Summary
Background
Innovative solutions are required to provide mental health support at scale in low-resource humanitarian contexts. We aimed to assess the effectiveness of a facilitator-guided, group-based, self-help intervention (Self-Help Plus) to reduce psychological distress in female refugees.
Methods
We did a cluster randomised trial in rural refugee settlements in northern Uganda. Participants were female South Sudanese refugees with at least moderate levels of psychological distress (cutoff ≥5 on the Kessler 6). The intervention comprised access to usual care and five 2-h audio-recorded stress-management workshops (20–30 refugees) led by briefly trained lay facilitators, accompanied by an illustrated self-help book. Villages were randomly assigned to either intervention (Self-Help Plus or enhanced usual care) on a 1:1 basis. Within 14 villages, randomly selected households were approached. Screening of women in households continued until 20–30 eligible participants were identified per site. The primary outcome was individual psychological distress, assessed using the Kessler 6 symptom checklist 1 week before, 1 week after, and 3 months after intervention, in the intention-to-treat population. All outcomes were measured at the individual (rather than cluster) level. Secondary outcomes included personally identified problems, post-traumatic stress, depression symptoms, feelings of anger, social interactions with other ethnic groups, functional impairment, and subjective wellbeing. Assessors were masked to allocation. This trial was prospectively registered at ISRCTN, number 50148022.
Findings
Of 694 eligible participants (331 Self-Help Plus, 363 enhanced usual care), 613 (88%) completed all assessments. Compared with controls, we found stronger improvements for Self-Help Plus on psychological distress 3 months post intervention (β −1·20, 95% CI −2·33 to −0·08; p=0·04; d −0·26). We also found larger improvements for Self-Help Plus 3 months post-intervention for five of eight secondary outcomes (effect size range −0·30 to −0·36). Refugees with different trauma exposure, length of time in settlements, and initial psychological distress benefited similarly. With regard to safety considerations, the independent data safety management board responded to six adverse events, and none were evaluated to be concerns in response to the intervention.
Interpretation
Self-Help Plus is an innovative, facilitator-guided, group-based self-help intervention that can be rapidly deployed to large numbers of participants, and resulted in meaningful reductions in psychological distress at 3 months among South Sudanese female refugees.
Funding
Research for Health in Humanitarian Crises (R2HC) Programme.
Introduction
Conflict-affected populations are at elevated risk of psychological distress and a range of mental health disorders.1 Over the past two decades, psychological treatments that are effective among conflict-affected populations have been identified (eg, cognitive behavioural interventions and interpersonal therapy).2 Although evidence of the effectiveness of these interventions is promising,3 and innovative strategies have been tested, important challenges to providing mental health and psychosocial support interventions at scale in low-resource humanitarian settings remain.
Current evidence-based treatments generally require a substantial clinical workforce not typically available in disrupted, under-resourced health systems.4 Task sharing with non-specialists has been a key strategy5 also in humanitarian settings.5–7 At the same time, non-specialists offering psychological interventions need to be well trained and supervised—a challenging requirement in insecure contexts.8
Current evidence-based interventions commonly target single mental disorders, whereas comorbidity is highly prevalent in humanitarian settings.9 Training providers in multiple evidence-based therapies for multiple disorders is resource prohibitive. Recent efforts have focused on developing and testing transdiagnostic approaches in humanitarian settings—ie, interventions that can address symptoms across a range of mental health disorders. For example, interventions such as the Common Elements Treatment Approach,10 Problem Management Plus,11 and Youth Readiness Intervention12 have combined elements from disorder-specific evidence-based treatments to target (signs and symptoms of) multiple mental disorders.
Studies on mental health interventions in humanitarian settings have predominantly focused on people scoring above cutoffs on symptom checklists associated with particular mental disorders (notably post-traumatic stress disorder [PTSD] and depression). However, subsyndromal psychological distress is also highly prevalent in conflict-affected populations.8 Psychological distress poses risk for subsequent mental disorders and causes marked impairment.13,14
Although non-specialist-delivered interventions reduce psychological symptoms with moderate to large effect sizes, they typically only reach individuals or small groups of people at a time. In settings of armed conflict, large groups of women are survivors of gender-based violence and experience gendered stressors.15 Although previous studies have evaluated effective treatment strategies with conflict-affected women and girls,5,16 there remains a paucity of knowledge on how to bring mental health supports to the required scale.17
Against these challenges, it is clear that addressing the substantive mental health needs in humanitarian settings will require further innovation. Many other areas of public health promote interventions with small individual health effects (eg, vaccinations against influenza, tobacco pricing, or injury messaging) that, at scale, add up to large population health effects.18 WHO has been seeking to apply such a public health approach to address vast mental health needs and has developed a multimedia guided (ie, audio recordings and book) self-help intervention called Self-Help Plus.19 The intervention’s format was informed by meta-analyses showing promising results for bibliotherapy, group-based prerecorded psychoeducational self-help interventions and guided self-help in general.20,21 The intervention builds on existing innovations in delivery of mental health interventions in humanitarian settings by relying on task sharing and addressing a broader range of mental health difficulties. At the same time, the intervention was designed to address challenges related to scale and access, by further reducing the burden and demand on a workforce of non-specialists through a preformatted multimedia delivery package, and to more quickly reach larger numbers of people by being able to be delivered in workshops of 20–30 people. In addition, the intervention’s focus on psychological distress broadly (by teaching stress management skills that might be applied across a range of difficulties) might further reduce needs for detailed diagnostic procedures, thus enhancing potential for scale-up.
Following formative research,22,23 this study aimed to evaluate the effectiveness of Self-Help Plus in a cluster randomised controlled trial (cRCT) with South Sudanese female refugees living in Uganda. We hypothesised that Self-Help Plus would result in larger improvements on indicators of psychological distress and functioning at the 3-month follow-up compared with controls.
Rhino Camp settlement is located in northwestern Uganda, and hosts more than 250 000 mainly South Sudanese refugees. Renewed armed conflict in South Sudan has instigated the third largest refugee crisis in the world. The population in the Rhino Camp refugee settlement consists, in large majority, of women and children. Female refugees have been exposed to high levels of gender-based violence. We were interested in testing an intervention that could reduce distress in this particular population, and Self-Help Plus materials briefly mention gender-based violence as a potential cause of psychological distress. At the same time, we were interested in testing an intervention that could strengthen skills to manage distress arising from a broader range of stressors in both men and women, to avoid potential stigma resulting from specifically targeting gender-based violence survivors, and enhance potential scale-up through keeping content more broadly applicable.
Methods
Study design
We did a single-blind, parallel-group cRCT in 14 villages and 694 female South Sudanese refugees in Rhino Camp settlement in northwestern Uganda (figure). The trial protocol was published previously,24 and no changes were made to design after the trial started. A cluster design was chosen to avoid contamination of intervention materials within villages, because participants might share self-help materials (eg, the book) with their neighbours. The project was approved by the MildMay Uganda Research Ethics Committee, the Uganda National Council for Science and Technology, and the WHO Ethical Review Committee and all participants provided informed consent.
Figure: Flow diagram.
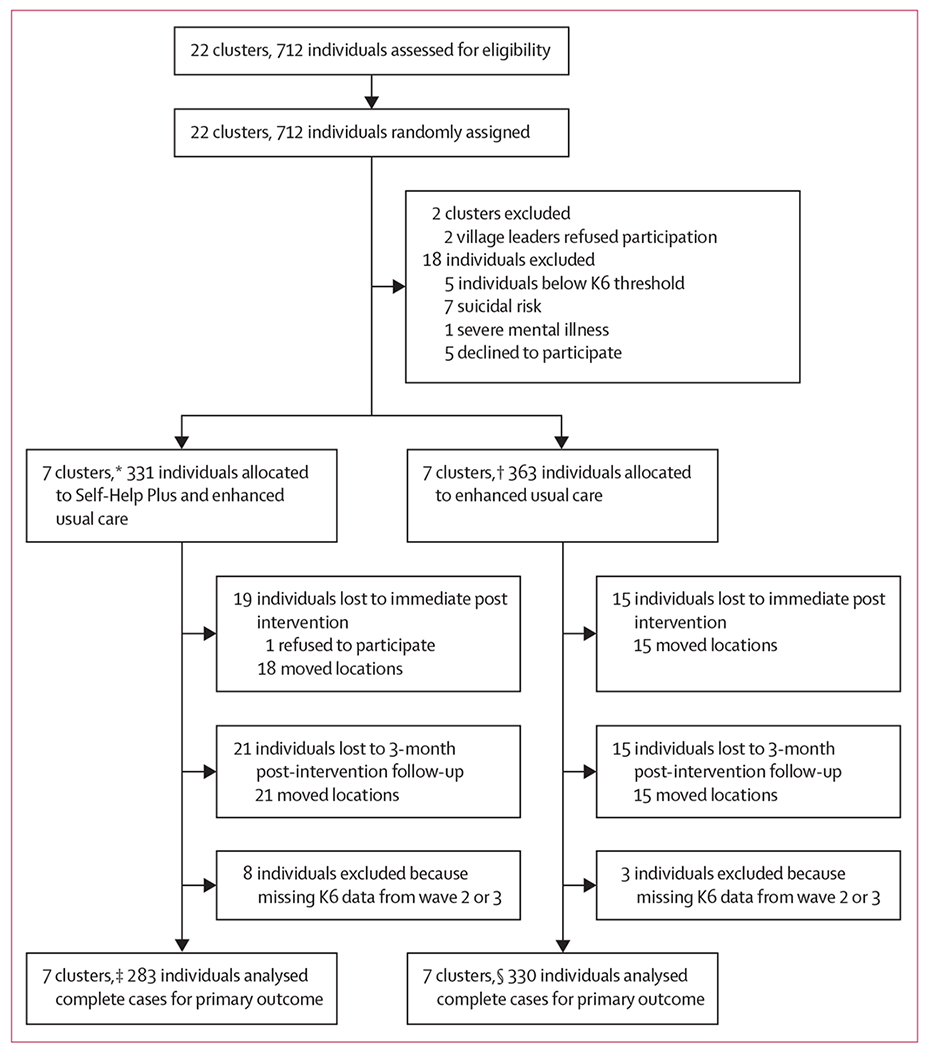
K6=Kessler 6. *Mean cluster size 47·3 participants (s2 43·6). †Mean cluster size 51·9 participants (s2 6·8). ‡Mean cluster size 40·43 participants (s2 79·62). §Mean cluster size 47·14 participants (s2 10·48).
Randomisation and masking
Randomisation was done by an independent epidemiologist at Johns Hopkins University (Baltimore, MD, USA). A simple random allocation sequence was generated using Stata 14 and villages were allocated to intervention with enhanced usual care or enhanced usual care alone, without applying stratification or matching, on 1:1 basis. All settlement villages listed by the Office of the Prime Minister at commencement of the study were eligible for randomisation, except for villages involved in prior formative research. The allocation sequence was hidden from assessors. Self-Help Plus facilitators were given names of Self-Help Plus villages immediately before implementation. To maintain masking, assessors worked in a separate office and visited the settlement on different days from Self-Help Plus facilitators, who were instructed not to disclose allocation.
Within villages, households were randomly selected by spinning a bottle and approaching the first household in the direction pointed to by the bottle and, then repeating this, every fifth household thereafter. We asked whether any Juba Arabic-speaking women were residing in each household. If only one Juba Arabic-speaking female adult lived in the household we approached her for consent. If there were multiple eligible women we randomly selected one by drawing slips. The independent assessors administered the Kessler 6 (K6) to assess psychological distress, applying a cutoff score of five or more for moderate-level psychological distress.14 Participants were excluded if they were at imminent risk of suicide (assessed with structured questionnaire); showing observable signs of severe mental disorder (eg, psychosis); or not able to understand basic instructions, with the latter two assessed with observation checklists. Screening continued until we could form two groups of 20–30 participants in each village. In smaller villages, screening stopped after every household in the village had been approached.
Procedures
The local project coordinator (MRL) approached village leaders to explain the study and ask for permission the day before data collection. Interviewers sought informed consent for baseline assessment the day after initial screening. Participants at imminent risk of suicide were immediately assisted by a trained clinical team, and participants showing observable signs of severe mental disorder (eg, psychosis) were referred to a standby psychiatric team. All questionnaires were administered in interview format. Assessors were Ugandan nationals residing in the settlement area, proficient in Juba Arabic and English, with at least an undergraduate diploma. Training of assessors took place in a 1-week course that emphasised skills-based learning through role playing.
Self-Help Plus is based on acceptance and commitment therapy (ACT), a modern variant of cognitive behavioural therapy. More detailed information about session content can be found in the appendix (pp 1–2). ACT builds on the cognitive behavioural therapy tradition and includes some common elements (such as engagement and psychoeducation); however, ACT uses specific techniques (eg, cognitive defusion, mindfulness exercises, and values clarification exercises) to help promote psychological flexibility—the ability to contact the present moment more fully and to maintain or change behaviour so that the person behaves in a way that is consistent with their subjectively identified values.25 Self-Help Plus incorporates many of these factors, with a strong focus on mindful practices and grounding, values clarification, and compassion (being kind to self and others), with the latter also encouraging a social support element through the practice of acts of kindness towards others outside of sessions. ACT is a-diagnostic, in that it is not a syndrome-based or symptom-based approach. Instead it aims to support people in finding more functional ways of coping with difficult life experiences given their self-identified values. A 2019 systematic review26 of ACT mediation studies found that of the five studies that examined this question, four showed psychological flexibility to mediate treatment outcomes. Although ACT focuses on promoting values-based living, rather than attempting to directly control or reduce symptoms, a substantial evidence base exists linking ACT with reductions in anxiety, depression, and stress,27 and evidence is emerging for mindfulness based-approaches and ACT28 in self-help formats. In this study, we therefore expected to find stronger improvements in the intervention condition on all symptom measures. Third-wave approaches (such as ACT and mindfulness-based approaches) have been piloted previously in humanitarian settings,29–31 but this is—to the best of our knowledge—the first randomised trial. Self-Help Plus comprises a prerecorded psycho-educational audio course of five weekly 2-h sessions, delivered in workshops with 20–30 participants. An illustration-based self-help book with minimal text (to enhance use by participants with basic literacy skills) covers key points from audio sessions. To enhance scalability, Self-Help Plus aims to reduce psychological distress arising in the context of diverse stressors (eg, interpersonal violence or chronic poverty) across a broad range of mental health conditions, regardless of whether people meet diagnostic criteria for particular disorders. Given that content is mainly delivered through audio-recorded materials, it can be delivered by non-specialists with brief training. Self-Help Plus is not intended for people with complex mental health problems (such as psychosis) or those at imminent risk of suicide.
Self-Help Plus was deemed a good fit for this setting after an initial needs assessment indicated the ubiquity of overthinking,32 a local idiom of psychological distress and an explicit target of ACT. Initial piloting with one group of male and female refugees each identified challenges with engagement and participation of male refugees.22 We subsequently decided to focus further piloting and the current trial on female refugees, and engage in a separate trajectory to adapt and test the intervention with male refugees. A feasibility cRCT23 found Self-Help Plus to be relevant, acceptable, and feasible among female South Sudanese refugees.
Self-Help Plus was delivered in pairs by eight female facilitators: seven Ugandans residing in the area, and one South Sudanese refugee. All finished secondary education, had experience working in the settlement, and were proficient in Juba Arabic and English. None had formal mental health training or work experience. Four of the facilitators were trained before the uncontrolled pilot trial (5 days)22 and feasibility trial (4 days)23 by master trainers (FB, KC). Four new facilitators were trained by listening through the audio, and taking part in practice Self-Help Plus sessions (led by intervention team leader; 4 days); and training in Self-Help Plus facilitation skills (4 days). The facilitator’s role was limited, focusing on playing the audio recording, responding to questions and disruptions, and facilitating highly scripted individual exercises and small group discussions.
One facilitator was intervention team leader and led post-session technical debriefs. Intervention supervision was provided by a Ugandan social worker, who was available for questions, attended the debriefs, and provided supervision every 2 weeks. Additional supervision was requested from the Self-Help Plus master trainer if necessary (amounting to <2 h per month). Fidelity was checked by the intervention supervisor through adherence forms completed by facilitators. In addition, the intervention supervisor observed 10% of the sessions and completed an adherence form.
Enhanced usual care was provided to participants in both study groups. After screening, all participants met once for 30 min with a trained community health worker who provided psychoeducation using a structured script covering overthinking and strategies for self-management. In addition, participants were provided information on where to access existing mental health services, which comprised psychosocial and pharmacological interventions, offered by a multidisciplinary mental health team that visited the four government primary health-care centres weekly; and a network of trained South Sudanese refugee community health workers providing basic psychosocial support.
Outcomes
All outcomes were measured at the individual (rather than cluster) level. Measures were translated using a structured procedure including: initial translation from English to Juba Arabic by a bilingual team, with immediate back-translation to English to ensure appropriate translation by the study team; review by an independent South Sudanese mental health expert to assess translations for clinical validity; and several rounds of piloting in which we checked item functioning and consulted with a bilingual team and the community advisory board about comprehensibility, acceptability and other response set issues, relevance, and completeness.33 The primary outcome psychological distress was assessed using the K6, first as a screener, and then re-administered at immediate post-treatment and 3-month follow-up assessment. We selected the K6, rather than a symptom checklist associated with a particular disorder, because it matched well with the idiom of overthinking identified in previous qualitative research,32 thus measuring a psychological construct of local salience; and assessing the broader stress-management aims of Self-Help Plus. The K6 asks six questions about sadness, nervousness, restlessness, hopelessness, feeling everything is an effort, and worthlessness in the last 30 days on a five-point response scale (range zero to 24).34 The K6 has been widely applied with good psychometric properties in a range of sociocultural settings.34 We applied the standard cutoff for moderate levels of psychological distress (≥5)14 with internal consistency (Cronbach α) of 0·65.
All other outcomes were secondary outcomes. Personally identified problems were examined with the Psychological Outcome Profiles instrument (PSYCHLOPS),35 which asks participants to describe two problems from their own perspective and rate problem severity on a six-point scale (range zero to 18; α=0·65). PTSD symptoms were assessed with the PTSD Checklist-Civilian six-item version (PCL-6), using a five-point scale (range six to 30; α=0·72).36 We measured depression symptoms with the Patient Health Questionnaire, nine-item version (PHQ-9), which has a four-point scale (range zero to 27; α=0·67). Anger was assessed using two dichotomous questions asking about explosive anger attacks.37 Based on formative research22 we included three questions concerning positive interactions between ethnic groups (greeting, conversing with, and meeting with people from other ethnic groups; scored on a four-point scale [range zero to 12]; α=0·74). Hazardous alcohol use was assessed but not included in analyses because only four participants reported using alcohol at baseline. We assessed psychological flexibility (both as outcome and putative mediator) using the Acceptance and Action Questionnaire (AAQ-II;38 seven items on a seven-point scale [range seven to 49]; α=0·77).
Functional impairment and subjective wellbeing were assessed with the WHO Disability Assessment Schedule 2·0 (WHODAS)39 and the WHO-5 Wellbeing Index (WHO-5).40 We used the 12-item version of the WHODAS, which uses a five-point scale (range 12–60; α=0·78). The WHO-5 contains five questions using a six-point scale (range zero to 25; α=0·78). In addition, we assessed several moderators (exposure to different levels of traumatic events, session attendance) and cost-effectiveness indicators (use and cost of health services, earnings). The results from the latter assessments will be presented elsewhere.
Statistical analysis
We predicted small-to-medium effect sizes at the 3-month follow-up, based on meta-analyses of similar self-help, psychoeducational interventions, and were interested in detecting an effect size of at least 0·20.20,28 We used the PowerUp! Tool to estimate sample size, using an average cluster size of 42 individuals, 14 clusters (equal assumed), intracluster correlation of 0·012, 20% attrition, 80% power, an α of 0·05, and a two-tailed test. Under these assumptions the minimum detectable effect size is 0·219 with a total sample size of 588. We did not plan interim analyses: trial participation ended after at least three attempts were made to locate all participants for follow-up assessment.
A statistical analysis plan was finalised and signed before data analysis. We followed an intention-to-treat approach; we analysed all participants randomly assigned to either study group, regardless of level of intervention participation. For participants lost at follow-up, we used listwise deletion (or complete case analysis), an acceptable approach when the level of missing data is minimal. Preliminary analyses included a comparison of baseline characteristics to ensure randomisation was successful. We used linear mixed-effects models to evaluate the impact of Self-Help Plus and to accommodate the hierarchical structure of the data using the lme4 package in R with village as a random effect. We present adjusted odds ratios, and 95% CIs using data from the same individual for baseline, post, and follow-up (weeks zero, 6, and 18) assessments. Demographics such as ethnicity, work status, marital status, and initial psychological distress were included as covariates in the random effect model. We explored moderation effects of initial psychological distress severity at baseline, gender-based violence exposure, exposure to trauma, and length of stay in the refugee camp. These moderation analyses involved inclusion of interaction terms (intervention status × moderator variable) in linear mixed-effects models.
Role of the funding source
The funders did not have a role in the research design; collection, analysis, or interpretation of data; writing the Article; nor the decision to submit for publication. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
After screening of 22 clusters containing 712 individuals, two clusters and 18 individuals were excluded. Two clusters were excluded because the village leaders refused participation; five participants (1%) were excluded for not meeting the moderate psychological distress inclusion criterion. Eight participants (1%) met exclusion criteria (seven for being at imminent risk of suicide and one for potential psychosis), and five declined to participate in screening. This left 694 individuals who met inclusion criteria and who were allocated to either Self-Help Plus (n=331) or enhanced usual care (n=363; figure). We could not interview 34 participants (5%) at the immediate post-intervention assessment and 36 participants (5%) at the 3-month post-intervention assessment. Most of these participants were lost to follow-up because they moved location. Participants lost to follow-up were similar in number across study groups, and attrition was not significantly related to study condition, marital status, work status, or education.
Sociodemographic characteristics are shown in table 1. Study conditions were largely similar with regard to sociodemographics and baseline scores on outcomes, with the exception of ethnicity and length of time in refugee settlement. We included both as covariates in effectiveness analyses. Mean participant age was 30·9 years (SD 10·9). Close to two-thirds (60%) were married, for about half (49%) primary school was the highest received level of education, and about half (49%) of the sample were of Kakwa ethnicity. Most women were either homemakers (46%) or unemployed (35%). The most commonly mentioned adversities from the Harvard Trauma Questionnaire were lack of food or clean water (n=643, 93%), lacking shelter (n=609, 88%), and losing a family member to violence (n=580, 84%). In this sample, 182 women (26%) reported lifetime physical violence perpetrated by an intimate partner, 70 (10%) reported sexual violence by an intimate partner, 167 (24%) women reported physical violence by someone other than their partner, and 46 (7%) reported sexual violence by someone other than their partner. The primary outcome, psychological distress, correlated as expected with other variables, indicating discriminant and convergent validity (appendix pp 4–5). With regard to safety considerations, the independent data safety management board responded to six adverse events, and none were evaluated to be concerns in response to the intervention.
Table 1:
Demographic characteristics
| Total (N=694) | Intervention (n=331) | Enhanced usual care (n=363) | |
|---|---|---|---|
| Age, years | 30·9 (10·9) | 30·9 (10·3) | 31·0 (11·4) |
|
| |||
| Education | |||
| No schooling | 205 (30%) | 98 (30%) | 107 (29%) |
| Primary school | 338 (49%) | 158 (48%) | 180 (50%) |
| Secondary and higher | 134 (19%) | 62 (19%) | 72 (20%) |
| Missing | 17 (3%) | 13 (4%) | 4 (1%) |
|
| |||
| Ethnicity | |||
| Kakwa | 337 (49%) | 151 (46%) | 186 (51%) |
| Dinka | 68 (10%) | 65 (20%)* | 3 (1%)* |
| Nuer | 43 (6%) | 20 (6%) | 23 (6%) |
| Other | 227 (33%) | 81 (25%)* | 146 (40%)* |
| Missing | 19 (3%) | 14 (4%) | 5 (1%) |
|
| |||
| Marital status | |||
| Single or never married | 260 (38%) | 121 (37%) | 139 (38%) |
| Married or living as married | 418 (60%) | 197 (60%) | 221 (61%) |
| Missing | 16 (2%) | 13 (4%) | 3 (1%) |
|
| |||
| Occupation | |||
| Paid work | 10 (1%) | 6 (2%) | 4 (1%) |
| Self-employed | 43 (6%) | 23 (7%) | 20 (6%) |
| Farming | 46 (7%) | 23 (7%) | 23 (6%) |
| Student | 5 (1%) | 2 (1%) | 3 (1%) |
| Homemaker | 318 (46%) | 149 (45%) | 169 (47%) |
| Retired | 1 (<1%) | 1 (<1%) | 0 (0%) |
| Unemployed | 245 (35%) | 111 (34%) | 134 (37%) |
| Other | 10 (1%) | 3 (1%) | 7 (2%) |
| Missing | 16 (2%) | 13 (4%) | 3 (1%) |
|
| |||
| Time in refugee settlement | |||
| <6 months | 237 (34%) | 153 (46%) | 84 (23%) |
| 6 months to 1 year | 196 (28%) | 76 (23%)* | 120 (33%)* |
| >1 year | 261 (38%) | 102 (31%)* | 159 (44%)* |
Data are mean (SD) or n (%).
Significant p value (ie, p<0·05) for a χ2 test of significant difference between study conditions.
Differences between study conditions on trajectories of the outcome measures are presented in table 2. With regard to the primary outcome, Self-Help Plus led to significantly greater reductions in psychological distress immediately after intervention (β −3·25, 95% CI −4·31 to −2·19; p<0·0001; d −0·72) and 3 months after intervention relative to the enhanced usual care (β −1·20, −2·33 to −0·08; p=0·04; d −0·26). The 3-month effect (our primary endpoint) was not moderated by gender-based violence exposure, exposure to trauma, length of stay in settlement, or levels of initial psychological distress (appendix pp 6–13).
Table 2:
Summary statistics and results from linear mixed-effects models
| Intervention | Enhanced usual care | Mixed-model analysis | p value | Effect size | |
|---|---|---|---|---|---|
| Primary outcome | |||||
|
| |||||
| K6 score (0–24) | |||||
| Baseline | 16·5 (4·1) | 16·8 (4·2) | .. | .. | .. |
| Post treatment | 10·4 (4·9) | 13·5 (4·8) | −3·25 (−4·31 to −2·19) | <0·0001 | −0·72 |
| Follow-up | 10·5 (4·5) | 12·0 (4·9) | −1·20 (−2·33 to −0·08) | 0·04 | −0·26 |
|
| |||||
| Secondary outcomes | |||||
|
| |||||
| PSYCHLOPS score (0–20) | |||||
| Baseline | 17·2 (2·8) | 16·9 (3·4) | .. | .. | .. |
| Post treatment | 12·2 (5·2) | 14·7 (4·6) | −2·79 (−4·07 to −1·51) | <0·0001 | −0·58 |
| Follow-up | 12·1 (4·9) | 13·1 (4·8) | −1·17 (−2·37 to 0·04) | 0·06 | −0·25 |
| PCL-6 score (6–30) | |||||
| Baseline | 22·0 (4·7) | 21·8 (4·8) | .. | .. | .. |
| Post treatment | 16·1 (5·5) | 19·2 (5·5) | −3·53 (−4·67 to −2·38) | <0·0001 | −0·68 |
| Follow-up | 16·1 (4·9) | 17·7 (5·8) | −1·55 (−2·87 to −0·24) | 0·02 | −0·30 |
| PHQ-9 score (0–27) | |||||
| Baseline | 15·1 (4·7) | 15·1 (4·8) | .. | .. | .. |
| Post treatment | 9·7 (5·4) | 12·8 (5·3) | −3·78 (−5·39 to −2·17) | 0·0003 | −0·75 |
| Follow-up | 9·5 (4·2) | 10·8 (5·1) | −1·46 (−2·77 to − 0·15) | 0·03 | −0·31 |
| Explosive anger* (4–16) | |||||
| Baseline | 79 (25·0) | 97 (27·1) | .. | .. | .. |
| Post treatment | 49 (15·8) | 99 (28·5) | 0·50 (0·32 to 0·50) | 0·002 | 0·50 |
| Follow-up | 42 (14·4) | 83 (24·9) | 0·63 (0·40 to 1·0) | 0·04 | 0·63 |
| Interethnic relationship score (3–12) | |||||
| Baseline | 7·5 (2·6) | 7·7 (2·3) | .. | .. | .. |
| Post treatment | 7·2 (2·6) | 7·5 (2·3) | −0·14 (−0·47 to 0·19) | 0·37 | −0·06 |
| Follow-up | 6·6 (3·0) | 7·2 (2·8) | −0·19 (−0·56 to 0·19) | 0·30 | −0·07 |
| AAQ-II score (7–49) | |||||
| Baseline | 21·9 (8·8) | 20·9 (7·9) | .. | .. | .. |
| Post treatment | 29·6 (10·1) | 25·0 (9·6) | 4·49 (0·90 to 8·09) | 0·02 | 0·42 |
| Follow-up | 30·2 (9·4) | 27·1 (9·0) | 1·11 (−4·26 to 6·48) | 0·66 | 0·09 |
| WHODAS 2.0 (0–48) | |||||
| Baseline | 23·9 (8·7) | 23·8 (8·4) | .. | .. | .. |
| Post treatment | 15·3 (8·5) | 20·7 (9·6) | −6·10 (−7·86 to −4·34) | <0·0001 | −0·77 |
| Follow-up | 15·0 (7·8) | 17·3 (9·0) | −2·52 (−5·01 to −0·03) | 0·05 | −0·30 |
| WHO-5 (0–25) | |||||
| Baseline | 7·3 (5·1) | 7·9 (5·3) | .. | .. | .. |
| Post treatment | 11·9 (6·1) | 9·5 (5·7) | 2·89 (1·52 to 4·27) | 0·0006 | 0·51 |
| Follow-up | 11·9 (5·7) | 10·4 (5·4) | 1·94 (0·81 to 3·06) | 0·0028 | 0·36 |
Data are mean (SD) or regression coefficients (95% CI).
K6=Kessler 6. PSYCHLOPS=Psychological Outcome Profiles instrument. PCL-6=PTSD Checklist-Civilian 6-item version. PHQ-9=Patient Health Questionnaire 9-item version. AAQ-II=Acceptance and Action Questionnaire version II. WHODAS 2.0=WHO Disability Assessment Schedule 2.0. WHO-5=WHO-5 Wellbeing Index.
Presence or not of explosive anger attacks, reported as odds ratio.
Self-Help Plus, compared with enhanced usual care, was also associated with larger improvements 3 months after intervention for the secondary outcomes of post-traumatic stress and depression symptoms, explosive anger, functional impairment, and subjective wellbeing, with effect sizes ranging from −0·30 to −0·36. For two secondary outcomes (ie, personally identified problems and psychological flexibility), significant intervention benefits were identified immediately after intervention, but not 3 months after intervention. There were no differences in interethnic relations (secondary outcome) either immediately after or 3 months after intervention.
None of the intervention effects at 3 months were moderated by violence exposure, length in settlement, or baseline levels of psychological distress (appendix p 6–13).
Assessment of more than 10% of Self-Help Plus sessions showed near-perfect fidelity: two minor mistakes across all eight observed groups were identified (a delay in restarting the audio and taking more time for smaller group discussion than allotted in the manual). Participation in the intervention was consistently high. Of the 331 individuals randomly assigned to Self-Help Plus, 293 (89%) participated in the first session. Participation dropped slightly at the second session, but remained stable and high (session 2, n=267 [81%]; session 3, n=272 [82%]; session 4, n=279 [84%]; and session 5, n=265 [80%]). We did not find evidence that masking of assessors was compromised: assessors correctly guessed the study condition of clusters 35% of the time (18 assessors guessed the study group for 14 villages, and correctly guessed 87 out of 252 observations). Semistructured interviews with 52 participants after the 3-month follow-up did not indicate exposure to intervention materials in control villages.
Our aim was to assess the effect of a highly scalable intervention that has the potential to rapidly reach larger groups of people in settings of mass adversity. To aid interpretability and ability to compare study results with evidence from past studies evaluating more resource-intensive psychotherapeutic interventions, we did the following post-hoc (non-specified) analyses (appendix pp 14–16).
First, we were interested in understanding intervention effects on participants with severe psychological distress (ie, scoring 13 or higher on the K6, which in studies done in other settings14 indicates a high likelihood of having a serious mental disorder causing functional limitations requiring treatment) as opposed to moderate levels of psychological distress (scores 5–12). We found that the majority of participants in this study met criteria for severe psychological distress (582 [84%] of 694). Immediately after intervention, 209 (58%) of 363 participants in the control condition, compared with 110 (33%) of 331 in the Self-Help Plus condition, continued to score 13 or more. This difference was also observed at the 3-month assessment, although it was smaller (n=174 [48%] vs n=130 [39%], respectively).
Second, we calculated the minimally important difference by comparing the proportions of participants in both study conditions showing positive changes of more than 0·5 SDs.41 We found a statistically significant difference between study conditions in favour of Self-Help Plus with regard to the proportion of participants achieving a minimally important difference between baseline and 3-month follow-up (Pearson χ2 9·63; p=0·022). For the primary outcome, psychological distress, this appears to be mainly a function of a larger group of people who deteriorate in the control condition (n=58 [16%]) versus Self-Help Plus condition (n=30 [9%]). We also found statistically significant differences in minimally important difference in favour of the Self-Help Plus condition for post-traumatic stress (Pearson χ2 26·58, p<0·0001) and depression symptoms (Pearson χ2 10·47, p=0·015). For post-traumatic stress symptoms, the difference appeared to be driven by a larger proportion of participants in the Self-Help Plus condition who improved (n=203 [61%] vs n=182 [50%]) and a smaller group of participants in the Self-Help Plus condition who deteriorated (n=35 [11%] vs n=76 [21%]). For depression, the difference appeared to be associated with a smaller group of participants who deteriorated in the Self-Help Plus condition (n=48 [15%] vs n=74 [20%]).
Discussion
We evaluated an intervention designed to overcome major obstacles to providing evidence-based mental health support at scale for conflict-affected populations. In low-resource settings, rapidly reaching large groups of people with evidence-based psychotherapies is inhibited by the resources required to train and adequately supervise a clinical workforce; challenges in maintaining fidelity to intervention manuals; the need to address psychological distress experienced by people with and without diagnosable mental disorders; and size of the affected population.4 The intervention attempted to meet these challenges by further innovation in the area of task sharing and intervention delivery (ie, decreasing requirements for training and supervision while delivering excellent intervention fidelity through use of audio recordings and a self-help book); targeting psychological distress regardless of whether people meet criteria for diagnosable mental disorders; and tripling the number of participants reached per session. To the best of our knowledge, this study is the first cRCT of a guided self-help intervention in a low-resource humanitarian setting.
In line with our hypotheses, compared with the control group, we found larger improvements at the 3-month post-intervention assessment in the Self-Help Plus group for the primary outcome of psychological distress and five of eight secondary outcomes. Identified effects were robust—ie, not moderated by trauma and gender-based violence exposure, length of time in settlement, or baseline levels of distress. Identified effect sizes were similar to psychoeducational courses evaluated in adversity-affected populations living in high-income countries (eg, the coping with depression course has a pooled effect size of d 0·28),20 and some transdiagnostic interventions in conflict-affected low-resource settings.12 Screening for moderate psychological distress resulted in neglible exclusion and de-facto implementation of Self-Help Plus as a universal intervention in these refugee settlements. Because of the diversity of mental health conditions in universally targeted populations, such interventions commonly have smaller effect sizes, but have greater feasibility and reach. Post-hoc analyses identified that the large majority of participants scored above the cutoff for severe psychological distress at baseline, and that a larger percentage of participants in the Self-Help Plus condition were below this level compared with the control condition at 3 months post intervention. Moreover, we found a pattern of larger minimally significant deterioration in the control condition compared with the Self-Help Plus condition for psychological distress, post-traumatic stress, and depression symptoms at 3 months post intervention. This is important to note, given the high level of continued stressors experienced by South Sudanese refugees in northern Uganda, including continued political instability in South Sudan, restrictions in access to basic needs, and gender-based violence (eg, intimate partner violence).
We note several limitations of the study. First, followup assessment was done 3 months after intervention. Long-term assessments would be helpful to understand benefits over time. Nonetheless, alleviation of suffering is a widely accepted objective of humanitarian action, and Self-Help Plus offers sizeable immediate effects. Second, our psychological distress measure had a lower than acceptable internal consistency of 0·65, indicating it might tap into multiple types of mental health phenomena rather than one unified concept, which might hamper consistent interpretation of change over time. Third, we did not control for frequency of contact with service providers between study conditions. Fourth, we randomised a limited number of clusters. Although we did not identify differences between study conditions at baseline, it is possible that clusters differed on unmeasured variables. Fifth, our study focused on female refugees, which has important implications for generalisability. Women are an important group in conflict-affected settings given their high exposure to systematic and gendered adversities, but it will also be crucial to understand how male mental health needs can be addressed.
Taken together, our findings indicate that Self-Help Plus might be well suited as a first-line intervention for large populations exposed to major stressors in low-resource settings. Where feasible, this intervention should be implemented within a stepped-care framework, where those for whom Self-Help Plus is not sufficient are offered a more potent intervention. Following WHO’s model of the optimal mix of mental health services,42 Self-Help Plus would fill an important role to strengthen self-care and informal community care. The moderation results suggest that the intervention benefits populations similarly across different trauma histories and levels of distress. Given these positive results, WHO will make the Juba Arabic version of Self-Help Plus publicly available, and will make the English version available after replication of this study.
Our findings raise several questions for future research. First, as with resource-intensive psychological treatments in humanitarian settings,3 it is important to understand why effect sizes reduce over time. A Cochrane review of psychological treatments—mostly consisting of relatively higher resource-intensive interventions—in humanitarian settings in low-income and middle-income countries found a drop in effect size for post-traumatic stress disorder symptoms from −1·07 immediately after treatment (16 studies), to −0·49 at 1–3 months after intervention (18 studies), and −0·37 at 6 months after intervention (five studies).3 Currently, there is little knowledge on whether these drops in effect sizes are due to intervention-related processes (eg, a loss of gained skills over time or a return to previous behaviour patterns), or context-related processes (eg, new or continued adversities associated with renewed psychological distress). Studies could explore whether booster sessions or integration within humanitarian programming aimed at addressing critical stressors (eg, poverty or gender-based violence) might assist in maintaining benefits. Second, a related question concerns how Self-Help Plus might have achieved its effects—ie, the mechanisms of change. Research on this topic would also assist in situating this third-wave intervention vis a vis cognitive behavioural treatment elements more commonly tested in humanitarian settings. Such research could consist of detailed mediation analyses, as well as an effort to understand participants’ own perspectives regarding identified benefits. Third, future research should address how Self-Help Plus delivery might be optimised for large-scale use in low-resource contexts (eg, through integration with primary health care, specialised mental health services, or stepped-care models). An important question for all psychological interventions tested in controlled research settings concerns how quality of implementation and monitoring of safety concerns can be guaranteed as part of routine service delivery. Additional questions concern whether Self-Help Plus might be an effective preventive intervention, and the cost-effectiveness of Self-Help Plus compared with established evidence-based psychotherapies.
In conclusion, among South Sudanese female refugees, a self-help intervention with enhanced usual care resulted in larger improvements in psychological distress, PTSD and depression symptoms, explosive anger, functional impairment, and subjective wellbeing at 3 months post intervention compared with enhanced usual care.
Supplementary Material
Research in context.
Evidence before this study
A meta-analysis of studies with populations affected by humanitarian crises in low-income and middle-income countries highlighted the potential that psychological therapies offer for reducing symptoms of post-traumatic stress disorder (16 trials; low-quality evidence), depression (14 trials; low-quality evidence), and anxiety (five studies; low-quality evidence).
Added value of this study
There is an opportunity to scale up existing evidence-based psychological therapies in humanitarian settings in low-income and middle-income countries by adapting them in innovative ways. This is, to the best of our knowledge, the first cluster randomised controlled trial evaluating the effectiveness of an innovative, facilitator-guided, group-based, self-help intervention. The intervention (Self-Help Plus) can be rapidly taught to non-specialist providers (ie, those without specialised mental health training), and is delivered to large groups of people in workshops through audio recordings and an illustrated self-help book. Compared with controls, Self-Help Plus was associated with higher levels of improvements on psychological distress, functioning, and wellbeing outcomes 3 months after the intervention.
Implications of all the available evidence
Guided self-help appears to be a promising first-line strategy for mental health support, that can be delivered rapidly to large groups of people in low-resource humanitarian settings.
Acknowledgments
This project is funded by the Research for Health in Humanitarian Crises (R2HC) Programme, managed by ELRHA. The authors alone are responsible for the views expressed in this Article and they do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated.
Footnotes
Declaration of interests
We declare no competing interests.
Data sharing
De-identified data and a data dictionary will be made available for individual patient data meta-analyses with publication of the trial after approval of a proposal and signed data access agreement (wtol@jhu.edu, vanommerenm@who.int).
References
- 1.Charlson F, van Ommeren M, Flaxman A, Cornett J, Whiteford H, Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet 2019; 394: 240–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tol WA, Barbui C, Galappatti A, et al. Mental health and psychosocial support in humanitarian settings: linking practice and research. Lancet 2011; 378: 1581–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Purgato M, Gastaldon C, Papola D, van Ommeren M, Barbui C, Tol WA. Psychological therapies for the treatment of mental disorders in low- and middle-income countries affected by humanitarian crises. Cochrane Database Syst Rev 2018; 7: CD011849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tol WA, Barbui C, Bisson J, et al. World Health Organization guidelines for management of acute stress, PTSD, and bereavement: key challenges on the road ahead. PLoS Med 2014; 11: e1001769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bass JK, Annan J, McIvor Murray S, et al. Controlled trial of psychotherapy for Congolese survivors of sexual violence. N Engl J Med 2013; 368: 2182–91. [DOI] [PubMed] [Google Scholar]
- 6.Weiss WM, Murray LK, Zangana GA, et al. Community-based mental health treatments for survivors of torture and militant attacks in Southern Iraq: a randomized control trial. BMC Psychiatry 2015; 15: 249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rahman A, Hamdani SU, Awan NR, et al. Effect of a multicomponent behavioral intervention in adults impaired by psychological distress in a conflict-affected area of Pakistan: a randomized clinical trial. JAMA 2016; 316: 2609–17. [DOI] [PubMed] [Google Scholar]
- 8.Silove D, Ventevogel P, Rees S. The contemporary refugee crisis: an overview of mental health challenges. World Psychiatry 2017; 16: 130–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Jong JT, Komproe IH, Van Ommeren M. Common mental disorders in postconflict settings. Lancet 2003; 361: 2128–30. [DOI] [PubMed] [Google Scholar]
- 10.Murray LK, Dorsey S, Haroz E, et al. A common elements treatment approach for adult mental health problems in low and middle income countries. Cognit Behav Pract 2014; 21: 111–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dawson KS, Bryant RA, Harper M, et al. Problem Management Plus (PM+): a WHO transdiagnostic psychological intervention for common mental health problems. World Psychiatry 2015; 14: 354–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Betancourt TS, McBain R, Newnham EA, et al. A behavioral intervention for war-affected youth in Sierra Leone: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry 2014; 53: 1288–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee YY, Stockings EA, Harris MG, et al. The risk of developing major depression among individuals with subthreshold depression: a systematic review and meta-analysis of longitudinal cohort studies. Psychol Med 2018; 49: 1–11. [DOI] [PubMed] [Google Scholar]
- 14.Prochaska JJ, Sung HY, Max W, Shi Y, Ong M. Validity study of the K6 scale as a measure of moderate mental distress based on mental health treatment need and utilization. Int J Methods Psychiatr Res 2012; 21: 88–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stark L, Ager A. A systematic review of prevalence studies of gender-based violence in complex emergencies. Trauma Violence Abuse 2011; 12: 127–34. [DOI] [PubMed] [Google Scholar]
- 16.Bolton P, Bass J, Betancourt T, et al. Interventions for depression symptoms among adolescent survivors of war and displacement in northern Uganda: a randomized controlled trial. JAMA 2007; 298: 519–27. [DOI] [PubMed] [Google Scholar]
- 17.Tol WA, Stavrou V, Greene MC, Mergenthaler C, van Ommeren M, García Moreno C. Sexual and gender-based violence in areas of armed conflict: a systematic review of mental health and psychosocial support interventions. Confl Health 2013; 7: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prabhakaran D, Anand S, Watkins DA, et al. Cardiovascular, Respiratory, and related disorders: key messages from Disease Control Priorities, 3rd edn. Lancet 2018; 391: 1224–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Epping-Jordan JE, Harris R, Brown FL, et al. Self-Help Plus (SH+): a new WHO stress management package. World Psychiatry 2016; 15: 295–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cuijpers P, Muñoz RF, Clarke GN, Lewinsohn PM. Psychoeducational treatment and prevention of depression: the “Coping with Depression” course thirty years later. Clin Psychol Rev 2009; 29: 449–58. [DOI] [PubMed] [Google Scholar]
- 21.Cuijpers P, Donker T, van Straten A, Li J, Andersson G. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychol Med 2010; 40: 1943–57. [DOI] [PubMed] [Google Scholar]
- 22.Tol WA, Augustinavicius J, Carswell K, et al. Translation, adaptation, and pilot of a guided self-help intervention to reduce psychological distress in South Sudanese refugees in Uganda. Glob Ment Health 2018; 5: e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tol WA, Augustinavicius J, Carswell K, et al. Feasibility of a guided self-help intervention to reduce psychological distress in South Sudanese refugee women in Uganda. World Psychiatry 2018; 17: 234–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brown FL, Carswell K, Augustinavicius J, et al. Self Help Plus: study protocol for a cluster-randomised controlled trial of guided self-help with South Sudanese refugee women in Uganda. Glob Ment Health 2018; 5: e27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hayes SC, Villatte M, Levin M, Hildebrandt M. Open, aware, and active: contextual approaches as an emerging trend in the behavioral and cognitive therapies. Annu Rev Clin Psychol 2011; 7: 141–68. [DOI] [PubMed] [Google Scholar]
- 26.Stockton D, Kellett S, Berrios R, Sirois F, Wilkinson N, Miles G. Identifying the underlying mechanisms of change during Acceptance and Commitment Therapy (ACT): a systematic review of contemporary mediation studies. Behav Cogn Psychother 2019; 47: 332–62. [DOI] [PubMed] [Google Scholar]
- 27.Hacker T, Stone P, MacBeth A. Acceptance and commitment therapy—Do we know enough? Cumulative and sequential meta-analyses of randomized controlled trials. J Affect Disord 2016; 190: 551–65. [DOI] [PubMed] [Google Scholar]
- 28.French K, Golijani-Moghaddam N, Schroder T. What is the evidence for the efficacy of self-help acceptance and commitment therapy? A systematic review and meta-analysis. J Contextual Behav Sci 2017; 6: 360–74. [Google Scholar]
- 29.Stewart C, White RG, Ebert B, Mays I, Nardozzi J, Bockarie H. A preliminary evaluation of Acceptance and Commitment Therapy (ACT) training in Sierra Leone. J Contextual Behav Sci 2016; 5: 16–22. [Google Scholar]
- 30.White RG, Gregg J, Batten S, Hayes LL, Kasujja R. Contextual behavioral science and global mental health: synergies and opportunities. J Contextual Behav Sci 2017; 6: 245–51. [Google Scholar]
- 31.Rees B, Travis F, Shapiro D, Chant R. Significant reductions in posttraumatic stress symptoms in Congolese refugees within 10 days of transcendental meditation practice. J Trauma Stress 2014; 27: 112–15. [DOI] [PubMed] [Google Scholar]
- 32.Adaku A, Okello J, Lowry B, et al. Mental health and psychosocial support for South Sudanese refugees in northern Uganda: a needs and resource assessment. Confl Health 2016; 10: 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.van Ommeren M, Sharma B, Thapa SB, et al. Preparing instruments for transcultural research: use of the Translation Monitoring Form with Nepali-speaking Bhutanese refugees. Transcult Psychiatry 1999; 36: 285–301. [Google Scholar]
- 34.Kessler RC, Green JG, Gruber MJ, et al. Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res 2010; 19 (suppl 1): 4–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ashworth M, Robinson SI, Godfrey E, et al. Measuring mental health outcomes in primary care: the psychometric properties of a new patient-generated outcome measure, ‘PSYCHLOPS’ (‘psychological outcome profiles’). Primary Care Mental Health 2005; 3: 261–70. [Google Scholar]
- 36.Lang AJ, Wilkins K, Roy-Byrne PP, et al. Abbreviated PTSD Checklist (PCL) as a guide to clinical response. Gen Hosp Psychiatry 2012; 34: 332–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Silove D, Mohsin M, Tay AK, et al. Six-year longitudinal study of pathways leading to explosive anger involving the traumas of recurrent conflict and the cumulative sense of injustice in Timor-Leste. Soc Psychiatry Psychiatr Epidemiol 2017; 52: 1281–94. [DOI] [PubMed] [Google Scholar]
- 38.Bond FW, Hayes SC, Baer RA, et al. Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: a revised measure of psychological inflexibility and experiential avoidance. Behav Ther 2011; 42: 676–88. [DOI] [PubMed] [Google Scholar]
- 39.Ustun TB, Kostanjsek S, Chatterji S, Rehm J. Measuring health and disability: manual for WHO Disability Assessment Schedule (WHODAS 2·0). Geneva: World Health Organization, 2010. [Google Scholar]
- 40.Topp CW, Østergaard SD, Søndergaard S, Bech P. The WHO-5 Well-Being Index: a systematic review of the literature. Psychother Psychosom 2015; 84: 167–76. [DOI] [PubMed] [Google Scholar]
- 41.Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 2003; 41: 582–92. [DOI] [PubMed] [Google Scholar]
- 42.WHO. The optimal mix of services for mental health. Geneva: World Health Organization, 2007. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


