Abstract
Purinergic receptors (PRs) have been reported as potential therapeutic targets for many viral infections including herpesviruses, which urges the investigation into their role in Marek’s disease (MD), a herpesvirus induced cancer in chickens that is an important pathogen for the poultry industry. MD is caused by MD virus (MDV) that has a similar viral life cycle as human varicella zoster virus in that it is shed from infected epithelial skin cells and enters the host through the respiratory route. In this report, PR responses during natural MDV infection and disease progression was examined in MD-resistant white Leghorns (WL) and MD-susceptible Pure Columbian (PC) chickens during natural infection. Whole lung lavage cells (WLLC) and liver tissue samples were collected from chickens infected but showing no clinical signs of MD (Infected) or presenting with clinical disease (Diseased). RNA was extracted followed by RT-qPCR analysis with gene specific primers against members of the P1, P2X, and P2Y PR families. Differential expression (p < 0.05) was observed in breed and disease conditions. Some PRs showed tissue specific expression (P1A1, P2X1, and P2X6 in WLLC) whereas others responded to MDV infection only in MD-susceptible (PC) chickens (P1A2A, P2X1, P2X5, P2X7). P2Y PRs had differential expression in both chicken lines in response to MDV infection and MD progression. This study is the first to our knowledge to examine PR responses during MDV infection and disease progression. These results suggest PR signaling may an important area of research for MDV replication and MD.
Subject terms: Virology, Herpes virus, Viral host response
Introduction
Marek’s disease (MD) is a highly contagious disease of chickens, caused by Marek’s disease herpesvirus (MDV) or Gallid alphaherpesvirus 21. MD has been partially controlled since 1969 through widespread use of vaccines that reduce lymphoma and viral replication but do not prevent viral shedding and spread within a flock2. The estimated economic impact of the prevention measures of MDV on the global poultry industry costs more than a billion US$ annually3. MDV infection is initiated through the respiratory route either by direct bird to bird contact or indirectly by inhalation of dust and dander from birds shedding infected virus4. The main target cells for MDV infection are associated with the host immune system (i.e., B and T lymphocytes, and macrophages) that results in notable release of different cytokines, especially during the primary and reactivation phases of infection5. Differences in genetic resistance to MD was first reported over 80 years ago6 resulting in selection and breeding of chickens for relative resistance and susceptibility to MD over time7.
In addition to acting as an energy source and the building blocks of nucleic acids, ATP, and its metabolites (ADP, cAMP, adenosine), have long been accepted as extracellular signaling molecules (eATP) in both physiological and pathological conditions. Infected or damaged cells release eATP into the extracellular environment of the damaged cells as a “find me signal”8,9. This eATP response counters bacterial, fungal, or viral infections by acting as autocrine and paracrine molecules on the cells responsible for its release and neighboring cells. After release into the extracellular environment, these purines (ATP and its metabolites) bind to a distinct class of membrane bound receptors collectively known as the purinergic receptors (PRs)8. These receptors are ubiquitously expressed in cells, including the target cells of MDV, and are key players of a wide array of biological processes, including neuromodulation, inflammation, endothelial-mediated vasodilatation, cell migration, wound healing, cell proliferation, differentiation, and apoptosis10. This vast PR family has been divided into P1 and P2 based on their binding ability to either adenosine or ATP/UTP, respectively. P1 receptors are comprised of four subfamilies (A1, A2A, A2B, and A3), while P2 receptors are divided into two subfamilies, P2X and P2Y, which are further divided into P2X (1–7) channels, activated by ATP, and G protein-coupled metabotropic P2Y (1–14) receptors11–13. Most of these receptors have been identified in chickens, at least at the genomic level. In addition to the above classifications and subdivisions, purinergic responses can be either early (short) or late (long) acting based on the infection and physiological condition of host14.
The activation of PRs can be either pro- or anti-infection15. Chen et al.16, recently demonstrated that the P2Y2 receptor increases replication of human cytomegalovirus (HCMV), while P2X5 inhibited HCMV replication. Similar differential response patterns have been seen where P2X7R activation enhances immune killing of tumor cells17, while A2BR signaling contributes to immunosuppression in tumors18. Zhang and colleagues19 demonstrated that P2Y13 is a potential antiviral target to restrict the replication of different types of viruses including Newcastle disease virus (NDV) and herpes simplex virus 1 (HSV1). The differential expression of PRs has previously been observed in other pathological conditions20,21. All this information, in combination with the clinical manifestation of MD and the functional changes induced in target cells (B and T cells) suggests potential roles for PRs (P1 and P2) in MD pathogenesis. Only a few studies have reported on the expression of PRs in response to herpesvirus infection11,16,22, and thus far no papers have been published on MDV and PRs.
MDV is a global economic threat to the poultry industry, but we still lack considerable understanding of pathophysiological mechanisms involved in MD. Current vaccines reduce replication and lymphoma development, but do not induce sterilizing protection23. Keeping in view that in-depth understanding of the parameters and signaling pathways involved in disease development are key points in developing better antiviral therapies24. The recent finding that P2Y2 and P2X5 are involved in controlling HCMV replication16 suggests PRs may play a role other herpesvirus infections, including MD. We hypothesize that: (1) PR expression is significantly changed during MDV infection in chickens; (2) the genetic background of the host chicken plays an important role in PR regulation, and (3) the regulation of these receptors is linked to disease progression and severity. To address this research gap, we used the natural MDV-chicken model to measure PRs mRNA responses during herpesvirus replication and disease progression. The respiratory tract is the natural route of entry for MDV where the virus initially infects pulmonary macrophages and B cells25, therefore whole lung lavage cells (WLLC) samples were used in our study, in addition to liver samples due to their importance as a major metabolic organ. Our results reveal differential PRs responses to MDV infection and disease progression when comparing both tissues and breed of chicken.
Materials and methods
Cell culture
All cells were maintained in humified atmosphere of 5% CO2 at 38 °C. Chick embryo cells (CECs) were prepared as reported earlier26. DF-1-Cre cells and have been previously described27 and were maintained in LM-based media with Zeocin28.
Generation of rMDV (v2001)
A dually fluorescent recombinant (r)MDV was generated using two fluorescent markers previously shown to have no effect on MDV replication29,30. Briefly, the coding sequence of the eGFP gene was inserted in frame at the C-terminus of the MDV UL47 gene by two-step Red-mediated mutagenesis31 in the previously described rMDV termed rRLORF4mRFP28 bacterial artificial chromosome (BAC) clone exactly as previously described30. The BAC clone was named 2001. All BAC clones were confirmed by restriction fragment length polymorphism analysis, analytic PCR, and DNA sequencing (Data not shown). Recombinant viruses (designated with a “v”) were reconstituted by transfecting DF-1-Cre cells using Lipofectamine reagent (Thermo Fisher) and then passaged directly into CECs and used at ≤ 5 passages for in vitro and in vivo studies.
Immunofluorescence assays (IFAs)
CECs were infected with reconstituted viruses in 6-well tissue culture plates at 100 plaque-forming units (PFU) per well. At 5 days post-infection (dpi), cells were fixed with PFA buffer (2% paraformaldehyde, 0.1% Triton X-100) for 15 min and then washed twice with PBS. The plaques were fluorescent red and green but for double confirmation the fixed cells also were stained with anti-MDV chicken sera plus goat anti-chicken IgY-Alexa Fluor 488 secondary antibody (Molecular Probes, Eugene, OR, USA). The virus plaques were observed using an EVOS FL Cell Imaging System (Thermo Fisher Scientific, Waltham, MA, USA) and compiled using Adobe Photoshop version 21.0.1.
Plaque size assays (PSA)
Plaque areas were measured in CECs exactly as previously described32 using anti-MDV chicken sera and goat anti-chicken IgY-Alexa Fluor 488 secondary antibody (Molecular Probes, Eugene, OR). Digital images of 36 individual plaques were collected using Nikon Eclipse-Ti-E inverted fluorescent microscope and plaque areas were measured using ImageJ33 version 1.41o software. Whisker plots were generated using Microsoft Excel 365 and significant differences were determined using IBM SPSS Statistics Version 28 software Package (https://www.ibm.com/analytics/spss-statistics-software).
Testing virulence of v2001 in chickens
Commercial SPF White Leghorn (WL) chickens were obtained from Hy-Line International (Dallas Center, Iowa) and were from MD-vaccinated parents (maternal antibody positive. Eighteen-day old chicks were inoculated intraabdominally with 1000 plaque forming units (PFU) of vRLORF4mRFP, vUL47eGFP, or v2001 in separate rooms for each group. An additional five chickens were left uninfected to act as contact controls to confirm each virus was able to transmit to uninfected chickens. Chickens were evaluated daily for symptoms of MD and euthanized when birds showed clinical signs of MD (e.g., lethargy, depression, paralysis, etc.) plus examined for gross MD lesions. Chickens positive for MD included birds succumbing to disease prior to the experimental termination date and birds positive for MD-related lesions at termination of the experiment. Fisher’s exact tests were used to determine statistical differences between groups of chickens for MD incidence at a significance level of p < 0.05.
Experimental approach for measuring PR responses
Day old chickens from two different chicken lines [Pure Columbian (PC); Susceptible (n = 60) and WL; Resistant (n = 60)] were purchased from the UIUC Poultry Research Farm. The major histocompatibility complex (MHC) haplotype for PC birds is not defined, but suggested to be B6-like, while WL are B2/B1234. Both chicken lines were housed in separate rooms. MDV is strictly cell-associated during cell culture propagation; therefore, we utilized our established experimental and natural infection model35 with some minor modifications. Briefly, three-days old chicks (n = 12 per chicken line) were “experimentally infected” by intraabdominal inoculation of 2,000 PFU of v2001 that mimics disease progression but bypasses the natural respiratory route. For “natural infection,” age-matched, naïve contact (n = 8 per chicken line) chickens from the same breed were also housed with experimentally infected chickens. Approximately 2 weeks after experimental infection, chickens shed infectious virus that can then infect naïve contact chickens, constituting natural infection. Another two sets (one per chicken line) of age-matched uninfected chickens (n = 4) were kept in two separate rooms to be used as uninfected control groups (Fig. 1).
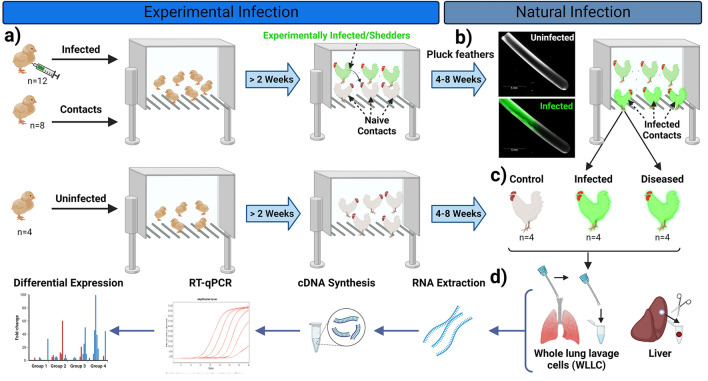
Figure 1.
Experimental approach. (a) Day old PC (n = 12) and WL (n = 12) chicks were experimentally infected with v2001 by intraabdominal inoculation and housed with naïve contact chicks (n = 8/chicken line) considered “experimental infection”. (b) After 2 weeks, MDV is shed into the environment, and naïve contact birds are infected considered “natural infection”. (c) Both “Infected”, based on fluorescent feathers and “Diseased”, based on clinical disease, were used for collection of whole lung lavage cell (WLLC) and liver sample collection. (d) RNA was extracted, cDNA synthesized, and RT-qPCR was performed to determine differential mRNA expression of PRs.
All the birds were screened weekly for infection by visualizing feathers for fluorescently tagged MDV as described previously36,37. All chickens were monitored for clinical disease signs such that we had samples at least one week prior to disease manifestation; however, typically symptoms progress over several days38. All MDV positive contact birds (naturally infected) were euthanized at different stages of disease progression based on clinical manifestations and were assigned to two groups (n = 4/group/line): Infected (no disease) or Diseased (Tumorigenic). Control birds were euthanized at end of experiment; therefore, a total of three groups were used for analysis; Uninfected, Infected, and Diseased.
Sample collection
The birds were euthanized at different time points to achieve sampling for the “Uninfected,” “Infected,” and “Diseased” groups for both chicken lines. At time of euthanasia, the chickens were processed to obtain single cell suspensions of lymphocytes and mononuclear cells (WLLC) in the lungs with minor modifications. Briefly, the lungs were perfused with PBS (~ 15 ml) via oral gavage, and then the solution was collected. The procedure was repeated three times, and the collections were centrifuged at 1000 × g for 10 min at 4 °C to obtain cell pellets. The cells were resuspended in PBS and aliquoted into 2 ml vials, recentrifuged to remove the PBS, and then frozen at −80 °C. Immediately after euthanasia, ~ 5 ml of whole blood was collected by heart puncture and stored at −80 °C in heparinized tubes. Within 15 min of exsanguination, the remaining bird’s body was processed for live tissue sampling and ~ 50 mg of liver tissue was used for RNA extraction in RNA STAT-60 (Tel-Test, Inc., Friendswood, TX) and subsequently stored at − 80 °C within 30–50 min.
Primers
Some primers have been previously described39 or were designed in our laboratory using previously reported procedures for primer design, primer testing, selection of internal control genes for normalization40,41. Briefly, gene specific primers were designed using gene bank mRNA sequences for P1 PRs [P1A1A (ADORA1), P1A2A (ADORA2A), P1A2B (ADORA2B), P1A3 (ADORA3)], P2X PRs (PX1- P2X7) and P2Y PRs (P2Y1, P2Y2, P2Y3/P2Y6, P2Y4, P2Y5, P2Y8, P2Y10, P2y12, P2Y13, P2Y14). Primer details are provided in Table 1.
Table 1.
Purinergic receptors primer sets used for RT-qPCR assays.
| Family | Gene Name | Gene ID1 | Accession No.2 | Primer3 | Sequence (5’-3’) | Fragment (bp)4 | Source5 |
|---|---|---|---|---|---|---|---|
| P1 | ADORA1 | 374212 | NM_204316.4 | F.433 | ATCAATATCGGACCGCAGAC | 159 | This report |
| R.591 | GGGTGTCACCACGCTCTTAT | ||||||
| ADORA2A | 427705 | XR_005854444.1 | F.1574 | CATTGTTGGGTTGTTTGCAG | 243 | This report | |
| R.1816 | GTTCCTGCTTTGAACTGCTC | ||||||
| ADORA2B | 395971 | NM_205087.2 | F.969 | GGACTTCCGCTACACCTTCC | 106 | This report | |
| R1074 | GTTGGTGACAGTCAGGTGCT | ||||||
| ADORA3 | 373956 | NM_204151.3 | F.375 | GCATCCCGTTCCATTTCTGC | 315 | This report | |
| R.689 | TGAGAGTCCACGCGAAGAAC | ||||||
| P2X | P2X1 | 395190 | NM_204519.2 | F.312 | ATACATCATAGGGTGGGTTT | 359 | 39 |
| R.670 | AGATTTCGCAGGTCTTCAT | ||||||
| P2X2 | 101749217 | XM_004934420.2 | F.512 | CGCAGTTCACCATCCTCATC | 338 | 39 | |
| R.849 | CTTGGCAAACCTGTAGTTGTAGC | ||||||
| P2X3 | 428856 | NM_001397208.2 | F.433 | CTCGGTGTTCGTGGTGGTC | 377 | This report | |
| R.809 | GCGGCTGTTGCTCGGGAT | ||||||
| P2X4 | 374166 | NM_204291.2 | F.529 | CTATCACATACCCAATCCG | 413 | 39 | |
| R.941 | TTTCAATGCCACTACTATCC | ||||||
| P2X5 | 395507 | NM_204748.2 | F.714 | TCCTACCTAAAGACCTGCCACT | 345 | 39 | |
| R.1058 | TGCCTTGCCATTCACCAT | ||||||
| P2X6 | 429367 | XM_040685095.1 | F.993 | CAGCCACGCTACTCCTTCAT | 207 | This report | |
| R.1199 | GGTTCCAAGGAATGCGATGC | ||||||
| P2X7 | 771952 | XM_001235162.6 | F.1300 | TCCTATGATCCTCGCACCT | 378 | 39 | |
| R.1677 | GATGATGGCTCTGTCCTCC | ||||||
| P2Y | P2Y1 | 396275 | NM_205333.2 | F.326 | ACCTGCCCACCGTCTACATC | 348 | 39 |
| R.673 | CGGCGTTCTTCTTCTTCAGC | ||||||
| P2Y2 | 428108 | XM_025146950.2 | F.38 | TTTCTGCCTGCTTTACCGTCA | 490 | This report | |
| R.527 | AACATGTACGTGGTGGAGGC | ||||||
| P2Y3/P2Y6 | 396114 | NM_205195.1 | F.484 | AGTGCCTGCCCACCTTTGT | 240 | 39 | |
| R.723 | CGGCCTTGTCCTTCTTCTTG | ||||||
| P2Y4 | 100857687 | XM_004940541.4 | F.13 | CCGTCATTAAGCTGTCCGCA | 370 | This report | |
| R.382 | CTCCTCGTTGAAGACGCACT | ||||||
| P2Y5 | 396118 | NM_205199.3 | F.556 | AACAACACGGAGCAAAGAA | 351 | 39 | |
| R.906 | CAGGGTGACAGGGTACATAG | ||||||
| P2Y8 | 418665 | NM_001008679.2 | F.669 | TGGAAAGCACGGATCTGACC | 569 | This report | |
| F.1227 | AGGCCATCCATAGGTCCACT | ||||||
| P2Y10 | 422148 | XM_040669411.1 | F.218 | GCAACTGGACTTGCTCTGAT | 653 | This report | |
| R.870 | GCTGTTGTTTTGCAGCGGTA | ||||||
| P2Y13 | 107049027 | XM_040679499.1 | F.493 | GCATAGTGCTCCTCGGTCTC | 662 | This report | |
| R.1154 | TGTGTCCAGTTCGGTTCTCG | ||||||
| P2Y14 | 101749627 | NM_001317401.2 | F.481 | ACTCCAGCACAAACTCCTCG | 524 | This report | |
| R.1004 | CTCGCTTTTAAGGCCGATGC |
1National Center for Biotechnology Information (NCBI) Gene ID for Gallus gallus (chicken).
2NCBI mRNA Accession No.
3Primer direction (F-forward; R-reverse) and hybridization position in gene.
4Amplicon size in base pairs.
5Source of primer sequence.
RNA extraction
For WLLC samples, the cell pellet was resuspended in 500 µl RNA STAT-60 and RNA was extracted using the manufacturer’s instructions for collection of RNA. For liver samples, 50 mg of tissue sample was crushed in liquid N and the powder was suspended in 500 µl RNA STAT-60 for RNA extraction. The RNA samples were treated with DNase (Thermo Fisher Scientific), to remove any residual genomic DNA. The RNA concentrations were measured using a Nano-Drop ND-1000 spectrophotometer (Nano-Drop Technologies, Wilmington, DE, USA). The purity of RNA (A260/A280) for all samples was above 1.81 and the quality of RNA was evaluated using 2% agarose gel, and the high-quality samples were used for cDNA synthesis.
RT-qPCR analysis
RT was performed using 2 µg DNase-treated total RNA using the High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher Scientific). Twenty-microliter RT reactions were carried out according to the manufacturer’s instructions with Oligo dT20 plus random primers. The reaction mixture was incubated at 25 °C for 10 min, then 37 °C for 120 min, followed by 85 °C for 5 min. Most cDNA reactions were diluted 1:4 in ddH2O prior to qPCR analysis.
For qPCR, 20 µl reactions were prepared with 4 µl diluted cDNA, specific primers (0.5 μM), 10 µl 2 × Power SYBR Green Master Mix (Thermo Fisher Scientific), and ddH2O as previously published40,41. For qPCR efficiency, serial tenfold dilutions of pooled cDNA of the respective samples were used for generating standard curves, starting with approximately 500 pg of cDNA. Thermal cycling conditions were as follows: 50 °C for 2 min and 95 °C for 10 min, followed by 40 cycles at 95 °C for 15 s and 60 °C for 1 min. All RT-qPCR assays were performed using an Applied Biosystems QuantStudio 3 real-time PCR system (Thermo Fisher Scientific), and the results were analyzed using QuantStudio Design & Analysis Software v1.4.2, supplied by the manufacturer. The final genes data set were normalized with geometric mean of chicken GAPDH and 18S rRNA.
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics version 28 software (SPSS Inc., Chicago, IL, USA). The significant differences for the plaque size assays were determined with Kruskal–Wallis tests (one-way non-parametric ANOVA), followed by multiple comparison tests. The normalized gene expression data (RT-qPCR) WLLC and liver samples were analyzed using two-way ANOVA followed by Tukey’s post-hoc tests; virus (V) and chicken breed (B) and all possible interactions (V × B) were used as fixed effects, and the relative mRNA were used as dependent variables. Statistical significance was declared at p < 0.05 and the mean tests associated with significant interactions (p < 0.05) were separated with Tukey’s tests.
Ethical approval
All animal procedures were preapproved by the university’s Institutional Animal Care and Use Committee (IACUC) and conducted according to national regulations and ARRIVE guidelines. The animal care facilities and programs meet all the requirements of the law (89–544, 91–579, 94–276) and NIH regulations on laboratory animals, and follow the Animal Welfare Act, PL 279. The University of Illinois at Urbana-Champaign (UIUC) is accredited by the Association for Assessment and Accreditation of Laboratory Animal Care (AAALAC). Water and food were provided ad libitum.
Results and discussion
Characterization of v2001 in cell culture and in chickens
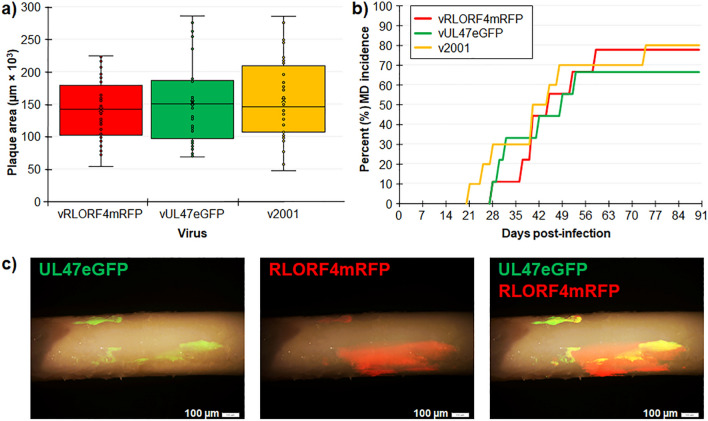
We previously reported that fusing fluorescent proteins to the C-terminus of the late gene pUL47 (vUL47eGFP) allows the visualization of infected cells and does not affect replication in cell culture and in vivo30. Similarly, we found that fusing mRFP to the C-terminus of the early RLORF4mRFP (vRLORF4mRFP) did not affect replication in cell culture and in chickens28. For another study, we generated a dually fluorescent virus termed v2001 by inserting eGFP at the C-terminus of the pUL47 in the previously described rRLORF4mRFP using two step Red-mediated recombination. Plaque size assays showed there were no significant differences between vRLORF4mRFP, vUL47eGFP, and the newly generated v2001 (Fig. 2a).
Figure 2.
Replication of v2001 in cell culture and in chickens. (a) Plaque areas were measured in CECs infected with vRLORF4mRFP, vUL47eGFP, and v2001. There were no significant differences between parental viruses using ANOVA. (b) Total MD incidence was determined for each group. There were no significant differences in the total number of chickens developing MD in experimentally infected chickens using Fisher’s exact tests. (c) Feathers were plucked from v2001-infected chickens at 35 days pi and expression of RLORF4mRFP and UL47eGFP were visualized using direct fluorescent stereomicroscopy.
Next, the ability of v2001 to induce MD in chickens and transmit to contact chickens (natural infection) was tested. There was no difference between all three viruses in inducing MD in experimentally infected chickens with vRLORF4mRFP, vUL47eGFP, and v2001 inducing MD in 78, 67, and 80% of WL chickens (Fig. 2b). Additionally, all five contact chickens housed with experimentally infected chickens were positive for virus in the feathers (data not known). Importantly, both UL47eGFP and RLORF4mRFP expression could be observed in feathers of v2001-infected contact chickens (Fig. 2c). These results show that v2001 retained it virulence and transmissibility in chickens.
The PR responses during MDV replication and MD pathogenesis
In contrast to mammals, avian macrophages are not present at the external surface of the lung’s airway epithelia in large numbers42–44. However, upon exposure to the infection, macrophages and other leukocytes are recruited to the surface, activating a cellular immune response in the avian respiratory tract44,45. During natural MDV infection, the recruitment and infection of macrophages, dendritic cells, and B and T lymphocytes is an important step in the replication of MDV and disease progression1; therefore, we targeted the lung’s airway for sampling in our study. WLLC is a technically easy and ideal collection of superficial, loosely attached cells from the lung epithelia46,47. On the other hand, the liver is one of the most important metabolic organs of the body, with up to 90% of fatty acid de novo synthesized in avian liver48,49. In poultry, the metabolism regulation processes, especially the lipid metabolism is similar to mammalian species with some exceptions49–51.
The relative expressions of three subtypes of PRs were measured in two chicken lines (Susceptible vs Resistant) in response to MDV infection and disease induction compared to uninfected controls. Based on the infection, physical condition, and internal pathology of the naturally infected susceptible (PC) and resistant (WL) birds were assigned into two different categories: Infected (MDV positive only), and Diseased (gross tumors). Uninfected birds were used as controls.
P1 PR responses during MDV replication and MD pathogenesis
P1A1 (Adenosine A1 Receptor: ADORA1) is widely expressed in tissues, and its role has been reported to be anti-inflammatory, anti-diuretic, and involved in tissue protection, particularly the lungs and kidneys52. It has also been studied during Epstein-Barr herpesvirus (EBV) infection. Du et al.53 showed that cordycepin (3-deoxyadenosine), a derivative of adenosine that has anti-proliferative, anti-inflammatory, and pro-apoptotic effects, induced EBV reactivation in EBV-transformed cells. However, Ryu et al.54 showed that cordycepin suppressed EBV replication. In WLLC, the relative mRNA of P1A1 expression increased in WL for both Infected and Diseased groups compared to uninfected controls (P < 0.05), while there was no difference in both PC groups (Fig. 3a). No P1A1 mRNA was detected in the liver for all groups suggesting tissue specific expression of this PR.
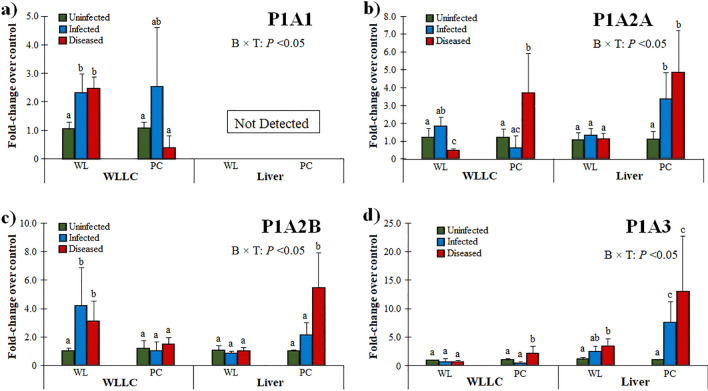
Figure 3.
Relative mRNA expression of P1 PRs in the MD-resistant (WL) and -susceptible (PC) chicken lines. PR expression was measured in WLLC and liver samples using RT-qPCR and fold-changes compared to uninfected controls is shown for P1A1 (a), P1A2A (b), P1A2B (c), and P1A3 (d). Data presented as mean ± standard deviation. Statistical significance was calculated with 2-way ANOVA [Chicken line (B) × Infection (T)]. Superscripts a-c indicates significant differences (P < 0.05) between different groups in specific tissues (WLLCS or Liver) of the two chicken lines.
The higher expression in the WLLC sample of the infected birds could be associated with tissue protection (Fig. 3a). Choi and colleagues recently demonstrated that adenosine partially requires ADORA1 signaling to upregulate BZLF1, a key regulator of EBV lytic replication. Furthermore, they also confirmed that at BZLF1 upregulation by adenosine is effective in suppressing or delaying EBV-associated gastric carcinoma development55. In relation to the data reported here, the higher expression of ADORA1 in WLLC of Infected WL chickens (Fig. 3a) suggests they may have a more robust anti-inflammatory reaction that could be involved in their being more resistant to MD development. Further experiments are warranted to better understand the role ADORA1 plays during MDV infection and viral pathogenesis.
The expression of P1A2A significantly increased in both WLLC and liver samples from the PC Diseased group (Fig. 3b). In WLLC samples, P1A2B expression was increased in WL chickens in response to MDV infection and induction of disease, while no change was observed in PC chickens (Fig. 3c). P1A2B (Adenosine A2B Receptor: ADORA2B), along with P2Y2, have been reported to regulate mucociliary clearance, which is a dominant component of pulmonary host defenses56. Higher expression of these receptors in WLLC of Infected WL suggests it may play a unique role in the lungs of WL chickens. However, PC chickens had significantly higher P1A2B expression in the liver in the Diseased group. Interestingly, P1A2B signaling has been reported to contribute to immunosuppression in tumors17, implicating its potential role during MD progression in the susceptible PC chicken line. The higher hepatic expression of P1A2B in PC could be associated with a unique role for hepatic cells such as ADORA2B singling as anti-inflammatory and liver protection during stress and disease condition reported by different studies57,58.
P1A3 (Adenosine A3 Receptor: ADORA3) has been demonstrated as a mediator of anti-inflammatory, -cancer. and -ischemic protective effects. P1A3 is overexpressed in cancer and inflammatory cells, while low expression is found in normal cells59. In cancer cells, the activation of the P1A3A corrects an imbalance in the downstream Wnt signaling pathway60,61. Administration of an A3 agonist to activate its cell surface receptor inhibits the formation of cAMP and indirectly decreases phosphorylation (and therefore decreased inactivation) of the serine/threonine kinase GSK-3β. The resulting increased phosphorylation of β-catenin results in it being removed from the cytoplasm by ubiquitination; therefore, preventing its nuclear import and thus resulting inhibition of cellular proliferation that results in cell growth inhibition. With respect to cancer, nuclear factor κB (NF-κB) is a potent anti-apoptotic agent in malignant cells and its activation is strongly associated with tumors62,63. Whereas regulation of NF-κB has been reported as central to MDV induced pathogenesis64, P1A3A induces specific anti-inflammatory and anticancer effects via a molecular mechanism that entails modulation of the Wnt and the NF-κB signal transduction pathways60,65,66. Interestingly, P1A3 was significantly increased in both Infected and Diseased liver samples in PC chickens (Fig. 3d), suggesting a role in inflammatory and pro-tumorigenic conditions development in these chickens.
MDV has been reported to induce inflammatory cytokines (response) in the lung’s epithelium1. During acute stages, the P1A2A and P1A3 functions are associated as anti-inflammatory and P1A2B to vascular barrier function in the lung67. The higher expression of these receptors in WLLC samples (Fig. 3) in the Diseased groups for both chicken lines suggests an anti-inflammatory response to higher stress. The higher expression of P1A2A and P1A3 in the lungs of Diseased birds may help to actively regulate the active transport across the epithelial during disease stress. Similarly, the higher hepatic expression of these receptors in the Infected and Diseased MD-susceptible (PC) birds only (Fig. 3b,d), indicates a role in MD pathogenesis and in tissue protection as previously been reported in acute hepatic inflammation that could impact fibrosis progression in the liver68–71. Overall, the differential expression of P1 PRs in MD-susceptible and -resistant chickens and tissue specificity suggests these receptors may be involved in the complex interactions during infection and disease development during MDV infection.
P2X PR responses during MDV replication and MD pathogenesis
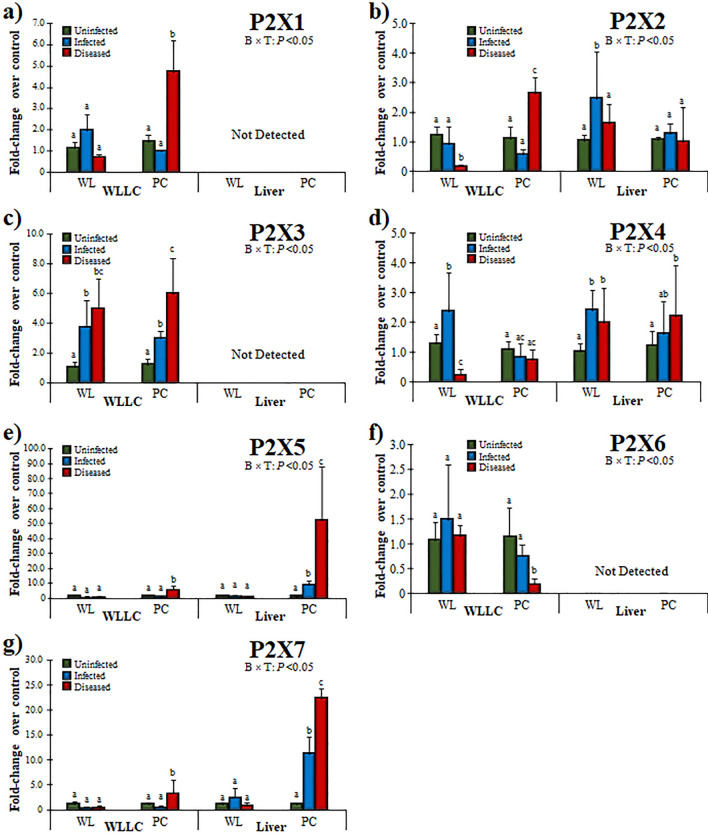
Overall, the expression of P2X1, P2X2, P2X3, P2X5, and P2X7 increased in WLLC samples of the Diseased PC chickens (Fig. 4). Interestingly, P2X4 was increased in Infected WL only, but was significantly decreased in Diseased birds (Fig. 4d). The expression of P2X1, P2X2, P2X5, P2X7 were significantly increased in Diseased PC birds, whereas P2X3 was increased during MDV infection, irrespective of disease condition or chicken line (Fig. 4c). In contrast, P2X6 expression decreased in Diseased PC birds, while no change was observed in WL compared to control (Fig. 4f).
Figure 4.
Relative mRNA expression of P2X PRs in the MD-resistant (WL) and -susceptible (PC) chicken lines. PR expression was measured in WLLC and liver samples using RT-qPCR and fold-changes compared to uninfected controls is shown for P2X1 (a), P2X2 (b), P2X3 (c), P2X4 (d), P2X5 (e), P2X6 (f), and P2X7 (g). Data and statistics are presented as in Fig. 3.
Among P2X receptors, P2X2 had differential expression in the lungs of Diseased birds between the chicken lines, with WL chickens having decreased P2X2 expression, while PC birds had increased expression (Fig. 4b). WL chickens also had decreased P2X4 expression in WLLC (Fig. 4d). Interestingly, P2X5 and P2X7 were highly increased in Infected PC chickens that was further increased in the Diseased groups (Fig. 4e,g). No transcripts were detected for P2X1, P2X3, and P2X6 in the liver (Fig. 4a,c,f).
The current studies reveal higher expression of P2X PRs in Diseased MD-susceptible PC chickens (Fig. 4). Similar increases in mRNA has been reported in the EBV-infected B cells by Lee et al.11, that was also confirmed using western blot. There is a substantial body of evidence accumulating supporting the involvement of P2X1, P2X4 and P2X7 in host defense against infection72. Most immune cells, including monocytes, macrophages, dendritic, neutrophils, and T cells express P2X1, P2X4, and P2X7 during anti-pathogenic signaling72, suggesting an important role for these receptor subtypes in these cells. Like P2X1, the receptor can form homo- and heteromeric (e.g., P2X2/P2X3) ion channels for different purposes, depending on the cell type they are expressed on and the intended response73. P2X3 expression was absent in the liver of chickens, but abundantly expressed in WLLC (Fig. 4c), indicating an importance in the airways and lungs where ATP acts as a trigger of the cough reflex via stimulation of P2X3 and P2X2/3 receptors74–76. Moreover, a crucial role of P2X PRs containing P2X2 and P2X3 subunits has been reported to mediate response to hypoxia77. In addition, the upper and lower respiratory tract has different P2X3 distributions, such as nodose fibers expressing P2X2 and P2X3 subunits (P2X2/P2X3heterotrimers), whereas neural crest derived afferents express P2X3 and respond as P2X3 homotrimers78–80. The increased expression of P2X3 and P2X2 suggests MDV infection activates this response in the lungs.
Alveolar macrophages have been reported to express P2X481,82. These cells phagocytize and kill microorganisms, release cytokines, and present peptides to T cells, thus triggering both cellular and humoral immune responses83. It has been demonstrated that P2X4-signalling promotes innate immunity in the immunopathologic response in lungs84. The increase in P2X4 expression in WL chickens infected with MDV that was decreased in Diseased birds (Fig. 4d) could be linked to its role in protecting against infections, inflammation, and organ injury82.
P2X5 is a basic requirement for the ATP-mediated inflammasome activation and IL-1β production by inflammatory stimuli85. The receptor has been reported as protective immune regulators during infection, mounting proper innate immune responses by regulating inflammasome activation and IL-1β production86. Chen et al.16 recently demonstrated that replication of HCMV was inhibited by P2X5. According to Lee et al.11, most P2 receptors are expressed on primary human B cells, while EBV-transformed cells dominantly express P2X5. In contrast to HCMV16, and similar to EBV11, the higher expression of P2X5 in MDV-Infected and Diseased PC chickens indicates a role for P2X5 in MD progression (Fig. 4e). Further research at different stages of MDV infection is warranted to delineate the role of P2X5 in the overall MD pathogenesis.
P2X7 is expressed by all tissues including different respiratory cells such as type I alveolar epithelium, pulmonary endothelial, and resident immune cells implicating it in respiratory infections. In response to pathogens, P2X7 induces alveolar macrophage activation, secretion of IL-1β and IL-1α, and neutrophil recruitment87–89. In addition, the receptor’s role has been linked to apoptosis by activating the inflammasome, caspases, and phospholipases90. The receptors also modulate intracellular signaling pathways, such as PI3K/AKT/mTOR, myeloid differentiation factor 88 (MyD88)/NF-κB, as well as the activation of mitogen-activated protein kinase (MAPK) pathway proteins (MEK, ERK 1/2)91–93. In the current study, the higher expression of P2X7 in MDV-infected PC chickens in both WLLC and liver (Fig. 4g) suggests an involvement in disease progression in these chickens.
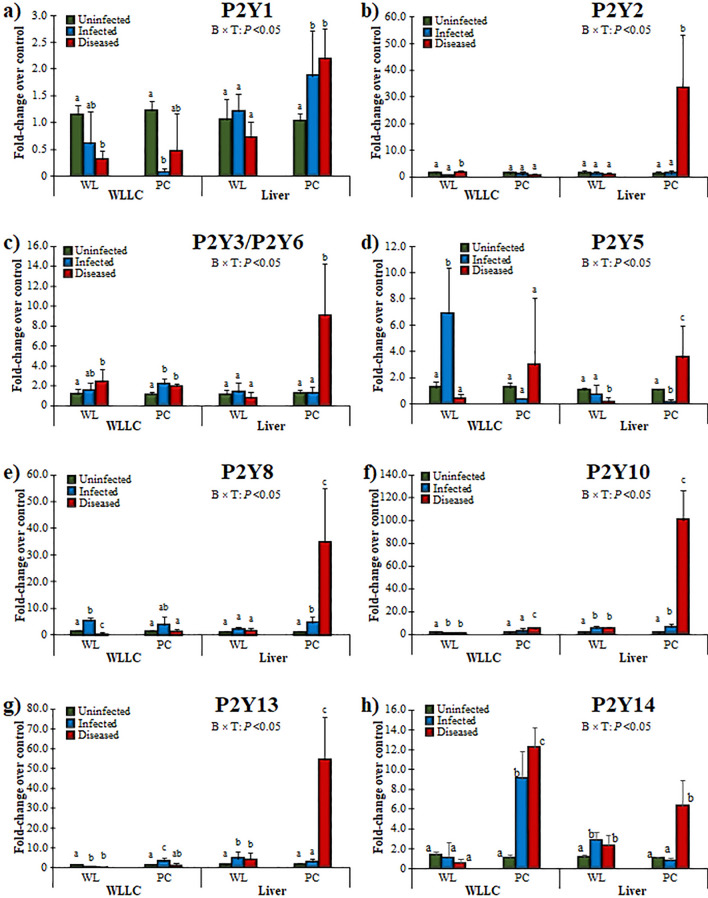
P2Y PR responses during MDV replication and MD pathogenesis
In general, MDV Infected and Diseased birds had significantly affected expression of P2Y receptors (Fig. 5); however, no expression was observed for P2Y12 (not shown). The expression of P2Y1 decreased with infection in WLLC but had higher hepatic expression in MDV-Infected and Diseased PC birds (Fig. 5a). P2Y1 is widely distributed in tissues94 and has been reported in both innate and adaptative immune responses by inducing endothelial cell activation and leukocyte rolling95,96. The lower expression of P2Y1 in WLLC in both chicken lines and higher expression in Infected and Diseased PC livers implicates a tissue specific expression pattern and a role in viral replication and disease progression. Endothelial cells are an essential component of the lungs97 and have been reported to express P2Y198–100 and exerts a protective role against infection in the lungs by ameliorating protein leakage and enhancing the proinflammatory cytokine response101. Therefore, the decreased expression in lungs due to MDV infection suggests MDV may downregulate its expression (Fig. 5a); however, further research is needed address the role of P2Y1 in MDV infection.
Figure 5.
Relative mRNA expression of P2Y PRs in the MD-resistant (WL) and -susceptible (PC) chicken lines. PR expression was measured in WLLC and liver samples using RT-qPCR and fold-changes compared to uninfected controls is shown for P2Y1 (a), P2Y2 (b), P2Y3/P2Y6 (c), P2Y5 (d), P2Y8 (e), P2Y10 (f), P2Y13 (g), and P2Y14 (h). Data and statistics are presented as in Fig. 3.
P2Y2 was significantly increased in the liver of Diseased PC chickens (Fig. 5b). A functional role for the P2Y2 ligand ATP was found in different inflammatory diseases but the overall outcome depends on the situation, infection type, and host102. For example, it plays a protective role in the lung during pneumonia virus infection in mice103. In contrast, others have reported tissue damage in the airway following inflammation and acute liver injury104–106. Macrophages are central during initiation of infection with different viruses, including MDV25. Infection triggers macrophages to perform different tasks ranging from perception of danger signals, engulfment of lipids and dead cells, secretion of reactive oxygen species (ROS) and inflammatory cytokines, and pro-resolving molecules. The macrophage-derived ROS oxidizes low-density lipoprotein (LDL) to oxidized LDL (oxLDL and stimulates IL-1β and IL-8 production107. Interestingly, oxLDL favors nucleotide release from endothelial cells108. Triggering of the P2Y2 receptor by ATP secreted by endothelial cells upon stimulation with oxLDL induces expression of receptors for advanced glycation end-products and adhesion molecules109. Furthermore, the release of ROS and ATP/UDP from endothelial cells upon exposure to oxLDL induce autocrine P2Y1-mediated upregulation of ICAM-1 and VCAM-1 with subsequent stimulation of leukocyte adhesion110. MD-susceptible and resistant chickens have significant differences in the metabolism of lipoprotein; LDL lipoprotein fraction increases with growth in the susceptible line111. Moreover, MD increases production of ROS leading to oxidative stress in the susceptible chickens112,113. Whereas this imbalance in the ambient redox level promotes oxidation of native LDL (oxLDL), thus the higher hepatic expression of P2Y1 and P2Y2 (Fig. 5a,b) in MD-susceptible Diseased birds could be linked with expected oxidation of LDL in response to stress levels.
The avian P2Y3 has been reported as an avian homologue of mammalian P2Y651. For mammals, P2Y6 has been reported to contribute to airway inflammation following the induction of the allergic response in mice114. The antiviral role of P2Y6 has been demonstrated in different studies under different viral infections. For example, inactivated avian influenza virus-H5N1 increases IL-6 and CXCL8 mRNA by a mechanism that involves activation of P2Y6115. In addition, vesicular stomatitis virus (VSV)-induced cell death and virus replication were both enhanced significantly by knocking down or out P2Y6 in different cells116. In WLLC, both chicken lines showed higher expression of P2X3/P2Y6 in response to Diseased conditions (Fig. 5c), whereas, higher hepatic expression of P2Y3/P2Y6 was observed in Diseased PC birds only (Fig. 5c). These results warrant further research to understand this receptor’s potential role during the innate immune response during natural MDV infection.
P2Y5 is a G protein-coupled receptor (GPCR) that binds and is activated by lysophosphatidic acid (LPA) and by farnesyl pyrophosphate (FPP)117. LPA levels have been reported to increase during pathological conditions118, whereas LPA has been reported to regulate the Gα12/13-Rho/ROCK pathway via LPAR4/P2Y9 and LPAR6/P2Y5119. Former studies by Richerioux and colleagues120 reported that Rho-ROCK pathways regulate MDV cell-to-cell spread in cell culture. LPA has been reported to contribute to the maintenance of the epithelial integrity121 by regulating cellular events such renewal and migration of epithelial cells and inflammation responses122. LPA-mediated induction has been reported to regulate p38 MAPK, PI3K, PLC, and PKC activity and the induction of ERK1/2 phosphorylation117. During natural infection, WL chickens had significantly increased levels of P2Y5 in the infected lungs, while PC chickens had higher hepatic expression (Fig. 5d). These data suggest the P2Y5 response may be involved in genetic differences in response to infection in the lungs and the progression of disease based on the liver response.
The expression of P2Y8 increased (4.94 ± 1.49-fold-change) in WLLC of WL with MDV infection but was decreased (0.46 ± 0.32-fold change) in Diseased chickens (Fig. 5e). However, P2Y8 expression was significantly increased in MDV-Infected and Diseased PC chickens, while it was unchanged in WL birds. Higher expression of P2Y8 has been reported in lymphocytes, while lower expression has been shown in the lungs and other visceral organs123. The receptor has been shown to have oncogenic potential124 and fusion with other proteins like cytokine receptor-like factor 2 (CRLF2) increases its complexity in different diseases124–126. Similar responses were observed for P2Y5 and P2Y8 where their expression was increased in WLLC of the MD-resistant WL chickens, while being increased in the livers of the MD-susceptible PC chickens (Fig. 5d,e). Considering the potential role of P2Y8 in oncogenesis124, it is tempting to speculate it may play an important role in oncogenesis in the PC chicken line. These data suggest an important role in MD; however, further studies in other tissues at early exposure will help to reveal the potential role of P2Y5 and P2Y8 in MDV infection and tumorigenesis.
No expression of P2Y12 was detected in our samples, while the relative higher expression of P2Y10, P2Y13 and P2Y14 were observed in Infected PC chickens, and were further increased in the Diseased group (Fig. 5f–h). However, MDV-infected WL showed significantly lower expression of P2Y10 and P2Y13. In summary the expression of P2Y10, P2Y13 and P2Y14 expression were affected by infection and diseased PC (susceptible) chickens.
P2Y10 is another GPCR expressed by B and T cells, monocytes, dendritic cells, and granulocytes127,128. The putative ligands for P2Y10 are still debatable but based on different studies, the receptor has been shown to be regulated by nucleotides, LPA, sphingosine-1-phosphate (S1P) and lysophosphatidylserine (LysoPS)129–132. Gurusamy and colleagues demonstrated that in response to auto/paracrine acting mediators such as LysoPS and ATP, P2Y10 facilitates activation of RhoA in CD4 + T cells, thus mediating chemokine-induced migration and finally, T cell-mediated diseases132. Only the MD-susceptible PC chickens had increased expression of P2Y10 in both WLLC and livers (Fig. 5f) indicating a potential role in disease progression and MD susceptibility.
P2Y13 is one of the most important PRs expressed in lungs133 and has been reported as a potential antiviral target19. The receptor has been reported to improve recurrence-free survival in hepatocellular carcinoma patients134. Zhang et al.19 also showed that P2Y13 expression restricted the replication of both DNA (HSV-1) and RNA (NDV and VSV) viruses via JAK–STAT signaling19. In the current study, the higher expression (3.13 ± 1.17 fold-change) of P2Y13 during earlier infection with MDV in PC chickens in WLLC and increased expression in the liver.
of MDV-infected PC chickens (Fig. 5g) highlights the potential importance of P2Y13 as an antiviral or antitumor target as mentioned before134 and suggests P2Y13 may play a significant role in MD progression in different chicken lines.
The current study also revealed higher expression of P2Y14 in MDV-infected PC chickens (Fig. 5h), which indicates a potential role in pathogenesis as has been reported in other diseases135. This receptor is an alternative therapeutic target based on its role in many complex physiological processes like inflammation, diabetes, and immune processes135. Therefore, several specific potent antagonists have been developed in recent years135. The gene is conserved among vertebrates such as chimpanzees, rhesus monkeys, dogs, cows, chickens, and frogs. The receptor is predominately present in immune cells, and ubiquitously present in most tissues such as placenta, spleen, bone marrow, thymus, stomach, intestine, adipose tissue, and brain. Most interesting, recent data demonstrated its role in mobility and recruitment of macrophages135. P2Y14 can be activated by nucleotide sugar conjugates such as uridine diphosphate (UDP)-glucose (UDPG), and UDP-glucose sugars (UDPG-sugars) are potent regulators of P2Y14 to initiate subsequent signal transduction pathways via Gi/o coupled protein136. UDPG has been reported to promote neutrophil and macrophage recruitment in the lung137. Interestingly, it has been documented that MDV increases the number of macrophages in the lungs of the infected chickens138. IFN-γ has been shown to be associated with immunity against MDV139. Moreover, IFN-γ treatment stimulates glycogen synthesis in macrophages that is channeled through glycogenolysis to generate G6P and further to NADPH, ensuring high levels of reduced glutathione for inflammatory macrophages survival140. This in turn, leads to increased UDPG levels and ultimately P2Y14 expression in macrophages140. Gilfernandez and colleagues141 completely abolished the replication of HSV-2 and African swine fever virus using a uridine 5'-diphosphate glucose analogues at 100 and 150 µg/ml, respectively. These all suggest a key role of P2Y14 in MD and potentially during recruitment of macrophages or other immune cells to the lungs.
Conclusions
In the current study, we measured the PR response during MDV infection. The findings from our study suggests the genetics of the host plays a key role during MDV infection and disease progression. Selection and breeding of chickens for relative resistance and susceptibility to MD has been a major parameter for the poultry industry7. Thus, using two different chicken lines (MD-susceptible and MD-resistant) were used here to determine whether the PR response was different in these two chicken lines. Interestingly, differential regulation in many PR was observed between MD-resistant and –susceptible chickens. Our study revealed interesting results regarding the differential expression of PRs in response to MDV infection and severity of MD. Both tissues and chicken breed had different expression patterns of PRs. The different expression levels confirmed that some PRs expression changes with pathophysiological conditions and tissue type. In general, the PRs involved in tissue protection and disease control were increased in MD-resistant WL chickens, whereas PRs involved in disease progression were increased in MD-susceptible PC chickens. As far as we are aware, this is the first study evaluating PR responses to natural MDV infection and MD pathogenesis and suggests further studies are warranted to elucidate the PR response to MD.
Author contributions
H.A. conceptualized the project and performed the experiments; J.F. and N.P. provided technical support; H.A. wrote the original draft; H.A. and K.J. reviewed and edited the final draft; K.J. supervised and acquired funding for this project. All authors have read and agreed to the published version of the manuscript.
Funding
This report was partially supported by Agriculture and Food Research Initiative Competitive Grant no. 2020-67015-21399 from the USDA National Institute of Food and Agriculture and the USDA National Institute of Food and Agriculture, Hatch project ILLU-888-96 to KWJ.
Data availability
The authors declare that all data supporting the findings of this work are available within the paper.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Boodhoo N, Gurung A, Sharif S, Behboudi S. Marek's disease in chickens: A review with focus on immunology. Vet. Res. 2016;47:119. doi: 10.1186/s13567-016-0404-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jarosinski KW, Tischer BK, Trapp S, Osterrieder N. Marek's disease virus: Lytic replication, oncogenesis and control. Exp. Rev. Vaccin. 2006;5:761–772. doi: 10.1586/14760584.5.6.761. [DOI] [PubMed] [Google Scholar]
- 3.Morrow, C. & Fehler, F. in Marek's Disease (eds F. Davison & V. Nair) 49–61 (Institute for Animal Health, Compton Laboratory, UK, 2004).
- 4.Jarosinski KW. Interindividual spread of herpesviruses. Adv. Anat. Embryol. Cell Biol. 2017;223:195–224. doi: 10.1007/978-3-319-53168-7_9. [DOI] [PubMed] [Google Scholar]
- 5.Schat KA, Markowski-Grimsrud CJ. Immune responses to Marek's disease virus infection. Curr. Top. Microbiol. Immunol. 2001;255:91–120. doi: 10.1007/978-3-642-56863-3_4. [DOI] [PubMed] [Google Scholar]
- 6.Biely J, Palmer VE, Lerner IM, Asmundson VS. Inheritance of resistance to fowl paralysis (Neurolymphomatosis Gallinarum) Science. 1933;78:42. doi: 10.1126/science.78.2011.42. [DOI] [PubMed] [Google Scholar]
- 7.Fulton JE, et al. Improving the outcome of a Marek's disease challenge in multiple lines of egg type chickens. Avian Dis. 2013;57:519–522. doi: 10.1637/10408-100212-Reg.1. [DOI] [PubMed] [Google Scholar]
- 8.Zimmermann H. Two novel families of ectonucleotidases: Molecular structures, catalytic properties and a search for function. Trends Pharmacol. Sci. 1999;20:231–236. doi: 10.1016/s0165-6147(99)01293-6. [DOI] [PubMed] [Google Scholar]
- 9.Fields RD, Burnstock G. Purinergic signalling in neuron-glia interactions. Nat. Rev. Neurosci. 2006;7:423–436. doi: 10.1038/nrn1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burnstock G. Purine-mediated signalling in pain and visceral perception. Trends Pharmacol. Sci. 2001;22:182–188. doi: 10.1016/s0165-6147(00)01643-6. [DOI] [PubMed] [Google Scholar]
- 11.Lee DH, Park KS, Kong ID, Kim JW, Han BG. Expression of P2 receptors in human B cells and Epstein-Barr virus-transformed lymphoblastoid cell lines. BMC Immunol. 2006;7:22. doi: 10.1186/1471-2172-7-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ralevic V, Burnstock G. Receptors for purines and pyrimidines. Pharmacol. Rev. 1998;50:413–492. [PubMed] [Google Scholar]
- 13.Di Virgilio F. Purines, purinergic receptors, and cancer. Cancer Res. 2012;72:5441–5447. doi: 10.1158/0008-5472.CAN-12-1600. [DOI] [PubMed] [Google Scholar]
- 14.Burnstock G. Short- and long-term (trophic) purinergic signalling. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 2016 doi: 10.1098/rstb.2015.0422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cekic C, Linden J. Purinergic regulation of the immune system. Nat. Rev. Immunol. 2016;16:177–192. doi: 10.1038/nri.2016.4. [DOI] [PubMed] [Google Scholar]
- 16.Chen S, Shenk T, Nogalski MT. P2Y2 purinergic receptor modulates virus yield, calcium homeostasis, and cell motility in human cytomegalovirus-infected cells. Proc. Natl. Acad. Sci. U S A. 2019;116:18971–18982. doi: 10.1073/pnas.1907562116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Awad MM, Shaw AT. ALK inhibitors in non-small cell lung cancer: Crizotinib and beyond. Clin. Adv. Hematol. Oncol. 2014;12:429–439. [PMC free article] [PubMed] [Google Scholar]
- 18.Ohta A, et al. A2A adenosine receptor protects tumors from antitumor T cells. Proc. Natl. Acad. Sci. U S A. 2006;103:13132–13137. doi: 10.1073/pnas.0605251103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang C, et al. IFN-stimulated P2Y13 protects mice from viral infection by suppressing the cAMP/EPAC1 signaling pathway. J. Mol. Cell Biol. 2019;11:395–407. doi: 10.1093/jmcb/mjy045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oliveira-Giacomelli A, et al. Purinergic receptors in neurological diseases with motor symptoms: Targets for therapy. Front. Pharmacol. 2018;9:325. doi: 10.3389/fphar.2018.00325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fekete R, et al. Microglia control the spread of neurotropic virus infection via P2Y12 signalling and recruit monocytes through P2Y12-independent mechanisms. Acta Neuropathol. 2018;136:461–482. doi: 10.1007/s00401-018-1885-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zandberg M, van Son WJ, Harmsen MC, Bakker WW. Infection of human endothelium in vitro by cytomegalovirus causes enhanced expression of purinergic receptors: A potential virus escape mechanism? Transplantation. 2007;84:1343–1347. doi: 10.1097/01.tp.0000287598.25493.a5. [DOI] [PubMed] [Google Scholar]
- 23.Bublot, M. & Sharma, J. in Marek's disease: An evolving problem Biology of Animal Infections (eds F. Davison & V Nair) Ch. 13, 168–185 (Elsevier Academic Press, 2004).
- 24.Bigger CB, et al. Intrahepatic gene expression during chronic hepatitis C virus infection in chimpanzees. J. Virol. 2004;78:13779–13792. doi: 10.1128/JVI.78.24.13779-13792.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baaten BJ, et al. Early replication in pulmonary B cells after infection with Marek's disease herpesvirus by the respiratory route. Viral Immunol. 2009;22:431–444. doi: 10.1089/vim.2009.0047. [DOI] [PubMed] [Google Scholar]
- 26.Schat, K. A. & Sellers, H. S. in A laboratory manual for the identification and characterization of avian pathogens (eds L. Dufour-Zavala et al.) 195–203 (American Association of Avian Pathologists, Jacksonville, FL, 2008).
- 27.Niikura M, Kim T, Silva RF, Dodgson J, Cheng HH. Virulent Marek's disease virus generated from infectious bacterial artificial chromosome clones with complete DNA sequence and the implication of viral genetic homogeneity in pathogenesis. J. Gen. Virol. 2011;92:598–607. doi: 10.1099/vir.0.026864-0. [DOI] [PubMed] [Google Scholar]
- 28.Jarosinski KW, Donovan KM, Du G. Expression of fluorescent proteins within the repeat long region of the Marek's disease virus genome allows direct identification of infected cells while retaining full pathogenicity. Virus Res. 2015;201:50–60. doi: 10.1016/j.virusres.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 29.Jarosinski KW. Marek's disease virus late protein expression in feather follicle epithelial cells as early as 8 days postinfection. Avian Dis. 2012;56:725–731. doi: 10.1637/10252-052212-Reg.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jarosinski KW, Arndt S, Kaufer BB, Osterrieder N. Fluorescently tagged pUL47 of Marek's disease virus reveals differential tissue expression of the tegument protein in vivo. J. Virol. 2012;86:2428–2436. doi: 10.1128/JVI.06719-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tischer BK, Smith GA, Osterrieder N. En passant mutagenesis: A two step markerless red recombination system. Methods Mol. Biol. 2010;634:421–430. doi: 10.1007/978-1-60761-652-8_30. [DOI] [PubMed] [Google Scholar]
- 32.Jarosinski KW, Osterrieder N, Nair VK, Schat KA. Attenuation of Marek's disease virus by deletion of open reading frame RLORF4 but not RLORF5a. J. Virol. 2005;79:11647–11659. doi: 10.1128/JVI.79.18.11647-11659.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Abramoff MD, Magalhaes PJ, Ram SJ. Image processing with ImageJ. Biophoton. Int. 2004;11:36–42. [Google Scholar]
- 34.Fulton JE, et al. MHC variability in heritage breeds of chickens. Poult. Sci. 2016;95:393–399. doi: 10.3382/ps/pev363. [DOI] [PubMed] [Google Scholar]
- 35.Jarosinski KW, et al. Horizontal transmission of Marek's disease virus requires US2, the UL13 protein kinase, and gC. J. Virol. 2007;81:10575–10587. doi: 10.1128/JVI.01065-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Krieter A, Xu H, Akbar H, Kim T, Jarosinski KW. The conserved Herpesviridae protein kinase (CHPK) of Gallid alphaherpesvirus 3 (GaHV3) is required for horizontal spread and natural infection in chickens. Viruses. 2022 doi: 10.3390/v14030586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vega-Rodriguez W, et al. The requirement of glycoprotein C (gC) for interindividual spread is a conserved function of gC for avian herpesviruses. Sci. Rep. 2021;11:7753. doi: 10.1038/s41598-021-87400-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Osterrieder N, Kamil JP, Schumacher D, Tischer BK, Trapp S. Marek's disease virus: From miasma to model. Nat. Rev. Microbiol. 2006;4:283–294. doi: 10.1038/nrmicro1382. [DOI] [PubMed] [Google Scholar]
- 39.Fodor J, et al. Ionotropic purinergic receptor P2X4 is involved in the regulation of chondrogenesis in chicken micromass cell cultures. Cell Calcium. 2009;45:421–430. doi: 10.1016/j.ceca.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 40.Akbar H, et al. Feed restriction, but not l-carnitine infusion, alters the liver transcriptome by inhibiting sterol synthesis and mitochondrial oxidative phosphorylation and increasing gluconeogenesis in mid-lactation dairy cows. J. Dairy Sci. 2013;96:2201–2213. doi: 10.3168/jds.2012-6036. [DOI] [PubMed] [Google Scholar]
- 41.Ponnuraj N, Tien YT, Vega-Rodriguez W, Krieter A, Jarosinski KW. The Herpesviridae conserved multifunctional infected-cell protein 27 (ICP27) is important but not required for replication and oncogenicity of Marek's disease Alphaherpesvirus. J. Virol. 2019;93:e01903–01918. doi: 10.1128/JVI.01903-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Esnault E, et al. A novel chicken lung epithelial cell line: Characterization and response to low pathogenicity avian influenza virus. Virus Res. 2011;159:32–42. doi: 10.1016/j.virusres.2011.04.022. [DOI] [PubMed] [Google Scholar]
- 43.Nganpiep LN, Maina JN. Composite cellular defence stratagem in the avian respiratory system: Functional morphology of the free (surface) macrophages and specialized pulmonary epithelia. J. Anat. 2002;200:499–516. doi: 10.1046/j.1469-7580.2002.00052.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reese S, Dalamani G, Kaspers B. The avian lung-associated immune system: A review. Vet. Res. 2006;37:311–324. doi: 10.1051/vetres:2006003. [DOI] [PubMed] [Google Scholar]
- 45.Maina JN. Some recent advances on the study and understanding of the functional design of the avian lung: Morphological and morphometric perspectives. Biol. Rev. 2002;77:97–152. doi: 10.1017/S1464793101005838. [DOI] [PubMed] [Google Scholar]
- 46.Gay P, et al. Efficacy of whole-lung lavage in pulmonary alveolar proteinosis: A multicenter international study of GELF. Respiration. 2017;93:198–206. doi: 10.1159/000455179. [DOI] [PubMed] [Google Scholar]
- 47.Brownback KR, Simpson SQ. Association of bronchoalveolar lavage yield with chest computed tomography findings and symptoms in immunocompromised patients. Ann. Thorac. Med. 2013;8:153–159. doi: 10.4103/1817-1737.114302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.O'Hea EK, Leveille GA. Lipid biosynthesis and transport in the domestic chick (Gallus domesticus) Comp. Biochem. Physiol. 1969;30:149–159. doi: 10.1016/0010-406x(69)91309-7. [DOI] [PubMed] [Google Scholar]
- 49.Li H, et al. Identification of a novel lipid metabolism-associated hepatic gene family induced by estrogen via ERalpha in chicken (Gallus gallus) Front. Genet. 2020;11:271. doi: 10.3389/fgene.2020.00271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dakovic N, et al. The loss of adipokine genes in the chicken genome and implications for insulin metabolism. Mol. Biol. Evol. 2014;31:2637–2646. doi: 10.1093/molbev/msu208. [DOI] [PubMed] [Google Scholar]
- 51.Li Q, Olesky M, Palmer RK, Harden TK, Nicholas RA. Evidence that the p2y3 receptor is the avian homologue of the mammalian P2Y6 receptor. Mol. Pharmacol. 1998;54:541–546. doi: 10.1124/mol.54.3.541. [DOI] [PubMed] [Google Scholar]
- 52.Varani K, Vincenzi F, Merighi S, Gessi S, Borea PA. Biochemical and pharmacological role of A(1) adenosine receptors and their modulation as novel therapeutic strategy. Protein Rev. 2017;19(1051):193–232. doi: 10.1007/5584_2017_61. [DOI] [PubMed] [Google Scholar]
- 53.Du Y, Yu J, Du L, Tang J, Feng WH. Cordycepin enhances Epstein-Barr virus lytic infection and Epstein-Barr virus-positive tumor treatment efficacy by doxorubicin. Cancer Lett. 2016;376:240–248. doi: 10.1016/j.canlet.2016.04.001. [DOI] [PubMed] [Google Scholar]
- 54.Ryu E, et al. Cordycepin is a novel chemical suppressor of Epstein-Barr virus replication. Oncoscience. 2014;1:866–881. doi: 10.18632/oncoscience.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Choi SJ, et al. Adenosine induces EBV lytic reactivation through ADORA1 in EBV-associated gastric carcinoma. Int. J. Mol. Sci. 2019 doi: 10.3390/ijms20061286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lazarowski ER, Boucher RC. Purinergic receptors in airway hydration. Biochem. Pharmacol. 2021 doi: 10.1016/j.bcp.2020.114387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Granja TF, et al. Adenosine receptor Adora2b plays a mechanistic role in the protective effect of the volatile anesthetic sevoflurane during liver ischemia/reperfusion. Anesthesiology. 2016;125:547–560. doi: 10.1097/Aln.0000000000001234. [DOI] [PubMed] [Google Scholar]
- 58.Zimmerman MA, et al. Signaling through hepatocellular A2B adenosine receptors dampens ischemia and reperfusion injury of the liver (Retraction of Vol 110, Pg 12012, 2013) Proc. Natl. Acad. Sci. U.S.A. 2017;114:E5279–E5279. doi: 10.1073/pnas.1708494114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fishman P, Bar-Yehuda S, Liang BT, Jacobson KA. Pharmacological and therapeutic effects of A3 adenosine receptor agonists. Drug Discov. Today. 2012;17:359–366. doi: 10.1016/j.drudis.2011.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bar-Yehuda S, et al. The A3 adenosine receptor agonist CF102 induces apoptosis of hepatocellular carcinoma via de-regulation of the Wnt and NF-kappaB signal transduction pathways. Int. J. Oncol. 2008;33:287–295. [PubMed] [Google Scholar]
- 61.Fishman P, et al. An agonist to the A3 adenosine receptor inhibits colon carcinoma growth in mice via modulation of GSK-3 beta and NF-kappa B. Oncogene. 2004;23:2465–2471. doi: 10.1038/sj.onc.1207355. [DOI] [PubMed] [Google Scholar]
- 62.Sarwar S, et al. Human papillomavirus, tobacco, and poor oral hygiene can act synergetically, modulate the expression of the nuclear factor kappa B signaling pathway for the development and progression of head and neck cancer in the Pakistani population. Chin. Med. J. (Engl.) 2022 doi: 10.1097/CM9.0000000000001970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mazziotta C, et al. Cancer biology and molecular genetics of A3 adenosine receptor. Oncogene. 2022;41:301–308. doi: 10.1038/s41388-021-02090-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kumar S, et al. Nuclear Factor kappa B is central to Marek's Disease herpesvirus induced neoplastic transformation of CD30 expressing lymphocytes in-vivo. BMC Syst. Biol. 2012 doi: 10.1186/1752-0509-6-123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fishman P, et al. The PI3K-NF-kappaB signal transduction pathway is involved in mediating the anti-inflammatory effect of IB-MECA in adjuvant-induced arthritis. Arthr. Res. Ther. 2006;8:R33. doi: 10.1186/ar1887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Varani K, et al. Expression and functional role of adenosine receptors in regulating inflammatory responses in human synoviocytes. Brit. J. Pharmacol. 2010;160:101–115. doi: 10.1111/j.1476-5381.2010.00667.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Liu H, Xia Y. Beneficial and detrimental role of adenosine signaling in diseases and therapy. J. Appl. Physiol. 2015;119:1173–1182. doi: 10.1152/japplphysiol.00350.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Day YJ, et al. Protection from ischemic liver injury by activation of A2A adenosine receptors during reperfusion: Inhibition of chemokine induction. Am. J. Physiol. Gastrointest. Liver Physiol. 2004;286:G285–293. doi: 10.1152/ajpgi.00348.2003. [DOI] [PubMed] [Google Scholar]
- 69.Fausther M. Extracellular adenosine: A critical signal in liver fibrosis. Am. J. Physiol.-Gastr. L. 2018;315:G12–G19. doi: 10.1152/ajpgi.00006.2018. [DOI] [PubMed] [Google Scholar]
- 70.Ohta A, Sitkovsky M. Role of G-protein-coupled adenosine receptors in downregulation of inflammation and protection from tissue damage. Nature. 2001;414:916–920. doi: 10.1038/414916a. [DOI] [PubMed] [Google Scholar]
- 71.Cohen S, Fishman P. Targeting the A3 adenosine receptor to treat cytokine release syndrome in cancer immunotherapy. Drug Des. Devel. Ther. 2019;13:491–497. doi: 10.2147/DDDT.S195294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Layhadi JA, Fountain SJ. P2X4 Receptor-dependent Ca(2+) influx in model human monocytes and macrophages. Int. J. Mol. Sci. 2017 doi: 10.3390/ijms18112261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Radford KM, Virginio C, Surprenant A, North RA, Kawashima E. Baculovirus expression provides direct evidence for heteromeric assembly of P2X2 and P2X3 receptors. The J. Neurosci. . 1997;17:6529–6533. doi: 10.1523/JNEUROSCI.17-17-06529.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pelleg A, Hurt CM. Mechanism of action of ATP on canine pulmonary vagal C fibre nerve terminals. J. Physiol.-Lond. 1996;490:265–275. doi: 10.1113/jphysiol.1996.sp021142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chou YL, Mori N, Canning BJ. Opposing effects of bronchopulmonary C-fiber subtypes on cough in guinea pigs. Am. J. Physiol.-Reg. 2018;I(314):R489–R498. doi: 10.1152/ajpregu.00313.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mai YL, et al. P2X receptors: Potential therapeutic targets for symptoms associated with lung cancer - a mini review. Front. Oncol. 2021 doi: 10.3389/fonc.2021.691956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rong W, et al. Pivotal role of nucleotide P2X2 receptor subunit of the ATP-gated ion channel mediating ventilatory responses to hypoxia. The J. Neurosci. 2003;23:11315–11321. doi: 10.1523/JNEUROSCI.23-36-11315.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ford AP, Undem BJ. The therapeutic promise of ATP antagonism at P2X3 receptors in respiratory and urological disorders. Front. Cell Neurosci. 2013 doi: 10.3389/fncel.2013.00267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kwong K, Kollarik M, Nassenstein C, Ru F, Undem BJ. P2X2 receptors differentiate placodal vs. neural crest C-fiber phenotypes innervating guinea pig lungs and esophagus. Am. J. Physiol.-Lung C. 2008;295:L858–L865. doi: 10.1152/ajplung.90360.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Nassenstein C, et al. Phenotypic distinctions between neural crest and placodal derived vagal C-fibres in mouse lungs. J. Physiol.-Lond. 2010;588:4769–4783. doi: 10.1113/jphysiol.2010.195339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Stokes L, Surprenant A. Dynamic regulation of the P2X4 receptor in alveolar macrophages by phagocytosis and classical activation. Eur. J. Immunol. 2009;39:986–995. doi: 10.1002/eji.200838818. [DOI] [PubMed] [Google Scholar]
- 82.Antonioli L, et al. P2X4 receptors, immunity, and sepsis. Curr. Opin. Pharmacol. 2019;47:65–74. doi: 10.1016/j.coph.2019.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Haveman JW, et al. The central role of monocytes in the pathogenesis of sepsis: Consequences for immunomonitoring and treatment. Neth. J. Med. 1999;55:132–141. doi: 10.1016/S0300-2977(98)00156-9. [DOI] [PubMed] [Google Scholar]
- 84.Schneider S, Merfort I, Idzko M, Zech A. Blocking P2X purinoceptor 4 signalling alleviates cigarette smoke induced pulmonary inflammation. Respir. Res. 2022;23:148. doi: 10.1186/s12931-022-02072-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kim H, et al. The purinergic receptor P2X5 regulates inflammasome activity and hyper-multinucleation of murine osteoclasts. Sci. Rep. 2017;7:196. doi: 10.1038/s41598-017-00139-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Jeong YH, et al. Mice lacking the purinergic receptor P2X5 exhibit defective inflammasome activation and early susceptibility to listeria monocytogenes. J. Immunol. 2020;205:760–766. doi: 10.4049/jimmunol.1901423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wang H, et al. P2RX7 sensitizes Mac-1/ICAM-1-dependent leukocyte-endothelial adhesion and promotes neurovascular injury during septic encephalopathy. Cell Res. 2015;25:674–690. doi: 10.1038/cr.2015.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Wang S, et al. Blockage of P2X7 attenuates acute lung injury in mice by inhibiting NLRP3 inflammasome. Int. Immunopharmacol. 2015;27:38–45. doi: 10.1016/j.intimp.2015.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Mishra A, et al. A critical role for P2X7 receptor-induced VCAM-1 shedding and neutrophil infiltration during acute lung injury. J. Immunol. 2016;197:2828–2837. doi: 10.4049/jimmunol.1501041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zhao HL, Chen YJ, Feng H. P2X7 receptor-associated programmed cell death in the pathophysiology of hemorrhagic stroke. Curr. Neuropharmacol. 2018;16:1282–1295. doi: 10.2174/1570159x16666180516094500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Bian S, et al. P2X7 integrates PI3K/AKT and AMPK-PRAS40-mTOR signaling pathways to mediate tumor cell death. PLoS ONE. 2013;8:e60184. doi: 10.1371/journal.pone.0060184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Savio LEB, et al. CD39 limits P2X7 receptor inflammatory signaling and attenuates sepsis-induced liver injury. J. Hepatol. 2017;67:716–726. doi: 10.1016/j.jhep.2017.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Savio LEB, de Andrade Mello P, da Silva CG, Coutinho-Silva R. The P2X7 receptor in inflammatory diseases: Angel or Demon? Front Pharmacol. 2018;9:52. doi: 10.3389/fphar.2018.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Sellers LA, et al. Adenosine nucleotides acting at the human P2Y1 receptor stimulate mitogen-activated protein kinases and induce apoptosis. J. Biol. Chem. 2001;276:16379–16390. doi: 10.1074/jbc.M006617200. [DOI] [PubMed] [Google Scholar]
- 95.Zerr M, et al. Major contribution of the P2Y(1)receptor in purinergic regulation of TNFalpha-induced vascular inflammation. Circulation. 2011;123:2404–2413. doi: 10.1161/CIRCULATIONAHA.110.002139. [DOI] [PubMed] [Google Scholar]
- 96.Ferrari D, la Sala A, Milani D, Celeghini C, Casciano F. Purinergic signaling in controlling macrophage and T cell functions during atherosclerosis development. Front. Immunol. 2021 doi: 10.3389/fimmu.2020.617804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Niethamer TK, et al. Defining the role of pulmonary endothelial cell heterogeneity in the response to acute lung injury. Elife. 2020 doi: 10.7554/eLife.53072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Burnstock G. Purinergic signalling in endocrine organs. Purinergic Signal. 2014;10:189–231. doi: 10.1007/s11302-013-9396-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Schuchardt M, Tolle M, van der Giet M. P2Y purinoceptors as potential emerging therapeutical target in vascular disease. Curr. Pharm. Des. 2012;18:6169–6180. doi: 10.2174/138161212803582504. [DOI] [PubMed] [Google Scholar]
- 100.Uehara K, Uehara A. P2Y1, P2Y6, and P2Y12 receptors in rat splenic sinus endothelial cells: An immunohistochemical and ultrastructural study. Histochem. Cell Biol. 2011;136:557–567. doi: 10.1007/s00418-011-0859-2. [DOI] [PubMed] [Google Scholar]
- 101.Geary C, et al. Increased susceptibility of purinergic receptor-deficient mice to lung infection with Pseudomonas aeruginosa. Am. J. Physiol. Lung Cellul. Mol. Physiol. 2005;289:L890–895. doi: 10.1152/ajplung.00428.2004. [DOI] [PubMed] [Google Scholar]
- 102.Klambt V, et al. A novel function for P2Y2 in myeloid recipient-derived cells during graft-versus-host disease. J. Immunol. 2015;195:5795–5804. doi: 10.4049/jimmunol.1501357. [DOI] [PubMed] [Google Scholar]
- 103.Vanderstocken G, et al. Protective role of P2Y2 receptor against lung infection induced by pneumonia virus of mice. PLoS ONE. 2012;7:e50385. doi: 10.1371/journal.pone.0050385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Kouzaki H, Iijima K, Kobayashi T, O'Grady SM, Kita H. The danger signal, extracellular ATP, is a sensor for an airborne allergen and triggers IL-33 release and innate Th2-type responses. J. Immunol. 2011;186:4375–4387. doi: 10.4049/jimmunol.1003020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Muller T, Vieira RD, Grimm M, Cicko S, Idzko M. The purinergic receptor P2Y2 mediates chemotaxis of dendritic cells and eosinophils in allergic lung inflammation. Allergy. 2010;65:26–27. doi: 10.1111/j.1398-9995.2010.02426.x. [DOI] [PubMed] [Google Scholar]
- 106.Ayata CK, et al. Purinergic P2Y(2) receptors promote neutrophil infiltration and hepatocyte death in mice with acute liver injury. Gastroenterology. 2012;143:1620. doi: 10.1053/j.gastro.2012.08.049. [DOI] [PubMed] [Google Scholar]
- 107.Ferrari D, et al. Eosinophils and purinergic signaling in health and disease. Front. Immunol. 2020 doi: 10.3389/fimmu.2020.01339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hitzel J, et al. Oxidized phospholipids regulate amino acid metabolism through MTHFD2 to facilitate nucleotide release in endothelial cells. Nat. Commun. 2018;9:2292. doi: 10.1038/s41467-018-04602-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jin H, Ko YS, Park SW, Kim HJ. P2Y2R activation by ATP induces oxLDL-mediated inflammasome activation through modulation of mitochondrial damage in human endothelial cells. Free Radic. Biol. Med. 2019;136:109–117. doi: 10.1016/j.freeradbiomed.2019.04.004. [DOI] [PubMed] [Google Scholar]
- 110.Eun SY, Park SW, Lee JH, Chang KC, Kim HJ. P2Y(2)R activation by nucleotides released from oxLDL-treated endothelial cells (ECs) mediates the interaction between ECs and immune cells through RAGE expression and reactive oxygen species production. Free Radical Bio. Med. 2014;69:157–166. doi: 10.1016/j.freeradbiomed.2014.01.022. [DOI] [PubMed] [Google Scholar]
- 111.Yuan P, et al. Lipoprotein metabolism differs between Marek's disease susceptible and resistant chickens. Poult. Sci. 2012;91:2598–2605. doi: 10.3382/ps.2011-01843. [DOI] [PubMed] [Google Scholar]
- 112.Trapp-Fragnet L, et al. Marek's disease virus prolongs survival of primary chicken B-cells by inducing a senescence-like phenotype. PLoS Pathog. 2021;17:e1010006. doi: 10.1371/journal.ppat.1010006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chu Q, et al. Marek's disease virus infection induced mitochondria changes in chickens. Int. J.Mol. Sci. 2019 doi: 10.3390/ijms20133150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Vieira RP, et al. Purinergic receptor type 6 contributes to airway inflammation and remodeling in experimental allergic airway inflammation. Am. J. Respir. Crit. Care Med. 2011;184:215–223. doi: 10.1164/rccm.201011-1762OC. [DOI] [PubMed] [Google Scholar]
- 115.Huipao N, et al. P2Y6 receptors are involved in mediating the effect of inactivated avian influenza virus H5N1 on IL-6 & CXCL8 mRNA expression in respiratory epithelium. PLoS ONE. 2017;12:e0176974. doi: 10.1371/journal.pone.0176974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Li R, et al. Extracellular UDP and P2Y6 function as a danger signal to protect mice from vesicular stomatitis virus infection through an increase in IFN-beta production. J. Immunol. 2014;193:4515–4526. doi: 10.4049/jimmunol.1301930. [DOI] [PubMed] [Google Scholar]
- 117.Lee M, et al. P2Y5 is a G alpha(i), G alpha(12/13) G protein-coupled receptor activated by lysophosphatidic acid that reduces intestinal cell adhesion. Am. J. Physiol.-Gastr. L. 2009;297:G641–G654. doi: 10.1152/ajpgi.00191.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Takahashi K, et al. Lysophosphatidic acid (LPA) signaling via LPA4 and LPA6 negatively regulates cell motile activities of colon cancer cells. Biochem. Biophys. Res. Commun. 2017;483:652–657. doi: 10.1016/j.bbrc.2016.12.088. [DOI] [PubMed] [Google Scholar]
- 119.Yang YM, Kuen DS, Chung Y, Kurose H, Kim SG. Galpha12/13 signaling in metabolic diseases. Exp. Mol. Med. 2020;52:896–910. doi: 10.1038/s12276-020-0454-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Richerioux N, et al. Rho-ROCK and Rac-PAK signaling pathways have opposing effects on the cell-to-cell spread of Marek's Disease Virus. PLoS ONE. 2012;7:e44072. doi: 10.1371/journal.pone.0044072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Sturm A, Sudermann T, Schulte KM, Goebell H, Dignass FU. Modulation of intestinal epithelial wound healing in vitro and in vivo by lysophosphatidic acid. Gastroenterology. 1999;117:368–377. doi: 10.1053/gast.1999.0029900368. [DOI] [PubMed] [Google Scholar]
- 122.Yanagida K, Ishii S, Hamano F, Noguchi K, Shimizu T. LPA4/p2y9/GPR23 mediates rho-dependent morphological changes in a rat neuronal cell line. J. Biol. Chem. 2007;282:5814–5824. doi: 10.1074/jbc.M610767200. [DOI] [PubMed] [Google Scholar]
- 123.Cantagrel V, et al. Disruption of a new X linked gene highly expressed in brain in a family with two mentally retarded males. J. Med. Genet. 2004;41:736–742. doi: 10.1136/jmg.2004.021626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Fujiwara SI, et al. Transforming activity of purinergic receptor P2Y, G protein coupled, 8 revealed by retroviral expression screening. Leuk. Lymphoma. 2007;48:978–986. doi: 10.1080/10428190701225882. [DOI] [PubMed] [Google Scholar]
- 125.Hertzberg L, et al. Down syndrome acute lymphoblastic leukemia, a highly heterogeneous disease in which aberrant expression of CRLF2 is associated with mutated JAK2: A report from the International BFM Study Group. Blood. 2010;115:1006–1017. doi: 10.1182/blood-2009-08-235408. [DOI] [PubMed] [Google Scholar]
- 126.Morak M, Attarbaschi A, Fischer S. Small sizes and indolent evolutionary dynamics challenge the potential role of P2RY8-CRLF2-harboring clones as main relapse-driving force in childhood ALL (vol 120, pg 5134, 2012) Blood. 2013;122:1328–1328. doi: 10.1182/blood-2013-07-515650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Rao S, Garrett-Sinha LA, Yoon J, Simon MC. The Ets factors PU.1 and Spi-B regulate the transcription in vivo of P2Y10, a lymphoid restricted heptahelical receptor. J. Biol. Chem. 1999;274:34245–34252. doi: 10.1074/jbc.274.48.34245. [DOI] [PubMed] [Google Scholar]
- 128.Hwang SM, et al. Lysophosphatidylserine receptor P2Y10: A G protein-coupled receptor that mediates eosinophil degranulation. Clin. Exp. Allergy. 2018;48:990–999. doi: 10.1111/cea.13162. [DOI] [PubMed] [Google Scholar]
- 129.Makide K, et al. Novel lysophosphoplipid receptors: Their structure and function. J. Lipid Res. 2014;55:1986–1995. doi: 10.1194/jlr.R046920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Murakami M, Shiraishi A, Tabata K, Fujita N. Identification of the orphan GPCR, P2Y(10) receptor as the sphingosine-1-phosphate and lysophosphatidic acid receptor. Biochem. Biophys. Res. Commun. 2008;371:707–712. doi: 10.1016/j.bbrc.2008.04.145. [DOI] [PubMed] [Google Scholar]
- 131.Im DS. Intercellular lipid mediators and GPCR drug discovery. Biomol. Ther. 2013;21:411–422. doi: 10.4062/biomolther.2013.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Gurusamy M, et al. G-protein-coupled receptor P2Y10 facilitates chemokine-induced CD4 T cell migration through autocrine/paracrine mediators. Nat. Commun. 2021 doi: 10.1038/s41467-021-26882-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Thompson RJ, Sayers I, Kuokkanen K, Hall IP. Purinergic receptors in the airways: Potential therapeutic targets for asthma? Front. Allergy. 2021;2:677677. doi: 10.3389/falgy.2021.677677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Maynard JP, et al. P2X3 purinergic receptor overexpression is associated with poor recurrence-free survival in hepatocellular carcinoma patients. Oncotarget. 2015;6:41162–41179. doi: 10.18632/oncotarget.6240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Lu R, Zhang Z, Jiang C. Recent progress on the discovery of P2Y14 receptor antagonists. Eur. J. Med. Chem. 2019;175:34–39. doi: 10.1016/j.ejmech.2019.04.068. [DOI] [PubMed] [Google Scholar]
- 136.Sesma JI, et al. UDP-glucose promotes neutrophil recruitment in the lung. Purinergic Signal. 2016;12:627–635. doi: 10.1007/s11302-016-9524-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Li H, et al. P2Y14 receptor has a critical role in acute gouty arthritis by regulating pyroptosis of macrophages. Cell Death Dis. 2020;11:394. doi: 10.1038/s41419-020-2609-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Abdul-Careem MF, et al. Induction of innate host responses in the lungs of chickens following infection with a very virulent strain of Marek's disease virus. Virology. 2009;393:250–257. doi: 10.1016/j.virol.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 139.Haq K, et al. Effects of interferon-gamma knockdown on vaccine-induced immunity against Marek's disease in chickens. Can. J. Vet. Res. 2015;79:1–7. [PMC free article] [PubMed] [Google Scholar]
- 140.Ma JW, et al. Glycogen metabolism regulates macrophage-mediated acute inflammatory responses. Nat. Commun. 2020 doi: 10.1038/s41467-020-15636-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Gilfernandez G, et al. Antiviral activity of uridine 5'-diphosphate glucose analogs against some enveloped viruses in cell-culture. Antiviral Res. 1987;8:299–310. doi: 10.1016/S0166-3542(87)80007-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors declare that all data supporting the findings of this work are available within the paper.