Abstract
Background:
Diabetes is a global health issue and the most prevalent chronic metabolic disease, which requires lifelong self-care behaviors. Thus, the present study was conducted with the aim of predicting the factors of self-care behaviors based on social cognitive theory in diabetic patients referred to comprehensive health service centers in Fasa.
Methods:
This cross-sectional research comprised 106 type 2 diabetes patients who were referred to Fasa service providers to determine the optimal solution. Outcomes were assessed using an existing demographic questionnaire, the diabetic self-care questionnaire, and a unique questionnaire to assess social cognitive theory, the validity and reliability of which were estimated. SPSS21 software with a Chi license was used for data analysis, and Spearman correlations, independent t-tests, and one-way ANOVA were performed.
Results:
The age range of patients was between 33 and 67 years. There was a significant relationship between gender, education, and type of treatment with self-care. According to the findings, the variables of self-efficacy (r = 0.200), self-efficacy of overcoming obstacles (r = 0.285), environmental factors (r = 0.334), observational learning ability (r = 0.148), situational perception (r = 0.297), emotional adaptation (r = 0.051), outcome assessment (r = 0.114) and outcome expectation (r = 0.082) had a positive and significant correlation with self-care behaviors. Also, the self-efficacy variable (Beta coefficient = 0.340) had the highest predictive value.
Conclusion:
In designing and implementing educational interventions for self-care of diabetic patients, the theory of social cognition can be used as a framework to promote and maintain public health in patients.
Keywords: Self-care behavior, social cognitive theory, diabetes type II, Iran
Introduction
Diabetes is a chronic disease caused by abnormalities in carbohydrate, protein, and fat metabolism1 and is regarded as the health crisis of the 21st century.2 As reported by the World Health Organization (WHO), in 2000, the number of afflicted was 171 million people, which is predicted to reach 366 million in 2030 if it is not properly controlled.3 The national rate of the disease in Iran is about 4 million, which is three-fold every 15 years, as global statistics show.4
As a chronic disease, diabetes accounts for many significant damages, mortalities, and health costs. Diabetic patients are prone to severe and fatal adverse effects such as retinal damage and blindness, peripheral neuropathy, myocardial infarction, peripheral vascular problems, End Stage Renal Disease (ESRD), diabetic foot, and amputation. These emerge if blood sugar is not properly controlled, and can cause severe damage and mortalities. Yet, good health care and control can help stop many of the bad effects, and if they do happen, they can stop the disabilities that come with them.5
Recent research revealed that diabetes and its adverse effects, such as optical, cardiovascular, and renal side effects can be prevented with the help of a healthy diet, regular physical activity, controlled blood pressure, controlled blood sugar, and a cholesterol-controlled diet.6 Specialists in diabetes perceive education and patients’ self-care behavior as the best strategies for preventing and treating acute adverse effects and lowering the risk of long-term adverse effects.7 The term “self-care” was first coined by Orem, who perceived self-care to include everything an individual does individually for themselves to maintain life and health and always feel happy.8 Self-care behavior among diabetic patients often includes adhering to a healthy diet, regular physical activity, self-monitoring for blood sugar, medication, foot care, and stress management skills.9 Concerning the correlation between healthcare problems and human behavior, behavioral theories and models can be used to determine what social and psychological factors are involved in healthy behaviors and the design of effective and efficient interventions. In fact, theories can be used to increase the efficiency and effectiveness of results.10
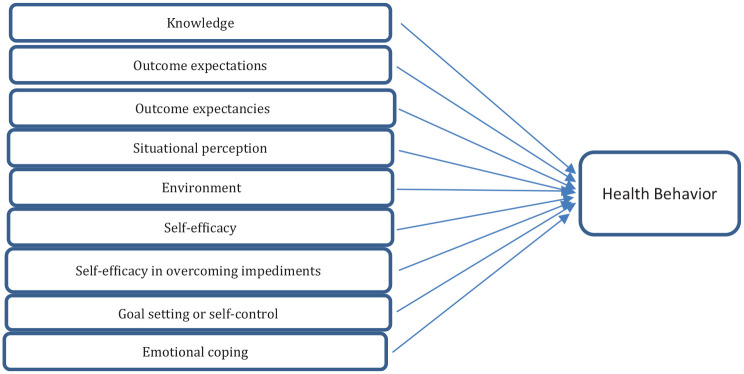
In Bandura’s social cognitive theory, learning is a dynamic interaction of an individual with their surroundings and behavior that finally results in a certain behavior. Bandura’s self-regulatory learning principle emphasizes the active role of an individual in controlling, regulating, and managing oneself and the surrounding environment.11 The constructs of this theory include: knowledge, outcome expectancy, outcome evaluation, situational understanding, self-efficacy, goal-setting or self-control, affective adaptation, and self-efficacy in overcoming barriers12 (Figure 1). The main goal of social cognitive theory (SCT) is to explain human behavior in the form of triangular causality, which includes behavior, the environment, and personal factors (such as cognitions, emotions, and biological events). The constructs of this theory are: knowledge (learning facts and gaining insight about an action, idea, thing, person, or situation); outcome expectation (prediction of the possible consequences that will occur as a result of a particular action); outcome expectancies (the value that a person places on the possible consequences of a behavior); Situational perception (how a person understands and interprets the environment around him), environment (physical or social conditions or situations that include a person), Self-efficacy (a person’s confidence in his ability to pursue a behavior); goal setting or self-control (setting by creating plans for selected behaviors); emotional coping (techniques used by a person to control the emotional and physiological states associated with performing a new behavior); self-sufficiency in overcoming obstacles (a person’s confidence in overcoming obstacles while performing a specific behavior). Considering the significance of diabetes and its adverse effects on physical, economic and social aspects of life and the main role self-care plays in preventing and treating the side effects, the present research aims to examine the prediction of self-care behaviors among diabetic patients based on social cognitive theory.
Figure 1.
Social cognitive theory constructs.
Methods
Study design and recruitment
The present study is a descriptive-analytical study that was conducted with the aim of determining the predictors of self-care behavior in diabetic patients referred to Fasa comprehensive health service centers based on social cognitive theory in 2019. These patients were clients of comprehensive health service centers in Fasa. To determine the sample size according to the information in previous studies and considering d = 0.5 and α = 0.05, the sample size according to the formula was calculated to be 106 people.13 The inclusion criteria were: being affected by diabetes type II for more than a year, ability to attend educational classes, being over 30 years of age, literacy, showing no symptoms of diabetes as diagnosed by a physician. The exclusion criteria were the side effects of diabetes during the educational intervention, hospitalization, immigration, and mortality, and incomplete questionnaire. Sampling was done by presenting a letter of introduction from Hormozgan University of Medical Sciences in the comprehensive health service centers of Fasa city in a simple random manner and based on inclusion criteria. The data collection instrument was a questionnaire comprising three parts, completed twice, once before the intervention and once again 3 months afterward. The demographic questionnaire consisted of two sets of questions: (a) open and closed questions enquiring about demographics, (b) Tubert & Glasgow’s standard questionnaire14: a self-rating questionnaire with 15 items exploring patients’ self-care behaviors within the past week concerning diabetic diets (five items), sports (two items), blood sugar testing (two items), medication (one item), smoking( one item) and foot care (four items). On this scale, except for smoking behavior, which is rated as 0 or 1, each behavior is rated between 0 and 7 and the overall adherence is scored as the sum of the scores for each item. The overall score for the scale ranges between 0 and 99. Tubert et al.15 confirmed the content validity of the questionnaire by a panel of eight experts. In the same research, the reliability was tested through Cronbach’s alpha and reported to be 0.78. (c) A novel questionnaire of the social cognitive theory. To test the face and content validity of the questionnaire, a panel of 10 health education and promotion specialists were consulted, and the required changes were made accordingly. To test the content validity quantitatively, CVI and CVR were used. To test the reliability of the instruments, a pilot test was run during which the questionnaires were submitted to 30 patients who were not in the main research groups. Finally, the reliability of the items was checked through Cronbach’s alpha (test of internal consistency) and shown to be all above 0.85. All constructs except for awareness were rated on a 5-level Likert scale (ranging from strongly disagree to strongly agree). The awareness construct was rated as multiple-choice items (nine items). Outcome expectancy, outcome evaluation, self-efficacy, self-efficacy in overcoming barriers, environment, understanding situation, self-regulation, affective adaptation, observational learning were respectively rated on 6, 9, 10, 7, 4, 4, 7, 3, and 5 items. Table 1 lists a number of questions for each construct for example.
Table 1.
Definitions of constructs and questions.
| Construct | Definition | Questions |
|---|---|---|
| Knowledge | Learning facts and gaining insights related to an action, idea, object, person, or situation | Which food groups are useful for eating? 1. Legumes 2. Cereals (bread, etc.) 3. Simple sugar 4. Low-fat sweets |
| Outcome expectations | Anticipation of the probable outcomes that would ensue as a result of engaging in the behavior under discussion | If I exercise daily, my diabetes will be better controlled. |
| Outcome expectancies | Value a person places on the probable outcomes that result from performing a behavior | It is very important for me to be aware of my illness. |
| Situational perception | How one perceives and interprets the environment around oneself | Access to food for diabetics is not available or limited in stores |
| Environment | Physical or social circumstances or conditions that surround a person | People around me help me when my blood sugar goes up or down. |
| Self-efficacy | Confidence in one’s ability to pursue a behavior | I can take my medication as recommended by my doctor. |
| Self-efficacy In overcoming impediments | Confidence that a person has in overcoming barriers while performing a given behavior | I can maintain my diet on trips and parties. |
| Goal setting or selfcontrol | Setting goals and developing plans to accomplish chosen behaviors | Seeing a doctor less than twice a year does not have good results. |
| Emotional coping | Techniques employed by the person to control the emotional and physiological states associated with acquisition of a new behavior | I wash my feet every day to keep myself healthy and calm. |
Data analysis
The analysis of the research was carried out using SPSS version 24. The research used descriptive analysis (frequency, percentage, average, and standard deviation) as well as statistical analysis (independent t-test, Spearman correlation coefficient, and one-way analysis) with a level of significance of p < 0.05.
Results
Descriptive statistics
The patients ranged in age from 33 to 67 years. 47.2% of the patients were female; 90.7% were married; 35% had a high school diploma; and 32% had a university education. 46.3% were employed, 72.65% had no family history of diabetes, and 72.7% had been sick for less than 10 years. The demographic information for the population covered is provided in Table 2. According to the results, the variables self-efficacy, self-efficacy of overcoming, environmental influences, observational learning, understanding the situation, emotional compatibility, outcome appraisal, and outcome anticipation showed a positive and substantial link with self-care behaviors (Table 3). Furthermore, there is a strong association between gender (compared with female participants, male participants were less likely to report good self-care. . .), education, type of therapy, and self-care, according to the study findings. According to the results, the factors self-efficacy, self-efficacy of overcoming, observational learning, outcome expectation, and emotional compatibility exhibited a strong link with self-care behavior. The last model for predicting structural units, the cognitive or social model, revealed self-care. The greatest degree of association is associated with self-efficacy (Beta coefficient = 0.34), which has a positive and substantial correlation with self-care and comes after overcoming obstacles (Beta coefficient = .30) (Table 4).
Table 2.
Relative frequency distribution of subjects in terms of demographic information.
| Variables | N | % | p-value | |
|---|---|---|---|---|
| Gender | Male | 56 | 52.8 | 1 |
| Female | 50 | 47.2 | ||
| Occupation | Employed | 49 | 46.3 | 0.92 |
| Unemployed | 57 | 53.7 | ||
| Education | Below diploma | 37 | 35 | 0.67 |
| Diploma | 35 | 33 | ||
| Higher degree | 34 | 32 | ||
| Marital status | Single | 4 | 3/7 | 0.24 |
| Married | 96 | 90/7 | ||
| Divorced | 5 | 4/7 | ||
| Widowed | 1 | 0/9 | ||
| Family history of diabetes | Yes | 29 | 27/35 | 0.76 |
| No | 77 | 72/65 | ||
| Salary | <2 million tomans | 50 | 47/2 | 0.56 |
| >2 million tomans | 56 | 52/8 | ||
| Duration of disease | <10 | 77 | 72/7 | 0.61 |
| 10–20 | 24 | 22/6 | ||
| >20 | 5 | 4/7 | ||
Table 3.
Pearson correlation coefficient matrix between dependent and independent variables in patients with type 2 diabetes.
| Variables | Self-care behavior | Awareness | Self-efficacy | Self-efficacy of overcoming | Environmental factors | Observational learning | Understand the situation | Self-regulation | Emotional compatibility | Outcome evaluation | Outcome expectancy |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Self-care behavior | 1 | −0.022 | 0.200 | 0.285* | 0.334 | 0.148 | 0.297* | 0.048 | 0.051 | 0.114 | 0.082 |
| Awareness | 0.022 | 1 | 0.068 | −0.030 | −0.131 | 0.019 | 0.043 | −0.239 | −0.149 | −0.233 | 0.059 |
| Self-efficacy | 0.200* | 0.068 | 1 | 0.476** | 0.351** | 0.005 | −0.185 | −0.209 | −0.247 | 0.052 | 0.107 |
| Self-efficacy of overcoming | 0.285* | −0.030 | 0.476** | 1 | 0.179 | −0.009 | −0.075 | −0.085 | 0.151 | 0.147 | 0.163 |
| Environmental factors | 0.334* | −0.131 | 0.351* | 0.179* | 1 | 0.092 | 0.179 | 0.109 | 0.294* | 0.159 | 0.078 |
| Observational learning | 0.148 | 0.019 | 0.005 | −0.009 | 0.092 | 1 | 0.207 | −0.006 | 0.027 | 0.052 | 0.046 |
| Understand the situation | 0.297* | 0.043 | 0.185 | 0.075 | 0.179 | 0.207 | 1 | 0.020 | 0.035 | 0.041 | 0.148 |
| Self-regulation | 0.048 | 0.239 | 0.209 | 0.082 | 0.109 | −0.006 | 0.020 | 1 | 0.178 | 0.194 | 0.119 |
| Emotional compatibility | 0.051 | 0.149 | 0.247 | 0.151 | 0.294* | 0.027 | −0.035 | 0.178 | 1 | 0.152 | −0.038 |
| Outcome evaluation | 0.114 | 0.231 | 0.052 | 0.147 | −0.159 | 0.052 | 0.041 | 0.194 | 0.152 | 1 | 0.382** |
| Outcome expectancy | 0.082 | 0.059 | 0.107 | 0.163 | −0.078 | 0.046 | 0.148 | 0.119 | 0.038 | 0.382* | 1 |
Pearson Correlation Coefficient *p < .05, **p < .01.
Table 4.
The results of the final model predict the constructs of cognitive or social model structures on self-care for Type 2 diabetes based on linear regression modeling.
| Variables | Standard regression coefficient Beta | The standard error | Non-standardized regression coefficient (B) | t | p-value |
|---|---|---|---|---|---|
| Age | −0.170 | 0.23 | 0.35 | 0.750 | 0.45 |
| Gender | 0.190 | 4.05 | 3.42 | 1.84 | 0.03 |
| Marital status | 0.140 | 4.91 | 7.44 | 1.51 | 0.13 |
| Education | 0.350 | 1.36 | 4.25 | −3.12 | 0.002 |
| BMI | 0.040 | 5.96 | 0.93 | 0.15 | 0.87 |
| Duration of disease | 0.080 | 3.44 | 2.55 | 0.73 | 0.45 |
| Type of treatment | 0.310 | 2.5 | 8.07 | 3.21 | 0.002 |
| Tobacco | 0.140 | 9.54 | 6.17 | 0.64 | 0.52 |
| Duration of smoking | 0.030 | 6.34 | 1.11 | 0.17 | 0.86 |
| Awareness | 0.050 | 0.112 | 0.064 | 0.57 | 0.56 |
| Self-efficacy of overcoming | 0.300 | 0.10 | 0.20 | 2.01 | 0.04 |
| Self-efficacy | 0.340 | 0.15 | 0.22 | 2.01 | 0.03 |
| Observational learning | 0.260 | 0.12 | −0.06 | 1.55 | 0.04 |
| Environmental factors | −0.030 | 0.18 | −0.05 | −0.28 | 0.75 |
| Emotional compatibility | 0.240 | 0.17 | −0.41 | 0.31 | 0.01 |
| Self-regulation | 0.000 | 0.21 | −0.002 | −0.008 | 0.99 |
| Understand the situation | −0.008 | 0.20 | −0.02 | −0.09 | 0.92 |
| Outcome evaluation | 0.080 | 0.22 | 0.20 | 0.92 | 0.35 |
| Outcome expectancy | 0.260 | 0.10 | 0.17 | 2.08 | 0.02 |
The results of linear regression for the predictors of diabetes self-care behaviors score show that the variables of gender, education, type of treatment and self-efficacy construct, self-efficacy to overcome obstacles, observational learning, emotional adaptation, and outcome expectation are significant predictors for performing self-care behaviors. Diabetes was one of the characteristics that might predict 48% of behavioral changes.
Discussion
The current study aims to evaluate the predictors of self-care behaviors in type 2 diabetes patients referred to comprehensive health service facilities in Fasa. According to the study’s findings, the majority of the female patients investigated (35.84%) in both the intervention and control groups were housewives. The majority of the patients evaluated (33.73%) had two to three family members. The majority of the patients in both the intervention and control groups had a diploma.
Self-efficacy, self-efficacy of overcoming, environmental influences, observational learning, understanding the situation, emotional compatibility, outcome assessment, and outcome expectation were all found to have strong and positive links with self-care behaviors.
Gender, education, and treatment type all had a significant relationship with self-care behavior among patients with type 2 diabetes, according to the findings of this study. According to the findings of this research, there is a link between gender and self-care. In the research, there was no statistically significant difference in self-care capacity and gender in diabetic patients.16 In the research by Parham et al., there was no significant difference in self-care practices between men and women with diabetes.17 In Vosoughi et al.’s18 study on diabetic patients, women had greater average self-care skills than males, although this difference was not statistically significant. In research that assessed the self-care capacity of patients with heart failure in the United States, Brouwer et al.19 discovered no significant link between gender and self-care ability. Other characteristics, such as knowledge level, physical-mental state, and behavioral state of people, seem to influence the impact of gender differences on self-care abilities. A substantial link between education and self-care abilities has been documented in various research.18,20,21 According to studies, patients with a higher level of education have greater judgment and decision-making abilities while performing caring behaviors.22 Thus, a high level of education facilitates disease self-care, whereas a low level of education makes this process difficult. Additionally, the mean scores of patients receiving insulin were significantly higher than those receiving oral therapy, indicating that people taking pills or insulin were less likely to require pills or insulin to treat the disease. They were aware of their blood sugar levels, and therefore they were obligated to take tablets or inject insulin for fear of developing chronic diabetes issues.23 They were aware of their blood sugar levels, and therefore they were obligated to take tablets or inject insulin for fear of developing chronic diabetes issues. The ratings of self-care behavior in patients with various medicines (insulin injection or hypoglycemic pills or both) were not substantially different in other studies,24,25 which were inconsistent with the current research. The results of this study showed that self-efficacy is the biggest predictor of self-care behavior in adults with type 2 diabetes. Other predictors include self-efficacy in overcoming obstacles, visible learning capacity, emotional adjustment, and anticipation of outcome. The more the respondents’ confidence in their efficiency and capacity to undertake self-care actions, the more likely they are to accomplish the targeted activity. Some research have shown this correlation.26,27 In their research of diabetic regime behaviors, McCaul et al. observed a strong link between self-efficacy and self-care behaviors in their research, while no correlation was seen in the Stevenson and Gillibrand investigation.28,29 Furthermore, in Chlebowy and Garvin’s study, which examined social support, self-efficacy, and result expectation, as well as self-care and glycemic control behaviors, self-efficacy, and correlation behavior were not significantly related.30 The use of different measuring instruments or the selection of different end variables in the two studies might explain the discrepancy. According to the findings of Salimi et al.’s31 research, social support and self-efficacy components were predictors of breakfast intake among female students among the structures of the social cognitive model. In one study, there was a substantial positive correlation between self-efficacy and self-care behaviors, and a significant negative correlation between perceived obstacles and self-care behaviors in another.32 According to another study, self-efficacy influences physical activity both directly and indirectly through result expectancies, indicating that both factors should be considered. Concentrate on sports behavior adherence treatments.33 Anderson et al.’s34 research on SCT in nutrition found that social support, result expectancies, self-efficacy, and self-regulation were the most significant factors impacting nutritional behavior and diet adoption. According to the findings of Qureshi et al.’s research, the area of emotional adjustment has the greatest degree of association, which has a positive and substantial link with self-care. After that, there is a strong and positive link between taking on challenges and self-control and self-care.35 The mean score of positive or negative emotional adjustment (coping styles) has been shown to vary between high and moderate in the extant research.15,36–38 How people deal with and adapt to daily stresses depends on their age, education, past experiences, culture, living environment, and the severity and frequency of the stresses.
Limitations
There are various limitations to this research that should be mentioned. Here, a question arise, is the approach viable? Diabetic patients’ self-report in the self-care review cited. The participants were over 30 years old, and the majority were married, which may influence self-care practices and collaboration. Another disadvantage of this research is the small number of patient cases.
Conclusion
The findings of the current study incorporate outcome expectation, emotional adjustment, self-efficacy, self-efficacy of overcoming hurdles, and observational learning as drivers of diabetic self-care in type 2 diabetes patients. Exposing patients to successful experiences, providing positive feedback, verbal encouragement, and strengthening existing networks appear to be effective strategies for improving these variables, with the goal of increasing emotional, informational, and instrumental support among patients while increasing the rate. Patients’ self-efficacy and social support may be increased by access, direct observation, and learning from the experiences of others. It is recommended that seminars, courses, and training programs be undertaken in order to strengthen these structures.
Acknowledgments
The authors of the article appreciate all the officials of the studied universities and all the students who participated in this research.
Footnotes
Author contributions: LH designed and performed the research, analyzed the data, and wrote the paper. AY performed research, analyzed data, and wrote the paper. AZ and LH analyzed data and wrote the paper. AZ and AZ designed research and analyzed data. LH and AZ supervised the research and wrote the paper.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Significance for public health: When creating and executing educational programs for patient care, terms of social cognition may be utilized as a choice to adopt programs to improve and preserve the health of these patients. The findings of this research indicated predictors of improved self-care behavior, which may save time and money in health interventions to increase the health of adult diabetes patients in the community. Social cognition theory, on the other hand, may be utilized as a framework for executing promotion programs and sustaining the health of diabetes patients when planning and implementing educational interventions for self-care. Based on predictions from social cognition theory and implementation, this study assists health planners, health and health promotion researchers, and policymakers in developing the most effective and optimal plans for targeted treatments for adult diabetes.
Ethics approval and consent to participate: Hormozgan University’s ethical committee (IR.HUMS.REC.1398.031) approved this study. Written consent was obtained and the samples were assured that the information would remain confidential. All procedures in this study followed the ethical standards of the Helsinki Declaration of 1964, as revised in 2013. Written informed consent was obtained from each participant.
Patient consent for publication: Consent from the patient for publication was taken before collecting the data from them.
Informed consent: Written informed consent was obtained from participation.
ORCID iD: Arash Ziapour  https://orcid.org/0000-0001-8687-7484
https://orcid.org/0000-0001-8687-7484
Availability of data and materials: All the data supporting our findings have been presented in the manuscript; the datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1. Baghianimoghadam MH, Ardekani M, Baghianimoghadam B. Effect of education on improvement of quality of life by SF-20 in type 2 diabetic patients. Acta Med Indonesiana 2009; 41(4): 175. [PubMed] [Google Scholar]
- 2. Jaacks LM, Siegel KR, Gujral UP, et al. Type 2 diabetes: A 21st century epidemic. Best Pract Res Clin Endocrinol Metab 2016; 30(3): 331–343. [DOI] [PubMed] [Google Scholar]
- 3. Shuman C. Diabetes mellitus: definition, classification, and diagnosis. In: Galloway P. (ed.) Diabetes mellitus Galloway. Indianapolis, IN: Lilly Research Laboratories, 1988, p. 168. [Google Scholar]
- 4. American Diabetes Association. 2. Classification and diagnosis of diabetes. Diabetes Care 2015; 38(Supplement_1): S8–S16. [DOI] [PubMed] [Google Scholar]
- 5. Alavi Nia M, Ghotbi M, Mahdavi Hezaveh A, et al. The national program to prevent and control type 2 diabetes, implemented in urban areas. 2012. Tehran: Sepid Barg, 2012. [Google Scholar]
- 6. Shi L, Shu X-O, Li H, et al. Physical activity, smoking, and alcohol consumption in association with incidence of type 2 diabetes among middle-aged and elderly Chinese men. PLoS One 2013; 8(11): e77919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Association AD. Standards of medical care in diabetes—2014. Diabetes Care 2014; 37(1): S14–S80. [DOI] [PubMed] [Google Scholar]
- 8. Ebadi Fard Azar F, Hedari H, Solhi M. Relationship between self-care behavior and health locus of control in patients with type II diabetes. Razi J Med Sci 2016; 23(146): 84–92. [Google Scholar]
- 9. Bohanny W, Wu SFV, Liu CY, et al. Health literacy, self-efficacy, and self-care behaviors in patients with type 2 diabetes mellitus. J Am Assoc Nurse Pract 2013; 25(9): 495–502. [DOI] [PubMed] [Google Scholar]
- 10. Caussidier C, El Hage F, Munoz F, et al. In search of a health education model: teachers’ conceptions in four Mediterranean countries. Glob Health Promot 2011; 18(4): 5–15. [DOI] [PubMed] [Google Scholar]
- 11. Illeris K. Contemporary theories of learning: learning theorists. In their own words. London: Routledge, 2018. [Google Scholar]
- 12. Safari M, Shojaei-Zadeh D, Ghofranipour F, et al. Theories, models and methods of health education and health promotion. Tehran: Asaresobhan, 2009. pp.64–75. [Google Scholar]
- 13. Morowati-Sharifabad M, Rouhani Tonekaboni N, Baghianimoghadam M. Predictors of self-care behaviors among diabetic patients referred to Yazd diabetes research Centre based on extended health belief model. J Shahid Sadoughi Univ Med Sci 2007; 15(3): 85–96. [Google Scholar]
- 14. Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care 2000; 23(7): 943–950. [DOI] [PubMed] [Google Scholar]
- 15. Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes care 2000; 23(7): 943–950. [DOI] [PubMed] [Google Scholar]
- 16. Baghaei P, Zandi M, Vares Z, et al. Self care situation in diabetic patients referring to Kashan Diabetes Center, in 2005. J Kashan Univ Med Sci 2008; 12(1): 88–93. [Google Scholar]
- 17. Parham M, Riahin A, Jandaghi M, et al. Self care behaviors of diabetic patients in Qom. Qom Univ Med S J 2012; 6(4): 81–87. [Google Scholar]
- 18. Vosoghi N, Daryasari GHA, Farahani B, et al. The study of self-care agecy in patients with diabetes (ardabil). Modern Care J 2012; 8: 197–204. [Google Scholar]
- 19. Brouwer BJ, Walker C, Rydahl SJ, et al. Reducing fear of falling in seniors through education and activity programs: a randomized trial. J Am Geriatr Soc 2003; 51(6): 829–834. [DOI] [PubMed] [Google Scholar]
- 20. Shakibazadeh E, Larigani B, SHojaeizadeh D, et al. The relationship between efficacy and perceived barriers to self-care functioning in patients with type 2 diabetes. J Hayat 2009; 15(4): 69–78. [Google Scholar]
- 21. Khazarloo S, Feizi A. Relation between self-efficacy perceived and self-care action in diabetic patients refer to Uromiey diabetes clinic. J Urmia Nurs Mid Fac 2011; 10(3): 369–375. [Google Scholar]
- 22. Barati M. Predicting factors related to self-care behaviors among type 2 diabetic patients based on health belief model. J Torbat Heydariyeh Univ Med Sci 2014; 1(4): 16–25. [Google Scholar]
- 23. Anbari K, Ghanadi K, Kaviani M, et al. The self care and its related factors in diabetic patients of khorramabad city. Yafteh 2012; 14(4): 49–57. [Google Scholar]
- 24. Taghipour A, Meshki M, Mirzaei N. Prediction of self-care behavior using extended theory of reasoned action among women with type 2 diabetes referred to health centers of Mashhad. Ranian J Health Educ Health Promot 2016; 4: 120–129. [Google Scholar]
- 25. Nouhjah S. Self-care behaviors and related factors in women with type 2 diabetes. Iran J Endocrinology Metabol 2015; 16(6): 393–401. [Google Scholar]
- 26. Bernal H, Woolley S, Schensul JJ, et al. Correlates of self-efficacy in diabetes self-care among Hispanic adults with diabetes. Diabetes Educ 2000; 26(4): 673–680. [DOI] [PubMed] [Google Scholar]
- 27. Kavanagh DJ, Gooley S, Wilson PH. Prediction of adherence and control in diabetes. J Behav Med 1993; 16(5): 509–522. [DOI] [PubMed] [Google Scholar]
- 28. McCaul KD, Glasgow RE, Schafer LC. Diabetes regimen behaviors: predicting adherence. Med Care 1987; 25: 868–881. [PubMed] [Google Scholar]
- 29. Gillibrand R, Stevenson J. The extended health belief model applied to the experience of diabetes in young people. Br J Health Psychol 2006; 11(1): 155–169. [DOI] [PubMed] [Google Scholar]
- 30. Chlebowy D, Garvin B. Impact on self-care behaviors and glycemic control in Caucasian and African American adults with type 2 diabetes. Diabetes Educ 2006; 32(5): 777–786. [DOI] [PubMed] [Google Scholar]
- 31. Salimi N, Karimi-Shahanjarini A, Roshanaei G. Regular breakfast consumption and its predictors based on the social cognitive theory in female students of Hamadan University of Medical Sciences. J Educ Community Health 2014; 1(3): 20–27. [Google Scholar]
- 32. Shakibazadeh E, Rashidian A, Larijani B, et al. Perceived barriers and self-efficacy: impact on self-care behaviors in adults with type 2 diabetes. J Hayat 2010; 15(4): 69–78. [Google Scholar]
- 33. White SM, Wójcicki TR, McAuley E. Social cognitive influences on physical activity behavior in middle-aged and older adults. J Gerontol Series B Psychol Sci Soc Sci 2011; 67B(1): 18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Anderson ES, Winett RA, Wojcik JR. Self-regulation, self-efficacy, outcome expectations, and social support: social cognitive theory and nutrition behavior. Ann Behav Med 2007; 34(3): 304–312. [DOI] [PubMed] [Google Scholar]
- 35. Ghoreishi MS, Vahedian SM, Esmaily H, et al. Predictive factors related to self-care behaviors among type2 diabetic patients by using social cognitive model. Iran J Health Edu Health Prom 2018; 6: 241–250. [Google Scholar]
- 36. Ouyang C-M. Factors affecting diabetes self-care among patients with type 2 diabetes in Taiwan. Medford, MA: Tufts University, 2007. [Google Scholar]
- 37. Samuel-Hodge CD, Watkins DC, Rowell KL, et al. Coping styles, well-being, and self-care behaviors among African Americans with type 2 diabetes. Diabetes Educ 2008; 34(3): 501–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kaboudi M, Dehghan F, Ziapour A. The effect of acceptance and commitment therapy on the mental health of women patients with type II diabetes. Ann Trop Med Public Health 2017; 10: 1709–1713. [Google Scholar]