Abstract
Background:
Chronic myeloid leukemia (CML) is mostly asymptomatic at diagnosis. Intracerebral hemorrhage (ICH), as the first presentation of CML in its chronic phase (CP) has only once been reported in the literature. In addition, CML (CP) patients developing ICH are equally rare, with only eight cases reported. ICH is more commonly associated with CML progressing to its end stage (accelerated phase [AP] and blast crisis [BC]). The pathophysiology of ICH in CML-CP is postulated to be due to leukostasis, unlike in the CML-AP/BC, where thrombocytopenia and coagulopathy are the underlying mechanisms. This case adds to the scarce literature on a rare and challenging complication of ICH in CML-CP, especially as these patients tend to rebleed and management is uncertain.
Case Description:
A 22-year-old male presented with a 2-week history of headaches and vomiting, associated with a 1-week history of the left-sided weakness. Initial blood work revealed hyperleukocytosis. The patient was investigated for CML with intracranial involvement. During his stay, his Glasgow coma score (GCS) dropped (from 14 to 11), prompting an urgent CT scan which revealed a large resolving ICH with perifocal edema and midline shift. A decompressive hemicraniectomy with expansion duraplasty was performed to alleviate the mass effect and reduce intracranial pressure. Three hours postoperatively, the patient developed an extradural hematoma which needed prompt evacuation. A postoperative CT revealed an improved midline shift, and after 7 days, his GCS improved to 15, and he began oncological treatment. Neurological symptoms were experienced by our patient at presentation with hyperleukocytosis on full blood count, which may implicate leukostasis as an underlying mechanism.
Conclusion:
Even in the CP, CML patients presenting with mild neurological symptoms should be investigated to exclude intracranial bleeds. As these patients tend to rebleed, they should be conservatively managed unless there is a need to alleviate intracranial pressure.
Keywords: Chronic myeloid leukemia, Chronic phase, Hyperleukocytosis, Intracerebral hemorrhage, Intracranial involvement, Leukostasis

INTRODUCTION
Chronic myeloid leukemia (CML) is a myeloproliferative disorder where there is neoplastic proliferation of mature myeloid lineage cells.[5] CML accounts for between one and two cases per 100,000 adults, and the median age of diagnosis is 64 years.[5,6] The central pathogenesis is the fusion of the ABL1 gene on chromosome 9 with the BCR gene on chromosome 22, leading to the formation of the oncoprotein BCR-ABL1.[5] This oncoprotein is a constantly switched-on tyrosine kinase promoting cellular proliferation by several downstream signaling pathways including as RAS, MYC, and STAT ultimately leading to leukemogenesis.[5]
There are three stages of CML. The chronic phase (CML-CP) represents 90–95% of all patients, the symptoms of which are due to bone marrow/hematological abnormalities.[5] Therefore, the most common presenting symptoms include bleeding or thrombosis (due to platelet dysfunction or deficiency), gout (increased urate), priapism (form leukocytosis or thrombocytosis), retinal hemorrhages, and gastrointestinal perforation.[5] Splenomegaly is the most common sign in up to 40% of CML-CP patients.[9] In addition, symptoms such as dyspnea, confusion, and loss of coordination are termed “leukostatic symptoms” and occur from leukemia cells clogging the pulmonary or cerebral blood vessels.[5] However, leukostasis is much rarer in CML-CP compared to its rate in acute leukemia.[5,12,15] It has been reported that, overall, leukostasis occurs in 9.7% of all patients with CML.[8,9]
Patients with CML-CP may evolve to the accelerated phase (CML-AP) and eventually progress to blast crisis (CML-BC) which presents as acute leukemia and worsening of fundamental symptoms of bleeding, fever, and infections as the blasts cells predominate and crowd the bone marrow impairing normal hematopoiesis leading to pancytopenias.[5]
Solid brain tumors are commonly known to manifest as intracerebral hemorrhages (ICHs).[10] In hematological malignancies, ICH is more common in acute leukemia.[3] CML overall rarely presents with ICH, and in fact, approximately half of all CML patients are asymptomatic at diagnosis.[5] When symptoms do present, these are more typical, as discussed above. ICH has been reported as a presentation of and is more common in CML-BC likely due to thrombocytopenia and coagulopathy.[3,4,15] However, CML-CP presenting with ICH is an rare entity, and when it does occur, its pathogenesis is postulated to be from leukostasis.[4,8,12,15,16,20] There is only one case reported in the literature, where nausea and vomiting were the first presenting symptom of CML-CP due to a spontaneous ICH, and a total of eight cases of CML-CP, where patients are reported to have developed an ICH in addition to exhibiting prior constitutional symptoms of CML-CP.[2,7,8,11,13,17,19,20] Here, we report the second case of ICH as the first and only symptomatic presentation of CML-CP in a 22-year-old male. A literature review is also presented.
CASE PRESENTATION
A 22-year-old male presented to medical acute receiving on July 15, 2022, with a 2-week history of intermittent headaches and vomiting. In addition, there was a 1-week history of the left-sided weakness and a 3-day history of altered sensorium. His initial Glasgow coma score (GCS) was 14 (E4, V4, M6), and his pupils were bilaterally reactive and normal in size. Neurological examination revealed weakness with left-sided power of grade 2 in his arm and leg (MRC scale). Babinski was upgoing. Marked splenomegaly was present on palpation of the abdomen and ultrasound spleen. His initial blood count revealed leukocytosis, and his total leukocyte count was 447 × 10^9/L (reference range 4–11 × 10^9/L). This raised suspicion of hematological malignancy. A full blood count (FBC) with peripheral smear showed 38% myelocytes, 7% metamyelocytes, and 1% blast cells, making CML the main provisional diagnosis with an intracerebral complication.
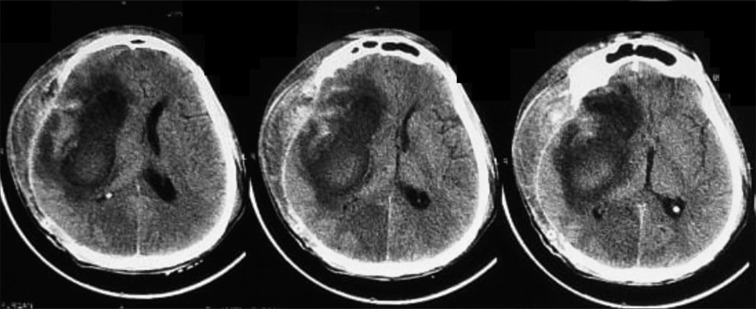
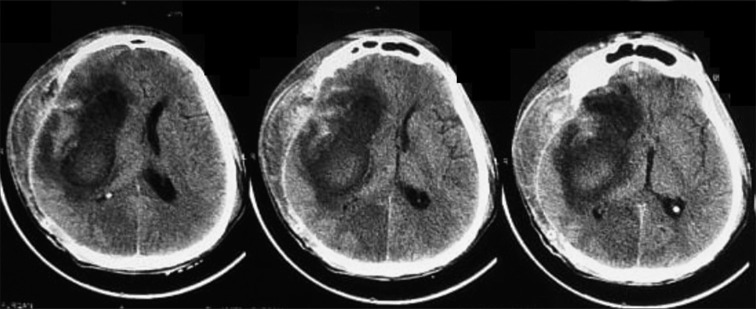
A CT scan and an urgent bone marrow biopsy were done the next day. During this time, the patient’s conscious level acutely deteriorated with a GCS of 11 (E3, V2, M6). He was administered mannitol 200 mL IV bolus and was referred to our neurosurgery department. The CT scan revealed a right frontal-temporal-parietal intracerebral hematoma with perifocal edema and a midline shift of 2.5 cm [Figure 1]. A right-sided frontal-temporal-parietal decompressive hemicraniectomy with expansion duraplasty was performed. Intraoperatively, the brain was tight and slightly pulsatile. The patient was shifted to neuro-ICU for mechanical ventilation and monitoring. Within 3 h, it was noted that his dressing was soaked, and his scalp wound was oozing blood. The scalp flap was swollen. The patient was immediately taken to the emergency operation theater, and a 60 mL extradural hematoma was evacuated. Hemostasis of bleeding scalp vessels was performed, and he was shifted back to the neuro-ICU. Postoperatively, he received sedation, paralysis, and mannitol. After 3 days, he was weaned from mechanical ventilation and shifted to the neurosurgical ward. A postoperative CT scan after 48 h revealed an improving midline shift (1.2 cm) with remaining perifocal edema [Figure 2]. After 1 week, the patient recovered without complication, and his GCS became 15/15 with persisting left-sided weakness (power 3/5).
Figure 1:
Preoperative CT scan.
Figure 2:
Postoperative CT scan (48 h).
His remaining investigations performed by the medical admissions team, as advised by hematology/oncology, before he was shifted to neurosurgery, revealed as follows. Platelet count was 202 × 10^9/L (reference range 150–300 × 10^9/L). A peripheral smear showing red blood cell morphology included anisocytosis with poikilocytosis and macrocytosis with a few teardrop cells. Differential leukocyte count confirmed that there were 50% neutrophils, 38% myelocyte, 7% metamyelocyte, 2% basophil, 1% lymphocyte, and 1% blast cells. Bone marrow aspirate taken from the posterior iliac crest showed hypercellular smears with reduced erythropoiesis and increased leucopoiesis with all stages of maturation seen. The myeloid-to-erythroid precursor ratio was 25:1. Megakaryocytes were present mainly hypolobulated, and blasts constituted 1% of nucleated marrow cells. CML in the CP was confirmed as blast cells in the bone marrow and peripheral blood were <10%.[1]
During his stay in the neurosurgical ward and transfer to our oncology colleagues, cytogenetics was performed, including fluorescence in situ hybridisation, and BCR-ABL t(9;22) (q34;q11.2). A BCR-ABL fusion confirmed the diagnosis of CML, as this translocation was detected in 82.5% of cells. The patient is now commenced on a tyrosine kinase inhibitor imatinib by our oncology colleagues with risk stratification based on the Sokal score.
DISCUSSION
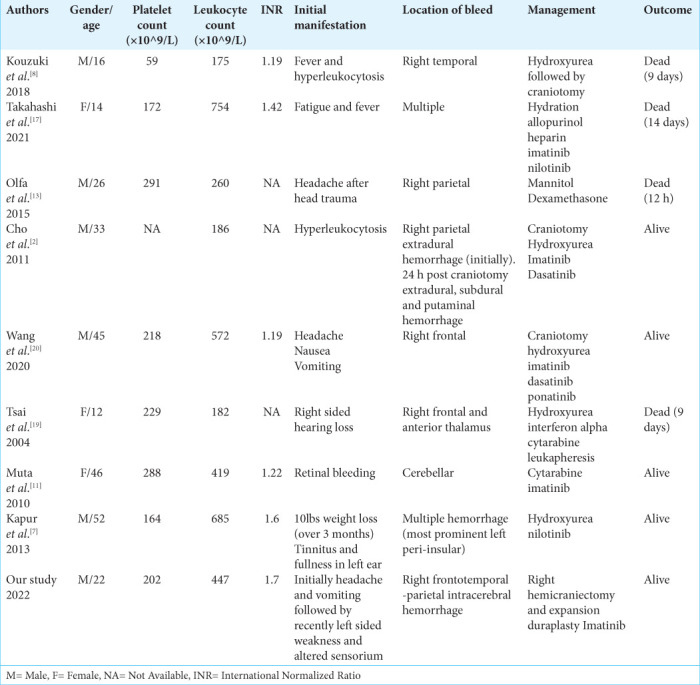
In our case, the patient did not have any history constitutional CML-CP symptoms, nor did they have any risk factors for ICH such as smoking, diabetes, hypertension, atrial fibrillation, and history of head trauma, and the patient did not drink alcohol. ICH is more prevalent in patients with AML and CML-BC than with CML-CP.[3,4,12,15,16] We found eight cases in the literature of CML-CP patients who developed ICH. Only one of these cases (Wang et al.[20]) had ICH as their first and only symptomatic presentation. This literature is summarized in Table 1. The World Health Organization stipulates that blast cells in the bone marrow or peripheral blood should exceed 20% to diagnose CML-BC, or there should be the presence of extramedullary blast proliferation, except in the spleen.[1]
Table 1:
Literature review summary of chronic myeloid leukemia (Chronic Phase) patients who developed an intracerebral hemorrhage.
The main cause of ICH in CML-BC is thrombocytopenia, but hyperleukocytosis is suggested as the main etiology of ICH in CML-CP.[4,8,12,15,16,20] The pathogenesis of ICH in such circumstances is not well understood. Still, authors have postulated that leukostasis is the pathogenesis of hyperleukocytosis and results from hypoxemia caused by vascular microthrombosis and occlusion in leukemic patients.[5,12,15,16,20] The risk of developing leukostasis is high in CML patients when their white blood cell count exceeds 100 × 10^9/L and a spleen size >10 cm.[5,9] Thus, it is evident that our patient was likely to develop leukostasis. Leukostasis is speculated when neurological or respiratory symptoms occur in patients with hyperleukocytosis,[12,15,16,20] and so our patient presenting with intermittent headaches and left-sided weakness supports the occurrence of leukostasis. It may be that the cerebral microvasculature was affected by leukostasis resulting in an ICH for this patient.
Based on the previous cases, in which craniotomies were performed, it was found that there is a high possibility of rebleeding in CML with ICH. However, some authors performed craniotomies for intracranial decompression to allow space for edema and to help confirm the diagnosis. Wang et al.[20] performed an emergent craniotomy due to the mass effect of the ICH. After decompressive craniectomy, to alleviate the still persistent swelling, 72 h postoperatively, they encountered a rebleed in the surgical area, which was initially managed conservatively, but after further deterioration in consciousness (GCS), a 2nd craniotomy was performed, and the patient improved. After surviving surgery, they were successfully treated using tyrosine kinase inhibitor (TKI’s). Wang et al.[20] biopsied the brain revealing myeloid cell hyperplasia with hemorrhage in tumor necrosis-like tissue that they excised in the second craniotomy, and immunohistochemical staining showed cells that were positive for myeloidperoxidase (MPO) with a Ki-67 of 30%. However, if the laboratory diagnosis of CML can be confirmed by blood work, we recommend the ICH may be left to resolve on its own or with decompressive craniectomy alone. In our case, we did evacuate the hematoma and still encountered a rebleed therefore the chances of rebleed may be more significant and consequential thus hematoma evacuation as a policy may not be recommended unless it pouts out of the cortical surface and lends itself to a very easy evacuation.
Similarly, Cho et al.[2] encountered an extradural hematoma and performed an emergent craniotomy to evacuate. Twenty-four hours postoperatively, the patient developed left-sided weakness and right pupil dilation, which prompted a CT scan that revealed a rebleed with new right parietal extradural hematoma and subdural and putaminal hemorrhages. Due to rebleeds, a second craniotomy was performed to remove hematomas. Hydroxyurea was administered initially, and then, the patient was commenced on Imatinib, leading to hematological and molecular remission. Like Wang et al.,[20] Cho et al.[2] biopsied the extradural hematoma excised and found focally increased blast-like cells on microscopic examination and immunohistochemistry positive for MPO and lysozyme staining.
Cases where patients were not or could not be operated on include the following. Olfa et al.[13] encountered a 26-year-old male with a right parietal ICH managed with mannitol and corticosteroid therapy. However, the patient died the same day from circulatory arrest, and further, intervention could not have been attempted. Interestingly, Tsai et al.[19] encountered a young patient with the right-sided hearing loss due to their CML-CP. This case supports that leukostasis can lead to sensorineural hearing loss. The patient was administered hydration therapy, allopurinol, hydroxyurea, and interferon alpha. However, the patient deteriorated by developing left-sided hearing loss and left eye blindness. Leukapheresis was performed, and low dose cytarabine was added to the regimen, but the patient died on the 9th postoperative day despite these efforts. The authors attempted auditory evoked potentials (which the patient did not cooperate to perform) and performed an MRI brain that revealed bleeds in the right lower frontal area and the anterior thalamus. Similarly, Takahashi et al.[17] diagnosed a CML-CP patient from blood work who presented with fever and fatigue. The patient received hydration therapy, allopurinol, and low molecular weight heparin after her admission, while imatinib was commenced when the diagnosis was confirmed. Similarly , the patient developed sensorineural hearing loss, which the authors considered to be from leukostasis, and hydroxyurea was administer which failed to reduced platelet and leukocyte count. The patient lost consciousness subsequent to developing a respiratory arrest. A CT scan brain was performed which revealed brain herniation and multiple ICHs and while the patient was supported in intensive care, she was declared brain dead by electroencephalography on the 14th admission day. Therefore, we recommend a high clinical suspicion of intracranial hemorrhage of CML patients and an emergent CT brain should be performed in patients with CML if neurological symptoms are experienced.
Following surgeries, patients have been treated with tyrosine kinase inhibitors which have revolutionized the treatment of CML and significantly improved overall survival by even decades.[14] Therefore, a good outcome was observed in cases who survived the ICH. The oncological management of our patient has only started. The treatment and monitoring response criterion is risk stratification according to the Sokal score and BCR-ABL mutation analysis, which guides which TKI is initiated.[18] Oncological drugs for CML-CP include imatinib, dasatinib, and ponatinib. Once commenced, patients are to be regularly checked with FBC and BCR-ABL levels at regular intervals using real-time polymerase chain reaction. Hydroxyurea can be used as cytoreductive therapy and helps reduce the risk of a rebleed.[17,20] Most cases of ICH in CML-CP have reported using hydroxyurea, allopurinol, and hydration with TKIs for definitive management.
Wang et al.[20] have the first case who reported ICH as the first presentation of CML-CP without any other prior symptoms similar to ours. These authors recommend chemotherapy and third-generation TKIs if the CP progress to CML-BC and the BCR-ABL level does not go down. They provided a relatively long follow-up and showed that once first-generation TKI (Imatinib) developed resistance, a second-generation TKI (Dasatinib) led to hematological remission. BCR-ABL levels were monitored, and the third-generation TKI ponatinib was commenced when dasatinib resistance developed. Similarly, Cho et al.[2] case had maintained a good response with imatinib for 2 years, and when BCR-ABL levels increased was placed on dasatinib. Close monitoring of BCR-ABL levels is crucial.
CONCLUSION
We report a rare presentation of CML-CP with an ICH causing the first symptomatic presentation. Intracranial involvement and ICH may be contributed to by leukostasis from hyperleukocytosis. When CML patients present with neurological symptoms, an urgent CT brain should be obtained. Rebleeding in CML patients is common, and they should be conservatively managed unless there is a need to alleviate intracranial pressure, in which case a craniotomy should be utilized. Patients should be monitored closely in neurosurgical high dependence and promptly be commenced oncological treatment with an appropriate TKI.
Footnotes
How to cite this article: Ashraf M, Naseeruddin G, Zahra SG, Sultan KA, Kamboh UA, Manzoor M, et al. Intracerebral hemorrhage as the first symptomatic manifestation of chronic myeloid leukemia (chronic phase): A case report and literature review. Surg Neurol Int 2023;14:5.
Contributor Information
Mohammad Ashraf, Email: mohammad_5676@hotmail.com.
Ghulam Naseeruddin, Email: rainaseerns@gmail.com.
Shah Gul Zahra, Email: shahgulzahra4@gmail.com.
Kashif Ali Sultan, Email: sultankashif11@gmail.com.
Usman Ahmad Kamboh, Email: usmanschemer644@hotmail.com.
Mehwish Manzoor, Email: mahwishmanzoor20@gmail.com.
Minaam Farooq, Email: minaamkemu2018@gmail.com.
Manzoor Ahmad, Email: manzoor63@gmail.com.
Naveed Ashraf, Email: drnashraf@yahoo.com.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Bonifacio M, Stagno F, Scaffidi L, Krampera M, Di Raimondo F. Management of chronic myeloid leukemia in advanced phase. Front Oncol. 2019;9:1132. doi: 10.3389/fonc.2019.01132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cho SF, Liu TC, Lu CY, Chang CS. Epidural leukemic involvement and intracranial hemorrhage as initial manifestations in a newly diagnosed chronic myeloid leukemia patient. Ann Hematol. 2011;90:607–9. doi: 10.1007/s00277-010-1061-7. [DOI] [PubMed] [Google Scholar]
- 3.Dayyani F, Mougalian SS, Naqvi K, Shan J, Ravandi F, Cortes J, et al. Prediction model for mortality after intracranial hemorrhage in patients with leukemia. Am J Hematol. 2011;86:546–9. doi: 10.1002/ajh.22031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gokce M, Unal S, Bayrakçı B, Tuncer M. Chronic myeloid leukemia presenting with visual and auditory impairment in an adolescent: An insight to management strategies. Indian J Hematol Blood Transfus. 2010;26:96–8. doi: 10.1007/s12288-010-0026-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jabbour E, Kantarjian H. Chronic myeloid leukemia: 2020 update on diagnosis, therapy and monitoring. Am J Hematol. 2020;95:691–709. doi: 10.1002/ajh.25792. [DOI] [PubMed] [Google Scholar]
- 6.Kalmanti L, Saussele S, Lauseker M, Proetel U, Müller MC, Hanfstein B, et al. Younger patients with chronic myeloid leukemia do well in spite of poor prognostic indicators: Results from the randomized CML study IV. Ann Hematol. 2014;93:71–80. doi: 10.1007/s00277-013-1937-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kapur S, Wax M, Miles L, Hussain A. Permanent sensorineural deafness in a patient with chronic myelogenous leukemia secondary to intracranial hemorrhage. Case Rep Hematol. 2013;2013:894141. doi: 10.1155/2013/894141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kouzuki K, Umeda K, Saida S, Kato I, Hiramatsu H, Funaki T, et al. Sudden intracranial hemorrhage in a patient with atypical chronic myeloid leukemia in chronic phase. J Pediatr Hematol Oncol. 2018;40:e553–6. doi: 10.1097/MPH.0000000000001061. [DOI] [PubMed] [Google Scholar]
- 9.Kurosawa H, Tanizawa A, Tono C, Watanabe A, Shima H, Ito M, et al. Leukostasis in children and adolescents with chronic myeloid leukemia: Japanese pediatric leukemia/ lymphoma study group. Pediatr Blood Cancer. 2016;63:406–11. doi: 10.1002/pbc.25803. [DOI] [PubMed] [Google Scholar]
- 10.Lieu AS, Hwang SL, Howng SL, Chai CY. Brain tumors with hemorrhage. J Formos Med Assoc. 1999;98:365–7. [PubMed] [Google Scholar]
- 11.Muta T, Sawada Y, Moriyama Y, Seike Y, Tokuyama T, Ueda Y, et al. Chronic myeloid leukemia complicated with cerebellar hemorrhage and acute hydrocephalus successfully treated with imatinib and intensive supportive care. Rinsho Ketsueki. 2010;51:1769–74. [PubMed] [Google Scholar]
- 12.Naunheim MR, Nahed BV, Walcott BP, Kahle KT, Soupir CP, Cahill DP, et al. Diagnosis of acute lymphoblastic leukemia from intracerebral hemorrhage and blast crisis. A case report and review of the literature. Clin Neurol Neurosurg. 2010;112:575–7. doi: 10.1016/j.clineuro.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 13.Olfa CW, Imen R, Leila K, Hichem K, Adnane A, Mourad C, et al. Diagnosis of chronic myeloid leukemia from acute intracerebral hemorrhage: A case report. J Acute Dis. 2015;4:252–4. [Google Scholar]
- 14.Seiter K. Update of recent studies in chronic myeloid leukemia. J Hematol Oncol. 2009;2:A2. [Google Scholar]
- 15.Sharma SR, Dey B. Blast crisis of chronic myeloid leukemia initially presenting as severe acute intracerebral hemorrhage. J Family Med Prim Care. 2020;9:1266–9. doi: 10.4103/jfmpc.jfmpc_940_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shiber JR, Fines RE. Cerebral hemorrhage due to hyperleukocytosis. J Emerg Med. 2011;40:674–77. doi: 10.1016/j.jemermed.2008.11.018. [DOI] [PubMed] [Google Scholar]
- 17.Takahashi N, Sano H, Mochizuki K, Kobayashi S, Ohara Y, Kikuta A. Intracranial hemorrhage in a pediatric patient with chronic myeloid leukemia in chronic phase: A case report. Case Rep Oncol. 2021;14:525–30. doi: 10.1159/000515011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Terasawa T, Dahabreh I, Trikalinos TA. BCR-ABL mutation testing to predict response to tyrosine kinase inhibitors in patients with chronic myeloid leukemia. PLoS Curr. 2010;2:RRN1204. doi: 10.1371/currents.RRN1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tsai CC, Huang CB, Sheen JM, Wei HH, Hsiao CC. Sudden hearing loss as the initial manifestation of chronic myeloid leukemia in a child. Chang Gung Med J. 2004;27:629–33. [PubMed] [Google Scholar]
- 20.Wang H, Cao F, Li J, Sun K, Jin J, Wang M. Intracerebral hemorrhage as the initial presentation of chronic myeloid leukemia: A case report and review of the literature. Front Neurol. 2020;11:571576. doi: 10.3389/fneur.2020.571576. [DOI] [PMC free article] [PubMed] [Google Scholar]