Abstract
Background
Electronic health record datasets have been used to determine the prevalence of musculoskeletal complaints in general practice but not to examine the associated characteristics and healthcare utilisation at the primary care level.
Aim
To describe the prevalence and characteristics of patients presenting to general practitioners with musculoskeletal complaints.
Design and setting
A five-year analysis within three Primary Health Networks (PHNs) in Victoria, Australia.
Method
We included patients with at least one face-to-face consultation 2014 to 2018 inclusive and a low back (≥ 18 years), and/or neck, shoulder or knee (≥ 45 years) complaint determined by SNOMED codes derived from diagnostic text within the medical record. We determined prevalence, socio-demographic characteristics and diagnostic codes for patients with an eligible diagnosis; and number of consultations within one year of diagnosis.
Results
324,793/1,294,021 (25%) presented with at least one musculoskeletal diagnosis, of whom 41% (n = 133,279) fulfilled our inclusion criteria. There were slightly more females (n = 73,428, 55%), two-thirds (n = 88,043) were of working age (18–64 years) and 83,816 (63%) had at least one comorbidity. Over half had a low back diagnosis (n = 76,504, 57%) followed by knee (n = 33,438, 25%), shoulder (n = 26,335, 20%) and neck (n = 14,492, 11%). Most codes included ‘pain’ and/or ‘ache’ (low back: 58%, neck: 41%, shoulder: 32%, knee 26%). Median (IQR) all-cause consultations per patient within one year of diagnosis was 7 (4–12).
Conclusion
The burden of MSK complaints at the primary care level is high as evidenced by the prevalence of people with musculoskeletal complaints presenting to a general practitioner, the preponderance of comorbidities and the numerous consultations per year. Identification and evaluation of strategies to reduce this burden are needed.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12875-023-01976-z.
Keywords: General practice, Low back pain, Shoulder pain, Knee pain, Neck pain, Big data
Background
General practitioners (GPs) are usually the first point of contact with the health care system in developed countries and provide ongoing care for many conditions. In 2017–18, 86% of the Australian population reported visiting their GP multiple times a year [1]. Musculoskeletal problems such as osteoarthritis and back pain are one of the most common reasons for seeking care from a GP [2], with estimates of one in five consultations being for a musculoskeletal complaint [3, 4].
Electronic health records from general practices can be a rich and efficient source of data. Using routinely collected data for research has the potential to improve health outcomes [5]. For example, these data can be used to examine patterns of care to identify where improvements are needed and then to evaluate whether interventions designed to improve care have the desired effect. General practice databases extract and deidentify patient-related information from every GP/patient encounter directly from the electronic medical records of consenting practices. They have been used internationally to examine patterns of care for various conditions including respiratory tract infection, [6] cardiovascular disease [7], chronic hepatitis C [8], chronic kidney disease [9], and diabetes [10–12].
General practice databases have been used to determine the prevalence of some musculoskeletal complaints including arthritis, chronic back pain, gout, osteoporosis, spondyloarthropathies and rheumatoid arthritis in various countries [13–17]. Trends and trajectories of opioid prescription for people with general musculoskeletal conditions, [18, 19] use of osteoporosis medicines in people with osteoporosis [16] and use of biologic drugs in people with psoriatic arthritis and ankylosing spondylitis [20] have also been examined. However, to date the characteristics of patients presenting to general practice with musculoskeletal complaints and the healthcare utilisation at the primary care level has not been comprehensively examined using primary care databases.
This study forms part of a larger project that is using data from the POpulation Level Analysis and Reporting (POLAR) dataset from 2014 to 2018 inclusive to examine patterns of care provided by GPs for people with musculoskeletal complaints [21]. In this paper we describe the prevalence of people with any musculoskeletal complaint and those of the low back, neck, shoulder and knee specifically, and the characteristics of patients who present to GPs with these complaints over a five-year period. We also describe the diagnostic codes and the number of all-cause GP consultations within one year following diagnosis.
Methods
Study design and setting
The protocol including a detailed description of the data source, setting, eligibility criteria and diagnostic codes used to identify eligible patients for this study, has been published previously [21]. In brief, this is an analysis of general practice care for patients with musculoskeletal complaints using routinely collected data from the POLAR database. This database contains deidentified patient-related data from electronic medical records of consenting general practices within three PHNs in Victoria, Australia. PHNs are independent organisations funded by the Australian Government to improve patient care by GPs and coordination of care within specific geographic boundaries. At the time of extract, 301 general practices had consented, representing approximately 30% of all general practices within the three participating PHNs. The study population consists of the adult patients attending these practices. Most patients in Australia usually attend the same practice and see the same GP within the practice [22]. In the POLAR database an ‘activity’ occurs anytime a patient record is accessed regardless of whether this was for clinical or administrative purposes. To ensure the ‘activity’ was for a clinical purpose, we restricted the underlying population to adult patients (aged 18 years and over) who had received at least one face-to-face GP consultation between 1/01/2014 and 31/12/2018.
Participants
We included patients with a low back (≥ 18 years), and/or neck, shoulder or knee complaint (≥ 45 years). Our age criteria were chosen because the prevalence of most musculoskeletal conditions increases markedly after the age of 45 except for low back pain which increases after 18 years [23]. We excluded traumatic diagnoses and other conditions typically primarily managed by a specialist (e.g. inflammatory and autoimmune rheumatic diseases). In Australia, coding is not embedded in the clinical process and needs to be conducted specifically for research purposes. Patients with an eligible musculoskeletal complaint were therefore selected using Outcome Health’s coding of diagnoses according to SNOMED CT-AU terminology, [24] a standardised method for recording medical terms. Clinical natural language processing is used to code narrative text written by GPs within the diagnostic field of the electronic medical record as SNOMED CT-AU terminology. For example, this allowed free-text items such as ‘back pain’, ‘lumbar ache’ and ‘low back pain’ to all sit under the same diagnostic code. Clinical natural language processing conducted by Outcome Health has previously demonstrated accurate coding of over 95% of the narrative text to SNOMED CT-AU terms in a sample of approximately 57,000 diagnosis records [25]. Since every complaint documented within the diagnostic field of the electronic record by a GP will be coded, there can be multiple diagnostic codes entered at the same time. Diagnoses provided by specialists and then documented by a GP will also be coded.
Variables
The patient-related variables extracted for this study included deidentified patient ID, year of birth, gender, postcode of residence, Statistical Area Level 3 (SA3) of residence [26], date and SNOMED-CT-AU diagnostic codes of eligible musculoskeletal complaint(s), presence of comorbidities and dates of GP consultations on or after the date of first eligible diagnosis until 31/12/2018. A list of eligible diagnostic codes and comorbidities is available from https://clinicalcodes.rss.mhs.man.ac.uk/medcodes/article/174/. Eligible comorbidities included chronic cardiovascular disease, chronic obstructive pulmonary disease, chronic musculoskeletal conditions, cancer, dementia, diabetes, depression/anxiety and obesity that had been present for at least six months prior to the index musculoskeletal complaint [21]. Deidentified practice ID and PHN were also extracted.
Data analysis
Relevant data were extracted from the POLAR SQL database and imported into Stata V.15 (StataCorp LLC, College Station, TX, USA). Relational data files were systematically merged using patient and practice IDs to select the study cohort. The prevalence of patients with any type of musculoskeletal complaint was calculated as well as those meeting our inclusion criteria. This was the proportion of patients with an eligible age and at least one musculoskeletal diagnostic code out of those with a face-to-face GP consultation during 2014 to 2018 inclusive. The number (%) of patients, general practices and GPs within each PHN was reported.
Socio-demographic characteristics and comorbidities of eligible patients categorised by body region of musculoskeletal complaint included age, gender, residential remoteness according to the Australian Statistical Geography Standard [26], and socio-economic status according to the Index of Relative Socioeconomic Advantage and Disadvantage [27]. Number and type of clinical diagnoses per patient were described according to body region(s) affected and specific SNOMED-CT-AU diagnostic codes. Follow-up period [median (interquartile range (IQR))] and number of all-cause consultations per patient [median (IQR)] within one year of diagnosis were also reported. Median (IQR) were reported as the data were positively skewed. For patients with more than one eligible diagnosis, these data were calculated from the first eligible diagnosis musculoskeletal diagnosis or ‘index’ diagnosis within the study period.
Results
Description of study cohort
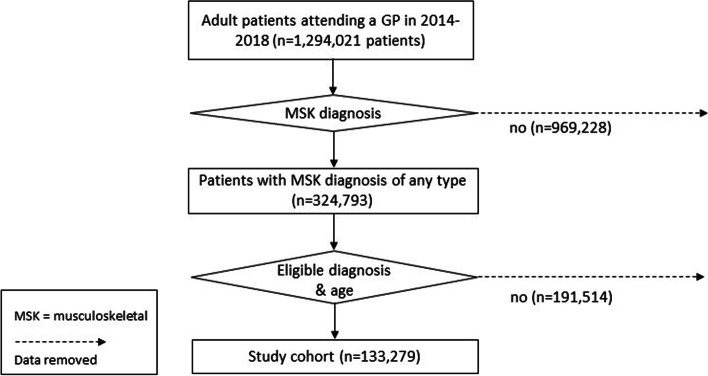
Selection of the study cohort from the POLAR dataset is presented in Fig. 1. Twenty-five percent (324,793/1,294,021) of adult patients with a face-to-face consultation with a GP during the study period were diagnosed with a musculoskeletal complaint of any type. Of these, 133,279 (41% or 10% of the underlying population) were of eligible age and had a musculoskeletal complaint that fulfilled our inclusion criteria (low back, neck, shoulder and/or knee complaint). 969,228 (75%) patients with a face-to-face consultation and diagnosis did not have a musculoskeletal diagnosis of any type and a further 191,514 (59%) patients with eligible musculoskeletal complaints were outside the age criteria for inclusion.
Fig. 1.
Study cohort flowchart
The included cohort of patients attended 4,538 GPs and 269 general practices (Table 1). The distribution of patients, GPs and general practices within each PHN were approximately proportional. Approximately 50% of patients, GPs and general practices were from Eastern Melbourne PHN, 40% were from South Eastern Melbourne PHN and 10% were from Gippsland PHN. These proportions are also similar to those of the general population living within these areas. Mean (SD) age of the study cohort at index diagnosis was 49.2 (18.5) years for those with low back complaints and 61.9 (12.0), 62.8 (11.8) and 64.2 (11.5) years for those with neck, shoulder and knee complaints respectively. These differences reflect our eligibility criteria where we restricted those with low back complaints to 18 years and over but those with neck, shoulder and knee complaints were restricted to 45 years and over. Fifty-five percent of our cohort were female, 87% lived in a metropolitan location and 11% lived in an area of greatest socioeconomic disadvantage (Table 2). The majority (66%) were of working age (18–64 years) with progressively fewer patients in each 10-year age bracket over 65 years (18.4% 65–74 years, 11.2% 75–84 years and 4.3% 85 years and over). Nearly two thirds (63%) had at least one comorbidity, most commonly cardiovascular (33%), musculoskeletal (27%), and/or depression/anxiety (25%). Median (IQR) follow-up was 2.3 (1–3.7) years.
Table 1.
Number (proportion) of patients, practices and general practitioners by primary health network
| Study cohort | |||
|---|---|---|---|
| Patients, n (%) | GPs, n (%) | Practices, n (%) | |
| Eastern Melbourne PHN | 69,467 (52.1) | 2,277 (50.2) | 139 (51.7) |
| South-Eastern Melbourne PHN | 53,149 (39.9) | 1,561 (34.4) | 106 (39.4) |
| Gippsland PHN | 10,663 (8.0) | 700 (15.4) | 24 (8.9) |
| Total | 133,279 (100) | 4,538 (100) | 269 (100) |
GP General practitioner, PHN Primary health network
Table 2.
Characteristics of study cohort
| Study population# n | Total study cohort n (%) | Low back* n (%) | Neck* n (%) | Shoulder* n (%) | Knee* n (%) | Multi-site^ n (%) | |
|---|---|---|---|---|---|---|---|
| Patients | 1,294,021 | 133,279 (100) | 65,612 (49.2) | 8,974 (6.7) | 18,253 (13.7) | 25,264 (19.0) | 15,176 (11.4) |
| Age at diagnosis in years | |||||||
| 18–44 | 694,705 (53.7) | 30,139 (22.6) | 29,977 (45.7) | N/A | N/A | N/A | 162 (1.07) |
| 45–54 | 192,397 (14.9) | 29,215 (21.9) | 11,153 (17.0) | 3,025 (33.7) | 5,345 (29.3) | 5,900 (23.4) | 3,792 (25.0) |
| 55–64 | 170,122 (13.1) | 28,689 (21.6) | 9,313 (14.2) | 2,492 (27.8) | 5,328 (29.2) | 7,312 (28.9) | 4,244 (28.0) |
| 65–74 | 130,085 (10.1) | 24,563 (18.4) | 7,554 (11.5) | 1,913 (21.3) | 4,269 (23.4) | 7,014 (27.8) | 3,813 (25.1) |
| 75–84 | 72,814 (5.6) | 14,947 (11.2) | 5,165 (7.9) | 1,127 (12.6) | 2,398 (13.1) | 3,841 (15.2) | 2,416 (15.9) |
| 85 + | 33,898 (2.6) | 5,726 (4.3) | 2,450 (3.7) | 417 (4.6) | 913 (5.0) | 1,197 (4.7) | 749 (4.9) |
| Gender | |||||||
| Male | 554,598 (42.9) | 59,692 (44.8) | 30,513 (46.5) | 3,670 (40.9) | 8,170 (44.8) | 11,124 (44.0) | 6,215 (41.0) |
| Female | 734,789 (56.8) | 73,460 (55.1) | 35,009 (53.4) | 5,297 (59.0) | 10,075 (55.2) | 14,121 (55.9) | 8,958 (59.0) |
| (Missing) | 4,634 (0.4) | 127 (0.1) | 90 (0.1) | 7 (0.1) | 8 (0.04) | 19 (0.08) | 3 (0.02) |
| Remoteness | |||||||
| Metropolitan | 1,143,398 (88.4) | 116,064 (87.1) | 57,253 (87.3) | 7,883 (87.8) | 15,920 (87.2) | 21,690 (85.9) | 13,318 (87.8) |
| Inner regional | 123,801 (9.6) | 14,256 (10.7) | 7,048 (10.7) | 885 (9.9) | 1,906 (10.4) | 2,840 (11.2) | 1,577 (10.4) |
| Outer regional | 20,024 (1.5) | 2,507 (1.9) | 1,072 (1.7) | 180 (2.0) | 373 (2.0) | 646 (2.6) | 236 (1.6) |
| Remote | 666 (0.05) | 53 (0.04) | 22 (0.03) | 5 (0.06) | 5 (0.03) | 14 (0.06) | 7 (0.05) |
| Very remote | 126 (<0.01) | 7 (<0.01) | 3 (<0.01) | 0 (0.0) | 1 (<0.01) | 2 (<0.01) | 1 (<0.01) |
| (Missing) | 6,006 (0.5) | 329 (0.3) | 214 (0.3) | 21 (0.2) | 48 (0.3) | 72 (0.3) | 37 (0.2) |
| Socioeconomic disadvantage | |||||||
| Quintile 1† | 122,617 (9.5) | 14,685 (11.0) | 7,826 (11.9) | 900 (10.0) | 1,700 (9.3) | 2,473 (9.8) | 1,786 (11.8) |
| Quintile 2 | 156,170 (12.1) | 18,196 (13.7) | 9,337 (14.2) | 1,052 (11.7) | 2,365 (13.0) | 3,403 (13.4) | 2,039 (13.4) |
| Quintile 3 | 195,170 (15.1) | 23,039 (17.3) | 11,156 (17.0) | 1,520 (17.0) | 3,240 (17.7) | 4,326 (17.1) | 2,797 (18.4) |
| Quintile 4 | 328,456 (25.4) | 34,167 (25.6) | 16,969 (25.9) | 2,198 (24.5) | 4,736 (25.9) | 6,358 (25.2) | 3,906 (25.7) |
| Quintile 5 | 484,662 (37.5) | 42,786 (32.1) | 20,102 (30.7) | 3,283 (36.6) | 6,161 (33.8) | 8,632 (34.2) | 4,608 (30.4) |
| (Missing) | 6,195 (0.5) | 406 (0.3) | 222 (0.3) | 21 (0.2) | 51 (0.3) | 72 (0.3) | 40 (0.3) |
| Comorbidity | |||||||
| At least 1 comorbidity | 480,951 (37.2) | 83,816 (62.9) | 36,178 (55.1) | 5,679 (63.3) | 11,916 (65.3) | 17,051 (67.5) | 12,992 (85.6) |
| Cancer | 29,582 (2.3) | 6,759 (5.1) | 2,401 (3.7) | 525 (5.9) | 1,193 (6.5) | 1,717 (6.8) | 923 (6.1) |
| Cardiovascular | 219,987 (17.0) | 43,628 (32.7) | 15,150 (23.1) | 3,219 (35.9) | 7,134 (39.1) | 10,656 (42.2) | 7,469 (49.2) |
| Dementia | 8,041 (0.6) | 1,188 (0.9) | 501 (0.8) | 79 (0.9) | 191 (1.1) | 256 (1.0) | 161 (1.1) |
| Depression/anxiety | 209,727 (16.2) | 33,422 (25.1) | 16,527 (25.2) | 2,264 (25.2) | 4,095 (22.4) | 5,164 (20.4) | 5,372 (35.4) |
| Diabetes | 75,465 (5.8) | 13,939 (10.5) | 4,947 (7.5) | 926 (10.3) | 2,522 (13.8) | 3,152 (12.5) | 2,392 (15.9) |
| Musculoskeletal | 101,101 (7.8) | 36,475 (27.4) | 15,438 (23.5) | 1,925 (21.5) | 4,300 (23.6) | 6,373 (25.2) | 8,439 (55.6) |
| Obesity | 38,475 (3.0) | 8,624 (6.5) | 3,756 (5.7) | 436 (4.9) | 991 (5.4) | 1,859 (7.4) | 1,582 (10.4) |
| Respiratory | 19,893 (1.5) | 4,927 (3.7) | 2,050 (3.1) | 399 (4.5) | 710 (3.9) | 859 (3.4) | 909 (6.0) |
| GP consultations during follow-up, n (% within 1 year of diagnosis) | 13,255,803 (42.7) | 2,295,769 (40.8) | 962,558 (43.9) | 142,937 (42.6) | 294,971 (42.0) | 407,309 (40.7) | 487,994 (33.5) |
| All-cause GP consultations per patient in 1st year post diagnosis, median (IQR) | 4 (2–8) | 7 (4–12) | 6 (3–12) | 7 (4–12) | 7 (4–12) | 7 (4–12) | 11 (6–17) |
| Age at diagnosis in years, mean (SD) | 45.0 (18.9) | 56.5 (17.0) | 49.2 (18.5) | 61.9 (12.0) | 62.8 (11.8) | 64.2 (11.5) | 63.9 (11.9) |
| Follow-up period in years, median (IQR) | 3.2 (1.6–4.6) | 2.3 (1.0–3.7) | 2.2 (1.0–3.6) | 2.1 (0.9–3.5) | 2.1 (1.0–3.5) | 2.2 (1.0–3.7) | 3.2 (1.9–4.2) |
All data presented as n (%) except where stated otherwise
# Study population includes adult patients (aged 18 years and over) who received at least one face-to-face consultation with a GP between 1/01/2014 and 31/12/2018
* Single body region affected by musculoskeletal complaint
^ Multiple body regions affected by an eligible musculoskeletal complaint
† A low score indicates relatively greater disadvantage
GP consultations
The study cohort had a total of 2,295,769 eligible consultations occurring on or after the index diagnosis date during the study period, of which 41% (n = 936,512) were within one year of the diagnosis being first recorded. There were a median (IQR) of seven (4–12) all-cause consultations per patient within one year of diagnosis compared to 4 (2–8) consultations per patient in the underlying study population of adult patients consulting a GP within the POLAR database (Table 2).
Nature of musculoskeletal complaint
Based upon eligible musculoskeletal diagnostic codes, over half of the cohort (n = 76,504, 57%) had a low back complaint, a quarter (n = 33,438, 25%) had a knee complaint, a fifth (n = 26,335, 20%) had a shoulder complaint, and 11% (n = 14,492) had a neck complaint (Fig. 2). Almost 90% (n = 118,103) had only a single body region complaint, proportionate to the overall body region breakdown (56% low back, 21% knee, 16% shoulder, 8% neck). The remainder had two (n = 13,049, 10%), three (n = 1,940, 1%) or four (n = 187, 0.1%) body region complaints. Of those with multiple body region complaints, the most common combinations were a low back and knee complaint (n = 4,984, 33%) and a low back and shoulder complaint (n = 4,563, 30%).
Fig. 2.
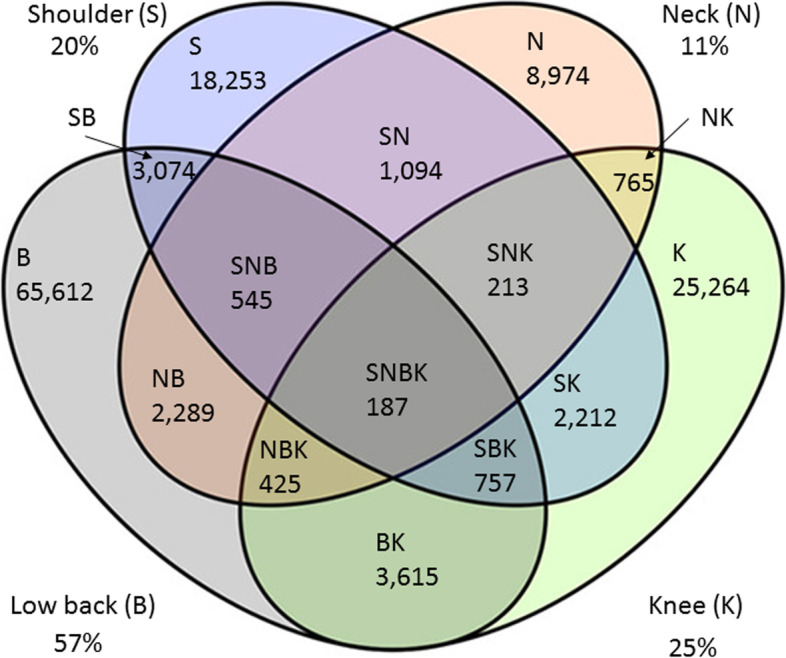
Number of patients by body region affected
Within each body region most patients (n = 97,216, 73%) had a complaint labelled with a single diagnostic code [median (IQR) 1 (1–1)], while 22,351 (17%) had two and 13,712 (10%) had three or more diagnoses. The most common diagnostic codes used for each body region are shown in Table 3 and those used in less 1% of diagnostic codes are provided in a supplementary file. There were 12 diagnostic codes used in at least 1% or more of diagnostic codes for low back complaints, 10 codes for neck complaints, 16 codes for shoulder complaints and 13 codes for knee complaints. Backache (46%) and low back pain (12%) were the most common diagnostic codes for low back complaints while neck pain (41%), shoulder pain (32%) and knee pain (26%) were the most common diagnostic codes for the other respective body regions.
Table 3.
Diagnostic codes (SNOMED CT-AU text) comprising at least 1% of all diagnoses for each body region
| Number (%) of patients labelled with each diagnostic code by body region | |
|---|---|
| Low back | |
| Backache | 50,284 (46.2) |
| Low back pain | 12,722 (11.7) |
| Intervertebral disc disorder | 6,946 (6.4) |
| Degeneration of intervertebral disc | 6,154 (5.7) |
| Chronic back pain | 5,559 (5.1) |
| Spinal stenosis | 3,022 (2.8) |
| Scoliosis deformity of spine | 2,368 (2.2) |
| Fracture of vertebral column | 2,237 (2.1) |
| Osteoarthritis of lumbar spine | 2,054 (1.9) |
| Laminectomy | 1,781 (1.6) |
| Lumbosacral spondylosis | 1,439 (1.3) |
| Injury of back | 1,185 (1.1) |
| Neck | |
| Neck pain | 7,792 (41.2) |
| Cervical spine degeneration | 3,806 (20.1) |
| Cervical radiculopathy | 2,421 (12.8) |
| Cervicogenic headache | 925 (4.9) |
| Cervical disc disorder | 755 (4.0) |
| Torticollis | 603 (3.2) |
| Whiplash injury to neck | 507 (2.7) |
| Cervico-occipital neuralgia | 250 (1.3) |
| Stiff neck | 249 (1.3) |
| Injury of cervical spine | 225 (1.2) |
| Shoulder | |
| Shoulder pain | 11,854 (32.1) |
| Subacromial bursitis | 6,236 (16.9) |
| Rotator cuff syndrome | 4,355 (11.8) |
| Adhesive capsulitis | 2,313 (6.3) |
| Injury of shoulder region | 1,873 (4.8) |
| Supraspinatus tear | 1,411 (3.8) |
| Capsulitis | 1,313 (3.6) |
| Supraspinatus tendinitis | 1,053 (2.9) |
| Impingement syndrome of shoulder region | 880 (2.4) |
| Inflammation of rotator cuff tendon | 699 (1.9) |
| Total shoulder replacement | 639 (1.7) |
| Osteoarthritis of shoulder | 596 (1.6) |
| Arthroscopy of shoulder | 569 (1.5) |
| Subdeltoid bursitis | 566 (1.5) |
| Repair of musculotendinous cuff of shoulder | 553 (1.5) |
| Rupture of tendon of biceps | 385 (1.0) |
| Knee | |
| Knee pain | 12,077 (26.4) |
| Total knee replacement | 8,699 (19.0) |
| Osteoarthritis of knee | 8,683 (19.0) |
| Arthroscopy of knee | 2,870 (6.3) |
| Injury of knee | 2,201 (4.8) |
| Synovial cyst of popliteal space | 2,000 (4.4) |
| Finding of tear meniscus | 1,895 (4.1) |
| Tear of meniscus of knee | 782 (1.7) |
| Acute meniscal tear, medial | 719 (1.6) |
| Prepatellar bursitis | 700 (1.5) |
| Tear of medial meniscus of knee | 685 (1.5) |
| Knee joint effusion | 550 (1.2) |
| Chondromalacia of patella | 514 (1.1) |
Discussion
Summary
Approximately one-quarter of patients attending general practice in three PHNs within Victoria, Australia during the five-year period between 2014 and 2018 had one or more musculoskeletal complaints. Forty-one percent were labelled with at least one low back, knee, shoulder, or neck eligible diagnostic code within our age criteria. There was a slight female preponderance, most people were of working age, had at least one comorbidity and lived in an area of relative socioeconomic advantage. Most commonly the diagnostic code used to label the regional complaint used a non-specific label, i.e., pain or ache. Our study cohort consulted with a GP numerous times within one year of diagnosis and those with multiple body regions affected attended more frequently than those with a single body region affected.
Comparison with existing literature
The overall prevalence of musculoskeletal complaints among patients consulting a GP in the POLAR database during the study period is consistent with estimates from the 2014–15 Australian National Health Survey which reported that approximately 30% of Australians have at least one musculoskeletal complaint [23] and that the majority of Australians visit their GP multiple times a year [1]. The sex and age breakdown of our cohort is in keeping with Australian Burden of Disease Study 2011 which reported slightly more females in general have a musculoskeletal condition (55%) and 61% of Australians with musculoskeletal conditions are of working age (25–64 years) [28]. Our data are also similar to the Bettering the Evaluation and Care of Health (BEACH) dataset which reported that among patients presenting to general practice with musculoskeletal complaints, 57% are female and 65% are aged 15–64 years [3].
The prevalence of comorbidities in our cohort was in keeping with National Health Survey data that observed 65% of Australians with back pain report having at least one other chronic complaint, of which arthritis (31%), cardiovascular disease (31%) and mental health problems (30%) were most common [23]. The co-occurrence of musculoskeletal complaints with comorbidities, particularly cardiovascular and mental health conditions, is also reported internationally [29, 30].
Our cohort of patients with regional musculoskeletal complaints consulted with a GP for any reason a median of seven times (IQR 4–12) within the first year following diagnosis. This is higher than that of adult patients consulting with a GP within the POLAR database for any reason [median 4 (IQR 2–8)] and that reported by MedicineInsight in the same Australian state during 2017–18 [31]. While this may be partially explained by the older age (due to our eligibility criteria) and female preponderance of our study cohort [31], the high number of GP encounters per year we observed may also be a reflection of the high burden of GP care amongst people with musculoskeletal complaints, especially since our younger cohort of people with back complaints had a similar number of all-cause consultations per year [median 6 (IQR 3–12)] as those with neck, shoulder and knee complaints [median 7 (IQR 4–12)]. This is consistent with an analysis of Australian-wide MedicineInsight data that demonstrated patients with arthritis, chronic back pain, gout, osteoporosis, spondyloarthropathies and/or rheumatoid arthritis attended general practices more frequently than those without these conditions between October 2013 and June 2016 [14]. Our results also suggest patients with multi-site musculoskeletal complaints consult with a GP more frequently than those with a single body region affected (median 11 and 7 occasions/year respectively). While only 11% of our cohort had a diagnosis relating to multiple body regions, this is likely to be an underestimate since we did not include general musculoskeletal terms such as sprain or osteoarthritis that could not be attributed to a specific body region.
Most patients with an eligible musculoskeletal complaint were labelled with a non-specific diagnostic code (e.g., pain, ache) rather than a more specific patho-anatomical or patho-aetiologic label (e.g., cervical radiculopathy, adhesive capsulitis). This is consistent with the non-specific nature of many regional musculoskeletal complaints. For example, in approximately 90% of patients with low back pain, a specific cause of the pain (e.g. disease, structural abnormality or serious injury) cannot be identified [32].
Implications for research and practice
Relative to the number of musculoskeletal-related SNOMED CT-AU codes available, few codes were used most often. In addition, many of the diagnostic labels describe the same condition (e.g., rotator cuff syndrome, supraspinatus tendinitis, inflammation of rotator cuff tendon), while others describe presumed or actual imaging findings that may or may not be clinically relevant (e.g., degeneration) or a specific treatment rather than a diagnosis (e.g., laminectomy, arthroscopy). This lack of mutually exclusive categories and redundancy has been observed in a study of low back pain coding [33]. Revision of the SNOMED CT-AU classification system to reduce redundancy while ensuring all conditions can be labelled may improve consistency and allow comparison across studies that use this system. GP involvement in assigning diagnostic codes from a list generated in real-time using clinical natural language processing may help to address these issues, but this approach would need to be validated in practice.
There is evidence that the management of patients with musculoskeletal complaints in general practice is suboptimal when compared to recommendations from clinical practice guidelines. Evidence to practice gaps include overuse of imaging, [34, 35] referral to specialist care [36], surgery [37, 38], and opioid prescription [39]. The ongoing use of these low value interventions may contribute to the high burden of GP consultations we observed in this study indicating an urgent need to identify effective strategies to implement evidence-based recommendations for people with musculoskeletal conditions into practice and policy. A 2016 Cochrane review found low quality evidence that guideline dissemination and educational opportunities alone may lead to little or no improvement in guideline-consistent GP care for people with low back pain (7 studies), but that additional strategies such as feedback (2 studies) and GP reminder messages (1 study) may lead to small improvements [40]. The value of audit and feedback is supported by a recent Australian-wide factorial cluster trial that found audit and feedback resulted in > 47,000 fewer selected low back, neck, knee and shoulder imaging tests over 18 months among high requesting GPs [41]. Other promising strategies include digital treatment alogorithms [42], other decision tools [43], and modifying imaging reports to include simple terminology and explicit consideration of context [44].
Strengths and limitations
The strengths of this study include its large sample size and comparability to population estimates in terms of patient demographics, PHN representation and body regions affected. Limitations of this study include missing data within the POLAR database and the potential for selection bias of consenting practices. Prior to merging the relational data files, nearly 20% of provider files did not include a provider type and 12% of diagnoses records had a missing diagnosis code or missing or implausible diagnosis date. Missing data may occur at random due to a lack of documentation within the electronic health record (responses are not mandated by GPs) or because a code could not be attributed by the clinical natural language process. This means our dataset of patients with musculoskeletal complaints may be incomplete. Despite this, our study cohort appears to be broadly representative of the wider Australian population attending a GP and to those with musculoskeletal complaints within the community. Although approximately 30% of general practices across south-eastern Victoria are included within the POLAR database, non-accredited, corporate-owned practices, and those not using electronic medical records are under-represented. While we do not have the information available to assess for any differences in the characteristics of GPs who were and were not included in this cohort, this potential for difference should be considered when interpreting the frequency of consultations provided by the GPs in this study. Our estimate of the all-cause consultations per year also includes consultations that may be for reasons other than a musculoskeletal complaint. Additionally, our estimate of the prevalence of regional low back, knee, shoulder and neck complaints is likely an underestimate due to our exclusion of selected age groups.
Conclusion
There is a high burden of patients with non-specific regional musculoskeletal complaints within general practice. Most occur in working age and are accompanied by at least one comorbidity, and many patients attend on multiple occasions. Identification and evaluation of strategies to reduce this burden are needed.
Supplementary Information
Additional file 1: Appendix 1. Diagnostic codes used in less than 1% of patients for each body region.
Acknowledgements
Not applicable
Authors’ contributions
RH, DOC and RB conceived the study. LB and AG were responsible for data coding and the statistical analysis plan. CP provided expertise in the use of the POLAR database. DM provided clinical context in managing musculoskeletal conditions in the general practice setting. All authors contributed to refining the manuscript and approved the submitted manuscript.
Funding
This work was supported by an Arthritis Queensland, Arthritis South Australia and the Allan and Beryl Stephens Grant from Arthritis Australia (ID N/A). Arthritis Australia did not contribute to the conduct of this study. It is also supported by an Australian National Health and Medical Research Council (NHMRC) Program Grant (APP1113532). DOC is supported by a TRIP Fellowship and RB is supported by an NHMRC Investigator Fellowship.
Availability of data and materials
The dataset supporting the conclusions of this article can be requested from the data custodians, Outcome Health (email:research@outcomehealth.org.au). The statistical analysis code is available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was reviewed and approved by the Cabrini Human Research Ethics Committee and Monash University Human Research Ethics Committee (Reference Numbers 02–21-01–19 and 16975, respectively) and was conducted in accordance with the Declaration of Helsinki. We did not obtain participant consent as all data were anonymised. Outcome Health holds a standing ethics approval for its collection and custodianship of the deidentified data from the Royal Australian College of General Practice. Outcome Health and the individual PHNs granted permission to access the data used in this study.
Consent for publication
Not applicable.
Competing interests
RH, DOC, RB and DM report grants from Arthritis Australia (not-for-profit organisation), during the conduct of the study. CP is an employee of Outcome Health, the not-for-profit organisation that developed the POLAR database and chairs the Product improvement group of the Australian Digital Health Agency. It has no relationship with the research but has provided grant funding to Outcome Health. LB reports consultancy fees paid to Monash University from Charite Medical University Berlin, Jesuit Social Services Victoria, and Swinburne University of Technology, outside the submitted work. AG reports no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Romi Haas, Email: romi.haas@monash.edu.
Alexandra Gorelik, Email: alexandra.gorelik@monash.edu.
Ljoudmila Busija, Email: lucy.busija@monash.edu.
Denise O’Connor, Email: denise.oconnor@monash.edu.
Christopher Pearce, Email: drchrispearce@mac.com.
Danielle Mazza, Email: danielle.mazza@monash.edu.
Rachelle Buchbinder, Email: rachelle.buchbinder@monash.edu.
References
- 1.Royal Australian College of General Practitioners. General Practice: Health of the Nation 2019. Available from: https://www.racgp.org.au/getmedia/bacc0983-cc7d-4810-b34a-25e12043a53e/Health-of-the-Nation-2019-report.pdf.aspx.. Accessed 20 Dec 2021.
- 2.Finley C, Chan DS, Garrison S, et al. What are the most common conditions in primary care? Can Fam Physician. 2018;64:832–840. [PMC free article] [PubMed] [Google Scholar]
- 3.Britt H MG, Henderson J, Bayram C, Harrison C, Valenti L, Pan Y, Charles J, Pollack AJ, Wong C, Gordon J. General practice activity in Australia 2015–16. General practice series no. 40. Sydney: Sydney University Press, 2016.
- 4.Ingram M, Symmons DP. The burden of musculoskeletal conditions. Medicine. 2018;46(3):152–155. doi: 10.1016/j.mpmed.2017.12.005. [DOI] [Google Scholar]
- 5.Canaway R, Boyle DI, Manski-Nankervis JAE, et al. Gathering data for decisions: best practice use of primary care electronic records for research. Med J Aust. 2019;210:S12–S16. doi: 10.5694/mja2.50026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yan J, Hawes L, Turner L, et al. Antimicrobial prescribing for children in primary care. J Paediatr Child Health. 2019;55(1):54–58. doi: 10.1111/jpc.14105. [DOI] [PubMed] [Google Scholar]
- 7.Hasselström J, Zarrinkoub R, Holmquist C, et al. The Swedish Primary Care Cardiovascular Database (SPCCD): 74 751 hypertensive primary care patients. Blood Press. 2014;23(2):116–125. doi: 10.3109/08037051.2013.814829. [DOI] [PubMed] [Google Scholar]
- 8.Chidwick K, Kiss D, Gray R, et al. Insights into the management of chronic hepatitis C in primary care using MedicineInsight. Aust J Gen Pract. 2018;47(9):639–645. doi: 10.31128/AJGP-02-18-4482. [DOI] [PubMed] [Google Scholar]
- 9.Allen AS, Forman JP, Orav EJ, et al. Primary care management of chronic kidney disease. J Gen Intern Med. 2011;26(4):386–392. doi: 10.1007/s11606-010-1523-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Greiver M, Williamson T, Barber D, et al. Prevalence and epidemiology of diabetes in Canadian primary care practices: a report from the Canadian Primary Care Sentinel Surveillance Network. Can J Diabetes. 2014;38(3):179–185. doi: 10.1016/j.jcjd.2014.02.030. [DOI] [PubMed] [Google Scholar]
- 11.Imai C, Li L, Hardie R-A, et al. Adherence to guideline-recommended HbA1c testing frequency and better outcomes in patients with type 2 diabetes: a 5-year retrospective cohort study in Australian general practice. BMJ Qual Saf. 2021;30(9):706–714. doi: 10.1136/bmjqs-2020-012026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Min T, Davies GI, Rice S, et al. Treatment choices for the glycaemic management of patients with type 2 diabetes and chronic kidney disease: Analysis of the SAIL patient linked dataset. Diabetes Metab Syndr. 2018;12(2):123–127. doi: 10.1016/j.dsx.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 13.Birtwhistle R, Morkem R, Peat G, et al. Prevalence and management of osteoarthritis in primary care: an epidemiologic cohort study from the Canadian Primary Care Sentinel Surveillance Network. CMAJ Open. 2015;3(3):E270. doi: 10.9778/cmajo.20150018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.González-Chica DA, Vanlint S, Hoon E, et al. Epidemiology of arthritis, chronic back pain, gout, osteoporosis, spondyloarthropathies and rheumatoid arthritis among 1.5 million patients in Australian general practice: NPS MedicineWise MedicineInsight dataset. BMC Musculoskelet Disord. 2018;19(1):1–10. doi: 10.1186/s12891-018-1941-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jordan KP, Jöud A, Bergknut C, et al. International comparisons of the consultation prevalence of musculoskeletal conditions using population-based healthcare data from England and Sweden. Ann Rheum Dis. 2014;73(1):212–218. doi: 10.1136/annrheumdis-2012-202634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Naik-Panvelkar P, Norman S, Elgebaly Z, et al. Osteoporosis management in Australian general practice: an analysis of current osteoporosis treatment patterns and gaps in practice. BMC Fam Pract. 2020;21(1):1–13. doi: 10.1186/s12875-020-01103-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ryan BL, Maddocks HL, McKay S, et al. Identifying musculoskeletal conditions in electronic medical records: a prevalence and validation study using the Del iver P rimary H ealthcare I nformation (DELPHI) database. BMC Musculoskelet Disord. 2019;20(1):1–8. doi: 10.1186/s12891-019-2568-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Black-Tiong S, Gonzalez-Chica D, Stocks N. Trends in long-term opioid prescriptions for musculoskeletal conditions in Australian general practice: a national longitudinal study using MedicineInsight, 2012–2018. BMJ Open. 2021;11(4):e045418. doi: 10.1136/bmjopen-2020-045418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith C, Hewison J, West RM, et al. Understanding patterns of care for musculoskeletal patients using routinely collected National Health Service data from general practices in England. Health Informatics J. 2020;26(4):2470–2484. doi: 10.1177/1460458220907431. [DOI] [PubMed] [Google Scholar]
- 20.Cooksey R, Rahman MA, Kennedy J, et al. Biologic use in psoriatic arthritis and ankylosing spondylitis patients: a descriptive epidemiological study using linked, routine data in Wales, UK. Rheumatol Adv Pract. 2021;5(2):rkab042. doi: 10.1093/rap/rkab042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haas R, Busija L, Gorelik A, et al. Patterns of care for people presenting to Australian general practice with musculoskeletal complaints based on routinely collected data: protocol for an observational cohort study using the Population Level Analysis and Reporting (POLAR) database. BMJ Open. 2021;11(9):e055528. doi: 10.1136/bmjopen-2021-055528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wright M, Hall J, Van Gool K, et al. How common is multiple general practice attendance in Australia? Aust J Gen Pract. 2018;47(5):289–296. doi: 10.31128/AJGP-11-17-4413. [DOI] [PubMed] [Google Scholar]
- 23.Australian Institute of Health and Welfare. Musculoskeletal conditions and comorbidity in Australia. Canberra: AIHW, 2019.
- 24.Hansen DP, Kemp ML, Mills SR, et al. Developing a national emergency department data reference set based on SNOMED CT. Med J Aust. 2011;194:S8–S10. doi: 10.5694/j.1326-5377.2011.tb02934.x. [DOI] [PubMed] [Google Scholar]
- 25.Pearce C, McLeod A, Patrick J, et al. Coding and classifying GP data: the POLAR project. BMJ Health Care Inform. 2019;26(1):e100009. doi: 10.1136/bmjhci-2019-100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Australian Bureau of Statistics. 1270.0.55.001 - Australian Statistical Geography Standard (ASGS): Volume 1 - Main Structure and Greater Capital City Statistical Areas, July 2016. Available from: https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/1270.0.55.001~July%202016~Main%20Features~Statistical%20Area%20Level%203%20(SA3)~10015. Accessed 20 Dec 2021.
- 27.Australian Bureau of Statistics. Socio-economic indexes for areas (SEIFA) - technical paper 2016. cat no 20330 55001. Available from: https://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001. Accessed 20 Dec 2021.
- 28.Rahman N, Gruber D. The burden of musculoskeletal conditions in Australia: a detailed analysis of the Australian Burden of Disease Study 2011: Australian Institute of Health and Welfare 2017.
- 29.Duffield SJ, Ellis BM, Goodson N, et al. The contribution of musculoskeletal disorders in multimorbidity: implications for practice and policy. Best Pract Res Clin Rheumatol. 2017;31(2):129–144. doi: 10.1016/j.berh.2017.09.004. [DOI] [PubMed] [Google Scholar]
- 30.Ramanathan S, Hibbert P, Wiles L, et al. What is the association between the presence of comorbidities and the appropriateness of care for low back pain? A population-based medical record review study. BMC Musculoskelet Disord. 2018;19(1):1–9. doi: 10.1186/s12891-018-2316-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.MedicineWise NPS. General practice Insights Report July 2017–June 2018. Sydney, NSW: NPS MedicineWise 2019
- 32.Koes BW, Van Tulder M, Thomas S. Diagnosis and treatment of low back pain. BMJ. 2006;332(7555):1430–1434. doi: 10.1136/bmj.332.7555.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tamrakar M, O’Keeffe M, Traeger AC, et al. Diagnostic codes for low back pain, nomenclature or noise? A descriptive study of disease classification system coding of low back pain. Int J Rheum Dis. 2022;25(3):272–280. doi: 10.1111/1756-185X.14264. [DOI] [PubMed] [Google Scholar]
- 34.Buchbinder R, Staples MP, Shanahan EM, et al. General practitioner management of shoulder pain in comparison with rheumatologist expectation of care and best evidence: an Australian national survey. PLoS ONE. 2013;8(4):e61243. doi: 10.1371/journal.pone.0061243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Naunton J, Harrison C, Britt H, et al. General practice management of rotator cuff related shoulder pain: A reliance on ultrasound and injection guided care. PLoS ONE. 2020;15(1):e0227688. doi: 10.1371/journal.pone.0227688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Speed C, Crisp A. Referrals to hospital-based rheumatology and orthopaedic services: seeking direction. Rheumatology. 2005;44(4):469–471. doi: 10.1093/rheumatology/keh504. [DOI] [PubMed] [Google Scholar]
- 37.Harris IA, Madan NS, Naylor JM, et al. Trends in knee arthroscopy and subsequent arthroplasty in an Australian population: a retrospective cohort study. BMC Musculoskelet Disord. 2013;14(1):1–6. doi: 10.1186/1471-2474-14-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Judge A, Murphy R, Maxwell R, et al. Temporal trends and geographical variation in the use of subacromial decompression and rotator cuff repair of the shoulder in England. The bone & joint journal. 2014;96(1):70–74. doi: 10.1302/0301-620X.96B1.32556. [DOI] [PubMed] [Google Scholar]
- 39.Donovan PJ, Arroyo D, Pattullo C, et al. Trends in opioid prescribing in Australia: a systematic review. Aust Health Rev. 2019;44(2):277–287. doi: 10.1071/AH18245. [DOI] [PubMed] [Google Scholar]
- 40.Brown VT, Underwood M, Mohamed N, et al. Professional interventions for general practitioners on the management of musculoskeletal conditions. Cochrane Database Syst Rev. 2016;(5):CD007495. [DOI] [PMC free article] [PubMed]
- 41.O’Connor DA, Glasziou P, Maher CG, et al. Effect of an Individualized Audit and Feedback Intervention on Rates of Musculoskeletal Diagnostic Imaging Requests by Australian General Practitioners: A Randomized Clinical Trial. JAMA. 2022;328(9):850–860. doi: 10.1001/jama.2022.14587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Priebe JA, Haas KK, Sanchez LFM, et al. Digital treatment of back pain versus standard of care: the cluster-randomized controlled trial, rise-uP. J Pain Res. 2020;13:1823. doi: 10.2147/JPR.S260761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Jayakumar P, Moore MG, Furlough KA, et al. Comparison of an Artificial Intelligence-Enabled Patient Decision Aid vs Educational Material on Decision Quality, Shared Decision-Making, Patient Experience, and Functional Outcomes in Adults With Knee Osteoarthritis: A Randomized Clinical Trial. JAMA Netw Open. 2021;4(2):e2037107–e2037207. doi: 10.1001/jamanetworkopen.2020.37107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bossen JK, Hageman MG, King JD, et al. Does rewording MRI reports improve patient understanding and emotional response to a clinical report? Cli Orthop Relat Res®. 2013;471(11):3637–44. doi: 10.1007/s11999-013-3100-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Appendix 1. Diagnostic codes used in less than 1% of patients for each body region.
Data Availability Statement
The dataset supporting the conclusions of this article can be requested from the data custodians, Outcome Health (email:research@outcomehealth.org.au). The statistical analysis code is available from the corresponding author on reasonable request.