Abstract
Background
First-generation migrants from South Asia account for a considerable proportion of the immigrant populations in high-income, western countries and are at a high risk of developing complex, chronic diseases such as cardiovascular disease and diabetes. Yet, previous systematic reviews have not synthesized information about the healthcare needs and preferences of such migrants and the best ways for health services to provide them with appropriate, culturally sensitive, patient-centered care. The aim of this study is to systematically review the international evidence about first-generation, South Asian migrants’ healthcare experiences from the patients’ perspectives.
Methods
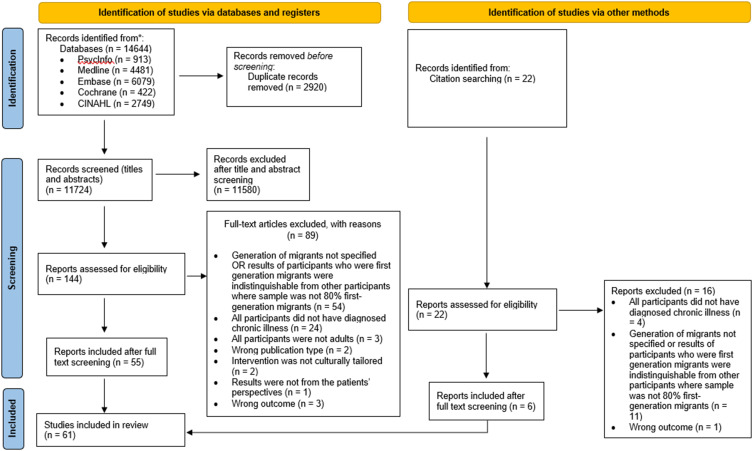
Five databases were searched for qualitative, quantitative, and mixed methods studies published between January 1990 and April 2020. Fourteen thousand, six hundred and forty-four papers were retrieved and screened using pre-determined eligibility criteria. Sixty-one papers were included in this narrative synthesis. Relevant qualitative findings from the included papers were thematically analyzed, and quantitative findings were summarized.
Results
Five themes emerged from findings: 1) Healthcare services engaged; 2) the language barrier; 3) experiences and perceptions of healthcare advice; 4) the doctor–patient relationship; and 5) the role of patients’ families in supporting access and delivery of healthcare.
Conclusion
The findings indicate that communication barriers reduce the cultural and linguistic appropriateness of healthcare. Potential solutions include employing healthcare staff from the same cultural background, training healthcare professionals in cultural competence, and proactively including first-generation, South Asian migrants in decision-making about their healthcare. Future research should explore South Asian migrants’ experiences of multimorbidity management, continuity of care, interdisciplinary collaboration, the formation of treatment plans and goals as little to no data were available about these issues.
Keywords: patient-centered care, patient participation, migrant, chronic disease, health services, sociological factors, systematic review
Plain Language Summary
Increasing numbers of South Asian migrants are settling in high-income, western countries. As South Asian migrant populations in high-income, western countries are at an elevated risk of developing long-term medical conditions such as type 2 diabetes, it is important that the healthcare experiences of South Asian migrants with long-term medical conditions are understood and addressed. Consequently, the authors undertook an international systematic review exploring the healthcare perspectives of first-generation, South Asian migrants who have long-term medical conditions and live in high-income, western countries. Conducting this review involved searching five major databases of scientific journal articles for relevant papers, extracting pertinent information from these papers, and analyzing the obtained data. This review identified various cultural barriers South Asian migrants experienced when accessing healthcare in high-income, western countries as well as their preferences and beliefs regarding healthcare for managing their long-term medical conditions. The lessons learned from this review suggest that efforts must be made by healthcare services to meet the needs of South Asian migrants with long-term medical conditions, thereby improving their experiences of care and ability to manage their own health.
Introduction
High-income, western societies are increasingly multicultural and are home to substantial numbers of South Asian migrants,1–4 that is, those originating from Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan or Sri Lanka.5 The World Migration Report conveyed that, in 2020, the largest international migrant population originated from India.6 The migrant corridor between the United States and India was one of the largest corridors, globally, with over two million migrants from India residing in the United States. India and Pakistan were among the top three countries of origin for migrants settling in the United Kingdom.6
Compared with people of other ethnicities, South Asian individuals are at a higher risk of developing type 2 diabetes and cardiovascular disease.9–12 Diabetes, cardiovascular disease and related mortality may manifest at a younger age for South Asian migrants than for other ethnic groups.9,11 Living with and managing chronic diseases is challenging,13 however, migration may pose additional barriers. Like other migrant groups, South Asian migrants may experience inequalities of access to healthcare following migration due to language barriers, low health literacy levels, an unfamiliar healthcare system, low socio-economic status, and incidents of discrimination.7 Low socio-economic status following migration and, consequently, residence in underprivileged areas can further exacerbate an increased incidence of chronic disease and poor access to healthcare services.7,8
Previous literature suggests that the provision of patient-centered care (healthcare that is appropriate, emotionally and physically supportive, readily accessible in a timely manner and delivered with respect for patients’ needs, beliefs and preferences) may improve patients’ satisfaction with clinical care, rapport with healthcare professionals, and self-management of chronic diseases.14–18 Inadequate understanding and consideration of patients’ cultures by healthcare professionals can lead to stereotyping and alienation of minorities, misunderstanding of patient barriers for engaging with healthcare services, poor communication between patients and healthcare professionals, and a lack of adherence by the patient to treatment, indicating the need for culturally tailored healthcare provision.17,19 However, systematic reviews exploring the effectiveness of culturally tailored, patient-centered care interventions have not consistently demonstrated or assessed improvements in patient health outcomes, and, at times, the included studies lacked rigour.20–23 Further consideration of migrants’ healthcare needs, such as the preferred duration and methods of culturally tailored healthcare interventions, the quality of communication between healthcare professionals and patients during these interventions, and cultural competency training for healthcare professionals, may be required when developing culturally appropriate, patient-centered care interventions for diverse populations.20–23
This systematic review aims to explore the patient-centered care experiences of first-generation South Asian migrants living with chronic diseases in high-income, western countries from the patients’ perspectives. The findings will assist in further understanding South Asian migrants’ healthcare experiences and support the development of a culturally and linguistically appropriate, patient-centered healthcare delivery approach for these populations.
Methods
Protocol and Registration
The systematic review protocol was informed by the Economic and Social Research Council guidelines for narrative syntheses24 and reporting was informed by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines.25 The protocol is registered on PROSPERO (PROSPERO registration number: CRD42020131096).
Literature Search and Screening
A comprehensive search strategy was developed with the assistance of a research librarian. Free text terms and relevant controlled vocabulary relating to healthcare, South Asian migrants, high-income, western countries, and chronic diseases were compiled. Boolean and proximity operators were used to refine the search strategy (see Supplementary Material 1 Medline search strategy).
The literature search was performed in April 2020 using the Cochrane, Embase, Medline, CINAHL, and PsycInfo databases, seeking papers published from January 1st, 1990, to April 27th, 2020, inclusive. The authors chose 1990 as a limiter because a considerable number of individuals migrated from South Asian countries to western countries between 1990 and 2020.2,26–29 Studies yielded from the literature search were exported to EndNote and duplicates were removed. The studies were uploaded to Rayyan QCRI for screening. Three authors independently screened titles, abstracts, and full texts of the retrieved articles (two authors per article). Additional articles were gathered using snowballing, whereby reference lists of systematic reviews and eligible articles were examined for further relevant papers. Titles, abstracts and full texts of these papers were also screened against the eligibility criteria.30 Conflicting assessments were resolved through discussion between the authors of this review.
Eligibility Criteria
A diverse range of study designs from any setting were eligible for inclusion. To be included in the review, the study sample needed to comprise of first-generation, South Asian migrants, aged 18 years or older, with at least one diagnosed chronic disease, living in high-income, western countries. South Asian migrants were those who originated from Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan or Sri Lanka.5 For studies involving migrants from multiple generations or ethnic groups, only results which clearly related to first-generation, South Asian participants were included. Findings were considered to represent first-generation South Asian migrant data, unless otherwise indicated, if at least 80% of South Asian participants were identified as first-generation. Chronic diseases were defined as illnesses that could last in the body for at least 6 months, which may require ongoing healthcare.31,32 Chronic diseases included, but were not limited to, conditions such as arthritis, asthma, chronic back pain, cancer, cardiovascular disease, chronic obstructive pulmonary disease (COPD), diabetes, kidney disease, mental health conditions, and osteoporosis.33 High-income, western countries were identified as high-income countries of Europe, high-income Asia and Pacific (ie Australia and New Zealand) and Northern America, where the majority of the population is of European origin.34 For the purpose of this review, patient experiences included beliefs, needs, preferences, attitudes, and expectations along with experiences of events regarding their healthcare.
For inclusion, studies needed to discuss at least one of the following outcomes:
Experiences, beliefs, needs, preferences, attitudes, and/or expectations relating to the patient-centeredness of healthcare18 delivered by healthcare services, healthcare professionals or informal healthcare providers to patients from the patients’ perspectives
Results of culturally tailored interventions for South Asian migrants, which explored the patient-centeredness or quality of care, changes in patients’ health behaviors or self-efficacy, health outcomes or satisfaction with decisions regarding their treatment plans
Single-case studies and studies which focused on participants that had departed their countries of origin less than a year ago or were on a student visa were excluded. Where study participants were not adequately defined for eligibility purposes, but eligibility was a possibility, corresponding authors were emailed for clarification and references were included if eligibility was confirmed.
Data Extraction and Appraisal
Data extracted from studies included participant demographics, methodological information for the study and results pertaining the outcomes listed above. Extracted information was entered into a data collection spreadsheet created by the authors using Microsoft Excel. The quality of included articles was evaluated using tools appropriate to the study design to ensure that the studies were methodologically sound (see Supplementary Material 3 for quality appraisal tables). Qualitative studies were appraised using COREQ,35 randomized control trials were appraised using CONSORT36 and other observational study designs such as surveys were appraised using STROBE.37 Where studies were of mixed methods, only the parts of the study which presented relevant results were appraised using one or more of the three aforementioned checklists. Checklist criteria were marked with either “yes”, “no” or “partially” depending on the extent to which the studies met the criteria. Scores were assigned for each criterion that was met (yes = 2, partially = 1, no = 0) and total scores were converted to percentages, with the maximum possible score as the denominator. Studies presenting quantitative results underwent a risk of bias assessment using tools relevant to their study design.38 Randomized controlled trials were assessed using ROB-2 for the effect of assignment to intervention.39 Non-randomized studies such as cross-sectional papers were assessed using the Risk of Bias Assessment tool for Non-randomized Studies (RoBANS).40 Criteria deemed as inapplicable to the study were excluded from the quality appraisal.
Data Analysis
Due to the broad scope of the review, diverse range of study designs and objectives, and the predominantly qualitative nature of included papers, a narrative synthesis approach was utilized to analyze the data.24 Qualitative data were analyzed inductively using the Braun & Clarke (2006) method of thematic analysis, while quantitative data was summarised.24,41 Extracted information from included studies was read in depth and coded line by line.41 A key word or code was assigned to each data segment leading to the development and continual evolution of a coding guide.41 The first four eligible papers were coded independently by two authors, following which the coding was discussed to address discrepancies. Thereafter, all coding was completed by one author. Themes were identified by grouping similar codes and were reviewed and refined through discussions with all authors to ensure consistency.41 Quantitative data were summarized using the data extraction spreadsheet. Quantitative data relating to outcomes of culturally tailored interventions were compared with each other. Quantitative results from cross-sectional studies and interventions were also compared with qualitative results. Summaries and outcomes of the quantitative results were described narratively. Trends were identified between the results of studies by examining factors such as participants’ demographics. Outlying results were also explored. The studies in this review were not sufficiently homogenous in their aims and methods to conduct a meta-analysis.
Results
Overview
The database search yielded 14,644 studies. Following full-text screening, 61 studies were included in this narrative synthesis, of which 6 studies were identified through the snowballing process (see Figure 1 for PRISMA flowchart). Forty-nine papers were qualitative studies, 4 were mixed methods studies, and 8 were quantitative studies (see Supplementary Material 2 for table of included studies). Studies were conducted in Australia (n = 3), Canada (n = 19), Denmark (n = 1), Norway (n = 4), UK (n = 30) and US (n = 4). Most studies explored the management of diabetes mellitus (n = 31), cardiovascular disease (n = 16) or cancer (n = 10). Fifty-five papers reported patient-centered care-related outcomes, and 6 papers evaluated culturally tailored interventions. Most participants in the included studies were born in Bangladesh, Pakistan, or India. See Tables 1 and 2 for a summary of the included studies.
Figure 1.
PRISMA flow diagram.
Notes: PRISMA figure adapted from Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. Creative Commons.25
Table 1.
Summary of Included Studies (See Supplementary Material 2 for Full Table of Included Studies)
| Study type (n=number of studies) | Qualitative (n=49) Quantitative: (n=8) Mixed Methods: (n=4) |
| Data collection method (n=number of studies utilizing the collection method) | Qualitative interviews (n=49) Focus groups (n=5) Surveys (n=9) Participant observation (n=3) Physical assessments (n=4) |
| Data analysis methods (n=number of studies utilizing the analysis method) | Thematic analysis (n=13) Content analysis (n=8) Constant comparison (n=14) Framework analysis (n=2) Other or un-named qualitative methods: (n=21) Descriptive statistics (n=12) Inferential statistics (n=10) |
| Outcomes investigated (n=number of studies) | Patient-centered care experiences (n=55) Culturally tailored intervention (n=6) |
Table 2.
Summary of Participants of Included Studies
| Number of Participants | Range: 4–268 |
| Mean: 39 | |
| Chronic disease(s) investigated (n=number of studies) | Diabetes mellitus (n=31) Cardiovascular disease (n=16) Cancer (n=10) Hypertension (n=2) Postnatal depression (n=1) Osteoporosis (n=1) Chronic kidney disease (n=1) Asthma (n=1) Leg and foot ulcers (n=1) Dementia (n=1) Heart failure (n=1) Atherosclerosis (n=1) |
| Participant gender (n=mean number of participants) Note: One paper was excluded from this section as no information was provided about gender. | Men (n=17) Women (n=23) |
| Participant age | Range: 21–87 years |
| South Asian country of origin (n=number of studies) | India (n=39) Pakistan: (n=26) Bangladesh (n=14) Sri Lanka (n=7) Nepal (n=1) Country unspecified but region broadly classed as South Asia (n=8) |
| Western country study was set in (n=number of studies) | Australia (n=3) Canada (n=19) Denmark (n=1) Norway (n=4) UK (n=30) US (n=4) |
The studies included in this review met 21% to 70% of the relevant reporting criteria outlined in the quality of reporting appraisal tools (see Supplementary Material 3). Risk of bias assessment showed that papers presenting quantitative data had a moderate to high risk of bias (see Supplementary Material 3). Quantitative papers did not identify the presence of confounding variables or perform sensitivity analyses, therefore presented results may contain unaddressed biases. Of the quantitative studies, only randomized controlled trials stated how the sample size was determined. Two papers reporting the same randomized controlled trial did not define the control group care processes.42,43 For nine papers presenting quantitative results, it was not clear whether the sample size was sufficient to obtain valid results. Most qualitative studies (n = 48) presented quotes to substantiate findings. Quotes presented by 47 of these studies were consistent with the conclusions made.
Five themes were identified (see Table 3).
Table 3.
Table of Themes
| Theme | Subthemes: |
|---|---|
| Theme 1: Healthcare services engaged |
|
| Theme 2: The language barrier |
|
| Theme 3: Experiences and perceptions of healthcare advice |
|
| Theme 4: The doctor-patient relationship |
|
| Theme 5: The role of patients’ families in supporting access and delivery of healthcare |
|
Theme 1: Healthcare Services Engaged
All included studies reported that South Asian participants accessed at least one healthcare service to manage their chronic diseases within community or hospital settings. Participants generally asserted that the healthcare services they received in the western countries they resided in had more accessible facilities,44 and were more beneficent,45–48 informative49 and affordable44,46 than those in South Asian countries.44–49 Some South Asian participants in the United Kingdom (UK) believed that healthcare received in hospitals was more thorough than general practitioner (GP) care as multiple services were provided during hospital appointments.46,50,51 Healthcare professionals most often consulted included doctors,42–102 nurses43,46,50,51,62,65,66,68,69,72–74,76,80–82,84,85,87,92,96,97 and dieticians.45,50,51,59,60,62,65–67,70,73,82,85,99,100 Cardiac rehabilitation and diabetes education classes had been attended by participants with cardiovascular disease49,61,65–67,69,76,79 and diabetes49,58,62,100,101 respectively. Participants valued the opportunities these services presented for supervised care by a multidisciplinary team,55,65–67 non-judgmental, in-depth discussions with healthcare professionals,49,65,66,87 and individualized, culturally appropriate advice.49,55,62,65,77 Group settings fostered a friendly environment.55,65,77 Participants appreciated sharing experiences with other patients.49,65,77,87 Few participants reported engaging with chronic disease organisations.45,49,63,84,86
Some participants reported accessing complementary or alternative South Asian therapies such as Ayurveda,63,84 therapeutic foods53,63,84,86 and treatments from Hakims or Fakirs51,63 as an adjunct or, in rare cases, as an alternative to their prescribed treatments for managing their chronic diseases.53,61,63,84,86,95 Negative views towards or failure of medical treatment prescribed by their treating doctors in their western countries of residence,84,86 encouragement from social circles,53,61,63,84,86 and familiarity with natural treatments53,63,86,95 encouraged participants to seek traditional treatments.53,63,84,86,95 The relegation of health outcomes to fate led some to reject medical intervention by doctors.65,67,71
The Role of the Healthcare Professional
Twenty-two studies indicated that South Asian participants expected and preferred doctors, rather than other health professionals, to provide consultations about healthcare.45–47,49,52,53,55,58,67,69,72,74,77,81,87,91,92,95,98–101 Participants held few expectations of healthcare professionals who were not doctors (eg, nurses and dieticians) despite appreciating their accessibility and advice provision as they were focused predominantly on the doctor’s care.50,51,68,81,92,97,101 Seven studies reported that when participants were dissatisfied with their experiences of communicating with their healthcare professionals including doctors, participants perceived that the healthcare professional’s role was limited to practical service provision such as prescribing or dispensing medication.45–47,49,51,53,92 Participants who were dissatisfied with their interactions with healthcare professionals often displayed a preference for obtaining information from alternate sources including doctors in their countries of origin, or from friends and family.45,46,49,51,69,92
Attendance at Appointments
A preference for frequent and regular appointments with GPs, for some, at least every 1–2 months,73 was commonly identified.43,47,51,61,72,73 Håkonsen et al47 reported that women attended appointments more regularly than men.47 Frequent appointments were perceived to increase familiarity between the GP and patient, thus enhancing the appropriateness of prescribed treatment and advice.61 Conversely, some participants did not feel compelled to attend appointments, seek healthcare services to monitor their chronic disease68 or action referrals.58,68,69,90,91,101 Many of these participants also believed healthcare services were unnecessary or unhelpful in managing their chronic diseases,58,67,69,101 particularly, when symptoms were absent,68 participants perceived their health outcomes could only be managed through religious faith,67 or adequate control of their chronic disease was achieved through self-management.67,101 Written referrals accompanied by discussions with a doctor and follow-up consultations with the doctor on an ongoing basis about participants’ health improved the likelihood of attending and adhering to referred healthcare services, however, such discussions were infrequently initiated by the doctor during appointments.55,69 Encouragement from participants’ social peers and other hospital patients also improved attendance.69
Logistical and Societal Barriers to Accessing Healthcare
For some participants, the expense of attending appointments reduced the accessibility of healthcare services.51,57,94 Long distances to medical clinics from participants’ homes inhibited consultation attendance for those of low socio-economic status and those without access to transport, delaying access to required care.51,65,69,75,79,87 Employment,51,55,75,79 family and childcare duties51,75,79,87 and housework obligations75,87 presented barriers to attending appointments or accessing healthcare altogether.51,55,75,79,87 Women’s attendance at healthcare services was also restricted by a fear of racial abuse while travelling to appointments, lack of family support, and the family’s concerns (and sometimes participant concerns) about the safety and cultural appropriateness of women travelling alone.51,60,79,83,87,94 Ens et al61 found that close proximity of clinics to migrants’ homes enabled frequent medical appointments and improved the doctor–patient relationship and efficiency of obtaining prescriptions.61 Some participants took lengthy vacations to their countries of origin to visit relatives during which they ceased adhering to their treatment plans and consulting their usual doctors in their western countries of residence.51,53,92 Clerical errors by clinic staff,51 unavailability of preferred doctors51,61 and long waiting times for appointments45,51,69 reduced satisfaction and motivation to attend healthcare services.45,51,61,69 Delays in referral provision for investigations by doctors hindered confirmation of diagnoses.51,56
Consulting Doctors of the Same Gender and Ethnic Background
First-generation, South Asian migrants mostly preferred to consult healthcare professionals with whom they shared an ethnic background and spoken language.46,47,50,51,58,60,61,65,71,80,87,95,96,101,102 Participants believed that a common ethnicity and language allowed healthcare professionals to better understand the participants’ needs and preferences,46,47,50,58,60,61,65,71,80,87,95,102 enabled the provision of culturally sensitive care and detailed advice,46,58,60,61,65,95,101,102 and improved healthcare service attendance.87
Most men and women preferred to consult healthcare workers of their own gender, particularly for sensitive illnesses such as those relating to the reproductive system.46,53,77,96,102 Physical assessments by healthcare professionals of the opposite gender caused feelings of shame.53,77,96,102 Karbani et al77 found that, due to such shame, some women used euphemisms and gestures to communicate information about their breast cancers to male healthcare professionals.77 Some participants were at ease and less inhibited when consulting with non-South Asian healthcare professionals of the opposite gender,46 or, for some women, when communicating with male healthcare professionals through female interpreters.47,96 Although, participants valued a shared culture and ethnicity with healthcare professionals, additional appreciation was expressed towards displays of approachability and kindness.51,79,80
Theme 2: The Language Barrier
Language barriers inhibited access to healthcare services, communication with healthcare professionals and comprehension of healthcare information,45,46,51,52,57–59,65,68,73,74,79,87,89,93,94,96,102 leaving participants affected by language barriers feeling isolated and helpless.45,57,79,94 Those who could not speak the official language in their western country of residence appeared to have less awareness of and access to available services and entitlements.57,68,72,94,102 For some women with breast cancer living in Canada, selecting the correct English words to communicate with healthcare professionals, while also coping with treatment side effects, was taxing,96 and frustrating.96 Rhodes et al51 found that non-English-speaking Bangladeshi participants living in the UK felt compelled to accept low quality advice from their Sylheti-speaking GPs because their choice of doctors was limited by their difficulties speaking the language of their western country of residence.51
Many participants preferred and needed written correspondence in their own language(s),57,62,71,73,81,87 but healthcare services often only distributed printed materials in the language of participants’ western countries of residence.52,57,59,73 Printed materials in South Asian languages were not always useful because the concepts described in the formal written language form were unsuitable for laypersons68 and those who were not literate or insufficiently literate in their own language.51,57,61,68,79 Many participants required assistance to read written information, even when presented in their preferred South Asian languages.52,61,68,87 Gupta et al49 and Rhodes et al51 found that informational cassettes and leaflets were given to participants without sufficient verbal instruction from a healthcare professional.49,51 King et al79 reported that older individuals with low education levels relied more on spoken information than written sources.79 Participants displayed trepidation towards consulting healthcare services where linguistically and culturally sensitive care was thought to be unavailable.45,49,87,89
The Use of Interpreter Services
Language barriers between South Asian migrants and healthcare professionals often indicated a need for interpreter services during consultations.45,46,51,52,57,61,68,74,79,96 Rhodes et al51 found that participants valued the provision of translation by bilingual reception staff due to a shared rapport between the participants and receptionists.51 Simply relying on South Asian healthcare staff to effectively communicate healthcare information and advice was not always appropriate. An example of this reliance was identified by Ens et al,61 where Punjabi-speaking participants attending a pharmacy with bilingual employees were unable to communicate effectively as the staff spoke Gujarati, a different language altogether.61 Translation services were infrequently provided by healthcare services due to an insufficient interpreter workforce,51 expense to the clinic45 and healthcare professionals defaulting to accompanying family for translation.45,46,51,58,74,79,96 Moreover, some participants reported that healthcare professionals made assumptions about the languages spoken by the participants resulting in linguistically inappropriate interpreters being provided.51,96 Lawton et al46 stated that some participants felt compelled to minimize their questions to avoid wasting the interpreters’ time.46 Despite these challenges, Singh-Carlson et al96 and Rhodes et al51 reported that participants appreciated having access to interpreters providing information regarding their illness and its treatment in their native languages.51,96
Theme 3: Experiences and Perceptions of Healthcare Advice
Many studies reported dissatisfaction amongst their participants with the quality of healthcare advice, with some participants asserting that no advice was provided about their chronic disease.45,49,50,52,59,65,70,71,73,78,79,82,85,92,98–101 Limited time available for consultations often reduced doctors’ ability to provide adequate self-management advice.45,47,50,92,101 Participants commonly only received information about their chronic diseases at the point of diagnosis,49,51,82 however reinforcement of medical advice and validation of self-management practices at subsequent consultations was desired.49,55,59,65,70,72,87,99 The need for reiteration of advice was evident in participants’ inconsistent recollection and comprehension of information.45,52,62,70,78,82,97–100
Depth and Applicability of Advice
Participants expressed a need for detailed advice about their illness,58,81,101 management of the physical and psychological impact of their diagnosis,71,97 treatment options,52,58,71,74,81 medications,52,81 lifestyle modifications45,58,62,65,70,99 and access to other information sources.101 Advice provided by healthcare professionals was often perceived as superficial and generic,49,52,56,62,70,73,78,82,92,99,100 resulting in poor self-efficacy and reduced self-management of their chronic diseases.49,52,56,58,59,62,70,73,77–79,82,92,99 The use of complex or vague terms by healthcare professionals reduced participants’ comprehension of their advice.62,82,96,98 Practical feedback from healthcare professionals about participants’ self-management improved participants’ attitudes towards the application of advice from healthcare professionals.62,65,70,82 Information received during group sessions such as diabetes education classes and cardiac rehabilitation was mostly well received.49,55,62,65–67,77,87
Provision of Individualized, Culturally Appropriate Advice
A dearth of culturally and individually tailored verbal and written medical advice was reported by participants.45,49,51,59,62,70,73,78,79,82,93,99,101 Some participants, lacking satisfactory medical advice, relied on leaflets50 and their own interpretations of culturally insensitive information to self-manage their chronic diseases.50,62 Generic, culturally inappropriate advice was attributed to the healthcare professional’s lack of awareness,45,49,62,73,87 interest46,101 and time.51
Much dietary advice related to western foods, ingredients and packaging without acknowledging participants’ dietary practices, beliefs or barriers to food preparation,45,49,59,62,73,78,79,82 reducing their self-efficacy and motivation for implementing dietary modification.45,59,62,73,78,79 Suggestions for alternative cooking methods to frying,68,82 substitution or elimination of traditional South Asian ingredients (e.g. ghee)49,73,82 and food consumption techniques49,62,82 were unacceptable to many participants.49,59,62,68,73,82 These participants believed such suggestions reduced the foods’ beneficial properties, but most importantly, palatability.49,68,73,82 Sweeping proposals made by doctors and dietitians alike, to avoid staples of Indian and Pakistani participants’ diets were met with resistance and dismay, and beliefs that doctors and dietitians did not recognize nutritional value or diversity of South Asian foods.62,82 Participants preferred to receive instructions on healthy, appetizing methods of preparing their own regional cuisines and were motivated to adhere to these recipes when provided with this information.45,49,62,73,78,82 Uppal et al100 and Galdas et al67 reported that the provision of culturally tailored dietary advice was more likely improve the uptake of dietary modifications if the advice was delivered to the individual in charge of food preparation (generally a female family member).67,100
Dietary advice did not always address the religious and social importance of food sharing and consumption in South Asian cultures or suggest methods to overcome barriers that food-related customs may pose.73,79,82 Abuelmagd et al52 reported that most participants received advice from their GPs regarding self-management during Ramadan fasting.52 There was no data pertaining to advice provided to participants of diverse religious groups for the management of their religious food practices.
Individually and culturally tailored instructions for exercise were preferred, which considered participants’ physical abilities and preferences of safety, modesty in public spaces, climate and setting of physical activity.66,67,70,83,99 Instructions on the safe undertaking of exercise were not always provided,66,70,83,99 which, for some female participants, had resulted in adverse health outcomes such as falls and anxiety when exercise was attempted83 and reduced participants’ confidence in undertaking general daily activities.66,83,99
Culturally tailored educational interventions reported improvements in participants’ self-management practices42,43,75 and self-efficacy42,43,75,93 with varying statistical significance. For example, Islam et al75 reported that after receiving an educational intervention for diabetes, the percentage of participants using dietary modification to self-manage their diabetes increased from 65.4% to 92.3% (P = 0.054) and those using exercise increased from 50% to 96.2% (P <0.001).75 Additionally, in the study by Hawthorne et al,43 a pilot-tested flashcard educational intervention for diabetes, the proportion of participants who reported self-monitoring their blood glucose after receiving the intervention increased from 63% to 92%, although the authors did not state whether the improvement was statistically significant.43 Poureslami et al93 reported that inhaler technique improved significantly following an asthma educational intervention for all participants (p < 0.001), although improvements in inhaler technique for Punjabi participants were less than Chinese participants (p < 0.001).42,43,93 Intervention studies for diabetes showed small and inconsistent impact on glycemic control.43,75 Hawthorne et al43 reported a small improvement in mean HbA1c levels in the intervention group (8.4% decreased to 8.3%, 95% CI) after receiving the educational intervention compared to the control group (8.6% to 8.64%, 95% CI).43 Islam et al75 showed significant improvements in Bangladeshi participants’ depression risk, with participants’ mean Personal Health Questionnaire Depression Scale (PHQ-2) scores reducing from 2.6 at baseline to 0.9 at 12 months post pilot educational intervention (P < 0.001).75 Information presented through respectful, culturally tailored interventions was appreciated by participants.43,87,97
Most culturally tailored interventions were developed through discussions with healthcare professionals and South Asian community members.42,43,75,93,97 Poureslami et al93 and Singh-Carlson et al97 also collaborated with South Asian patients with chronic diseases and their family carers to develop their interventions.93,97
Theme 4: The Doctor–Patient Relationship
South Asian participants reported regarding doctors as respected experts, who held a high status within the South Asian community.45,53,55,68,72,74,95 Due to the doctors’ expertise, many participants reported following their doctors’ prescribed plan faithfully,45,53,55,63,68,74,95 despite some individuals having differing preferences regarding their treatment.63,74,84 Many participants wished to build rapport with their doctors and sought feedback and encouragement for their efforts to self-manage their chronic diseases.45,49,55,61,65,70,72,99
Many South Asian participants expressed dissatisfaction with the doctor–patient relationship due to the provision of culturally insensitive advice by the doctor, experiencing language barriers,45,102 time-poor consultations45,51 and the doctor’s unapproachable demeanour.45,46,50,51,94,101,102 Participants’ concerns were reported to be discouraged from being expressed or ignored by their doctors.45,51,54,74,94 Inattentiveness or rudeness on the doctor’s part was interpreted by some as discrimination.45,46,102 Some participants reported that doctors merely urged them to adhere to their prescribed medication regimen in response to their questions about their chronic diseases and, in some cases, suggested the participant did not require the requested information.51,61,79,100 Discontentment with their doctors could motivate participants to change services.45,49,51 Although participants generally reported trusting their doctors and the western healthcare system,48,53,63,68,72,74 repeatedly poor experiences reduced some participants’ confidence in healthcare professionals.45,51
Undivided attention, emotional support and empathy from the doctor, and access to culturally appropriate healthcare facilities afforded participants the respect and reassurance they desired,45,51,55,56,71,79,87,96,102 particularly for those undergoing invasive treatments.56,71,96
Preservation of Patient Autonomy
Passive acceptance of and dependence on the doctor’s care was displayed more by older or less acculturated participants45,74,85 due to their perceived lack of control over their chronic disease74,85 and belief that their doctor was best qualified to provide care.45,53,68,72,74,85,95
Participants often reported a preference for self-management advice containing easily applicable, explicit directives rather than having to adapt the general suggestions they received from healthcare professionals to their lifestyles.45,62,70,78,80,99 Participants preferred receiving encouragement and regular reinforcement to follow advice,49,55,61,70,87 although some participants expressed dissatisfaction if they felt pressured to comply with advice by the doctor.61,101 Participants appreciated collaborating with doctors to create a treatment plan.45,71,96,101 Where decisions were made regarding their treatments without sufficient discussion, participants felt their autonomy was compromised.51,74 Lawton et al46 and Fagerli et al45 reported that excessive requests by doctors for participants’ views on advice or treatments prompted some participants to question the doctors’ medical expertise or sense of responsibility to manage patients’ illnesses.45,46 Those who were self-reliant in accessing healthcare appeared more active in making decisions and seeking information about management of their illnesses compared to those who were dependent on their families, such as older women and those facing a language barrier.71,74,79,94,102
Theme 5: The Role of Patients’ Families in Supporting Access and Delivery of Healthcare
Vulnerable participants such as less educated women who faced language barriers47,51,79,94 and those who had migrated to stay with their children at a later age79 required and expected family assistance and support to access healthcare.47,51,51,60,65,77,79,83,87,88,94 Family members organized medical appointments and transport,51,61,65,87 and obtained prescription medication from the pharmacy.47 Participants relied on family members to accompany them to medical appointments.51,61,65,74,77,79,81,86,97 Some participants avoided discussing the full extent of their concerns in front of family members.51,58,87 Participants’ families alerted healthcare professionals to participants’ health concerns.51,54,61,74,88,102 Ens et al61 reported that family members also provided “cultural context”61 to the information provided by healthcare professionals.61,76,102 Those who were able to speak to their healthcare professionals directly or had family members to advocate on their behalf were more likely to report consideration for their cultural or religious needs than those who belonged to isolated populations such as asylum seekers.51,76,94,96 Worth et al102 found that participants were appreciative of healthcare services that were inclusive of their families.102
Family and Decision Making
Participants looked to family members for encouragement and guidance to select their treatment plan74 and attend healthcare services.55,87,88 Families could discourage participants from seeking healthcare for chronic diseases stigmatized in the South Asian community such as depression,87 addiction disorders57 and breast cancer,77 which could delay treatment.57,77 Such family interference aimed to protect the family reputation57 and reflected the family’s lack of understanding for the need to access care.79,87
Family Assisted Translation
Family members, including younger children, offered translation during consultations.46,47,51,58,61,74,79,86,96 Miscommunication between participants and healthcare professionals during family assisted translation occurred due to misinterpretation,51,79 incomplete translation46,51,74,79 and withholding of information by family members.71,74,79,102 In rare cases, participants were excluded from conversations about their treatment, and family members acting as translators made decisions on their behalf without informed consent from the participant.71,74,79 Healthcare professionals did not always obtain permission from participants who relied on family for translation prior to disclosing their cancer diagnosis to family members.71,74 Nevertheless, healthcare professionals and participants continued to rely on family members for translation51,74 and participants reported satisfaction with family support and the privacy this approach afforded.51,74
Discussion
This systematic review examines the patient-centered care experiences, perceptions, attitudes, and preferences among first-generation South Asian migrants with chronic diseases living in high-income, western countries. The authors are not aware of any previous efforts to synthesize the global evidence base around South Asian migrant experiences of western healthcare and preferences for care in such a comprehensive manner.
Thematic analysis identified key themes that represented participants’ experiences of patient-centeredness, which related to accessing appropriate healthcare services, the language barrier, quality and comprehension of healthcare advice, the doctor–patient relationship, and the role of patients’ families. Inadequate or no communication with healthcare professionals seemed to be the primary driver of poor patient-centeredness of care and unsatisfactory interactions, stymieing the development of rapport, which was much valued by migrants from South Asian countries. Participants’ perceptions, identified in this review, that doctors were unwilling or too busy to engage with them concords with results from Franklin et al,103 in which healthcare professionals reported that limited time and heavy workloads hampered their ability to provide self-management support during consultations.103 Worth et al102 found that healthcare professionals felt they lacked awareness of South Asian cultural or religious requirements, and only reported addressing the cultural preferences of patients if raised by the patient or carer.102 Similar to the findings of this review, Shahin et al104 reported in their systematic review that refugees from the Middle East who settled in Sweden reported a high level of reliance on their doctors for self-management support and attributed type 2 diabetes to fate or supernatural causes, which could negatively impact their footcare.104
Cultural barriers driven by the principles of collectivism rooted in South Asian cultural norms may have influenced the experiences of communication between South Asian migrants and healthcare professionals identified in this review.105 Ahmed et al105 found that South Asian individuals are family oriented and experience a strong sense of responsibility to selflessly provide for their families and uphold their families’ perceived pride.105 This sense duty may have motivated participants’ families to support the management of participants’ chronic diseases.47,51,60,65,77,79,83,87,88,94,105 Reliance on family members for translation by South Asian migrants and healthcare professionals was a common finding in the literature, despite the, often, suboptimal quality of the family members’ interpretation. A systematic review by Suphanchaimat et al106 reported that employing phone interpreters to communicate with patients who are migrants added to nursing staff workloads and hindered the provision of healthcare in emergency cases, which could discourage healthcare staff from using interpreter services.106 Zendelel et al,107 when exploring the role of informal interpreters for Turkish patients in Norway, reported that advocacy and translation by family dominated the consultation, misrepresented patients’ symptoms, and disrupted trust between the healthcare professional and patient.107 Despite recognizing this disruption, doctors persisted in the belief that the patient preferred a family member as their translator.107 Additionally, Khosla et al108 found the presence of multiple family members could make it difficult to identify the appropriate person with whom to communicate.108 Conversely, this review found that family carers negotiating care for South Asian participants, more commonly, enhanced the patient’s access to advice and culturally appropriate healthcare, leading to positive outcomes for patients, despite possible shortcomings. The discrepancy between these results is possibly due to healthcare professionals’ perspectives being different from the patients’ perspectives explored in this review.
Kullgren et al109 stated that while logistical barriers such as household responsibilities and lack of access to transport could limit access to healthcare services in the US for ethnic minorities as well as white non-Hispanic adults, white non-Hispanic adults in the US were less likely to experience non-financial barriers (e.g. accommodation barriers such as work and family commitments) to accessing healthcare than Hispanic and non-Hispanic minorities (excluding African American adults).109 Accommodation barriers were more likely to affect women than men,109 which is similar to the findings of this review. Such barriers to healthcare access in South Asian migrants identified in our review may be influenced by members of South Asian communities holding patriarchal beliefs.105,110–112 Traditional gender roles may be enforced due to the collectivist family dynamics and patriarchal beliefs noted in South Asian households.105,113 Gendered expectations of men to financially support the family and of women to assume a subsidiary position to their male spouses while undertaking domestic duties, may have influenced some participants to prioritize their perceived family responsibility over their own health, inhibiting healthcare access.51,55,75,79,87,105 The pressure to uphold the family’s reputation may be associated with some participants’ reluctance to seek help for or openly discuss stigmatized medical conditions with healthcare professionals.57,105
South Asian participants’ dependence upon, preference for and passive acceptance of the doctor’s care, despite appreciating healthcare received from other healthcare professionals,45,50,51,68,81,92,97,101 may be entrenched in previous experiences with traditionally physician-centric, paternalistic healthcare in their countries of origin,114,115 Participants’ preferences for intensive self-management support from doctors and perceptions of the limited roles of other healthcare professionals could conflict with the multidisciplinary healthcare delivered in their western countries of residence, which hold patients equally responsible for their self-management and decision-making.45,114,116 Khosla et al108 added that healthcare professionals in the US believed that South Asian patients were not forthcoming in expressing their preferences regarding their healthcare and cultural needs to avoid disagreements with family members and healthcare professionals.108
A recent scoping review of barriers and facilitators to patient-centered care for migrant and refugee women from multiple ethnic backgrounds excluding those from South Asian countries corroborated many of our findings including the need for longer appointments with healthcare professionals, access to staff from the same ethnic background, and the delivery of linguistically appropriate care.117 While the scoping review identified some broad issues relating to accessing patient-centered care, due to the limited number of papers included and the vast range of ethnicities of study participants, culture and gender-specific issues were not captured in detail.104,117
Strengths, Limitations, and Challenges
Results for this review were drawn from a large number of studies, enabling detailed examination of data from a highly heterogeneous participant cohort in terms of demographics, and settings. Inductively analyzing data enabled themes to arise directly from the data without crucial information being overlooked or misinterpreted due to the researchers’ inflexible, predefined beliefs regarding the themes.118
Quality appraisal of the included papers (Supplementary Material 3) suggested a need for increased methodological rigor and transparency in reporting. However, appraisals should be considered in context of the tools available for use; while they allow comprehensive appraisal, overall scores are, arguably, not always indicative of the value or validity of the findings. For example, because COREQ lends equal importance to criteria such as the reporting of methodology and consistency of results as it does to less relevant criteria such as researcher training, which may not commonly be included in manuscripts, some qualitative papers may have been underrated or overrated.119 Likewise, STROBE is designed with a focus on assessment of epidemiological studies based on observational data. Hence, descriptive, and exploratory studies which do not seek to examine issues such as cause-effect relationships or confounding factors, may be deemed less rigorous.37
The disease states investigated were not diverse as most papers explored cardiovascular disease or diabetes management. Demographic information reported in the included studies was inadequate to determine study eligibility, particularly around migrant generations. While authors were contacted to seek clarity, some did not respond and others indicated the data were not collected, hence some studies with valuable data may have been excluded from the review. However, adhering to strict inclusion criteria ensured that only data pertinent to the population of interest was included in this synthesis.
To guarantee transparency, rigorous documentation of methods and a well-structured coding tree were maintained.120 Including predominantly qualitative papers with limited diversity in participants’ countries of origin and medical conditions could have reduced the transferability of the results.121 To reduce screening errors and optimize the validity and reliability of the review, researcher triangulation was employed throughout the screening process and during the pilot analysis of data.120 The results of the included studies were re-read multiple times and constantly compared to each other to establish credibility of results.120 Regular discussion between authors was undertaken throughout the entirety of the thematic analysis process to review the constant comparisons between the outcomes of studies and ensure that the results of the analysis were logical and faithful to the source data.120,121 The methods used and results obtained at each stage of the review were documented in detail to ensure reproducibility.120
Implications and Conclusions
The results of this systematic review demonstrate that interventions to increase the patient-centeredness of care for first generation, South Asian migrants with chronic diseases living in high-income, western countries may be beneficial for communication between patients and healthcare professionals. At the level of individual healthcare professionals and healthcare services, this review suggests several relatively simple strategies, primarily addressing communication barriers between patients and healthcare professionals, which may support an improved patient experience. These include ensuring a diversity of South Asian healthcare staff, proactively inquiring about patients’ individual, family involvement, linguistic and cultural preferences, and providing cultural competence training for healthcare professionals. Health promotions presented in South Asian community hubs such as places of worship and seniors’ groups could also assist in facilitating conversations about chronic diseases and reducing associated stigmas.122 At a policy level, the results of this review suggest that ensuring adequate support for linguistically appropriate interpreter services at healthcare services could improve the patient centeredness of healthcare.
There are a number of areas for further exploration arising from this work. Studies included in this review were overwhelmingly focused on the management of single diseases, predominantly cardiovascular diseases, and diabetes. There are a range of other highly prevalent and stigmatized conditions and health issues such as neurological and mental illnesses for which data is scarce, not to mention the rising burden of multimorbidity,123 which could increasingly affect individuals as they become older.123 Such clinical issues need to be explored further, particularly for South Asian individuals given their increased vulnerability to type 2 diabetes and its sequalae,124,125 and distinct challenges apparent around access to peer support, and multidisciplinary healthcare for chronic diseases. There is a great need to undertake research that supports development of lifestyle and other interventions to ensure cultural appropriateness, and to support increased access to digital health and multidisciplinary care, particularly as many countries migrate, post-pandemic, towards increasingly telehealth and digital healthcare delivery models.
Acknowledgments
Blair Kelly (Deakin University): Development of search strategy.
Peta Trinder (Deakin University): Organization of literature search results.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interests. No funding was received by the authors to support this systematic review.
References
- 1.United States Census Bureau. 2017 American Community survey 1-year estimates: Asian alone or in any combination by selected groups USA; 2017. Available from: https://www.census.gov/history/pdf/acs15yr-korean62017.pdf. Accessed December 29, 2022.
- 2.Australian Bureau of Statistics. Australia’s population by country of birth; 2022. Available from: https://www.abs.gov.au/statistics/people/population/australias-population-country-birth/latest-release. Accessed December 29, 2022.
- 3.Office for National Statistics. Population of the UK by country of birth and nationality: year ending June 2021; 2021. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/internationalmigration/bulletins/ukpopulationbycountryofbirthandnationality/yearendingjune2021. Accessed December 29, 2022.
- 4.Statistics Canada. Data tables, 2016 census; 2016. Available from: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/dt-td/Rp-eng.cfm?TABID=2&Lang=E&APATH=3&DETAIL=0&DIM=0&FL=A&FREE=0&GC=0&GID=1341679&GK=0&GRP=1&PID=110525&PRID=10&PTYPE=109445&S=0&SHOWALL=0&SUB=0&Temporal=2017&THEME=120&VID=0&VNAMEE=&VNAMEF=&D1=0&D2=0&D3=0&D4=0&D5=0&D6=0. Accessed December 29, 2022.
- 5.The World Bank. South Asia; 2021. Available from: https://www.worldbank.org/en/region/sar. Accessed December 29, 2022.].
- 6.International Organisation for Migration. World Migration Report 2020. Geneva; 2021. Available from: https://worldmigrationreport.iom.int/wmr-2020-interactive/. Accessed December 29, 2022. [Google Scholar]
- 7.Rechel B, Mladovsky P, Ingleby D, Mackenbach JP, McKee M. Migration and health in an increasingly diverse Europe. Lancet. 2013;381(9873):1235–1245. doi: 10.1016/S0140-6736(12)62086-8 [DOI] [PubMed] [Google Scholar]
- 8.Davies A, Blake C, Dhavan P. Social determinants and risk factors for non-communicable diseases (NCDs) in South Asian migrant populations in Europe. Asia Eur J. 2011;8(4):461–473. doi: 10.1007/s10308-011-0291-1 [DOI] [Google Scholar]
- 9.Gholap N, Davies M, Patel K, Sattar N, Khunti K. Type 2 diabetes and cardiovascular disease in South Asians. Prim Care Diabetes. 2011;5(1):45–56. doi: 10.1016/j.pcd.2010.08.002 [DOI] [PubMed] [Google Scholar]
- 10.Cheng YJ, Kanaya AM, Araneta MRG et al. Prevalence of diabetes by race and ethnicity in the United States, 2011–2016. JAMA. 2019;322(24):2389–2398. doi: 10.1001/jama.2019.19365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang H, Naghavi M, Allen C et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459–1544. doi: 10.1016/S0140-6736(16)31012-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Misra A, Tandon N, Ebrahim S et al. Diabetes, cardiovascular disease, and chronic kidney disease in South Asia: current status and future directions. BMJ. 2017;357. doi: 10.1136/bmj.j1420 [DOI] [PubMed] [Google Scholar]
- 13.Van Houtum L, Rijken M, Groenewegen P. Do everyday problems of people with chronic illness interfere with their disease management? BMC Public Health. 2015;15(1):1–9. doi: 10.1186/s12889-015-2303-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. 2012;70(4):351–379. doi: 10.1177/1077558712465774 [DOI] [PubMed] [Google Scholar]
- 15.Michie S, Miles J, Weinman J. Patient-centredness in chronic illness: what is it and does it matter? Patient Educ Couns. 2003;51(3):197–206. doi: 10.1016/S0738-3991(02)00194-5 [DOI] [PubMed] [Google Scholar]
- 16.Bodenheimer T, Lorig K, Holman H, Grumbach K. Patient self-management of chronic disease in primary care. JAMA. 2002;288(19):2469–2475. doi: 10.1001/jama.288.19.2469 [DOI] [PubMed] [Google Scholar]
- 17.Brandenberger J, Tylleskär T, Sontag K, Peterhans B, Ritz N. A systematic literature review of reported challenges in health care delivery to migrants and refugees in high-income countries - The 3C model. BMC Public Health. 2019;19(1):1–11. doi: 10.1186/s12889-019-7049-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Picker Institute. Principles of person centred care; 2021. Available from: https://www.picker.org/about-us/picker-principles-of-person-centred-care/. Accessed December 29, 2022.
- 19.Napier AD, Ancarno C, Butler B et al. Culture and health. Lancet. 2014;384(9954):1607–1639. doi: 10.1016/S0140-6736(14)61603-2 [DOI] [PubMed] [Google Scholar]
- 20.Renzaho AMN, Romios P, Crock C, Sønderlund AL. The effectiveness of cultural competence programs in ethnic minority patient-centered health care—a systematic review of the literature. Int J Qual Health Care. 2013;25(3):261–269. doi: 10.1093/intqhc/mzt006 [DOI] [PubMed] [Google Scholar]
- 21.Anderson LM, Scrimshaw SC, Fullilove MT, Fielding JE, Normand J. Culturally competent healthcare systems: a systematic review. Am J Prev Med. 2003;24(3):68–79. doi: 10.1016/s0749-3797(02)00657-8 [DOI] [PubMed] [Google Scholar]
- 22.Huang Y-C, Garcia AA. Culturally-tailored interventions for chronic disease self-management among Chinese Americans: a systematic review. Ethn Health. 2020;25(3):465–484. doi: 10.1080/13557858.2018.1432752 [DOI] [PubMed] [Google Scholar]
- 23.Zeh P, Sandhu HK, Cannaby AM, Sturt JA. The impact of culturally competent diabetes care interventions for improving diabetes-related outcomes in ethnic minority groups: a systematic review. Diabet Med. 2012;29(10):1237–1252. doi: 10.1111/j.1464-5491.2012.03701.x [DOI] [PubMed] [Google Scholar]
- 24.Popay J, Roberts H, Sowden A et al. Guidance on the conduct of narrative synthesis in systematic reviews. Product ESRC Methods Prog Ver. 2006;1:b92. [Google Scholar]
- 25.Page M, Moher D, Bossuyt PM et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. Br Med J. 2021;372. doi: 10.1136/bmj.n160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Australian Bureau of Statistics. 2016 census quickstats country of birth: people in Australia who were born in Sri Lanka. Australia; 2016. Available from: https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/7107_036. Accessed December 29, 2022. [Google Scholar]
- 27.O’Brien R, Potter-Collins A. 2011 Census analysis: ethnicity and religion of the non-UK born population in England and Wales: 2011. UK: Office for National Statistics; 2015. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/culturalidentity/ethnicity/articles/2011censusanalysisethnicityandreligionofthenonukbornpopulationinenglandandwales/2015-06-18. Accessed December 29, 2022. [Google Scholar]
- 28.Statistics Canada. Immigrant status and period of immigration by place of birth and citizenship: Canada, provinces and territories and census metropolitan areas with parts; 2022. Available from: https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=9810030201. Accessed December 29, 2022.].
- 29.Pew Research Centre. Key facts about Asian Americans, a diverse and growing population; 2021. Available from: https://www.pewresearch.org/fact-tank/2021/04/29/key-facts-about-asian-americans/. Accessed December 29, 2022.
- 30.Greenhalgh T, Peacock R. Effectiveness and efficiency of search methods in systematic reviews of complex evidence: audit of primary sources. BMJ. 2005;331(7524):1064–1065. doi: 10.1136/bmj.38636.593461.68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Australian Institute of Health and Welfare. Exploring the definition of chronic conditions for collective monitoring in Australia. Canberra; 2021. Available from: https://www.aihw.gov.au/getmedia/0e6ef970-84cf-4731-aa15-a03065c16b92/aihw-cvd-91.pdf.aspx?inline=true. Accessed December 29, 2022. [Google Scholar]
- 32.Department of Health. Managing long-term illness and chronic conditions. Victorian Government; 2015. Available from: https://www.betterhealth.vic.gov.au/health/ServicesAndSupport/managing-long-term-illness-and-chronic-conditions. Accessed December 29, 2022. [Google Scholar]
- 33.Australian Bureau of Statistics. Health Conditions Prevalence; 2022. Available from: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/health-conditions-prevalence/latest-release. Accessed December 29, 2022.
- 34.United Nations Department of Economic and Social Affairs. World economic situation and prospects 2021. New York; 2021. [Google Scholar]
- 35.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- 36.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Trials. 2010;11(1):1–8. doi: 10.1186/1745-6215-11-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vandenbroucke JP, Von Elm E, Altman DG et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. PLoS Med. 2007;4(10):e297. doi: 10.1371/journal.pmed.0040297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wang Z, Taylor K, Allman-Farinelli M et al. A systematic review: Tools for assessing methodological quality of human observational studies; 2019.
- 39.Sterne JA, Savović J, Page MJ et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:1. [DOI] [PubMed] [Google Scholar]
- 40.Kim SY, Park JE, Lee YJ et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013;66(4):408–414. doi: 10.1016/j.jclinepi.2012.09.016 [DOI] [PubMed] [Google Scholar]
- 41.Braun V, Clarke V. Using thematic analysis in psychology: Qualitative research in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 42.Hawthorne K. Effect of culturally appropriate health education on glycaemic control and knowledge of diabetes in British Pakistani women with type 2 diabetes mellitus. Health Educ Res. 2001;16(3):373–381. doi: 10.1093/her/16.3.373 [DOI] [PubMed] [Google Scholar]
- 43.Hawthorne K, Tomlinson S. One-to-one teaching with pictures--flashcard health education for British Asians with diabetes. Br J Gen Pract. 1997;47(418):301–304. [PMC free article] [PubMed] [Google Scholar]
- 44.Venkatesh S, Weatherspoon LJ, Kaplowitz SA, Song WO. Acculturation and glycemic control of Asian Indian adults with type 2 diabetes. J Community Health. 2013;38(1):78–85. doi: 10.1007/s10900-012-9584-6 [DOI] [PubMed] [Google Scholar]
- 45.Fagerli R, Lien M, Wandel M. Health worker style and trustworthiness as perceived by Pakistani-born persons with type 2 diabetes in Oslo, Norway. Health. 2007;11(1):109–129. doi: 10.1177/1363459307070810 [DOI] [PubMed] [Google Scholar]
- 46.Lawton J, Ahmad N, Hanna L, Douglas M, Hallowell N. Diabetes service provision: A qualitative study of the experiences and views of Pakistani and Indian patients with Type 2 diabetes. Diabet Med. 2006;23(9):1003–1007. doi: 10.1111/j.1464-5491.2006.01922.x [DOI] [PubMed] [Google Scholar]
- 47.Håkonsen H, Toverud E-L. Cultural influences on medicine use among first-generation Pakistani immigrants in Norway. Eur J Clin Pharmacol. 2012;68(2):171–178. doi: 10.1007/s00228-011-1111-7 [DOI] [PubMed] [Google Scholar]
- 48.Lawton J, Ahmad N, Hallowell N, Hanna L, Douglas M. Perceptions and experiences of taking oral hypoglycaemic agents among people of Pakistani and Indian origin: qualitative study. Br Med J. 2005;330(7502):1247. doi: 10.1136/bmj.38460.642789.E0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gupta SS, Teede H, Aroni R. Spicing up your advice for South Asian and Anglo-Australians with type 2 diabetes and CVD: Do cultural constructions of diet matter? Appetite. 2018;120:679–697. doi: 10.1016/j.appet.2017.10.007 [DOI] [PubMed] [Google Scholar]
- 50.Singh H, Cinnirella M, Bradley C. Support systems for and barriers to diabetes management in South Asians and Whites in the UK: Qualitative study of patients’ perspectives. BMJ Open. 2012;2:6. doi: 10.1136/bmjopen-2012-001459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rhodes P, Nocon A, Wright J. Access to diabetes services: The experiences of Bangladeshi people in Bradford, UK. Ethn Health. 2003;8(3):171–188. doi: 10.1080/1355785032000136407 [DOI] [PubMed] [Google Scholar]
- 52.Abuelmagd W, Håkonsen H, Mahmood KQ-U-A, Taghizadeh N, Toverud E-L. Living with diabetes: Personal interviews with Pakistani women in Norway. J Immigr Minor Health. 2018;20(4):848–853. doi: 10.1007/s10903-017-0622-4 [DOI] [PubMed] [Google Scholar]
- 53.Alhomoud F, Dhillon S, Aslanpour Z, Smith F. South Asian and Middle Eastern patients’ perspectives on medicine-related problems in the United Kingdom. Int J Clin Pharm. 2015;37(4):607–615. doi: 10.1007/s11096-015-0103-6 [DOI] [PubMed] [Google Scholar]
- 54.Balneaves L, Bottorff J, Grewal S, Naidu P, Johnson J, Howard F. Family support of immigrant Punjabi women with breast cancer. Fam Community Health. 2007;30(1):16–28. doi: 10.1097/00003727-200701000-00004 [DOI] [PubMed] [Google Scholar]
- 55.Banerjee A, Grace S, Thomas S, Faulkner G. Cultural factors facilitating cardiac rehabilitation participation among Canadian South Asians: A qualitative study. Heart Lung. 2010;39(6):494–503. doi: 10.1016/j.hrtlng.2009.10.021 [DOI] [PubMed] [Google Scholar]
- 56.Banerjee S, Camacho-Rivera M, Haque N et al. Understanding cognitive and emotional illness representations of South Asian head and neck cancer survivors: A qualitative study. Ethn Health. 2019:1–18. doi: 10.1080/13557858.2019.1625872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bedi H, LeBlanc P, McGregor L, Mather C, King K. Older immigrant Sikh men’s perspective of the challenges of managing coronary heart disease risk. J Mens Health. 2008;5(3):218–226. doi: 10.1016/j.jomh.2008.04.006 [DOI] [Google Scholar]
- 58.Choudhury S, Brophy S, Williams R. Understanding and beliefs of diabetes in the UK Bangladeshi population. Diabet Med. 2009;26(6):636–640. doi: 10.1111/j.1464-5491.2009.02741.x [DOI] [PubMed] [Google Scholar]
- 59.de Brito-ashurst I, Perry L, Sanders T, Thomas J, Yaqoob M, Dobbie H. Barriers and facilitators of dietary sodium restriction amongst Bangladeshi chronic kidney disease patients. J Hum Nutr Diet. 2011;24(1):86–95. doi: 10.1111/j.1365-277X.2010.01129.x [DOI] [PubMed] [Google Scholar]
- 60.Duthie-Nurse G. An anthropological study into the views on diet and disease of a sample of Hindu Gujarati-speaking women with type 2 diabetes. Pract Diabetes Int. 1998;15(4):109–111. doi: 10.1002/pdi.1960150406 [DOI] [Google Scholar]
- 61.Ens T, Seneviratne C, Jones C, King-Shier K. Factors influencing medication adherence in South Asian people with cardiac disorders: An ethnographic study. Int J Nurs Stud. 2014;51(11):1472–1481. doi: 10.1016/j.ijnurstu.2014.02.015 [DOI] [PubMed] [Google Scholar]
- 62.Fagerli R, Lien M, Wandel M. Experience of dietary advice among Pakistani-born persons with type 2 diabetes in Oslo. Appetite. 2005;45(3):295–304. doi: 10.1016/j.appet.2005.07.003 [DOI] [PubMed] [Google Scholar]
- 63.Fleming E, Carter B, Pettigrew J. The influence of culture on diabetes self-management: Perspectives of Gujarati Muslim men who reside in northwest England. J Nurs Healthc Chronic Illn. 2008;17(1):51–59. doi: 10.1111/j.1365-2702.2007.02178.x [DOI] [PubMed] [Google Scholar]
- 64.Galdas P, Cheater F, Marshall P. What is the role of masculinity in white and South Asian men’s decisions to seek medical help for cardiac chest pain? J Health Serv Res Policy. 2007;12(4):223–229. doi: 10.1258/135581907782101552 [DOI] [PubMed] [Google Scholar]
- 65.Galdas PM, Kang HBK. Punjabi Sikh patients’ cardiac rehabilitation experiences following myocardial infarction: A qualitative analysis. J Clin Nurs. 2010;19(21):3134–3142. doi: 10.1111/j.1365-2702.2010.03430.x [DOI] [PubMed] [Google Scholar]
- 66.Galdas PM, Oliffe JL, Kang HBK, Kelly MT. Punjabi Sikh patients’ perceived barriers to engaging in physical exercise following myocardial infarction. Public Health Nurs. 2012;29(6):534–541. doi: 10.1111/j.1525-1446.2012.01009.x [DOI] [PubMed] [Google Scholar]
- 67.Galdas PM, Oliffe JL, Wong ST, Ratner PA, Johnson JL, Kelly MT. Canadian Punjabi Sikh men’s experiences of lifestyle changes following myocardial infarction: Cultural connections. Ethn Health. 2012;17(3):253–266. doi: 10.1080/13557858.2011.610440 [DOI] [PubMed] [Google Scholar]
- 68.Greenhalgh T, Helman C, Chowdhury AM. Health beliefs and folk models of diabetes in British Bangladeshis: A qualitative study. Br Med J. 1998;316(7136):978–983. doi: 10.1136/bmj.316.7136.978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Grewal K, Leung YW, Safai P et al. Access to cardiac rehabilitation among South-Asian patients by referral method: A qualitative study. Rehabilit Nurs. 2010;35(3):106–112. doi: 10.1002/j.2048-7940.2010.tb00285.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gupta SS, Aroni R, Teede H. Experiences and perceptions of physical activity among South Asian and Anglo-Australians with type 2 diabetes or cardiovascular disease: implications for clinical practice. Qual Health Res. 2017;27(3):391–405. doi: 10.1177/1049732316660690 [DOI] [PubMed] [Google Scholar]
- 71.Gurm BK, Stephen J, MacKenzie G, Doll R, Barroetavena MC, Cadell S. Understanding Canadian Punjabi-speaking South Asian women’s experience of breast cancer: a qualitative study. Int J Nurs Stud. 2008;45(2):266–276. doi: 10.1016/j.ijnurstu.2006.08.023 [DOI] [PubMed] [Google Scholar]
- 72.Hawthorne K, Tomlinson S. Pakistani moslems with type 2 diabetes mellitus: Effect of sex, literacy skills, known diabetic complications and place of care on diabetic knowledge, reported self-monitoring management and glycaemic control. Diabet Med. 1999;16(7):591–597. doi: 10.1046/j.1464-5491.1999.00102.x [DOI] [PubMed] [Google Scholar]
- 73.Hempler NF, Nicic S, Ewers B, Willaing I. Dietary education must fit into everyday life: A qualitative study of people with a Pakistani background and type 2 diabetes. Patient Prefer Adherence. 2015;9:347–354. doi: 10.2147/PPA.S77380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Howard AF, Bottorff JL, Balneaves LG, Grewal SK. Punjabi immigrant women’s breast cancer stories. J Immigr Minor Health. 2007;9(4):269–279. doi: 10.1007/s10903-007-9044-z [DOI] [PubMed] [Google Scholar]
- 75.Islam NS, Wyatt LC, Patel SD et al. Evaluation of a community health worker pilot intervention to improve diabetes management in Bangladeshi immigrants with type 2 diabetes in New York City. Diabetes Educ. 2013;39(4):478–493. doi: 10.1177/0145721713491438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Jolly K, Greenfield SM, Hare R. Attendance of ethnic minority patients in cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2004;24(5):308–312. doi: 10.1097/00008483-200409000-00004 [DOI] [PubMed] [Google Scholar]
- 77.Karbani G, Lim JNW, Hewison J et al. Culture, attitude and knowledge about breast cancer and preventive measures: A qualitative study of South Asian breast cancer patients in the UK. APJCP. 2011;12(6):1619–1626. [PubMed] [Google Scholar]
- 78.Khajuria S, Thomas J. Traditional Indian beliefs about the dietary management of diabetes - An exploratory study of the implications for the management of Gujarati diabetics in Britain. J Hum Nutr Diet. 1992;5(5):311–321. doi: 10.1111/j.1365-277X.1992.tb00170.x [DOI] [Google Scholar]
- 79.King KM, LeBlanc P, Sanguins J, Mather C. Gender-based challenges faced by older Sikh women as immigrants: Recognizing and acting on the risk of coronary artery disease. Can J Nurs Res. 2006;38(1):16–40. [PubMed] [Google Scholar]
- 80.King-Shier K, Singh S, Khan N et al. Ethno-cultural considerations in cardiac patients’ medication adherence. Clin Nurs Res. 2017;26(5):576–591. doi: 10.1177/1054773816646078 [DOI] [PubMed] [Google Scholar]
- 81.Kumar DM, Symonds RP, Sundar S, Ibrahim K, Savelyich B, Miller E. Information needs of Asian and White British cancer patients and their families in Leicestershire: A cross-sectional survey. Br J Cancer. 2004;90(8):1474–1478. doi: 10.1038/sj.bjc.6601774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Lawton J, Ahmad N, Hanna L, Douglas M, Bains H, Hallowell N. ‘We should change ourselves, but we can’t’: Accounts of food and eating practices amongst British Pakistanis and Indians with type 2 diabetes. Ethn Health. 2008;13(4):305–319. doi: 10.1080/13557850701882910 [DOI] [PubMed] [Google Scholar]
- 83.Lawton J, Ahmad N, Hanna L, Douglas M, Halloweir N. ‘I can’t do any serious exercise’: Barriers to physical activity amongst people of Pakistani and Indian origin with Type 2 diabetes. Health Educ Res. 2006;21(1):43–54. doi: 10.1093/her/cyh042 [DOI] [PubMed] [Google Scholar]
- 84.Lewis C. Healthcare beliefs of Indian patients living with leg and foot ulcers. Br J Nurs. 2007;16(Sup2):S22–S6. doi: 10.12968/bjon.2007.16.Sup2.23695 [DOI] [PubMed] [Google Scholar]
- 85.Macaden L, Clarke CL. The influence of locus of control on risk perception in older South Asian people with type 2 diabetes in the UK. J Nurs Healthc Chronic Illn. 2010;2(2):144–152. doi: 10.1111/j.1752-9824.2010.01054.x [DOI] [Google Scholar]
- 86.Majeed‐Ariss R, Jackson C, Knapp P, Cheater FM. British‐Pakistani women’s perspectives of diabetes self‐management: The role of identity. J Clin Nurs. 2015;24(17):2571–2580. doi: 10.1111/jocn.12865 [DOI] [PubMed] [Google Scholar]
- 87.Masood Y, Lovell K, Lunat F et al. Group psychological intervention for postnatal depression: A nested qualitative study with British South Asian women. BMC Womens Health. 2015;15:1–8. doi: 10.1186/s12905-015-0263-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.McCleary L, Persaud M, Hum S et al. Pathways to dementia diagnosis among South Asian Canadians. Dementia. 2013;12(6):769–789. doi: 10.1177/1471301212444806 [DOI] [PubMed] [Google Scholar]
- 89.McKenna J, Ludwig AF. Osteoporotic Caucasian and South Asian women: A qualitative study of general practitioners’ support. J R Soc Promot Health. 2008;128(5):263–270. doi: 10.1177/1466424008092796 [DOI] [PubMed] [Google Scholar]
- 90.Mohan S, Wilkes L, Jackson D. Lifestyle of Asian Indians with coronary heart disease: The Australian context. Collegian. 2008;15(3):115–121. doi: 10.1016/j.colegn.2007.03.001 [DOI] [PubMed] [Google Scholar]
- 91.Pardhan S, Mahomed I. Knowledge, self-help and socioeconomic factors in South Asian and Caucasian diabetic patients. Eye. 2004;18(5):509–513. doi: 10.1038/sj.eye.6700680 [DOI] [PubMed] [Google Scholar]
- 92.Patel NR, Kennedy A, Blickem C, Reeves D, Chew-Graham C. ”I’m managing my diabetes between two worlds”: Beliefs and experiences of diabetes management in British South Asians on holiday in the East- A qualitative study. J Diabetes Res. 2016;2016:5436174. doi: 10.1155/2016/5436174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Poureslami I, Nimmon L, Doyle-Waters M et al. Effectiveness of educational interventions on asthma self-management in Punjabi and Chinese asthma patients: A randomized controlled trial. J Asthma. 2012;49(5):542–551. doi: 10.3109/02770903.2012.682125 [DOI] [PubMed] [Google Scholar]
- 94.Schwind JK, Fredericks S, Metersky K, Porzuczek VG. What can be learned from patient stories about living with the chronicity of heart illness? A narrative inquiry. Contemp Nurse. 2016;52(2):216–229. doi: 10.1080/10376178.2015.1089179 [DOI] [PubMed] [Google Scholar]
- 95.Sidhu MS, Griffith L, Jolly K, Gill P, Marshall T, Gale NK. Long-term conditions, self-management and systems of support: An exploration of health beliefs and practices within the Sikh community, Birmingham, UK. Ethn Health. 2016;21(5):498–514. doi: 10.1136/bmjopen-2012-001459 [DOI] [PubMed] [Google Scholar]
- 96.Singh-Carlson S, Neufeld A, Olson J. South Asian immigrant women’s experiences of being respected within cancer treatment settings. Can Oncol Nurs J. 2010;20(4):188–192. doi: 10.5737/1181912x204188192 [DOI] [PubMed] [Google Scholar]
- 97.Singh-Carlson S, Wong F, Oshan G. Evaluation of the delivery of survivorship care plans for South Asian female breast cancer survivors residing in Canada. Curr Oncol. 2018;25(4):e265–e74. doi: 10.3747/co.25.3734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Singh–Carlson S, Nguyen S, Wong F. Perceptions of survivorship care among South Asian female breast cancer survivors. Curr Oncol. 2013;20(2):e80. doi: 10.3747/co.20.1205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Sriskantharajah J, Kai J. Promoting physical activity among South Asian women with coronary heart disease and diabetes: What might help? Fam Pract. 2007;24(1):71–76. doi: 10.1093/fampra/cml066 [DOI] [PubMed] [Google Scholar]
- 100.Uppal G, Sibbald SL, Melling J. Exploring diabetes management amongst immigrant Sikhs in the Greater Toronto Area: A qualitative study. Ethn Health. 2016;21(6):551–563. doi: 10.1080/13557858.2016.1143088 [DOI] [PubMed] [Google Scholar]
- 101.Venkatesh S, Weatherspoon L. Social and health care provider support in diabetes self-management. Am J Health Behav. 2013;37(1):112–121. doi: 10.5993/AJHB.37.1.13 [DOI] [PubMed] [Google Scholar]
- 102.Worth A, Irshad T, Bhopal R et al. Vulnerability and access to care for South Asian Sikh and Muslim patients with life limiting illness in Scotland: Prospective longitudinal qualitative study. Br Med J. 2009;338:b183. doi: 10.1136/bmj.b183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Franklin M, Lewis S, Willis K, Bourke-Taylor H, Smith L. Patients’ and healthcare professionals’ perceptions of self-management support interactions: systematic review and qualitative synthesis. Chronic Illn. 2018;14(2):79–103. doi: 10.1177/1742395317710082 [DOI] [PubMed] [Google Scholar]
- 104.Shahin W, Stupans I, Kennedy G. Health beliefs and chronic illnesses of refugees: A systematic review. Ethn Health. 2021;26(5):756–768. doi: 10.1080/13557858.2018.1557118 [DOI] [PubMed] [Google Scholar]
- 105.Ahmed SM, Lemkau JP. Cultural issues in the primary care of South Asians. J Immigrant Health. 2000;2(2):89–96. doi: 10.1023/A:1009585918590 [DOI] [PubMed] [Google Scholar]
- 106.Suphanchaimat R, Kantamaturapoj K, Putthasri W, Prakongsai P. Challenges in the provision of healthcare services for migrants: a systematic review through providers’ lens. BMC Health Serv Res. 2015;15(1):390. doi: 10.1186/s12913-015-1065-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zendedel R, Schouten BC, van Weert JC, van den Putte B. Informal interpreting in general practice: Comparing the perspectives of general practitioners, migrant patients and family interpreters. Patient Educ Couns. 2016;99(6):981–987. doi: 10.1016/j.pec.2015.12.021 [DOI] [PubMed] [Google Scholar]
- 108.Khosla N, Washington KT, Shaunfield S, Aslakson R. Communication challenges and strategies of US health professionals caring for seriously ill South Asian patients and their families. J Palliat Med. 2017;20(6):611–617. doi: 10.1089/jpm.2016.0167 [DOI] [PubMed] [Google Scholar]
- 109.Kullgren JT, McLaughlin CG, Mitra N, Armstrong K. Nonfinancial barriers and access to care for US adults. Health Serv Res. 2012;47(1pt2):462–485. doi: 10.1111/j.1475-6773.2011.01308.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ahmad F, Riaz S, Barata P, Stewart DE. Patriarchal beliefs and perceptions of abuse among South Asian immigrant women. Violence Against Women. 2004;10(3):262–282. doi: 10.1177/1077801203256000 [DOI] [Google Scholar]
- 111.Tummala-Narra P, Houston-Kolnik J, Sathasivam-Rueckert N, Greeson M. An examination of attitudes toward gender and sexual violence among Asian Indians in the United States. Asian Am J Psychol. 2017;8(2):156. doi: 10.1037/aap0000078 [DOI] [Google Scholar]
- 112.Yoon E, Cabirou L, Bhang C, Galvin S. Acculturation and patriarchal beliefs among Asian American young adults: A preliminary investigation. Asian Am J Psychol. 2019;10(2):122. doi: 10.1037/aap0000130 [DOI] [Google Scholar]
- 113.Yoon E, Chang H, Adams K. Interrelations of patriarchal beliefs, gender, collectivism/ individualism, and mental health. Couns Psychol Q. 2020;33(2):199–217. doi: 10.1080/09515070.2018.1511520 [DOI] [Google Scholar]
- 114.Rao KD, Sundararaman T, Bhatnagar A, Gupta G, Kokho P, Jain K. Which doctor for primary health care? Quality of care and non-physician clinicians in India. Soc Sci Med. 2013;84:30–34. doi: 10.1016/j.socscimed.2013.02.018 [DOI] [PubMed] [Google Scholar]
- 115.Moore M. What does patient‐centred communication mean in Nepal? Med Educ. 2008;42(1):18–26. doi: 10.1111/j.1365-2923.2007.02900.x [DOI] [PubMed] [Google Scholar]
- 116.Bensing J. Bridging the gap.: The separate worlds of evidence-based medicine and patient-centered medicine. Patient Educ Couns. 2000;39(1):17–25. doi: 10.1016/s0738-3991(99)00087-7 [DOI] [PubMed] [Google Scholar]
- 117.Filler T, Jameel B, Gagliardi AR. Barriers and facilitators of patient centered care for immigrant and refugee women: A scoping review. BMC Public Health. 2020;20(1):1–12. doi: 10.1186/s12889-020-09159-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Gioia DA, Corley KG, Hamilton AL. Seeking qualitative rigor in inductive research: Notes on the Gioia methodology. Organl Res Methods. 2013;16(1):15–31. doi: 10.1177/1094428112452151 [DOI] [Google Scholar]
- 119.Dossett LA, Kaji AH, Cochran A. SRQR and COREQ reporting guidelines for qualitative studies. JAMA Surg. 2021;156(9):875. doi: 10.1001/jamasurg.2021.0525 [DOI] [PubMed] [Google Scholar]
- 120.Leung L. Validity, reliability, and generalizability in qualitative research. J Fam Med Prim Care. 2015;4(3):324. doi: 10.4103/2249-4863.161306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Korstjens I, Moser A. Series: practical guidance to qualitative research. Part 4: Trustworthiness and publishing. Eur J Gen Pract. 2018;24(1):120–124. doi: 10.1080/13814788.2017.1375092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Heijnders M, Van Der Meij S. The fight against stigma: An overview of stigma-reduction strategies and interventions. Psychol Health Med. 2006;11(3):353–363. doi: 10.1080/13548500600595327 [DOI] [PubMed] [Google Scholar]
- 123.Vos T, Barber RM, Bell B et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the global burden of disease study 2013. Lancet. 2015;386(9995):743–800. doi: 10.1016/S0140-6736(15)60692-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Sohal T, Sohal P, King-Shier KM, Khan NA. Barriers and facilitators for type-2 diabetes management in South Asians: A systematic review. PLoS One. 2015;10(9):e0136202. doi: 10.1371/journal.pone.0136202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Teljeur C, Smith SM, Paul G, Kelly A, O’Dowd T. Multimorbidity in a cohort of patients with type 2 diabetes. Eur J Gen Pract. 2013;19(1):17–22. doi: 10.3109/13814788.2012.714768 [DOI] [PubMed] [Google Scholar]