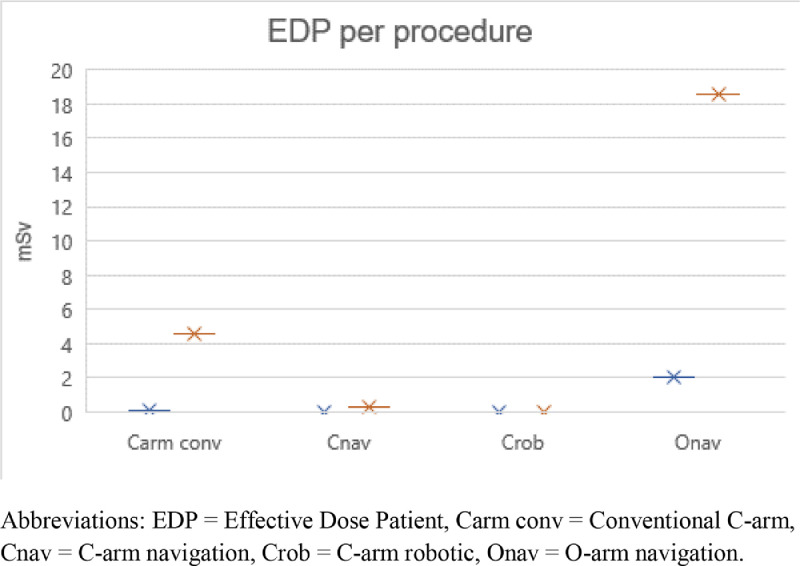
Figure 2.
Ranges of EDP (mSv) per procedure for conventional C-arm group, C-arm navigation group, C-arm robotic group and O-arm navigation group. The blue bar is the lowest value of the range and the orange bar is the highest value.
Abbreviations: EDP = Effective Dose Patient, Carm conv = Conventional C-arm,
Cnav = C-arm navigation, Crob = C-arm robotic, Onav = O-arm navigation.
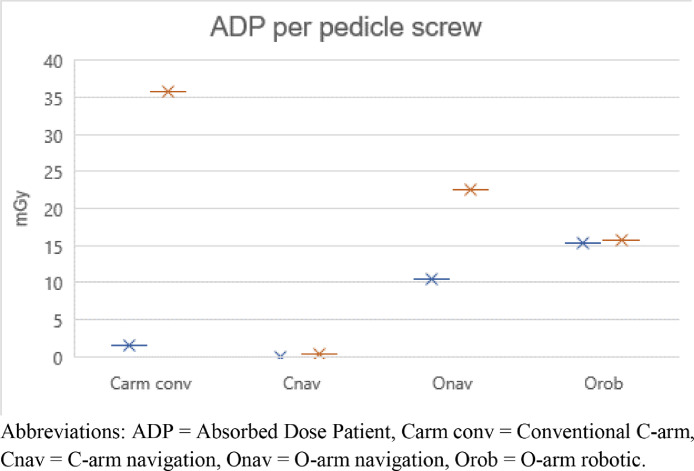
Figure 3.
Ranges of ADP (mGy) per procedure for conventional C-arm group, C-arm navigation group, O-arm navigation group and O-arm robotic group. The blue bar is the lowest valuer of the range and the orange bar is the highest value.
Abbreviations: ADP = Absorbed Dose Patient, Carm conv = Conventional C-arm, Cnav = C-arm navigation, Onav = O-arm navigation, Orob = O-arm robotic.
Study results
Study characteristics of the 35 included studies are summarized per image-guided technique in to 5 of additional files 4 to 8. The included studies are divided in five groups, resulting in 25 studies reporting on conventional C-arm [[18], [19], [20], [21], [22], [23], [24], [25],[28], [29], [30], [31], 33,34,36,39,40,[42], [43], [44], [45],[47], [48], [49], 53], eight studies on C-arm navigation [18,23,25,26,33,34,40,52], four studies on C-arm robotic [19,20,35,36], nine studies on O-arm navigation [27,30,[37], [38], [39], 41,46,50,51] and three studies on O-arm robotic [27,37,38]. Fourteen studies described two different image-guided techniques whose results were reported separately.
Thirteen studies reported retrospective data [18,27,28,35,[37], [38], [39], [40], 45,46,[50], [51], [52]]. Year of publication ranged from 1999 to 2021. Type of surgery was Minimal Invasive Surgery-Transforaminal Lumbar Interbody Fusion (MIS-TLIF) in 26 studies [18,[20], [21], [22], [23], 26,30,31,[33], [34], [35], [36], [37], [38], [39], [40],[42], [43], [44], [45], [46], [47], 49,[51], [52], [53]], Posterolateral Fusion (PLF) in nine studies [19,24,25,27,29,34,41,44,50], open-TLIF in three studies [20,36,37], Lateral Lumbar Interbody Fusion (LLIF) with posterior fixation in two studies [47,48], Anterior Lumbar Interbody Fusion (ALIF) with posterior fixation in two studies [44,47], Posterior Lumbar Interbody Fusion (PLIF) in one study [28] and Extreme Lateral Interbody Fusion (XLIF) with posterior fixation in one study [44]. Surgery was exclusively performed between L1 and S1. Single level surgery took place in 12 studies [[21], [22], [23], 25,26,30,33,41,43,45,49,53], single and double level surgery in seven studies [20,34,35,37,38,42,51], surgery up to three levels in three studies [24,46,47], surgery up to four levels in two studies [39,48] and it was not further specified in 11 studies [18,19,[27], [28], [29], 31,36,40,44,50,52]. Number of included patients ranged from five to 201 patients. Mean age of the included patients ranged from 51.4 to 67.9 years. Mean Body Mass Index (BMI), mentioned in 21 studies, ranged from 23.9 to 33.0 kg/m2 [21,23,24,27,28,31,[34], [35], [36], [37], [38], [39], [40], 43,45,46,[48], [49], [50], [51], [52]].
After data extraction, two articles were excluded from the analyses since in this review, only unprotected dosimeters placed on the thyroid or the chest were included. Hyun et al. did not mention the position of the dosimeter [20]. Grelat et al. only measured ED using dosimeters protected by lead aprons [30]. Results of radiation doses per procedure are described in table 1 and figures 1 to 4, and radiation doses per pedicle screw are described in table 2 and figures 5 to 8. The ranges of all modalities are wide. Looking at the highest numbers of the ranges, it is noticeable that EDS, ADP and exposure of C-arm conventional are the highest.
Table 1.
Mean ranges of EDS, EDP, ADP and exposure per procedure for conventional C-arm group, C-arm navigation group, C-arm robotic group, O-arm navigation group and O-arm robotic group.
| EDS (mSv) per procedure | EDP (mSv) per procedure | ADP (mGy) per procedure | Exposure (mGycm2 or mGycm) per procedure | |
|---|---|---|---|---|
| Carm conv (mean) | 0.009 - 0.3 | 0.1 - 4.6 | 5.4 – 143.2 | 513.0 – 6550.0 |
| Carm conv (median) | - | - | 102.0 - 113.0 | - |
| Cnav | 0.003 – 0.08 | 0.3 | 1.7 – 3.0 | 470.0 – 4700.0 |
| Cnav (median) | - | - | 47.0 | - |
| Crob | 0.03 – 0.04 | 0.02 | - | - |
| Onav | - | 2.0 – 18.6 | 42.9 – 75.8 | 128.3 - 798.3 |
| Orob | - | - | 58.5 – 66.2 | - |
Abbreviations: EDS = Effective Dose Surgeon, EDP = Effective Dose Patient, ADP = Absorbed Dose Patient, Carm conv = Conventional C-arm, Cnav = C-arm navigation, Crob = C-arm robotic, Onav = O-arm navigation, Orob = O-arm robotic.
Figure 1.
Ranges of EDS (mSv) per procedure for conventional C-arm group, C-arm navigation group and C-arm robotic group. The blue bar is the lowest value of the range and the orange bar is the highest value.
Abbreviations: EDS = Effective Dose Surgeon, Carm conv = Conventional C-arm, Cnav = C-arm navigation, Crob = C-arm robotic.
Figure 4.
Ranges of Exposure (mGycm2 or mGycm) per procedure for conventional C-arm group, C-arm navigation group and O-arm navigation group. The blue bar is the lowest value of the range and the orange bar is the highest value.
Abbreviations: Carm conv = Conventional C-arm, Cnav = C-arm navigation, Onav = O-arm navigation.
Table 2.
Mean ranges of EDS, EDP, ADP and exposure per pedicle screw for conventional C-arm group, C-arm navigation group, C-arm robotic group, O-arm navigation group and O-arm robotic group.
| EDS (mSv) per screw | EDP (mSv) per screw | ADP (mGy) per screw | Exposure (mGycm2 or mGycm) per screw | |
|---|---|---|---|---|
| Carm conv (mean) | 0.001 - 0.07 | 0.2 - 1.0 | 1.6 - 35.8 | 617.5 – 1333.1 |
| Cnav | 0.0008 | - | 0.4 | 117.5 – 874.6 |
| Crob | 0.007 - 0.008 | 0.004 | - | - |
| Onav | - | 2.0 - 4.6 | 10.4 - 22.5 | 135.7 |
| Orob | - | - | 15.4 – 15.8 | - |
Abbreviations: EDS = Effective Dose Surgeon, EDP = Effective Dose Patient, ADP = Absorbed Dose Patient, Carm conv = Conventional C-arm, Cnav = C-arm navigation, Crob = C-arm robotic, Onav = O-arm navigation, Orob = O-arm robotic.
Figure 5.
Ranges of EDS (mSv) per pedicle screw for conventional C-arm group, C-arm navigation group and C-arm robotic group. The blue bar is the lowest value of the range and the orange bar is the highest value.
Abbreviations: EDS = Effective Dose Surgeon, Carm conv = Conventional C-arm, Cnav = C-arm navigation, Crob = C-arm robotic.
Figure 8.
Ranges of Exposure (mGycm2 or mGycm) per pedicle screw for conventional C-arm group, C-arm navigation group and O-arm navigation group. The blue bar is the lowest value of the range and the orange bar is the highest value.
Abbreviations: Carm conv = Conventional C-arm, Cnav = C-arm navigation, Onav = O-arm navigation.
ED for the surgeons (EDS) per procedure was calculated in ten conventional C-arm studies [18,19,[21], [22], [23], 25,36,42,44,48], three C-arm navigation studies [18,23,25] and two C-arm robotic studies [19,36]. EDS per pedicle screw was determined in six conventional C-arm studies [19,21,25,36,42,44], one C-arm navigation study [25] and two C-arm robotic studies [19,36]. EDS was not mentioned in O-arm navigation or robotic studies. ED for the patients (EDP) per procedure was calculated in five conventional C-arm studies [23,24,29,39,53], one C-arm navigation study [23], one C-arm robotic study [35] and two O-arm navigation studies [39,51]. EDP per pedicle screw was described in three conventional C-arm studies [24,29,39], one C-arm robotic study [35] and two O-arm navigation studies [39,51]. EDP was not mentioned in O-arm robotic studies. AD for the surgeons (ADS) was not mentioned in any of the included studies and is therefore not described in tables 1 and 2. Mean AD for the patients (ADP) per procedure was mentioned in eight conventional C-arm studies [19,21,22,34,42,44,47,48], two C-arm navigation studies [33,34], four O-arm navigation studies [27,37,38,46] and three O-arm robotic studies [27,38,46]. Median ADP per procedure was mentioned in two conventional C-arm studies [28,45] and in one C-arm navigation study [52]. Mean ADP per pedicle screw was determined in six conventional C-arm studies [21,31,33,42,44,47], one C-arm navigation study [33], two O-arm navigation studies [27,38] and two O-arm robotic studies [27,38]. Exposure per procedure was mentioned in seven conventional C-arm studies [23,33,39,40,43,49,53], four C-arm navigation studies [23,26,33,40] and three O-arm navigation studies [39,41,50]. Exposure per pedicle screw was calculated in four conventional C-arm studies [33,40,43,49], two C-arm navigation studies [33,40] and one O-arm navigation study [41]. None of the C-arm and O-arm robotic studies described exposure.
Discussion
This systematic review compared radiation doses for surgeons and patients using five different image-guided techniques in lumbar fusion surgery with pedicle screw insertion. The majority of patients undergo spinal fusion surgery only once, a minority will need repeated surgery. Surgeons on the other hand are continuously exposed to ionizing radiation during their career [3]. From the patient perspective, all image-guided techniques are safe and associated with comparable patient reported outcomes and complication rates [2]. However, they differ in terms of radiation.
Because of the career-long exposure of their employees, healthcare institutes are obliged to minimize radiation dose of their personnel according to the ALARA principle. In order to implement this ALARA principle for lumbar fusion surgery, it is important to know what the lowest reasonable achievable radiation dose for this type of procedure is. This knowledge should be incorporated when purchasing new image-guided equipment. Potential higher purchasing costs are justified by reducing the risk of DNA-damage-related illness in healthcare professionals.
A total of 35 studies were included for final analyses. Overall risk of bias was intermediate for RCTs and high for NRCTs. Level of evidence was high for the majority of the included studies. Due to heterogeneity, it was not possible to determine pooled means of each image-guided technique.
EDS per procedure and per pedicle screw was higher in conventional C-arm studies compared to C-arm navigation and C-arm robotic studies. It is difficult to directly compare our results to those of Pennington et al., since they have not distinguished between types of radiation measurements like ED, AD or exposure. However, they also stated that overall radiation dose of surgeons was higher using conventional C-arm [9]. The difference between conventional C-arm and C-arm navigation and C-arm robotic can probably be explained by the fact that the surgeon is not present when the preoperative X-rays are made. The maximum radiation dose allowed for healthcare professionals is 20 mSv per year. Using the maximum EDS of the mentioned ranges for conventional C-arm and C-arm navigation/robotic, this results in a total number of allowed lumbar fusion surgeries of 62 per year per healthcare professional using C-arm conventional versus 250 per year per healthcare professional using C-arm navigation and 500 per year per healthcare professional using C-arm robotic.
Studies that directly compare EDP of conventional C-arm with C-arm or O-arm navigation show different results; a lower EDP is found for conventional C-arm in short-segment surgery [23,39], but in long-segment surgery a lower EDP is found for C-arm and O-arm navigation [39]. C-arm and O-arm navigation results in a higher cumulative radiation dose because of preoperative CT-scans, intraoperative 3D navigation and a final check after pedicle screw insertion. In case of long-segment surgery, the cumulative radiation dose for C-arm and O-arm navigation remains the same, while the radiation dose of conventional C-arm increases due to the need of more intraoperative fluoroscopy. Since most patients included in this review underwent single level surgery, radiation dose per pedicle screw is also higher in O-arm navigation compared to conventional C-arm.
Results per procedure and pedicle screw of ADP and exposure are opposite to results of EDP; equal or higher doses of ADP using conventional C-arm compared to O-arm navigation, and higher exposure using conventional C-arm compared to O-arm and C-arm navigation. The difference between ADP, exposure and EDP in this review could be explained by the fact that EDP depends on radiation sensitivity of the radiated tissue and therefor depends on direction of radiation. For example, ADP and exposure of lateral fluoroscopy result in a lower EDP than ADP and exposure in anterior-posterior direction. This is also described by Chang et al., with lateral exposure of 4.16 and anterior-posterior exposure of 2.39, with conversion coefficients to determine EDP of, respectively, 0.092 and 0.22 [39]. This results in a reversed result for EDP.
Results of this systematic review were described in ranges due to heterogeneity between studies, which is caused by multiple aspects. First, radiation dose is dependent on type of surgery. Wang et al. compared radiation dose of open-TLIF with MIS-TLIF and concluded that the open approach resulted in lower ADP [37]. These findings are comparable with a review of Yu et al., and may be the result of decreased visual feedback in case of minimal invasive surgery [54]. Due to heterogeneity and lack of data, it is not possible to distinguish between type of surgeries in this systematic review.
Second, as described in to 5 of additional files 4 to 8, the number of surgical levels differed between studies. For this reason, doses per pedicle screw were calculated. However, number of pedicle screws per procedure was not available for every study, which resulted in missing data.
Third, differences in imaging-plane can occur when using conventional C-arm. Images can be made in the lateral plane, anterior-posterior plane, oblique plane or a combination. This could influence the amount of radiation dose. For example, Tumialan et al. and Clark et al. used lateral conventional C-arm images. They described lower exposure doses compared to Fomekong et al., who used lateral and anterior-posterior images [40,43,49].
Fourth, multiple studies determined a positive correlation between radiation dose and BMI [31,39,45,46,48,49], since higher radiation doses are needed, to adequatly penetrate the tissues. BMI differs between study populations, which could have affected the comparison between studies.
Fifth, publication year and time of research may have affected the results, using more advanced knowledge and technology regarding image-guided techniques in more recent studies. For example, Fan et al., published in 2017, described an ADP of 0.58 mGy, while Slomczykowski et al. and Jones et al., published in, respectively, 1999 and 2000, described an ADP of, respectively, 1.0 mGy and 4.6 mGy [24,29,32]. In addition, learning curves of surgeons could influence total radiation dose [22,26,42,46,47]. Kukreja et al. (conventional C-arm), Hyun et al. (conventional C-arm and C-arm robotic) and Balling et al. (O-arm navigation) described that having more experienced surgeons will lead to lower radiation exposure of OR staff [20,41,45]. However, Vaishnav et al. (C-arm navigation) and Khan et al. (O-arm navigation and O-arm robotic) did not find a learning curve based on fluoroscopy time or radiation dose [38,52]. Furthermore, the type of hospital might also affect results. For example, radiation dose could be higher in a teaching/academic hospital due to participation of less experienced residents, compared to a general hospital. None of the included studies discuss this topic.
Figure 6.
Ranges of EDP (mSv) per pedicle screw for conventional C-arm group, C-arm navigation group, C-arm robotic group and O-arm navigation group. The blue bar is the lowest value of the range and the orange bar is the highest value.
Abbreviations: EDP = Effective Dose Patient, Carm conv = Conventional C-arm,
Cnav = C-arm navigation, Crob = C-arm robotic, Onav = O-arm navigation.
Figure 7.
Ranges of ADP (mGy) per pedicle screw for conventional C-arm group, C-arm navigation group, O-arm navigation group and O-arm robotic group. The blue bar is the lowest value of the range and the orange bar is the highest value.
Abbreviations: ADP = Absorbed Dose Patient, Carm conv = Conventional C-arm, Cnav = C-arm navigation, Onav = O-arm navigation, Orob = O-arm robotic.
Differences between studies in reported radiation doses, could not be associated with risk of bias, study design (prospective or retrospective) or level of evidence.
Lastly, this study included only full text, published studies and excluded conference proceedings, PhD dissertations and other grey literature. Furthermore, bibliographies of included studies were not checked for missing studies. This might have resulted in publication bias.
After finalizing this systematic review, we can conclude that comparison between techniques is challenging due to the lack of standardization of research on image-guided procedures. For example, surgeons should wear unprotected dosimeters on the chest or thyroid region. Standardization could help to adequately compare radiation doses of image-guided techniques. Moreover, studies reporting on radiation doses, should give extended information about the image-guided technique and settings that were used.
Conclusion
This systematic review compared radiation dose experienced by patients and surgeons during pedicle screw insertion in lumbar fusion surgery. Healthcare professionals should be exposed to radiation as low as reasonably achievable (ALARA) to minimize the risk of developing DNA-damage related illnesses. Ranges of radiation doses using different modalities during pedicle screw insertion in lumbar fusion surgery are wide. Based on the highest numbers in the ranges, conventional C-arm may lead to a higher effective dose for surgeons, higher absorbed dose for patients and higher exposure, compared to C-arm-, and O-arm navigation/robotic. The maximum radiation dose allowed for healthcare professionals is 20 mSv per year. Using the maximum EDS, this results in an total number of allowed lumbar fusion surgeries of 62 per year per healthcare professional using conventional C-arm, 250 per year per healthcare professional using C-arm navigation and 500 per year per healthcare professional using C-arm /robotic. However, due to heterogeneity, comparability is limited. For this reason, standardization of measurement methods and description of image-guided technique settings are recommended in future practice in order to aid prospective scientific research on this topic.
Declaration of Competing Interest
Ethics approval and consent to participate: not applicable.
Acknowledgments
Consent of publication
Not applicable.
Availability data and materials
All data generated or analyzed during this study are included in this article and its supplementary information files.
Funding
Not applicable.
Authors’ contributions
I.C., R.B., R.D. and N.P. worked on the search, data analyses en wrote the main manuscript. All authors reviewed the manuscript.
Acknowledgements
We would like to thank Mr. Gregor Franssen, medical information specialist Maastricht University, the Netherlands, for his assistance in optimizing the search strategy.
Footnotes
FDA device/drug status: Not applicable.
Author disclosures: IJMHC: Nothing to disclose. RCMB: Nothing to disclose. RD: Nothing to disclose. NJJP: Nothing to disclose. KR: Nothing to disclose. WLWVH: Nothing to disclose. RADB: Nothing to disclose. HVS: Nothing to dislose.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.xnsj.2023.100199.
Appendix. Supplementary materials
References
- 1.Bushberg J.T., Seibert J.A., Leidholdt E.M., Boone J.M. 2nd ed. Lippincott Williams & Wilkins; 2002. The Essential Physics of Medical Imaging. [Google Scholar]
- 2.Caelers I.J.M.H., Van Santbrink H., Rijkers K., Van Kuijk S.M.J., De Bie R.A., Van Hemert W.L.W. Neurological events due to pedicle screw malpositioning with lateral fluoroscopy–guided pedicle screw insertion. J Neurosurg Spine. 2020:1–6. doi: 10.3171/2020.5.SPINE20550. [DOI] [PubMed] [Google Scholar]
- 3.Hadelsberg U.P., Harel R. Hazards of ionizing radiation and its impact on spine surgery. World Neurosurg. 2016;92:353–359. doi: 10.1016/j.wneu.2016.05.025. [DOI] [PubMed] [Google Scholar]
- 4.Stokell P J., Croft J R., Lochard J., Lombard J. In: From theory towards practice. CotE Communities., editor. Luxembourg; 1991. Alara. [Google Scholar]
- 5.Mitchell E.L., Furey P. Prevention of radiation injury from medical imaging. J Vasc Surg. 2011;53:22–27. doi: 10.1016/j.jvs.2010.05.139. [DOI] [PubMed] [Google Scholar]
- 6.Euler E., Heining S., Riquarts C., Mutschler W. C-Arm-based three-dimensional navigation: a preliminary feasibility study. Comput Aided Surg. 2003;8:35–41. doi: 10.3109/10929080309146101. [DOI] [PubMed] [Google Scholar]
- 7.Burström G., Balicki M., Patriciu A., et al. feasibility and accuracy of a robotic guidance system for navigated spine surgery in a hybrid operating room: a cadaver study. Nat Res. 2020;10(7522):1–9. doi: 10.1038/s41598-020-64462-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Verma S.K., Singh P.K., Agrawal D., et al. O-arm with navigation versus C-arm: a review of screw placement over 3 years at a major trauma center. Br J Neurosurg. 2016;30(6):658–661. doi: 10.1080/02688697.2016.1206179. [DOI] [PubMed] [Google Scholar]
- 9.Pennington Z., Cottrill E., Westbroek E.M., et al. Evaluation of surgeon and patient radiation exposure by imaging technology in patients undergoing thoracolumbar fusion: systematic review of the literature. Spine J. 2019;19:1397–1411. doi: 10.1016/j.spinee.2019.04.003. [DOI] [PubMed] [Google Scholar]
- 10.Grotle M., Småstuen M.C., Fjeld O., et al. Lumbar spine surgery across 15 years: trends, complications and reoperations in a longitudinal observational study from Norway. BMJ Open. 2019;9:1–7. doi: 10.1136/bmjopen-2018-028743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Caelers I.J.M.H., De Kunder S.L., Rijkers K., et al. Comparison of (Partial) economic evaluations of transforaminal lumbar interbody fusion (TLIF) versus Posterior lumbar interbody fusion (PLIF) in adults with lumbar spondylolisthesis: a systematic review. PLoS One. 2021;16(2):1–12. doi: 10.1371/journal.pone.0245963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fisher D.R., Fahey F.H. Appropriate use of effective dose in radiation protection and risk assessment. Health Phys. 2017;113(2):102–109. doi: 10.1097/HP.0000000000000674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nickoloff E.L., Lu Z.F., Dutta A.K., So J.C. Radiation dose descriptors: BERT, COD, DAP, and other strange creatures. Radiographics. 2008;28:1439–1450. doi: 10.1148/rg.285075748. [DOI] [PubMed] [Google Scholar]
- 14.Moher D., Liberati A., Tetzlaff J., Altman D.G., The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Howick J., Chalmers I., Glasziou P., et al. 2011. Oxford Centre for Evidence-Based Medicine 2011 Levels of Evidence.http://www.cebm.net/index.aspx?o=5653 Available from. [Google Scholar]
- 16.Higgins J.P.T., Altman D G., Sterne J.A.C. In: Cochrane Handbook for Systematic Reviews of Interventions Version 510. Higgins J.P.T., editor. The Cochrane Collaboration; 2011. Chapter 8: Assessing risk of bias in included studies. [Google Scholar]
- 17.Sterne J.A.C., Hernán M.A., Reeves B.C., et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;335:1–7. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim C.W., Lee Y., Taylor W., Oygar A., Kim W.K. Use of navigation-assisted fluoroscopy to decrease radiation exposure during minimally invasive spine surgery. Spine J. 2008;8:584–590. doi: 10.1016/j.spinee.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 19.Feng S., Tian W., Sun Y., Liu Y., Wei Y. Effect of robot-assisted surgery on lumbar pedicle screw internal fixation in patients with osteoporosis. World Neurosurg. 2019;125 doi: 10.1016/j.wneu.2019.01.243. e1057-e62. [DOI] [PubMed] [Google Scholar]
- 20.Hyun S., Kim K., Jahng T., Kim H. Minimally invasive robotic versus open fluoroscopic-guided spinal instrumented fusions, a randomized controlled trial. Spine. 2017;42(6):353–358. doi: 10.1097/BRS.0000000000001778. [DOI] [PubMed] [Google Scholar]
- 21.Wang T.Y., Harrison S., Perkins S.S., et al. Internally randomized control trial of radiation exposure using ultra-low radiation imaging versus traditional C-arm fluoroscopy for patients undergoing single-level minimally invasive transforaminal lumbar interbody fusion. Spine. 2017;42(4):217–223. doi: 10.1097/BRS.0000000000001720. [DOI] [PubMed] [Google Scholar]
- 22.Fan G., Fu Q., Gu G., Zhang H., et al. Radiation exposure to surgeon in minimally invasive transforaminal lumbar interbody fusion with novel spinal locators. J Spinal Disord Tech. 2015;28 doi: 10.1097/BSD.0000000000000210. e178-e80. [DOI] [PubMed] [Google Scholar]
- 23.Klingler J., Scholz C., Krüger M.T., et al. Radiation exposure in minimally invasive lumbar fusion surgery; a randomized controlled trial comparing conventional fluoroscopy and 3d fluoroscopy-based navigation. Spine. 2020;46(1):1–8. doi: 10.1097/BRS.0000000000003685. [DOI] [PubMed] [Google Scholar]
- 24.Slomczykowski M., Roberto M., Schneeberger P., Ozdoba C., Vock P. Radiation dose for pedicle screw insertion, fluoroscopic method versus computer-assisted sugery. Spine. 1999;24(10):975–983. doi: 10.1097/00007632-199905150-00009. [DOI] [PubMed] [Google Scholar]
- 25.Smith H.E., Welsch M.D., Sasso R.C., Vaccaro A.R. Comparison of radiation exposure in lumbar pedicle screw placement with fluoroscopy vs computer-assisted image guidance with intraoperative three-dimensional imaging. J Spinal Cord Med. 2008;31:532–537. doi: 10.1080/10790268.2008.11753648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rieger B., Jiang H., Reinshagen C., et al. Effects of preoperative simulation on minimally invasive hybrid lumbar interbody fusion. World Neurosurg. 2017;106:578–588. doi: 10.1016/j.wneu.2017.06.184. [DOI] [PubMed] [Google Scholar]
- 27.Khan A., Meyers J.E., Yavorek S., et al. Comparing next-generation robotic technology with 3-dimensional computed tomography navigation technology for the insertion of posterior pedicle screws. World Neurosurg. 2019;123 doi: 10.1016/j.wneu.2018.11.190. e474-e81. [DOI] [PubMed] [Google Scholar]
- 28.Kageyama H., Yoshimura S., Uchida K., Iida T. Advantages and disadvantages of multi-axis intraoperative angiography unit for percutaneous pedicle screw placement in the lumbar spine. Neurol Med Chir. 2017;57:481–488. doi: 10.2176/nmc.oa.2017-0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jones D.P.G., Robertson P.A., Lunt B., Jackson S.A. Radiation exposure during fluoroscopically assisted pedicle screw insertion in the lumbar spine. Spine. 2000;25(12):1538–1541. doi: 10.1097/00007632-200006150-00013. [DOI] [PubMed] [Google Scholar]
- 30.Grelat M., Zairi F., Quidet M., Marinho P., Allaoui M., Assaker R. Assessment of the surgeon radiation exposure during a minimally invasive TLIF: comparison between fluoroscopy and O-arm system. Neurochirurgie. 2015;61:255–259. doi: 10.1016/j.neuchi.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 31.Godzik J., Nayar G., Hunter W.D., Tumialan L.M. Decreasing radiation emission in minimally invasive spine surgery using ultra-low-radiation imaging with image enhancement: a prospective cohort study. World Neurosurg. 2019;12 doi: 10.1016/j.wneu.2018.10.150. e805-e11. [DOI] [PubMed] [Google Scholar]
- 32.Fan G., Zhang H., Gu X., et al. Significant reduction of fluoroscopy repetition with lumbar localization system in minimally invasive spine surgery, a prospective study. Medicine. 2017;96(21):1–9. doi: 10.1097/MD.0000000000006684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dusad T., Kundnani V., Dutta S., Patel A., Mehta G., Singh M. Comparative prospective study reporting intraoperative parameters, pedicle screw perforation, and radiation exposure in navigation-guided versus non-navigated fluoroscopy-assisted minimal invasive transforaminal lumbar interbody fusion. Asian Spine J. 2018;12(2):309–316. doi: 10.4184/asj.2018.12.2.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hamouda F., Wang T.Y., Gabr M., et al. A prospective comparison of the effects of instrument tracking on time and radiation during minimally invasive lumbar interbody fusion. World Neurosurg. 2021:E1–E11. doi: 10.1016/j.wneu.2021.05.058. [DOI] [PubMed] [Google Scholar]
- 35.Du J., Gao L., Huang D., et al. Radiological and clinical differences between robotic‑assisted pedicle screw fixation with and without real‑time optical tracking. Eur Spine J. 2021;30:142–150. doi: 10.1007/s00586-020-06641-y. [DOI] [PubMed] [Google Scholar]
- 36.Zhang Q., Han X., Xu Y., et al. Robot-assisted versus fluoroscopy-guided pedicle screw placement in transforaminal lumbar interbody fusion for lumbar degenerative disease. World Neurosurg. 2019;125 doi: 10.1016/j.wneu.2019.01.097. e429-e34. [DOI] [PubMed] [Google Scholar]
- 37.Wang E., Manning J., Varlotta C.G., et al. Radiation exposure in posterior lumbar fusion: a comparison of ct image-guided navigation, robotic assistance, and intraoperative fluoroscopy. Global Spine J. 2021;11(4):450–457. doi: 10.1177/2192568220908242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khan A., Rho K., Mao J.Z., et al. Comparing cortical bone trajectories for pedicle screw insertion using robotic guidance and three-dimensional computed tomography navigation. World Neurosurg. 2020;141 doi: 10.1016/j.wneu.2020.05.257. e625-e32. [DOI] [PubMed] [Google Scholar]
- 39.Chang C., Chang H., Wu J., Tu T., Cheng H., Huang W. Comparison of radiation exposure between O-Arm navigated and C-Arm guided screw placement in minimally invasive transforaminal lumbar interbody fusion. World Neurosurg. 2020;139 doi: 10.1016/j.wneu.2020.04.052. e489-e95. [DOI] [PubMed] [Google Scholar]
- 40.Fomekong E., Pierrard J., Raftopoulos C. Comparative cohort study of percutaneous pedicle screw implantation without versus with navigation in patients undergoing surgery for degenerative lumbar disc disease. World Neurosurg. 2018;111 doi: 10.1016/j.wneu.2017.12.080. E110-E7. [DOI] [PubMed] [Google Scholar]
- 41.Balling H. Learning curve analysis of 3D-fluoroscopy image-guided pedicle screw insertions in lumbar single-level fusion procedures. Arch Orthop Trauma Surg. 2018;138:1501–1509. doi: 10.1007/s00402-018-2994-x. [DOI] [PubMed] [Google Scholar]
- 42.Bindal R.K., Glaze S., Ognoskie M., Tunner V., Malone R., Ghosh S. Surgeon and patient radiation exposure in minimally invasive transforaminal lumbar interbody fusion. J Neurosurg Spine. 2008;9:570–573. doi: 10.3171/SPI.2008.4.08182. [DOI] [PubMed] [Google Scholar]
- 43.Clark J.C., Jasmer G., Marciano F.F., Tumialán L.M. Minimally invasive transforaminal lumbar interbody fusions and fluoroscopy: a low-dose protocol to minimize ionizing radiation. Neurosurg Focus. 2013;35(2):1–7. doi: 10.3171/2013.5.FOCUS13144. [DOI] [PubMed] [Google Scholar]
- 44.Harrison S., Nayar G., Desai R., et al. Radiation exposure to the surgeon during minimally invasive spine procedures is directly estimated by patient dose. Eur Spine J. 2018;27:1911–1917. doi: 10.1007/s00586-018-5653-6. [DOI] [PubMed] [Google Scholar]
- 45.Kukreja S., Haydel J., Nanda A., Sin A.H. Impact of body habitus on fluoroscopic radiation emission during minimally invasive spine surgery. J Neurosurg Spine. 2015;22:211–218. doi: 10.3171/2014.10.SPINE14163. [DOI] [PubMed] [Google Scholar]
- 46.Safaee M.M., Oh T., Pekmezci M., Clark A.J. Radiation exposure with hybrid image-guidance-based minimally invasive transforaminal lumbar interbody fusion. J Clin Neurosci. 2018;48:122–127. doi: 10.1016/j.jocn.2017.09.026. [DOI] [PubMed] [Google Scholar]
- 47.Spitz S.M., Sandhu F.A., Voyadzis J. Percutaneous “K-wireless” pedicle screw fixation technique: an evaluation of the initial experience of 100 screws with assessment of accuracy, radiation exposure, and procedure time. J Neurosurg Spine. 2015;22:422–431. doi: 10.3171/2014.11.SPINE14181. [DOI] [PubMed] [Google Scholar]
- 48.Taher F., Hughes A.P., Sama A.A., et al. 2013 Young investigator award winner: how safe is lateral lumbar interbody fusion for the surgeon? Spine. 2013;38(16):1386–1392. doi: 10.1097/BRS.0b013e31828705ad. [DOI] [PubMed] [Google Scholar]
- 49.Tumialan L.M., Clark J.C., Snyder L.A., Jasmer G., Marciano F.F. Prospective evaluation of a low-dose radiation fluoroscopy protocol for minimally invasive transforaminal lumbar interbody fusion. Operat Neurosurg. 2015;11:537–544. doi: 10.1227/NEU.0000000000000960. [DOI] [PubMed] [Google Scholar]
- 50.Reynolds A.W., Philp F.H., Gandhi S., Schmidt G.L. Patient radiation exposure associated with the use of computer navigation during spinal fusion. Int J Spine Surg. 2020;14(4):534–537. doi: 10.14444/7070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Venier A., Croci D., Robert T., Distefano D., Presilla S., Scarone P. Use of intraoperative computed tomography improves outcome of minimally invasive transforaminal lumbar interbody fusion: a single-center retrospective cohort study. World Neurosurg. 2021;148 doi: 10.1016/j.wneu.2021.01.041. e572-e80. [DOI] [PubMed] [Google Scholar]
- 52.Vaishnav A.S., Gang C.H., Qureshi S.A. Time-demand, radiation exposure and outcomes of minimally invasive spine surgery with the use of skin-anchored intraoperative navigation; the effect of the learning curve. Clin Spine Surg. 2021 doi: 10.1097/BSD.0000000000001167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Fan G., Fu Q., Zhang J., et al. Radiation reduction of minimally invasive transforaminal lumbar interbody fusion with localisation system in overweight patients. Bone Joint J. 2017;99B(7) doi: 10.1302/0301-620X.99B7.BJJ-2016-0853.R1. [DOI] [PubMed] [Google Scholar]
- 54.Yu E., Khan S.N. Does less invasive spine surgery result in increased radiation exposure? A systematic review. Clin Orthop Relat Res. 2014;472:1738–1748. doi: 10.1007/s11999-014-3503-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.