Abstract
Objective
The early outbreak period of Coronavirus Disease (COVID-19) has affected the emergency department (ED) and hospital services in many countries. This study aimed to investigate the association between COVID-19 outbreak and in-hospital mortality in Jakarta, Indonesia.
Methods
This retrospective cohort study was conducted in a single-centre referral hospital in Jakarta, Indonesia. Data were collected between May and October 2020. All patients who visited the ED and required inpatient care during the early COVID-19 outbreak period at the study location (March to April 2020) were included in the exposure group. All patients who visited the ED and required inpatient care during the non-outbreak period (March to April 2019) were included in the non-exposure group. In-hospital mortality was the primary outcome, whereas other variables, such as sex, age, triage categories, trauma cases, referral cases, and ED length of stay (LOS), were measured to identify confounding and effect modifications. Multivariate logistic regression analysis was performed to assess this association.
Results
A total of 2,808 patients during the outbreak period and 2,423 patients during the non-outbreak period participated in the study. The odds of in-hospital mortality increased during the outbreak period compared to that during the non-outbreak period (odds ratio [OR], 1.41; 95%CI 1.04–1.91; p = 0.01) after adjusting for age, sex, triage categories, trauma case, ED LOS, and interaction between the outbreak period and ED LOS.
Conclusion
COVID-19 outbreaks have been associated with an increased risk of in-hospital mortality in referral hospitals in Jakarta, Indonesia.
Keywords: COVID-19, Emergency department, Indonesia, Mortality, Outbreak
1. Introduction
In March 2020, Indonesia declared that the coronavirus disease-19 (COVID-19) has caused a national disaster.1 , 2 In the initial outbreak period, Jakarta was one of the regions with the highest COVID-19-related transmission and mortality rates in Indonesia.3 At the end of April 2020, mortality due to confirmed cases in Indonesia was 765, of which 379 were from Jakarta.4 , 5 As of October 2020, the total number of positive cases in Indonesia was 336,716, and the mortality rate was 3.5%.4
Many countries have developed various public health interventions to respond to the initial COVID-19 outbreak, which would impact hospital services, especially in the emergency department (ED). European countries, the United States, and other Asian countries have reported decreases in emergency visits, inpatient admissions, and fewer ambulance calls6, 7, 8 owing to lockdown policies and work-from-home campaigns.9
To manage the surge in COVID-19 cases, restrictions on mass gathering and work- and school-from-home policies were impleneted in Jakarta, Indonesia. Public hospitals in Jakarta were then divided into dedicated COVID-19 referral hospitals and regular referral hospitals (which did not manage patients with COVID-19).10 Nevertheless, in Indonesia and other countries, the number of COVID-19 cases exceeded the capacity of COVID-19 referral hospitals, leading to many ambulance diversions to the EDs of regular hospitals.11
This condition became a double burden in regular hospitals because suspected COVID-19 cases were sporadically admitted to the ED for simultaneous management with non-COVID-19 cases. As a result, the ED should perform routine COVID-19 screening in many patients with respiratory diseases and divide the ED service into two areas, the COVID-19 related isolation room and the regular ED area.12
Due to the lack of testing capacity for reverse transcriptase polymerase chain reaction (RT-PCR) for the detection of Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2) at the beginning of the COVID-19 outbreak in Indonesia,13 , 14 the ED became overcrowded because of prolongation in the decision to admit to the ward.
Studies from several countries have reported that ED services for both COVID-19 and non-COVID-19 cases were severely affected during the early outbreak in 2020.11, 12, 13 There are no previous reports on the ED situation related to the outbreak of COVID-19 and its effect on clinical outcomes in Indonesia. Thus, we performed an observational study to evaluate the association between the COVID-19 outbreak and in-hospital mortality in a regular referral hospital in Jakarta, Indonesia and adjusted for other ED-related variables.
2. Methods
This was a retrospective cohort study to identify the association of the COVID-19 outbreak with in-hospital mortality, conducted from May to October 2020 at Dr. Cipto Mangunkusumo Hospital, an academic tertiary hospital in Jakarta, Indonesia. The hospital had 73 beds in the ED and a 927 bed capacity for inpatient care; the annual census of the ED was approximately 30,000 visits per year.15 , 16 At the beginning of the outbreak (March to April 2020), the hospital was a regular referral hospital (not a COVID-19-referral hospital).10 This study was approved by the institutional ethics board of the hospital. The protocol number was 20-06-0700 (Supplementary File 1). All patient data were treated with confidentiality, in accordance with the Declaration of Helsinki. This observational study conforms to the STROBE statement (Supplementary File 2).17
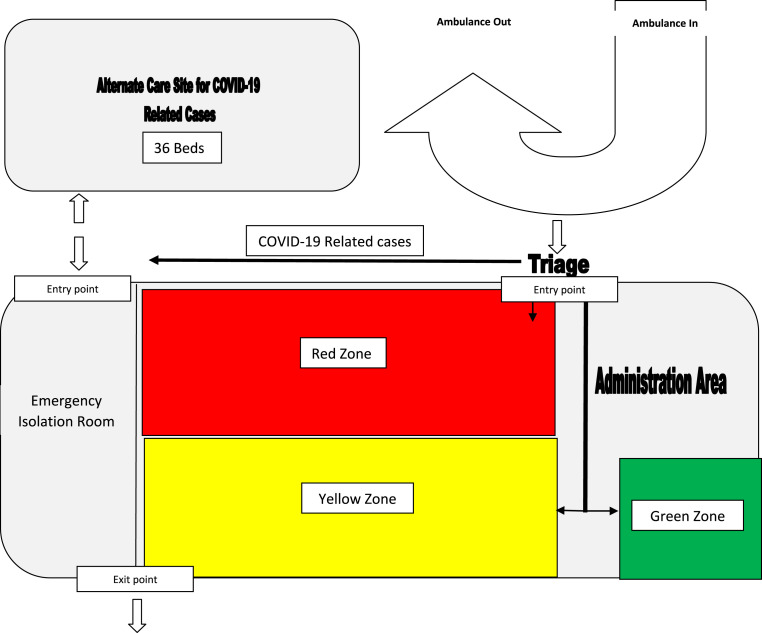
The primary outcome of the study (dependent variable) was in-hospital mortality. Patients who were referred to another hospital were considered alive as a hospital outcome. The ED admission period was the independent variable, consisting of the exposure group (initial outbreak period in Jakarta from March to April 2020) and non-exposure group (non-outbreak period from March to April 2019). We limited the initial outbreak period to March to April 2020 because the ED became the backbone of the management of the surge influx of COVID-19-related cases during this period (Schematic map of ED zone is available in Fig. 1 ). The hospital's definitive COVID-19 isolation service was fully operational in May 2020.
Fig. 1.
ED zone and flow during early outbreak of COVID-19 March 2020.
Sex, age in years, triage categories based on the local triage system,15 number of patients with trauma (including minor trauma such as strained ankle as well as major trauma), and ED length of stay (LOS) were identified as potential confounders. ED LOS was defined as the time from patient admission to the ED until administrative discharge from the ED (outpatient, inpatient, referred to another hospital, or died). We included referral status as an exploratory variable to evaluate its effect on the association between the main independent variable and dependent variable because Indonesia had not yet established a system of emergency medical services to manage referral and ambulance services; thus, many referral cases from other healthcare facilities were sent to our ED without any pre-hospital coordination. COVID-19-related cases (suspected or confirmed) in the ED were identified and descriptively reported.18
2.1. Population and sample
The source population consisted of all patients who visited the ED at Dr. Cipto Mangunkusumo Hospital, excluding patients with visits that were administratively recorded as ED visits for non-ED purposes such as outpatient paediatric haemodialysis, routine intravenous treatment, intrauterine foetal death (IUFD), death on arrival (DOA), newborns, and visits for visum and repertum purposes. The eligible population included patients who visited the ED and required inpatient care (excluding cancelled treatment and outpatient care after the ED assessment). If repeated ED visits occurred during the study period, only the last visit was included.
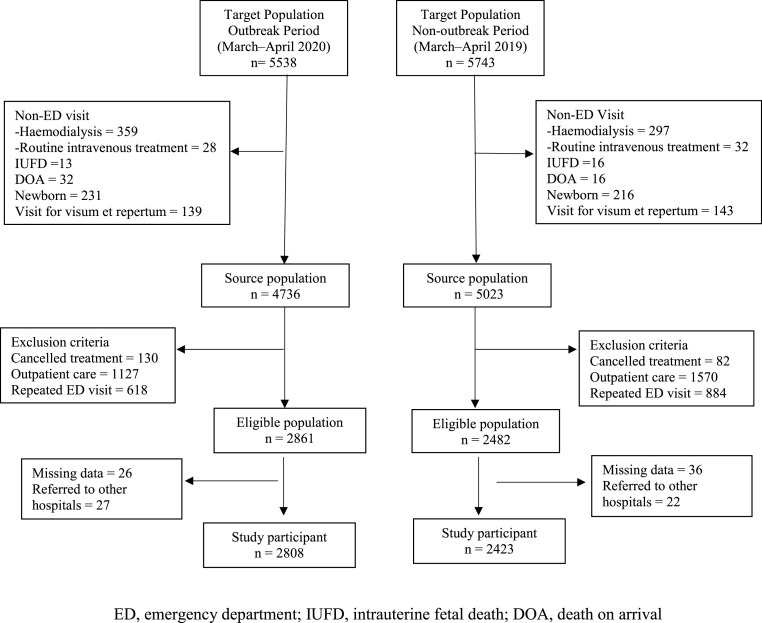
Patients referred to another hospital from the ED were excluded from the study. Study participants with complete data on these variables were considered eligible (Fig. 2 ). As the required information was obtained from the Electronic Health Record (EHR), blinding during data collection of the exposure and outcome was not required. The patients were not included in any research stage in this study.
Fig. 2.
Flow chart of study participant selection process
ED, emergency department; IUFD, intrauterine fetal death; DOA, death on arrival.
Using an electronic database, the ED data management team provides a database of all patient visits during the non-outbreak and outbreak periods. The study authors (HH,IAA,SS,RMM) identified and included all eligible patients for the analysis (total sampling) and obtained demographic, laboratory, and ED flow data from each eligible patient.
2.2. Data analysis
The descriptive information is presented in tables. Categorical data were reported using proportions, normal distribution of numerical data was reported as means, and non-normal distribution of numerical data was reported as medians. Bivariate analysis was performed to compare the data from the outbreak and non-outbreak periods. The statistical significance of categorical data was determined using the chi-square test, two independent samples with normal distribution were analysed using the Student's t-test, and two independent samples with non-normal distribution were analysed using the Mann-Whitney U test. Bivariate associations were considered statistically significant at p < 0.05.
Multivariate analysis was performed using logistic regression analysis. All potential confounders were incorporated into the causal model. Interaction terms were considered between ED LOS and the outbreak period because the limitation of the isolation ward during the early outbreak period caused prolonged stay of patients in the ED while patients waited for the availability of hospital isolation rooms. The adjusted odds ratio (OR) was used to indicate the association between admissions during the outbreak period and mortality. Data analysis was performed using SPSS version 16.1.
3. Results
All eligible patients with complete information regarding the study were included as study participants (Fig. 2), resulting in 2,808 participants in the outbreak period and 2,423 in the non-outbreak period. Demographic data are presented in Table 1 . The total number of participants was higher during the outbreak. The mean age, proportion of men, trauma cases, and in-hospital mortality were not significantly different between the participants admitted during the outbreak and non-outbreak periods.
Table 1.
Comparison of the basic variables between the outbreak and non-outbreak periods.
| Variables | Outbreak (%) | Non-outbreak (%) | P |
|---|---|---|---|
| Total cases | 2808 | 2423 | <0.01a |
| Mean Age (SD) | 37.7 (21.3) | 36.9 (22.5) | 0.17b |
| Male (%) | 1333 (47.5) | 1163 (48) | 0.72a |
| Triage categories | |||
| Resuscitation (%) | 608(21.7) | 518(21.4) | <0.01a |
| Urgent (%) | 1854 (66) | 1835 (75.7) | |
| Non-urgent (%) | 346 (12.3) | 70 (2.9) | |
| Trauma cases (%) | 251 (8.9) | 214 (8.8) | 0.89a |
| Referral cases (%) | 331 (11.8) | 525 (21.7) | <0.01a |
| Median ED LOS in minutes (IQR) | 815 (Q1 = 484; Q3 = 1364) | 738 (Q1 = 454; Q3 = 1172) | <0.01c |
| ED LOS ≥8 h | 2113 (75.2) | 1787 (73.7) | 0.20a |
| In-hospital mortality | 439(15.6) | 396(16.3) | 0.49a |
COVID-19, Corona Virus Disease-19, ED, emergency department; IQR, interquartile range; LOS, length of stay; SD, standard deviation.
chi-square test.
Student t-test.
Mann–Whitney U test.
The proportion of urgent triage was lower during the outbreak period than that during the non-outbreak period (66% vs. 75.7%), and the proportion of non-urgent triage was higher during the outbreak period (12.3% vs. 2.9%). The proportion of referral cases was lower in the non-outbreak period (11.8% vs. 21.7%) and the median ED LOS was higher during the outbreak period (815 min vs. 738 min).
Bivariate analysis between admission during the outbreak period and in-hospital mortality (Model 1) showed a non-significant association (OR, 0.94; 95%CI 0.82–1.10) (Table 2 ). Model 2 is a well-formulated hierarchical model. The referral case was considered an exploratory variable and was further excluded from the multivariate analysis because it showed no OR changes in Model 3.
Table 2.
The association between the outbreak period of COVID-19 and ED mortality.
| Variables | Model 1 (crude) |
Model 2 |
Model 3 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95%CI | P | OR | 95%CI | P | OR | 95%CI | P | |
| Outbreak period | |||||||||
| No (reference) | 1 | 1 | 1 | ||||||
| Yes | 0.94 | 0.82–1.10 | 0.47 | 1.39 | 1.03–1.89 | 0.03 | 1.41 | 1.04–1.91 | 0.01 |
| Age (years) | – | 1.01 | 1.01–1.02 | <0.01 | 1.01 | 1.0–1.01 | <0.01 | ||
| Sex | |||||||||
| Female (reference) | 1 | 1 | |||||||
| Male | – | 1.20 | 1.02–1.41 | 0.02 | 1.20 | 1.02–1.41 | 0.03 | ||
| Triage categories | |||||||||
| Non-urgent (reference) | 1 | 1 | |||||||
| Urgent | – | 5.06 | 2.73–9.36 | <0.01 | 5.04 | 2.72–9.32 | <0.01 | ||
| Resuscitation | – | 23.92 | 12.87–44.45 | <0.01 | 23.72 | 12.77–44.05 | <0.01 | ||
| Trauma cases | |||||||||
| No (reference) | 1 | 1 | |||||||
| Yes | – | 0.26 | 0.17–0.38 | <0.01 | 0.25 | 0.17–0.38 | <0.01 | ||
| Referral cases | |||||||||
| No (reference) | 1 | ||||||||
| Yes | – | 0.94 | 0.76–1.16 | 0.57 | – | – | – | ||
| ED LOS | |||||||||
| <8 h (reference) | 1 | 1 | |||||||
| ≥8 h | – | 1.01 | 0.78–1.31 | 0.03 | 1.01 | 0.78–1.31 | 0.91 | ||
| Outbreak period*ED LOS ≥8 h | – | 0.64 | 0.45–0.91 | 0.01 | 0.64 | 0.44–0.90 | 0.01 | ||
| Intercept | – | 0.015 | 0.01 | ||||||
OR, odds ratio; CI, confidence interval; ED, emergency department; LOS, length of stay.
Model 3 was the final model that included all important confounders and modifiers. The odds of in-hospital mortality increased during the outbreak period compared to the non-outbreak period (OR 1.41; 95%CI 1.04–1.91; p = 0.01) after adjusting for age, sex, triage categories, trauma case, ED LOS, and interaction between outbreak period and ED LOS (Hosmer–Lemeshow test <0.01; area under the curve 0.75; 95% CI 0.73–0.77).
Age and prolonged ED LOS in Model 3 had a non-significant effect on in-hospital mortality during the COVID-19 outbreak. There were higher odds of in-hospital mortality in males than in females(OR 1.2; 95%CI 1.02–1.41) and in the urgent triage (OR 5.04; 95%CI 2.72–9.32) and resuscitation categories (OR 23.72; 95%CI 12.77–44.05) than in the non-urgent triage category.
In Model 3, trauma cases and the interaction between ED attendance during the outbreak period and prolonged ED LOS showed a protective effect on in-hospital mortality (OR 0.25; 95%CI 0.17–0.38 and OR 0.64; 95%CI 0.44–0.90, respectively).
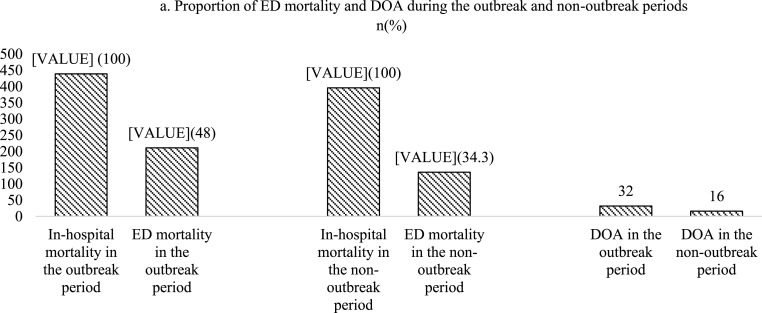
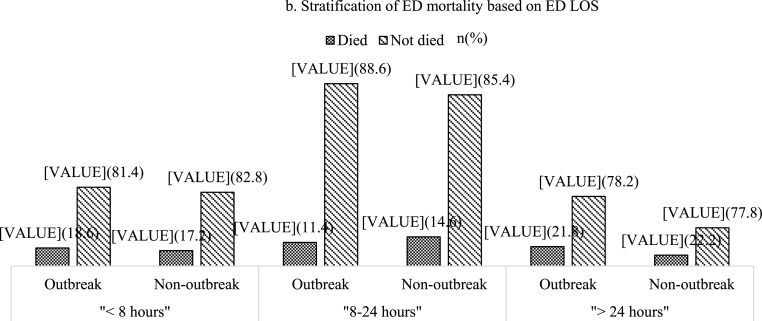
Subgroup analysis of in-hospital mortality showed that ED mortality and death on arrival were higher during the COVID-19 outbreak than during the non-outbreak period (Fig. 3 a). Further stratification of ED LOS (<8 h, 8–24 h, and >24 h) showed consistent results; ED mortality was higher among participants who stayed in the ED for more than 24 h during the outbreak period than among those who stayed in the ED for more than 24 h in the non-outbreak period (Fig. 3b).
Fig. 3.
Subgroup analysis on ED mortality during the outbreak and non-outbreak periods
a. Proportion of ED mortality and DOA during the outbreak and non-outbreak periods
b Stratification of ED mortality based on ED LOS
ED, emergency department; DOA, death on arrival.
Table 3 shows the subgroups of participants admitted due to COVID-19-related conditions (suspected or confirmed cases of COVID-19) during the outbreak period who needed inpatient care (n = 418 patients). Most participants were female (57.9%) and adults (age >18–59 years, 68.2%) and belonged to the non-urgent triage category (42.8%). Half of the participants (51.4%) had an ED LOS ≥8 h, and the in-hospital mortality of all COVID-19 related cases was 16%. There were 53 confirmed COVID-19 cases (12.6%) and the COVID-19-specific mortality rate was 22.6%.
Table 3.
COVID-19-related cases during the outbreak period (n = 418).
| Variables | N(%) |
|---|---|
| Female | 242 (57.9) |
| Male | 176 (42.1) |
| Age groups | |
| <1 years | 10 (2.4) |
| 1–5 years | 27 (6.5) |
| >5–18 years | 17 (4.1) |
| >18–59 years | 285 (68.2) |
| ≥60 years | 79 (18.9) |
| Triage categories | |
| Non-urgent | 179 (42.8) |
| Urgent | 145 (34.7) |
| Resuscitation | 94 (22.5) |
| Trauma cases | 1 (0.2) |
| Referral cases | 24 (5.7) |
| ED LOS ≥8 h | 215 (51.4) |
| In-hospital mortality | 67 (16) |
| Confirmed cases of COVID-19 | 53 (12.6) |
| COVID-19-specific mortality rate | 12 (22.6) |
COVID-19, Coronavirus disease; ED, Emergency Department; LOS, length of stay.
4. Discussion
The association between outbreak period and in-hospital mortality showed different results in bivariate (OR 0.94. p = 0.47; 95%CI 0.82–1.10) and multivariate analyses (adjusted OR 1.4, p < 0.01; 95% CI 1.04–1.9). It shows the contribution of demographic variables (age and sex) and ED-based variables (triage category and ED LOS) to the risk of mortality.
The increased risk of in-hospital mortality during the early COVID-19 period in Jakarta, Indonesia, was consistent with reports of increased overall mortality in the same period in Jakarta compared to the previous year (8,695 in March–April 2020 vs. 5,853 in March–April 2019).19 The internal consistency of the result was supported by the report of increased DOA in the ED during the outbreak period (Fig. 3a), and similar conditions were reported during the Severe Acute Respiratory Syndrome (SARS) outbreak in Hong Kong and Taiwan.20 , 21
The absolute number of in-hospital mortality during the outbreak (n = 439) was higher than during the non-outbreak (n = 396) period (Table 1) meanwhile, mortalities related to confirmed cases of COVID-19 in March to April 2020 were only 12. Higher overall in-hospital mortality during the COVID-19 outbreak compared to the previous year implied that the outbreak produced collateral damage to patients without COVID-19.22 , 23
In the multivariate model, although the triage categories had very wide confidence intervals, the increased risk of mortality in participants with higher acuity (resuscitation and urgent triage categories) showed a consistent pattern. A plausible explanation is that participants with higher triage acuity (resuscitation category) had the most critical condition, and the risk of mortality became more pronounced.15
Many studies have reported that prolonged ED LOS was associated with higher risks of non-optimal medication and mortality,24 but our study showed no increase in the odds of in-hospital mortality among participants with prolonged ED LOS (adjusted OR 1.01; 95%CI 0.78–1.31). This could be because even though the median time of ED LOS was longer during the outbreak period, there was no difference between the proportions of prolonged ED LOS during the outbreak period and that during the non-outbreak period (Table 1). More than 70% of participants in the ED who needed inpatient care had an ED LOS ≥8 h in both groups; nevertheless, ED mortality of participants who stayed for more than 24 h in the ED was higher during the outbreak period (Fig. 3b).
A multicentre study in the ED across the United States reported that consistent conditions related to prolonged ED LOS were significantly higher during the COVID-19 outbreak period than during the pre-outbreak period.25
Table 1 shows a higher proportion of participants in the non-urgent triage category during the outbreak period (12.3%) and sub-group participants in COVID-19 related conditions (Table 3) also showed the highest proportion in the non-urgent triage categories (42.8%), implying that during the early outbreak, there were limitations in managing suspected COVID-19 cases with mild symptoms in the outpatient unit or primary care system; thus, many patients with mild symptoms of suspected COVID-19 sought medical attention in the ED, which could lead to an increased risk of ED overcrowding and nosocomial infection.26 This contradicts reports in South Korea wherein during the COVID-19 outbreak period the ED experienced a higher number of patient visits with emergent and urgent triage.27
In the first two months of the COVID-19 outbreak, our hospital laboratory had a limited capacity for RT-PCR testing. All nasopharyngeal swab samples were sent to other out-of-hospital laboratories, which required more than a week to obtain the test results after the samples were sent. This delay contributed to a prolonged occupation of the isolation room as RT-PCR (COVID-19 or non-COVID-19) results were pending, and many patients eventually were discharged home or died in the hospital with clinical diagnosis of suspected COVID-19, and the RT-PCR test results were available later. Similar conditions have been reported during the (Severe Acute Respiratory Syndrome) SARS and (Middle East Respiratory Syndrome) MERS outbreaks in Taiwan, Hong Kong, and South Korea.20 , 28 , 29
The proportion of positive RT-PCR test results for SARS-CoV-2 among participants in the ED who needed inpatient care at our institution was 12.9%; this was relatively higher than that reported in other countries during the initial outbreak. For example, California reported an ED positivity rate of 6.8%30 to 10.2%,31 and the ED positivity rate in Singapore was 3.8% of all cases with respiratory problems.32 The COVID-19-specific in-hospital mortality rate among confirmed cases of COVID-19 in our hospital was 22.6%, which was higher than the COVID-19-specific in-hospital mortality rate in Jakarta in the same period (12.9%).33
This study had good internal validity owing to its large sample size which increased the precision of the analysis, showed a clear temporal relationship, and had minimal loss to follow-up of eligible patients (less than 10%) in the outbreak and non-outbreak groups. Since this was a single-centre study, the generalisability is limited to other typical hospitals in Jakarta and other cities in Indonesia (referral hospitals).
5. Limitation
Confirmed cases of COVID-19 could be a potential confounder that cannot be elaborated upon in the analysis owing to the limited testing capability of our institution. We only included confounder variables from patient demographics and ED factors without incorporating any variables from other service areas in the hospital (inpatient ward or intensive care unit). Thus, although the model was able to measure the effect of the main independent variable on the outcome, we should not use the model for prediction purposes.
Hospital mortality was determined by checking administrative reports of patient outcomes from the medical records, which did not provide accurate information about the cause of death.
The description of emergency services in this study may be different from that in other countries owing to differences in healthcare systems and strategies implemented by their respective governments for the COVID-19 outbreak.
Future research related to collateral damage of the COVID-19 outbreak in hospital services should evaluate different outcomes in COVID-19 and non-COVID-19 patients, such as hospital length of stay, ICU admission, intubation rate, and duration of mechanical ventilation.
6. Conclusion
Outbreaks of COVID-19 have been associated with an increased risk of in-hospital mortality in referral hospitals in Jakarta, Indonesia. Male sex and higher triage acuity contributed to the higher odds of mortality. During the initial period of the COVID-19 outbreak, every hospital urgently needed to simultaneously manage patients with and without COVID-19 to reduce in-hospital mortality.
Authorship
Hadiki Habib: Conceptualisation, methodology, software, and formal analysis. Yogi Prabowo: Conceptualisation and supervision. Muharris Mulyana: Writing, reviewing, and editing. Septo Sulistio and Imamul Aziz Albar: investigation, validation, and data curation.
Source of funding
This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Ethics approval statement
This study was approved by the Ethical Committee of Cipto Mangukusumo Hospital/Faculty of Medicine Universitas Indonesia (protocol number 20-06-0700).
Declaration of competing interest
The authors declare no conflicts of interest.
Acknowledgments
We acknowledge the staff of the Emergency Department and Kiara Ultimate COVID-19 Service Centre of Dr. Cipto Mangunkusumo Hospital, Jakarta, Indonesia. We also acknowledge the data management teams Friska Putri Amalia, Indah, and Rasmawati.
We would like to thank Elsevier Languange Editing Services for English languange editing.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.cegh.2023.101219.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Arifin D. Presiden tetapkan Covid-19 sebagai bencana nasional. Badan Nasional Penanggulangan Bencana (BNPB) 2020 https://bnpb.go.id/berita [cited 2020 May, 25]; Available from URL. [Google Scholar]
- 2.World Health Organization WHO timeline - COVID-19. 2020. https://www.who.int/news-room/detail/27-04-2020-who-timeline–-covid-19 [cited 2020 June, 16th]: Available from URL.
- 3.Tim Komunikasi Publik Gugus Tugas Nasional . 2020. Kasus Positif COVID-19 Melesat Naik 1.241, Total 34.316.https://covid19.go.id/p/berita/kasus-positif-covid-19-melesat-naik-1241-total-34316 [cited 2020 June 10th]: Available from URL. [Google Scholar]
- 4.Satuan tugas Penanganan Covid-19. Peta Sebaran. 2020 https://covid19.go.id/ [cited 2020 October,12]: Available from URL. [Google Scholar]
- 5.Dki Jakarta Pemprov. Jakarta Tanggap Corona. 2020. https://corona.jakarta.go.id/id [cited 2020 October,12]: Available from URL.
- 6.Castoldi L., Solbiati M., Costantino G., Casiraghi E. Variations in volume of emergency surgeries and emergency department access at a third level hospital in Milan, Lombardy, uring the COVID-19 outbreak. BMC Emerg Med. 2021;21:1–9. doi: 10.1186/s12873-021-00445-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Souza J.L., Jr., Teich V.D., Dantas A.C.B., et al. Impact of the COVID-19 pandemic on emergency department visits: experience of a Brazilian reference center. Einstein (Sao Paulo). 2021;19:1–5. doi: 10.31744/einstein_journal/2021AO6467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hartnett K.P., Kite-Powell A., al DJe. Impact of the COVID-19 pandemic on emergency department visits — United States. 2020 MMWR Morb Mortal Wkly Rep. 2020;69:699–704. doi: 10.15585/mmwr.mm6923e1. January1, 2019–May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wongtanasarasin W., Srisawang T., Yothiya W., Phinyo P. Impact of national lockdown towards emergency department visits and admission rates during the Covid-19 pandemic in Thailand: a Hospital-Based Study. Emerg Med Australas. 2021;33:316–323. doi: 10.1111/1742-6723.13666. [DOI] [PubMed] [Google Scholar]
- 10.Menteri Kesehatan Republik Indonesia . 2020. Keputusan Menteri Kesehatan Republik Indonesia Nomor HK.01.07/Menkes/169/2020 Tentang Penetapan Rumah Sakit Rujukan Penanggulangan Penyakit Infeksi Emerging Tertentu; pp. 1–19. [Google Scholar]
- 11.Tan R.M.R., Ong G.Y., Chong S.L., Ganapathy S., Tyebally A., Lee K.P. Dynamic adaptation to COVID-19 in a Singapore paediatric emergency department. Emerg Med J. 2020;37:252–254. doi: 10.1136/emermed-2020-209634. [DOI] [PubMed] [Google Scholar]
- 12.Abad C.L., Lansang M.A.D., Cordero C.P., et al. Early experience with COVID-19 patients in a private tertiary hospital in the Philippines: implications on surge capacity, healthcare systems response, and clinical care. Clin Epidemiol Glob Health. 2021;10:100695. doi: 10.1016/j.cegh.2020.100695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Firdaus F. Indonesian screening may be missing virus carriers. 2020. https://foreignpolicy.com/category/analysis/argument/?_ga=.13618807.1914361107.1602557616-1481208809.1602557616 [cited 2020, October 12]: Available from URL.
- 14.Firdaus F., Ratcliffe R. Indonesia's hidden coronavirus cases threaten to overwhelm hospitals. 2020. https://www.theguardian.com/global-development/global-development [cited 2020 October 12]: Available from URL.
- 15.Habib H., Sulistio S., Albar I.A., Mulyana R.M. N Y. Validation of the Cipto triage method: a single-centre study from Indonesia. Open Access Emerg Med. 2020;12:137–143. doi: 10.2147/OAEM.S246598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Utama Rsupn dr Direktur. Cipto Mangunkusumo. Keputusan Direktur Utama RSUP nasional dr. Cipto Mangunkusumo No: HK.01.07/3.3/12068/2019 Tentang Kapasitas Tempat Tidur RSUPN dr. Cipto Mangunkusumo. 2019;2019:1–7. [Google Scholar]
- 17.von Elm E., Altman D.G., Egger M., et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–808. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Direktorat Jenderal Pencegahan dan Pengendalian Penyakit Pedoman Pencegahan dan Pengendalian coronavirus disease-19 (Covid-19) Kementerian Kesehatan Republik Indonesia. 2020:3–136. [Google Scholar]
- 19.Taufan S.A. Baru September, jumlah penguburan jenazah COVID-19 DKI sudah lewati 2019. JawaPos.com. 2020 https://www.jawapos.com/jabodetabek/12/09/2020/baru-september-jumlah-penguburan-jenazah-di-dki-sudah-lewati-2019/ [Cited 2020 October 12] Available from URL. [Google Scholar]
- 20.Chen T.A., Lai K.H., Chang H.T. Impact of a severe acute respiratory syndrome outbreak in the emergency department: an experience in Taiwan. Emerg Med J. 2004;21:660–662. doi: 10.1136/emj.2003.010678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Man C.Y., Yeung R.S., Chung J.Y., Cameron P.A. Impact of SARS on an emergency department in Hong Kong. Emerg Med. 2003;15:418–422. doi: 10.1046/j.1442-2026.2003.00495.x. [DOI] [PubMed] [Google Scholar]
- 22.Feral-Pierssens A.L., Claret P.G., Chouihed T. Collateral damage of the COVID-19 outbreak: expression of concern. Eur J Emerg Med. 2020;4:233–234. doi: 10.1097/MEJ.0000000000000717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Santi L., Golinelli D., Tampieri A., et al. Non-COVID-19 patients in times of pandemic: emergency departments visits, hospitalizations and cause-specific mortality in Northern Italy. PLoS One. 2021;16 doi: 10.1371/journal.pone.0248995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Boudi Z., Lauque D., Alsabri M., et al. Association between boarding in the emergency department and in-hospital mortality: a systematic review. PLoS One. 2020;15 doi: 10.1371/journal.pone.0231253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lucero A., Sokol K., Hyun J., et al. Worsening of emergency department length of stay during the COVID-19 pandemic. J Am Coll Emerg Physicians Open. 2021;2 doi: 10.1002/emp2.12489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ceccarelli G., Spagnolello O., Borrazzo C., et al. Impact of the 2017 measles outbreak on the emergency care system of a large tertiary-care teaching hospital in Italy: a retrospective analysis. Eur J Publ Health. 2019;29:966–971. doi: 10.1093/eurpub/ckz056. [DOI] [PubMed] [Google Scholar]
- 27.Kim Y.S., Kim I.B., Kim S.R., Cho B.J. Changes in emergency department case severity and length of stay before and after COVID-19 outbreak in Korea. Healthcare (Basel). 2022;10:1540. doi: 10.3390/healthcare10081540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Boutis K., Stephens D., Lam K., Ungar W.J., Schuh S. The impact of SARS on a tertiary care pediatric emergency department. CMAJ. 2004;171:1353–1358. doi: 10.1503/cmaj.1031257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paek S.H., Kim D.K., Lee J.H., Kwak Y.H. The impact of Middle East respiratory syndrome outbreak on trends in emergency department Utilization patterns. J Kor Med Sci. 2017;32:1576–1580. doi: 10.3346/jkms.2017.32.10.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Duanmu Y., Brown I.P., Gibb W.R., et al. Characteristics of emergency department patients with COVID-19 at a single site in Northern California: clinical observations and public health implications. Acad Emerg Med. 2020;27:505–509. doi: 10.1111/acem.14003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tolia V.M., Chan T.C., Castillo E.M. Preliminary results of initial testing for coronavirus (COVID-19) in the emergency department. West J Emerg Med. 2020;21:503–506. doi: 10.5811/westjem.2020.3.47348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wee L.E., Fua T.P., Chua Y.Y., et al. Containing COVID-19 in the emergency department: the role of improved case detection and segregation of suspect cases. Acad Emerg Med. 2020;27:379–387. doi: 10.1111/acem.13984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Surendra H., Elyazar I.R.F., DJaafara B.A., et al. Clinical characteristics and mortality associated with COVID-19 in Jakarta, Indonesia : a hospital-based retrospective cohort study. The Lancet Regional Health-Western Pacific. 2021;9:100108. doi: 10.1016/j.lanwpc.2021.100108. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.