Abstract
The incidence of anterior cruciate ligament injuries in skeletally immature patients has increased in recent years. The gold standard treatment of this type of trauma in children is not yet established. Conservative management may underestimate the risk of new meniscal and chondral tears; on the other hand, a more interventional approach may expose the patient to iatrogenic damage to the growth plate. A correct approach to the skeletally immature patient with knee trauma is therefore essential to guide the decision-making process. This review article aims to present an update on the epidemiology and diagnostic process of pediatric patients with anterior cruciate ligament tears and possible associated injuries.
Level of Evidence: V.
Keywords: Anterior cruciate ligament, ACL, pediatric, skeletally immature
Introduction
Anterior cruciate ligament (ACL) injury in the skeletally immature patient is a controversial area in sports trauma. 1 ACL tears have been considered rare injuries in younger patients, but the increasing participation in contact sports activity, especially at the competitive level, a greater awareness of the injured athlete, and the availability of more effective and less invasive diagnostic methods, have found an increase in ACL injuries in children and adolescents.2–4 However, the gold standard treatment for these patients remains controversial, and we are torn between maintaining a conservative stance or being more interventional. Proposing rest and a protocol for incorporation into sports practice underestimates the meniscal and chondral injuries that could occur due to secondary instability. It is the price to avoid possible iatrogenic physeal injuries, with a possible dysmetria and alteration of the axes.5–8 On the other hand, new types of surgery gaining popularity minimize risk of physeal plate damage and help restoring joint stability, preventing possible future meniscal and chondral lesions.9–16
The pediatric knee
The ACL image can be visualized starting from the eighth week of gestation, together with the rest of the intra-articular structures. Around the 24th week, collagen fibers are observed in the intercondylar notch that run from the periosteum of the femoral condyle to the proximal tibia. The definitive and organized anchorage of the ACL to the subchondral bone is observed at week 36.17,18
The infant knee has interesting anatomical characteristics. Evidently, it presents growth cartilages (physis) and the epiphyses of the infant knee present a high percentage of cartilaginous tissue. But the growth is not only longitudinal, generated by the physis; there is also a growth in thickness, latitudinal, both physeal and epiphyseal, the latter generated by the articular cartilage. The physes near the knee are more fertile and responsible for 65%–70% of the total longitudinal growth of the lower extremity. 19 Any alteration of the physeal function will produce growth disorders, triggering asymmetries and angular deformities.
The distance from the physeal plate to the femoral attachment of the ACL remains constant during growth, being approximately 3 mm. 20 However, the distance from the tibial attachment to the proximal tibial physis varies slightly during growth. 21 Variations according to age and sex have also been observed in terms of the position and angulation of the tibial insertion of the ACL with a slightly more horizontal ligament in younger age stabilizing around the age of 18 years. 22
The intercondylar notch grows and widens considerably until the age of 11 years, then subtly until skeletal maturity. 23 The presence of the lateral intercondylar ridge or “resident’s ridge” is less frequent and less defined, being observed in 44%–63% of patients younger than 12 years of age.24,25
The size of the two fascicles, antero-medial and postero-lateral, of the ACL varies according to the height and weight of the patients during growth. 26 There is little information on the biomechanics of the ACL in immature patients; in animal studies, age-related changes have been observed, and differences in laxity in relation to age and sex have also been observed.27–29
The knee environment of pediatric and adolescent patients is also different compared with adults in terms of response to a traumatic injury. Interestingly, a recent study showed a better regulation of the acute inflammatory response in skeletally immature patients, supporting the thesis of a higher healing potential of young subjects. 30
Epidemiology
The actual prevalence of ACL tears is unknown. Some small studies were carried out at the end of the last century. In one of them, they observed an incidence of 16 per 1000 in high school athletes, especially in girls with early specialization in sports. 31 Beck et al. 32 found that the incidence of ACL tears in pediatric patients has increased over the last 20 years. Higher incidence was observed in girls, with a peak incidence during high school years. Gender-related incidence studies described a significant decline in the incidence of ACL tears among males aged 14 to 18; in contrast, the incidence of ACL tears in female subjects remained relatively stable (Figure 1). 33 Several factors are associated to the higher incidence of ACL lesion in the female sex: hyperlaxity, higher Q angle, larger size of the femoral intercondylar notch, and a smaller ligament in diameter, in addition to hormonal and neuromuscular factors.29,34–38
Figure 1.
Gender-related incidence of ACL injury. 39
An epidemiologic analysis of a New York State administrative database revealed that the rate of ACL reconstruction in children less than 20 years of age had increased nearly threefold over a 20-year period and indicated that adolescents and teenagers represent the largest per capita demographic of ACL reconstructions. 39 (33) In another registry, the Pediatric Health Information System, it has been observed that ACL reconstructions showed 5.7-fold increases over 10 years. 40 This trend has been increasing between 2016 and 2021; there were fewer than expected during the COVID-19 pandemic. There was a 30% decrease in the number of Anterior Cruciate Ligamente Reconstructions (ACLRs) overall from the pre-pandemic to the intra-pandemic times. Notably, there has been a disparate impact of the pandemic on patients depending on their race and insurance status. 41
In Europe, the European Society for Sports Traumatology, Knee Surgery and Arthroscopy. (ESSKA) has promoted the Pediatric Anterior Cruciate Ligament Initiative (PAMI) registry, which began in 2018 and has recently presented the preliminary results of the recruitment and follow-up experience of the first 100 patients. 42 The nationwide population-based study observed that the incidence of pediatric ACL injury increased during the 18-year study period; nearly twofold increase was noted during the last 10 years of the study period in Finland. 43
Shea et al. suggested that a greater awareness and a more accurate diagnosis, together with a higher participation of children in competitive sports and sports specialization at an early age, concurred to this increased trend in ACL reconstruction surgeries in pediatric and adolescent patients.3,44,45
Studying the incidence rate in relation to gender and sports, we can observe that the incidence of ACL injury is influenced also by the nature of player-to-player contact inherent in the sport. Female athletes had greater ACL injury rates than male athletes in contact and fixed-object and high impact rotational landing sports (Figure 2). 46 Bram et al. 47 in a systematic review and meta-analysis concluded that the risk of ACL injuries overall approached nearly 1 per 10,000 for female athletes, who were almost 1.5 times as likely as male athletes to suffer an ACL injury across all adolescent sports. A multisport female athlete was estimated to have a nearly 10% risk of ACL injuries over her entire high school or secondary school career. Specifically, male and female adolescents playing soccer, basketball, lacrosse, and football appeared at particular risk of injuries. 47
Figure 2.
ACL incidence rate in relation to gender and sports. 47
Anatomical factors related to increased risk of ACL tear have also been observed, such as increased tibial slope, narrow intercondylar notch, and patella alta.48–50
Clinical evaluation of the pediatric patient with ACL tear
Previous studies have identified combined multi-planar loading including anterior tibial shear, knee valgus, and internal tibial rotation to be the worst-case scenario and primary mechanism of non-contact ACL injury. A hyperextension of the knee with a valgus or rotational force has also been described. 51
The clinical history is usually revealing as patients report that after a turn with the foot fixed, they noticed a clicking sound in the knee sometimes audible even by the closest players. 52 The effusion and joint swelling are immediate, and the pain is variable, but usually increases, in the days after the injury. In general, the sensation of instability is less frequent than in skeletally mature patients.
Physical examination usually shows joint effusion, with diffuse pain and limited range of motion. In the event of a traumatic effusion, arthrocentesis is an option for both pain relief and diagnostic tool. Hemarthrosis in pediatric patients has been found in 10%–65% of ACL tears due to acute trauma; this finding should suggest a possible cruciate ligament tear.31,53
The maneuvers to assess the stability of the knee are the same as in adults. The uninjured knee should also be examined to evaluate healthy joint characteristics and have a comparison with the injured leg. 54 Although in the acute setting patients usually present an involuntary muscular defense that does not allow an accurate exploration, a second evaluation after some days is recommended in case of difficulties at the first visit. The most used clinical maneuvers are the Lachmann test, the pivot-shift, together with anterior and posterior drawers with internal and external tibial rotation. It is important to notice that in ACL injured patients, the pivot-shift test is positive up to 98% of the time after anesthesia, while in conscious patients it only reaches 35% of the cases. 15
In the evaluation of pediatric patients, it is mandatory to evaluate the degree of maturity using the Tanner scale. 55 Dysmetria of the lower extremities and the angular alterations prior to the intervention are also important to explore to have a baseline evaluation.
Imaging
An X-ray should be a routine test to rule out osteo-cartilaginous injuries and physeal fractures (Figure 3). A baseline knee radiograph is also useful to initially evaluate the skeletal maturity of the patient: open, closing, and closed physis are the three main class. 56
Figure 3.
(a) Radiographic lateral view of knee after trauma with a spinal avulsion. (b) Radiographic anteroposterior view of an osteochondral lesion of the medial femoral condyle.
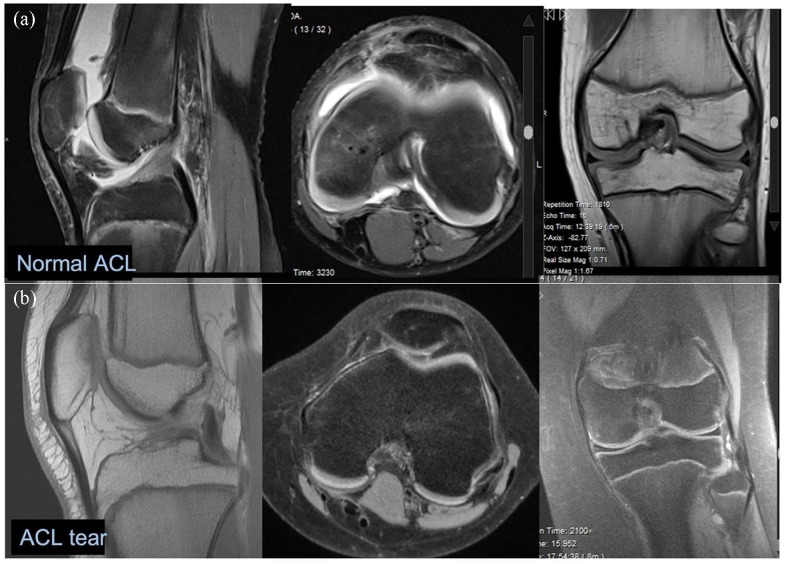
Magnetic resonance imaging is the method of choice to evaluate an injured knee with a clinical suspect of ACL tear (Figure 4). Primary findings are an abnormal signal intensity of the ACL, discontinuity of the ligament, and Blumensaat’s angle of >9.5° (Figure 5). 57 Secondary criteria include lateral compartment bone bruise, anterior tibial displacement, uncovered posterior horn of the lateral meniscus, change in the posterior cruciate line, and posterior cruciate angle <115° (Figure 6). In the study published by Lee et al., 57 the magnetic resonance imaging (MRI) sensitivity was 95%, and specificity was 88%. Moreover, the MRI is also useful to define ACL pattern of lesion.
Figure 4.
MRI of the knee. (a) Normal ACL images. (b) ACL tear.
Figure 5.
Primary findings that suggest an ACL injury are abnormal signal intensity of the ACL (a), discontinuity of the ligament (b), a Blumensaat’s angle > 9.5° (c).
Figure 6.
Secondary criteria for ACL injury diagnose include lateral compartment bone bruise (a), anterior tibial displacement (b), uncovered posterior horn of the lateral meniscus (c), change in the posterior cruciate line, and posterior cruciate angle < 115° (d).
A good MRI quality of image is also important to define the level of the ACL lesion. A classification proposed by Van Der List et al. 58 describe five categories based on tear location in terms of distal remnant expressed as a percentage of ligament length: (1) proximal avulsion tears (Type I, > 90%), (2) proximal tears (Type II, 75%–90%), (3) midsubstance tears (Type III, 25%–75%), (4) distal tears (Type IV, 10%–25%), or (5) distal avulsion tears (Type V, <10%). The characterization of the ACL tear level is important to take in consideration ACL repair surgery in case of proximal ACL tears. 59
In Type I and V is also important to distinguish two other categories: soft tissue ACL lesion or bony avulsion tear. Distal bony avulsion tears are further graded according to the Meyers–McKeever classification modified by Zaricznyj. 60 In open physis patients with normal radiographs, it is important also to consider the presence of a chondral spine avulsion; the avulsed fragment may appear as a double-POsterior Cruciate Ligament (PCL) sign. 41
MRI is also the most accurate imaging method to detect the presence of concomitant meniscal and chondral injuries with a high degree of reliability. 61 The prevalence of bone bruises in pediatric patients with ACL tears is high, close to 70% of the cases. 62 Bone bruise without ACL injury or partial injuries have been observed frequently in this age group.63,64 The area and the distribution pattern of bone bruises are similar among different ages.
The preoperative evaluation of a skeletally immature patient with ACL tear should be completed with a radiographic assessment of skeletal age using the Greulich and Pyle method by counting the ossification nuclei of the carpal bones in a dorsal-palmar radiograph of the non-dominant hand. 65 Other locations such as the pelvis, the elbow, and the calcaneus have also been used.66–68 The knee MRI is also useful to assess the bone age; an Atlas of skeletal development of the knee was recently published and is demonstrated to provide a precise estimation of the residual bone growth. 69
In addition, it is recommended to obtain standing full-length lower limb radiograph to explore potential preoperative limb length discrepancy and angular alterations.15,70
In conclusion, a careful evaluation is essential to determine knee stability after trauma, especially in very young patients. The diagnostic process needs to follow precise steps to assess the presence of ligament injuries, tear level, and concomitant injuries, along with measuring skeletal maturity. All clinical information must be mixed with the patient’s sport level and parent’s considerations to probe the delicate treatment decision process.
Footnotes
Author contributions: JDC participated in the design of the study and drafted the manuscript. LR participated in the design of the study and manuscript drafting and revision. MB helped with the manuscript drafting and revision. MSK participated in the design of the study and manuscript revision.
Compliance with ethical standards: No data sets were generated or analyzed during the current study. The study was approved by the local Ethical Committee and conforms to the principles outlined in the WMA Declaration of Helsinki.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Julio Duart  https://orcid.org/0000-0003-3121-3669
https://orcid.org/0000-0003-3121-3669
Luca Rigamonti  https://orcid.org/0000-0001-8547-3074
https://orcid.org/0000-0001-8547-3074
References
- 1. Parikh SN, Jaquith BP, Brusalis CM, et al. Skeletally immature anterior cruciate ligament injuries: controversies and management. Instr Course Lect 2017; 66: 461–474. [PubMed] [Google Scholar]
- 2. Louw QA, Manilall J, Grimmer KA. Epidemiology of knee injuries among adolescents: a systematic review. Br J Sports Med 2008; 42(1): 2–10. [DOI] [PubMed] [Google Scholar]
- 3. Shea KG, Grimm NL, Ewing CK, et al. Youth sports anterior cruciate ligament and knee injury epidemiology: who is getting injured? In what sports? When? Clin Sports Med 2011; 30(4): 691–706. [DOI] [PubMed] [Google Scholar]
- 4. Bigoni M, Turati M, Zatti G, et al. Intra-articular cytokine levels in adolescent patients after anterior cruciate ligament tear. Mediators Inflamm 2018; 2018: 4210593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Koman JD, Sanders JO. Valgus deformity after reconstruction of the anterior cruciate ligament in a skeletally immature patient. A case report. J Bone Joint Surg Am 1999; 81: 711–715. [DOI] [PubMed] [Google Scholar]
- 6. Kocher MS, Saxon HS, Hovis WD, et al. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: survey of the Herodicus Society and The ACL Study Group. J Pediatr Orthop 2002; 22(4): 452–457. [PubMed] [Google Scholar]
- 7. Yoo WJ, Kocher MS, Micheli LJ. Growth plate disturbance after transphyseal reconstruction of the anterior cruciate ligament in skeletally immature adolescent patients: an MR imaging study. J Pediatr Orthop 2011; 31(6): 691–696. [DOI] [PubMed] [Google Scholar]
- 8. Vavken P, Murray MM. Treating anterior cruciate ligament tears in skeletally immature patients. Arthroscopy 2011; 27(5): 704–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. DeLee JC, Curtis R. Anterior cruciate ligament insufficiency in children. Clin Orthop Relat Res 1983; 172: 112–118. [PubMed] [Google Scholar]
- 10. Engebretsen L, Svenningsen S, Benum P. Poor results of anterior cruciate ligament repair in adolescence. Acta Orthop Scand 1988; 59(6): 684–686. [DOI] [PubMed] [Google Scholar]
- 11. Brief LP. Anterior cruciate ligament reconstruction without drill holes. Arthroscopy 1991; 7: 350–357. [DOI] [PubMed] [Google Scholar]
- 12. Anderson AF. Transepiphyseal replacement of the anterior cruciate ligament using quadruple hamstring grafts in skeletally immature patients. J Bone Joint Surg Am 2004; 86-A(Suppl. 1): 201–209. [DOI] [PubMed] [Google Scholar]
- 13. Kocher MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents. J Bone Joint Surg Am 2005; 87: 2371–2379. [DOI] [PubMed] [Google Scholar]
- 14. McCarthy MM, Graziano J, Green DW, et al. All-epiphyseal, all-inside anterior cruciate ligament reconstruction technique for skeletally immature patients. Arthrosc Tech 2012; 1(2): e231–e239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Fabricant PD, Jones KJ, Delos D, et al. Reconstruction of the anterior cruciate ligament in the skeletally immature athlete: a review of current concepts: AAOS exhibit selection. J Bone Joint Surg Am 2013; 95: e28. [DOI] [PubMed] [Google Scholar]
- 16. Schilaty ND, Martin RK, Ueno R, et al. Mechanics of cadaveric anterior cruciate ligament reconstructions during simulated jump landing tasks: lessons learned from a pilot investigation. Clin Biomech 2021; 86: 105372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ellison AE, Berg EE. Embryology, anatomy, and function of the anterior cruciate ligament. Orthop Clin North Am 1985; 16(1): 3–14. [PubMed] [Google Scholar]
- 18. Merida-Velasco JA, Sanchez-Montesinos I, Espin-Ferra J, et al. Development of the human knee joint. Anat Rec 1997; 248: 269–278. [DOI] [PubMed] [Google Scholar]
- 19. Pritchett JW. Longitudinal growth and growth-plate activity in the lower extremity. Clin Orthop Relat Res 1992; 275: 274–279. [PubMed] [Google Scholar]
- 20. Behr CT, Potter HG, Paletta GA., Jr. The relationship of the femoral origin of the anterior cruciate ligament and the distal femoral physeal plate in the skeletally immature knee. An anatomic study. Am J Sports Med 2001; 29(6): 781–787. [DOI] [PubMed] [Google Scholar]
- 21. Swami VG, Mabee M, Hui C, et al. MRI anatomy of the tibial ACL attachment and proximal epiphysis in a large population of skeletally immature knees: reference parameters for planning anatomic physeal-sparing ACL reconstruction. Am J Sports Med 2014; 42(7): 1644–1651. [DOI] [PubMed] [Google Scholar]
- 22. Shea KG, Apel PJ, Pfeiffer RP, et al. The anatomy of the proximal tibia in pediatric and adolescent patients: implications for ACL reconstruction and prevention of physeal arrest. Knee Surg Sports Traumatol Arthrosc 2007; 15(4): 320–327. [DOI] [PubMed] [Google Scholar]
- 23. Tuca M, Hayter C, Potter H, et al. Anterior cruciate ligament and intercondylar notch growth plateaus prior to cessation of longitudinal growth: an MRI observational study. Knee Surg Sports Traumatol Arthrosc 2016; 24(3): 780–787. [DOI] [PubMed] [Google Scholar]
- 24. Liu RW, Farrow LD, Messerschmitt PJ, et al. An anatomical study of the pediatric intercondylar notch. J Pediatr Orthop 2008; 28(2): 177–183. [DOI] [PubMed] [Google Scholar]
- 25. Samora W, Beran MC, Parikh SN. Intercondylar roof inclination angle: is it a risk factor for ACL tears or tibial spine fractures? J Pediatr Orthop 2016; 36: e71–e74. [DOI] [PubMed] [Google Scholar]
- 26. Kopf S, Pombo MW, Szczodry M, et al. Size variability of the human anterior cruciate ligament insertion sites. Am J Sports Med 2011; 39(1): 108–113. [DOI] [PubMed] [Google Scholar]
- 27. Noyes FR, Barber-Westin SD. Neuromuscular retraining intervention programs: do they reduce noncontact anterior cruciate ligament injury rates in adolescent female athletes? Arthroscopy 2014; 30(2): 245–255. [DOI] [PubMed] [Google Scholar]
- 28. Woo SL, Debski RE, Withrow JD, et al. Biomechanics of knee ligaments. Am J Sports Med 1999; 27: 533–543. [DOI] [PubMed] [Google Scholar]
- 29. Hinton RY, Rivera VR, Pautz MJ, et al. Ligamentous laxity of the knee during childhood and adolescence. J Pediatr Orthop 2008; 28(2): 184–187. [DOI] [PubMed] [Google Scholar]
- 30. Turati M, Franchi S, Leone G, et al. Resolvin E1 and cytokines environment in skeletally immature and adult ACL tears. Front Med 2021; 8: 610866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Vahasarja V, Kinnuen P, Serlo W. Arthroscopy of the acute traumatic knee in children. Prospective study of 138 cases. Acta Orthop Scand 1993; 64(5): 580–582. [DOI] [PubMed] [Google Scholar]
- 32. Beck NA, Lawrence JTR, Nordin JD, et al. ACL tears in school-aged children and adolescents over 20 years. Pediatrics 2017; 139(3): e20161877. [DOI] [PubMed] [Google Scholar]
- 33. Sanders TL, Maradit Kremers H, Bryan AJ, et al. Incidence of anterior cruciate ligament tears and reconstruction: a 21-year population-based study. Am J Sports Med 2016; 44(6): 1502–1507. [DOI] [PubMed] [Google Scholar]
- 34. Komatsuda T, Sugita T, Sano H, et al. Does estrogen alter the mechanical properties of the anterior cruciate ligament? An experimental study in rabbits. Acta Orthop 2006; 77(6): 973–980. [DOI] [PubMed] [Google Scholar]
- 35. Hewett TE, Zazulak BT, Myer GD. Effects of the menstrual cycle on anterior cruciate ligament injury risk: a systematic review. Am J Sports Med 2007; 35: 659–668. [DOI] [PubMed] [Google Scholar]
- 36. Dragoo JL, Padrez K, Workman R, et al. The effect of relaxin on the female anterior cruciate ligament: analysis of mechanical properties in an animal model. Knee 2009; 16(1): 69–72. [DOI] [PubMed] [Google Scholar]
- 37. Gornitzky AL, Lott A, Yellin JL, et al. Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: a systematic review and meta-analysis. Am J Sports Med 2016; 44(10): 2716–2723. [DOI] [PubMed] [Google Scholar]
- 38. Ford KR, Shapiro R, Myer GD, et al. Longitudinal sex differences during landing in knee abduction in young athletes. Med Sci Sports Exerc 2010; 42(10): 1923–1931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dodwell ER, Lamont LE, Green DW, et al. 20 years of pediatric anterior cruciate ligament reconstruction in New York state. Am J Sports Med 2014; 42(3): 675–680. [DOI] [PubMed] [Google Scholar]
- 40. Tepolt FA, Feldman L, Kocher MS. Trends in pediatric ACL reconstruction from the PHIS database. J Pediatr Orthop 2018; 38(9): e490–e494. [DOI] [PubMed] [Google Scholar]
- 41. Kiani SN, Yellin JL, Houlihan NV, et al. Trends in pediatric ACL reconstruction: the impact of COVID-19. J Athl Train 2022; 57: 972–977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mouton C, Moksnes H, Janssen R, et al. Preliminary experience of an international orthopaedic registry: the ESSKA Paediatric Anterior Cruciate Ligament Initiative (PAMI) registry. J Exp Orthop 2021; 8: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Weitz FK, Sillanpaa PJ, Mattila VM. The incidence of paediatric ACL injury is increasing in Finland. Knee Surg Sports Traumatol Arthrosc 2020; 28(2): 363–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Werner BC, Yang S, Looney AM, et al. Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop 2016; 36(5): 447–452. [DOI] [PubMed] [Google Scholar]
- 45. Beynnon BD, Vacek PM, Newell MK, et al. The effects of level of competition, sport, and sex on the incidence of first-time noncontact anterior cruciate ligament injury. Am J Sports Med 2014; 42(8): 1806–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Montalvo AM, Schneider DK, Webster KE, et al. Anterior cruciate ligament injury risk in sport: a systematic review and meta-analysis of injury incidence by sex and sport classification. J Athl Train 2019; 54(5): 472–482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Bram JT, Magee LC, Mehta NN, et al. Anterior cruciate ligament injury incidence in adolescent athletes: a systematic review and meta-analysis. Am J Sports Med 2021; 49(7): 1962–1972. [DOI] [PubMed] [Google Scholar]
- 48. Degnan AJ, Maldjian C, Adam RJ, et al. Comparison of Insall-Salvati ratios in children with an acute anterior cruciate ligament tear and a matched control population. AJR Am J Roentgenol 2015; 204(1): 161–166. [DOI] [PubMed] [Google Scholar]
- 49. Dare DM, Fabricant PD, McCarthy MM, et al. Increased lateral tibial slope is a risk factor for pediatric anterior cruciate ligament injury: an MRI-based case-control study of 152 patients. Am J Sports Med 2015; 43(7): 1632–1639. [DOI] [PubMed] [Google Scholar]
- 50. Swami VG, Mabee M, Hui C, et al. Three-dimensional intercondylar notch volumes in a skeletally immature pediatric population: a magnetic resonance imaging-based anatomic comparison of knees with torn and intact anterior cruciate ligaments. Arthroscopy 2013; 29(12): 1954–1962. [DOI] [PubMed] [Google Scholar]
- 51. Levine JW, Kiapour AM, Quatman CE, et al. Clinically relevant injury patterns after an anterior cruciate ligament injury provide insight into injury mechanisms. Am J Sports Med 2013; 41(2): 385–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Bales CP, Guettler JH, Moorman CT, III. Anterior cruciate ligament injuries in children with open physes: evolving strategies of treatment. Am J Sports Med 2004; 32(8): 1978–1985. [DOI] [PubMed] [Google Scholar]
- 53. Stanitski CL, Harvell JC, Fu F. Observations on acute knee hemarthrosis in children and adolescents. J Pediatr Orthop 1993; 13(4): 506–510. [DOI] [PubMed] [Google Scholar]
- 54. Yen YM. Assessment and treatment of knee pain in the child and adolescent athlete. Pediatr Clin North Am 2014; 61(6): 1155–1173. [DOI] [PubMed] [Google Scholar]
- 55. Marshall WA, Tanner JM. Variations in pattern of pubertal changes in girls. Arch Dis Child 1969; 44(235): 291–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Turati M, Rigamonti L, Zanchi N, et al. An arthroscopic repair technique for proximal anterior cruciate tears in children to restore active function and avoid growth disturbances. Knee Surg Sports Traumatol Arthrosc 2021; 29(11): 3689–3696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lee K, Siegel MJ, Lau DM, et al. Anterior cruciate ligament tears: MR imaging-based diagnosis in a pediatric population. Radiology 1999; 213(3): 697–704. [DOI] [PubMed] [Google Scholar]
- 58. Van Der List JP, Mintz DN, DiFelice GS. The locations of anterior cruciate ligament tears in pediatric and adolescent patients: a magnetic resonance study. J Pediatr Orthop 2019; 39(9): 441–448. [DOI] [PubMed] [Google Scholar]
- 59. Turati M, Rigamonti L, Giulivi A, et al. Management of anterior cruciate ligament tears in Tanner stage 1 and 2 children: a narrative review and treatment algorithm guided by ACL tear location. J Sports Med Phys Fitness. Epub ahead of print 5 October 2021. DOI: 10.23736/S0022-4707.21.12783-5. [DOI] [PubMed] [Google Scholar]
- 60. Zaricznyj B. Avulsion fracture of the tibial eminence: treatment by open reduction and pinning. J Bone Joint Surg Am 1977; 59(8): 1111–1114. [PubMed] [Google Scholar]
- 61. Piasecki DP, Spindler KP, Warren TA, et al. Intraarticular injuries associated with anterior cruciate ligament tear: findings at ligament reconstruction in high school and recreational athletes. An analysis of sex-based differences. Am J Sports Med 2003; 31(4): 601–605. [DOI] [PubMed] [Google Scholar]
- 62. Bordoni V, Di Laura Frattura G, Previtali D, et al. Bone bruise and anterior cruciate ligament tears: presence, distribution pattern, and associated lesions in the pediatric population. Am J Sports Med 2019; 47(13): 3181–3186. [DOI] [PubMed] [Google Scholar]
- 63. Snearly WN, Kaplan PA, Dussault RG. Lateral-compartment bone contusions in adolescents with intact anterior cruciate ligaments. Radiology 1996; 198(1): 205–208. [DOI] [PubMed] [Google Scholar]
- 64. Prince JS, Laor T, Bean JA. MRI of anterior cruciate ligament injuries and associated findings in the pediatric knee: changes with skeletal maturation. AJR Am J Roentgenol 2005; 185(3): 756–762. [DOI] [PubMed] [Google Scholar]
- 65. Heyworth BE, Osei DA, Fabricant PD, et al. The shorthand bone age assessment: a simpler alternative to current methods. J Pediatr Orthop 2013; 33(5): 569–574. [DOI] [PubMed] [Google Scholar]
- 66. Dimeglio A, Charles YP, Daures JP, et al. Accuracy of the Sauvegrain method in determining skeletal age during puberty. J Bone Joint Surg Am 2005; 87(8): 1689–1696. [DOI] [PubMed] [Google Scholar]
- 67. Nicholson AD, Sanders JO, Liu RW, et al. The relationship of calcaneal apophyseal ossification and Sanders hand scores to the timing of peak height velocity in adolescents. Bone Joint J 2015; 97-B(12): 1710–1717. [DOI] [PubMed] [Google Scholar]
- 68. Sanders JO, Khoury JG, Kishan S, et al. Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Joint Surg Am 2008; 90(3): 540–553. [DOI] [PubMed] [Google Scholar]
- 69. Pennock AT, Bomar JD, Manning JD. The creation and validation of a knee bone age atlas utilizing MRI. J Bone Joint Surg Am 2018; 100: e20. [DOI] [PubMed] [Google Scholar]
- 70. Shifflett GD, Green DW, Widmann RF, et al. Growth arrest following ACL reconstruction with hamstring autograft in skeletally immature patients: a review of 4 cases. J Pediatr Orthop 2016; 36(4): 355–361. [DOI] [PubMed] [Google Scholar]