Abstract
Background:
Children in mental health crises are increasingly admitted to children’s hospitals awaiting inpatient psychiatric placement. During hospitalization, patients may exhibit acute agitation prompting pharmacologic restraint use.
Objective:
To determine hospital-level incidence and variation of pharmacologic restraint use among children admitted for mental health conditions in children’s hospitals.
Design, Setting, and Participants:
We examined data for children (5 to ≤18 years) admitted to children’s hospitals with a primary mental health condition from 2018 to 2020 using the Pediatric Health Information System database. Hospital rates of parenteral pharmacologic restraint use per 1000 mental health bed days were determined and compared after adjusting for patient-level and demographic factors. Cluster analysis (k-means) was used to group hospitals based on overall restraint use (rate quartiles) and drug class. Hospital-level factors for pharmacologic restraint use were compared.
Results:
Of 29,834 included encounters, 3747 (12.6%) had pharmacologic restraint use. Adjusted hospital rates ranged from 35 to 389 pharmacologic restraint use days per 1000 mental health bed days with a mean of 175 (standard deviation: 72). Cluster analysis revealed three hospitals were high utilizers of all drug classes. No significant differences in pharmacologic restraint use were found in the hospital-level analysis.
Conclusions:
Children’s hospitals demonstrate wide variation in pharmacologic restraint rates for mental health hospitalizations, with a 10-fold difference in adjusted rates between highest and lowest utilizers, and high overall utilizers order medications across all drug classes.
INTRODUCTION
In 2021, the American Academy of Pediatrics, the American Academy of Child and Adolescent Psychiatry, and the Children’s Hospital Association declared a national state of emergency for children’s mental health.1 Part of this declaration was in response to the rising need for mental health services for children. In 2009, 3% of all admissions to children’s hospitals were for a primary mental health diagnosis.2 From 2008 to 2015, suicidal ideation or attempt increased to 2% of all pediatric emergency department (ED) encounters, and ED visits for all mental health problems comprised 5% of total visits.3–5
Children and adolescents presenting to the ED in a mental health crisis who require inpatient psychiatric treatment are ideally transferred directly to a psychiatric facility.5 However, pediatric psychiatric bed shortages, a surge in psychiatric hospitalization needs, and limitations in access due to insurance coverage can create long wait times.6–8 While awaiting disposition, many children with mental health conditions are admitted to acute care nonpsychiatric children’s hospitals. In previous studies, this practice has been termed “psychiatric boarding.”6,9,10 A systematic review showed an average ED boarding time of 5–41 h and 2–3 days on inpatient units, with a range of 1–51 days.11
Patients boarding on inpatient units may exhibit aggression and agitation due to underlying psychiatric conditions, an unfamiliar environment, or increased stimulation.12,13 A survey of pediatric hospitalists found 20% of providers managed acute agitation and behavioral escalation more than once per week, and 34% three times a month.14 Aggression and agitation may lead to safety concerns for the patient and staff necessitating physical and/or pharmacologic restraints.15 Pharmacologic restraint is defined as the deliberate use of medication to control behavior and/or restrict movement when a patient’s behavior places themselves or others at risk of imminent harm.16 There are no expert guidelines for pharmacologic restraint use in hospitalized children and adolescents. Most guidelines on pharmacologic restraint focus on use in the ED or psychiatric hospitals.17–20 A recent study identified 3.5% of pediatric mental health ED visits required pharmacologic restraint.21 Despite this work, little is known about care practice surrounding pharmacologic restraint use in the acute care nonpsychiatric pediatric hospital setting. The objective of this study was to determine hospital-level incidence and variation of pharmacologic restraint use among children admitted for a primary diagnosis of a mental health condition in acute care children’s hospitals.
METHODS
Study design and database
We conducted a multicenter, retrospective cohort study using data from the Pediatric Health Information System (PHIS) database, which is an administrative database that contains demographic, billing, and resource use data from 49 tertiary-care pediatric hospitals in the United States affiliated with the Children’s Hospital Association (Lenexa, KS). Excluding healthy newborns, this database accounts for 15% of all inpatient pediatric care in the United States.22 Data quality is assured through a joint effort between the Children’s Hospital Association and participating hospitals.
Study population
We examined data for children (5 to ≤18 years) hospitalized (inpatient and observation status) between January 1, 2018 and January 1, 2020, with primary mental health discharge diagnoses from acute care nonpsychiatric hospital stays. Mental health discharge diagnoses were identified using the Child and Adolescent Mental Health Disorders Classification System.23,24 This system classifies mental health disorders across the International Classification of Diseases, Tenth Revision, diagnostic coding system into 30 groups that align with the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-V) psychiatric diagnosis groups.25 We a priori excluded feeding and eating disorders, accidental or undetermined poisoning, elimination disorders, sleep–wake disorders, personality disorders, and substance abuse-related medical illness (6% of the cohort) as these diagnoses are managed distinctly from other mental health conditions. Similar to previous studies, we further categorized mental health diagnosis by type: anxiety disorders, disruptive disorders, mood disorders, neurocognitive disorders (including autism), psychotic disorders, somatic disorders, substance-related and addictive disorders, suicide or self-injury, trauma and stressor-related disorders, and other24 (Supporting Information: Table S1).
We excluded patients who died during hospitalization and patients who were admitted directly to inpatient psychiatric units from the ED. We also excluded encounters with an operating room charge since it is not possible in PHIS to ascertain if a medication was used for procedural sedation or pharmacologic restraint. For the same reason, days of a hospital stay during which the patient was in the intensive care unit (ICU) were excluded. Non-ICU days for these encounters were included in the data analysis.
Outcome measures
Medications used for pharmacologic restraint in hospitalized children were defined using emergency medicine consensus guidelines given the lack of inpatient pediatric guidelines.16–19,21,26–30 Medication indication, such as scheduled or as-needed dosing, is not available in PHIS. While oral medications may be used as a pharmacological restraint, they are more frequently used in the hospital setting as the continuation of a home medication or initiation of a new antipsychotic medication. To increase the specificity of our exposure, we restricted our pharmacologic restraint definition to parenteral use (Table 1), similar to other recent studies.21 Parenteral use in our population was defined as intramuscular or intravenous administration.
TABLE 1.
Parenteral medications defined as pharmacologic restraint
| Drug class | Drug name |
|---|---|
| Benzodiazepines | Lorazepam |
| Diazepam | |
| Midazolam | |
| Barbiturates | Phenobarbital |
| Methohexital | |
| Pentobarbital | |
| Antipsychotics | Ziprasidone |
| Aripiprazole | |
| Haloperidol | |
| Olanzapine | |
| Paliperidone | |
| Prochlorperazine | |
| Chlorpromazine | |
| Risperidone | |
| Droperidol | |
| Antihistamines | Diphenhydramine |
| Hydroxyzine | |
| Promethazine | |
| Other | Ketamine |
| Benztropine |
The primary outcome measure was individual hospital rates of pharmacologic restraint use per 1000 mental health bed days adjusted for patient-level factors. The numerator was pharmacologic restraint use days during all inpatient/observation encounters, including time spent in the ED. The denominator was 1000 mental health bed days. A mental health bed day was defined as each day of a hospitalization (ICU days excluded). One day of pharmacologic restraint use was defined as the administration of any included parenteral medication given during a 24-h period, regardless of the number of doses administered. For example, a patient who received one administration of medication for pharmacologic restraint, two administrations of the same medication, or two different medication classes were all considered one pharmacologic restraint use day. We also performed a sensitivity analysis limiting our definition of pharmacologic restraint to three antipsychotic medications (haloperidol, ziprasidone, and olanzapine), which, when administered parenterally, are medications given almost exclusively for pharmacologic restraint.
Additional analyses included the determination of pharmacologic restraint use days in which more than one drug class was used, an unadjusted/adjusted comparison of pharmacologic restraint use per 1000 mental health bed days between PHIS hospitals, a hospital-level cluster analysis of pharmacologic restraint use by drug class with resultant heat map by rate use quartiles, and an assessment of hospital-level factors that may impact hospital variation.
Covariates
Demographic variables examined included age, sex, race/ethnicity (non-Hispanic White, non-Hispanic Black, Hispanic, Asian, Other), season, the payor (government, private, other), median household income quartiles for the patient’s residential zip code, rurality of the patient’s residential zip code, and hospital disposition (home, psychiatric facility/other).
Patient-level variables included DSM-V categories (anxiety disorders, disruptive disorders, mood disorders, neurocognitive disorders, psychotic disorders, somatic disorders, substance-related and addictive disorders, suicide or self-injury, trauma and stressor-related disorders, and others), presence of complex chronic conditions (CCCs), ICU stay, length of stay, and Hospitalization Resource Intensity Scores for Kids (H-RISK). CCCs are defined as medical conditions expected to last at least 12 months, involve multiple organ systems, and have a high probability of hospitalization.31 H-RISK is a relative resource intensity weight assigned to each encounter based on their diagnosis-related groups and level of severity and is used as a proxy for severity.32
Hospital-level variables included average daily census, hospital region, mental health encounters as a total of inpatient/observation encounters, and the presence of an inpatient psychiatric unit.
Statistical analysis
We used descriptive statistics of patient-level demographic factors to characterize the cohort. We calculated the rate of pharmacologic restraint use days per 1000 mental health bed days. Hospital pharmacologic restraint rates were compared after adjusting for patient-level variables (DSM-V category, CCCs, ICU stay, length of stay, and H-RISK) and several demographic variables (age, sex, payor, and hospital disposition) using Poisson regression and accounting for hospital clustering. We used k-means clustering to assign each hospital to one of three groups based on overall patterns of restraint use (rate quartiles) and by drug class. We removed barbiturates as a drug class from this analysis due to the rarity of use through all encounters. Hospital-level factors for pharmacologic restraint use were compared as pharmacologic use days per total mental health days. We also determined the proportion of pharmacologic restraint use days that used multiple medication classes—a proxy (but underestimate) for days in which patients received >1 dose of medication. All analyses were performed using SAS, version 9.4 (SAS Institute Inc.), and p < .05 was considered statistically significant. The Vanderbilt University Medical Center Institutional Review Board determined that this study of deidentified data did not meet the criteria for human subjects research.
RESULTS
Study population
We identified 29,834 acute care hospitalizations with a primary mental health discharge diagnosis. Pharmacologic restraints were used in 3747 (12.6%) of these hospitalizations (Table 2). Children aged 10 to ≤18 comprised most of the encounters (91.4%), and the majority were female (64.3%). Across mental health diagnoses, pharmacologic restraints were used most frequently during hospitalizations for psychotic disorders (40.2%) and least often during hospitalizations for mood disorders (5.8%). The median length of stay for encounters was 2 days [interquartile range (IQR): 1–3]. There was a total of 8411 pharmacologic restraint days and 98,042 mental health bed days for an aggregated unadjusted use rate of 85.7 per 1000 mental health bed days. Of the 8441 pharmacologic restraint use days, 2149 (25.5%) days included two or more different medication classes.
TABLE 2.
Characteristics of pediatric mental health hospitalizations, 2018–2020 (N = 29,834)
| Overall | Hospitalizations without pharmacologic restraint | Hospitalizations with pharmacologic restraint | |
|---|---|---|---|
| Hospitalizations | 29,834 | 26,087 (87.4) | 3747 (12.6) |
| Age | |||
| 5–9 | 2548 (8.5) | 2159 (84.7) | 389 (15.3) |
| 10–14 | 13,015 (43.6) | 11,496 (88.3) | 1519 (11.7) |
| 15–18 | 14,271 (47.8) | 12,432 (87.1) | 1839 (12.9) |
| Sex | |||
| Female | 19,165 (64.3) | 17,040 (88.9) | 2125 (11.1) |
| Male | 10,654 (35.7) | 9033 (84.8) | 1621 (15.2) |
| Race | |||
| Non-Hispanic White | 16,732 (56.1) | 14,701 (87.9) | 2031 (12.1) |
| Non-Hispanic Black | 6198 (20.8) | 5328 (86) | 870 (14) |
| Hispanic | 3812 (12.8) | 3306 (86.7) | 506 (13.3) |
| Asian | 535 (1.8) | 462 (86.4) | 73 (13.6) |
| Other | 2557 (8.6) | 2290 (89.6) | 267 (10.4) |
| Season | |||
| Spring | 8174 (27.4) | 7147 (87.4) | 1027 (12.6) |
| Summer | 5527 (18.5) | 4778 (86.4) | 749 (13.6) |
| Fall | 8544 (28.6) | 7550 (88.4) | 994 (11.6) |
| Winter | 7589 (25.4) | 6612 (87.1) | 977 (12.9) |
| Payor | |||
| Government | 15,079 (50.5) | 13,132 (87.1) | 1947 (12.9) |
| Private | 12,874 (43.2) | 11,320 (87.9) | 1554 (12.1) |
| Other | 1881 (6.3) | 1635 (86.9) | 246 (13.1) |
| Median household income | |||
| Q1 | 5409 (18.1) | 4760 (88) | 649 (12) |
| Q2 | 19,965 (66.9) | 17,463 (87.5) | 2502 (12.5) |
| Q3 | 4333 (14.5) | 3755 (86.7) | 578 (13.3) |
| Q4 | 127 (0.4) | 109 (85.8) | 18 (14.2) |
| Patient location | |||
| Rural | 3465 (11.6) | 3063 (88.4) | 402 (11.6) |
| Urban | 25,942 (87) | 22,658 (87.3) | 3284 (12.7) |
| Hospital disposition | |||
| Home | 16,135 (54.1) | 13,874 (86) | 2261 (14) |
| Psychiatric facility/other | 16,028 (53.7) | 14,244 (88) | 1784 (12) |
| DSM-V category | |||
| Anxiety disorders | 1030 (3.5) | 915 (88.8) | 115 (11.2) |
| Disruptive disorders | 1642 (5.5) | 1338 (81.5) | 304 (18.5) |
| Mood disorders | 4792 (16.1) | 4516 (94.2) | 276 (5.8) |
| Neurocognitive disorders | 1806 (6.1) | 1438 (79.6) | 368 (20.4) |
| Othera | 2094 (7) | 1750 (83.6) | 344 (16.4) |
| Psychotic disorders | 567 (1.9) | 339 (59.8) | 228 (40.2) |
| Somatic disorders | 2281 (7.6) | 1795 (78.7) | 486 (21.3) |
| Substance-related and addictive disorders | 1050 (3.5) | 801 (76.3) | 249 (23.7) |
| Suicide or self-injury | 13,624 (45.7) | 12,331 (90.5) | 1293 (9.5) |
| Trauma and stressor-related disorders | 948 (3.2) | 864 (91.1) | 84 (8.9) |
| CCC | |||
| No | 24,824 (83.2) | 22,020 (88.7) | 2804 (11.3) |
| Yes | 5010 (16.8) | 4067 (81.2) | 943 (18.8) |
| ICUb | |||
| No | 26,345 (88.3) | 22,908 (87) | 3437 (13) |
| Yes | 3489 (11.7) | 3179 (91.1) | 310 (8.9) |
| Length of stay (days) | 2 [1, 3] | 2 [1, 3] | 2 [1, 5] |
| H-RISK | 0.9 (0.5) | 0.8 (0.5) | 1 (0.8) |
Note: Data are presented as N (%) or median [IQR].
Abbreviations: CCC, complex chronic conditions; DSM-V, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition; H-RISK, Hospitalization Resource Intensity Scores for K; ICU, intensive care unit.
Other includes mental health symptom, sexuality and gender identity disorders, and dissociative disorders.
ICU days were excluded from the primary outcome measurement.
Hospital variability
There was substantial variation in pharmacologic restraint use across hospitals ranging from 6 to 282 pharmacologic restraint use days/1000 mental health bed days with a mean of 131 (standard deviation [SD]: 59). After adjusting for patient-level and demographic factors, hospital rates ranged from 35 to 389 pharmacologic restraint use days/1000 mental health bed days with a mean of 175 (SD: 72) (Figure 1). In a sensitivity analysis limiting the definition of pharmacologic restraint use to only haloperidol, ziprasidone, and olanzapine, adjusted hospital rates ranged from 3 to 51 pharmacologic restraint use days/1000 mental health bed days with a mean of 23 (SD: 14).
FIGURE 1.
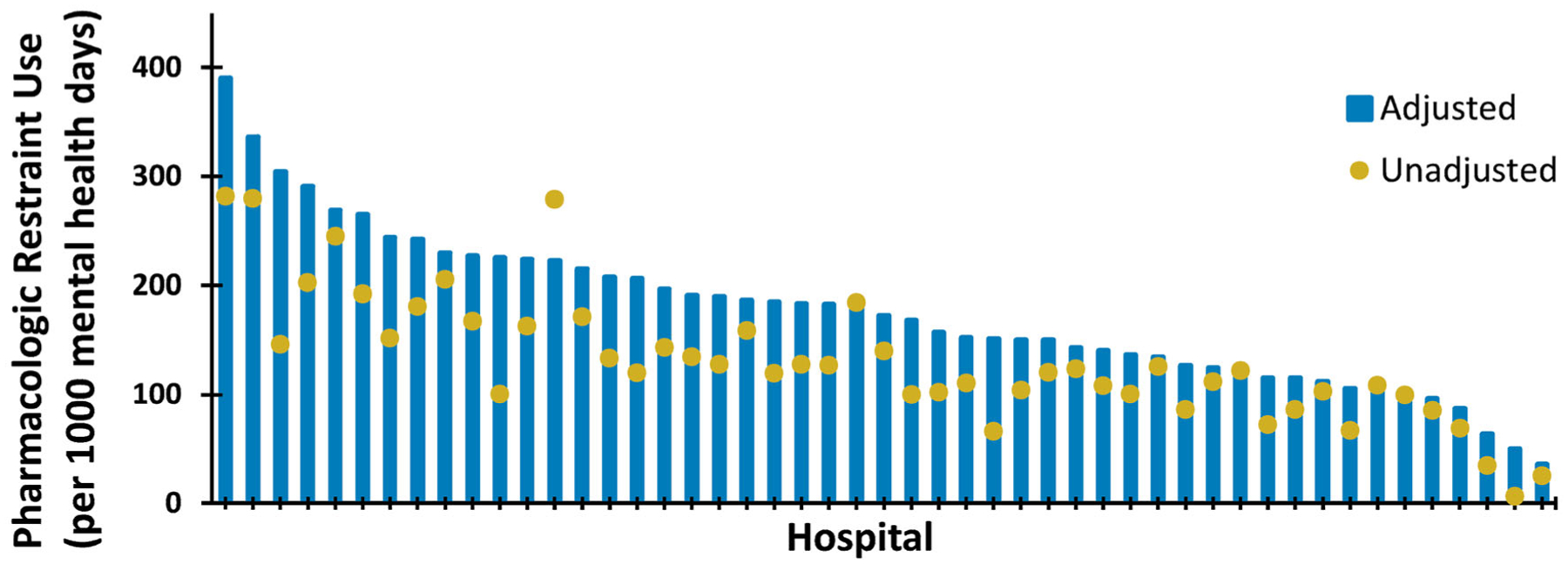
Adjusted and unadjusted pharmacologic restraint use by hospital. Covariates adjusted for include DSM-V category, CCC, ICU stay, length of stay, H-RISK, age, sex, payor, and hospital disposition. CCC, complex chronic conditions; DSM-V, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition; H-RISK, Hospitalization Resource Intensity Scores for K; ICU, intensive care unit.
The cluster analysis demonstrated three clusters of hospitals based on their use of pharmacological restraints. The first cluster contained the three highest-utilizing hospitals and was characterized by high utilization of most or all drug classes. The second cluster contained 22 hospitals that were high utilizers of one or two classes. The last cluster contained 24 hospitals and were generally low utilizers of most or all classes (Figure 2).
FIGURE 2.
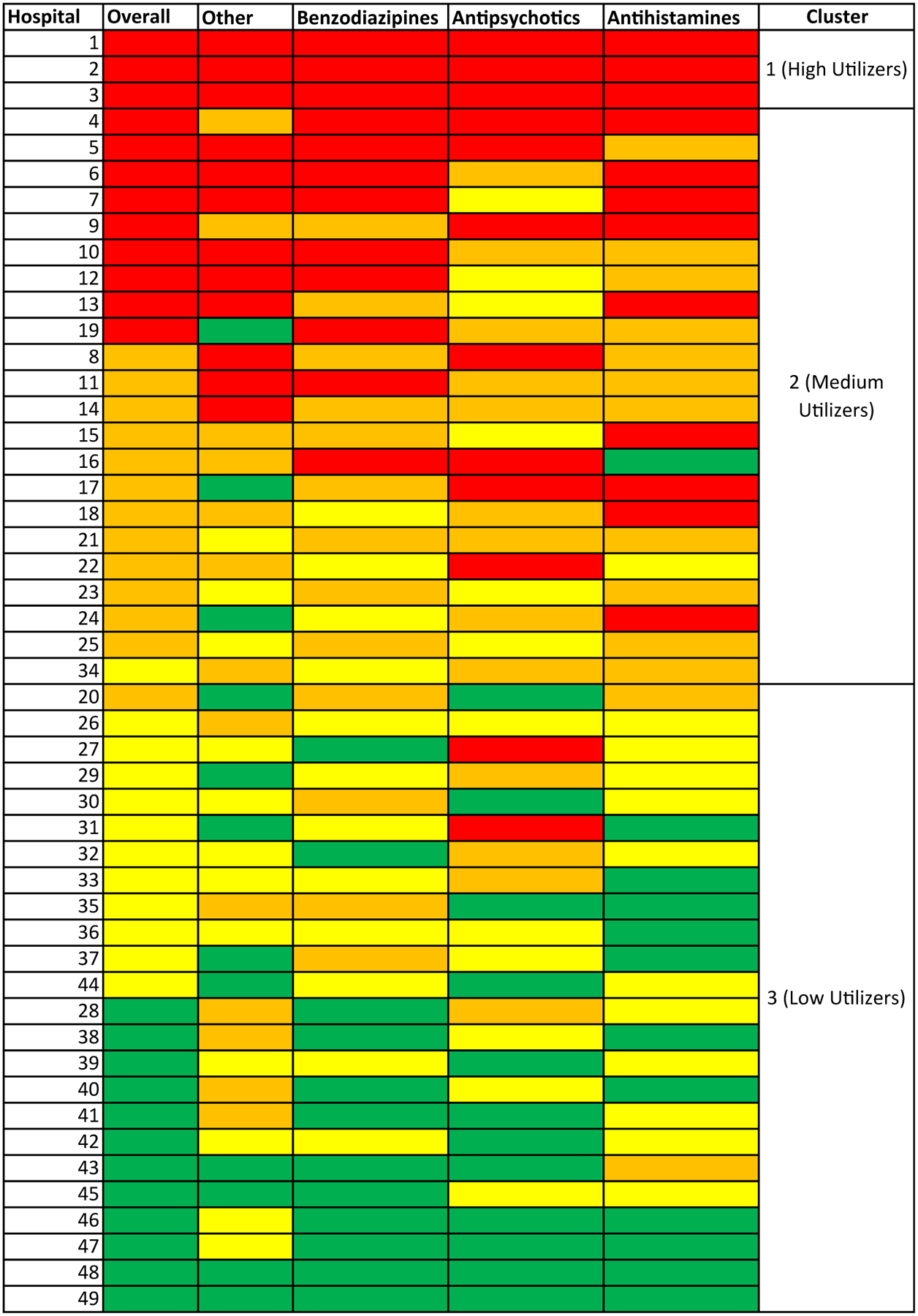
Heatmap and cluster analysis of pharmacologic restraint use. Hospitals are sorted by highest to lowest overall use with the cluster number indicated. Overall drug use and drug use by class are displayed as columns. Color values correspond to use quartiles, with red shading indicating higher use, followed by orange, yellow, and finally, green shading indicating lower use.
Differences in pharmacologic restraint use between hospitals were not significant when examining the average daily census of participating hospitals, the regional grouping of hospitals, the percent of mental health encounters relative to overall hospital encounters, or the presence of an inpatient psychiatric unit in the same facility (Table 3).
TABLE 3.
Hospital-level analysis of pharmacologic restraint use between hospitals
| Effect | Level | Number of hospitals | Median [IQR] adjusteda rate | p Value |
|---|---|---|---|---|
| Average daily census | <125 | 3 | 229.5 [111.5, 243.5] | .313 |
| 126–200 | 14 | 168.5 [123, 204.4] | ||
| 201–300 | 25 | 189.5 [150.1, 225.1] | ||
| 301+ | 7 | 134.2 [95.7, 214.4] | ||
| Hospital region | Midwest | 14 | 146.3 [119.6, 196] | .106 |
| Northeast | 6 | 110.3 [103.6, 184.7] | ||
| South | 17 | 179.9 [151.7, 214.4] | ||
| West | 12 | 215 [137.6, 228.1] | ||
| Mental health encountersb (as a total of inpatient/observation encounters) | Q1 | 12 | 185.6 [107.6, 223.7] | .099 |
| Q2 | 12 | 167 [138.2, 255.3] | ||
| Q3 | 13 | 190.8 [151.7, 243.5] | ||
| Q4 | 12 | 141.5 [91.1, 177.3] | ||
| Presence of inpatient psychiatric unit | No | 21 | 182.9 [136.4, 226.6] | .460 |
| Yes | 28 | 159.5 [119.6, 206.8] |
Abbreviations: CCC, complex chronic conditions; DSM-V, Diagnostic and Statistical Manual of Mental Disorders, 5th Edition; H-RISK, Hospitalization Resource Intensity Scores for K; ICU, intensive care unit.
Covarities adjusted for include DSM-V category, CCC, ICU stay, length of stay, H-RISK, age, sex, payor, and hospital disposition.
Quartile 1 is the bottom quartile of the number of mental health encounters and quartile 4 is the top quartile.
DISCUSSION
In this multicenter retrospective cohort study of nearly 30,000 acute care mental health hospitalizations, there was significant variation in rates of pharmacologic restraint use, with a 10-fold difference in rates for the highest and lowest utilizing hospitals after adjusting for patient-level and several demographic factors. Sensitivity analysis when restricting our definition of pharmacologic restraint to three medications highly specific for pharmacologic restraint use continued to show a 10-fold difference between the lowest and highest pharmacologic restraint utilizers. Importantly, the cluster analysis revealed different utilization patterns for groups of hospitals. To our knowledge, this is the first multicenter study to assess pharmacologic restraint use in children’s hospitals for patients boarding on inpatient pediatric units.
The overall percent of pharmacologic restraint use for primary mental health encounters in hospitalized children (12.6%) was higher than a recent publication for pediatric ED visits (3.5%).21 However, there was a similar amount of variation in pharmacologic restraint use observed between the two settings. Important distinctions exist between the ED and inpatient pediatric units when it comes to caring for patients in mental health crises. A reverse triage system occurs where patients who are more difficult to place from the ED due to high psychiatric acuity instead board on an inpatient unit due to an inability to quickly find a psychiatric bed.33 An ED may have a different level of comfort with patient agitation or specific rooms meant to support mental health patients compared to a pediatric floor. These variables contribute to the need to better understand how to manage these patients in both settings and the reasons for variability between hospitals. Patients admitted waiting for psychiatric placement can spend extensive time in the hospital.11 Thus, our determination of pharmacologic restraint use days per 1000 mental health bed days may provide a better representation of use over prolonged inpatient stays. During hospitalization, many patients are often offered a choice between oral or intramuscular PRN (pro re nata, as needed) medication when aggressive or agitated.33 Because our findings do not include oral medications and 25% of pharmacologic restraint use days involved administration of at least two medication classes, the rate of pharmacologic restraint measured in actual doses of medication may be higher than our rate presented.
Our cluster analysis results are similar to other studies on hospital variability, such as electrolyte testing or antibiotic prescribing, in that hospitals with overall high utilization tend to be high utilizers across categories.34–37 Several hospitals demonstrate low overall restraint use but high use in one drug class. These findings could be from clinical practice guidelines recommending a singular drug class as the first agent of choice. Variation could also be from provider comfort with a medication, lack of high-quality evidence on medication management for acute agitation, or different medications available on the formulary. However, it is important to note we could not assess outcomes related to hospital variation of pharmacologic restraint use. Patients boarding on an inpatient pediatric unit whose behavior compromises safety may receive pharmacologic restraint, but other methods are utilized. Ideally, prompt recognition of an impending episode of agitation or aggression followed by patient-centered verbal de-escalation is used first. When verbal de-escalation is not successful many clinicians turn to pharmacologic restraint use followed by physical restraint.14 Thus, our study exclusively looking at the use of pharmacologic restraint does not detail the entire potential spectrum of patient restraint.
Interhospital variability of the magnitude observed suggests an opportunity to standardize and improve care. Consensus national practice guidelines around the management of children with mental health crises boarding on inpatient pediatric units currently do not exist and could be the first step towards this goal. Given the known variability, further studies could help describe which type of de-escalation strategy may be best for the patient and hospital system at large.
Despite disparate access to mental health care for children across the United States, we did not find significant regional differences between hospitals in pharmacologic restraint use. The Southern and Western United States have poorer mental health access for youth.38 We hypothesized that the dearth of mental health resources and lack of preventive care in these regions may lead to children presenting with higher acuity to children’s hospitals and this may manifest as higher rates of pharmacologic restraints in these regions. However, there were no differences in our hospital-level analyses.
The volume of mental health encounters proportional to total encounters and associated inpatient psychiatric units were not statistically significant. We hypothesized that these measures would be a proxy for increased staff comfort in taking care of patients with mental health diagnoses and that these factors might lead to decreased use of pharmacological restraint. Future studies could assess additional hospital-level factors that are not available in databases like PHIS to better understand variation including the amount/bed availability of inpatient psychiatric facilities located near a hospital, the presence of a dedicated behavioral health emergency response team trained in de-escalation, the availability of child and adolescent psychiatry consultation service, the existence of standardized clinical practice guidelines at each hospital, and the frequency of physical restraint use.
Limitations
There are several limitations to this study. It includes data from large tertiary care children’s hospitals which may not be generalizable to community settings. We collected data prior to the COVID-19 pandemic. Recent data show ED visits for mental health conditions increased during the pandemic though overall visits decreased.39,40 Staffing shortages and psychiatric bed availability during the pandemic affected children’s hospitals differently, which could result in more or less pharmacologic restraint. Our definition of pharmacologic restraint as parenteral medications omits medications given orally and therefore underestimates the true rate of pharmacological restraint utilization. We also assumed that a medication given parenterally was intended as a form of pharmacologic restraint. Due to limitations in the database, our subanalysis could not determine if the same medication was given multiple times in a calendar day, only if different medication classes were used. Additionally, the PHIS database cannot differentiate whether medications are successfully administered, only that they were billed. Furthermore, physical restraints utilization was not captured in our analysis due to variable reporting within PHIS. It is possible that some of the lower pharmacologic restraints utilizing hospitals preferentially utilize physical restraints for agitated children and adolescents instead of medications. Although we intended to characterize pharmacologic restraint use for children hospitalized with mental health discharge diagnoses, the data includes all medications provided during a hospital stay, including in the ED. Thus, a small proportion of the pharmacologic restraint use days may not represent pharmacological restraint administered in the acute care inpatient environment, but instead represent the administration in the ED prior to admission to the hospital floor.
CONCLUSION
Our study demonstrates significant interhospital variation in pharmacologic restraint use for children and adolescents hospitalized in pediatric hospitals with mental health crises. Understanding reasons for variation in pharmacologic restraint use, including when and how it is used in conjunction with verbal de-escalation and physical restraints for aggressive and agitated patients, may help provide ways to reduce unnecessary variation. Ultimately, improving the quality and safety of care will be key to improving pediatric mental health care while patients await transfer to a psychiatric facility.
Supplementary Material
ACKNOWLEDGMENTS
Dr. Antoon was supported by the National Institute for Allergy and Infectious Diseases Institutes of Health (K23 AI168496). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Dr. Carroll was supported by grant number T32HS026122 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest.
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
REFERENCES
- 1.American Academy of Pediatrics. AAP-AACAP-CHA Declaration of a National Emergency in Child and Adolescent Mental Health. American Academy of Pediatrics; 2022. http://www.aap.org/en/advocacy/child-and-adolescent-healthy-mental-development/aap-aacap-cha-declaration-of-a-national-emergency-in-child-and-adolescent-mental-health/ [Google Scholar]
- 2.Bardach NS, Coker TR, Zima BT, et al. Common and costly hospitalizations for pediatric mental health disorders. Pediatrics. 2014;133(4):602–609. doi: 10.1542/peds.2013-3165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Plemmons G, Hall M, Doupnik S, et al. Hospitalization for suicide ideation or attempt: 2008–2015. Pediatrics. 2018;141(6):e20172426. doi: 10.1542/peds.2017-2426 [DOI] [PubMed] [Google Scholar]
- 4.Cutler GJ, Rodean J, Zima BT, et al. Trends in pediatric emergency department visits for mental health conditions and disposition by presence of a psychiatric unit. Acad Pediatr. 2019;19(8):948–955. doi: 10.1016/j.acap.2019.05.132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chun TH, Katz ER, Duffy SJ, Gerson RS. Challenges of managing pediatric mental health crises in the emergency department. Child Adolesc Psychiatr Clin N Am. 2015;24(1):21–40. [DOI] [PubMed] [Google Scholar]
- 6.Claudius I, Donofrio JJ, Lam CN, Santillanes G. Impact of boarding pediatric psychiatric patients on a medical ward. Hosp Pediatr. 2014;4(3):125–132. doi: 10.1542/hpeds.2013-0079 [DOI] [PubMed] [Google Scholar]
- 7.Mansbach JM, Wharff E, Austin SB, Ginnis K, Woods ER. Which psychiatric patients board on the medical service. Pediatrics. 2003;111(6 pt 1):e693–e698. [DOI] [PubMed] [Google Scholar]
- 8.Hoffmann JA, Stack AM, Monuteaux MC, Levin R, Lee LK. Factors associated with boarding and length of stay for pediatric mental health emergency visits. Am J Emerg Med. 2019;37(10):1829–1835. doi: 10.1016/j.ajem.2018.12.041 [DOI] [PubMed] [Google Scholar]
- 9.Gallagher KAS, Bujoreanu IS, Cheung P, et al. Psychiatric boarding in the pediatric inpatient medical setting: a retrospective analysis. Hosp Pediatr. 2017;7(8):444–450. doi: 10.1542/hpeds.2017-0005 [DOI] [PubMed] [Google Scholar]
- 10.Worsley D, Barrios E, Shuter M, Pettit AR, Doupnik SK. Adolescents’ Experiences during “boarding” hospitalization while awaiting inpatient psychiatric treatment following suicidal ideation or suicide attempt. Hosp Pediatr. 2019;9(11):827–833. doi: 10.1542/hpeds [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McEnany FB, Ojugbele O, Doherty JR, McLaren JL, Leyenaar JK. Pediatric mental health boarding. Pediatrics. 2020;146(4):e20201174. doi: 10.1542/peds.2020-1174 [DOI] [PubMed] [Google Scholar]
- 12.Noah A, Andrade G, DeBrocco D, et al. Patient risk factors for violent restraint use in a children’s hospital medical unit. Hosp Pediatr. 2021;11(8):833–840. doi: 10.1542/hpeds.2020-000273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gerson R, Malas N, Feuer V, et al. Best Practices for Evaluation and Treatment of Agitated Children and Adolescents (BETA) in the emergency department: consensus statement of the American Association for Emergency Psychiatry. West J Emerg Med. 2019; 20(2):409–418. doi: 10.5811/westjem.2019.1.41344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malas N Pediatric agitation and behavioral escalation: a survey of 38 North American hospitals. J Am Acad Child Adolesc Psychiatry. 2017;56(10 suppl):S42. doi: 10.1016/j.jaac.2017.07.166 [DOI] [Google Scholar]
- 15.Gangopadhyay M Barriers to management of agitation on the medical floor. J Am Acad Child Adolesc Psychiatry. 2017;56(10 suppl): S42. doi: 10.1016/j.jaac.2017.07.165 [DOI] [Google Scholar]
- 16.de Bruijn W, Daams JG, van Hunnik FJG, et al. Physical and pharmacological restraints in hospital care: protocol for a systematic review. Front Psychiatry. 2020;10:921. doi: 10.3389/fpsyt.2019.00921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carubia B, Becker A, Levine BH. Child psychiatric emergencies: updates on trends, clinical care, and practice challenges. Curr Psychiatry Rep. 2016;18(4):41. doi: 10.1007/s11920-016-0670-9 [DOI] [PubMed] [Google Scholar]
- 18.Gorman DA, Gardner DM, Murphy AL, et al. Canadian guidelines on pharmacotherapy for disruptive and aggressive behaviour in children and adolescents with attention-deficit hyperactivity disorder, oppositional defiant disorder, or conduct disorder. Can J Psychiatry. 2015;60(2):62–76. doi: 10.1177/070674371506000204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gerson R, Malas N, Mroczkowski MM. Crisis in the emergency separtment. Child Adolesc Psychiatr Clin North Am. 2018;27(3): 367–386. doi: 10.1016/j.chc.2018.02.002 [DOI] [PubMed] [Google Scholar]
- 20.Hoffmann JA, Pergjika A, Konicek CE, Reynolds SL. Pharmacologic management of acute agitation in youth in the emergency department. Pediatr Emerg Care. 2021;37(8):417–422. doi: 10.1097/PEC.0000000000002510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Foster AA, Porter JJ, Monuteaux MC, Hoffmann JA, Hudgins JD. Pharmacologic restraint use during mental health visits in pediatric emergency departments. J Pediatr. 2021;236(2):276–283.e2. doi: 10.1016/j.jpeds.2021.03.027 [DOI] [PubMed] [Google Scholar]
- 22.PHIS. Leverage Clinical and Resource Utilization Data. Children’s Hospital Association; 2022. https://www.childrenshospitals.org/phis [Google Scholar]
- 23.Zima BT, Rodean J, Hall M, Bardach NS, Coker TR, Berry JG. Psychiatric disorders and trends in resource use in pediatric hospitals. Pediatrics. 2016;138(5):e20160909. doi: 10.1542/peds.2016-0909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carroll AR, Hall M, Brown CM, et al. Association of race/ethnicity and social determinants with rehospitalization for mental health conditions at acute care children’s hospitals. J Pediatr. 2022;240: 228–234.e1. doi: 10.1016/j.jpeds.2021.08.078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013. [Google Scholar]
- 26.Rudolf F, Hollenbach K, Carstairs KL, Carstairs SD. A retrospective review of antipsychotic medications administered to psychiatric patients in a tertiary care pediatric emergency department. J Pediatr Pharmacol Ther. 2019;24(3):234–237. doi: 10.5863/1551-6776-24.3.234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kowalski JM, Kopec KT, Lavelle J, Osterhoudt K. A novel agent for management of agitated delirium: a case series of ketamine utilization in the pediatric emergency department. Pediatr Emerg Care. 2017;33(9):e58–e62. doi: 10.1097/PEC.0000000000000578 [DOI] [PubMed] [Google Scholar]
- 28.Kendrick JG, Goldman RD, Carr RR. Pharmacologic management of agitation and aggression in a pediatric emergency department—a retrospective cohort study. J Pediatr Pharmacol Ther. 2018;23(6): 455–459. doi: 10.5863/1551-6776-23.6.455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dorfman DH, Mehta SD. Restraint use for psychiatric patients in the pediatric emergency department. Pediatr Emerg Care. 2006;22(1): 7–12. doi: 10.1097/01.pec.0000195758.12447.69 [DOI] [PubMed] [Google Scholar]
- 30.Holloman G, Zeller S. Overview of Project BETA: best practices in evaluation and treatment of agitation. West J Emerg Med. 2012; 13(1):1–2. doi: 10.5811/westjem.2011.9.6865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr. 2014;14(1):199. doi: 10.1186/1471-2431-14-199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Richardson T, Rodean J, Harris M, Berry J, Gay JC, Hall M. Development of Hospitalization Resource Intensity Scores for Kids (H-RISK) and comparison across pediatric populations. J Hosp Med. 2018;13(9):602–608. doi: 10.12788/jhm.2948 [DOI] [PubMed] [Google Scholar]
- 33.Carlson GA, Chua J, Pan K, et al. Behavior modification is associated with reduced psychotropic medication use in children with aggression in inpatient treatment: a retrospective cohort study. J Am Acad Child Adolesc Psychiatry. 2020;59(5):632–641.e4. doi: 10.1016/j.jaac.2019.07.940 [DOI] [PubMed] [Google Scholar]
- 34.Gerber JS, Newland JG, Coffin SE, et al. Variability in antibiotic use at children’s hospitals. Pediatrics. 2010;126(6):1067–1073. doi: 10.1542/peds.2010-1275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brogan TV, Hall M, Williams DJ, et al. Variability in processes of care and outcomes among children hospitalized with community-acquired pneumonia. Pediatr Infect Dis J. 2012;31(10): 1036–1041. doi: 10.1097/INF.0b013e31825f2b10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Neubauer HC, Hall M, Wallace SS, et al. Variation in diagnostic test use and associated outcomes in Staphylococcal scalded skin syndrome at children’s hospitals. Hosp Pediatr. 2018;8(9):530–537. doi: 10.1542/hpeds.2018-0032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tchou MJ, Hall M, Shah SS, et al. Patterns of electrolyte testing at children’s hospitals for common inpatient diagnoses. Pediatrics. 2019;144(1):e20181644. doi: 10.1542/peds.2018-1644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mental Health America. Ranking the States. Mental Health America; 2022. https://www.mhanational.org/issues/ranking-states [Google Scholar]
- 39.Krass P, Dalton E, Doupnik SK, Esposito J. US pediatric emergency department visits for mental health conditions during the COVID-19 pandemic. JAMA Network Open. 2021;4(4):e218533. doi: 10.1001/jamanetworkopen.2021.8533 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Radhakrishnan L, Carey K, Hartnett KP, et al. Pediatric emergency department visits before and during the COVID-19 pandemic—United States, January 2019–January 2022. Morb Mortal Wkly Rep. 2022;71(8):313–318. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


